Abstract
The purpose of this pilot study was to understand how historical oppression relates to changes in outcomes for people who participate in the culturally grounded Weaving Healthy Families (WHF) program (i.e., alcohol and drug use, symptoms of anxiety, parenting practices, and communal mastery [CM]). This nonexperimental and longitudinal design used repeated measures regression analysis and generalized estimating equations (GEE) to examine postintervention changes according to reported levels of historical oppression among 24 participants in eight families. How do postintervention changes differ for WHF participants reporting lower and higher levels of historical oppression? Results indicated that participants reporting lower historic oppression reported greater postintervention improvements as indicated by declines in alcohol use, anxiety, and poor parental monitoring. All participants reported increases in CM, regardless of the level of historical oppression. Given historical oppression drives psychosocial conditions, such as substance abuse, mental health, and family challenges, settler colonial oppression must be addressed within social service interventions. Social service providers must work redress historical oppression rather than replicate them. The WHF program holds promise to center structural determinants in social service programs. Future inquiries assessing longitudinal changes in perceptions of historical oppression change and how they are associated with psychosocial outcomes are needed.
Keywords: Indigenous, Native American, prevention, substance use and abuse, anxiety, parenting, community resilience, historical oppression, interventions, families, social service provision
Introduction
Structural oppression, in the form of historical oppression, may pose a risk and exacerbate psychosocial inequities among Indigenous peoples. Historical oppression undermines Indigenous peoples and families through historical traumas that have removed children from the socialization and care of their families, while also exposing them to forced assimilation, abuse, and trauma (Burnette & Figley, 2017; Linjean et al., 2022; Weaver et al., 2021). Historical oppression encompasses many atrocities of settler colonialism, structures that are imposed and replicated inter-generationally and drive persistent sociostructural and health inequities and environmental injustices (Burnette & Figley, 2017). Historical oppression, along with community and family resilience (including parenting), are well-documented factors driving the disproportionate levels of substance use disorder (SUD) and anxiety experienced by U.S. Indigenous peopled (Burnette & Figley, 2016; Gone & Trimble, 2012; Ka’apu & Burnette, 2019; Liddell & Burnette, 2017).
Settler colonial historical oppression is imposed and institutionalized through social service, religious, government, judicial, and educational systems (Burnette & Figley, 2017). The Council on Social Work Education (CSWE) endorsed statements acknowledging social work’s direct role in supporting colonizing practices through a report entitled, “CSWE statement of accountability and reconciliation for harms done to Indigenous and Tribal peoples”, along with an associated teaching tool (Weaver et al., 2021). Indigenous families were targeted through governmental policies enacted by social service providers (Weaver et al., 2021), including the 1860–1978 Boarding School Era and Indian Adoption Policy Act, where between 1941 and 1967 alone, 85% of Indigenous children were removed from their families (Weaver et al., 2021). Because family and psychosocial inequities stem from structural causes, family and parenting programs must situate these inequities in context. However, an absence of empirically informed family – and culturally grounded programs are available to promote these relational factors preclude mental health equity among these peoples (Burnette & Figley, 2016; Gone & Trimble, 2012).
Historical oppression drives disproportionately high prevalence of the primary presenting issues for Indigenous peoples seeking social service treatment: substance abuse, mental health, and family challenges. Indeed, historical oppression may predict psychosocial health inequities, and in fact, explain many psychosocial health inequities experienced by Indigenous peoples. Connecting psychosocial conditions to structural causes may ameliorate internalized oppression and externalizing factors, such as SUD and poor parenting (McKinley, Boel-Studt, et al., 2020; McKinley, Miller Scarnato, et al., 2020). Yet, to our knowledge, existing programs have not incorporated historical oppression into their framework, nor is it known whether such a program prevent SUD and promotes psychosocial health and family resilience Indigenous peoples describe the heterogeneous groups of peoples who are the original inhabitants of the United States and share a history of settler colonization (for this inquiry, the scope is limited to U.S. Indigenous peoples). The persistent and disproportionately high rates of SUD occur across the lifespan and drive increased mortality rates (Whitesell et al., 2012). Indeed, U.S. Indigenous peoples die an average of 5–6 years earlier than non-Indigenous peoples (at age 73 compared to at age 78.5; Indian Health Service, 2019). SUD is also closely associated with mental health disorders, including anxiety, post-traumatic stress disorder (PTSD), suicide, depression, and family violence (Masten & Monn, 2015).
Despite historical oppression being a primary driver of health inequities, an absence of empirical and culturally grounded family programs that integrate historical oppression to promote behavioral and mental health precludes health equity for Indigenous peoples (Burnette & Figley, 2016; Gone & Trimble, 2012). Existing programs tend not to integrate the centrality of family (Klostermann et al., 2010; Kraanen et al., 2013; Tutty, 2013) or culture (Urban Indian, 2014). Griner and Smith (2006) found culturally grounded programs are approximately four times more effective than nonculturally specific interventions. Culturally relevant interventions reduce risk for harm (Griner & Smith, 2006; Whitbeck et al., 2012), as nonculturally specific interventions have worsened substance use outcomes for Indigenous youth (Dixon et al., 2007). Yet, culturally grounded interventions are scarce; only 20% of SUD interventions for Indigenous youth are culturally specific (Urban Indian, 2014). Moreover, although family-based SUD interventions have reported effect sizes two to nine times higher than child-centered interventions (Tutty, 2013), a systematic review of such interventions found none were family-based (Liddell & Burnette, 2017). This absence of family-based interventions is a critical barrier to SUD prevention, given that parental SUD is a primary determinant of youth SUD (Burnette & Figley, 2016; Dusenbury, 2000). The absence of family and cultural programs also represents an alarming neglect of the U.S. federal government’s trust responsibility – through around 400 treaties with 564 sovereign tribes – to ensure Indigenous peoples’ health and wellness (Bureau of Indian Affairs, 2021; Le & Aptekar, 2019).
This study examined the Weaving Healthy Families (WHF), or Chukka Auchaffi’ Natana (in Choctaw), program (McKinley & Theall, 2021), which integrates the culturally grounded FHORT (Burnette & Figley, 2017) to understand how differing levels of historical oppression are related to significant differences in change on key ecological factors before and after participation in the WHF program. This research study addresses the gap in culturally grounded programs and was developed through systematic community-based participatory research (CBPR) addressing the primary drivers of physical, mental, and behavioral health inequities. The purpose of this longitudinal study was to examine how participants reporting high and low levels of historical oppression who complete the WHF differ in changes across outcomes falling across ecological levels over time, including (a) individual: of alcohol and drug use and symptoms of anxiety; (b) relational: parenting practices; (c) community: communal mastery (CM).
The Weaving Healthy Families Program: Chukka Auchaffi’ Natana (in Choctaw)
The WHF program was developed through a decade of CBPR with more than a thousand Indigenous peoples (McKinley, Figley, et al., 2019; McKinley, Miller Scarnato, et al., 2019; McKinley & Theall, 2021; McKinley et al., 2023). Whitbeck’s (2006) guidance on developing culturally grounded SUD interventions with Indigenous peoples framed the WHF program development. The WHF is an adapted and abridged form of the “Celebrating Families!” program (National Association for Children of Alcoholics [NACA], 2011; White Bison, 2015). The WHF is a holistic, relational, and wellness-based approach to SUD and violence prevention that promotes wellness and resilience by infusing the Indigenous FHORT, an empirically based framework developed through over a decade of research with the focal tribal communities (Burnette & Figley, 2017).
The WHF program consisted of 10 sessions lasting two-and-a-half hours each and covered SUD and violence prevention and family and community wellness across mental and behavioral dimensions. The WHF program focused on promoting the skills necessary to offset SUD and violence while building family resilience and wellness though such topics as healthy living, communication, managing emotions, substance use and the family, setting goals, making positive choices and problem solving, setting boundaries and fostering healthy relationships, promoting resilience, and celebrating personal and familial accomplishments. The program also incorporated talking circles and smudging.
