Abstract
Background:
The hypertensive crisis is characterized by poorly controlled hypertension, which can lead to unfavorable outcomes and high utilization. The purpose of this study was to examine the prevalence, clinical characteristics, and factors associated with hypertensive emergency.
Material and Methods:
This cross-sectional study collected data from the hospital information system that included patients greater than or equal to 18 years who were diagnosed with hypertensive crisis (blood pressure ≥180 and/or 120 mmHg) and receiving care from the primary care unit and emergency department from 2020 to 2022. The prevalence and clinical characteristics of these patients were examined. Multiple logistic regression analysis was used to analyze factors associated with hypertensive emergency.
Results:
Among 3329 patients with hypertension, 17.33% had a hypertensive crisis (16.64 vs. 0.69%, urgency and emergency types). Most patients were female (63.6%), with a median age of 66 years. Almost half the patients (42.2%) with hypertensive crisis presented without specific symptoms, and the most common presenting symptom was vertigo/dizziness (27.7%). The initial and after treatment blood pressures were 203/98 and 174/91 mmHg. In the hypertensive emergency, the most common end-organ damage was ischemic stroke (33.3%), hemorrhagic stroke (25%), and acute heart failure (20.8%). An oral angiotensin-converting enzyme (57.5%) was the most commonly administered medication. Multiple logistic regression was performed but did not reveal any statistically significant.
Conclusion:
Our result revealed a high prevalence of hypertensive crises; most were of hypertensive urgency. The most common presenting symptom was vertigo/dizziness. There was no factor significantly associated with the hypertensive emergency in this study. Further studies should explore the cause of the hypertensive crisis to improve care delivery to patients with hypertension.
Keywords: hypertension, hypertensive crisis, hypertensive emergency, hypertensive urgency
Introduction
Highlights
Our study is one of the few studies, especially in Southeast Asia, that explored the prevalence, clinical characteristics, and risk factors of hypertensive crises. Our findings may provide insights on the prevention of hypertensive crisis, which may lead to decreased morbidity and mortality in the future. Moreover, this research studied patients in two settings, ER and the primary care unit, showing differences in the characteristics of patients between both groups.
Our results revealed a relatively high prevalence of hypertensive crises. Furthermore, the majority of cases had hypertensive urgency, and we suggest that further studies should explore the causes of hypertensive crisis to improve the care of hypertensive patients.
Hypertension is a common chronic disease, affecting 1 billion people worldwide in 20201. The number of deaths involving hypertension and related cardiovascular complications in low- and middle-income countries has been rising to over 80%, and the prevalence of hypertension is predicted to reach more than 29% globally by 20252.
Despite receiving antihypertensive drugs, patients with uncontrolled hypertension are more likely to develop damage to the heart, brain, and kidneys than others. Hypertensive crisis, a serious condition characterized by poorly controlled hypertension3, was defined as systolic blood pressure (SBP) greater than or equal to 180 and/or diastolic blood pressure (DBP) greater than or equal to 120 mmHg4,5. It is classified into two types, hypertensive emergency or hypertensive urgency, depending on the evidence of end-organ damage (EOD). Hypertensive emergency is severe hypertension with evidence of EOD, whereas hypertensive urgency is severe hypertension without evidence of EOD. It can occur de novo in patients without any known history of hypertension and develop in patients with uncontrolled hypertension6.
The prevalence of hypertensive crisis is increasing and varies depending on the country and region7. Hypertensive emergencies increased from 3309 per million cases in 2006 to 6178 per million cases in 20136. Gebresillassie et al.1 revealed that ~1% of patients with hypertension may develop a hypertensive crisis at some point in their lives. Hypertensive crises (76% urgencies, 24% emergencies) presented 25% of all medical conditions in emergency departments8. Hypertensive emergencies increase the risk of morbidity, mortality, and hospitalization3,9. The treatment of hypertensive emergencies requires rapid blood pressure control with the administration of intravenous antihypertensive medications to avoid further EOD or deterioration. However, in severe hypertensive emergencies, admission to the ICU is recommended for frequent BP monitoring3,6. Patients with hypertensive urgency can be treated with oral antihypertensive drugs2.
Understanding the risk factors for hypertensive crisis is the first step in improving care delivery to patients with hypertension while reducing the healthcare burden3. However, few studies have investigated hypertensive crises’ prevalence, clinical characteristics, and risk factors, especially in Southeast Asia. Moreover, most of previous studies on hypertensive crisis took place in emergency settings, and data from primary care was currently limited. Therefore, this study aimed to assess the prevalence, clinical characteristics, and risk factors of patients with hypertensive crisis receiving care in the primary care unit (PCU) and emergency department (ER) at a tertiary hospital. Ultimately, the researchers hope that the results of this study could be applied to patients with hypertension and improve the prevention of hypertensive crisis, which may lead to decreased morbidity and mortality in the future.
