Abstract
Study Design
Retrospective cohort study
Objectives
This study aimed to report the incidence and potential risk factors of polyetheretherketone (PEEK) cage subsidence following oblique lateral interbody fusion (OLIF) for lumbar degenerative diseases. We proposed also an algorithm to minimize subsidence following OLIF surgery.
Methods
The study included a retrospective cohort of 107 consecutive patients (48 men and 59 women; mean age, 67.4 years) who had received either single- or multi-level OLIF between 2012 and 2019. Patients were classified into subsidence and non-subsidence groups. PEEK cage subsidence was defined as any violation of either endplate from the computed tomography scan in both sagittal and coronal views. Preoperative variables such as age, sex, body mass index, bone mineral density (BMD) measured by preoperative dual-energy X-ray absorptiometry, smoking status, corticosteroid use, diagnosis, operative level, multifidus muscle cross-sectional area, and multifidus muscle fatty degeneration were collected. Age-related variables (height and length) were also documented. Univariate and multivariate logistic regression analyses were used to analyze the risk factors of subsidence.
Results
Of the 107 patients (137 levels), 50 (46.7%) met the subsidence criteria. Higher PEEK cage height had the strongest association with subsidence (OR = 9.59, P < .001). Other factors significantly associated with cage subsistence included age >60 years (OR = 3.15, P = .018), BMD <−2.5 (OR = 2.78, P = .006), and severe multifidus muscle fatty degeneration (OR = 1.97, P = .023).
Conclusions
Risk factors for subsidence in OLIF were age >60 years, BMD < −2.5, higher cage height, and severe multifidus muscle fatty degeneration. Patients who had subsidence had worse early (3 months) postoperative back and leg pain.
Keywords: interbody cage, oblique lateral interbody fusion, risk factors, polyetheretherketone cage subsidence, lumbar degenerative disease
Introduction
Lumbar interbody fusion has become a commonly performed procedure for the treatment of degenerative lumbar disorders refractory to conservative care. The goals are to achieve adequate neural decompression and solid fusion while correcting or maintaining spinal alignment. Various types of lumbar interbody fusion have been advocated including posterior lumbar interbody fusion, transforaminal lumbar interbody fusion, lateral lumbar interbody fusion (LLIF), and anterior lumbar interbody fusion (ALIF). Minimally invasive anterior approaches such as ALIF and LLIF can help achieve an “indirect” posterior decompression by restoring intervertebral disc height, thereby widening the neural foramen and spinal canal.1-3 LLIF is further divided into the transpsoas approach, commonly known as direct or extreme lateral lumbar interbody fusion (DLIF or XLIF), and the prepsoas or antepsoas approach (oblique lumbar interbody fusion; OLIF). Among LLIF procedures, OLIF has several advantages, including less psoas muscle and lumbar plexus violation, direct visualization of sensory nerves and structures such as the ureter and sympathetic chain, no need for neuromonitoring, and access to spinal pathology down to the L5-S1 level. 3
However, OLIF can result in several complications. The subsidence of the polyetheretherketone (PEEK) cage is considered the most common potential perioperative complication. 4 Patients experiencing subsidence may be asymptomatic or have symptoms which necessitate revision surgery. Moreover, to our knowledge, potential risk factors for cage subsidence have not been published elsewhere in the literature.
Therefore, this study aimed to report the incidence, pattern of endplate violation, and potential risk factors of PEEK cage subsidence following OLIF for lumbar degenerative diseases and to provide reference or guidance in clinical decision making for spinal surgeons.
Material and Methods
Study Design
For this study, a retrospective cohort of 107 consecutive patients (48 men and 59 women; mean age, 67.4 years) who received either single- or multi-level OLIF between 2012 and 2019 were included. The mean follow-up period was 34.2 months (24–72 months). Inclusion criteria were: (1) symptomatic lumbar degenerative disease (spondylolisthesis, degenerative scoliosis, degenerative disc disease, or others) that did not improve after at least 3 months of conservative measure(s); (2) patients whose magnetic resonance imaging (MRI) and computed tomography (CT) scans correlated with clinical symptoms; and (3) operative level included from L2 to L5. Exclusion criteria were as follows: (1) patients who underwent combined/additional lumbar interbody fusion or additional posterior direct decompression; (2) patients who had previous lumbar instrumentation; (3) patients who did not complete at least 24 months of follow-up; (4) patients who had a major accident/fall, which proved to be the cause of subsidence; and (5) patients who had intraoperative endplate injury, as proven by the contrast medium filling technique.
Ethical Considerations
All procedures were performed in compliance with relevant laws and institutional guidelines approved by the Institutional Review Board of the institution. The participants provided written informed consent for the study and publication.