The WHF was facilitated by Indigenous community health representatives (CHRs) who reside in the local community. Family participants included all household members, including extended and adopted family members. The program structure began with a family meal to promote positive family rituals, after which families split into developmental age groups (e.g., parents, adolescents [ages 12–17], children [ages 8–11], and young children [ages 5–7]) to share with talking circles and learn about the session topic in developmentally tailored ways. Finally, families rejoin and reinforce teachings in fun and experiential ways while spending quality time together (McKinley & Theall, 2021). Two CHRs facilitated each age group and two lead CHRs coordinated operations, including conducting weekly fidelity checks and assisting CHRs with implementation. Each CHR attended at least 6 d of training, in which they learned and practiced facilitating the WHF program.
Both the WHF and FHORT promote resilience, or the recovery, adaptation, and skills needed to overcome adversity (Burnette & Figley, 2017; Masten & Monn, 2015; McKinley & Theall, 2021). FHORT targets wellness promotion by enhancing ecological risk, promotive, and protective factors across structural, community, cultural, familial, and individual levels (Burnette & Figley, 2017). The WHF promotes cultural, community, family, and individual health by infusing the FHORT into its sessions and contextualizes problems within the historical and structural oppression that has imposed and perpetuated them (Burnette & Figley, 2017). The WHF program integrates an Indigenous wellness approach by integrating the FHORT medicine wheel approach to wellness, including psycho-social, mental, spiritual, physical dimensions emotional, and environmental aspects of health (Burnette & Figley, 2017). The frames settler colonization as a structural determinant of health and extends pathways to resilience through incorporation of tribal values and culturally teachings (McKinley & Theall, 2021).
As depicted in Figure 1, FHORT examines risk, promotive, and protective factors across ecological levels to predict wellness, or the balance of mental, behavioral, spiritual, physical, social, familial, community, and structural levels. This article examines how the WHF program is associated with changes in risk (signified by −) and protective (signified by +) factors across, community (+CM), familial (+positive parenting and − poor monitoring), and mental and behavioral (−alcohol and − drug use and − anxiety) dimensions for participants reporting higher levels of historical oppression compared to those reporting lower levels.
Figure 1.
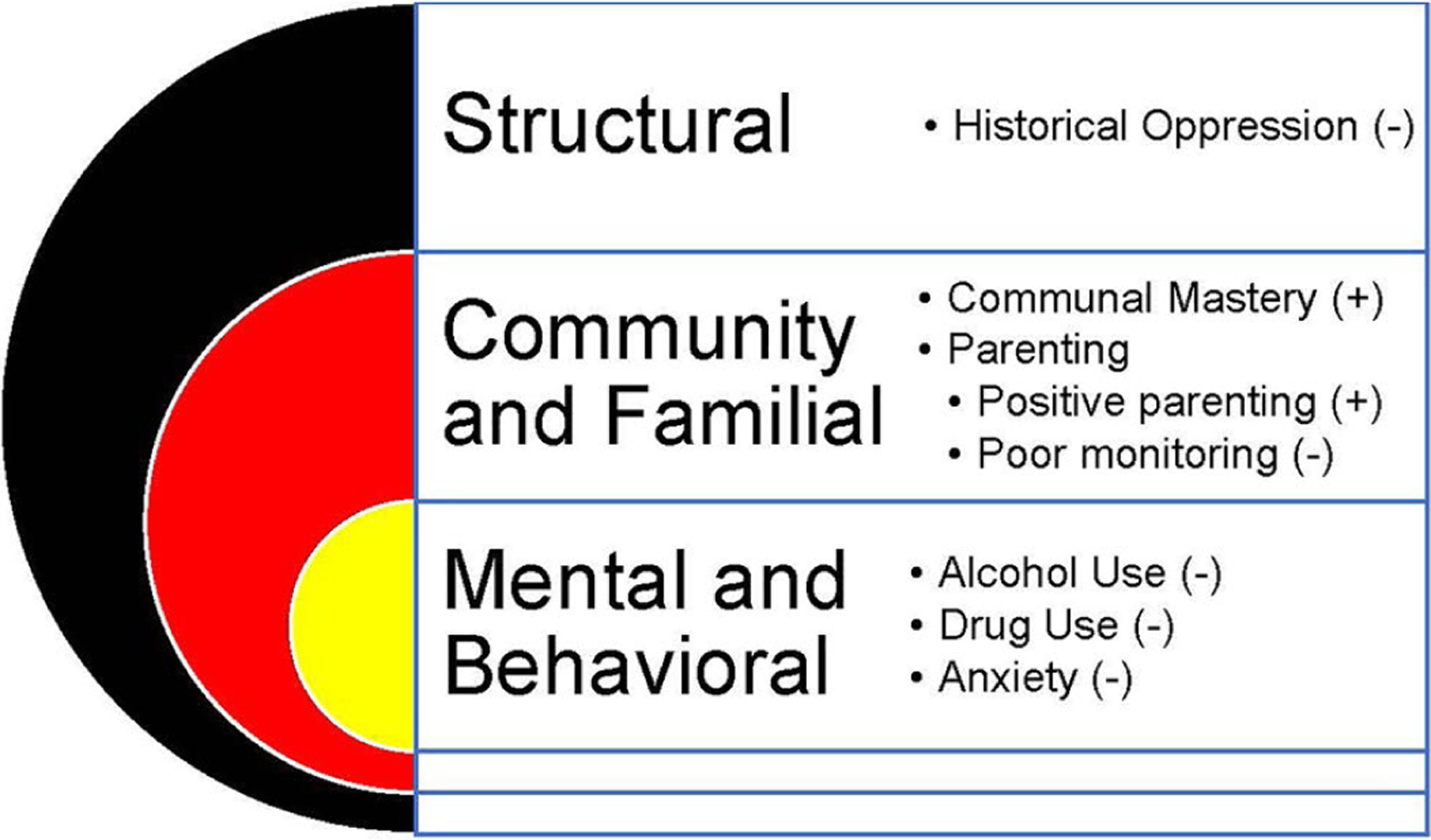
Note. (+) indicates protective or promotive factors, whereas (−) indicates risk factors. The FHORT examines risk, promotive, and protective factors across ecological levels to predict wellness, or balance across mental, behavioral, spiritual, physical, social, familial, community, and structural levels. for this inquiry, we examined how the WHF program is associated with changes in risk and protective factors across structural (−historical oppression), community (+communal mastery), familial (+positive parenting and −poor monitoring), and mental/behavioral (−alcohol and −drug use and −anxiety) levels for those reporting higher levels of historical oppression compared to those reporting lower levels of historical oppression.
The WHF is a culturally and family-grounded cognitive-behavioral and psychoeducational prevention program that promotes wellness by using a medicine wheel and its mental, social, spiritual, emotional, and physical domains of health. The program enhances participants’ skills and resilience in matters related to relationships, healthy living, problem-solving, parenting practices (e.g., setting and retaining limits, affirming children, communicating with children), SUD, boundaries, violence prevention, and emotional regulation (see Figure 2). The WHF also integrates cultural components (see Figure 3); tribal foodways are integrated with meals, for example, and talking circles are used to foster culturally congruent communication, ceremonies, and conflict resolution (McKinley & Theall, 2021).
Figure 2.
