Abstract
Objective
Group-based trajectory modeling holds promise for the study of mood disorders because the courses they follow are so highly variable. However, trajectory analyses of major depressive disorder have so far not included some of the more robust predictors of mood disorder outcome, nor have they described interactions between these predictors.
Method
A group of 186 individuals aged 15 to 20 years with past or current depressive symptoms, who had recently begun taking an SSRI antidepressant, underwent extensive baseline evaluations and were then followed for up to two years. Trajectory analyses used weekly ratings of depressive symptoms and the resulting groups were compared by the risk factors of sex, psychiatric comorbidity, negative emotionality, and childhood adversity.
Results
A three-group solution provided the best statistical fit to the two-year symptom trajectory. Negative emotionality and childhood adversity, though correlated, independently predicted membership in higher-morbidity groups. Female sex and comorbidity with generalized anxiety disorder (GAD) were also significantly more likely in the trajectory groups with higher symptom levels. However, the presence of GAD, rather than female sex, was the most important determinant of group membership. Negative emotionality was predictive of group membership only among women.
Conclusions
Childhood adversity and negative emotionality independently contribute to higher symptom levels. The greater likelihood of GAD co-occurrence in females may account for much of the widely observed relationship between female sex and depressive morbidity. Negative emotionality appears to be prognostically important among women rather than men.
Keywords: depressive symptoms, trajectory, adolescents, follow-up, childhood adversity
Introduction
The one-year prevalence of depressive disorders in U.S. adults is around 10% (Kessler et al., 2003), accounting for most of the years lived with disability of any illness (Ustun et al., 2004). While depressive disorders result in substantial impairment over time for many individuals, some individuals have only a few, discrete episodes. Numerous prospective studies have sought to categorize diverse courses of illness and to identify their clinical and biological correlates.
The metrics used to classify courses of illness have included likelihoods of, or times to, recovery, remission, and relapse, as well as morbidity indices derived from averages of symptom levels over a period of observation. However, none of these measures adequately captures temporal trends. One individual might recover within a few weeks and then relapse into a chronic episode, and another might recover many months after an episode’s onset but then remain well for an extended period. The individuals in either case might differ markedly in average symptom levels as reflected in a morbidity index but such a number would not adequately describe the disparate courses over time.
These problems are, of course, not unique to mood disorders and, in aggregate, they account for an increasing interest in trajectory analyses (Nagin and Odgers, 2010). Such approaches provide person-centered perspectives that identify subgroups based on common patterns in longitudinal observations (Shore et al., 2018). Trajectory analyses of mood disorders in adolescents are particularly important because this age group encompasses the years of onset for a substantial proportion of individuals who experience mood disorders.
A recent meta-analysis of trajectory studies described 20 prospective follow-up studies with identified trajectories that ranged in number from three to eleven (Shore et al., 2018). To summarize the findings of risks factors that distinguished between trajectories, the authors subsumed the symptom patterns in these studies into three groups: “low”, “moderate”, and “high or increasing”. Female sex was more often associated with the highest symptom trajectory. At least four studies found low SES, substance abuse, or a “negative parental relationship” to be also significantly more characteristic of the highest symptom trajectory.
Notably, this meta-analysis did not examine childhood trauma. Yet, childhood trauma is firmly established as a risk factor for later development of depressive disorders, particularly those characterized by early onset, chronicity, and treatment resistance (Nelson et al., 2017, Barnhofer et al., 2014). Childhood trauma also increases the likelihood of anxiety disorders to at least the same degree as it does of depressive disorders (Li et al., 2016) and is also associated with high levels of neuroticism (Hengartner et al., 2015). Both anxiety disorders (Coryell et al., 2009, Newman et al., 2013, Coryell et al., 2012) and neuroticism (Coryell et al., 2017) are, in turn, well established risk factors for symptom persistence in depressive disorders. However, efforts to describe interactions between anxiety disorders and neuroticism on the course of depressive illness are scarce and we are aware of no studies that do so in a trajectory analysis.
With this in mind, the following describes a trajectory analysis of depressive symptoms in a cohort of individuals in late adolescence and tests the relationships between the resulting groupings and the variables of sex, childhood adversity, negative emotionality, and anxiety. We endeavor to assess the degree to which each makes independent contributions to the course of depressive morbidity.
