Abstract
Introduction and importance:
It is rare for calcium oxalate renal stone, presented mainly in sterile urine, to result in urinary tract infection. The stone-related infection could develop spondylodiscitis, causing neurological deficits. To date, there are no reports about calcium oxalate partial staghorn stone and spondylodiscitis.
Case presentation:
A 62-year-old male suffered from haematuria, fever, and flank pain. He came to the urology outpatient department, where acute pyelonephritis was diagnosed, and a left partial staghorn stone was seen on computed tomography. Oral antibiotics were prescribed with improvement. Two weeks after antibiotics treatment, he developed bilateral lower limb weakness and numbness under the nipple level. He was brought to the emergency department, where the spine MRI revealed T2–T3 spondylodiscitis with epidural abscess and spinal cord compression. He underwent T2–T3 spine operation with improvement in muscle power and hypesthesia. The culture of the surgical lesion yielded Citrobacter koseri, the same as the urine culture obtained at his first visit. Left-side percutaneous nephrolithotomy was performed 1 month after with successful stone removal and resolution of pyuria. Stone analyses reported calcium oxalate. Follow-up MRI showed marked improvement with resolution of spondylodiscitis.
Clinical discussion:
Urinary tract infection resulting from partial staghorn stone, with additional hematogenous spread causing spondylodiscitis, is scarcely discussed. The authors illustrated a case with calcium oxalate stone, belonging to sterile Jensen’s classification type 1. However, a urinary tract infection could be seen in urine stasis or obstruction.
Conclusion:
With accurate diagnosis and essential interventions, the patient had immediate neurological improvement and reached disease-free status.
Keywords: case report, citrobacter koseri, spondylodiscitis, staghorn stone, urinary tract infection
Introduction
Highlights
Infected calcium oxalate partial staghorn stone leads to pyogenic spondylodiscitis is a rare occurrence.
This patient was initially diagnosed with acute pyelonephritis but later developed bilateral lower limb weakness and numbness due to spinal cord involvement.
Spondylodiscitis was not anticipated, highlighting the difficulty in diagnosing the underlying cause.
Surgical intervention resulted in improved muscle power and hypesthesia, with culture confirming pathogen corresponding with the previous urine culture.
This case highlights the connection between urinary tract infection, calcium oxalate stones, and the development of pyogenic spondylodiscitis.
Urolithiasis is the most common urological pathology, with an estimated incidence rate of around 10–15%1. The connection between renal stones and infections has been identified with urinary alkalinity, phosphate calculi, and increased urinary ammonia2. Infection stones would mainly form staghorn, which could be complete or partial3. Usually, they are composed of struvite (magnesium ammonium phosphate), linked to some urease-producing bacteria, including Proteus, Providencia, Staphylococcus, and Klebsiella4.
Calcium oxalate is the predominant stone composition, with a 60% occurrence rate, while struvite accounts for 7%5. Notably, calcium oxalate stones are rarely associated with urinary tract infections.
Spondylodiscitis is a rare disease characterized by an infection or inflammation of the intervertebral disc6,7. The aetiology could be a transient bacteremia causing seeding to the spine or direct extension from an infected lesion, even as a complication of urinary tract infection8. Hematogenous spread of bacteria is the most common cause of pyogenic spondylodiscitis and is reported chiefly caused by Staphylococcus aureus (>50%)9.
The association between renal stones and spondylodiscitis is rarely discussed. Rehman et al. 10 have reported that a 74-year-old woman with ureteric stone causing acute flank pain received ureteric stent initially, which led to E. coli-associated bacteremia and subsequent spondylodiscitis. The case Rehman and colleagues presented did not experience any neurological deficit. We demonstrate a calcium oxalate partial staghorn case, which later developed thoracic spondylodiscitis and bilateral lower limb muscle asthenia without prior stone interventions and systemic bacteremia. The case has been reported in line with the SCARE criteria11.