Surgical Technique
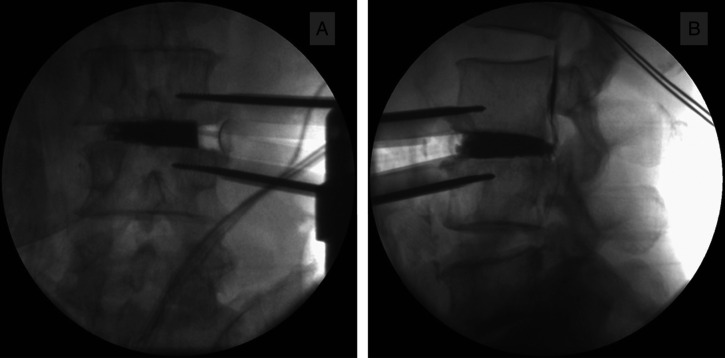
Preoperative retroperitoneal oblique corridor from MRI was assessed in each patient to ensure available access to the intervertebral disc (IVD) space. All OLIF procedures were performed by the senior author (K.JS) using the OLIF25 Clydesdale Spinal System (Medtronic Sofamor Danek, Minneapolis, MN, USA) as described previously. 5 Briefly, patients were placed in the right lateral decubitus position, and skin marking was performed under intraoperative fluoroscopic guidance. A 5- to 10-cm skin incision was made, and serial abdominal muscle dissection was performed using the muscle splitting technique. Serial dilators were sequentially applied, and a 22-mm diameter tubular retractor with a measured length was docked in. The intervertebral disc space was exposed after blunt dissection and anterior peritoneal mobilization. After the index level confirmation, careful IVD removal and endplate preparation were performed using pituitary forceps, disc shavers, curettes, and Cobb elevators. We used the intraoperative contrast medium filling technique to ensure adequate discectomy and endplate preparation or to detect any intraoperative endplate injury or violation (Figure 1A and 1B). After sizing, a similar PEEK cage design was used in all participants (6 °Clydesdale; Medtronic Sofamor Danek, Memphis, Tennessee, USA]) and filled with demineralized bone matrix and rhBMP2. Fluoroscopic images were obtained to confirm the appropriate length of the cage that must be seated on the apophyseal ring bilaterally. Then, additional percutaneous posterior pedicular screw fixation in all fusion segments was performed in the prone position for all patients.
Figure 1.
“Contrast filling technique” from fluoroscopic anteroposterior (A) and lateral (B) views to ensure the adequacy of the intervertebral discectomy and look for any intraoperative endplate injury.
Radiological and Clinical Evaluation
The patients were classified into either the subsidence or non-subsidence group. We collected preoperative variables including age, sex, body mass index (BMI), bone mineral density (BMD), smoking status, steroid use, diagnosis, operative level, multifidus muscle cross-sectional area, and multifidus muscle atrophy. 6 The age-related variables (height and length) were also documented. Radiographically, we measured the preoperative anterior disc height (ADH), posterior disc height (PDH), segmental lordosis (SL), pelvic incidence (PI), sacral slope (SS), pelvic tilt (PT), lumbar lordosis (LL), and sagittal vertical axis (SVA) and compared them with the immediate postoperative and 1-year follow-up measures. CT was performed at 6 and 12 months postoperatively to justify a solid fusion and evaluate the subsidence patterns.
Regarding the clinical outcomes, we collected the visual analog scale (VAS) score for back and leg pain (range, 0–100) and the Oswestry Disability Index (ODI) score (range, 0–100) prior to surgery, and at 3, 6, and 12 months postoperatively.
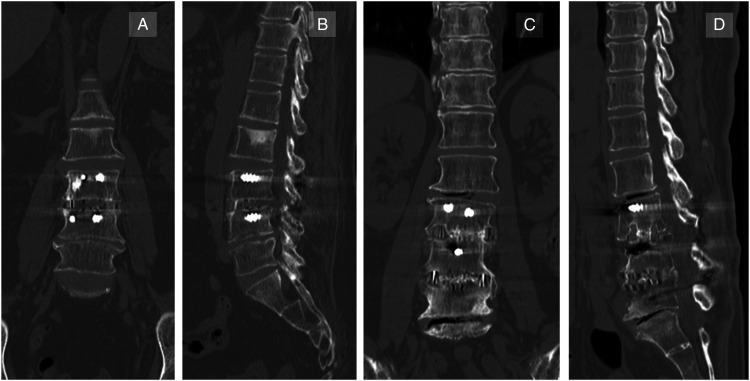
Subsidence and Fusion Evaluation
Subsidence of the PEEK cage was defined as any violation of either endplate as seen from the lateral plain radiograph and confirmed by the thin-slice CT scan in both sagittal and coronal views; every image cut was enlarged 200% before measurement to increase accuracy (Figure 2). Time-to-subsidence was obtained by tracing back the follow-up lateral radiography; any earliest endplate violation from the plain radiography was taken as the time-to-subsidence. The patterns of subsidence were classified based on the characteristics of endplate violations. Fusion was evaluated using the Bridwell fusion grading system on CT scans; grades 1 and 2 were defined as fused spinal constructs. All measurements and evaluations concerning radiography were initially performed by the first author, and the two other surgeons reviewed and confirmed the results. Interobserver reliability was examined using Pearson’s correlation coefficients of the first and second measurements. A biostatistician performed the analyses.
Figure 2.
Thin-slice postoperative computed tomography (CT) scan showing the fusion level without subsidence (A, B) and the fusion level with subsidence (C, D).
Statistical Analysis
Descriptive statistics were presented as mean ± standard deviation for continuous variables and as frequency and percentage for categorical variables. Univariate logistic regression analysis was used to determine the correlation between independent outcome variables and dichotomous variables (i.e., subsidence and non-subsidence). Among these statistically significant and clinically meaningful variables, we further conducted a multivariate logistic regression analysis to control for confounding effects. A chi-squared test (χ2) was used, and the adjusted odds ratios (ORs) with 95% confidence intervals (CIs) for each variable were expressed. Furthermore, we compared the clinical outcomes between the subsidence and non-subsidence groups using the independent-samples t-test. A P-value of less than or equal to .05 was considered statistically significant. Statistical analyses were performed by a biostatistician using SPSS software (version 23.0; IBM SPSS Statistics for Windows, IBM Corp, Armonk, NY).
