Abstract
Ultrasound-guided quadratus lumborum block (QLB) has been gradually carried out in clinical practice. However, some clinical evidence is contradictory, and no studies have summarized and described these results. The authors reviewed the anatomical characteristics of QLB and summarized the advantages and disadvantages of four puncture methods, so as to facilitate the clinical application of QLB.
Keywords: clinical application, quadratus lumborum block, thoracolumbar fascia, ultrasound
Introduction
Highlights
The anatomy of quadratus lumborum block (QLB) is systematically introduced.
The advantages and disadvantages of four methods of QLB are summarized.
The application of QLB in different types of surgery is reported.
The quadratus lumborum block (QLB), first proposed by Blanco in 20071, is a well-established method for perioperative analgesia. It is an extension method of transversus abdominis plane block (TAPB) and has been shown in previous studies to provide better pain relief and longer duration compared to TAPB by blocking both surface somatic pain and visceral pain2,3. While patient-controlled epidural analgesia or patient-controlled intravenous analgesia are commonly used, they carry the risk of postoperative nausea and vomiting, excessive sedation, enteroparalysis, and even respiratory depression4.
In contrast, nerve blocks are free of these risks, making QLB a promising method for clinical application. With advancements in technology, the proficiency of anesthesiologists in using ultrasound has also increased, making ultrasound-guided nerve blocks more accurate, less invasive, and more beneficial for patients5. Because there is no obvious breakthrough sensation, QLB can only be performed using ultrasound-guided puncture techniques. Based on the increasing clinical interest in QLB, we summarize the anatomical structure of QLB and the four techniques of QLB systematically. The application of QLB in different surgical procedures is described in combination with the latest research findings.
Anatomical basis of QLB
The quadratus lumborum (QL) muscle is located in the posterior region of the abdomen, positioned on either side of the spine. It begins at the inferior border of the 12th rib and L1–L4 transverse process, and terminates at the superior border of the iliac crest. The QL is situated medially to the psoas muscle (PM), laterally to the latissimus dorsi, and posterior to the erector spinae (ES)6. The primary function of the QL is to provide stability to the spine, while also assisting in respiration and maintaining stability in the thorax. The thoracolumbar fascia (TLF), which is a fusion of tendon and fascia that encases the back muscles extending from the thorax to the lumbar spine, is a crucial anatomical structure for ultrasound-guided puncture as it affects the diffusion and distribution of drugs7. The anterior layer of the TLF is positioned anterior to the QL and the PM and is a continuation of the transversus abdominis fascia. It can be divided cephalad into two layers, with the inner layer being continuous with the internal thoracic fascia and the outer layer being fused with the arcuate ligament of the diaphragm. The middle layer of the TLF extends laterally to the lateral side of the QL and anterior to the latissimus dorsi, and joins with the anterior TLF to form the tendon membrane at the beginning of the transversus abdominis muscle. The posterior layer of the TLF covers the back of the ES7–10. The drug may diffuse along the TLF, posterior to the arcuate ligament, into the thoracic paravertebral space and intercostal space, thereby blocking the thoracic nerve and thoracic sympathetic trunk. Additionally, the TLF serves as not only a pathway for drug diffusion but also has branches of the spinal nerve and sympathetic nerve and is rich in mechanical stimuli and pain receptors11,12.
Four piercing routes of QLB
The four puncture approaches for QLB (QLB1 or lateral QLB, QLB2 or posterior QLB, QLB3 or anterior/transmuscular QLB, and QLB4 or intramuscular QLB) are named according to the position of the needle tip in relation to the QL13. QLB1 means that the patient should lie supine with the ultrasound probe placed under the costal margin of the midaxillary line and between the anterior superior iliac spine. After penetrating the transversus abdominia aponeurosis with the tip of the needle under direct vision, the anesthesiologist can push the local anaesthetic between the transversus abdominis and the QL. At this time, the local anaesthetic can spread into the paravertebral space of the thoracic segment14. QLB2 means that the patient is in the lateral position and the convex array probe is placed perpendicular to the midaxillary line between the ilium and the costal margin. The probe is moved posteriorly until the QL, the PM and the ES are displayed. Compared with other methods, the injection position of QLB2 is more superficial and the ultrasonic imaging is clearer. The QL is separated from the tip of the needle and the peritoneum, making QLB safer and avoiding the risk of intraperitoneal injection and intestinal injury15. QLB3 means that the liquid is injected between the QL and the PM, reaching deep into the anterior layer of the TLF16. The patient is placed in the lateral decubitus position, and the convex array probe is placed vertically on the posterior axillary line at the level of the iliac crest, where the cloverleaf pattern can be visualized. The puncture needle is inserted at a 30° angle from the posterior edge of the probe and passes through the QL to reach the space between the QL and the ES, where local anaesthetic can be injected. The rotation of the probe by 90° longitudinally confirms the distribution of the local anaesthetic, which spreads longitudinally from the iliac crest to the 12th rib between the QL and the ES. QLB4 is different from other QLB techniques. It involves the penetration of the QL fascia, where the local anaesthetic is injected17. Figure 1 shows the puncture direction of QLB.