Case presentation
The patient was a 62-year-old male without systemic medical diseases and denied social history. He experienced gross haematuria, accompanying intermittent fever up to 38.5°C, and acute left flank pain. He was treated at our urology clinic where urine analysis revealed pyuria [white blood cell (WBC):≥100/high power field (HPF)], and ultrasonography showed a left renal stone. Acute pyelonephritis was impressed and oral cefuroxime was prescribed. Urine culture was obtained and yielded Citrobacter koseri. An abdominal computed tomography scan showed a left partial staghorn renal stone (Fig. 1). Retrograde intrarenal surgery was suggested, yet the patient hesitated.
Figure 1.

Computed tomography scan of the abdomen and pelvis in coronal view showed left partial staghorn renal stones measuring 1.8 cm, with Hounsfield unit (HU) around 1100.
Two weeks later, he developed acute bilateral lower limbs weakness with numbness under the nipple level. He then came to our emergency department. The physical exam showed decreased bilateral lower limbs muscle power (4/5). Lab data yielded leukocytosis (WBC: 9.22 K/μl Seg:78.1%) and pyuria (WBC:≥100/HPF). Spine MRI revealed T2–T3 discitis with pyogenic infection resulting in retropulsion and compression of the spinal cord (Fig. 2).
Figure 2.
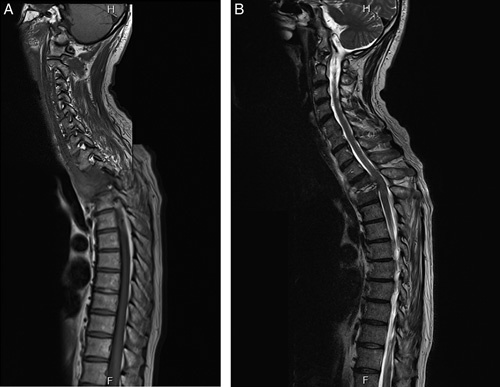
Contrast-enhanced MRI of the spine showed irregular endplate change and disc destruction with heterogeneous paraspinal enhancing soft tissue and abscess formation at T2–3 level [(A) T1WI sagittal view; (B) T2WI sagittal view].
Thoracic myelopathy due to T2–T3 spondylodiscitis with epidural abscess and spinal cord compression was diagnosed. The patient received T2–T3 laminoplasty/pediculectomy/facetectomy and T2–3 discectomy to remove the epidural abscess and spinal cord decompression, as well as bilateral T1, T2, and T4 posterior fixation with pedicle screw. His muscle power and hypesthesia had improved after the operation. The culture of the surgical lesion yielded Citrobacter koseri, the same as the prior urine culture result.
Postoperative laboratory data showed resolved leukocytosis and pyuria, and follow-up MRI showed marked improvement with spinal stenosis and epidural abscess (Fig. 3). Cefixime for 6–8 weeks was prescribed.
Figure 3.
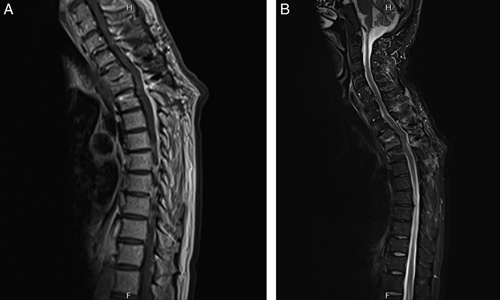
Contrast-enhanced MRI of the spine showed residual enhancement at T2 and T3 vertebrae and fluid accumulation in the intervertebral disc [(A) T1WI sagittal view; (B) STIR sagittal view]. Moreover, no more spinal stenosis and epidural components were seen.
One month after the spine surgery, urine analysis showed mild pyuria (WBC: 10–19/HPF), and Ceftriaxone was administered 3 days before nephrolithotomy. Left-side percutaneous nephrolithotomy was performed smoothly with no complication. Ceftriaxone was kept until discharge. The stone analysis reported the composition of calcium oxalate. Outpatient department follow-ups showed bilateral no hydronephrosis and negative pyuria in urine analysis.
