Abstract
Study Design
Retrospective clinical case series.
Objectives
To investigate the risk factors for intraoperative endplate violations and delayed cage subsidence after oblique lateral interbody fusion (OLIF) surgery. Secondly, to examine whether low Hounsfield unit (HU) values at different regions of the endplate are associated with intraoperative endplate violation or delayed cage subsidence.
Methods
61 patients (aged 65.1 ± 9.5 years; 107 segments) who underwent OLIF with or without posterior instrumentation from May 2015 to April 2019 were retrospectively studied. Intraoperative endplate violation was measured on sagittal reconstructed computerized tomography (CT) images immediate postoperatively, while delayed cage subsidence was evaluated using lateral radiographs and defined at 1-month follow-up or later. Demographic information and clinical parameters such as age, body mass index, bone mineral density, number of surgical levels, cage dimension, disc height restoration, visual analogue scale (VAS), and HU at different regions of the endplate were obtained.
Results
Total postoperative cage subsidence was identified in 45 surgical levels (42.0%) in 26 patients (42.6%) up till postoperative 1-year follow-up. Low HU value at the ipsilateral epiphyseal ring was an independent risk factor for intraoperative endplate violation (P = .008) with a cut-off value of 326.21 HUs. Low HU values at the central endplate had a significant correlation with delayed cage subsidence in stand-alone cases (P = .013) with a cut-off value of 296.42 HUs. VAS scores were not different at 1 week postoperatively in cases with or without intraoperative endplate violation (3.12 ± .73 vs 2.89 ± .72, P = .166) and showed no difference at 1 year with or without delayed cage subsidence (1.95 ± .60 vs 2.26 ± .85, P = .173).
Conclusions
Intraoperative endplate violation and delayed cage subsidence are not uncommon with OLIF surgery. HUs of the endplate are good predictors for intraoperative endplate violation and cage subsidence since they can represent the regional bone quality of the endplate in contact with the implant. VAS improvements were not affected by intraoperative endplate violation or delayed cage subsidence at 1-year follow-up.
Level of Evidence
Level III.
Keywords: lumbar, cage, subsidence, Hounsfield unit, endplate violation, oblique lateral interbody fusion
Introduction
In recent years, favorable clinical results of the oblique lateral interbody fusion (OLIF) without additional posterior pedicle screw fixation (stand-alone OLIF) have been reported.1-3 For indirect decompression purposes, OLIF, similar to the lateral lumbar interbody fusion (LLIF) approach, can be performed without posterior surgery, laminectomy, facetectomy or stripping of spinal or paraspinal musculature, preserving the anterior and posterior longitudinal ligaments, which leads to improved biomechanical stability of the spinal segment.4,5 One of the major complications of LIF is cage subsidence as it may lead to compromised clinical results, such as the loss of indirect decompression and recurrence of neural compression. 6 Previous studies have described two types of cage subsidence, one results from intraoperative endplate violation and the other (delayed cage subsidence) occurs gradually over the postoperative course.7,8
The endplate is the interface between implants and the vertebral bodies, and plays an important role in distributing the compressive load across a functional spinal unit. The epiphyseal ring, also known as ring apophysis, is a bony labrum surrounding the outer rim of the vertebral body surface. 9 Previous biomechanical tests have demonstrated that spanning the fusion cage across the ring apophysis could provide more strength in compression and potentially reduce subsidence. 10 As a bone quality assessment, Hounsfield units (HUs) of the endplate are measured from routine computerized tomography (CT) scans that are readily available as a part of the preoperative assessments. 11 The HU of the epiphyseal ring and the central endplate can provide detailed information regarding the bone quality across the endplates at the surgical levels.
Despite an increasing body of evidence about the potential risk factors for cage subsidence, the role of HU values at the endplate remains unclear. The objective of this study was to investigate the risk factors for intraoperative endplate violations and delayed cage subsidence after OLIF surgery. We hypothesized that the risk of cage subsidence after OLIF may be associated with HU at different regions of the endplate.
Patients and Methods
Study Design
A retrospective review was conducted on patients who underwent OLIF procedure with or without posterior instrumentation from May 2015 to April 2019 at a tertiary referral spine center.
Study Subjects
The inclusion criteria were as follows: (1) lumbar spinal stenosis; (2) lumbar segmental instability defined by a sagittal plane translation of 3 mm, or a rotational angle greater than 15° on preoperative flexion and extension radiographs; (3) Grade 1 or 2 spondylolisthesis; (4) degenerative disc disease/discogenic back pain; and (5) degenerative scoliosis. The exclusion criteria were as follows: (1) Grade 3 or 4 spondylolisthesis; (2) preoperative endplate defects such as Schmorl’s nodes; (3) severe osteoporosis (a T-score ≤-2.5); (4) missing preoperative CT scans; and (5) follow-up of <12 months. Ethical approval was obtained from the local Medical Ethics Committee. In addition, all patients gave written informed consent for their information to be stored in the hospital’s database and used for research.
Description of Study Population
There were 72 consecutive patients originally enrolled for the study, but 11 patients were excluded due to incomplete follow-up (n = 7) and preoperative endplate defects (n = 4). Hence, 61 patients (107 levels) were included in this study (Figure 1). There were 30 males (49.2%) and 31 females (50.8%). The mean age was 65.5 ± 9.3 years. 26 patients (42.6%, 49 levels) underwent a second phase posterior instrumentation, while 35 patients (57.4%, 58 levels) remained stand-alone throughout the follow-up period. A summary of the patient demographic and treatment information is provided in Table 1. There were no missing data.
Figure 1.
A flowchart of patients included in the study.
Table 1.
Patient Demographic and Treatment Information.
| Parameter | Patient Data (n = 61) |
|---|---|
| Age (years) | 65.1 ± 9.5 |
| Female | 31 (51%) |
| BMI (kg/m2) | 23.7 ± 3.0 |
| Preoperative VAS score | 4.9 ± 1.1 |
| Primary diagnosis | |
| Lumbar spinal stenosis | 30 (49.2%) |
| Adjacent segment disease | 2 (3.2%) |
| Spondylolisthesis | 11 (18%) |
| Discogenic low back pain | 4 (6.5%) |
| Degenerative scoliosis | 7 (11.4%) |
| Disc herniation | 22 (36%) |
| Fixation type | |
| Stand-alone cage | 36 (59.0%) |
| Cage with transpedicular bilateral fixation | 25 (40.1%) |
| Levels treated (n = 107) | |
| L1-L2 | 8 (7.5%) |
| L2-L3 | 22 (20.6%) |
| L3-L4 | 40 (37.4%) |
| L4-L5 | 44 (41.1%) |
| L5-S1 | 1 (.9%) |
BMI, body mass index; VAS, visual analogue scale.