Figure 1.
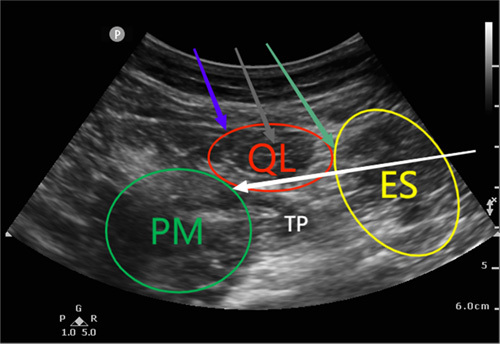
Place the ultrasound probe horizontally above the iliac crest, revealing the three layers of muscles for transversus abdominis plane block. Continue to slide the probe horizontally towards the posterior abdominal wall. Under ultrasound guidance, the “clover” structure formed by the psoas major (PM), erector spinae (ES), and quadratus lumborum (QL) muscles, with the transverse process as the handle, can be seen. The blue, green, white, and grey arrows represent the puncture directions and injection positions for QLB1, QLB2, QLB3, and QLB4, respectively.
Clinical studies and autopsy studies have shown that the block levels of QLB1 are between T7 and L1 and that the drug mainly diffuses in the transversus abdominis plane18; the block levels of QLB2 are between T7 and L1 and the drug diffuses in the middle layer of the TIF18; the block levels of QLB3 are between T7 and L2, and the drug can spread to the lumbar and thoracic paravertebral spaces12. According to the method described by Murouchi, the block levels of QLB4 are between T7 and T12, and this method has some analgesic effect after caesarean section19. Table 1 summarizes the characteristics of QLB in the four puncture approaches.
Table 1.
Comparison of the four puncture approaches for QLB
| QLB1 | QLB2 | QLB3 | QLB4 | |
|---|---|---|---|---|
| Block range | T7–L1 | T7–L1 | T7–L2 | T7–T12 |
| Patient position | Supine/lateral position | Supine/lateral position | Lateral position | Supine/lateral position |
| Injection site | Lateral border of the QL at the junction with the transversus abdominis fascia | Middle layer of the TLF on the posterolateral side of the QL | Anterior layer of the TLF between the PM and the QL | Internal the QL |
| Operation difficulty | Simple | Simple | Difficult | Simple |
| Safety | Low risk of puncture | Low risk of puncture | Risk of intraperitoneal organ injury and lower limb muscle weakness | Low risk of puncture |
| Applicable surgeries | Abdominal operation | The best puncture approach for cesarean section | Hip surgery | Lower abdominal operation |
PM, psoas major; QLB, quadratus lumborum block; QLB1, lateral QLB; QLB2, posterior QLB; QLB3, anterior/transmuscular QLB; QLB4, intramuscular QLB; TLF, thoracolumbar fascia.
Clinical application of QLB
Currently, ultrasound-guided QLB is commonly used in hip joint and lower limb surgeries, caesarean section surgeries, urological surgeries, paediatric surgeries, gastrointestinal surgeries, and spinal surgeries.
Hip joint and lower limb surgeries
The findings from a meta-analysis indicate that the use of QLB has the potential to decrease postoperative pain and the need for opioid medication in individuals undergoing total hip joint replacement surgery who receive general anaesthesia or spinal anaesthesia20. Cadaveric specimens studies have found that QLB3 is different from QLB1 and QLB2, with a more consistent spread of the dye in different specimens, reaching the L1 to L3 nerve roots within the QL and the PM18. Therefore, there is currently research exploring the application of QLB3 for postoperative pain management after total hip joint replacement surgery. Altparmak and colleagues reported a case of using a combination of QLB3 and sciatic nerve block as an anaesthetic method for hip surgery in a patient with multiple injuries. This method provided satisfactory anaesthesia for the patient without interfering with their airway and without changing their position21. Tulgar et al. 22. compared the effectiveness of traditional erector spinae plane block (ESPB) and QLB in providing postoperative pain relief for patients undergoing hip joint and proximal femur surgery, and found that compared to the standard intravenous pain control regimen, both ESPB and QLB improved patients’ pain quality. Compared to the lumbar plexus block, the QLB injection site is relatively superficial, with advantages such as relatively simple and safe operation, less pain during the procedure, and fewer complications. Research by Kukreja et al. 23. shows that in patients undergoing total hip joint replacement surgery, QLB3 can provide satisfactory postoperative pain relief, reduce the visual analogue scale pain score in the first 24 h after surgery, decrease the cumulative use of opioids, and improve patient satisfaction. A recent study on total hip replacement surgery indicated that multimodal pain control combined with a posterior lumbar fascia block did not reduce the use of opioid drugs in the 24 h post-surgery. This may be due to the fact that the posterior lumbar fascia block does not block the lumbar plexus24.
