Abstract
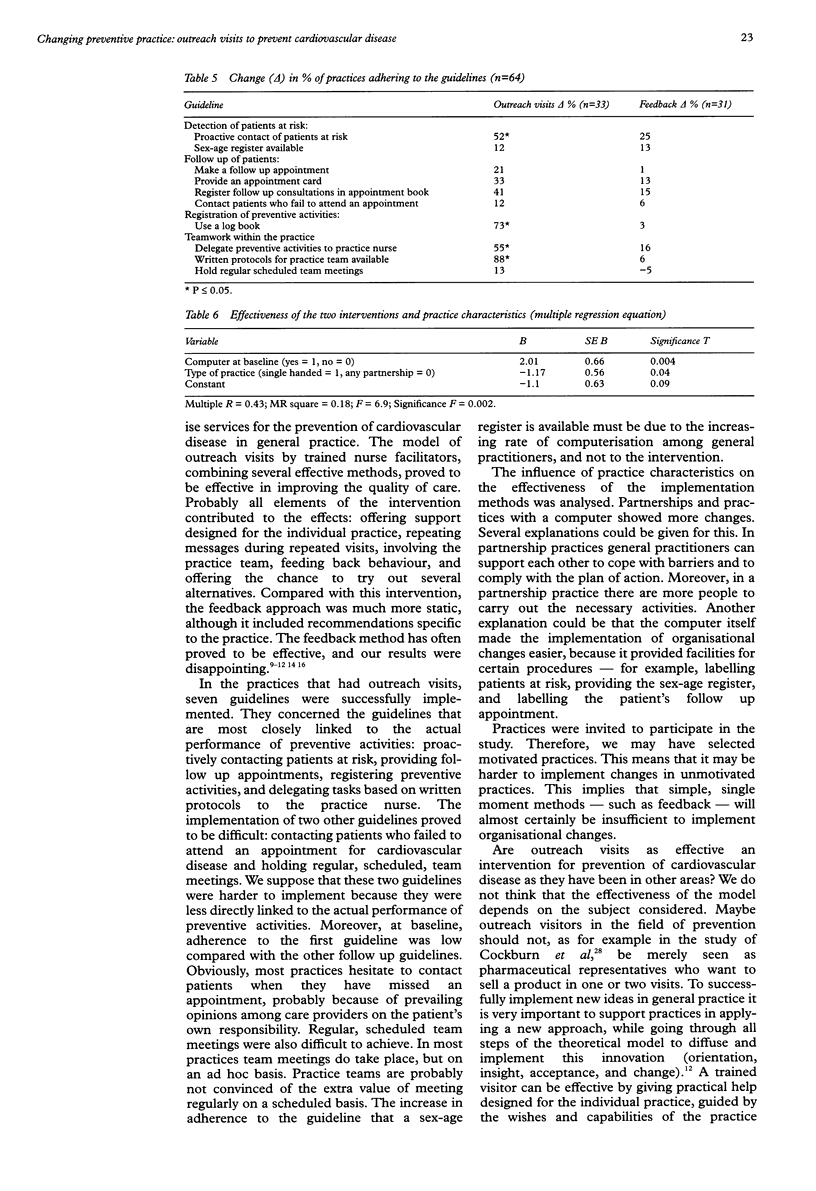
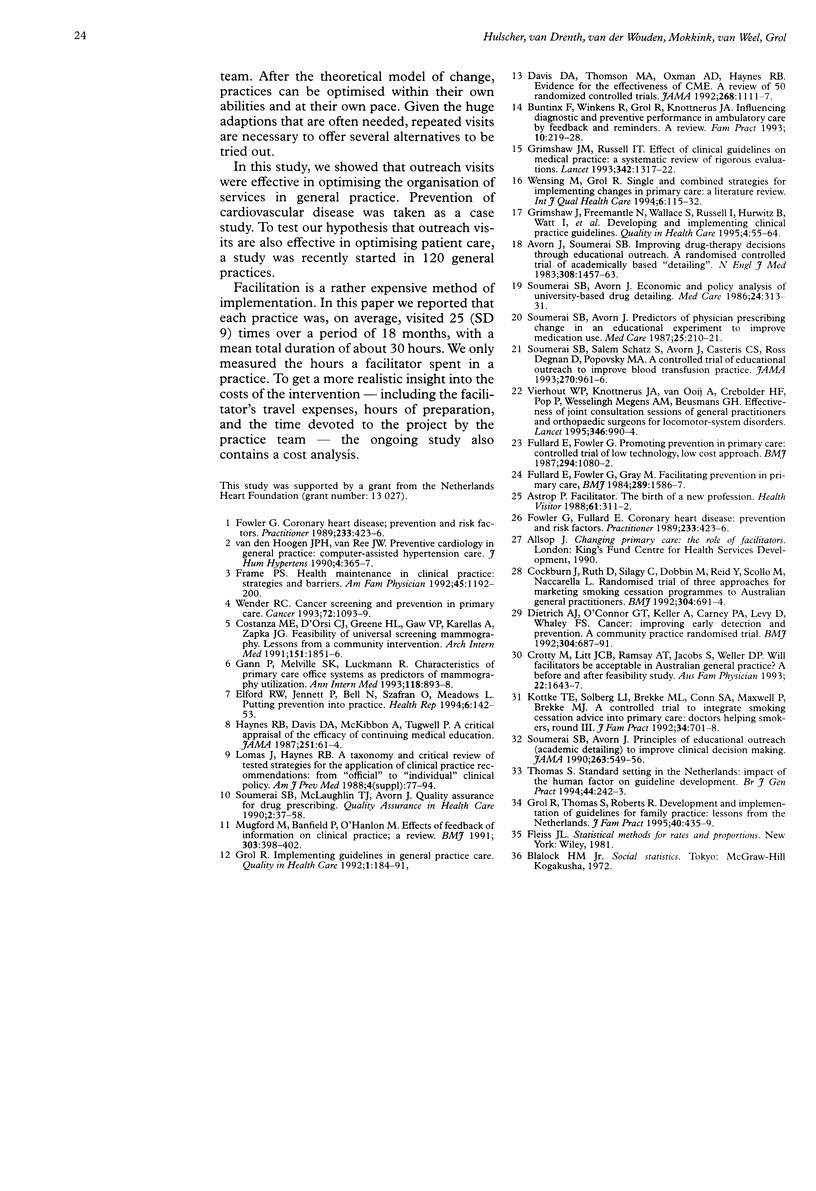
OBJECTIVES: To assess the effects of outreach visits by trained nurse facilitators on the organisation of services used to prevent cardiovascular disease. To identify the characteristics of general practices that determined success. DESIGN: A non-randomised controlled trial of two methods of implementing guidelines to organise prevention of cardiovascular disease: an innovative outreach visit method compared with a feedback method. The results in both groups were compared with data from a control group. SETTING AND SUBJECTS: 95 general practices in two regions in The Netherlands. INTERVENTIONS: Trained nurse facilitators visited practices, focusing on solving problems in the organisation of prevention. They applied a four step model in each practice. The number of visits depended on the needs of the practice team. The feedback method consisted of the provision of a feedback report with advice specific to each practice and standardised instructions. MAIN OUTCOME MEASURES: The proportion of practices adhering to 10 different guidelines. Guidelines were on the detection of patients at risk, their follow up, the registration of preventive activities, and teamwork within the practice. RESULTS: Outreach visits were more effective than feedback in implementing guidelines to organise prevention. Within the group with outreach visits, the increase in the number of practices adhering to the guidelines was significant for six out of 10 guidelines. Within the feedback group, a comparison of data before and after intervention showed no significant differences. Partnerships and practices with a computer changed more. CONCLUSION: Outreach visits by trained nurse facilitators proved to be effective in implementing guidelines within general practices, probably because their help was practical and designed for the individual practice, guided by the wishes and capabilities of the practice team.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Astrop P. Facilitator--the birth of a new profession. Health Visit. 1988 Oct;61(10):311–312. [PubMed] [Google Scholar]