Description of Surgery
All patients underwent single-level or multilevel OLIF through a single incision, mini-open direct visualizing approach. The cage (CLYDESDALE; Medtronic, Inc., Minneapolis, Minnesota, USA) packed with injectable calcium sulfate graft (MIIG, Wright, UK) was placed to span the entire ring apophysis. The main indications for posterior instrumentation were surgical levels ≥3 and the presence of postoperative segmental instability after OLIF stand-alone procedure, defined by a sagittal plane translation of 3 mm, or a rotational angle greater than 15° on the postoperative flexion and extension radiographs.
Study Parameters
Standing anteroposterior and lateral radiographs were obtained preoperatively and immediate postoperatively for disc height measurement, and at the 1-month, 3-month, 6-month, and 1-year follow-up to assess the incidence of cage subsidence. CT scans were performed preoperatively and immediate postoperatively. As potential explanatory variables, age, gender, body mass index (BMI), operating level, preoperative clinical diagnosis, number of levels fused, and bone mineral density (BMD) of the superior vertebral body were documented. The BMD of each vertebral body was measured by dual-energy x-ray absorptiometry (DEXA), and since the BMD of the inferior vertebral body of L4/L5 (44 levels, 41.1% of all levels) could not be accurately measured by DEXA due to the interference of the pelvis, the BMD of the superior vertebral body of all treated levels were measured in this study.
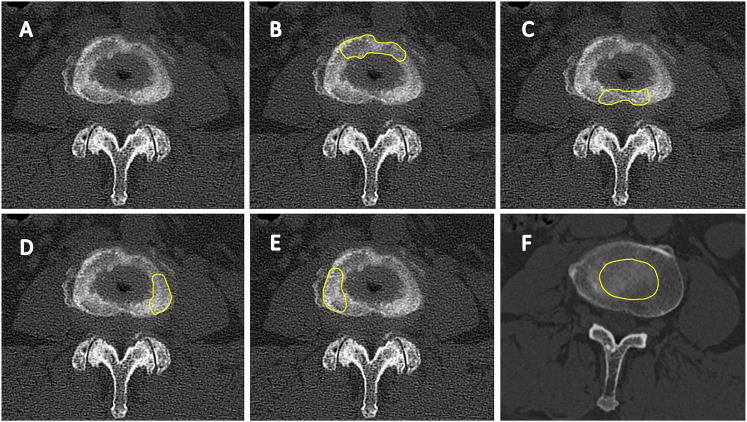
HU in 5 different regions was measured on both the upper and lower endplates of the treated level in preoperative CT images: (1) anterior epiphyseal ring; (2) posterior epiphyseal ring; (3) ipsilateral epiphyseal ring; (4) contralateral epiphyseal ring; and (5) central endplate. The ipsilateral and contralateral sides of the epiphyseal ring were determined based on the side on which the cage was introduced. The preoperative axial CT image layer used for HU measurement was the one visualizing the largest area of cortical bone in the endplate region being measured. The region of interest (ROI) was chosen manually to fit the shape of each structure (Figure 2). At the layer of CT where the structure of interest was present, HU of the ROI was measured. In addition, special attention was taken to make sure the HU of the cortical bone at the endplate was measured.
Figure 2.
(A) The epiphyseal ring on an axial computerized tomography image. (B) The ROI of the anterior epiphyseal ring. (C) The ROI of the posterior epiphyseal ring. (D) The ROI of the ipsilateral epiphyseal ring. (E) The ROI of the contralateral epiphyseal ring. (F) The ROI of the central endplate. ROI, region of interest.
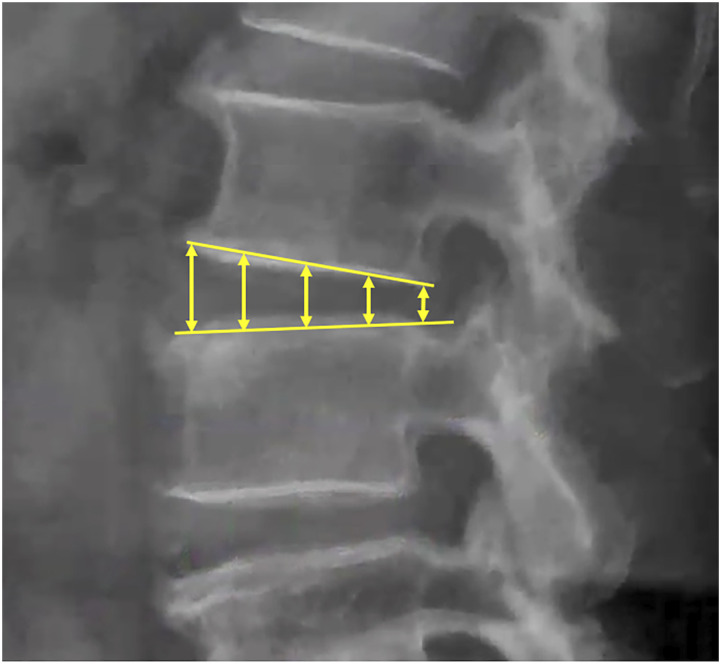
The intervertebral disc height was measured using standing neutral lateral radiographs, evaluated as an average of 5 measurements between the anterior and posterior margins of the intervertebral space (Figure 3). Expected disc height restoration was defined as the difference between the cage height and the preoperative disc height. Actual disc height restoration was calculated based on the difference between the disc height before and immediately after the operation.
Figure 3.
The intervertebral disc height was measured as an average of 5 height measurements between the anterior and posterior margins of the intervertebral space on standing lateral radiographs.
One reader independently made all measurements without knowledge of the patients’ clinical information. Interobserver reliability was performed with another reader with ten random subjects retrieved from a cohort of normal individuals. Intraobserver reliability was performed with the same 10 subjects 2 months after the initial assessment. Blinding and allocation were performed prior to measurements by another investigator.