Methods
Participants
As part of a study designed to examine the effects of selective serotonin reuptake inhibitors (SSRIs) on bone metabolism in adolescents and emerging adults, individuals 15 to 20 years of age were recruited from inpatient and outpatient settings, and through e-mail solicitations, to comprise two groups.(Calarge et al., 2014, Calarge et al., 2017) Those in one were taking no psychotropic medications and those in the other had begun taking an SSRI within the previous month. Treatment with psychotropics, other than SSRIs, during the two years prior to study entry resulted in exclusion, with the exception of the use of benzodiazepines, trazodone, α2‐ agonists, or a stable dose of psychostimulants. Also excluded were individuals with an eating disorder, substance dependence, pregnancy, significant medical or surgical history, chronic use of medications potentially affecting bone metabolism, or with plans to move out of state within a year.
The local Institutional Review Board approved the study and adult participants provided written informed consent. The parent/guardian of minor participants provided written informed consent while the minors gave written assent to the study.
As the presence of a mood disorder was not a requirement for either group, the current analyses were restricted to participants who had ever met criteria for a major depressive disorder (MDD) or who endorsed depressive symptoms at study entry, including among those who were naive to psychotropic medications (n= 186).
Procedures
Experienced research coordinators collected demographic and clinical data in an initial interview that included the NIMH Diagnostic Interview Schedule for Children (DISC-IV)(Shaffer et al 2000)(Shaffer et al., 2000) as well as an unstructured interview by a child psychiatrist (CAC). Consensus diagnoses were generated based on the structured interview, an unstructured assessment, and information from self-completed symptom rating scales. Parents of minors were also interviewed.
The intake assessment included the Early Trauma Inventory - Self Report (ETISR).(Bremner et al., 2007) This is a 19-item questionnaire that covers general adverse life events that occurred before the age of 18 and that includes scores for physical, sexual, and emotional abuse, as well as a total score. Participants also completed the Multidimensional Personality Questionnaire (MPQ) (Patrick et al., 2002) at their first follow-up visit. This is a factor-analytically derived inventory of personality that generates 11 primary scales. These load, in turn, on three higher- order factors: positive emotionality (wellbeing, social potency, social closeness, and achievement), negative emotionality (stress reaction, alienation and aggression), and constraint (control, harm avoidance and traditionalism). The negative emotionality measure has been shown to strongly correlate with the NEO Personality Inventory dimension of neuroticism (McCrae and Costa, 1987, Church, 1994). Some attrition occurred between the first visit and the first follow-up so the number of individuals with MPQ data is smaller.
Face-to-face visits occurred at four-month intervals over the subsequent two years. The symptom status of the disorder considered to be primary at the initial evaluation was also monitored with monthly telephone calls to the participants. Interviewers guided individuals to identify any change points in levels of psychopathology that had taken place since the last interview. Participants then quantified the number of symptoms present between those change points and results were recorded according to conventions in the A-LIFE (Calarge et al., 2014), a modification of the Longitudinal Interval Follow-up Evaluation (LIFE) (Keller et al., 1987) that includes additional disorders more commonly seen in youth. This yielded symptom level ratings for each disorder during each week of follow-up interval on a scale of 1 to 6 for MDD and generalized anxiety disorder (GAD). The time period for this coverage included the four months preceding the initial face-to-face interview.
Statistical Methods
Participants’ weekly MDD symptom levels from the A-LIFE were analyzed using group-based trajectory modeling (GBTM), a statistical method used to find clusters of individuals following similar patterns of progression over time (Nagin and Odgers, 2010). Models with 2, 3, and 4 groups were generated using the censored normal distribution and the polynomial function of time (linear, quadratic, or cubic) that best fit the data. In each model individuals were assigned to the group where the GBTM-determined probability of membership was highest. The choice of best fitting model was informed by model fit indices (Akaike, 1974) and ultimately made by maximizing the number of non-redundant MDD patterns. The GBTM analysis was conducted using PROC TRAJ in SAS 9.4 (Jones et al., 2001).
Baseline characteristics of the three trajectory groups were then compared using chi-square tests for categorical variables and ANOVA models for continuous variables. Group differences for ETISR (from baseline) and MPQ (from the first follow up visit) scores were also examined using ANOVA models. An ordinal logistic regression model assessed the relationship of the GTBM groups with multiple predictors (sex, total ETISR, negative emotionality, and GAD) and all possible 2-way interaction effects.