Results
Of the 107 patients, 50 patients (46.7%) met the subsidence criteria. The mean BMI was 25.36 kg/m2. Forty-eight (44.9%) were men, and 59 (55.1%) were women. Thirty-three patients (30.8%) had a BMD below −2.5, 51 patients (47.7%) had a BMD between −2.5 and −1.5, and 23 patients (24.6%) had a BMD above −1.5. Tobacco use was found in 16 patients (25.6%), and 4 patients (6.3%) used corticosteroids. The diagnoses were degenerative scoliosis (30 patients, 28.0%), degenerative spondylolisthesis (37 patients, 34.6%), isthmic spondylolisthesis (32 patients, 29.9%), and recurrent lumbar disc herniation (8 patients, 7.48%). Sixty-four (59.8%) patients underwent single-level and 43 (40.2%) underwent multi-level surgery. The mean multifidus muscle cross-sectional area was 778.37 m2. Twenty-four patients (22.4%) had no atrophy, 24 patients (22.4%) had mild atrophy, 27 patients (25.2%) had moderate atrophy, and 32 patients (29.9%) had severe atrophy (Table 1). For the PEEK cage characteristics, 20 levels used 8-mm, 37 levels used 10-mm, and 33 levels used 12-mm cage height. Seven levels used 40-mm, 87 levels used 45-mm, and 13 levels used 50-mm cage length. L4/5 was the most operated level, followed by L3/4 and L2/3 (Table 2).
Table 1.
Comparison of Preoperative Parameters of the Subsidence and Non-subsidence groups.
| Subsidence Group (N = 50) | Non-subsidence Group (N = 57) | P-Value | |
|---|---|---|---|
| Age (years)* | 64.41 ± 16.23 | 59.36 ± 17.74 | .033 |
| Sex (male: female) | 24: 26 | 24: 33 | .722 |
| BMI (kg/m2) | 25.43 ± 4.63 | 24.22 ± 6.41 | .513 |
| BMD* | −.85 ± .92 | −.13 ± .88 | .015 |
| Tobacco use | 7 | 9 | .714 |
| Steroid use | 2 | 2 | .189 |
| Diagnosis | |||
| Degenerative scoliosis | 14 | 16 | .092 |
| Spondylolisthesis (Degen.) | 18 | 19 | .121 |
| Spondylolisthesis (Isthmic) | 14 | 18 | .077 |
| DDD, recurrent HNP, others | 4 | 4 | 1.000 |
| Preoperative anterior disc height | 7.75 ± 1.24 | 7.83 ± 1.53 | .553 |
| Preoperative posterior disc height | 8.06 ± 1.63 | 8.21 ± 1.29 | .298 |
| Fusion segments | |||
| Single-level | 30 | 34 | .317 |
| More than 1 levels | 20 | 23 | .532 |
| Multifidus muscle area (mm2)* | 832.32 ± 82.53 | 864.18 ± 91.24 | .036 |
| Multifidus muscle fatty degeneration | |||
| Grade I (normal) | 8 | 16 | .066 |
| Grade II (mild) | 8 | 16 | .066 |
| Grade III (moderate) | 12 | 15 | .178 |
| Grade IV (severe)* | 22 | 10 | .042 |
Values indicate absolute numbers or mean ± SD.
BMD indicates bone mineral density; DDD indicates degenerative disc disease; HNP indicates herniated nucleus pulposus; BMI indicates body mass index.
*Statistically significant difference (P < .05).
Table 2.
Radiographic Variables and Polyetheretherketone Cage-Related Variables.
| Subsidence Levels (N = 57) | Non-subsidence Levels (N = 80) | P Value | |
|---|---|---|---|
| Radiographic variables (mean) | |||
| ADH (mm) | |||
| Pre | 5.03 ± 3.65 | 4.85 ± 6.79 | .544 |
| Post | 6.24 ± 2.99 | 9.14 ± 5.72 | .035* |
| PDH (mm) | |||
| Pre | 4.58 ± 3.87 | 4.25 ± 5.43 | .314 |
| Post | 5.89 ± 5.43 | 8.54 ± 6.16 | .042* |
| SL (o) | |||
| Pre | 4.36 ± 2.31 | 5.12 ± 6.83 | .131 |
| Post | 6.44 ± 4.65 | 7.44 ± 4.65 | .901 |
| PI (o) | |||
| Pre | 54.21 ± 13.29 | 51.88 ± 22.17 | .081 |
| Post | |||
| SS (o) | |||
| Pre | 25.67 ± 8.11 | 27.32 ± 6.89 | .094 |
| Post | 29.23 ± 9.91 | 32.23 ± 5.21 | .064 |
| PT (o) | |||
| Pre | 11.75 ± 6.42 | 12.85 ± 8.27 | .112 |
| Post | 15.24 ± 12.12 | 17.18 ± 10.26 | .087 |
| LL (o) | |||
| Pre | 26.67 ± 12.77 | 25.79 ± 13.02 | .226 |
| Post | 32.21 ± 10.35 | 36.21 ± 19.56 | .019* |
| SVA (mm) | |||
| Pre | 48.22 ± 21.53 | 47.22 ± 18.33 | .199 |
| Post | 40.91 ± 18.24 | 38.13 ± 15.61 | .077 |
| Operated levels | |||
| L2/3 | 11 | 15 | .322 |
| L3/4 | 18 | 25 | .096 |
| L4/5 | 28 | 40 | .061 |
| PEEK height | |||
| 8 mm | 10 | 20 | .078 |
| 10 mm | 20 | 37 | .015* |
| 12 mm | 27 | 16 | .042* |
| PEEK length | |||
| 40 mm | 8 | 9 | .893 |
| 45 mm | 39 | 58 | .058 |
| 50 mm | 10 | 13 | .112 |
Values indicate mean and absolute numbers.