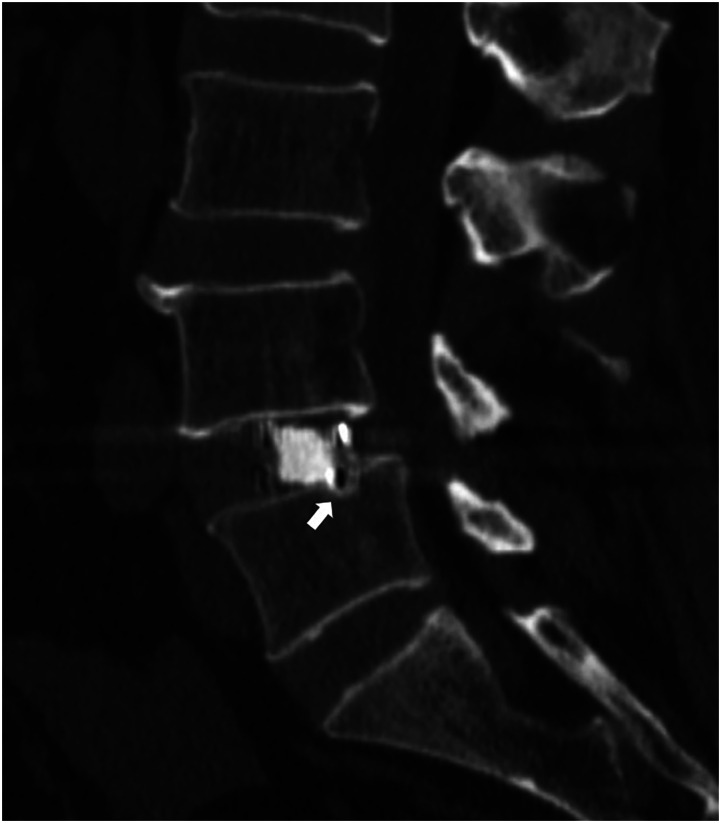
Intraoperative Endplate Violation and Delayed Cage Subsidence
The two main outcomes of study were intraoperative endplate violation and delayed cage subsidence. Intraoperative endplate violation was identified when the postoperative day 2 CT scan showed an endplate collapse larger than 2 mm (Figure 4). Endplate violation was confirmed by comparing the preoperative and immediate postoperative CT scans of the endplate to ensure that the endplate injury occurred during the operation. The distance of the interbody cage collapsing into the endplate was measured on CT scans.
Figure 4.
The intraoperative endplate violation was defined as more than 2 mm collapse of the cage into the endplate of adjacent vertebral body on immediate postoperative computerized tomography images.
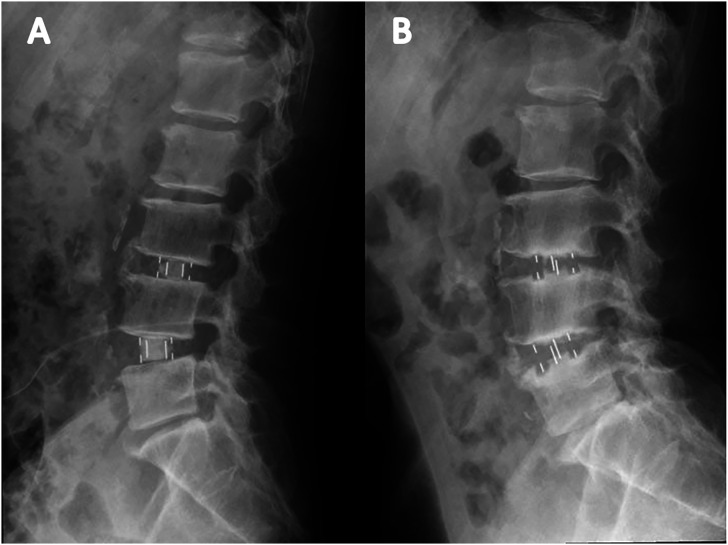
The sagittal planes of each surgical level were evaluated on standing lateral lumbar spine radiographs, and subsidence was defined as a cage sinking more than 2 mm into the adjacent vertebral endplate. If the postoperative day 2 CT images showed that the inserted cages spanned the epiphyseal ring on both sides with no evidence of endplate violation but subsidence was detected on subsequent radiographs during the follow-up period, it was deemed delayed cage subsidence (Figure 5).
Figure 5.
A patient who underwent oblique lumbar interbody fusion at L3/4 and L4/5. (A) No intraoperative endplate violation was observed. (B) Delayed cage subsidence was observed at both levels at 1-year follow-up.
Clinical Evaluation
Pain quantity at low back area using a visual analogue scale (VAS) with a scale graduation of 0-10 (0 means no pain, and 10 means maximal pain imaginable) were obtained from patients preoperatively, at 1-week postoperatively, and at 1-year follow-up. VAS at 1-week postoperatively was collected for this study instead of at day 2 after the surgery to minimize the influence of wound pain, although some patients reported wound pain up to 2 weeks postoperatively. Postoperative complications including psoas hematoma, transient psoas weakness, and thigh weakness or numbness were recorded at each visit.
Statistical Analysis
Demographic information and clinical parameters such as age, BMI, BMD, cage dimension, disc height restoration, VAS score assessed preoperatively and at the last follow-up, and HU at different regions of the endplate was analyzed using independent-samples t-tests. Shapiro–Wilk tests and normal q–q plots were used and confirmed normality of the measurements. Chi-square test was used to determine the difference in the number of surgical levels between patients with or without endplate violation. Multivariate logistic regression analyses were used to determine the significance of contributors for intraoperative endplate violation and delayed cage subsidence. Factors that showed a significant correlation (P < .05) with endplate violation or delayed subsidence in the univariate analysis were analyzed in the multivariate analysis. Statistical analyses were performed using R (version 3.6.2) and a measured P value of <.05 was considered statistically significant. Receiver operating characteristic (ROC) curves were used to establish separation criteria between surgical levels with or without intraoperative violation, and between levels with or without delayed subsidence. VAS improvements in patients with or without cage subsidence were compared. The area under curve (AUC) was calculated for each ROC. Cronbach’s alpha statistics was calculated using SPSS 20.0 software (SPSS Inc., Chicago, IL) to assess interobserver and intraobserver reliability. The Cronbach’s alpha for all HU value measurements were larger than .95, showing excellent interobserver and intraobserver reliability.