Material and methods
Study setting, design, and population
This cross-sectional study collected secondary data from hospital information systems that included patients greater than or equal to 18 years who were diagnosed with hypertensive crisis (BP ≥180 and/or 120 mmHg) and receiving care from the PCU or ER at a tertiary care university hospital, from 2020 to 2022. The research was reported in line with the STROCCS checklist10 and registered at www.researchregistry.com, with Research Registry UIN: researchregistry. Ethical approval was obtained from the Institutional Review Board (REC.65-519-9-1).
The primary objective of this research was to explore the prevalence of hypertensive crises. The sample size was calculated using an infinite proportion formula referenced from Frederick A. Waldron et al.11 (2019) for the prevalence of hypertensive crisis. We assigned the proportions, errors, and alpha values of 0.114, 0.05, and 0.05, respectively. The study sample size was 156 patients.
The secondary objective was to determine the clinical characteristics of patients experiencing hypertensive crisis. The sample size was calculated using the infinite proportion formula. As there was no previous information on the proportion of clinical characteristics, we assigned the values of proportion, error, and alpha as 0.5, 0.05, and 0.05, respectively. The sample size was 385 patients (Fig. 1).
Figure 1.

Infinite proportion formula.
The third objective was to assess the risk factors of hypertensive emergencies. The sample size was calculated using logistic regression using the G-power program (Desta et al., 2020). According to Desta et al.12, the female sex [adjusted odds ratio (AOR) 2.494; 95% CI: 1.11–5.59) was found to be independently associated factors with a hypertensive emergency. Therefore, we assigned type 1 error and power 0.05 and 0.8, respectively. The sample size was 178 patients. Thus, the total number of participants was 385 patients.
Eligibility criteria and operational definitions
Patients with hypertension aged greater than or equal to 18 years who presented with a hypertensive crisis (SBP ≥180 and/or DBP ≥120 mmHg) and had complete medical records were included. However, patients who were transferred to other hospitals to complete the treatment of hypertensive crisis, were diagnosed with secondary hypertension, were pregnant, or had incomplete medical records of blood pressure before and after treatment were excluded. They were classified into two types: hypertensive urgency is characterized by a sudden increase in blood pressure without evidence of EOD, whereas hypertensive emergency is a severe life-threatening condition presenting evidence of vital organ damage, such as in the brain, heart, kidney, and eyes.
Data collection
The research teams requested hospital numbers for patients with hypertension during the study period from the Division of Digital Innovation and Data Analytics. Electronic case record forms were used to collect information, such as patient’s age, sex, BMI, clinical presentation, history of smoking and alcohol drinking, underlying disease (diabetes mellitus (E11), dyslipidemia (E780-E785), hypertension (I10), stroke (I64, I694), coronary artery disease (I210-214, I219, I220, I 221, I228, I229), heart failure (I50), chronic kidney disease (N18, N189), drug compliance, SBP and DBP on the date of visit, number of recurrences of hypertensive crisis, investigation; blood urea nitrogen, creatinine, complete blood count, electrolyte, urinalysis, electrocardiogram, chest radiography, brain imaging, cardiac biomarkers, an antihypertensive drug used to treat, status after treatment, EOD, such as ischemic stroke (I64, I694), AKI (N171-179) and acute myocardial infarction (I210-214, I219-I 221, I228-229). To ensure content validity, three experts, including one emergency physician and two family physicians (all item-objective congruence=1), were assigned to review and validate the case record form. The research team members were instructed to ensure the standardization of data recording. Data were imported into a computer using Microsoft Excel 365 version 2301. This study was conducted using secondary data from Hospital Information Systems (HIS). It could be abstaining the informed consent.
Data analysis
Data analysis was performed using R software version 4.1.3. The prevalence of hypertensive urgency and emergencies was calculated based on the total number of patients who visited the ER and PCU during the study period. Descriptive statistics were performed using the number, percentage, mean, SD, or median with the first and third quartile. Multiple logistic regression was used to analyze factors associated with hypertensive emergencies. We selected these variables from a literature review. Odds ratios, AOR, and 95% CI were calculated, and variables with P<0.05 were considered statistically significant.
Results
First, 3450 patients with hypertension who received care in the PCU and emergency department during a 3-year period were included. Subsequently, 121 were excluded based on the exclusion criteria. Thus, 3329 patients with hypertension receiving care from the ED and PCU at a tertiary care university hospital during the 3-year study period (2020–2022) were enrolled in this study. Among the 3329 patients with hypertension, 17.3% (577 of 3329) have hypertensive crisis, 0.7% (23 of 3329) were of the emergency type, and 16.6% (554 of 3329) were of the urgency type (Fig. 2).
Figure 2.

Flowchart of participant enrollment during the 3-year study period.