Results
A three-group trajectory model offered the best statistical fit (Figure 1) regardless of whether linear, quadratic, or cubic modeling was used. Symptom levels in the first group began at a relatively low level and declined somewhat over time. The second group began at high symptom levels but then decreased markedly such that the depression ratings resembled those of the first group by the end of follow-up. This pattern is consistent with a remitting depressive episode. The last group began at a high symptom level and showed minimal decline over time, suggestive of a chronic, persistent course. Accordingly, we assigned the descriptors of “Low”, “Remitting”, and “Persistent” to the three groups.
Figure 1 -.
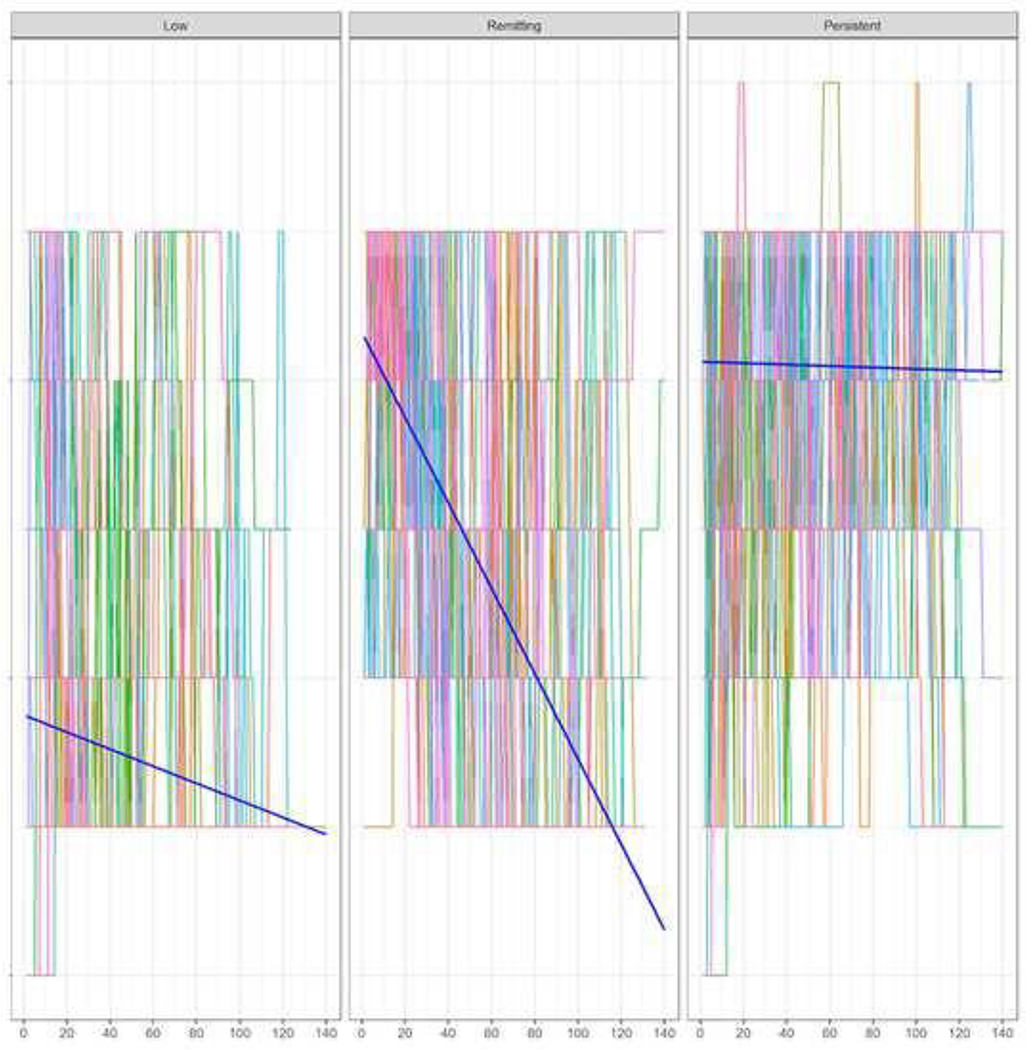
Observed A-Life Depression Scores by Trajectory Group Across Weekly Follow-up
The proportion of females increased in a stepwise fashion with increasing morbidity across the groups, as did the likelihood of the presence of GAD (Table 1). Negative emotionality, and each of the ETISR childhood adversity scores, showed equivalent stepwise increases across the three groups such that NE and ETISR scores were highest in the “Persistent” group (Table 2). Positive emotionality decreased progressively across the groups while constraint did not vary significantly.