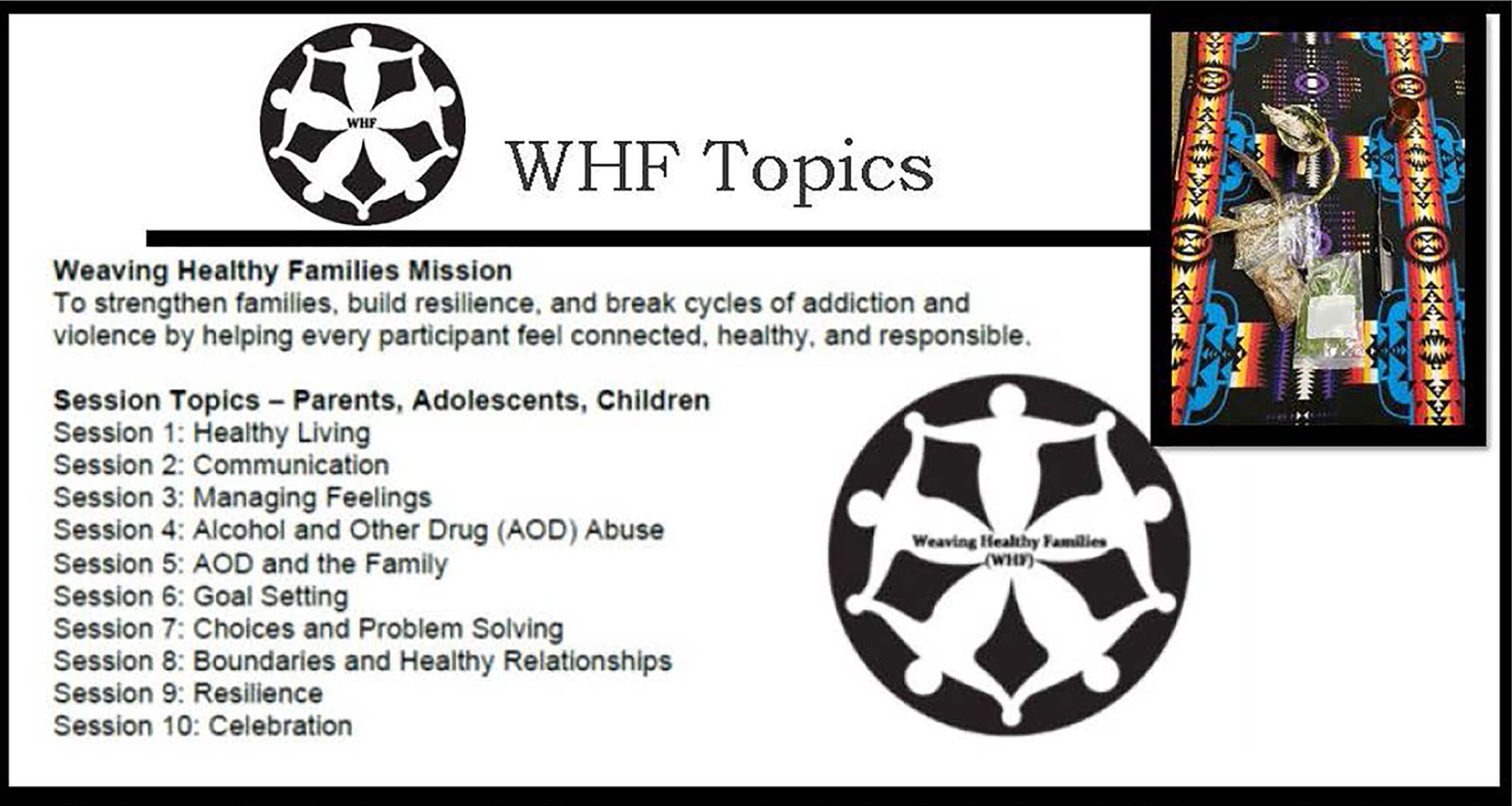
Weaving healthy families Program Topics.
Note. The WHF program focused on promoting the skills necessary tooffset SUD and violence while building family resilience and wellness through topics including:healthy living, communication, managing emotions, substance use and the family, setting goals,making positive choices and problem solving, setting boundaries and fostering healthyrelationships, promoting resilience, and celebrating personal and familial accomplishments. The WHF incorporated talking circles and smudging (top right).
Figure 3.
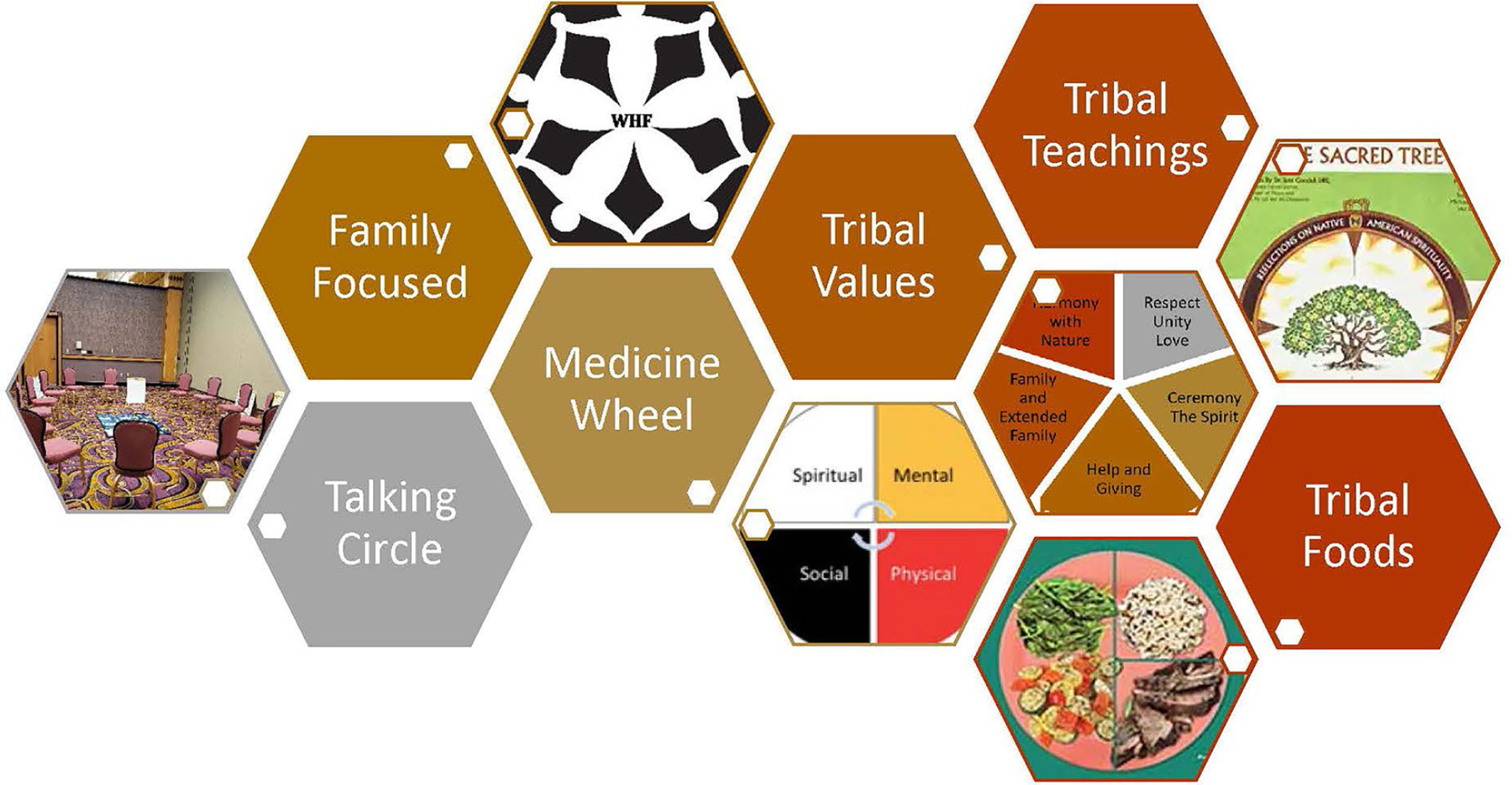
Snapshot of WHF cultural components.