Results
Total postoperative cage subsidence was identified in 45 surgical levels (42.0%) in 26 patients (42.6%) until postoperative 1 year. These consisted of 25 intraoperative endplate violation segments (23.4%) and 20 levels (18.7%) with delayed cage subsidence. The majority of cage subsidence (37 levels, 34.6%) was located at the lower endplate. On the other hand, cage subsidence at the upper endplate was found in 15 levels (14.0%). 7 levels (6.5%) were found with cage subsidence at both endplates.
The BMD of the upper vertebral body of the surgical level was lower in segments that suffered intraoperative endplate violation (1.27 ± .25 vs 1.13 ± .28), but the difference was not statistically significant (P = .105). The BMD of the upper vertebral body was lower in levels with delayed cage subsidence of stand-alone patients (1.37 ± .26 vs 1.26 ± .2), but the difference was not statistically significant (P = .205).
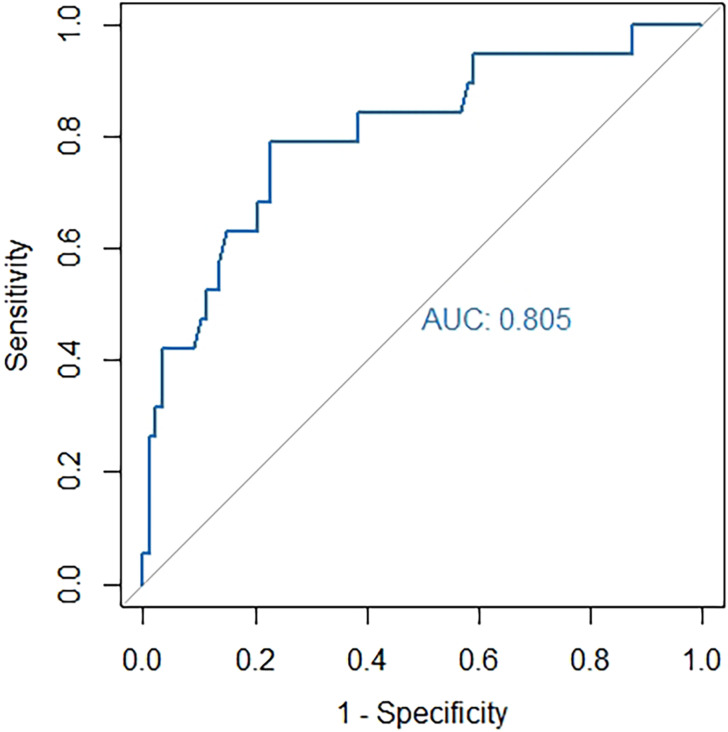
Of 107 treated levels, 25 levels (23.0%) suffered endplate violation at either endplate (Table 2). Lower endplate violation occurred in 19 levels (18%), while upper endplate violation occurred in 10 levels (9%). Three levels suffered endplate violation at both endplates (3%). Single-level cases were associated with significantly less intraoperative endplate violations (12% vs 68%, P < .001). The expected disc height restoration was higher in the endplate-violation group (6.97 ± 2.52 mm) than those without endplate-violation (5.30 ± 2.38 mm) (P = .003). VAS improvements at 1-week postoperatively showed no significant difference between segments with or without intraoperative endplate violations (P = .431). The endplate-violation group showed lower HU values in all endplate regions except in the upper posterior epiphyseal ring and the lower contralateral epiphyseal ring (Table 2). Based on the multivariate analysis, low HU value of the ipsilateral epiphyseal ring in the lower endplate was an independent risk factor for intraoperative endplate violation (OR .986 [95% CI 0.974‐.995]; P = .008) (Table 3). ROC curve (Figure 6) established separation criteria between levels with or without intraoperative endplate violation (AUC: .81; [95% CI 0.687‐.922]), and the most appropriate threshold was 326.21 HUs (sensitivity 79.0%, specificity 77.3%) at the ipsilateral epiphyseal ring of the lower endplate.
Table 2.
Univariate Analysis for Intraoperative Endplate Violation.
| Parameter | Groups | P value | |
|---|---|---|---|
| No Endplate Violation | Endplate Violation | ||
| No. of patients | 44 (72.1%) | 17 (27.9%) | |
| No. of levels | 82 (76.6%) | 25 (23.4%) | |
| Mean age (years) | 65.2 ± 9.7 | 66.7 ± 7.8 | .460 |
| Mean BMI (kg/m2) | 23.8 ± 3.0 | 23.4 ± 3.4 | .568 |
| Single-level cases | 30 (68.2%) | 2 (11.8%) | .001 |
| BMD (mg/cm3) a | 1.27 ± .25 | 1.13 ± .28 | .105 |
| Cage height (mm) | 15.0 ± 1.5 | 15.6 ± 1.3 | .060 |
| Cage length (mm) | 51.8 ± 4.1 | 50.3 ± 4.0 | .263 |
| Expected disc height restoration (mm) | 5.3 ± 2.4 | 7.0 ± 2.5 | .003 |
| Actual disc height restoration (mm) | 4.6 ± 2.1 | 3.7 ± 1.7 | .066 |
| VAS at 1-week postoperatively | 2.9 ± .7 | 3.1 ± .7 | .166 |
| VAS improvement at 1-week postoperatively | 2.0 ± 1.1 | 1.8 ± 1.3 | .431 |
| VAS at 1-year follow-up | 1.9 ± .3 | 2.2 ± 0.8 | .111 |
| Upper endplate Hounsfield unit | |||
| Anterior epiphyseal ring | 506.7 ± 109.5 | 421.3 ± 95.5 | .001 |
| Posterior epiphyseal ring | 536.2 ± 122.1 | 500.7 ± 136.9 | .220 |
| Ipsilateral epiphyseal ring | 577.8 ± 129.1 | 504.1 ± 120.6 | .013 |
| Contralateral epiphyseal ring | 532.2 ± 92.5 | 465.8 ± 115.6 | .004 |
| Central endplate | 426.4 ± 99.2 | 347.2 ± 103.7 | .001 |
| Lower endplate Hounsfield unit | |||
| Anterior epiphyseal ring | 448.0 ± 98.5 | 376.7 ± 100.7 | .009 |
| Posterior epiphyseal ring | 450.7 ± 77.3 | 410.0 ± 80.0 | .024 |
| Ipsilateral epiphyseal ring | 495.5 ± 95.4 | 409.1 ± 85.5 | .001 |
| Contralateral epiphyseal ring | 504.3 ± 105.3 | 467.0 ± 125.9 | .141 |
| Central endplate | 364.6 ± 80.0 | 321.8 ± 55.1 | .016 |
BMI: body mass index; BMD: bone mineral density.
a36 patients (58 levels) underwent bone mineral density scanning preoperatively.