Table 1.
Baseline Demographic and Clinical Characteristics of the Participants Divided in Three Trajectory Groups
| Low | Remitting | Persistent | |
|---|---|---|---|
| n=58 | n=69 | n=59 | |
| Female sex, n (%) 1 | 32 (55.2) | 43 (62.3) | 50 (84.7) |
| Age, years, mean (SD) | 18.9 (1.6) | 18.9 (1.7) | 19.0 (1.6) |
| SSRI, n (%) 2 | 21 (36.2) | 57 (82.6) | 41 (69.5) |
| History of suicide attempt, n (%) | 0 | 5 (7.2) | 5 (8.5) |
| GAD, n (%) 3 | 10 (17.2) | 27 (39.1) | 29 (49.2) |
| Alcohol use disorder, n (%) | 5 (8.6) | 13 (19.1) | 14 (23.7) |
| Cannabis use disorder, n (%) | 6 (10.3) | 9 (13.0) | 7 (11.9) |
| Social phobia, n (%) | 15 (25.9) | 20 (29.0) | 24 (40.7) |
| ADHD, n (%) | 6 (10.3) | 8 (11.6) | 8 (13.6) |
| Mean (SD) scores | |||
| Beck Depression Inventory4 | 6.7 (6.7) | 17.6 (9.8) | 18.6 (10.7) |
| Beck Anxiety Inventory5 | 6.7 (7.2) | 12.4 (10.4) | 12.8 (7.7) |
| Inventory of Depressive | 10.0 (7.0) | 20.6 (9.0) | 21.5 (10.4) |
| Symptomatology |
X2 = 12.8, p = .002; 2<3, X2 = .0, p = 0.005; 1<3, X2 = 12.2, p = .000
X2 = 30.6, p = .000; 1<2, X2 = 28.6, p = .000; 1<3, X2 = 13.0, p = .000
X2 = 13.6, p = 0.001; 1<2, X2 = 5.6, p = .014; 1<3, X2 = 13.0, p = .000
F = 30.4, p = 0.000; Bonferroni: 1<2, p = .000; 1<3, p = .000
F = 9.1, p = .000; Bonferroni: 1<2, p = .001; 1<3, p = .001
F = 31.0, p = .000; Bonferroni: 1<2, p = .000; 1<3, p = .000
SSRI: selective serotonin reuptake inhibitor use at study entry, GAD: generalized anxiety disorder ADHD: attention deficit hyperactivity disorder
Table 2.
Measures of Temperament and Childhood Adversity for the Participants Divided in Three Trajectory groups, mean (SD)
| Low | Remitting | Persistent | |
|---|---|---|---|
| MPQ Temperament | |||
| Scores, n | 55 | 56 | 51 |
| Positive Emotionality 1 | 74.8 (13.9) | 72.4 (12.7) | 64.7 (14.4) |
| Negative Emotionality 2 | 34.4 (15.0) | 40.9 (14.5) | 44.0 (17.0) |
| Constraint | 71.8 (13.8) | 72.9 (13.2) | 74.9 (14.6) |
| ETISR scores, n | 55 | 62 | 54 |
| General | 1.9 (1.6) | 2.0 (1.9) | 2.4 (2.1) |
| Physical 3 | 0.6 (0.6) | 1.2 (1.5) | 1.4 (1.4) |
| Emotional 4 | 0.9 (1.3) | 1.2 (1.5) | 1.6 (1.6) |
| Sexual | 0.3 (1.0) | 0.4 (1.0) | 0.4 (1.1) |
| Total 5 | 3.7 (3.6) | 4.8 (3.8) | 5.9 (4.4) |
F = 7.9, p = 0.001; Bonferroni: 1<3, p = 0.001; 2<3, p = 0.012
F = 5.3, p = 0.006; Bonferroni: 1<3, p = 0.005
F = 4.0, p = 0.019; Bonferroni: 1<3, p = 0.021
F = 3.4, p = 0.037; Bonferroni: 1<3, p = .032
F = 4.1, p = 0.019; Bonferroni: 1<3, p = .015
MPQ: Multidimensional personality questionnaire from the first follow up visit, ETISR: early trauma inventory – self-report from baseline visit.