Among the 577 participants with hypertensive crisis, 367 were females, and 210 were males. Among these samples, 489 participants (84.7%) were from the ED and 88 (15.3%) were from the PCU. The median patient age was 66 years. The median SBP and DBP were 203 and 98 mmHg, respectively. The median BMI was 24.77 kg/m2. There were 472 participants (81.8%) that had previously been diagnosed with hypertension: 397 (81.2%) in the ED and 75 (85.2%) in the PCU. Other underlying diseases included dyslipidemia (45.1%), DM (30.3%), and CKD (14.4%). There were 185 (66.5%) participants who had poor drug compliance’s behavior. Most of them never experienced the recurrence of a hypertensive crisis, smoked, or consumed alcohol (Table 1).
Table 1.
Baseline characteristics of participants, n=577 patients.
| Variables | Emergency department (n=489) | Primary care Unit (n=88) | Total (n=577) | P |
|---|---|---|---|---|
| Sex, n (%) | 0.070a | |||
| Male | 186 (38) | 24 (27.3) | 210 (36.4) | |
| Female | 303 (62) | 64 (72.7) | 367 (63.6) | |
| Age (year), Median (Q1, Q3) | 65 (56, 76) | 70 (61, 70) | 66 (56, 77) | 0.019b |
| Blood pressure (mmHg) | ||||
| SBP, Median (Q1, Q3) | 205 (192, 217) | 190 (185, 200) | 203 (191, 215) | <0.001b |
| DBP, Median (Q1, Q3) | 99 (52, 163) | 94 (58, 140) | 98 (52, 163) | <0.001d |
| BMI (kg/m2), Median (Q1, Q3) | 24.75 (22.1, 28.1) | 24.80 (22.6, 28.1) | 24.77 (22.3, 28.1) | 0.607b |
| Underlying disease, n (%) | ||||
| Hypertension | 397 (81.2) | 75 (85.2) | 472 (81.8) | 0.451a |
| Dyslipidemia | 202 (41.3) | 58 (65.9) | 260 (45.1) | <0.001a |
| DM | 141 (28.8) | 34 (38.6) | 175 (30.3) | 0.086a |
| CKD | 76 (15.5) | 7 (7.9) | 83 (14.4) | 0.089a |
| Coronary artery disease | 44 (9.0) | 3 (3.4) | 47 (8.2) | 0.121a |
| Ischemic stroke | 30 (6.1) | 1 (1.1) | 31 (5.4) | 0.069c |
| Hemorrhagic stroke | 5 (1.0) | 1 (1.1) | 6 (1.0) | 1.000c |
| Heart failure | 4 (0.8) | 0 (0) | 4 (0.7) | 1.000c |
| No | 87 (17.8) | 13 (14.8) | 100 (17.3) | 0.592a |
| Drug compliance, n (%) | 0.07a | |||
| Regular | 64 (30.3) | 29 (43.3) | 93 (33.5) | |
| Not regular | 147 (69.7) | 38 (56.7) | 185 (66.5) | |
| Recurrence of HT crisis, n (%) | <0.001a | |||
| Yes | 52 (10.6) | 25 (28.4) | 77 (13.3) | |
| No | 437 (89.4) | 63 (71.6) | 500 (86.7) | |
| Smoking, n (%) | 0.943a | |||
| Current | 25 (8.8) | 4 (7.4) | 29 (8.6) | |
| Ex-smoker | 25 (8.8) | 5 (9.3) | 30 (8.9) | |
| Never | 234 (82.4) | 45 (83.3) | 279 (82.5) | |
| Alcohol Drinking, n (%) | 0.723c | |||
| Current | 29 (11.4) | 6 (12.5) | 35 (11.5) | |
| Ex-drinker | 21 (8.2) | 2 (4.2) | 23 (7.5) | |
| Never | 205 (80.4) | 40 (83.3) | 245 (80.9) | |
Data are expressed as median (Q1, Q3) or number (%).
χ 2test.
Mann–Whitney U test.
Fisher’s exact test.
T test; n, number of patients.
CKD, chronic kidney disease; DBP, diastolic blood pressure; DM, diabetes mellitus; HT, hypertension; kg, kilogram; m, meter; Q1, 1st quartile; Q3, 3rd quartile; mmHg, millimeters of mercury; SBP, systolic blood pressure.
Table 2 presents the clinical presentations of the participants. The total number of hypertensive crises cases were 577, with 654 visits divided into 24 hypertensive emergency visits and 630 hypertensive urgency visits, which showed that most patients with hypertensive crisis presented with nonspecific symptoms (42.2%) and various symptoms, including vertigo/dizziness (27.7%), headache (14.4%), palpitations (5.4%), dyspnea (4.4%), and chest pain (3.5%), arranged from most to least common.
Table 2.