Caesarean section surgeries
The pain after caesarean section surgery includes physical pain caused by the incision in the abdominal wall, inflammatory pain caused by the release of inflammatory substances after trauma, and strong and persistent uterine contractions caused by the uterine involution after pregnancy and delivery. QLB can block both physical and visceral pain at the same time and is a non-systemic medication without the use of opioid drugs, which is beneficial for breastfeeding. It has unique advantages in postoperative pain relief after caesarean section12,25,26. QLB can reduce the consumption of opioid pain relievers after surgery, which helps to reduce the occurrence of adverse reactions such as excessive sedation, respiratory depression, nausea, vomiting, and others caused by opioid pain relievers after caesarean section. It does not affect the care of newborns and breastfeeding by the puerperae27. The application of 0.2% ropivacaine for QLB2 with a continuous catheter and combined with non-steroidal anti-inflammatory drugs and acetaminophen for postoperative pain relief can significantly reduce the visual analogue scale pain score of postoperative mothers (0 at rest and 3 during activity). The puerperae can remove the catheter on the third day after surgery, achieving opioid-free pain relief after caesarean section28. As previously mentioned, ESPB and QLB have comparable pain-relieving effects after hip joint surgery. There are no significant differences in the pain-relieving effects, complications, and recovery quality of the two in caesarean section surgery29. When patients receive intrathecal morphine, QLB only improves the pain score at rest for the first 6 h after surgery (no significant improvement in pain score at other time points within 48 h after surgery), and QLB cannot reduce the consumption of morphine in the first 24 h after surgery30.
Urological surgeries
Patients with bladder cancer often need to undergo radical cystectomy and have a high mortality rate after surgery. Epidural analgesia has been commonly used in the past, but it may increase the likelihood of low blood pressure, postoperative nausea and vomiting, and the duration of catheterization31. A group of authors have found that although epidural analgesia is better than QLB2 for pain relief in bladder cancer patients 2 and 4 h after surgery, there is no significant difference in pain 24 h after surgery, and there is no significant difference in the consumption of opioid drugs in the first 2 days after surgery with both methods32. In addition, patients undergoing percutaneous nephrolithotomy, preoperative QLB on the surgical side can reduce the consumption of opioid drugs after surgery and shorten the time from PACU to the first time walking after surgery, reducing the length of hospital stay33.
Paediatric surgeries
Surgeries often come with pain, which can cause a lot of distress for children. Insufficient pain relief may result in reduced long-term pain tolerance and more pain response34. Dexmedetomidine, a highly selective α-2 adrenergic receptor agonist, is becoming increasingly popular in paediatric surgeries due to its ability to produce dose-dependent sedation, anxiolysis, and analgesia without causing respiratory depression35. Interfascial administration of dexmedetomidine as an adjuvant to QLB has been found to have a better analgesic effect than intravenous administration, leading to a reduction in the amount of morphine used, lower pain scores, and an extended time to the first request for pain relief36. In comparison to TAPB in surgeries such as unilateral inguinal hernia repair or testicular excision, QLB has been shown to reduce the number of patients who require pain relief within 24 h after surgery, extend postoperative pain relief time, and result in higher satisfaction among parents of children37. Additionally, QLB reduces the possibility of a prolonged hospital stay, which can be a potential side effect of traditional caudal epidural block38. In lower abdominal surgeries, the transmuscular approach of the QL (TQL) may provide a more effective analgesic effect in comparison to the intramuscular approach of the QL. However, it is important to note that the TQL approach may also elevate the likelihood of quadriceps muscle weakness3.