PDH, posterior disc height; SL, segmental lordosis; PI, pelvic incidence; SS, sacral slope; PT, pelvic tilt; LL, lumbar lordosis; SVA, sagittal vertical axis; Pre, preoperative; Post, postoperative (at 1 year); PEEK, polyetheretherketone; ADH, anterior disc height.
*Statistically significant difference (P < .05).
Radiological Outcomes and Pelvic Parameter
The preoperative ADH and PDH were 5.03 ± 3.65 mm and 4.58 ± 3.87 mm in the subsidence group and 4.85 ± 6.79 mm and 4.25 ± 5.43 mm in the non-subsidence group, respectively. The difference between the groups was not statistically significant. The 1-year postoperative ADH and PDH after surgery were 6.24 ± 2.99 mm and 5.89 ± 5.43 mm in the subsidence group, and 9.14 ± 5.72 mm and 8.54 ± 6.16 mm in the non-subsidence group with statistically significant difference between groups (P = .035 and P = .042, respectively). Preoperative and follow-up SL did not differ between the 2 groups (P = .131 and P = .901, respectively).
Preoperative pelvic parameters (PI, SS, PT, LL, and SVA) showed no statistical difference between the groups. The 1-year follow-up parameter demonstrated that only the LL achieved was statistically different, 32.21 ± 10.35o vs 36.21 ± 19.56o (P = .019), indicating that patients in the non-subsidence group achieved more lumbar lordosis than patients in the subsidence group.
Subsidence Times and Fusion
The mean time-to-fusion was 9.6 ± 3.5 months in the subsidence group and 9.2 ± 4.1 months in the non-subsidence group. The non-subsidence group achieved a higher fusion rate at 1 year than the subsidence group (97.5% [78/80] vs 93.0% [53/57]). Moreover, the average time-to-subsidence was 3.7 ± 2.2 months (Table 3).
Table 3.
Fusion Rate and Time-to-Subsidence.
| Subsidence Levels (N = 57) | Non-subsidence Levels (N = 80) | |
|---|---|---|
| Fusion rate (at 1 year) | 93.0% (53/57) | 97.5% (78/80) |
| Fusion time (mo) | 9.6 ± 3.5 | 9.2 ± 4.1 |
| Time-to-subsidence (mo) | 3.7 ± 2.2 |
Subsidence Pattern
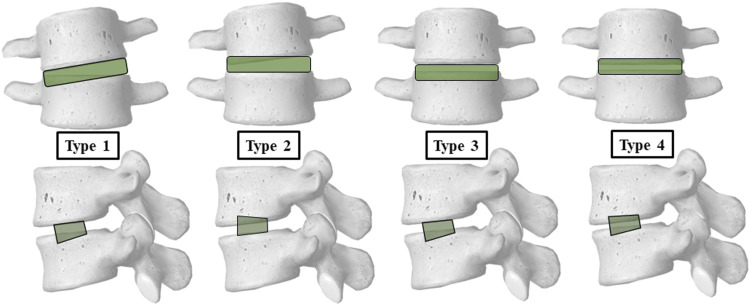
We observed the subsidence pattern at each specific level and categorized them into 4 types as follows (Figure 3):
Type 1. Contralateral caudal endplate subsidence: 35.09% (20/57 levels)
Type 2. Contralateral cranial endplate subsidence: 22.81% (13/57 levels)
Type 3. Bilateral caudal endplate subsidence: 14.04% (8/57 levels)
Type 4. Bilateral caudal and cranial endplate subsidence: 9.12% (16/57 levels)
Figure 3.
Subsidence type observed from this study; Type 1: Contralateral caudal endplate subsidence; Type 2: Contralateral cranial endplate subsidence; Type 3: Bilateral caudal endplate subsidence; and Type 4: Bilateral caudal and cranial endplate subsidence.
As the cage was inserted from the left side of the patient in the right lateral decubitus position, the contralateral endplate subsidence referred to subsidence involving the endplate on the right side of the patient while the bilateral referred to subsidence involving both the left and right sides of the endplate.
Risk Factor and ORs of Risk Factors Affecting Postoperative Subsidence
Patients who underwent surgery using a 12-mm PEEK cage were more than 9-fold more likely to exhibit subsidence than those who underwent surgery with the use of an 8-mm PEEK cage (OR = 9.59; P < .001). The patients were categorized into 2 age groups based on a cutoff of 60 years, and the risk of subsidence was higher in patients aged 60 years and older than in those younger than 60 years (OR = 3.15; P = .018). Furthermore, patients with a BMD of −2.5 and below were almost thrice more likely to display subsidence than those whose BMD was −1.5 and above (OR = 2.78; P = .006). Lastly, patients with preoperative severe multifidus muscle fatty degeneration were twice more likely to have postoperative subsidence than those with normal or no multifidus muscle fatty degeneration (OR = 1.97; P = .023). However, preoperative BMI and smoking status did not appear to affect postoperative subsidence (Table 4).