Table 3.
Multivariate Analysis for Intraoperative Endplate Violation.
| Factors | Odds Ratio (95% CI) | P value |
|---|---|---|
| Expected disc height restoration | .239 (.030‐1.247) | .118 |
| Single-level cases | 1.313 (.971‐1.849) | .093 |
| Upper endplate Hounsfield units | ||
| Anterior epiphyseal ring | .996 (.988‐1.004) | .359 |
| Ipsilateral epiphyseal ring | 1.001 (.993‐1.009) | .801 |
| Contralateral epiphyseal ring | 1.002 (.995‐1.009) | .663 |
| Central endplate | 1.000 (.990‐1.009) | .947 |
| Lower endplate Hounsfield units | ||
| Anterior epiphyseal ring | .997 (.987‐1.005) | .418 |
| Posterior epiphyseal ring | .997 (.987‐1.007) | .569 |
| Ipsilateral epiphyseal ring | .986 (.974‐.995) | .008 |
| Central endplate | .996 (.985‐1.007) | .528 |
CI, confidence interval.
Figure 6.
Receiver operating characteristic curve of the Hounsfield unit value at ipsilateral epiphyseal ring predicting intraoperative endplate violation. The area under curve was .805.
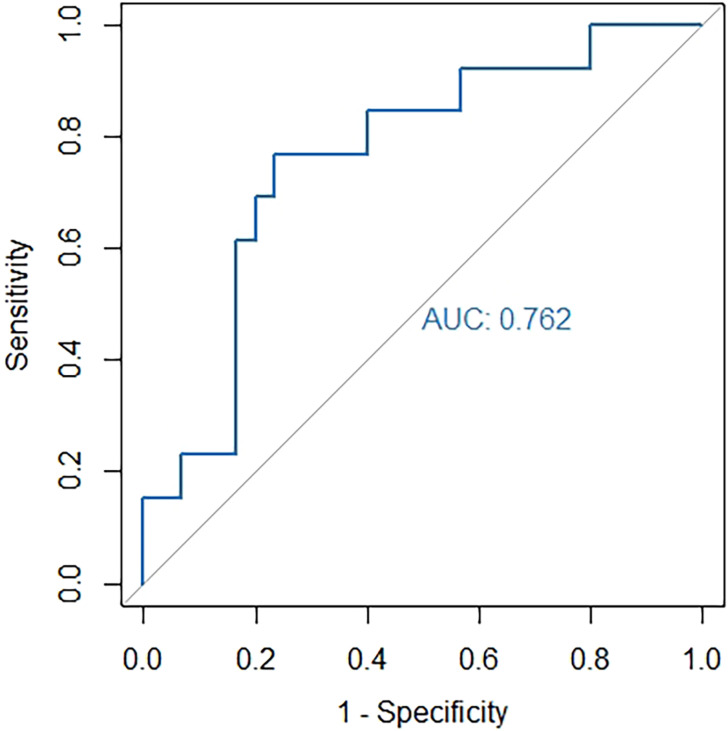
After excluding surgical levels with intraoperative endplate violation, 55 patients (82 levels) remained in the study. Of these 55 patients, 32 patients (58.2%, 42 levels) remained stand-alone throughout the follow-up period, and 23 patients (41.8%, 40 levels) had posterior instrumentation. No significant difference regarding the rate of delayed subsidence was found between patients who remained stand-alone and patients with posterior fixation (P > .05). VAS improvements at 1-year follow-up showed no significant difference between segments with or without delayed subsidence (P = .173). In stand-alone patients, delayed subsidence occurred in 10 patients (31.2%). 11 surgical levels (26.2%) had delayed subsidence in the lower endplate, and 3 surgical levels (7.1%) had delayed subsidence in the upper endplate. Delayed subsidence occurred at both endplates in 2 levels (4.8%). The HU value of the lower central endplate (Table 4) was the only factor significantly associated with delayed subsidence (P = .01). ROC curve (Figure 7) established separation criteria between stand-alone surgical levels with or without delayed subsidence (AUC: .76; [95% CI 0.604-.919]), and the most appropriate threshold was 296.42 HUs at the central endplate of the lower endplate (sensitivity 76.9%, specificity 76.6%). In patients who had posterior instrumentation, delayed subsidence occurred in 8 patients (34.8%). 7 surgical levels (17.5%) had delayed subsidence in the lower endplate, and 2 surgical levels (5%) had delayed subsidence in the upper endplate. Delayed subsidence occurred to both endplates in 1 level (2.5%). No significant correlation between HU values and delayed subsidence was found in patients with posterior fixation.
Table 4.
