Abstract
BACKGROUND
Extracranial vertebral aneurysms or pseudoaneurysms are rare and result primarily from trauma. Large pseudoaneurysms can masquerade as mass lesions, making it challenging to identify the correct diagnosis.
OBSERVATIONS
This is a case report in which a large vertebral pseudoaneurysm posed as a schwannoma and biopsy was attempted. It was later identified as a vascular lesion and treated appropriately with no complications.
LESSONS
Vascular etiologies should always be included in the differential diagnosis of spine and nerve pathologies especially lesions that are in the vicinity of major vascular channels such as the transverse foramina of the cervical spine.
Keywords: cervical mass, nerve sheath tumor, vascular lesion, angiography
ABBREVIATIONS: BTO = balloon test occlusion, CT = computed tomography, CTA = computed tomography angiography, MRI = magnetic resonance imaging
Extracranial vertebral aneurysms or pseudoaneurysms are rare and result primarily from trauma.1,2 Proximal aneurysms in the V1 and V2 portions are likely attributed to penetrating trauma, whereas distal aneurysms in V3 and V4 are attributed to blunt trauma.3 Here, we report the case of an atraumatic giant pseudoaneurysm of the left vertebral artery mimicking a schwannoma.
Illustrative Case
A 46-year-old male was referred for neurosurgical evaluation after magnetic resonance imaging (MRI) of the cervical spine and brachial plexus showed a lobulated enhancing lesion centered on the left C5–6 neural foramen measuring 4.3 × 2.4 × 2.4 cm and extending into the left C4–5 and C6–7 neural foramina (Fig. 1). He reported an 18-month history of neck discomfort, as well as left scapular pain radiating to the left arm associated with numbness primarily along the C6 distribution. This pain did not respond to physical therapy or chiropractor manipulations and massage. The pain did improve with gabapentin. The patient denied any history of trauma. On examination, he had full strength in all the muscle groups of the left upper limb and diminished sensation over the left C6 distribution. As part of the workup, a computed tomography angiography (CTA) of the head and neck was performed, redemonstrating the mass and suggesting that the vertebral artery coursed on the medial surface of the tumor (Fig. 1E). There was significant remodeling of the left C5–6 neural foramen and vertebral bodies as well as expansion of the left C5 foramen transversarium. A computed tomography (CT)-guided biopsy of the mass showed benign fibrous tissue and no evidence of neoplasm; the needle likely, and luckily, missed the lesion. To define the vertebral artery’s relationship to the tumor better, diagnostic angiography and a balloon test occlusion (BTO) were completed prior to resection. The findings were unexpected, because the angiogram demonstrated a large vertebral artery pseudoaneurysm (Fig. 2). There was robust filling of the left vertebral artery and branches from a right vertebral artery injection (Fig. 3A), and he passed the BTO. The patient was started on full-dose aspirin. After discussing the findings in our vascular multidisciplinary conference that includes neurosurgeons and neuroradiologists, we proceeded with proximal and distal coil embolization of the pseudoaneurysm without any intraoperative or postoperative complications (Fig. 3B). He had resolution of the pain and numbness in the left arm within 2 weeks of surgery and continued to do well at the 15-month follow-up.
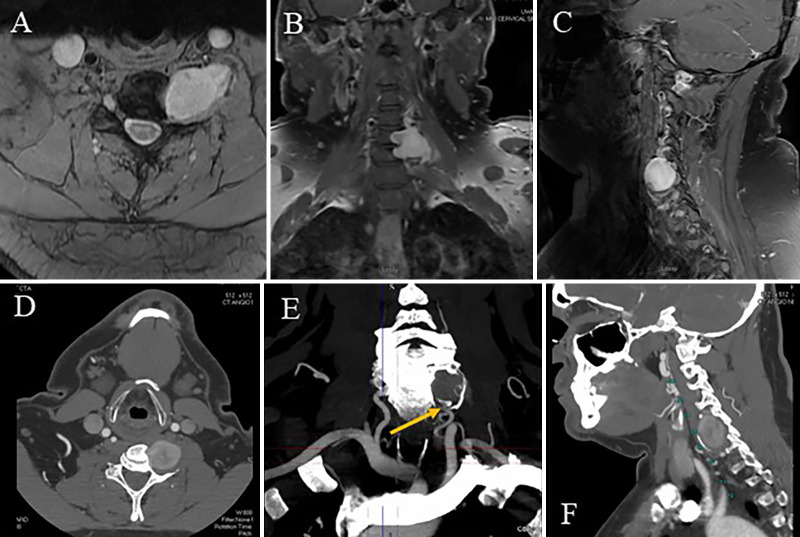
FIG. 1.