Table 4.
Multivariate Logistic Regression Analysis of Risk Factors for Polyetheretherketone Cage Subsidence.
| Variables | Adjusted Odds Ratio (95% CI) | P |
|---|---|---|
| Age (yr) | ||
| ≤60 | Reference | 1 |
| >60* | 3.149 (1.588-16.864) | .018* |
| BMI (m2/kg) | ||
| Normal (<25) | Reference | 1 |
| Overweight (≥25) | .626 (.215-1.822) | .39 |
| BMD | ||
| ≤ −2.5* | 2.777 (1.155-3.903) | .006* |
| −1.5 to −2.5 | .429 (.083-2.212) | .312 |
| ≥ −1.5 | Reference | 1 |
| Tobacco use | ||
| No | Reference | 1 |
| Yes | 2.366 (.459-12.193) | .303 |
| PEEK cage height | ||
| 8 | Reference | 1 |
| 10 | 3.112 (.834-5.281) | .342 |
| 12 | 9.588 (3.364-27.894) | <.001* |
| Multifidus muscle fatty degeneration | ||
| Normal | Reference | 1 |
| Mild | .315 (.014-7.316) | .472 |
| Moderate | .974 (.04-23.719) | .987 |
| Severe | 1.965 (1.523-40.774) | .023* |
PEEK, Polyetheretherketone; CI, confidence interval; BMI, body mass index; BMD, bone mineral density.
*Statistically significant difference (P < .05).
Clinical Outcomes
We measured the ODI and VAS scores for the back and leg before surgery and immediately postoperatively and at 3 months, 6 months, and 1 year after surgery. Preoperatively, the ODI score and the back and leg VAS scores were 44.65 ± 11.38, 6.27 ± 1.64, and 5.52 ± 1.93, respectively, in the subsidence group and 43.13 ± 13.6, 5.93 ± 1.55, and 5.22 ± 1.26, respectively, in the non-subsidence group. The follow-up postoperative periods showed a significant reduction in the ODI and VAS scores for the back and leg at 3 months, 6 months, and 1 year postoperatively.
However, between-group results revealed only the VAS reduction at the 3-month follow-up was significantly higher in the non-subsidence group (−1.89 ± 1.22 vs −3.24 ± .83, P = .032). Otherwise, there were no significant differences in the ODI score and the back and leg VAS scores between the two groups before and after surgery (P > .05) (Table 5).
Table 5.
Subsidence Correlated with Clinical Outcomes.
| Variables | Subsidence Group (N = 50) | Non-subsidence Group (N = 57) | |
|---|---|---|---|
| Mean ± SD. | Mean ± SD. | P | |
| ODI | |||
| Preoperative | 44.65 ± 11.38 | 43.13 ± 13.6 | .647 |
| Immediate PO | 32.45 ± 14.23 | 33.13 ± 15.25 | .202 |
| 3 months | 30.06 ± 11.81 | 27.29 ± 11.53 | .386 |
| 6 months | 24.76 ± 9.36 | 24.42 ± 9.85 | .897 |
| 1 year | 19.47 ± 8.27 | 17.63 ± 6.35 | .392 |
| Change at 3 months | −14.59 ± 10.03 | −15.84 ± 9.87 | .649 |
| Change at 6 months | −19.89 ± 11.38 | −18.71 ± 8.32 | .685 |
| Change at 1 year | −25.18 ± 9.73 | −25.5 ± 9.93 | .906 |
| VAS back | |||
| Preoperative | 6.27 ± 1.64 | 5.93 ± 1.55 | .285 |
| Immediate PO | 3.21 ± 1.68 | 3.26 ± 2.45 | .412 |
| 3 months | 2.58 ± 1.45 | 1.95 ± 1.35 | .111 |
| 6 months | 1.93 ± 1.29 | 1.79 ± 1.08 | .671 |
| 1 year | 1.89 ± 1.47 | 1.62 ± 0.9 | .379 |
| Change at 3 months | −1.89 ± 1.22 | −3.24 ± .83 | .032* |
| Change at 6 months | −3.33 ± 1.38 | −3.01 ± 1.53 | .296 |
| Change at 1 year | −3.58 ± 1.39 | −3.37 ± 1.54 | .495 |
| VAS leg | |||
| Preoperative | 5.52 ± 1.93 | 5.22 ± 1.26 | .474 |
| Immediate PO | 2.62 ± 1.67 | 2.35 ± 1.73 | .242 |
| 3 months | 2.44 ± 1.33 | 2.21 ± 1.29 | .151 |
| 6 months | 1.57 ± 1.09 | 1.44 ± .62 | .574 |
| 1 year | 1.53 ± 1.18 | 1.78 ± .73 | .326 |
| Change at 3 months | −2.47 ± 1.56 | −2.61 ± 1.53 | .08 |
| Change at 6 months | −2.95 ± 1.46 | −2.78 ± 1.44 | .666 |
| Change at 1 year | −2.98 ± 1.66 | −2.29 ± 1.21 | .129 |
SD, standard deviation; ODI, Oswestry disability index; VAS, visual analog scale; PO, postoperative.