- Avorn J., Soumerai S. B. Improving drug-therapy decisions through educational outreach. A randomized controlled trial of academically based "detailing". N Engl J Med. 1983 Jun 16;308(24):1457–1463. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- Buntinx F., Winkens R., Grol R., Knottnerus J. A. Influencing diagnostic and preventive performance in ambulatory care by feedback and reminders. A review. Fam Pract. 1993 Jun;10(2):219–228. doi: 10.1093/fampra/10.2.219. [DOI] [PubMed] [Google Scholar]
- Cockburn J., Ruth D., Silagy C., Dobbin M., Reid Y., Scollo M., Naccarella L. Randomised trial of three approaches for marketing smoking cessation programmes to Australian general practitioners. BMJ. 1992 Mar 14;304(6828):691–694. doi: 10.1136/bmj.304.6828.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costanza M. E., D'Orsi C. J., Greene H. L., Gaw V. P., Karellas A., Zapka J. G. Feasibility of universal screening mammography. Lessons from a community intervention. Arch Intern Med. 1991 Sep;151(9):1851–1856. [PubMed] [Google Scholar]
- Crotty M., Litt J. C., Ramsay A. T., Jacobs S., Weller D. P. Will facilitators be acceptable in Australian general practice? A before and after feasibility study. Aust Fam Physician. 1993 Sep;22(9):1643–1647. [PubMed] [Google Scholar]
- Davis D. A., Thomson M. A., Oxman A. D., Haynes R. B. Evidence for the effectiveness of CME. A review of 50 randomized controlled trials. JAMA. 1992 Sep 2;268(9):1111–1117. [PubMed] [Google Scholar]
- Dietrich A. J., O'Connor G. T., Keller A., Carney P. A., Levy D., Whaley F. S. Cancer: improving early detection and prevention. A community practice randomised trial. BMJ. 1992 Mar 14;304(6828):687–691. doi: 10.1136/bmj.304.6828.687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elford R. W., Jennett P., Bell N., Szafran O., Meadows L. Putting prevention into practice. Health Rep. 1994;6(1):142–153. [PubMed] [Google Scholar]
- Fowler G., Fullard E. Coronary heart disease: prevention and risk factors. Practitioner. 1989 Mar 22;233(1465):423–426. [PubMed] [Google Scholar]
- Fowler G., Fullard E. Coronary heart disease: prevention and risk factors. Practitioner. 1989 Mar 22;233(1465):423–426. [PubMed] [Google Scholar]