Contrasted magnetic resonance images in the axial (A), coronal (B), and sagittal (C) planes showing an enhanced lesion at the C5–6 level. CT images demonstrating the relationship of the mass to the vertebral bodies in the axial (D), coronal (E), and sagittal (F) planes. The vertebral artery (arrow, E) is at the medial inferior surface of the mass and later (more distally) disappears.
FIG. 2.
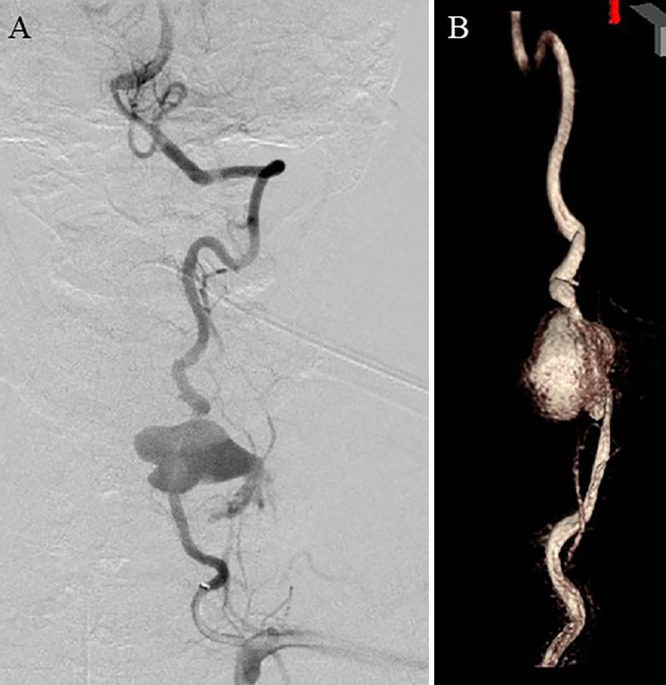
A: Diagnostic cerebral angiogram demonstrating the large pseudoaneurysm. B: Three-dimensional reconstruction of the aneurysm.
FIG. 3.
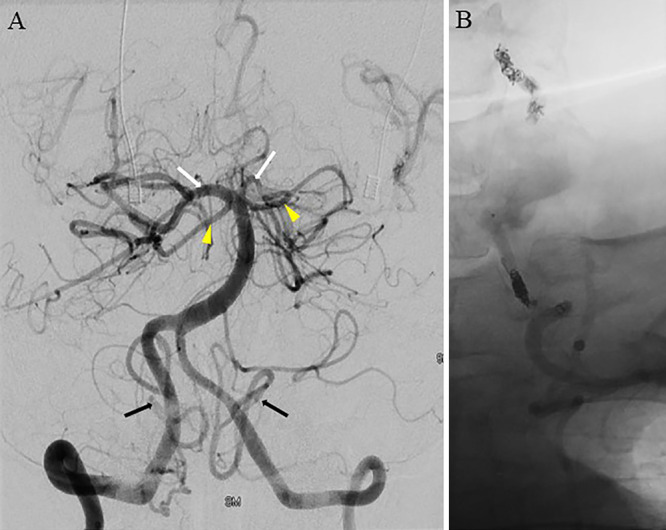
A: Right vertebral artery angiogram demonstrating robust filling of bilateral posterior cerebral arteries (white arrows), anterior inferior cerebellar arteries (arrowheads), and posterior inferior cerebellar arteries (black arrows). B: Proximal and distal coils occluding the left vertebral artery and trapping the aneurysm.
Patient Informed Consent
The necessary patient informed consent was obtained in this study.