Discussion
Cage subsidence after interbody fusion negatively affects surgical outcomes and is one of the most common complications after OLIF surgery. To optimize the outcomes following OLIF, we identified risk factors leading to cage subsidence and the correlation with clinical outcomes and fusion rate, including age >60 years, osteoporosis, use of 12-mm PEEK cage height, and multifidus muscle fatty degeneration. In this study, the radiographic subsidence rates following OLIF were 46.7% of the patients (50/107) and 41.6% of the patients (57/137), which were higher than those reported in previous studies, which reported rates of approximately 11%–27%.5,7-11 Malham et al. reported a 10% (13/128) subsidence rate after OLIF and an incidence of 8% (14 of 178 levels) in only 3% of symptomatic patients. 8 Le et al. reported a 14.3% subsidence rate (20/140) in 8.8% of levels, with symptomatic subsidence observed in 15%. 7 The relatively higher subsidence rate in this study was possible due to a low threshold for defining the subsidence that included any level with any amount of endplate violation as identified by thin-slice CT scan in either sagittal or coronal views at 200% magnification. Most of the subsidence was also classified as the involvement of the contralateral caudal (Type 1) or cranial endplate (Type 2), which were considered as minor subsidence. 8 In the current study, the fusion rate at 1 year and the time-to-fusion in both groups were not found to be related to cage subsidence. Both groups had a reliably high fusion rate, which is consistent with previous studies.5,12 However, delayed union or pseudarthrosis may be expected if the subsidence grading was more severe than that of the participants in this study. 13
We analyzed patient-related factors, preoperative radiographic parameters, and age-related variables associated with cage subsidence. Our results showed that patients aged 60 years and older were at significantly higher risk of subsidence, similar to a study by Campbell et al 14 Bone and muscle mass tends to decrease with the aging process. As with previous studies, we found that patients with osteoporosis were more likely to develop cage subsidence due to a negative effect on bone microstructure.15-17 Palepu et al. reported a biomechanical analysis of cage subsidence and found that trabecular bone quality was highly correlated with subsidence force, regardless of cage type. 17 Xi et al. also reported that low Hounsfield units (HU) of the vertebral body on CT scan, which indicate a low BMD, may contribute to subsidence. The authors recommended measuring lumbar HU in the preoperative CT prior to LLIF surgery. 16 The use of alendronate was also suggested postoperatively in patients undergoing L4-5 LLIF to reduce the subsidence rate. 18
According to the multivariate analysis, the use of a 12-mm PEEK cage height was shown to increase the risk of subsidence, compared to an 8-mm and 10-mm height. Previous studies have also reported an association between cage subsidence and instrument-related factors. However, studies regarding cage height and its effect on subsidence following OLIF are lacking. Kaliya-Perumal et al. reported that over-corrected postoperative disc height was correlated with subsequent disc height loss during early follow-up. 19 Accordingly, the study of subsidence following standalone anterior cervical discectomy and fusion cage by Igarashi et al. also reported a higher risk of cage subsidence when using greater cage height. 20 Thus, we strongly recommend an optimal cage height of less than 12 mm to avoid excessive mechanical stress on the vertebral endplate. Additionally, previous studies also recommended the use of wider cages to adequately occupy the endplate peripheries and achieve more bone–cage–bone interfaces to reduce the risk of subsidence.7,21
In this study, multifidus muscle degeneration (either a decrease in muscle volume or a higher degree of muscle fatty degeneration) was also identified as a risk factor leading to subsidence in OLIF. The multifidus muscle is a paraspinal muscle that acts as a posterior tension band structure and provides support for the lumbar spine and intervertebral discs. It is also involved in the axial compressive force transmission. 6 When muscle degeneration occurs, the anterior column of the spine, including the OLIF cage construct, absorbs higher compressive forces and is more likely to develop endplate violation and subsequent cage subsidence. 22 Therefore, the paraspinal muscles should be protected from iatrogenic injury during surgery, and core back muscle strengthening should be encouraged in all patients.
Unlike some published studies, other factors, such as materials or supplementary fixation, were not included in our study. A standalone OLIF cage may increase the risk of subsidence. Jones et al. reported that standalone OLIF, especially when combined with osteoporosis, was significantly associated with subsidence by a 2.5-fold increased risk. 23 In our study, subsidence was categorized based on location and severity. Amini et al also reported a severe subsidence rate of 18.5% when using a standalone interbody PEEK cage. They proposed using titanium cages, which showed significantly less subsidence. 24 Surgical techniques are another important consideration. Satake et al. reported that intraoperative endplate injury increased the risk of subsidence and surgeons should be cautious, especially in patients with osteoporosis or degenerative scoliosis due to unparallel endplate orientation. 13 Likewise, in our study, the most common subsidence type involved bilateral cage subsidence into the anterior aspect of the caudal endplate, producing an anterior tilt of the cage. To protect patients from subsidence after OLIF, surgeons should avoid damage to the caudal endplate during cage insertion. If subsidence is detected intraoperatively, we strongly recommend adding the supplementary posterior fixation to prevent the progression of subsidence and facilitate fusion. However, in this study, the posterior fixation was performed in all participants with or without intraoperative evidence of endplate injury or cage subsidence. We used the “contrast filling technique” to ensure that there was no intraoperative destruction of the endplates, which could lead to an early or immediate postoperative subsidence. We filled the space with a radiocontrast medium and evaluated the endplate injury using intraoperative fluoroscopy. This technique also enabled surgeons to confirm adequate intervertebral disc removal before inserting an interbody PEEK cage.
