Abstract
Purpose
Stem cell therapy is a promising therapeutic approach for inherited retinal diseases (IRDs). This study aims to quantitatively examine the effectiveness and safety of stem cell therapy for patients with IRDs, including retinitis pigmentosa and Stargardt disease (STGD).
Methods
We searched PubMed, EMBASE, Web of Science, Cochrane Library databases, and the ClinicalTrials.gov website. The latest retrieval time was August 20, 2023. The primary outcomes were rates and mean difference (MD) of best-corrected visual acuity (BCVA) improvement. Subgroup analyses were conducted according to administration routes and stem cell types. This study was registered with PROSPERO (CRD42022349271).
Results
Twenty-one prospective studies, involving 496 eyes (404 RP and 92 STGD) of 382 patients (306 RP and 76 STGD), were included in this study. For RP, the rate of BCVA improvement was 49% and 30% at 6 months and 12 months, respectively, and the BCVA was significantly improved in the operative eyes at 6 months post-treatment (MD = − 0.12 logMAR, 95% CI .17 to − 0.06 logMAR; P < 0.001), while there was no significant difference at 12 months post-treatment (MD = -0.06 logMAR; 95% CI − 0.13 to 0.01 logMAR; P = 0.10). For STGD, the rate of BCVA improvement was 60% and 55% at 6 months and 12 months, respectively, and the BCVA was significantly improved in the operative eyes at 6 months (MD = − 0.14 logMAR, 95% CI − 0.22 to − 0.07 logMAR; P = 0.0002) and 12 months (MD = − 0.17 logMAR, 95% CI − 0.29 to − 0.04 logMAR; P = 0.01). Subgroup analyses showed suprachoroidal space injection of stem cells may be more efficient for RP. Eleven treated-related ocular adverse events from three studies and no related systemic adverse events were reported.
Conclusions
This study suggests stem cell therapy may be effective and safe for patients with RP or STGD. The long-term vision improvement may be limited for RP patients. Suprachoroidal space injection of stem cells may be a promising administration route for RP patients. Limited by the low grade of evidence, large sample size randomized clinical trials are required in the future.
Keywords: Stem cell, Inherited retinal diseases (IRD), Retinitis pigmentosa (RP), Stargardt disease (STGD), Meta-analysis
Introduction
Inherited retinal diseases (IRDs) are a group of complex and heterogeneous diseases that are mainly characterized by progressive photoreceptors (PRs) and/or loss of retinal pigment epithelium (RPE) cells, eventually leading to irreversible vision loss [1]. It is estimated that approximately 1 in 2000 to 4000 people are affected by IRDs [2, 3]. IRDs such as retinitis pigmentosa (RP) and Stargardt disease (STGD) have become the most common cause of blindness in the working-age population (16–64 years) in some Western countries [4, 5], which would impair the life quality of patients [6, 7], and cause severe social economic burden [8, 9]. In the past, only genetic testing and low-vision rehabilitation were used for the management of IRDs and these could not effectively slow or stop vision loss of patients with IRDs. However, recent emerging treatments including gene therapy, stem cell therapy, and retinal prosthesis have entered the stage of clinical trials and some therapies have shown inspiring therapeutic benefits in these vision-threatening disorders [10].
Among these treatment approaches for IRDs, stem cell therapy is considered a potential therapeutic method, which aims to replace lost cells in the retina with stem cells, mainly for those patients with IRDs who remained some useful retinal ganglion cells. Several types of stem cells, including retinal progenitor cells (RPCs), mesenchymal stem cells (MSCs), human embryonic stem cells-derived RPE (hESCs-RPE) cells, and induced pluripotent stem cells-derived RPE (iPSCs-RPE) cells, have been examined their efficacy or safety for IRDs patients in clinical trials [11].
Despite some results with small sample sizes from reviewed trials showing effectiveness and safety, no studies have been empowered to prove statistically significant efficacy for humans, and no stem cell therapy is approved for patients with IRDs [12]. The long-term efficacy and safety are controversial and required to be determined [13–17]. In addition, some parameters of stem cell therapy for IRDs, such as administration routes and types of transplanted stem cells, are needed to optimize [18]. To date, no systematic review or meta-analysis has quantitatively examined the effectiveness of vision improvement and adverse events of stem cell therapy for patients with IRDs. Therefore, this study aims to quantitatively assess these outcomes of stem cell therapy for patients with IRDs including RP and STGD and perform subgroup analyses stratified by administration routes and stem cell types in RP.