To simplify subsequent analyses, we selected the total ETISR score to represent childhood adversity and focused on negative emotionality from among the three measures of temperament. Females were somewhat more likely than males to have a diagnosis of GAD (50/125 or 40.0% and 16/61 or 26.2%, respectively, X2 = 3.4, df = 1, p = 0.065) but the sexes did not differ by total ETISR or NE scores. Nor did those who had a GAD diagnosis differ significantly from those without it, either by total ETISR or by NE scores. Of note, the ETISR and NE scores were significantly correlated (Spearman’s r= 0.25, p = 0.002).
A non-significant (p=0.133) test of parallel lines justified the use of ordinal logistic regression. Using this, each of these four variables was significantly related to trajectory groupings (Table 3). The presence of a GAD diagnosis was by far the variable most robustly related to trajectory groupings. Moreover, a GAD diagnosis was also more important in predicting symptom trajectory grouping than was anxiety measured in cross-section. The addition of the baseline BAI score to the model had little effect on the strength of the relationship between the presence of GAD and group membership (OR=3.48, 95% CI=0.59,1.90, X2=13.8, p=.000). The relationship of BAI score to group membership when included in the model did not reach significance (OR=1.04, 95% CI=0.00,0.07, X2=3.3, p=0.067).
Table 3.
Trajectory Groupings: Risk Factors in Ordinal Logistic Regression
| OR (95% CI) | X 2 | p | |
|---|---|---|---|
| Sex | 2.23 (1.1, 4.4) | 5.5 | 0.019 |
| Negative emotionality | 1.03 (1.01, 1.05) | 6.6 | 0.010 |
| Total ETISR score | 1.09 (1.00, 1.18) | 4.1 | 0.044 |
| GAD | 3.65 (1.9, 7.02) | 15.2 | 0.000 |
Of the six possible interaction effects between these four variables only the sex by NE interaction effect was significant (X2 = 5.8, p = 0.016). Further exploration revealed that the relationship between NE and trajectory grouping existed for females but not for males. Specifically, for females, mean (SD) NE scores were 31.5 (15.4), 42.6 (16.1) and 44.9 (15.9) across the three trajectory groups (F= 6.9, p = 0.002). In contrast, for males, the corresponding mean (SD) values were 37.8 (15.4), 38.0 (11.2) and 38.5 (23.5), respectively (F=1.3, p=0.994).
Discussion
The most consistent finding among studies of depressive symptom trajectories is the association of female sex with higher levels of morbidity (Shore et al., 2018). The present results are in full accord with the predicted pattern in showing a progressively higher percent of women across the three groups. The likelihood of GAD comorbidity also increased across trajectory groups in order of increasing depressive symptom morbidity (Brown et al., 1998). The novel finding in this report is that the presence of GAD was a stronger predictor of high morbidity group membership than was female sex while controlling for negative emotionality.
Twin studies show that genetic diatheses for GAD and MDD overlap substantially (Kendler et al., 1992) and this may account for the observation that GAD is the most likely of the DSM disorders to co-exist, either sequentially or concurrently, with MDD (Moffitt et al., 2007) . Both GAD and MDD are associated with disability but the disability is substantially higher when the two disorders occur together (Kessler et al., 2002). The importance of GAD to the persistence of MDD symptoms over time helps to explain observations that the prognosis of mood disorders worsens progressively with increasing levels of anxiety symptoms, whatever the quality of those symptoms (Coryell et al., 2012, Coryell et al., 2009). However, most earlier studies of the prognostic importance of anxiety to mood disorder outcome used either an anxiety diagnosis or a measure of those anxiety symptoms present at the time of interview. They did not test whether diagnosis or a cross-sectional measure was the more important for prognosis. The findings described here suggest that the diagnosis of GAD is the stronger predictor of morbidity, perhaps because it requires a persistence of symptoms of at least six months.
Of six possible interaction effects between the four risk factors tested in this analysis, only the one between sex and NE was significant. This personality measure was robustly associated with trajectories of higher symptom morbidity in women but had little relation to these groupings in men. These results are consistent with findings from a large twin study in which neuroticism was over 30% more potent as a risk factor for the development of MDD in women than it was in men (Kendler and Gardner, 2014). Also in support of these results are those of a large community-based study in which the inclusion of neuroticism in a regression model substantially reduced the relationship between female sex and the diagnosis of major depression (Goodwin and Gotlib, 2004).