Past WHF intervention research found improvements in violence and conflict resolution, substance use, emotional regulation, mental health, health behaviors, resilience, social support, and family and parenting skills (McKinley & Theall, 2021). This article extends these findings by examining differential changes in the following ecological outcomes among WHF participants reporting higher and lower levels of historical oppression: (a) behavioral, defined as alcohol and drug use; (b) mental, defined as symptoms of anxiety; (c) familial, defined as positive parenting and poor parental monitoring; and (d) community, defined as CM. Our focus now turns to these constructs.
Family and community protective factors associated with mental and behavioral health
Parental and community factors are well-established risk and protective factors for mental and behavioral outcomes among Indigenous youth and adults. Parenting quality is a well-documented promotive factor that prevents mental health problems and SUD (Burnette & Figley, 2016). A systematic review of risk and protective factors for mental and behavioral inequities among Indigenous youth reported positive parenting practices have extensive implications for Indigenous wellness, as they were associated with the prevention of substance use, suicide, and depression; poor parental practices, in contrast, posed risks (Burnette & Figley, 2016). Parental warmth and connection have also been found to prevent Indigenous youth SUD (Cheadle & Whitbeck, 2011; LaFromboise et al., 2006).
Community and family support are associated with family resilience (McKinley et al., 2021) and protect against mental health problems. For example, community and social support are associated with lower levels of PTSD (McKinley, Figley, et al., 2019; McKinley, Miller Scarnato, et al., 2019), suicide (FitzGerald et al., 2017; Hill, 2009), anxiety (McKinley et al., 2021), and depression (Schure & Goins, 2017). CM is “defined as the belief that one is capable of successful goal attainment by being closely interconnected with others” (Hobfoll et al., 2002, p. 362). It is considered to be a form of community resilience that includes community efficacy, connection and strength, and has been found to promote wellness and an ability to overcome challenges (Hobfoll et al., 2002; Meyer, 2015).
Historical oppression driving SUD and mental health inequities
Historical oppression has been linked with mental and behavioral outcomes. As predicted by the FHORT, historical oppression and greater daily stress were associated with higher depressive symptoms, whereas family resilience and life satisfaction, measures of transcendence, were both associated with lower depressive symptoms (Burnette et al., 2019). Research has found that while spiritual well-being and family resilience were associated with lower depressive symptoms, historical losses, contemporary and proximal stress (e.g., stress from recent loss of a loved one), and oppression (e.g., structural oppression in the form of lower income) were associated with higher symptoms of depression (McKinley, Boel-Studt, et al., 2020; McKinley, Miller Scarnato, et al., 2020).
Research has found historical losses, such as language, family, spirituality, culture, land, culture, and respect for others, have been associated with mental and behavioral health problems among Indigenous youth (Burnette & Figley, 2016), including depressive symptoms (Whitbeck et al., 2004) and delinquent behaviors (Mmari et al., 2010). For adults, Evans-Campbell et al. (2012) identified historical oppression in the form of boarding school experiences and historical losses of land and culture increased risks for PTSD. Historical oppression in the form of trauma and loss, poverty, and unemployment were risks for suicide (Caetano et al., 2013). Historical oppression and loss were also risks for SUD (Whitbeck et al., 2004). Despite associations with historical oppression and behavioral, familial, and mental outcomes, no interventions incorporating or addressing historical oppression have been tested. This research study fills a gap in culturally grounded programs that approach SUD, anxiety, parenting, and CM with the FHORT and historical oppression in mind.
This research study goes beyond identifying structural, community, and familial factors associated with key mental and behavioral health inequities to exploring how a culturally grounded intervention incorporating the FHORT is associated with changes across ecological dimensions of wellness and moderated by historical oppression. This article examined the following overarching research question: How do postintervention changes differ for WHF participants reporting lower and higher levels of historical oppression? Hypotheses predict participants reporting lower levels of historical oppression would experience greater improvements in the following ecological outcomes: (a) behavioral: alcohol and drug use; (b) mental: symptoms of anxiety; (c) familial: positive parenting and poor parental monitoring; and (d) community: CM.
Methods
Research design
This article extends previous research (McKinley, Figley, et al., 2019; McKinley, Miller Scarnato, et al., 2019; McKinley & Theall, 2021; McKinley et al., 2023), through a nonrandomized and pre-experimental pilot WHF intervention. Taking a nonexperimental and longitudinal design, survey data were collected across the following time-points: before the WHF program (pretest), immediately after the WHF program (posttest), and 6, 9, and 12 months after the completion of the WHF program. Repeated measures regression analysis using generalized estimating equations (GEE; Schober & Vetter, 2018) was used to understand how ecological outcomes differed before and after the WHF program for participants reporting high and low levels of historical oppression. (a) behavioral, defined as alcohol and drug use; (b) mental, defined as symptoms of anxiety; (c) familial, defined as positive parenting and poor parental monitoring; and (d) community, defined as CM (see Figure 1).
Sample
Participant recruitment occurred through word of mouth and convenience sampling with the community advisory board and CHRs. Data for this article were drawn from a broader pilot (McKinley & Theall, 2021); this article focuses on postintervention changes in outcomes as differentiated by initial levels of reported perceived historical oppression. Eight families enrolled in the program, all of whom completed all 10 sessions and program components (McKinley & Theall, 2021). Participants included family members ages 5 and older, but the scope of this inquiry is limited to participants ages 12 and older as they were given measures of the study’s focal outcomes (with the exception of the substance use and parenting measures, which were only given to the adults). Eligible families included those with: (a) at least one Indigenous caregiver or parent; (b) an adolescent child between the ages of 12 and 17; (c) availability to attend sessions; and (d) the ability to complete online surveys with assistance. No families with active addiction or safety concerns participated in this prevention program, as such challenges would warrant a higher level of care.
Families were recruited from a federally recognized Southeastern tribe whose identity is kept confidential to honor tribal agreements and to follow recommendations for culturally sensitive and ethical research with tribes (Burnette et al., 2014; McKinley, Figley, et al., 2019; McKinley, Miller Scarnato, et al., 2019). These tribal communities have their own educational, family services, law enforcement, behavioral health, social services, and criminal justice systems. Session locations were determined by the community advisory board and held at a local site accessible to all families and large enough to hold the CHRs and all eight families, which comprised 35 participants: parents (n = 14), adolescents ages 12–17 (n = 10), children ages 8–11 (n = 8), and young children ages 5–7 (n = 3). The scope of this study included the 24 adults and adolescents (see Table 1 for the demographics of the sample).
Table 1.
Participant demographics (n = 24).
| Demographic characteristics | Adult sample (n = 14) | Adolescent sample (n = 10) |
|---|---|---|
| n (%) | n (%) | |
| Participant sex | ||
| Male | 5 (35.71) | 6 (60.00) |
| Female | 9 (64.29) | 4 (40.00) |
| Age at pretest (M) | 34 (range 19–48) | 13.80 (range 12–17) |
| Yes | 12 (85.71) | 10 (100.00) |
| No | 2 (14.29) | - |
| Relationship status | ||
| Married | 6 (42.86) | - |
| Single | 4 (28.57) | - |
| cohabitating | 3 (21.43) | - |
| Divorced | 1 (7.14) | - |
| Annual household income | ||
| $15,000–$25,000 | 1 (7.14) | - |
| $25,001–$50,000 | 13 (92.86) | - |
| Financial difficulty | ||
| Very difficult | 2 (14.29) | - |
| Somewhat difficult | 7 (50.00) | - |
| A little difficult | 5 (35.71) | - |
| Not at all difficult | 0 (0.00) | |
| Working full-time | 11 (91.67) | - |
| Education | ||
| Some high school | 3 (21.43) | - |
| High school/GED | 3 (21.43) | - |
| Some college | 6 (42.86) | - |
| Bachelor’s degree | 2 (14.29) | - |
| M (SD) | ||
| Average household size at pretest | 6.14 (range 2–8) | - |
| Average number of biological children | 3.71 (1.94) | |
Note. Reported from the adult and adolescent sample at pretest only. Financial difficulty indicated: “In your opinion, how difficult is it for you and your family to live on your current monthly income at this time”. Adapted table reprinted with permission from McKinley et al., 2023.