Clinical presentation of participants, n=654 visits.
| Clinical presentation (n, %) | Total | Emergency department (n=541) | Primary care unit (n=113) | P |
|---|---|---|---|---|
| No specific symptoms | 276 (42.2) | 188 (34.8) | 88 (77.9) | <0.001a |
| Vertigo/dizziness | 181 (27.7) | 166 (30.7) | 15 (13.3) | <0.001a |
| Headache | 94 (14.4) | 89 (16.5) | 5 (4.4) | 0.002a |
| Palpitations | 35 (5.4) | 33 (6.1) | 2 (1.8) | 0.066b |
| Dyspnea | 29 (4.4) | 28 (5.2) | 1 (0.9) | 0.044b |
| Chest pain | 23 (3.5) | 23 (4.3) | 1 (0.9) | 0.010b |
| Blur vision | 16 (2.5) | 13 (2.4) | 3 (2.7) | 0.747b |
| Weakness | 15 (2.3) | 14 (2.6) | 1 (0.9) | 0.488b |
| Generalized fatigue | 15 (2.2) | 14 (2.6) | 1 (0.9) | 0.488b |
| Epistaxis | 14 (2.1) | 14 (2.6) | 0 (0) | 0.145b |
| Paresthesia | 12 (1.8) | 12 (2.2) | 0 (0) | 0.237b |
| Alteration of consciousness | 9 (1.4) | 9 (1.7) | 0 (0) | 0.371b |
| Dysarthria | 5 (0.8) | 5 (0.9) | 0 (0) | 0.594b |
| Oliguria | 2 (0.3) | 2 (0.4) | 0 (0) | 1.000b |
| Hematuria | 2 (0.3) | 2 (0.4) | 0 (0) | 1.000b |
χ 2test.
Fisher’s exact test; n, number of visits.
Table 3 presents the assessment of EOD among the visited patients in the ED and PCU, in which 457 tests (69.9%) were ordered for management. Hypertensive emergencies significantly needed further investigation than hypertensive urgency (95.8 vs. 68.9%, P=0.003). Furthermore, 12-lead EKG was prescribed for most patients (59.6%), followed by blood urea nitrogen or creatinine (33.5%), electrolytes (29.8%), chest radiography (28.1%), complete blood count (28%), urinalysis (11.6%), brain imaging (9.5%), troponin test (6.3%), and chest computed tomography (0.2%), respectively.
Table 3.
Investigation and management of hypertensive crisis, n=654 visits.
| Hypertensive urgency (n=630) | Hypertensive emergency (n=24) | Total (n=654) | P | |
|---|---|---|---|---|
| The investigation, n (%) | 434 (68.9) | 23 (95.8) | 457 (69.9) | 0.003b |
| EKG-12 leads | 373 (59.2) | 17 (70.8) | 390 (59.6) | 0.354a |
| BUN or Cr | 198 (31.4) | 21 (87.5) | 219 (33.5) | <0.001b |
| Electrolyte | 174 (27.6) | 21 (87.5) | 195 (29.8) | <0.001b |
| CXR | 166 (26.4) | 18 (75.0) | 184 (28.1) | <0.001a |
| CBC | 162 (25.7) | 21 (87.5) | 183 (28.0) | <0.001b |
| UA | 70 (11.1) | 6 (25.0) | 76 (11.6) | 0.079a |
| Brain imaging (CT or MRI) | 47 (7.5) | 15 (62.5) | 62 (9.5) | <0.001a |
| Trop-T | 34 (5.4) | 7 (29.2) | 41 (6.3) | <0.001a |
| CT chest | 1 (0.2) | 0 (0) | 1 (0.2) | 1.000b |
| No investigation, n (%) | 196 (31.1) | 1 (4.2) | 197 (30.1) | 0.003b |
χ 2test.
Fisher’s exact test; n, number of visits.
BUN, blood urea nitrogen; CBC, complete blood count; Cr, creatinine; CT, computerized tomography; CXR, chest radiograph; EKG, electrocardiogram; UA, urinary analysis.
Figure 3 shows the EOD associated with hypertensive emergencies in terms of the number of visits to the ED and PCU. The top five common types of EOD were ischemic stroke (33.3%), hemorrhagic stroke (25%), acute heart failure (20.8%), acute myocardial infarction (16.7%), and acute renal failure (12.5%).
Figure 3.

End-organ damage associated with hypertensive emergency.
Table 4 shows the antihypertensive drugs used for hypertensive crises. In this setting, oral antihypertensive drugs were used more frequently than intravenous antihypertensive drugs to treat hypertensive crises (80.9 and 1.8%). Oral antihypertensive drugs were used significantly more frequently in hypertensive urgency than in hypertensive emergency (81.6 vs. 62.5%), with per oral angiotensin-converting enzyme (ACEI) (57.5%) being the most commonly prescribed among oral drug.
Table 4.