Discussion and conclusions
We presented a case of unusual infective renal calculi, ensuing hematogenous pyogenic spondylodiscitis with epidural abscess at the T2–T3 level causing bilateral lower limb muscle weakness. This case demonstrates the resolution of symptoms after surgical management.
Calcium oxalate stones have rarely formed into staghorn stones, less likely to develop spondylodiscitis. Even so, the stone compositional analysis is crucial in defining the aetiology and determining treatment12. Identification of the stone compositions could be classified according to Jensen’s system13. Type I stones are defined as those found in sterile and acidic urine, commonly with calcium-based calculi. Type II stones are infection calculi and alkaline urine, whereas type III stones result from metabolic abnormalities, such as uric acid-based calculi. According to this classification, calcium oxalate, classified as Jensen type 1, is present in sterile urine and less associated with infection. However, conditions causing urine stasis or urinary tract obstruction could result in urinary tract infection14.
The infection mechanism hypothesizes that the preceding formed-calcium oxalate stone encounters episodes of urinary tract infection, which turn the sterile calculi into an infection staghorn stone, complicating with systemic bacteremia and subsequent general illness. Few cases describe urolithiasis-related urinary tract infection (UTI)-causing spondylodiscitis. Rehman et al. 10 reported that a 74-year-old female underwent retrograde intrarenal surgery for ureteric stone, which later developed Escherichia coli bacteriemia and subsequent spondylodiscitis at T10/T11. Secondary spondylodiscitis of L3, L4, and L5 as a complication of urosepsis related to extracorporeal shock wave lithotripsy was observed by Gallina et al. 15. Those studies shared the element of pre-existing intervention to stones, causing bacteriemia and urosepsis, or local abscess formation invading kidney-level vertebrae, ultimately resulting in spondylodiscitis.
Contrarily, there was no precedent stone intervention and no observed systematic bacteremia in our case. However, distant infection to T2–T3 pyogenic spondylodiscitis was presented, implying the hematogenous spread of bacteria10. In conclusion, the infective renal calculi have the potential to progress into bacteremia from urinary tract infection, leading to severe diseases.
In our case, the surgical wound and urine culture yielded a Gram-negative bacillus of the Enterobacteriaceae family named Citrobacter. Among its species, the most commonly isolated from human and infection-associated are C. koseri and C. freundii 16. Citrobacter infection is rarely identified and almost exclusively presented in infants, and immune-compromised hosts, resulting primarily in meningitis17. Nonetheless, in adult patients, C. freundii was frequently isolated from the gastrointestinal tract, and C. koseri most commonly leads to urinary tract infections, most of which are pyelonephritis18.
Few cases describe Citrobacter koseri-related UTI and spondylodiscitis. Hayati et al. 18 reported a 75-year-old female with lower urinary tract symptoms and Citrobacter koseri bacteremia complicated by spondylodiscitis. Stewart and colleagues demonstrated a case of staghorn calculus and C. koseri UTI progressing to a peri-nephric abscess and empyema. They both pointed out the potential for systemic illness in patients with C. koseri UTI, especially in the setting of nephrolithiasis17.
Calcium oxalate partial staghorn with Citrobacrter koseri urinary tract infection is uncommon, let alone the complication of pyogenic spondylodiscitis. This case highlights the association between Citrobacrter koseri infection and hematogenous-related spondylodiscitis; moreover, signifying the importance of possible severe complications and neurological sequelae in staghorn stone patients.
Ethical approval
None declared.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
No funding was declared for this article.
Author contribution
C.-Ya.W. analyzed the patient data, wrote the main manuscript text, and prepared figures. C.-S.T. and Y.-J.L. provided expertise and edited the manuscript. All authors read and approved the final manuscript.
Conflicts of interest disclosure
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Research registration unique identifying number (UIN)
None declared.
Guarantor
Yuan-Ju Lee and Chi-Shin Tseng.
Data availability
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Provenance and peer review
Not commissioned, externally peer-reviewed
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 1 September 2023
Contributor Information
Cheng-Yang Wu, Email: fantasy7386@gmail.com.