Univariate Analysis of Delayed Cage Subsidence in Stand-alone Patients.
| Parameter | Groups | P value | |
|---|---|---|---|
| No Delayed Subsidence | Delayed Subsidence | ||
| No. of patients | 22 (68.8%) | 10 (31.2%) | |
| No. of levels | 30 (71.4%) | 12 (28.6%) | |
| Mean age (years) | 64.3 ± 12.7 | 67.8 ± 7.4 | .385 |
| Mean BMI (kg/m2) | 24.3 ± 2.9 | 24.7 ± 3.8 | .703 |
| Single-level cases | 16 (72.7%) | 4 (40.0%) | .168 |
| BMD (mg/cm3) a | 1.37 ± .26 | 1.26 ± 0.2 | .205 |
| Cage height (mm) | 15.2 ± 1.3 | 15.1 ± 1.7 | .919 |
| Cage length (mm) | 52.5 ± 3.2 | 54.4 ± 4.2 | .231 |
| Expected disc height restoration (mm) | 5.4 ± 2.3 | 5.0 ± 2.0 | .643 |
| Actual disc height restoration (mm) | 4.9 ± 1.9 | 5.1 ± 2.8 | .743 |
| VAS at 1-year follow-up | 2.3 ± .9 | 2.0 ± 0.6 | .136 |
| VAS improvement at 1-year follow-up | 2.8 ± 1.5 | 2.4 ± 1.0 | .173 |
| Upper endplate Hounsfield unit | |||
| Anterior epiphyseal ring | 489.9 ± 105.7 | 538.2 ± 115.3 | .200 |
| Posterior epiphyseal ring | 560.2 ± 123.5 | 524.0 ± 121.5 | .394 |
| Ipsilateral epiphyseal ring | 594.3 ± 108 | 565.1 ± 151.1 | .486 |
| Contralateral epiphyseal ring | 549.2 ± 108.4 | 517.4 ± 75.7 | .360 |
| Central endplate | 448.8 ± 103.8 | 406.8 ± 70.9 | .206 |
| Lower endplate Hounsfield unit | |||
| Anterior epiphyseal ring | 447.7 ± 116.4 | 436.2 ± 76.4 | .755 |
| Posterior epiphyseal ring | 480.6 ± 66.4 | 468.1 ± 81.0 | .607 |
| Ipsilateral epiphyseal ring | 506.1 ± 96.8 | 452.3 ± 88.2 | .104 |
| Contralateral epiphyseal ring | 520.0 ± 95.3 | 521.2 ± 134.3 | .974 |
| Central endplate | 401.2 ± 78.1 | 336.3 ± 55.8 | .013 |
BMI, body mass index; BMD, bone mineral density; VAS, visual analogue scale.
a36 patients (58 levels) underwent bone mineral density scanning preoperatively.
Figure 7.
Receiver operating characteristic curves of the Hounsfield unit value at the central endplate predicting delayed subsidence in patients with stand-alone cages. The area under curve was .762.
Discussion
Endplate violation and delayed cage subsidence are potential complications after LIF surgery and may lead to poor surgical outcomes.12,13 It is crucial to identify risk factors for intraoperative endplate violation and delayed cage subsidence before the surgery so that these conditions can be optimized to maximize surgical outcomes. We found that low HU value at the ipsilateral epiphyseal ring of the lower endplate is an independent risk factor for intraoperative endplate violation, and low HU values at the central endplate of the lower endplate had significant correlation with delayed cage subsidence in stand-alone OLIF cases. HUs of the endplate are good predictors for intraoperative endplate violation and cage subsidence since they represent the regional bone quality of the endplate in contact with the implant.
In this study, the 23% rate of intraoperative endplate violation is in accordance with the previously reported rate of 16.8%, 20%, 24.8%, and 33.1% after LLIF procedures.8,14-16 The 42% rate of total postoperative cage subsidence in our study is at the upper end compared to previously reported range for stand-alone LLIF, with subsidence rate of 14%, 30%, and 32%. 8 As a variant of LLIF, OLIF offers a minimally invasive approach to achieve interbody distraction and fusion of the lumbar spine. Subsidence is a radiographic phenomenon after lumbar fusion surgery that manifests through the intervertebral cage collapsing into the adjacent vertebral endplates. In this study, the VAS scores were not significantly different between patients with and without intraoperative endplate violation at 1-week postoperatively, which is in accordance with the VAS changes reported by Marchi et al. 17 In addition, no significant difference in VAS score was found between patients with or without delayed cage subsidence at 1-year follow-up, similar to the results from previous reports.7,8,17,18 Further, patients with either intraoperative endplate violation or delayed cage subsidence showed no difference in VAS score at 1-year postoperatively. Although no clear correlation between the radiological subsidence and negative clinical outcomes has been reported,17-19 graft subsidence can be detrimental to the surgical goals of the LIF surgery, namely, mechanical stabilization, correction of sagittal alignment, distraction of the disc space, and decompression of neural elements.
Although low BMD was reported to be a risk factor for cage subsidence, 20 the same trend was not statistically significant in this study for both intraoperative endplate violation and delayed cage subsidence (P > .05). As the interface between implants and the vertebral bodies, endplates play an important role in distributing the compressive load on the vertebral bodies. Information concerning regional strength of the endplate can help the preoperative decision-making process and potentially improve the clinical outcome. Although BMD is considered the gold standard to measure bone quality, it is usually applied to a generalized structure and can be susceptible to overlying density such as the posterior arch and osteophytes. In an aging population including most of our patients, DEXA can also result in spuriously elevated BMD measurements in patients with degenerative disease, compression fractures, and vascular calcifications. 21 On the other hand, HU of the endplate can provide information about the bone density in a more specific region, which can be more relevant to the interaction between the implant and the endplate. In this study, routine preoperative CT imaging is conducted to examine the ossification of the herniated tissue or ligamentum flavum, which are contraindications for indirect decompression. Previous studies have shown that HU measurements correlate with success of lumbar interbody fusion, posterolateral fusion, cage subsidence, adjacent segment fractures, pedicle screw loosening, and risk of incidental durotomy.11,21 In addition, Xi et al. reported that the segmental HU values of the trabecular bone in vertebral bodies were associated with cage subsidence after LLIF. 22 Furthermore, Schreiber et al. have shown significant correlations between HU and BMD, and between HU and compressive strength using mechanical testing on polyurethane foam blocks (P < .001). 11 Further research may be necessary to determine the relationship between HU measurement and the strength of cortical bone shell on the surface of the vertebral endplate.