Antihypertensive drugs for hypertensive crisis, n=654 visits.
| Antihypertensive drug (n, %) | Hypertensive urgency (n=630) | Hypertensive emergency (n=24) | Total (n=654) | P |
|---|---|---|---|---|
| The oral antihypertensive drug, n (%) | 514 (81.6) | 15 (62.5) | 529 (80.9) | 0.038a |
| ACEI | 369 (58.6) | 7 (29.2) | 376 (57.5) | 0.008a |
| Vasodilators | 164 (26.0) | 10 (41.7) | 174 (26.6) | 0.143a |
| CCB | 116 (18.1) | 9 (37.5) | 125 (19.1) | 0.038a |
| Beta-blockers | 24 (3.8) | 2 (8.3) | 26 (4.0) | 0.246b |
| Diuretic | 7 (1.1) | 5 (20.8) | 12 (1.9) | <0.001a |
| ARBs | 11 (1.8) | 0 (0) | 11 (1.7) | 1.000b |
| Alpha1-blocker | 4 (0.6) | 1 (4.2) | 5 (0.8) | 0.171b |
| Combined α and β-blockers | 4 (0.6) | 0 (0) | 4 (0.6) | 1.000b |
| IV antihypertensive drugs, n (%) | 3 (0.5) | 9 (37.5) | 12 (1.8) | <0.001b |
| Nicardipine | 2 (0.3) | 5 (20.8) | 7 (1.1) | <0.001b |
| Nitroglycerine | 0 (0) | 4 (16.7) | 4 (0.6) | <0.001b |
| Others | 1 (0.2) | 1 (4.2) | 2 (0.3) | 0.072b |
| Labetalol | 0 (0) | 0 (0) | 0 (0) | 1.000b |
| Esmolol | 0 (0) | 0 (0) | 0 (0) | 1.000b |
χ 2test.
Fisher’s exact test; n, number of visits.
ACEI, angiotensin-converting enzyme inhibitors drug; ARBs, angiotensin receptor blockers drug; CCB, calcium channel blocker drug.
Intravenous medication was significantly more common in hypertensive emergencies than in hypertensive urgencies (37.5 vs. 0.5%). The most commonly used medication in this setting was intravenous nicardipine (1.1%).
Figure 4 shows that in the hypertensive urgency type, the mean SBP at initial (before treatment) and after treatment was found to be 204.6 and 173.6 mmHg, respectively. Furthermore, the mean DBP at initial and after treatment was found to be 98 mmHg and 90.8 mmHg. In the hypertensive emergency type, the mean SBP at initial and after treatment was found to be 209.8 mmHg and 148.9 mmHg. Moreover, the mean DBP at initial and after treatment was found to be 103.5 mmHg and 85.9 mmHg. The figure showed a significant reduction in blood pressure from initial to discharge.
Figure 4.
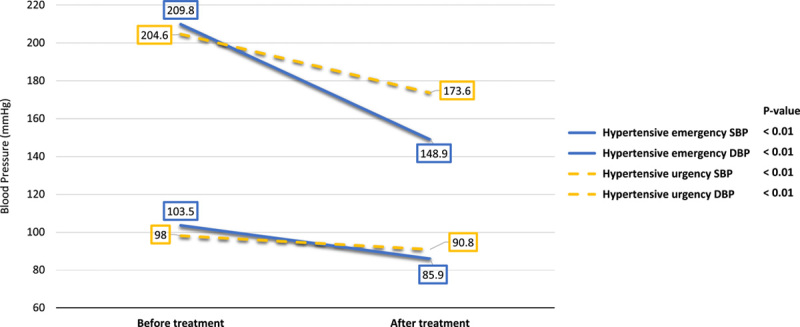
Before-treatment and after-treatment comparison of the blood pressure control pattern of patients with hypertensive crisis during the 3-year study period (2020–2022).
Table 5 Treatment outcomes between hypertensive emergency and hypertensive urgency. Of the 654 visits, most visit of 654 visits, most patients were discharged to their homes 607 (92.8%), and 47 (7.2%) were admitted to the hospital. Approximately 34 (72.3%) were admitted to the ward, followed by 12 (25.5%) to the short observation unit and 1 (2.2%) to the ICU. Most patients with hypertensive urgency were discharged 601 visits (95.4%), and 29 (4.6%) were admitted to the hospital. On the other hand, patients with a hypertensive emergency were majority admitted 18 (75%), 6 (25%) were discharged to their home, and 1 (4.2%) died. The median length of hospital stay for admitted patients was 5.5 days in the ward, 1.5 days in the short observation unit, and 7.5 days in the ICU. The mortality rate was 0.17% (1 in 577 patients).
Table 5.