Gastrointestinal surgeries
Stomach and colon cancers are frequently encountered in surgical procedures for lower abdominal cancers. The main approaches to treatment are open radical surgery and laparoscopic surgery. While laparoscopic surgery is minimally invasive, it can still result in moderate to severe postoperative pain, which can impede the patient’s recovery process. Although TAPB has the ability to alleviate postoperative pain and enhance the quality of patient recovery, its scope of coverage is limited and its duration is brief, and it is not effective in mitigating visceral pain39–41. On the other hand, QLB has been shown to be more effective in pain management following abdominal surgery compared to TAPB. This could be due to its broader diffusion of local anaesthetic, which might obstruct the pathways of both the abdominal wall nerves and the visceral nerves42. A clinical study involving 77 patients demonstrates that QLB is able to significantly decrease the use of morphine by patients in the 24 h following laparoscopic colorectal cancer surgery. Furthermore, the pain scores of patients in the QLB group are lower than those of the TAPB group during periods of rest or activity. In contrast, no significant differences are found between QLB and TAPB in regards to other factors, including morphine consumption after 48 h, postoperative nausea and vomiting, sedation scores, time taken for first walking, bowel function recovery time, and hospital stay43. A study evaluating the effects of QLB on postoperative pain and recovery in colorectal cancer patients reveals that QLB significantly reduces the consumption of sufentanil during the perioperative period of laparoscopic colorectal surgery and eases postoperative pain44. A meta-analysis of eight studies demonstrates that compared to TAPB, QLB significantly improves postoperative pain for abdominal surgery patients in the first 2, 4, 6, 12, and 24 h following surgery, extends the duration of pain relief, and decreases the consumption of morphine after 24 h45.
Spinal surgeries
Lumbar disc surgery is a frequently performed procedure for alleviating leg and lower back pain; however, it is often accompanied by intense postoperative discomfort. It is crucial for patients to have access to effective postoperative analgesia methods that produce minimal adverse reactions. Adequate postoperative pain management can enhance the patient’s ability to be active, decrease the risk of complications like deep vein thrombosis, and increase overall patient satisfaction46,47. General anaesthesia is a commonly used anaesthetic regimen, but the use of larger amounts of anaesthetic drugs can result in a slow awakening post-surgery and a higher occurrence of adverse reactions. If the amount of anaesthetic drugs is reduced to ensure anaesthetic safety, it can negatively impact the effectiveness of the anaesthesia48. General anaesthesia is a commonly used anaesthetic regimen, but the use of larger amounts of anaesthetic drugs can result in a slow awakening post-surgery and a higher occurrence of adverse reactions. Decreasing the usage of anaesthetic drugs for the purpose of ensuring anaesthetic safety can negatively affect the efficacy of the anaesthesia48. Two earlier studies49,50 indicated that QLB demonstrated favourable results in spinal surgical applications, where local anaesthetic drugs could target the transverse processes and inhibit the posterior branches of the lumbar nerves, resulting in pain relief. Regrettably, both of these studies have since been withdrawn. In a more recent study examining the impact of QLB on postoperative pain management following lumbar disc herniation surgery, it was found that administering QLB after the surgery enhanced the patient’s comfort levels both during periods of rest (0 and 2 h postoperatively) and activity (0, 2, 4, 8, and 16 h postoperatively)51. Wilton et al. 52. successfully utilized the continuous QLB to decrease the amount of postoperative morphine needed by patients undergoing lumbar spinal fusion. At present, there are limited reports on the application of QLB in spinal surgery. Other nerve blocking techniques, such as the transversus thoracis muscle block46 and the thoracolumbar interfascial plane block53, have demonstrated effectiveness in spinal surgical procedures, but there is not yet a widely agreed upon conclusion regarding their efficacy and safety compared to other methods.
Mechanism of action of QLB under ultrasound guidance
At present, the specific anaesthetic mechanism of QLB is not yet fully understood. The diffusion of local anaesthetics from the TIF to the paravertebral space may play an important role in paravertebral blockade. The TLF contains mechanoreceptors, nociceptors, and sympathetic nerve fibres. Local anaesthetics can spread along the TIF to the paravertebral space of the thoracic vertebrae, blocking multiple segmental somatic nerves and thoracic sympathetic trunks. Cadaver studies have shown that when performing the TQL at the L4, the dye can spread cranially to the thoracic paravertebral space, staining the thoracic sympathetic trunk and ventral branches of the T9–T10 spinal nerves12. Similarly, in cadaver studies of posterior lumbar block at the L3–4, the spread of the dye to the T10 paravertebral space was observed, blocking the T10–L1 nerve roots. When performing subcostal TQL at the L1–2 level, the dye can spread to the T9–T12 paravertebral space, blocking the T9–L1 nerve roots and even reaching the T7 level54. However, some studies suggest that the amount of local anaesthetic spreading to the paravertebral space is small, and paravertebral blockade may not play a major role. Instead, the primary mechanism of action of QLB may be the direct action of local anaesthetics on spinal nerve branches, sympathetic nerves, mechanoreceptors, and nociceptors within the TLF55.