Procedure
Approvals from the university institutional review board and tribal council, along with written informed consent and assent from each participant, were acquired prior to data collection, which occurred from August 2019 to October 2020. Participants received $50 on Clincards, from which they could withdraw cash or use as credit, for completing each of the pretest, posttest, and 6-, 9-, and 12-month follow-up online surveys using REDCap electronic data capture tools hosted by Tulane University (Harris et al., 2019). Individual survey links and offers of assistance with survey completion were sent to participants’ email addresses, along with phone and text reminders.
Instruments
Table 2 displays all measures and their scoring information. Following Whitbeck’s (2006) recommendations for developing culturally grounded interventions, all measures have been piloted with the focal tribe (Burnette et al., 2019). Historical oppression was assessed using the historical oppression scale (HOS), which was developed, tested, and validated through a decade of mixed methods research with the focal tribe (see Supplemental Materials; McKinley, Boel-Studt, et al., 2020; McKinley, Miller Scarnato, et al., 2020). Alcohol use was assessed using the Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993), drug use and abuse was assessed using the Drug Abuse Screening Test (DAST; Skinner, 1982), and symptoms of anxiety were assessed with the Generalized Anxiety Disorder Scale (GAD; Spitzer et al., 2006). Parenting practices were assessed with the positive parenting and poor monitoring subscales of the Alabama Parenting Questionnaire-Short Form (APQ; Kyriazos & Stalikas, 2019). CM, a measure of community resilience as indicated by a collective sense of self-efficacy, was measured with the CM scale (Hobfoll et al., 2002).
Table 2.
Table of measures.
| Name | Number of items | Purpose | Examples of items | Response type | Scoring | cronbach’s alpha |
|---|---|---|---|---|---|---|
| HOSa | 10 | Historical oppression | “Have taken out frustrations on each other and hurt each other (through family and community violence).” | 1 (not at all) to 5 (a great deal) | Total score obtained by adding all items. Higher scores reflect greater experiences of historical oppression. Range: 10–50. | Adult (a = 0.95) Adolescent (a = 0.96) combined (a = 0.96) |
| AUDITb | 13 | Frequency, number, and concern about alcohol consumption | “Has a relative or friend or doctor or another health worker been concerned about your drinking or suggested you cut down?” | 0 (never) to 4 (daily or almost daily) | Summed with scores ranging from 0 to 40 (0 = abstainer, 1–7 = low-risk; 8–14 = harmful alcohol consumption; 15 = likely alcohol dependence) |
(a = 0.938) |
| DASTc | 10 | Drug use and abuse | “Have you used drugs other than those required for medical reasons?” | 1 (yes) or 0 (no) | Summed with scores ranging from 0 to 10 (0 = no problem, 1–2 = low problem, 3–5 = moderate problem, 6–8 = substantial problem, 9–10 = severe problem) |
(a = 0.629) |
| GADd | 7 | Symptoms and impairment related to generalized anxiety | “Over the last two weeks, how often have you been bothered by the following problems: feeling nervous, anxious, or on edge; or worrying too much about different things?” | 0 (not at all) to 3 (nearly every day) | Summed with scores ranging from 0 to 21 (0–4 = minimal anxiety; 5–9 = mild anxiety; 10–14 = moderate anxiety; 15–21 = severe anxiety) |
(a = 0.952) |
| APQe | 6 | Assessment of parenting practices | Positive parenting: “You praise your child if he/she behaves well”; Poor monitoring: “Your child is out with friends you don’t know” | 1 (never) to 5 (always) | Total score obtained by adding scores for each subscale. Higher scores indicate higher levels of each subscale. | Positive parenting (a = 0.85) Poor monitoring (a = 0.88) |
| CMf | 10 | Perception of community resilience | “Working together with people close to me I can overcome most of the problems I have” | 1 (strongly disagree) to 4 (strongly agree) | Total score obtained by adding all items. Higher scores indicate higher levels of communal mastery. Range: 10–40 | Adult (a = 0.87) Adolescent (a = 0.82) combined (a = 0.86) |
Note.
Historical Oppression Scale (see Supplemental Materials for full scale),
Alcohol Use Disorders Identification Test,
Drug Abuse Screening Test,
Generalized Anxiety Disorder Scale,
Alabama Parenting Questionnaire,
Communal Mastery.
Data analysis
After confirming data normality, homogeneity of variance, the first and second authors scanned for outlier and missing data. After the second author did a preliminary scan, the first author, who was involved in all aspects of data collection and management removed outlier scores where there were clear errors. Where post-test scores were missing, the post-test median was imputed. Next descriptive statistics were examined before conducting repeated measures regressions with GEE to examine changes in key outcomes (Schober & Vetter, 2018) and modification by historical oppression. Strata of oppression were created based on the 75th percentile of HOS scores; the 30% of individual respondents (n = 7) with a score of 38 or above were classified as having high historical oppression and those with scores below 38 classified as having lower historical oppression. Unlike the most widely used statistical methods, GEE limits bias by not assuming independence of longitudinal observations (Schober & Vetter, 2018). GEE estimates expected means yet accounts for repeated measures within the same person and family may be more similar than different people from different families across units (Schober & Vetter, 2018).
Results
Table 3 presents the means and standard deviations at each time point of assessment (i.e., pretest, posttest, and 6, 9, and 12 months after the program) by age group (e.g., adults or adolescents) and by sex. Perceived historical oppression increased for adult females and adolescent males, whereas it decreased for adult males and adolescent females. Total historical oppression scores increased for both adolescents and adults, indicating greater awareness and reported perception of historical oppression after completing the program. On average, adult males indicated hazardous drinking levels but not at any point after completing the program.
Table 3.
Means by outcome, event, sex, and age.