The outcome of treatment between hypertensive emergency and hypertensive urgency, n=654 visits.
| Outcome (n, %) | Hypertensive emergency (n=24) | Hypertensive urgency (n=630) | Total (n=654) |
|---|---|---|---|
| Discharge | 6 (25.0) | 601 (95.4) | 607 (92.8) |
| Admission | 18 (75.0) | 29 (4.6) | 47 (7.2) |
| Ward | 15 (83.3) | 19 (65.5) | 34 (72.3) |
| SOU | 2 (11.1) | 10 (34.5) | 12 (25.5) |
| ICU | 1 (5.6) | 0 (0) | 1 (2.2) |
| Death | 1 (4.2) | 0 (0) | 1 (0.2) |
| Length of hospital stay (days) | |||
| Ward Median (Q1, Q3) | 5 (4, 20) | 7 (3, 12.5) | 5.5 (4, 13.8) |
| SOU Median (Q1, Q3) | 2 (1.5, 2.5) | 1.5 (1, 2) | 1.5 (1, 2) |
| ICU Median (Q1, Q3) | 7.5 (1, 18) | – | 7.5 (1, 18) |
n, number of visits.
SOU, short observation unit.
Table 6 showed the univariate and multiple logistic regression analyses showing that no factors, such as age, sex, BMI, underlying disease, SBP, or recurrence of hypertensive crisis, were significantly associated with hypertensive emergencies.
Table 6.
Results of univariate and multiple logistic regression analysis with factors associated with hypertensive emergency.
| Hypertensive emergency | |||
|---|---|---|---|
| Variables | Crude OR (95% CI) | Adjusted OR (95% CI) | P |
| Age (ref: <65 years) | |||
| ≥65 years | 0.53 (0.22,1.32) | 0.42 (0.16,1.10) | 0.078 |
| Sex (ref: female) | |||
| Male sex | 1.68 (0.68, 4.14) | 1.28 (0.50, 3.29) | 0.614 |
| BMI (ref: <25 kg/m2) | |||
| ≥25 kg/m2 | 0.49 (0.19, 1.31) | 0.4 (0.14, 1.11) | 0.078 |
| Underlying: CKD (ref: no) | |||
| Yes | 2.54 (0.98, 6.58) | 2.24 (0.83, 6.05) | 0.112 |
| SBP (cont. var.) | 1.01 (0.99, 1.04) | 1.01 (0.98, 1.03) | 0.524 |
| Recurrence (ref: no) | |||
| Recurrence HTN-C | 0.28 (0.04, 2.11) | 0.25 (0.03, 1.95) | 0.187 |
CKD, chronic kidney disease; Cont. var., continuous variable; HTN-C, hypertensive crisis; OR, odds ratio; SBP, systolic blood pressure.
Discussion
In this study, we assessed the prevalence, clinical characteristics, and factors associated with hypertensive crisis. The findings of this study are as follows: (I) 17.33% of patients with hypertension had a hypertensive crisis, 0.69% were of the emergency type, and 16.64% were of the urgency type; (II) the characteristic presentation of patients with a hypertensive crisis composed of nonspecific symptoms (42.2%), vertigo/dizziness (27.7%), and headache (14.4%); (III) EOD associated with a hypertensive emergency were ischemic stroke (33.3%), hemorrhagic stroke (25%), and acute heart failure (20.8%); (IV) oral ACEI (58.6%) was the most commonly prescribed among patients with hypertensive urgency; (V) intravenous nicardipine (20.8%) was significantly more common in a hypertensive emergency than in a hypertensive urgency; (VI) 7.2% of patients were admitted to the hospital; and (VII) there were no significant associations between the factors and hypertensive emergency.
This study found that 17.33% of patients with hypertension had a hypertensive crisis; 0.69% were of the emergency type and 16.64% were of the urgency type. Our findings are consistent with those of Kotruchin et al.4, who reported a 16.2% prevalence of hypertensive crisis, in which 2.2% were of the emergency type, and 14.0% were of the urgency type. On the contrary, our findings are inconsistent with those of Zampaglione et al.13, which reported a 27.5% prevalence of hypertensive crisis, in which 20.9% were of hypertensive urgency, and 6.6% were of hypertensive emergency. Meanwhile, a study conducted by Kim et al.14 showed a 5.9% prevalence of hypertensive crisis, in which 1.44% were of the emergency type, and 4.46% were of the urgent type. This indicates diversity in the prevalence of hypertensive crises worldwide. This might be explained by differences in baseline sociodemographic characteristics, settings, variations in the study, and the ability to obtain healthcare services.
In this study, we found that patients who experienced a hypertensive crisis had a high rate of poor compliance, up to 66.5%. This can be explained by Saguner et al.15 who reported that poor compliance was associated with an increased risk of developing a hypertensive crisis (P<0.01). Furthermore, nearly half the patients (42.2%) with hypertensive crisis presented without any specific symptoms, while the most common presenting symptom was vertigo/dizziness (27.7%), followed by headache (14.4%), which is inconsistent with the study of Desta et al.12 who reported that the most common symptoms were headache, nausea, vomiting, and chest pain, or a previous study in Thailand16.