Types, concentrations, dosages, and duration of action for local anaesthetics in ultrasound-guided QLB
At present, there is no clinical consensus on the types, volumes, and concentrations of local anaesthetics for QLB. Ropivacaine, a novel long-acting, pure levorotatory amide local anaesthetic, has lower cardiotoxic and neurotoxic effects compared to bupivacaine and is now widely used in QLB. For unilateral QLB, the recommended local anaesthetic dosage is 0.2–0.4 mL/kg, with the option of using 0.2–0.5% ropivacaine10. When performing bilateral blocks, the dosage should be adjusted to ensure that it does not exceed the toxicity threshold; 150 mg of ropivacaine is considered relatively safe for QLB19. The increased intra-thoracic and intra-abdominal pressure in pregnant women may lead to a wider range of QLB blockade. Mitchell et al. 56. reported the use of bupivacaine as a local anaesthetic for QLB, with concentrations of 0.125–0.175% and volumes of 0.2–0.4 mL/kg. The dosages for paediatric patients depend on factors such as weight, age, and the surgical site, and there is currently no uniform dosing regimen. The duration of action for QLB may last for over 24 h19.
Concurring complications of QLB under ultrasound guidance
Overall, QLB is a relatively safe nerve block technique, and reports of complications associated with QLB are rare. When performing QLB under ultrasound guidance, it is important to ensure that there are no blood vessels in the path of the needle to prevent abdominal organ injury, bleeding, and haematoma. Currently, there have been two reported cases of haematoma after QLB57. According to a report by Wikner58, a patient undergoing gynaecological laparoscopic surgery received QLB1 (0.25% bupivacaine 20 ml). The patient displayed unilateral hip flexion and knee joint extension weakness that lasted for 18 h post-surgery. This adverse effect may have been caused by the spread of the local anaesthetic to the L2 intervertebral space or the lumbar plexus. The blocking of the sympathetic nerve by QLB can reduce peripheral vascular resistance, leading to a decrease in blood pressure and a compensatory increase in heart rate. According to a report by Sá et al. 59, two patients undergoing gastrointestinal surgery received QLB2. After 30–40 min, the patients exhibited a noticeable decrease in blood pressure and an increase in heart rate. After excluding other factors, it was believed that this adverse reaction may have been related to sympathetic blockade caused by the spread of the local anaesthetic to the intervertebral space and epidural space. This was corrected by administration of atropine and rapid fluid resuscitation.
Conclusion
As perioperative pain management receives increasing attention, multimodal analgesic approaches dominated by regional anaesthesia are widely advocated. QLB is a highly effective regional anaesthesia technique that is known for its wide blocking range, long-lasting pain relief, and excellent pain management results. With a simple and safe administration process and minimal risk of complications, QLB can be effectively utilized as part of a comprehensive pain management plan following surgery. Compared to the conventional TAPB, QLB offers a wider range of pain relief and can extend the duration of pain relief while reducing the amount of pain medication required. QLB is characterized by its ability to block visceral pain, making it a promising approach in abdominal surgical pain management. It is expected to be an effective method for postoperative pain control, reducing the use of opioid medications, promoting gastrointestinal function recovery, shortening time to first ambulation, and accelerating postoperative recovery. In the future, further research is needed to explore the use of QLB for the treatment of chronic pain. Additionally, the mechanism of local anaesthetic diffusion via different techniques of QLB remains unclear, and the optimal administration method, drug concentration, and dose have yet to be determined. Due to the unclear mechanism of local anaesthetic diffusion through various QLB approaches, and as the diffusion of local anaesthetic affects the ultimate clinical outcome, more research is required in the future to investigate diffusion mechanisms and conduct randomized controlled trials on perioperative analgesia. It is expected that the use of QLB in clinical practice will continue to increase in popularity.
Ethical approval
Ethics approval was not required for this Review.
Consent
Informed consent was not required for this Review.
Source of funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author contribution
All authors listed have made contributions to the review. X.C.L. participated in collecting the data, analyzing the data, and drafting the manuscript. X.C.L. designed the study and revised the manuscript.
Conflicts of interest disclosure
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Research registration unique identifying number (UIN)
Name of the registry: NIL.
Unique Identifying number or registration ID: NIL.
Hyperlink to your specific registration (must be publicly accessible and will be checked): NIL.
Guarantor
Xuechen Long.
Data availability statement
All data quoted in the paper are extracted from available published literature.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article
Published online 1 September 2023
Contributor Information
Xuechen Long, Email: 458844740@qq.com.
Yibo Yin, Email: 780331939@qq.com.
Wenjun Guo, Email: lxc01200017@163.com.
Ling Tang, Email: x1255125543@sina.cn.