Endplates with lower HU at the ipsilateral epiphyseal ring (odds ratio = .986) are more likely to suffer intraoperative endplate injury. Intraoperative endplate violation is a common complication in LIF procedure that can potentially lead to poor clinical results and accelerated subsidence. Santoni et al. conducted a biomechanical study using a cadaver model of endplate injury in LIF and concluded that segmental stability may be compromised by the injury. 23 In addition, Tohmeh et al. reported a greater magnitude of subsidence progression in surgical levels that suffer intraoperative endplate injury. 15 During an OLIF surgery, the disc space is sequentially distracted with metal trials until adequate disc height was restored. In the process of distraction, the ipsilateral side of the epiphyseal ring is in the most frequent contact with the metal trial and withstands the largest impact. Based on the ROC curves, the most appropriate cut-off value for intraoperative endplate violation was 326.21 HUs at the ipsilateral epiphyseal ring of the lower endplate (sensitivity 79.0% and specificity 77.3%). In addition, we found that a multilevel procedure is a significant risk factor for intraoperative endplate violations, in accordance with previous reports. 24 For patients who undergo multilevel procedure for deformity correction, posterior instrumentation should be considered as they have higher risks of suffering cage subsidence. Furthermore, the expected disc height restoration was significantly larger in levels with endplate violation, suggesting that overly aggressive distraction for disc height restoration can lead to unwanted endplate injury. Although disc height restoration is an important goal of OLIF surgery, inserting a cage too tall for the intervertebral space can lead to endplate violation and consequently compromised clinical results.
HU of the central endplate was the only parameter that showed a significant association with delayed subsidence in stand-alone patients, while no significant correlation was found between HU of the epiphyseal ring and delayed subsidence. Delayed cage subsidence is considered by some to be part of the normal healing process. Choi et al. described postoperative cage subsidence in anterior interbody fusion as a normal incorporation process of the cage to achieve better contact with both endplates, which have different surface shapes. 25 It is worth noting that a certain degree of bone settling process occurs naturally during the arthrodesis process. 6 This minimal integration occurs during primary stabilization (resorptive phase) and does not interfere with subsequent bone formation. Due to the shape and dimension of the cage, the anterior epiphyseal ring and posterior epiphyseal ring were usually not in direct contact with the fusion cage. In the endplates where delayed subsidence occurs, 10 cases showed collapse at the anterior interface between the cage and the endplate, 7 cases showed collapse at the posterior interface, and 3 cases had collapse at both interfaces. Except for the endplate collapses which resulted from intraoperative endplate violation, no delayed collapse occurred to the two lateral sides of the epiphyseal ring. Although rim-bearing placement of the cage is the goal of the OLIF procedure, the convex surface of the cage will inevitably be in contact with the central endplate after the natural settling during the resorptive phase. Due to stronger mechanical properties of the ipsilateral and contralateral epiphyseal ring compared to that of the central endplate, their involvement in the subsidence process may be reduced. Based on the ROC curve, the most appropriate threshold to predict delayed subsidence in stand-alone OLIF cases is 296.42 HUs at the central endplate of the lower endplate (sensitivity 76.9% and specificity 76.6%). Based on the radiological results, if the cage can be successfully placed over the epiphyseal ring without violating the endplate, the epiphyseal ring can provide solid support for the cage, as no delayed collapse at the epiphyseal ring was observed.
There are a few limitations in this study. Firstly, the assessment of VAS after OLIF surgery may not coincide directly with the timing of subsidence. To have a standardized timepoint of VAS assessment, we set up pain evaluation 1 week after the surgery, which can still be later than the occurrence of intraoperative endplate violation. Secondly, this study mainly focused on the radiographic subsidence after OLIF surgery. Comparison of corrections in alignment and fusion rates should be studied in future studies. In addition, the use of dynamic radiographs to see the degree of segmental instability is warranted.26,27 Further studies with longer follow-up periods may be needed to investigate whether posterior instrumentation in OLIF surgery reduces the progression from intraoperative endplate violation to more severe cage subsidence.
Conclusions
This study showed that endplate violations and delayed cage subsidence is not uncommon for OLIF surgery. Low HU value at the ipsilateral epiphyseal ring is an independent risk factor for intraoperative endplate violation after OLIF surgery. Low HU value at the central endplate is significantly associated with delayed cage subsidence in stand-alone cases. HU of the central endplate is a good addition to BMD as a predictor for cage subsidence since it can represent the regional bone quality of the endplate in contact with the implant. VAS improvements were not affected by intraoperative endplate violation or delayed cage subsidence at 1-year follow-up. Measures may be taken preoperatively to maximize the HU to reduce the risk of surgical complications related to endplate violation and cage subsidence. Meanwhile, patients with higher HU values at the endplate may be better candidates for stand-alone OLIF surgery.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the S.K. Yee Medical Foundation Grant (#2171223) and the AOSpine Asia Pacific Regional Research Project Grant.
Ethics Approval: Ethical approval was obtained from the Institutional Ethics Committee of Sir Run Run Shaw Hospital, Zhejiang University (ref#: 20200914-30).