Methods
The protocol of this study was registered at PROSPERO (CRD42022349271, [http://www.crd.york.ac.uk/PROSPERO/]). This meta-analysis was performed according to the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020 statement) [19].
Search strategy
We searched the PubMed, EMBASE, Web of Science, and Cochrane Library databases. We also screened the references from retrieved papers and the ClinicalTrials.gov website to identify additional related clinical studies and unpublished studies with available data. The following literature search terms were used (“Stem cell” OR “stem cells” OR “progenitor cell” OR “bone marrow”) AND (“Inherited retinal diseases” OR “inherited retinal degeneration” OR “hereditary retinal diseases” OR “inherited retinal dystrophy” OR “retinitis pigmentosa” OR “Stargardt disease” OR “Stargardt macular dystrophy”). Neither the article language nor the retrieval time was limited. The latest retrieval time was August 20, 2023.
Inclusion and exclusion criteria
The inclusion criteria were as follows:
Patients who are diagnosed with IRDs, including RP and STGD.
Patients who have undergone stem cell therapy.
Any clinical trials.
The exclusion criteria were as follows:
Patients with other ocular disease except RP or STGD.
Preclinical studies, letters to the editor, editorials, case reports, conference abstracts, and reviews.
Studies without the assessment of primary outcome.
Data extraction
Two researchers independently screened titles and abstracts according to the eligible criteria. All discrepancies were resolved through adjudication by a third researcher. Extracted information included author name, publication year, country, study design, number of participants, number of treated eyes, follow-up time, age, gender, diagnosis, stem cells, administration routes, and cell concentration. For studies that reported similar results, only the most complete publication was included. The improvement of best-corrected visual acuity (BCVA) and ocular and systemic adverse events related to stem cell therapy were examined. The primary outcomes were the rate and mean difference (MD) of improvement of BCVA measured in the logarithm of the Minimum Angle of Resolution (logMAR).
Quality assessment
The Newcastle–Ottawa Quality Assessment Scale (NOS) was used to assess the risk of bias in each cohort study [20]. Two researchers independently evaluate the quality of studies. All discrepancies were resolved through adjudication by a third researcher.
Statistical analysis
Meta-analyses were conducted using the Review Manager (version 5.3; Cochrane Collaboration) and Stata SE (version 15.1). Visual acuity values were recorded as Snellen or logMAR, and Snellen values were converted to logMAR for analyses. LogMAR values corresponding to count fingers (CF), hand movements (HM), and light perception (PL) were substituted with 2.0, 3.0, and 4.0 logMAR, respectively, in accordance with the previous study [21]. Besides, no light perception (NLP) was substituted with 5.0. Snellen values provided in studies were converted to logMAR equivalents [22]. For studies provided The Early Treatment Diabetic Retinopathy Study (ETDRS) letter scores, we converted them to logMAR equivalents using the following formula logMAR = 1.7–(0.02) * (ETDRS letter scores) [23]. The mean difference (MD) and 95% confidential interval (CI) were used to calculate. A fixed-effects model was used to assess the pool effect of changed logMAR, when no significant heterogeneity was detected (I2 ≤ 50% or P-value for heterogeneity ≥ 0.1). Otherwise, a random-effects model was used (I2 > 50% or p-value for heterogeneity < 0.1). Subgroup analyses were performed stratified by types of stem cells and administration routes. The publication bias was detected using funnel plots and Begg’s test. The statistical significance was set at P < 0.05.