References
- 1.Blanco R. Tap block under ultrasound guidance: the description of a “no pops” technique: 271. Regi Anesth Pain Med 2007;32:130. [Google Scholar]
- 2.Wang Y, Wang X, Zhang K. Effects of transversus abdominis plane block versus quadratus lumborum block on postoperative analgesia: a meta-analysis of randomized controlled trials. BMC Anesthesiol 2020;20:103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hussein MM. Ultrasound-guided quadratus lumborum block in pediatrics: trans-muscular versus intra-muscular approach. J Anesth 2018;32:850–855. [DOI] [PubMed] [Google Scholar]
- 4.Salicath JH, Yeoh EC, Bennett MH. Epidural analgesia versus patient-controlled intravenous analgesia for pain following intra-abdominal surgery in adults. Cochrane Database Syst Rev 2018;8:D10434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cunat T, Mejia J, Tatjer I, et al. Ultrasound-guided genicular nerves block vs. local infiltration analgesia for total knee arthroplasty: a randomised controlled non-inferiority trial. Anaesthesia 2023;78:188–196. [DOI] [PubMed] [Google Scholar]
- 6.Ueshima H, Otake H, Lin JA. Ultrasound-guided quadratus lumborum block: an updated review of anatomy and techniques. Biomed Res Int 2017;2017:2752876–2752877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.El-Boghdadly K, Elsharkawy H, Short A, et al. Quadratus lumborum block nomenclature and anatomical considerations. Reg Anesth Pain Med 2016;41:548–549. [DOI] [PubMed] [Google Scholar]
- 8.Benedicta R, Jain MK, Dixit N, et al. The efficacy of ultrasound-guided transversus abdominis plane block versus quadratus lumborum block for postoperative analgesia in lower-segment cesarean section with low-dose bupivacaine: a randomized controlled trial. Anesth Essays Res 2022;16:203–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Farag E, Seif J, Kolli S. Quadratus lumborum block versus transversus abdominal plane block—The Debate is Still Going on. Editorial. J Clin Anesth 2020;66:109969. [DOI] [PubMed] [Google Scholar]
- 10.Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: anatomical concepts, mechanisms, and techniques. Anesthesiology 2019;130:322–335. [DOI] [PubMed] [Google Scholar]
- 11.Elsharkawy H, Pawa A, Mariano ER. Interfascial plane blocks: back to basics. Reg Anesth Pain Med 2018;43:341–346. [DOI] [PubMed] [Google Scholar]
- 12.Dam M, Moriggl B, Hansen CK, et al. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesth Analg 2017;125:303–312. [DOI] [PubMed] [Google Scholar]
- 13.Akerman M, Pejcic N, Velickovic I. A review of the quadratus lumborum block and ERAS. Front Med (Lausanne) 2018;5:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kelly T, Wolla CD, Wolf BJ, et al. Comparison of lateral quadratus lumborum and lumbar plexus blocks for postoperative analgesia following total hip arthroplasty: a randomized clinical trial. Reg Anesth Pain Med 2022;47:541–546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S, Kang RA, Kim GS, et al. Comparison of postoperative analgesic effects of posterior quadratus lumborum block and intrathecal morphine in laparoscopic donor hepatectomy: a prospective randomized non-inferiority clinical trial. Reg Anesth Pain Med 2022;47:527–533. [DOI] [PubMed] [Google Scholar]
- 16.Li H, Shi R, Shi D, et al. Anterior quadratus lumborum block at the lateral supra-arcuate ligament versus transmuscular quadratus lumborum block for postoperative analgesia in patients undergoing laparoscopic nephrectomy: a randomized controlled trial. J Clin Anesth 2021;75:110561. [DOI] [PubMed] [Google Scholar]
- 17.Yoshida K, Tanaka S, Watanabe K, et al. The effectiveness of the intramuscular quadratus lumborum block in postoperative analgesia after cesarean section with vertical incision: a randomized, double-blinded placebo-controlled study. J Anesth 2020;34:849–856. [DOI] [PubMed] [Google Scholar]
- 18.Carline L, McLeod GA, Lamb C. A cadaver study comparing spread of dye and nerve involvement after three different quadratus lumborum blocks. Br J Anaesth 2016;117:387–394. [DOI] [PubMed] [Google Scholar]
- 19.Murouchi T, Iwasaki S, Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg Anesth Pain Med 2016;41:146–150. [DOI] [PubMed] [Google Scholar]
- 20.Hussain N, Brull R, Speer J, et al. Analgesic benefits of the quadratus lumborum block in total hip arthroplasty: a systematic review and meta-analysis. Anaesthesia 2022;77:1152–1162. [DOI] [PubMed] [Google Scholar]
- 21.Altiparmak B, Korkmaz TM, Uysal AI, et al. Supine coronal approach to quadratus lumborum block in combination with anterior approach Sciatic block for sole anesthesia of hip fracture surgery. J Clin Anesth 2021;72:110303. [DOI] [PubMed] [Google Scholar]