Chi-Shin Tseng, Email: clifford1987tcs@gmail.com.
Yuan-Ju Lee, Email: leeyuanju@hotmail.com.
References
- 1.Li S, Huang X, Liu J, et al. Trends in the Incidence and DALYs of Urolithiasis From 1990 to 2019: Results From the Global Burden of Disease Study 2019. Front Public Health 2022;10:825541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karki N, Leslie SW. Struvite And Triple Phosphate Renal Calculi StatPearls. 2023. [PubMed] [Google Scholar]
- 3.Diri A, Diri B. Management of staghorn renal stones. Ren Fail 2018;40:357–362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Torricelli FCM, Monga M. Staghorn renal stones: what the urologist needs to know. Int Braz J Urol 2020;46:927–933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Partin AW, Dmochowski RR, Kavoussi LR, et al. Campbell-Walsh-Wein urology. Twelfth edition ed. Elsevier; 2021. [Google Scholar]
- 6.Rotzinger R, Omidi R, Gebhard H, et al. [Spondylodiscitis and epidural abscesses]. Radiologe . 2021;61:275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryang YM, Akbar M. [Pyogenic spondylodiscitis: symptoms, diagnostics and therapeutic strategies]. Orthopade 2020;49:691–701. [DOI] [PubMed] [Google Scholar]
- 8.Subramanian V, Hughes P, Soni B, et al. Discitis following urinary tract infection manifesting as recurrent autonomic dysreflexia related to truncal movements in a person with tetraplegia. BMJ Case Rep 2020;13. doi: 10.1136/bcr-2020-238202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Herren C, Jung N, Pishnamaz M, et al. Spondylodiscitis: diagnosis and treatment options. Dtsch Arztebl Int 2017;114:875–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rehman Z, Cullen J, Withey S, et al. Ureteric stone-related Escherichia coli bacteraemia associated with spondylodiscitis. Uro 2021;1:198–201. [Google Scholar]
- 11.Agha RAFT, Sohrabi C, Mathew G. for the SCARE Group., The SCARE 2020 Guideline: Updating Consensus Surgical CAse REport (SCARE) Guidelines. Int J Surg 2020;84:226–230. [DOI] [PubMed] [Google Scholar]
- 12.Mandel NS, Mandel IC, Kolbach-Mandel AM. Accurate stone analysis: the impact on disease diagnosis and treatment. Urolithiasis 2017;45:3–9. [DOI] [PubMed] [Google Scholar]
- 13.Hsu TC, Chen J, Huang HS, et al. Association of changes in the pattern of urinary calculi in Taiwanese with diet habit change between 1956 and 1999. J Formos Med Assoc 2002;101:5–10. [PubMed] [Google Scholar]
- 14.Heyns CF. Urinary tract infection associated with conditions causing urinary tract obstruction and stasis, excluding urolithiasis and neuropathic bladder. World J Urol 2012;30:77–83. [DOI] [PubMed] [Google Scholar]
- 15.Gallina P, Dardo M, Pedone A, et al. Clinical image: spondylodiscitis as a complication of urosepsis caused by extracorporeal shock wave lithotripsy for kidney stones. Oxf Med Case Rep 2023;2023:omac144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Samonis G, Karageorgopoulos DE, Kofteridis DP, et al. Citrobacter infections in a general hospital: characteristics and outcomes. Eur J Clin Microbiol Infect Dis 2009;28:61–68. [DOI] [PubMed] [Google Scholar]
- 17.Stewart ZE, Shaker M, Baxter JD. Urinary tract infection caused by Citrobacter koseri in a patient with spina bifida, an ileal conduit and renal caluli progressing to peri-nephric abscess and empyema. Urol Case Rep 2017;11:22–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hayati SN, Leong CL, Kumar CS, et al. Citrobacter koseri bacteraemia complicated by paraspinal abscess and spondylodiscitis—a case report. Med J Malaysia 2012;67:337–339. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.