- Frame P. S. Health maintenance in clinical practice: strategies and barriers. Am Fam Physician. 1992 Mar;45(3):1192–1200. [PubMed] [Google Scholar]
- Fullard E., Fowler G., Gray M. Promoting prevention in primary care: controlled trial of low technology, low cost approach. Br Med J (Clin Res Ed) 1987 Apr 25;294(6579):1080–1082. doi: 10.1136/bmj.294.6579.1080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gann P., Melville S. K., Luckmann R. Characteristics of primary care office systems as predictors of mammography utilization. Ann Intern Med. 1993 Jun 1;118(11):893–898. doi: 10.7326/0003-4819-118-11-199306010-00011. [DOI] [PubMed] [Google Scholar]
- Grimshaw J. M., Russell I. T. Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet. 1993 Nov 27;342(8883):1317–1322. doi: 10.1016/0140-6736(93)92244-n. [DOI] [PubMed] [Google Scholar]
- Grimshaw J., Freemantle N., Wallace S., Russell I., Hurwitz B., Watt I., Long A., Sheldon T. Developing and implementing clinical practice guidelines. Qual Health Care. 1995 Mar;4(1):55–64. doi: 10.1136/qshc.4.1.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grol R. Implementing guidelines in general practice care. Qual Health Care. 1992 Sep;1(3):184–191. doi: 10.1136/qshc.1.3.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grol R., Thomas S., Roberts R. Development and implementation of guidelines for family practice: lessons from The Netherlands. J Fam Pract. 1995 May;40(5):435–439. [PubMed] [Google Scholar]
- Haynes R. B., Davis D. A., McKibbon A., Tugwell P. A critical appraisal of the efficacy of continuing medical education. JAMA. 1984 Jan 6;251(1):61–64. [PubMed] [Google Scholar]
- Kottke T. E., Solberg L. I., Brekke M. L., Conn S. A., Maxwell P., Brekke M. J. A controlled trial to integrate smoking cessation advice into primary care practice: Doctors Helping Smokers, Round III. J Fam Pract. 1992 Jun;34(6):701–708. [PubMed] [Google Scholar]
- Mugford M., Banfield P., O'Hanlon M. Effects of feedback of information on clinical practice: a review. BMJ. 1991 Aug 17;303(6799):398–402. doi: 10.1136/bmj.303.6799.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soumerai S. B., Avorn J. Economic and policy analysis of university-based drug "detailing". Med Care. 1986 Apr;24(4):313–331. doi: 10.1097/00005650-198604000-00003. [DOI] [PubMed] [Google Scholar]