- 22.Tulgar S, Kose HC, Selvi O, et al. Comparison of ultrasound-guided lumbar erector spinae plane block and transmuscular quadratus lumborum block for postoperative analgesia in hip and proximal femur surgery: a prospective randomized feasibility study. Anesth Essays Res 2018;12:825–831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kikuchi M, Mihara T, Mizuno Y, et al. Anterior quadratus lumborum block for postoperative recovery after total hip arthroplasty: a study protocol for a single-center, double-blind, randomized controlled trial. Trials 2020;21:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Brixel SM, Biboulet P, Swisser F, et al. Posterior quadratus lumborum block in total hip arthroplasty: a randomized controlled trial. Anesthesiology 2021;134:722–733. [DOI] [PubMed] [Google Scholar]
- 25.Stopar-Pintaric T, Blajic I, Visic U, et al. Posteromedial quadratus lumborum block versus wound infiltration after caesarean section: a randomised, double-blind, controlled study. Eur J Anaesthesiol 2021;38(suppl 2):S138–S144. [DOI] [PubMed] [Google Scholar]
- 26.Steingrimsdottir GE, Hansen CK, Borglum J. Ultrasound-guided transmuscular quadratus lumborum catheters for elective caesarean section: a protocol for a single-centre, double-blind randomised trial. Acta Anaesthesiol Scand 2020;64:1218–1223. [DOI] [PubMed] [Google Scholar]
- 27.Kang W, Lu D, Yang X, et al. Postoperative analgesic effects of various quadratus lumborum block approaches following cesarean section: a randomized controlled trial. J Pain Res 2019;12:2305–2312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hernandez N, Ghebremichael SJ, Sen S, et al. Opioid-free cesarean section with bilateral quadratus lumborum catheters. Local Reg Anesth 2020;13:17–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Priya TK, Singla D, Talawar P, et al. Comparative efficacy of quadratus lumborum type-II and erector spinae plane block in patients undergoing caesarean section under spinal anaesthesia: a randomised controlled trial. Int J Obstet Anesth 2023;53:103614. [DOI] [PubMed] [Google Scholar]
- 30.Irwin R, Stanescu S, Buzaianu C, et al. Quadratus lumborum block for analgesia after caesarean section: a randomised controlled trial. Anaesthesia 2020;75:89–95. [DOI] [PubMed] [Google Scholar]
- 31.Aditianingsih D, Pryambodho, Anasy N, et al. A randomized controlled trial on analgesic effect of repeated Quadratus Lumborum block versus continuous epidural analgesia following laparoscopic nephrectomy. BMC Anesthesiol 2019;19:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Korgvee A, Veskimae E, Huhtala H, et al. Posterior quadratus lumborum block versus epidural analgesia for postoperative pain management after open radical cystectomy: a randomized clinical trial. Acta Anaesthesiol Scand 2023;67:347–355. [DOI] [PubMed] [Google Scholar]
- 33.Dam M, Hansen CK, Poulsen TD, et al. Transmuscular quadratus lumborum block for percutaneous nephrolithotomy reduces opioid consumption and speeds ambulation and discharge from hospital: a single centre randomised controlled trial. Br J Anaesth 2019;123:e350–e358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zacha S, Andrzejewska A, Jastrzebska-Ligocka B, et al. Intercostal nerve cryoanalgesia in the treatment of pain in patients operated on by the modified Nuss method with the BackOnFeet application-a new strategy to improve outcomes. Front Pediatr 2022;10:1069805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Raof RA, El MS, Alia DA, et al. Dexmedetomidine decreases the required amount of bupivacaine for ultrasound-guided transversus abdominis plane block in pediatrics patients: a randomized study. J Clin Anesth 2017;37:55–60. [DOI] [PubMed] [Google Scholar]
- 36.Abdellatif AA, Kasem AA, Bestarous JN, et al. Efficacy of dexmedetomidine as an adjuvant to Quadratus lumborum block for pediatrics undergoing laparoscopic pyeloplasty. A prospective randomized double blinded study. Minerva Anestesiol 2020;86:1031–1038. [DOI] [PubMed] [Google Scholar]
- 37.Oksuz G, Bilal B, Gurkan Y, et al. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med 2017;42:674–679. [DOI] [PubMed] [Google Scholar]
- 38.Ipek CB, Kara D, Yilmaz S, et al. Comparison of ultrasound-guided transversus abdominis plane block, quadratus lumborum block, and caudal epidural block for perioperative analgesia in pediatric lower abdominal surgery. Turk J Med Sci 2019;49:1395–1402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liu KY, Lu YJ, Lin YC, et al. Transversus abdominis plane block for laparoscopic colorectal surgery: a meta-analysis of randomised controlled trials. Int J Surg 2022;104:106825. [DOI] [PubMed] [Google Scholar]