The clinical correlation between subsidence and clinical outcomes primarily depends on the severity of the subsidence. A greater depth of endplate violation and cage settling directly causes more foraminal height loss and less indirect decompression effect, leading to indirect decompression failure. 7 The cage subsidence found in our study was considered minor because interbody fusion rates and clinical outcomes were not affected by radiographic subsidence and, more importantly, further surgical intervention was not needed. The main symptom of subsidence is usually a new episode of abrupt back pain after surgery, which resolves within 2 weeks. These findings are consistent with those of previous studies.13,25 However, symptomatic subsidence could become more pronounced in cases with severe subsidence without any posterior supplementary fixation, thereby protecting the indirect decompression effect. 7 Our study did not find any significant difference in clinical outcomes between the groups.
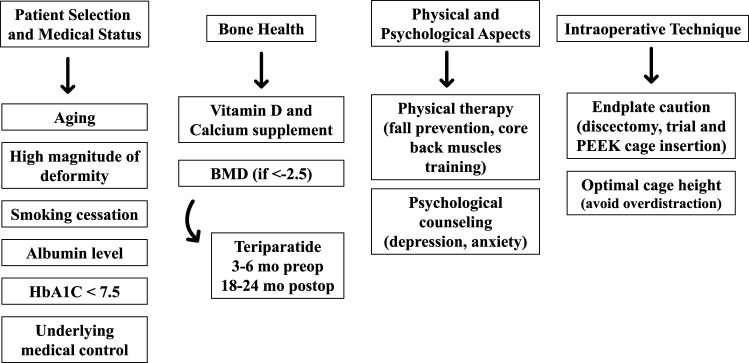
Combining our data with previously published studies, we propose a strategy to avoid cage subsidence and optimize outcomes following OLIF. Since the causes of subsidence are multifactorial, surgeons should pay attention to every aspect to optimize the outcome, including careful patient selection, improvement of bone health, consideration of physical and psychological aspects, and meticulous intraoperative technique, as illustrated in Figure 4.
Figure 4.
A proposed algorithm for optimization in oblique lateral interbody fusion surgery aiming to minimize the cage subsidence.
The strength of this study included a novelty to report on the risk factors for subsidence of PEEK cages after OLIF for lumbar degenerative conditions with a very low threshold for defining subsidence as identified by thin-slice CT scan. The outcome assessment focused on health-related quality of life instruments such as ODI, VAS scores, and not just radiographic parameters.
This study had several limitations. The retrospective design is subject to certain biases and lack of consistency in the follow-up time of patients, which affected the variations in time-to-subsidence and time-to-fusion. Some important factors were not included in this study, such as comorbidities, cage width and length, and use of different cage designs. However, adequate cage length that seated on the bilateral apophyseal ring was confirmed in fluoroscopic images in all participants intraoperatively. Small intraoperative vertebral endplate defects may not be picked up by the contrast filling technique. Clinical manifestations of subsidence may have been underestimated due to the relatively small degree of subsidence and the limited follow-up period. We believe that subsidence could significantly reduce the adequacy of nerve decompression, especially in patients undergoing indirect decompression alone. Therefore, further prospective randomized studies with a longer follow-up period are needed.
Conclusion
The risk factors for subsidence in OLIF were age >60 years, BMD < −2.5, higher cage height, and severe multifidus muscle fatty degeneration. The patients who had subsidence had worse early (3 months) postoperative back and leg pain than those without subsidence.
Acknowledgments
The authors would like to thank Miss Eun-Jin Park for her dedication in gathering the data and her support for this study. Also, we would like to thank Miss Chuenrutai Yeekian, PhD, for the statistical consultant and analysis in this study.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: JS Kim is currently a consultant for RIWOSpine, GmbH, Germany and Elliquence, LLC, USA. W Singhatanadgige and W Limthongkul are currently a speaker for Medtronic company. For the remaining authors none were declared.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
IRB approval/Research Ethics Committee: IRB approval was obtained from The Catholic University of Korea, Seoul St.Mary’s Hospital (KC160ISI0392)
Patient consent: Written informed consent was obtained from the patient.
Device Status Statement: The device(s)/drug(s) that is/are the subject of this manuscript is/are FDA-approved for this indication and is/are commercially available in the United States.