An earlier publication from this cohort assessed the relationships between mean symptom levels over the first year of follow-up and baseline measures of erythrocyte concentrations of eicosapentaenoic acid (EPA), an omega-3 essential fatty acid, negative emotionality and childhood adversity (Coryell et al., 2017). Both EPA concentrations and ETISR emotional adversity scores were independently predictive of morbidity during follow-up but both exerted these effects largely through their influence on NE. In the current analysis, both ETISR scores and NE were again predictive of depressive morbidity, this time expressed as depressive symptom trajectories assumed over a two-year prospective follow-up. With this new measure of depressive chronicity, however, NE and childhood adversity, though significantly correlated with each other, were independently related to trajectory groupings reflecting higher symptom levels.
Weaknesses attached to these analyses include the fact that they were secondary in nature. Participants were recruited to examine the effects of recently initiated SSRI treatment on bone density in a late adolescent population. This study was not powered by design to test the hypothesis addressed here. In particular, additional interactions between risk factors for high morbidity trajectories may have manifested had the sample been larger. The age range of the participants was also quite limited and the sample was heavily skewed toward college students, a reflection of the study’s setting. This, in turn, limited the range of socioeconomic status and, possibly, childhood adversity. Findings may not generalize well to other sociodemographic groups.
Among the study’s strengths is the breadth of baseline assessments. These extended well beyond what was necessary to test the original hypotheses. The surveillance intensity of the prospective follow-up comprised another strength. Few follow-up studies have employed triannual, in-person visits supplemented with intervening telephone assessments of the disorder considered primary at intake. As such these findings invite particular attention to interactions between sex, sustained symptoms of anxiety and negative emotionality as they affect the course of depressive illness.
Financial Support
This research received support from the National Center for Advancing Translational Sciences (2UL1TR000442-06) and the National Institute of Mental Health (R01MH090072).
Footnotes
Conflict of Interest
None.
References
- AKAIKE H 1974. A new look at the statistical model identification. IEEE Transactions on Automatic Control, 19, 716–723. [Google Scholar]
- BARNHOFER T, BRENNAN K, CRANE C, DUGGAN D & WILLIAMS JM 2014. A comparison of vulnerability factors in patients with persistent and remitting lifetime symptom course of depression. J Affect Disord, 152-154, 155–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BREMNER JD, BOLUS R & MAYER EA 2007. Psychometric properties of the Early Trauma Inventory- Self Report. J Nerv Ment Dis, 195, 211–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BROWN TA, CHORPITA BF & BARLOW DH 1998. Structural relationships among dimensions of the DSM-IV anxiety and mood disorders and dimensions of negative affect, positive affect, and autonomic arousal. J Abnorm Psychol, 107, 179–92. [DOI] [PubMed] [Google Scholar]
- CALARGE CA, BUTCHER BD, BURNS TL, CORYELL WH, SCHLECHTE JA & ZEMEL BS 2014. Major depressive disorder and bone mass in adolescents and young adults. J Bone Miner Res, 29, 2230–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CALARGE CA, MILLS JA, JANZ KF, BURNS TL, SCHLECHTE JA, CORYELL WH & ZEMEL BS 2017. The Effect of Depression, Generalized Anxiety, and Selective Serotonin Reuptake Inhibitors on Change in Bone Metabolism in Adolescents and Emerging Adults. J Bone Miner Res, 32, 2367–2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CHURCH AT 1994. Relating the Tellegen and five-factor models of personality structure. J Pers Soc Psychol, 67, 898–909. [DOI] [PubMed] [Google Scholar]