| Event | PRE | POST | 6 Months | 9 Months | 12 Months | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Sex | Mean | SD | Mean | SD | Mean | SD | Mean | SD | Mean | SD |
| Historical oppression (n = 24) | Male | 27.50 | 10.55 | 26.00 | 15.99 | ||||||
| Female | 24.57 | 13.73 | 28.21 | 17.48 | |||||||
| Total | 25.79 | 12.34 | 27.29 | 16.55 | |||||||
| Adol. | 20.80 | 11.42 | 29.50 | 16.45 | |||||||
| Adult | 29.36 | 12.10 | 25.71 | 17.06 | |||||||
| Total | 25.79 | 12.34 | 27.29 | 16.55 | |||||||
| Positive parenting (n = 12) | Male | 12.75 | 1.50 | 13.00 | 2.45 | 12.75 | 2.87 | 13.75 | 1.50 | 14.75 | 1.26 |
| Female | 14.00 | 1.41 | 14.13 | 1.25 | 14.38 | 1.06 | 14.13 | 1.13 | 13.63 | 2.07 | |
| Total | 13.58 | 1.51 | 13.75 | 1.71 | 13.83 | 1.90 | 14.00 | 1.21 | 14.00 | 1.86 | |
| Poor monitoring (n = 12) | Male | 5.50 | 4.36 | 4.75 | 3.50 | 4.75 | 4.19 | 4.00 | 2.00 | 4.50 | 1.91 |
| Female | 3.75 | 1.16 | 4.00 | 1.41 | 4.13 | 1.55 | 3.75 | 1.04 | 4.50 | 1.69 | |
| Total | 4.33 | 2.61 | 4.25 | 2.18 | 4.33 | 2.53 | 3.83 | 1.34 | 4.50 | 1.68 | |
| Alcohol use (n = 12) | Male | 8.80 | 12.99 | 5.60 | 8.32 | 5.20 | 4.97 | 4.40 | 4.62 | 4.80 | 4.55 |
| Female | 4.56 | 6.21 | 2.11 | 3.33 | 1.78 | 2.28 | 4.13 | 6.13 | 2.89 | 4.11 | |
| Total | 6.07 | 8.95 | 3.36 | 5.58 | 3.00 | 3.70 | 4.23 | 5.39 | 3.57 | 4.20 | |
| Drug use (n = 12) | Male | 0.60 | 0.55 | 0.80 | 0.45 | 0.60 | 0.55 | .40 | 0.55 | 0.80 | 0.45 |
| Female | 0.44 | 1.01 | 0.56 | 0.53 | 0.33 | 0.50 | .63 | 0.74 | 0.44 | 0.53 | |
| Total | 0.50 | 0.85 | 0.64 | 0.50 | 0.43 | 0.51 | .54 | 0.66 | 0.57 | 0.51 | |
| Anxiety (n = 12) | Male | 3.60 | 3.78 | 2.00 | 2.83 | 0.40 | 0.55 | ||||
| Female | 5.33 | 7.25 | 4.67 | 5.50 | 3.00 | 4.66 | |||||
| Total | 4.71 | 6.12 | 3.71 | 4.78 | 2.07 | 3.89 | |||||
| Communal mastery (n = 24) | Male | 20.78 | 3.49 | 21.11 | 3.48 | 32.67 | 5.55 | ||||
| Female | 18.08 | 5.35 | 18.27 | 5.85 | 29.20 | 4.81 | |||||
| Total | 19.18 | 4.78 | 19.33 | 5.20 | 30.50 | 5.27 | |||||
| Adol. | 18.70 | 4.08 | 17.00 | 4.52 | 30.70 | 4.69 | |||||
| Adult | 17.21 | 8.38 | 19.57 | 4.40 | 29.36 | 5.30 | |||||
| Total | 17.83 | 6.84 | 18.50 | 4.54 | 29.92 | 4.99 | |||||
Note. Numbers displayed are mean (standard deviation). Historical oppression was assessed using the HOS (Historical Oppression Scale), alcohol use was assessed with AUDIT (Alcohol Use Disorders Identification Test), drug use was assessed with DAST (Drug Abuse Screening Test), anxiety was assessed with GAD (Generalized Anxiety Disorder Scale), positive parenting and poor monitoring were assessed using the APQ(Alabama Parenting Questionnaire), communal mastery was assessed using the CM ((Communal Mastery Scale), and discrimination was assessed using the EDS (Everyday Discrimination Scale). Adol.: Adolescent.
When examining historical oppression’s differential effects on outcomes, significant interaction or effect modification by historical oppression was demonstrated in the changes in alcohol use (interaction Z = −2.90, p < 0.01), symptoms of anxiety (interaction Z = −1.87, p = 0.05), and poor parental monitoring (interaction Z = −3.64, p < 0.01). Table 4 presents results stratified by historical oppression (i.e., high versus low), with greater changes observed among participants reporting lower levels of historical oppression at baseline. Table 4 presents results stratified by historical oppression (i.e., high versus low). Participants reporting high historical oppression at baseline reported significant increase in CM after completing the WHF program. Respondents reporting low levels of historic oppression at pretest also reported significant declines in alcohol use, symptoms of anxiety, poor parental monitoring, and increases in CM after the WHF program.
Table 4.
Changes in outcomes over time, stratified by historical oppression scores.
| Ecological Level of FHORT | outcome | High historical oppression | Low historical oppression | Timepoints | ||
|---|---|---|---|---|---|---|
| Beta estimate (S.E.) for time/wave | Z (p value) | Beta estimate (S.E.) for time/wave | Z (p value) | |||
| Behavioral | Substance use | |||||
| Alcohol use | −0.06 (0.20) | −0.30 (0.76) | −3.19 (1.17) | −2.71 (<0.01) | Primary | |
| Drug use | 0.02 (0.09) | 0.21 (0.83) | −0.01 (0.07) | −0.16 (0.88) | Primary | |
| Mental | Anxiety | −0.54 (0.39) | −1.40 (0.16) | −1.02 (0.41) | −2.48 (0.01) | Primary |
| Familial | Parenting | |||||
| Positive Parenting | 0.12 (0.24) | 0.49 (0.62) | 0.25 (0.21) | 1.20 (0.23) | Primary | |
| Poor Monitoring | −0.02 (0.22) | −0.07 (0.96) | −0.16 (0.07) | −2.44 (0.01) | Primary | |
| community | communal mastery | 2.96 (0.53) | 5.54 (<0.01) | 2.59 (0.40) | 6.40 (<0.01) | Secondary |
Note. High historical oppression is defined as scores of 38 or higher (75th percentile) on the HOS, and low historical oppression defined as scores lower than 38; 30% of respondents indicated having high levels of historical oppression. Primary measures were asked at pretest, posttest, and 6-, 9-, and 12-month post interventions; secondary measures were asked at pretest, posttest, and 12-month postintervention.
Discussion
WHF participants reporting higher and lower levels of historical oppression experience differential changes after participation in the WHF program. Results of this pilot study must be taken with caution due to the small sample size and nonrandom sample, and a lack of control group. Overall, participants reporting lower levels of historical oppression at baseline reported greater declines across behavioral (alcohol use), mental (symptoms of anxiety), familial (poor parental monitoring), and increased in community, CM. Participants reporting higher levels of historical oppression and pretest reported significant increases in CM after completing the program. Changes in positive parenting and drug use were not significant, likely due to small sample sizes. Very few participants reported any drug use, making the variance and ability to detect differences in this small sample difficult.
Overall, alcohol use declined after participating in the WHF program; 12-month alcohol use for males was 45.4% lower than pretest alcohol use, and female alcohol use was 36.6% lower than pretest use (41.2% lower overall). Perceived historical oppression increased for both adolescents and adults, though this varied by sex (reported historical oppression increased for adult females and adolescent males and decreased for adult males and adolescent females). Total historical oppression scores, indicated greater awareness and reported perception of historical oppression after completing the program. Given that information about the effect of historical oppression on families and communities was integrated into the WHF program. Perceived historical oppression translated into differential outcomes for participants reporting higher and lower levels of historical oppression. Those reporting lower historical oppression at pretest overall, reported greater declines in alcohol use, anxiety, and poor monitoring. All participants, regardless of levels of historical oppression, reported significant increases in CM.
Strengths and limitations
The strengths of this culturally grounded study and intervention developed with CBPR included piloting all measures with focal tribal communities; this includes the CM (Hobfoll et al., 2002) and the HOS, which was developed and validated with Indigenous communities (McKinley, Boel-Studt, et al., 2020; McKinley, Miller Scarnato, et al., 2020). Despite these strengths, the results of this pilot study are exploratory and only preliminary. Limitations include a small sample size, which limited the power to detect true and significant differences. Moreover, this study only assessed differences according to pretest historical oppression scores. Future inquiries assessing longitudinal changes in perceptions of historical oppression change and how they are associated with psychosocial outcomes are needed. Moreover, qualitative interviews may inform the ways participants understand historical oppression to related to outcome, an important inquiry for future research. The convenience sample and lack of a control group in this longitudinal design make the results ungeneralizable, though they may be applied and tested in other contexts. Still, given the aim of this study was to test for acceptability and feasibility of the WHF program (McKinley & Theall, 2021), the significant outcomes are promising, despite the limited sample. Future clinical trial research to examine the intervention’s efficacy in a scaled version of the WHF program is underway.