Furthermore, our research showed that ischemic stroke was the most common EOD (33.3%), followed by hemorrhagic stroke (25%), and acute heart failure (20.8%), which is consistent with the findings of Kotruchin et al.4 who reported that the most common EODs were ischemic stroke (49.8%), followed by acute heart failure (19.3%) and hemorrhagic stroke (13.2%). After collecting data on drugs used to treat patients with hypertensive crisis who were divided into hypertensive urgency treatment, the most commonly used drugs were the ACEI group. This was in accordance with the research of Monteiro et al.17 who reported that the medication most frequently used at the baseline visit during hypertensive crisis was captopril. Physicians have primarily used intravenous nicardipine for the treatment of hypertensive emergencies in accordance with the International Society of Hypertension Global Hypertension Practice Guidelines for the pharmacological treatment of hypertension in adults (2020)18. There were no significant associations between factors and hypertensive emergency. By contrast, a previous study by Frederick et al.11 found that advanced age, chronic kidney disease, coronary artery disease, and stroke were all-cause risk factors for hypertensive emergency. We believe that this important factor is insignificant because the sample size of hypertensive emergencies had only 24 visits, resulting in a small ratio of hypertensive emergency to hypertensive urgency.
We found that the hospital admission rate in a hypertensive ED was consistent with that in a previous study by Kotruchin et al.4. Our admission rate was 75.0%, whereas Kotruchin et al.4 reported that patients with a hypertensive emergency were admitted at 79.2%. The mortality rate in this study was 0.17% (1 of 577 patients) and entirely attributed to hypertensive emergencies, similar to the study of Kotruchin et al.4 (0.1%), but lower than that of Guiga et al.19 (12.5%). On the other hand, our study found that the mortality rate in hypertensive urgency was 0%, which is inconsistent with that of Guiga et al.19, which reported a mortality rate during admission of 1.8%. This variation may be due to differences in hospital bed occupancy at the time of admission and different baseline characteristics of the patients.
Strengths of the study
Our study is one of the few studies, especially in Southeast Asia, that explored the prevalence, clinical characteristics, and risk factors of hypertensive crises. Moreover, this research studied patients in two settings, ER and PCU, showing differences in the characteristics of patients between both groups.
In this study, we collected possible confounders, such as age, sex, and underlying disease, then adjusted for the confounder’s influence on hypertensive emergency during the analysis process (multivariable logistic regression).
Limitations
A limitation of this study is the missing data due to incomplete medical records, especially the history of drug compliance, smoking, and alcohol consumption, which were not recorded for all patients.
Suggestion
Multicenter studies should be conducted throughout the country including large populations to determine the prevalence of hypertensive crises and events of hypertensive emergencies since this study was conducted in a single tertiary care center and might not represent all regional situations.
Future studies should be conducted in the other departments of the hospital to provide an overview of hypertensive crisis management in this tertiary care setting.
Conclusion
Our results revealed a relatively high prevalence of hypertensive crises. Furthermore, the majority of cases had hypertensive urgency, and we suggest that further studies should explore the causes of hypertensive crisis to improve the care of hypertensive patients.
Ethics approval
This study was approved by the Prince of Songkla University Institutional Review Board, Faculty of Medicine, Songklanagarind Hospital, Prince of Songkla University (REC.65-519-9-1). The date of approval by the ethics committee was 18 January 2023.
Consent
We could not perform any written consent, as our study was performed retrospectively using secondary data from electronic medical records.
Sources of funding
This research did not receive any specific grant from funding agencies in public, commercial, or not-for-profit sectors.
Author contribution
R.C.: writing study concept, methodology, data analysis, and writing the paper; W.P. and M.A.: writing the study concept; S.S., T.C.: writing the paper; K.C.: data analysis; P.W. and P.K.: data collection and writing the paper. All the authors have read and approved the final manuscript.
Conflicts of interest disclosure
The authors report no conflicts of interest in this study.
Research registration unique identification number (UIN)
Name of the registry: http://www.researchregistry.com
Unique identifying number or registration ID: researchregistry 9124.
Hyperlink to your specific registration (must be publicly accessible and will be checked): here: https://www.researchregistry.com/browse-the-registry#home/
Guarantor
Rattanaporn Chootong, M.D. Department of Family and Preventive Medicine, Prince of Songkla University, Hat Yai, Songkla 90110, Thailand. E-mail: rattanaporn.ch2529@gmail.com
Data availability statement
The datasets used during the study are available from the corresponding author on reasonable request.
Provenance and peer review
Not commissioned, externally peer reviewed.
Acknowledgements
The authors sincerely thank The Division of Digital Innovation and Data Analytics (DIDA), Faculty of Medicine, Prince of Songkhla University, for providing information on hypertensive patients (hospital numbers).