ORCID iDs
Vit Kotheeranurak https://orcid.org/0000-0002-9593-429X
Weerasak Singhatanadgige https://orcid.org/0000-0001-7166-1381
Worawat Limthongkul https://orcid.org/0000-0002-0116-8791
References
- 1.Takahashi K, Kitahara H, Yamagata M, et al. Long-term results of anterior interbody fusion for treatment of degenerative spondylolisthesis. Spine (Phila Pa 1976). 1990;15(11):1211-1215. [DOI] [PubMed] [Google Scholar]
- 2.Kepler CK, Sharma AK, Huang RC, et al. Indirect foraminal decompression after lateral transpsoas interbody fusion. J Neurosurg Spine. 2012;16(4):329-333. [DOI] [PubMed] [Google Scholar]
- 3.Fujibayashi S, Hynes RA, Otsuki B, Kimura H, Takemoto M, Matsuda S. Effect of indirect neural decompression through oblique lateral interbody fusion for degenerative lumbar disease. Spine (Phila Pa 1976). 2015;40(3):E175-E182. [DOI] [PubMed] [Google Scholar]
- 4.Abe K, Orita S, Mannoji C, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: Perspectives and indications from a retrospective, Multicenter Survey. Spine (Phila Pa 1976). 2017;42(1):55-62. [DOI] [PubMed] [Google Scholar]
- 5.Jin C, Jaiswal MS, Jeun SS, Ryu KS, Hur JW, Kim JS. Outcomes of oblique lateral interbody fusion for degenerative lumbar disease in patients under or over 65 years of age. J Orthop Surg Res. 2018;13(1):38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kader DF, Wardlaw D, Smith FW. Correlation between the MRI changes in the lumbar multifidus muscles and leg pain. Clin Radiol. 2000;55(2):145-149. [DOI] [PubMed] [Google Scholar]
- 7.Le TV, Baaj AA, Dakwar E, et al. Subsidence of polyetheretherketone intervertebral cages in minimally invasive lateral retroperitoneal transpsoas lumbar interbody fusion. Spine (Phila Pa 1976). 2012;37(14):1268-1273. [DOI] [PubMed] [Google Scholar]
- 8.Malham GM, Parker RM, Blecher CM, Seex KA. Assessment and classification of subsidence after lateral interbody fusion using serial computed tomography. J Neurosurg Spine. 2015;23(5):589-597. [DOI] [PubMed] [Google Scholar]
- 9.Wewel JT, Hartman C, Uribe JS. Timing of lateral lumbar interbody subsidence: Review of exclusive intraoperative subsidence. World Neurosurg. 2020;137:e208-e12. [DOI] [PubMed] [Google Scholar]
- 10.Frisch RF, Luna IY, Brooks DM, Joshua G, O’Brien JR. Clinical and radiographic analysis of expandable versus static lateral lumbar interbody fusion devices with two-year follow-up. J Spine Surg. 2018;4(1):62-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tempel ZJ, McDowell MM, Panczykowski DM, et al. Graft subsidence as a predictor of revision surgery following stand-alone lateral lumbar interbody fusion. J Neurosurg Spine. 2018;28(1):50-56. [DOI] [PubMed] [Google Scholar]
- 12.Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. 2017;17(4):545-553. [DOI] [PubMed] [Google Scholar]
- 13.Satake K, Kanemura T, Nakashima H, Yamaguchi H, Segi N, Ouchida J. Cage subsidence in lateral interbody fusion with transpsoas approach: Intraoperative endplate injury or late-onset settling. Spine Surg Relat Res. 2017;1(4):203-210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Campbell PG, Cavanaugh DA, Nunley P, et al. PEEK versus titanium cages in lateral lumbar interbody fusion: A comparative analysis of subsidence. Neurosurg Focus. 2020;49(3):E10. [DOI] [PubMed] [Google Scholar]
- 15.Tempel ZJ, Gandhoke GS, Okonkwo DO, Kanter AS. Impaired bone mineral density as a predictor of graft subsidence following minimally invasive transpsoas lateral lumbar interbody fusion. Eur Spine J. 2015;24(suppl 3):414-419. [DOI] [PubMed] [Google Scholar]
- 16.Xi Z, Mummaneni PV, Wang M, et al. The association between lower Hounsfield units on computed tomography and cage subsidence after lateral lumbar interbody fusion. Neurosurg Focus. 2020;49(2):E8. [DOI] [PubMed] [Google Scholar]
- 17.Palepu V, Helgeson M, Molyneaux-Francis M, Nagaraja S. The effects of bone microstructure on subsidence risk for Alif, Llif, Plif, and Tlif spine cages. J Biomech Eng. 2018;141(3):031002. [DOI] [PubMed] [Google Scholar]
- 18.Samtani RG, Bernatz JT, Harrison R, Roy S, Gupta S, O’Brien JR. The effect of alendronate on subsidence after lateral transpsoas interbody fusion: A preliminary report. Int J Spine Surg. 2019;13(3):289-295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaliya-Perumal AK, Soh TLT, Tan M, Oh JY. Factors influencing early disc height loss following lateral lumbar interbody fusion. Asian Spine J. 2020;14(5):601-607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Igarashi H, Hoshino M, Omori K, et al. Factors influencing interbody cage subsidence following anterior cervical discectomy and fusion. Clin Spine Surg. 2019;32(7):297-302. [DOI] [PubMed] [Google Scholar]
- 21.Lang G, Navarro-Ramirez R, Gandevia L, et al. Elimination of subsidence with 26-mm-wide cages in extreme lateral interbody fusion. World Neurosurg. 2017;104:644-652. [DOI] [PubMed] [Google Scholar]
- 22.Singhatanadgige W, Sukthuayat A, Tanaviriyachai T, et al. Risk factors for polyetheretherketone cage subsidence following minimally invasive transforaminal lumbar interbody fusion. Acta Neurochir. 2021;163:2557-2565. [DOI] [PubMed] [Google Scholar]
- 23.Jones C, Okano I, Salzmann SN, et al. Endplate volumetric bone mineral density is a predictor for cage subsidence following lateral lumbar interbody fusion: a risk factor analysis. Spine J. 2021;21:1729-1737. [DOI] [PubMed] [Google Scholar]
- 24.Adl Amini D, Okano I, Oezel L, et al. Evaluation of cage subsidence in standalone lateral lumbar interbody fusion: novel 3D-printed titanium versus polyetheretherketone (PEEK) cage. Eur Spine J. 2021;30(8):2377-2384. [DOI] [PubMed] [Google Scholar]
- 25.Chen E, Xu J, Yang S, et al. Cage subsidence and fusion rate in extreme lateral interbody fusion with and without fixation. World Neurosurg. 2019;122:e969-e77. [DOI] [PubMed] [Google Scholar]