- CORYELL W, FIEDOROWICZ JG, SOLOMON D, LEON AC, RICE JP & KELLER MB 2012. Effects of anxiety on the long-term course of depressive disorders. Br J Psychiatry, 200, 210–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CORYELL W, SOLOMON DA, FIEDOROWICZ JG, ENDICOTT J, SCHETTLER PJ & JUDD LL 2009. Anxiety and outcome in bipolar disorder. Am J Psychiatry, 166, 1238–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CORYELL WH, LANGBEHN DR, NORRIS AW, YAO JR, DINDO LN & CALARGE CA 2017. Polyunsaturated fatty acid composition and childhood adversity: Independent correlates of depressive symptom persistence. Psychiatry Res, 256, 305–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- GOODWIN RD & GOTLIB IH 2004. Gender differences in depression: the role of personality factors. Psychiatry Res, 126, 135–42. [DOI] [PubMed] [Google Scholar]
- HENGARTNER MP, COHEN LJ, RODGERS S, MULLER M, ROSSLER W & AJDACIC-GROSS V 2015. Association between childhood maltreatment and normal adult personality traits: exploration of an understudied field. J Pers Disord, 29, 1–14. [DOI] [PubMed] [Google Scholar]
- JONES BL, NAGIN DS & ROEDER K 2001. A SAS procedure based on mixture models for estimating developmental trajectories. Sociological Methods & Research, 29, 374–393. [Google Scholar]
- KELLER MB, LAVORI PW, FRIEDMAN B, NIELSEN E, ENDICOTT J, MCDONALD-SCOTT P & ANDREASEN NC 1987. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch Gen Psychiatry, 44, 540–8. [DOI] [PubMed] [Google Scholar]
- KENDLER KS & GARDNER CO 2014. Sex differences in the pathways to major depression: a study of opposite-sex twin pairs. Am J Psychiatry, 171, 426–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KENDLER KS, NEALE MC, KESSLER RC, HEATH AC & EAVES LJ 1992. Major depression and generalized anxiety disorder. Same genes, (partly) different environments? Arch Gen Psychiatry, 49, 716–22. [DOI] [PubMed] [Google Scholar]
- KESSLER RC, BERGLUND P, DEMLER O, JIN R, KORETZ D, MERIKANGAS KR, RUSH AJ, WALTERS EE, WANG PS & NATIONAL COMORBIDITY SURVEY R 2003. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA, 289, 3095–105. [DOI] [PubMed] [Google Scholar]
- KESSLER RC, BERGLUND PA, DEWIT DJ, USTUN TB, WANG PS & WITTCHEN HU 2002. Distinguishing generalized anxiety disorder from major depression: prevalence and impairment from current pure and comorbid disorders in the US and Ontario. Int J Methods Psychiatr Res, 11, 99–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LI M, D’ARCY C & MENG X 2016. Maltreatment in childhood substantially increases the risk of adult depression and anxiety in prospective cohort studies: systematic review, meta-analysis, and proportional attributable fractions. Psychol Med, 46, 717–30. [DOI] [PubMed] [Google Scholar]
- MCCRAE RR & COSTA PT JR. 1987. Validation of the five-factor model of personality across instruments and observers. J Pers Soc Psychol, 52, 81–90. [DOI] [PubMed] [Google Scholar]
- MOFFITT TE, CASPI A, HARRINGTON H, MILNE BJ, MELCHIOR M, GOLDBERG D & POULTON R 2007. Generalized anxiety disorder and depression: childhood risk factors in a birth cohort followed to age 32. Psychol Med, 37, 441–52. [DOI] [PubMed] [Google Scholar]
- NAGIN DS & ODGERS CL 2010. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol, 6, 109–38. [DOI] [PubMed] [Google Scholar]
- NELSON J, KLUMPARENDT A, DOEBLER P & EHRING T 2017. Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry, 210, 96–104. [DOI] [PubMed] [Google Scholar]
- NEWMAN MG, LLERA SJ, ERICKSON TM, PRZEWORSKI A & CASTONGUAY LG 2013. Worry and generalized anxiety disorder: a review and theoretical synthesis of evidence on nature, etiology, mechanisms, and treatment. Annu Rev Clin Psychol, 9, 275–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PATRICK CJ, CURTIN JJ & TELLEGEN A 2002. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychol Assess, 14, 150–63. [DOI] [PubMed] [Google Scholar]
- SHAFFER D, FISHER P, LUCAS CP, DULCAN MK & SCHWAB-STONE ME 2000. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): description, differences from previous versions, and reliability of some common diagnos es. J Am Acad Child Adolesc Psychiatry, 39, 28–38. [DOI] [PubMed] [Google Scholar]
- SHORE L, TOUMBOUROU JW, LEWIS AJ & KREMER P 2018. Review: Longitudinal trajectories of child and adolescent depressive symptoms and their predictors - a systematic review and meta- analysis. Child and Adolescent Mental Health, 23, 107–120. [DOI] [PubMed] [Google Scholar]
- USTUN TB, AYUSO-MATEOS JL, CHATTERJI S, MATHERS C & MURRAY CJ 2004. Global burden of depressive disorders in the year 2000. Br J Psychiatry, 184, 386–92. [DOI] [PubMed] [Google Scholar]