Results
Literature search
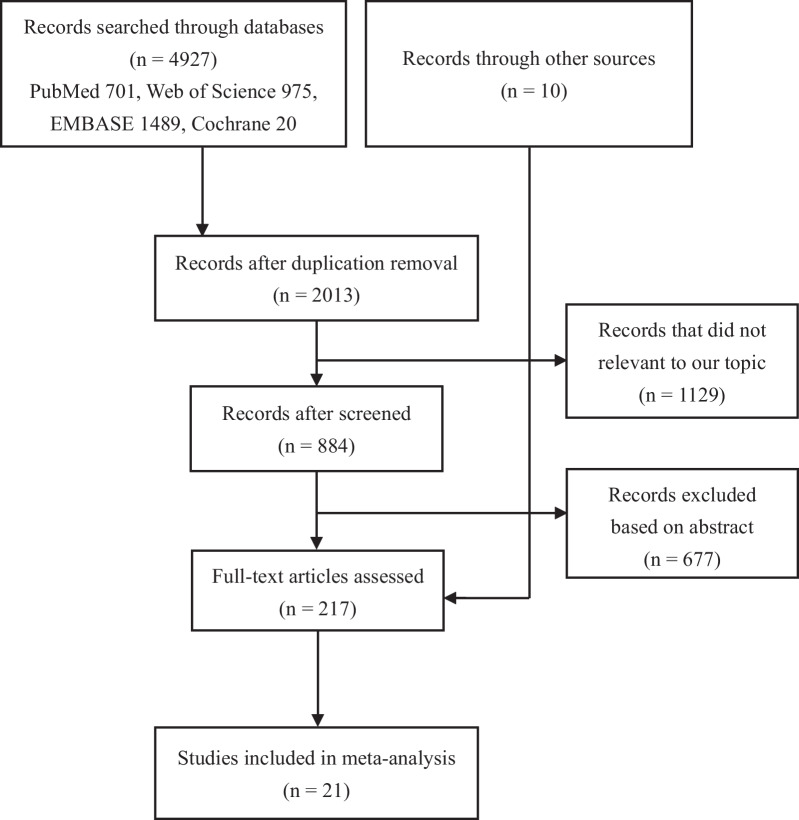
The initial retrieval identified 2013 nonduplicated articles. Records that were not relevant to our topic were excluded (n = 1129). After screening titles and abstracts, studies were excluded according to inclusion criteria (n = 677). Full-text evaluation was performed in the remaining 217 studies. Ultimately, 21 unique studies were included in this meta-analysis (Fig. 1).
Fig. 1.
The selection process of included studies
Characteristics of included studies
Twenty-one prospective studies, involving 496 eyes (404 RP and 92 STGD) of 382 patients (306 RP and 76 STGD), were included in this study [14, 15, 24–42]. One study included RP and STGD patients [25]. Eight studies were for STGD [26, 28, 29, 36–38, 40, 42], and twelve studies were for RP [14, 15, 24, 27, 30–35, 39, 41], of which one study involved pediatric patients [41]. The mean follow-up duration was 14.4 ± 12.8 months (RP: 10.5 ± 5.0 months; STGD: 19.1 ± 18.1 months), ranging from 6 to 60 months (5 years). Detailed characteristics of the included studies are presented in Table 1.
Table 1.
Study characteristics
| References | Study design | Country | Patients | Female (%) | eyes | Age | Diagnosis | Stem cells | Administration routes | Follow-up | Quality scores |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Siqueira et al., [24] | Nonrandomized PCT | Brazil | 5 | 2 [40] | 5 |
Mean (SD) [range] 31.4 (5.0) [23–35] |
RP or cone-rod dystrophy | BM with CD34 + SCs | Intravitreal | 10 | 6 |
| Park et al., [25] | PCT | USA | 6 | 2 (33.3) | 6 |
Mean (SD) [range] 48.3 (25.7) [23–85] |
Advanced RP or STGD or AMD or CRAO | BM with CD34 + SCs | Intravitreal | 6 | 6 |
| Schwartz et al., [26] | PCT | USA | 18 | 5 (27.8) | 18 |
Median (IQR) STGD: 50 (20–71) AMD: 77 (70–88) |
STGD or AMD | hESC-RPE (MA09) | Subretinal | 22 | 8 |
| Liu et al., [37] | PCT | China | 8 | 5 (62.5) | 8 |
Mean (SD) [range] 35.5 (12.1) [19–53] |
Advanced RP | RPCs | Subretinal | 24 | 8 |
| Weiss et al., [38] | Nonrandomized PCT | USA | 17 | 7 (41.2) | 33 |
Mean (SD) [range] 48.8 (13.9) [28–70] |
RP | BMSCs | SCOT combination | 6 | 7 |
| Oner et al., [41] | PCT | Turkey | 8 | 3 (37.5) | 8 |
Mean (SD) [range] 44.8 (23.6) [19–75] |
STGD or AMD | ADMSCs | Suprachoroidal | 6 | 6 |
| Mehat et al., [29] | PCT | UK | 12 | 1 (8.3) | 12 |
Mean (SD) [range] 45.3 (5.3) [34–53] |
STGD | hESC-RPE | Subretinal | 12 | 8 |
| Oner et al., [30] | PCT | Turkey | 14 | 5 (35.7) | 14 |
Mean (SD) [range] 39.1 (8.9) [26–57] |
Severe RP | ADMSCs | Subretinal | 12 | 7 |
| Özmert and Arslan, [31] | PCT | Turkey | 32 | 14 (43.8) | 34 |
Median [range] 38.7 [18–58] |
RP | WJMSCs | Subtenon | 6 | 6 |