Discussion
Pseudoaneurysms of the vertebral artery are rare, especially the atraumatic ones. When the patient initially presented, workup showed a cervical mass causing compression of the C6 nerve root and radicular symptoms. Given the lack of history of trauma, risk factors, or predisposition to aneurysms or pseudoaneurysms such as Marfan syndrome, Ehlers-Danlos syndrome, or smoking, a pseudoaneurysm was not high among the differential diagnoses; we even proceeded with a biopsy, which was nondiagnostic. It is only after the diagnostic angiogram that the pseudoaneurysm was identified. However, it is possible that subtle clues on MRI and CTA could have led us to suspect the pathology early on and thus avoid the biopsy.
Observations
After reviewing the imaging and discussing the treatment options in a multidisciplinary conference, the question at hand was whether to sacrifice the vertebral artery since the right vertebral fills all the posterior circulation robustly or do we just place Pipeline stents across the aneurysm. With the advent of endovascular surgery and technology, there are means of treating this aneurysm in a minimally invasive manner. Stavrinou et al.4 treated a similar patient who also presented with C6 radiculopathy due to a pseudoaneurysm with proximal occlusion of the left vertebral artery. Detwiler et al.5 reported the case of a nontraumatic large pseudoaneurysm in a patient with von Recklinghausen’s disease that was treated similarly by embolization. Other case reports in the literature document pseudoaneurysms secondary to trauma, which were also treated by proximal ligation, distal ligation, or both prior to the endovascular era of embolization.6
Lessons
Vascular etiologies should always be included in the differential diagnosis of spine and nerve pathologies, especially lesions that are in the vicinity of major vascular channels such as the transverse foramina of the cervical spine. We could have injured this patient if the needle biopsy had punctured the aneurysm. It is important to be comprehensive in our presurgery workup especially in the era of endovascular surgery. This is a one-case report of our experience treating one giant pseudoaneurysm masquerading as a mass lesion. Fortunately, these are extremely rare phenomena with few cases reported in the literature, the last one more than 20 years ago.
Disclosures
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in this paper.
Author Contributions
Conception and design: Larson, Ahmed, Hanna. Acquisition of data: Larson, Ahmed, Hanna. Analysis and interpretation of data: all authors Drafting the article: Koueik, Larson, Hanna. Critically revising the article: Koueik, Ahmed, Hanna. Reviewed submitted version of manuscript: Koueik, Hanna. Approved the final version of the manuscript on behalf of all authors: Koueik Study supervision: Hanna.
Supplemental Information
Previous Presentations
This was presented at the European Association of Neurosurgical Societies at their virtual meeting on October 3, 2021.
References
- 1. Gallo P, Dalacorte A, Raupp E, Santos AJ, Frank MR, Saraiva GA. Giant pseudoaneurysm of the extracranial vertebral artery: case report. Arq Neuropsiquiatr. 1996;54(2):297–303. doi: 10.1590/s0004-282x1996000200019. [DOI] [PubMed] [Google Scholar]
- 2. Matas R. Traumatisms and traumatic aneurisms of the vertebral artery and their surgical treatment with the report of a cured case. Ann Surg. 1893;18(5):477–521. [PMC free article] [PubMed] [Google Scholar]
- 3. Kaplan SS, Ogilvy CS, Gonzalez R, Gress D, Pile-Spellman J. Extracranial vertebral artery pseudoaneurysm presenting as subarachnoid hemorrhage. Stroke. 1993;24(9):1397–1399. doi: 10.1161/01.str.24.9.1397. [DOI] [PubMed] [Google Scholar]
- 4. Stavrinou LC, Stranjalis G, Stavrinou PC, Bontozoglou N, Sakas DE. Extracranial vertebral artery aneurysm presenting as a chronic cervical mass lesion. Case Rep Med. 2010;2010:938219. doi: 10.1155/2010/938219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Detwiler K, Godersky JC, Gentry L. Pseudoaneurysm of the extracranial vertebral artery. Case report. J Neurosurg. 1987;67(6):935–939. doi: 10.3171/jns.1987.67.6.0935. [DOI] [PubMed] [Google Scholar]
- 6. Schittek A. Pseudoaneurysm of the vertebral artery. Tex Heart Inst J. 1999;26(1):90–95. [PMC free article] [PubMed] [Google Scholar]