- 40.Viderman D, Aubakirova M, Abdildin YG. Transversus abdominis plane block in colorectal surgery: a meta-analysis. Front Med (Lausanne) 2021;8:802039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Oh TK, Yim J, Kim J, et al. Effects of preoperative ultrasound-guided transversus abdominis plane block on pain after laparoscopic surgery for colorectal cancer: a double-blind randomized controlled trial. Surg Endosc 2017;31:127–134. [DOI] [PubMed] [Google Scholar]
- 42.Carney J, Finnerty O, Rauf J, et al. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthesia 2011;66:1023–1030. [DOI] [PubMed] [Google Scholar]
- 43.Huang D, Song L, Li Y, et al. Posteromedial quadratus lumborum block versus transversus abdominal plane block for postoperative analgesia following laparoscopic colorectal surgery: a randomized controlled trial. J Clin Anesth 2020;62:109716. [DOI] [PubMed] [Google Scholar]
- 44.Wang D, He Y, Chen X, et al. Ultrasound guided lateral quadratus lumborum block enhanced recovery in patients undergoing laparoscopic colorectal surgery. Adv Med Sci 2021;66:41–45. [DOI] [PubMed] [Google Scholar]
- 45.Liu X, Song T, Chen X, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in patients undergoing abdominal surgeries: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol 2020;20:53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wetmore DS, Dalal S, Shinn D, et al. Erector spinae plane block reduces immediate postoperative pain and opioid demand after minimally invasive transforaminal lumbar interbody fusion. Spine (Phila Pa 1976) 2023;10:1097; Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 47.Pan M, Li Q, Li S, et al. Percutaneous endoscopic lumbar discectomy: indications and complications. Pain Physician 2020;23:49–56. [PubMed] [Google Scholar]
- 48.Ammar MA, Taeimah M. Evaluation of thoracolumbar interfascial plane block for postoperative analgesia after herniated lumbar disc surgery: a randomized clinical trial. Saudi J Anaesth 2018;12:559–564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ueshima H, Hiroshi O. RETRACTED: Lumbar vertebra surgery performed with a bilateral posterior quadratus lumborum block. J Clin Anesth 2017;41:61. [DOI] [PubMed] [Google Scholar]
- 50.Iwamitsu R, Ueshima H, Otake H. RETRACTED: Intermittent bilateral posterior quadratus lumborum block was effective for pain management in lumbar spinal fusion. J Clin Anesth 2017;42:16. [DOI] [PubMed] [Google Scholar]
- 51.Alver S, Bahadir C, Tahta AC, et al. The efficacy of ultrasound-guided anterior quadratus lumborum block for pain management following lumbar spinal surgery: a randomized controlled trial. BMC Anesthesiol 2022;22:394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wilton J, Chiu H, Codianne N, et al. Continuous quadratus lumborum block as post-operative strategy for pain control in spinal fusion surgery. Indian J Anaesth 2020;64:869–873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ciftci B, Ekinci M, Celik EC, et al. Ultrasound-guided erector spinae plane block versus modified-thoracolumbar interfascial plane block for lumbar discectomy surgery: a randomized, controlled study. World Neurosurg 2020;144:e849–e855. [DOI] [PubMed] [Google Scholar]
- 54.Elsharkawy H, El-Boghdadly K, Kolli S, et al. Injectate spread following anterior sub-costal and posterior approaches to the quadratus lumborum block: a comparative cadaveric study. Eur J Anaesthesiol 2017;34:587–595. [DOI] [PubMed] [Google Scholar]
- 55.Blanco R, Ansari T, Riad W, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med 2016;41:757–762. [DOI] [PubMed] [Google Scholar]
- 56.Mitchell KD, Smith CT, Mechling C, et al. A review of peripheral nerve blocks for cesarean delivery analgesia. Reg Anesth Pain Med 2019;10:1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Visoiu M, Pan S. Quadratus lumborum blocks: two cases of associated hematoma. Paediatr Anaesth 2019;29:286–288. [DOI] [PubMed] [Google Scholar]
- 58.Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthesia 2017;72:230–232. [DOI] [PubMed] [Google Scholar]
- 59.Sa M, Cardoso JM, Reis H, et al. Quadratus lumborum block: are we aware of its side effects? A report of 2 cases. Braz J Anesthesiol 2018;68:396–399. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data quoted in the paper are extracted from available published literature.