| Kahraman and Oner, [32] | PCT | Turkey | 82 | 32 (39.0) | 124 |
Median (IQR) 38.5 (34.0–46.0) |
RP | UCMSCs | Suprachoroidal | 6 | 5 |
| Limoli et al., [33] | PCT | Italy | 25 | 11 (44.0) | 34 |
Mean (SD) [range] 45.9 (18.4) (19–86) |
RP | ADMSCs | Suprachoroidal | 6 | 7 |
| Zhao et al., [34] | PCT | China | 32 | 20 (62.5) | 64 |
Mean (SD) [range] 36 (2.5) [16–61] |
Advanced RP | UCMSCs | Intravenous | 12 | 6 |
| Tuekprakhon et al., [15] | Nonrandomized PCT | Thailand | 14 | 5 (35.7) | 14 |
Mean (SD) [range] 46.2 (9.3) [32–61] |
Advanced RP | BMSCs | Intravitreal | 12 | 7 |
| Wiącek et al., [35] | Nonrandomized PCT | Poland | 30 | 18 (60.0) | 30 |
Mean (SD) [range] 41.7 (12.8) [19–64] |
RP | BM-derived Lineage-negative cells | Intravitreal | 12 | 6 |
| Sung et al., [36] | Nonrandomized PCT | Korea | 3 | 0 (0.0) | 3 |
Mean (SD) [range] 41.7 (2.89) [40–45] |
STGD | hESC-RPE (MA09) | Subretinal | 36 | 7 |
| Li et al., [37] | PCT | China | 7 | 5 (71.4) | 7 |
Mean (SD) [range] 23.3 (3.6) [19–27] |
STGD | hESC-RPE | Subretinal | 60 | 8 |
| Weiss et al., [38] | PCT | USA | 17 | 5 (29.4) | 34 |
Mean (SD) [range] 48.2 (16.1) [26–72] |
STGD | BMSCs | SCOT combination | 12 | 8 |
| Khairullah et al., [39] | PCT | Malaysia | 2 | 1 (50.0) | 4 |
Mean (SD) [range] 61.0 (5.7) [57–65] |
Advanced RP | WJMSCs | Subtenon | 12 | 4 |
| Fernandes et al., [40] | PCT | Brazil | 12 | 9 (75.0) | 12 |
Mean (SD) [range] 41.5 (7.1) [30–53] |
STGD | hESC-RPE | Subretinal | 12 | 8 |
| Oner et al., [41] | PCT | Turkey | 46 | 18 (39.0) | 46 |
Median (IQR) 13.4 (9.0–17.0) |
RP | UCMSCs | Suprachoroidal | 12 | 6 |
| Cotrim et al, [42] | Nonrandomized PCT | Brazil | 10 | 6 (60.0) | 10 |
Mean (SD) [range] 33.0 (8.6) [23–48] |
STGD | BMMF with CD34 + SCs | Intravitreal | 6 | 7 |
PCT Prospective clinical trial, IQR Interquartile range, CRAO Central Retinal Artery Occlusion, RP Retinitis pigmentosa, STGD Stargardt disease, AMD Age-related macular degeneration, RPCs Retinal progenitor cells, BMSCs Bone marrow-derived mesenchymal stem cells, ADMSC Adipose tissue-derived mesenchymal stem cells, UCMSCs Umbilical cord mesenchymal stem cells, hESC-RPE Human embryonic stem cell-derived retinal pigment epithelium, SCOT combination The Stem Cell Ophthalmology Treatment Study, BMMF Bone Marrow Mononuclear Fraction, SCOT used various administration routes to treat
The rate of best-corrected vison acuity improvement after stem cell therapy
For RP, 49% and 30% operative eyes achieved better BCVA at 6 months and 12 months post-treatment, respectively. For STGD, 60% and 55% operative eyes achieved better BCVA at 6 months and 12 months post-treatment, respectively (Table 2).
Table 2.