Conclusions and implications
This pilot study’s results must be taken with caution given its exploratory nature. However, historical oppression was found to be a salient concept that meaningfully differentiated across key outcomes. Perceived historical oppression was not only significantly related to key mental, behavioral, family, community, and structural outcomes that meaningfully predict health equity and wellness, but outcomes differed depending on initial levels of historical oppression. Historical oppression may help people have a structural understanding of behavioral, mental, and family health challenges, but may also pose a risk, or one more layer of oppression to negotiate to attain wellness. Prior research has established a link between historical oppression and loss (Burnette et al., 2019; Caetano et al., 2013; Evans-Campbell et al., 2012; McKinley, Figley, et al., 2019; McKinley, Miller Scarnato, et al., 2019; Mmari et al., 2010) with SUD, anxiety, and other behavioral and mental outcomes. This pilot study provides fruitful groundwork for exploring this topic further. If historical oppression is partly driving such outcomes, it should be meaningfully incorporated into treatment. Prior to this study, its integration and examination has been absent.
The WHF program holds promise to center structural determinants of psychosocial outcomes child welfare, juvenile justice, and behavioral health programs. Participation in the WHF program was associated with an increase in the awareness of perceived historical oppression and differential improvements in outcomes depending on perceptions of historical oppression. Reported levels of historical oppression meaningfully differentiated change across important outcomes among Indigenous youth, namely SUD, anxiety, and other mental health outcomes (Cheadle & Whitbeck, 2011; Hobfoll et al., 2002; LaFromboise et al., 2006; McKinley, Boel-Studt, et al., 2020; McKinley, Miller Scarnato, et al., 2020; Meyer, 2015). Given structural factors are known predictors of mental and behavioral health outcomes, integrating structural and social determinants of health are critically important. Research has too long treated mental, behavioral, and familial outcomes as separate from the context in which they are situated (Gone & Trimble, 2012; Liddell & Burnette, 2017). Prevention programs must center and structural determinants of health that perpetuate extant inequities.
Social service providers have been complicit in knowingly or unknowingly perpetuating historical oppression through enacting the removals of Indigenous children from their families in the Boarding School Era and the Indian Adoption Act and institutionalized bias throughout the child welfare and social service systems (Weaver et al., 2021). Thus, social service providers must gain a critical consciousness about the ways that historical oppression may affect Indigenous peoples psychosocial outcomes (Weaver et al., 2021). Given their salience in key psychosocial outcomes, social service providers may become aware of their role and ways to redress contemporary forms of historical oppression rather than replicate. Resources, such as the CSWE teaching tool can help (see Linjean et al., 2022; Weaver et al., 2021).
Supplementary Material
Acknowledgments
The authors thank the dedicated work and participation of the tribes and collaborators who contributed to this work. We thank Jennifer Lilly, Jessica Liddell, Hannah Knipp, Jennifer Martin, Tamela Solomon, Nikki Comby, Harold Comby, Patricia Haynes, Kathleen Ferris, Juannina Mingo, Dan Isaac, Clarissa Stewart, Mariah Lewis, and Jeremy Chickaway for their incredible commitment, time and energy devoted to the WHF Program. We also thank Dana Kingfisher, Emily Matt Salois, d’Shane Barnett, and all the staff at the All Nations Health Center in Missoula, Montana for their important contributions to the pilot program. We thank Charles R. Figley, Karina Walters, James Allen, and Tonette Krousel-Wood for their support and mentorship for this pilot program. We thank The National Association for Children of Addiction for the original program from which the WHF program was developed, and White Bison for introducing cultural components.
Funding
This work was supported by the National Institutes of Health.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
Supplemental data for this article can be accessed online at https://doi.org/10.1080/01488376.2023.2178596
References
- Bureau of Indian Affairs. (2021). About us. https://www.bia.gov/bia
- Burnette CE, & Figley CR (2016). Risk and protective factors related to the wellness of American Indian and Alaska Native youth: A systematic review. International Public Health Journal, 8(2), 137–154. http://www.nova-publishers.org/catalog/product_info.php?products_id=58073 [Google Scholar]
- Burnette CE, & Figley CR (2017). Historical oppression, resilience, and transcendence: Can a holistic framework help explain violence experienced by Indigenous peoples? Social Work, 62(1), 37–44. 10.1093/sw/sww065 [DOI] [PubMed] [Google Scholar]
- Burnette CE, Renner LM, & Figley CR (2019). The Framework of Historical Oppression, Resilience, and Transcendence to understand disparities in depression among Indigenous Peoples. British Journal of Social Work, 49(4), 943–962. 10.1093/bjsw/bcz041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette CE, Sanders S, Butcher HK, & Rand JT (2014). A toolkit for ethical and culturally sensitive research: An application with Indigenous communities. Ethics and Social Welfare, 8(4), 364–382. 10.1080/17496535.2014.885987 [DOI] [Google Scholar]
- Caetano R, Kaplan MS, Huguet N, McFarland BH, Conner K, Giesbrecht N, & Nolte KB (2013). Acute alcohol intoxication and suicide among United States ethnic/racial groups: Findings from the national violent death reporting system. Alcoholism, Clinical and Experimental Research, 37(5), 839–846. 10.1111/acer.12038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheadle JE, & Whitbeck LB (2011). Alcohol use trajectories and problem drinking over the course of adolescence: A study of North American indigenous youth and their caretakers. Journal of Health and Social Behavior, 52(2), 228–245. 10.1177/0022146510393973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon AL, Yabiku ST, Okamoto SK, Tann SS, Marsiglia FF, Kulis S, & Burke AM (2007). The efficacy of a multicultural prevention intervention among urban American Indian youth in the southwest US. The Journal of Primary Prevention, 28(6), 547–568. 10.1007/s10935-007-0114-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dusenbury L (2000). Family-based drug abuse prevention programs: A review. Journal of Primary Prevention, 20(4), 337–352. 10.1023/A:1021366721649 [DOI] [Google Scholar]
- Evans-Campbell T, Walters KL, Pearson CR, & Campbell CD (2012). Indian boarding school experience, substance use, and mental health among urban two-spirit American Indian/Alaska Natives. The American Journal of Drug and Alcohol Abuse, 38(5), 421–427. 10.3109/00952990.2012.701358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- FitzGerald CA, Fullerton L, Green D, Hall M, & Penaloza LJ (2017). The association between positive relationships with adults and suicide-attempt resilience in American Indian youth in New Mexico. American Indian and Alaska Native Mental Health Research (Online), 24(2), 40–53. 10.5820/aian.2402.2017.40 [DOI] [PubMed] [Google Scholar]
- Gone JP, & Trimble JE (2012). American Indian and Alaska Native mental health: Diverse perspectives on enduring disparities. Annual Review of Clinical Psychology, 8, 131–160. 10.1146/annurev-clinpsy-032511-143127 [DOI] [PubMed] [Google Scholar]
- Griner D, & Smith TB (2006). Culturally adapted mental health intervention: A meta-analytic review. Psychotherapy: Theory, Research, Practice, Training, 43(4), 531–548. 10.1037/0033-3204.43.4.531 [DOI] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, & Duda SN, on behalf of the REDCap Consortium. (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill DL (2009). Relationship between sense of belonging as connectedness and suicide in American Indians. Archives of Psychiatric Nursing, 23(1), 65–74. 10.1016/j.apnu.2008.03.003 [DOI] [PubMed] [Google Scholar]
- Hobfoll SE, Jackson A, Hobfoll I, Pierce CA, & Young S (2002). The impact of communal-mastery versus self-mastery on emotional outcomes during stressful conditions: A prospective study of Native American women. American Journal of Community Psychology, 30(6), 853–871. 10.1023/A:1020209220214 [DOI] [PubMed] [Google Scholar]