- Soumerai S. B., Avorn J. Predictors of physician prescribing change in an educational experiment to improve medication use. Med Care. 1987 Mar;25(3):210–221. doi: 10.1097/00005650-198703000-00005. [DOI] [PubMed] [Google Scholar]
- Soumerai S. B., Avorn J. Principles of educational outreach ('academic detailing') to improve clinical decision making. JAMA. 1990 Jan 26;263(4):549–556. [PubMed] [Google Scholar]
- Soumerai S. B., McLaughlin T. J., Avorn J. Quality assurance for drug prescribing. Qual Assur Health Care. 1990;2(1):37–58. doi: 10.1093/intqhc/2.1.37. [DOI] [PubMed] [Google Scholar]
- Soumerai S. B., Salem-Schatz S., Avorn J., Casteris C. S., Ross-Degnan D., Popovsky M. A. A controlled trial of educational outreach to improve blood transfusion practice. JAMA. 1993 Aug 25;270(8):961–966. [PubMed] [Google Scholar]
- Thomas S. Standard setting in The Netherlands: impact of the human factor on guideline development. Br J Gen Pract. 1994 Jun;44(383):242–243. [PMC free article] [PubMed] [Google Scholar]
- Vierhout W. P., Knottnerus J. A., van OOij A., Crebolder H. F., Pop P., Wesselingh-Megens A. M., Beusmans G. H. Effectiveness of joint consultation sessions of general practitioners and orthopaedic surgeons for locomotor-system disorders. Lancet. 1995 Oct 14;346(8981):990–994. doi: 10.1016/s0140-6736(95)91686-5. [DOI] [PubMed] [Google Scholar]
- Wender R. C. Cancer screening and prevention in primary care. Obstacles for physicians. Cancer. 1993 Aug 1;72(3 Suppl):1093–1099. doi: 10.1002/1097-0142(19930801)72:3+<1093::aid-cncr2820721326>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Wensing M., Grol R. Single and combined strategies for implementing changes in primary care: a literature review. Int J Qual Health Care. 1994 Jun;6(2):115–132. doi: 10.1093/intqhc/6.2.115. [DOI] [PubMed] [Google Scholar]
- van den Hoogen J. P., van Ree J. W. Preventive cardiology in general practice: computer-assisted hypertension care. J Hum Hypertens. 1990 Aug;4(4):365–367. [PubMed] [Google Scholar]