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 7 September 2023
Contributor Information
Rattanaporn Chootong, Email: rattanaporn.ch2529@gmail.com.
Wasuntaraporn Pethyabarn, Email: kwang.wsp@gmail.com.
Supinya Sono, Email: supi.sono@gmail.com.
Thitiworn Choosong, Email: cthitiwo@medicine.psu.ac.th.
Kittisakdi Choomalee, Email: kittisak.c@psu.ac.th.
Maimoonah Ayae, Email: amaimoon@medicine.psu.ac.th.
Punnisa Wisan, Email: punpunpun53@hotmail.com.
Phappim Kantalak, Email: 6010310139@psu.ac.th.
References
- 1.Gebresillassie BM, Debay YB. Characteristics, treatment, and outcome of patients with hypertensive crisis admitted to University of Gondar Specialized Hospital, northwest Ethiopia: a cross-sectional study. J Clin 2020;22:2343–2353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Samuel N, Nigussie S, Jambo A, et al. Treatment outcome and associated factors among patients admitted with hypertensive crisis in public hospitals at Harar Town, Eastern Ethiopia: a cross-sectional study. Integr Blood Press Control 2022;15:113–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Benenson I, Waldron FA, Jadotte YT, et al. Risk factors for hypertensive crisis in adult patients: a systematic review. JBI Evid Synth 2021;19:1292–1327. [DOI] [PubMed] [Google Scholar]
- 4.Kotruchin P, Pratoomrat W, Mitsungnern T, et al. Clinical treatment outcomes of hypertensive emergency patients: results from the hypertension registry program in Northeastern Thailand. The Journal of Clinical Hypertension 2020;23:621–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mancia G, Fagard R, Narkiewicz K, et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens 2013;31:1281–1357. [DOI] [PubMed] [Google Scholar]
- 6.Kulkarni S, Glover M, Kapil V, et al. Management of hypertensive crisis: British and Irish Hypertension Society Position document. J Hum Hypertens 2022:1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kotruchin P, Tangpaisarn T, Mitsungnern T, et al. Hypertensive emergencies in Asia: a brief review. J Clin Hypertens (Greenwich) 2022;24:1226–1235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Almas A, Ghouse A, Iftikhar AR, et al. Hypertensive crisis, burden, management, and outcome at a tertiary care center in Karachi. Int J Chronic Dis 2014;2014:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shin JH, Kim BS, Lyu M, et al. Clinical characteristics and predictors of all-cause mortality in patients with hypertensive urgency at an emergency department. JCM 2021;10:4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mathew G, Agha R, for the STROCSS Group . STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 2021;96:106165. [DOI] [PubMed] [Google Scholar]
- 11.Waldron FA, Benenson I, Jones-Dillon SA, et al. Prevalence and risk factors for hypertensive crisis in a predominantly African American inner-city community. Blood Press 2019;28:114–123. [DOI] [PubMed] [Google Scholar]
- 12.Desta DM, Wondafrash DZ, Tsadik AG, et al. Prevalence of hypertensive emergency and associated factors among hospitalized patients with hypertensive crisis: a retrospective cross-sectional study. Integr Blood Press Control 2020;13:95–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bruno Zampaglione CP, Marco Marchisio PC-P. Hypertensive urgencies and emergencies: prevalence and clinical presentation. AHAjournals 1996;27:144–147. [DOI] [PubMed] [Google Scholar]
- 14.Kim BS, Kim H-J, Lyu M, et al. Clinical characteristics, practice patterns, and outcomes of patients with acute severe hypertension visiting the emergency department. Journal of Hypertension 2021;39:2506–2513. [DOI] [PubMed] [Google Scholar]
- 15.Saguner AM, Dür S, Perrig M, et al. Risk factors promoting hypertensive crises: evidence from a longitudinal study. Am J Hypertens 2010;23:775–780. [DOI] [PubMed] [Google Scholar]
- 16.Piyanuttapull S, Angsanakul J. Prevalence of hypertensive emergency in emergency room of Rajavithi Hospital. J Hypertens Manag, 2:010. [Google Scholar]
- 17.Monteiro Júnior FD, Anunciação FA, Salgado Filho N, et al. Prevalence of true hypertensive crises and appropriateness of the medical management in patients with high blood pressure seen in a general emergency room. Arq Bras Cardiol 2008;90:247–251English, Portuguese. [DOI] [PubMed] [Google Scholar]
- 18.Unger T, Borghi C, Charchar F, et al. 2020 international society of hypertension global hypertension practice guidelines. Hypertension 2020;75:1334–1357. [DOI] [PubMed] [Google Scholar]
- 19.Guiga H, Decroux C, Michelet P, et al. Hospital and out-of-hospital mortality in 670 hypertensive emergencies and urgencies. J Clin Hypertens 2017;19:1137–1142. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used during the study are available from the corresponding author on reasonable request.