- Indian Health Service. (2019). Indian health disparities. https://www.ihs.gov/sites/newsroom/themes/responsive2017/display_objects/documents/factsheets/Disparities.pdf
- Ka’apu K, & Burnette CE (2019). A culturally informed systematic review of mental health disparities among adult Indigenous men and women of the USA: What is known? British Journal of Social Work, 49(4), 880–898. 10.1093/bjsw/bcz009.PMC6615176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klostermann K, Kelley ML, Mignone T, Pusateri L, & Fals-Stewart W (2010). Partner violence and substance abuse: Treatment interventions. Aggression and Violent Behavior, 15(3), 162–166. 10.1016/j.avb.2009.10.002 [DOI] [Google Scholar]
- Kraanen FL, Vedel E, Scholing A, & Emmelkamp PM (2013). The comparative effectiveness of integrated treatment for substance abuse and partner violence (I-StoP) and substance abuse treatment alone: A randomized controlled trial. BMC Psychiatry, 13(1), 1–14. 10.1186/1471-244X-13-189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyriazos TA, & Stalikas A (2019). Alabama Parenting Questionnaire-Short Form (APQ-9): Evidencing construct validity with factor analysis, CFA MTMM and measurement invariance in a Greek sample. Psychology, 10(12), 1790–1817. 10.4236/psych.2019.1012117 [DOI] [Google Scholar]
- LaFromboise TD, Hoyt DR, Oliver L, & Whitbeck LB (2006). Family, community, and school influences on resilience among American Indian adolescents in the upper Midwest. Journal of Community Psychology, 34(2), 193–209. 10.1002/jcop.20090 [DOI] [Google Scholar]
- Le P, & Aptekar S (2019). For American Indians, health is a human and legal right. The Health Care Blog. https://thehealthcareblog.com/blog/2019/03/29/for-american-indians-health-is-a-human-and-legal-right/ [Google Scholar]
- Linjean M, Russell J, Weaver HN, & Sloan LM (2022). Teaching guide: Repairing harms done to indigenous and tribal peoples. Council on Social Work Education. https://www.cswe.org/getmedia/a77aeb76-3b0f-442f-a166-43acca1fb652/7842-cswe_TeachersGuide_proof5_web.pdf [Google Scholar]
- Liddell J, & Burnette CE (2017). Culturally-informed interventions for substance abuse among Indigenous youth in the United States: A review. Journal of Evidence-Based Social Work, 14(5), 329–359. 10.1080/23761407.2017.1335631 [DOI] [PubMed] [Google Scholar]
- Masten AS, & Monn AR (2015). Child and family resilience: A call for integrated science, practice, and professional training. Family Relations, 64(1), 5–21. 10.1111/fare.12103 [DOI] [Google Scholar]
- McKinley CE, Boel-Studt S, Renner LM, Figley CR, Billiot S, & Theall K (2020). The historical oppression scale: Preliminary conceptualization and measurement of historical oppression among Indigenous Peoples of the United States. Transcultural Psychiatry, 57(2), 288–303. 10.1177/1363461520909605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley CE, Boel-Studt S, Renner LM, & Figley CR (2021). Risk and protective factors for anxiety and depression among American Indians: Understanding the roles of resilience and trauma. Psychological Trauma: Theory, Research, Practice and Policy, 13(1), 16–25. 10.1037/tra0000950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley CE, Figley CR, Woodward S, Liddell J, Billiot S, Comby N, & Sanders S (2019). Community-engaged and culturally relevant research to develop mental and behavioral health interventions with American Indian and Alaska Natives. American Indian and Alaska Native Mental Health Research (Online), 26(3), 79–103. 10.5820/aian.2603.2019.79 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley CE, Miller Scarnato J, Liddell J, Knipp H, & Billiot S (2019). Hurricanes and Indigenous families: Understanding connections with discrimination, social support, and violence on PTSD. Journal of Family Strengths, 19(1), 10. https://digitalcommons.library.tmc.edu/jfs/vol19/iss1/10 [PMC free article] [PubMed] [Google Scholar]
- McKinley CE, Miller Scarnato J, & Sanders S (2020). Why are so many Indigenous peoples dying and no one is paying attention? Depressive symptoms and “loss of loved ones” as a result and driver of health disparities. Omega—Journal of Death and Dying, 85, 88–113. 10.1177/0030222820939391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley CE, & Theall KP (2021). Weaving Healthy Families program: Promoting resilience while reducing violence and substance use. Research on Social Work Practice, 31(5), 476–492. 10.1177/1049731521998441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinley CE, Saltzman LY, & Theall KP (2023). The weaving healthy families program: Promoting parenting practices, family resilience, and communal mastery. Family Process. 10.1111/famp.12854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer IH (2015). Resilience in the study of minority stress and health of sexual and gender minorities. Psychology of Sexual Orientation and Gender Diversity, 2(3), 209–213. 10.1037/sgd0000132 [DOI] [Google Scholar]
- Mmari KN, Blum RW, & Teufel-Shone N (2010). What increases risk and protection for delinquent behaviors among American Indian youth? Findings from three tribal communities. Youth & Society, 41(3), 382–413. 10.1177/0044118X09333645 [DOI] [Google Scholar]
- National Association for Children of Alcoholics. (2011). Celebrating Families! curriculum. http://www.celebrating-families.net/curriculum.htm
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, & Grant M (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction (Abingdon, England), 88(6), 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Schober P, & Vetter TR (2018). Repeated measures designs and analysis of longitudinal data: If at first you do not succeed-try, try again. Anesthesia and Analgesia, 127(2), 569–575. 10.1213/ane.0000000000003511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schure M, & Goins RT (2017). Psychometric examination of the center for epidemiologic studies depression scale with older American Indians: The native elder care study. American Indian & Alaska Native Mental Health Research: The Journal of the National Center, 24(3), 1–13. 10.5820/aian.2403.2017.1 [DOI] [PubMed] [Google Scholar]
- Skinner HA (1982). The drug abuse screening test. Addictive Behaviors, 7(4), 363–371. 10.1016/0306-4603(82)90005-3 [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB, & Löwe B (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Tutty L (2013). An evaluation of strengthening families: The Calgary Counselling Centre’s program for couples dealing with intimate partner violence and substance use. Yarro Creek Enterprises. [Google Scholar]
- Urban Indian, H. I. (2014). Supporting sobriety among American Indians and Alaska Natives: A literature review. http://www.uihi.org/wp-content/uploads/2014/02/Supporting-Sobriety_A-Literature-Review_WEB.pdf
- Weaver HN, Sloan LM, Barkdull C, & Lee P (2021). CSWE statement of accountability and reconciliation for harms done to Indigenous and Tribal peoples. Council on Social Work Education. https://www.cswe.org/getattachment/Education-Resources/Indigenous-and-Tribal-Content/CSWE-Statement-of-Accountability-and-Reconciliation-for-Harms-Done-to-Indigenous-and-Tribal-Peoples.pdf [Google Scholar]
- Whitbeck LB (2006). Some guiding assumptions and a theoretical model for developing culturally specific preventions with Native American people. Journal of Community Psychology, 34(2), 183–192. 10.1002/jcop.20094 [DOI] [Google Scholar]
- Whitbeck LB, Chen X, Hoyt DR, & Adams GW (2004). Discrimination, historical loss and enculturation: Culturally specific risk and resiliency factors for alcohol abuse among American Indians. Journal of Studies on Alcohol, 65(4), 409–418. 10.15288/jsa.2004.65.409 [DOI] [PubMed] [Google Scholar]
- Whitbeck LB, Walls ML, & Welch ML (2012). Substance abuse prevention in American Indian and Alaska Native communities. The American Journal of Drug and Alcohol Abuse, 38(5), 428–435. 10.3109/00952990.2012.695416 [DOI] [PubMed] [Google Scholar]
- White Bison. (2015). Celebrating families! http://whitebison.org/Training/Families.aspx
- Whitesell NR, Beals J, Crow CB, Mitchell CM, & Novins DK (2012). Epidemiology and etiology of substance use among American Indians and Alaska Natives: Risk, protection, and implications for prevention. The American Journal of Drug and Alcohol Abuse, 38(5), 376–382. 10.3109/00952990.2012.694527 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