ORCID iDs
Teng Zhang https://orcid.org/0000-0002-5310-8766
Fengdong Zhao https://orcid.org/0000-0002-2945-8707
References
- 1.Mehren C, Mayer HM, Zandanell C, et al. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res. 2016;474:2020-2027. doi: 10.1007/s11999-016-4883-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Zeng ZY, Xu ZW, He DW, et al. Complications and prevention strategies of oblique lateral interbody fusion technique. Orthop Surg. 2018;10:98-106. doi: 10.1111/os.12380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zhu G, Hao Y, Yu L, et al. Comparing stand-alone oblique lumbar interbody fusion with posterior lumbar interbody fusion for revision of rostral adjacent segment disease: A STROBE-compliant study. Medicine (Baltimore). 2018;97:e12680. doi: 10.1097/md.0000000000012680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cappuccino A, Cornwall GB, Turner AW, et al. Biomechanical analysis and review of lateral lumbar fusion constructs. Spine (Phila Pa 1976). 2010;35:S361-S367. doi: 10.1097/BRS.0b013e318202308b. [DOI] [PubMed] [Google Scholar]
- 5.Ohtori S, Mannoji C, Orita S, et al. Mini-open anterior retroperitoneal lumbar interbody fusion: Oblique lateral interbody fusion for degenerated lumbar spinal kyphoscoliosis. Asian Spine J. 2015;9:565-572. doi: 10.4184/asj.2015.9.4.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rentenberger C, Okano I, Salzmann SN, et al. Perioperative risk factors for early revisions in stand-alone lateral lumbar interbody fusion. World Neurosurg. 2020;134:e657-e663. doi: 10.1016/j.wneu.2019.10.164. [DOI] [PubMed] [Google Scholar]
- 7.Malham GM, Parker RM, Blecher CM, et al. Assessment and classification of subsidence after lateral interbody fusion using serial computed tomography. J Neurosurg Spine. 2015;23:589-597. doi: 10.3171/2015.1.Spine14566. [DOI] [PubMed] [Google Scholar]
- 8.Satake K, Kanemura T, Nakashima H, et al. Cage subsidence in lateral interbody fusion with transpsoas approach: Intraoperative endplate injury or late-onset settling. Spine Surg Relat Res. 2017;1:203-210. doi: 10.22603/ssrr.1.2017-0004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dar G, Masharawi Y, Peleg S, et al. The epiphyseal ring: A long forgotten anatomical structure with significant physiological function. Spine (Phila Pa 1976). 2011;36:850-856. doi: 10.1097/BRS.0b013e3181e9b19d. [DOI] [PubMed] [Google Scholar]
- 10.Briski DC, Goel VK, Waddell BS.et al. Does spanning a lateral lumbar interbody cage across the vertebral ring apophysis increase loads required for failure and mitigate endplate violation. Spine (Phila Pa 1976). 2017;42:E1158-e1164. doi: 10.1097/brs.0000000000002158. [DOI] [PubMed] [Google Scholar]
- 11.Schreiber JJ, Anderson PA, Rosas HG, et al. Hounsfield units for assessing bone mineral density and strength: A tool for osteoporosis management. J Bone Joint Surg Am. 2011;93:1057-1063. doi: 10.2106/jbjs.J.00160. [DOI] [PubMed] [Google Scholar]
- 12.Zhang T, Bai S, Dokos S, et al. XLIF interbody cage reduces stress and strain of fixation in spinal reconstructive surgery in comparison with TLIF cage with bilateral or unilateral fixation: a computational analysis. Conf Proc IEEE Eng Med Biol Soc; 2019; 23-27 July 2019; Berlin, Germany, pp. 1887-1890. doi: 10.1109/embc.2019.8856592. [DOI] [PubMed] [Google Scholar]
- 13.Zhang T, Ren X, Feng X, et al. Failure mechanisms of pedicle screws and cortical screws fixation under large displacement: A biomechanical and microstructural study based on a clinical case scenario. J Mech Behav Biomed Mater. 2020;104:103646. doi: 10.1016/j.jmbbm.2020.103646. [DOI] [PubMed] [Google Scholar]
- 14.Kim SJ, Lee YS, Kim YB, et al. Clinical and radiological outcomes of a new cage for direct lateral lumbar interbody fusion. Korean J Spine. 2014;11:145-151. doi: 10.14245/kjs.2014.11.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tohmeh AG, Khorsand D, Watson B, et al. Radiographical and clinical evaluation of extreme lateral interbody fusion: Effects of cage size and instrumentation type with a minimum of 1-year follow-up. Spine (Phila Pa 1976). 2014;39:E1582-E1591. doi: 10.1097/brs.0000000000000645. [DOI] [PubMed] [Google Scholar]
- 16.Shiga Y, Orita S, Inage K, et al. Evaluation of the location of intervertebral cages during oblique lateral interbody fusion surgery to achieve sagittal correction. Spine Surg Relat Res. 2017;1:197-202. doi: 10.22603/ssrr.1.2017-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marchi L, Abdala N, Oliveira L, et al. Radiographic and clinical evaluation of cage subsidence after stand-alone lateral interbody fusion. J Neurosurg Spine. 2013;19:110-118. doi: 10.3171/2013.4.Spine12319. [DOI] [PubMed] [Google Scholar]
- 18.Bocahut N, Audureau E, Poignard A, et al. Incidence and impact of implant subsidence after stand-alone lateral lumbar interbody fusion. Orthop Traumatol Surg Res. 2018;104:405-410. doi: 10.1016/j.otsr.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 19.Oh KW, Lee JH, Lee JH, et al. The correlation between cage subsidence, bone mineral density, and clinical results in posterior lumbar interbody fusion. Clin Spine Surg. 2017;30:E683-e689. doi: 10.1097/bsd.0000000000000315. [DOI] [PubMed] [Google Scholar]
- 20.Wu H, Shan Z, Zhao F, Cheung JPY. Poor bone quality, multilevel surgery, and narrow and tall cages are associated with intraoperative endplate injuries and late-onset cage subsidence in lateral lumbar interbody fusion: A systematic review. Clin Orthop Relat Res. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zaidi Q, Danisa OA, Cheng W. Measurement techniques and utility of hounsfield unit values for assessment of bone quality prior to spinal instrumentation: A review of current literature. Spine (Phila Pa 1976). 2019;44:E239-E244. doi: 10.1097/BRS.0000000000002813. [DOI] [PubMed] [Google Scholar]
- 22.Xi Z, Mummaneni PV, Wang M, et al. The association between lower Hounsfield units on computed tomography and cage subsidence after lateral lumbar interbody fusion. Neurosurg Focus. 2020;49:E8. doi: 10.3171/2020.5.Focus20169. [DOI] [PubMed] [Google Scholar]
- 23.Santoni BG, Alexander GE,, 3rd, Nayak A, et al. Effects on inadvertent endplate fracture following lateral cage placement on range of motion and indirect spine decompression in lumbar spine fusion constructs: A cadaveric study. Int J Spine Surg. 2013;7:e101-108. doi: 10.1016/j.ijsp.2013.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Le TV, Baaj AA, Dakwar E, et al. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 2012;37:1268-1273. doi: 10.1097/BRS.0b013e3182458b2f. [DOI] [PubMed] [Google Scholar]
- 25.Choi JY, Sung KH. Subsidence after anterior lumbar interbody fusion using paired stand-alone rectangular cages. European Spine Journal. 2006;15:16-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheung JP, Cheung PW, Cheung KM, et al. Decompression without fusion for low-grade degenerative spondylolisthesis. Asian Spine J. 2016;10:75-84. doi: 10.4184/asj.2016.10.1.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Cheung JPY, Fong HK, Cheung PWH. Predicting spondylolisthesis correction with prone traction radiographs. Bone Joint J. 2020;102-B:1062-1071. doi: 10.1302/0301-620x.102b8.Bjj-2020-0528.R1. [DOI] [PubMed] [Google Scholar]