The rate of the best-corrected visual acuity improvement after stem cell therapy at 6 months and 12 months
| References | Improved operative eyes at 6 months | Total operative eyes at 6 months | Improved operative eyes at 12 months | Total operative eyes at 12 months |
|---|---|---|---|---|
| RP | ||||
| Siqueira et al., [24] | 3 | 3 | NA | NA |
| Park et al., [25] | 1 | 1 | NA | NA |
| Liu et al., [26] | 5 | 8 | 3 | 8 |
| Weiss et al., [27] | 15 | 33 | NA | NA |
| Oner et al., [28] | 3 | 11 | NA | NA |
| Özmert and Arslan, [31] | 32 | 34 | NA | NA |
| Limoli et al., [33] | 25 | 34 | NA | NA |
| Kahraman and Oner, [41] | 57 | 124 | NA | NA |
| Wiącek et al., [35] | 16 | 30 | 17 | 30 |
| Zhao et al., [34] | 12 | 64 | 11 | 64 |
| Khairullah et al., [39] | 0 | 2 | 0 | 2 |
| Total | 169 | 344 | 31 | 104 |
| Rate | 49% | 30% | ||
| STGD | ||||
| Park et al., 2015 | 2 | 2 | NA | NA |
| Cotrim et al., [42] | 8 | 10 | NA | NA |
| Fernandes et al., [40] | 10 | 12 | 10 | 12 |
| Li et al., [37] | 2 | 7 | 1 | 6 |
| Mehat et al., [29] | 4 | 12 | 5 | 12 |
| Oner et al., [28] | 4 | 4 | NA | NA |
| Schwartz et al., [26] | 3 | 8 | 3 | 7 |
| Sung et al., [36] | 2 | 3 | 3 | 3 |
| Total | 35 | 58 | 22 | 40 |
| Rate | 60% | 55% | ||
NA Not available; RP Retinitis pigmentosa; STGD Stargardt disease
Improvement in best-corrected visual acuity after stem cell therapy
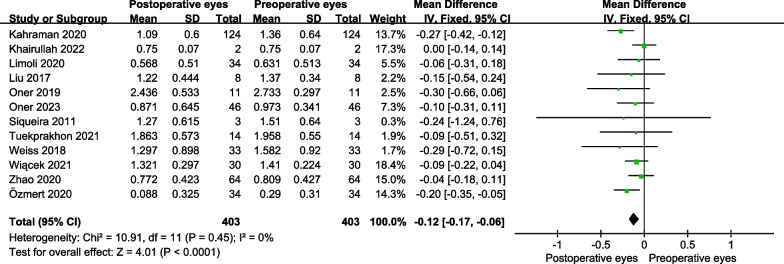
For RP, the BCVA was significantly improved in the operative eyes at 6 months post-treatment (MD = − 0.12 logMAR, 95% CI − 0.17 to − 0.06 logMAR; P < 0.001) (Fig. 2), while there was no significant difference at 12 months post-treatment (MD = 0.06 logMAR; 95% CI − 0.13 to 0.01 logMAR; P = 0.10) (Fig. 3).
Fig. 2.
The forest plot showed the best-corrected visual acuity improvement for patients with RP at 6 months
Fig. 3.
The forest plot showed the best-corrected visual acuity improvement for patients with RP at 12 months
For STGD, the BCVA was significantly improved in the operative eyes at 6 months post-treatment (MD = − 0.14 logMAR, 95% CI − 0.22 to − 0.07 logMAR; P = 0.0002) (Fig. 4) and 12 months (MD = − 0.17 logMAR, 95% CI − 0.29 to − 0.04 logMAR; P = 0.01) (Fig. 5).
Fig. 4.
The forest plot showed the best-corrected visual acuity improvement for patients with STGD at 6 months
Fig. 5.
The forest plot showed the best-corrected visual acuity improvement for patients with STGD at 12 months
Subgroup analyses
For improvement in BCVA of RP patients at 6 months post-treatment, we performed subgroup analyses according to the administration routes and types of stem cells. For administration routes, suprachoroidal space injection showed the best BCVA improvement at 6 months post-treatment (MD = − 0.18 logMAR, 95% CI − 0.29 to − 0.07 logMAR; P = 0.001) (Fig. 6). For types of stem cells, umbilical cord MSCs (UCMSCs) injection showed the best BCVA improvement at 6 months post-treatment (MD = − 0.14 logMAR, 95% CI − 0.23 to − 0.04 logMAR; P = 0.004) (Fig. 7).
Fig. 6.
Subgroup analyses showed different administration routes on the best-corrected visual acuity improvement for RP at 6 months
Fig. 7.
Subgroup analyses showed different stem cell types on the best-corrected visual acuity improvement for RP at 6 months
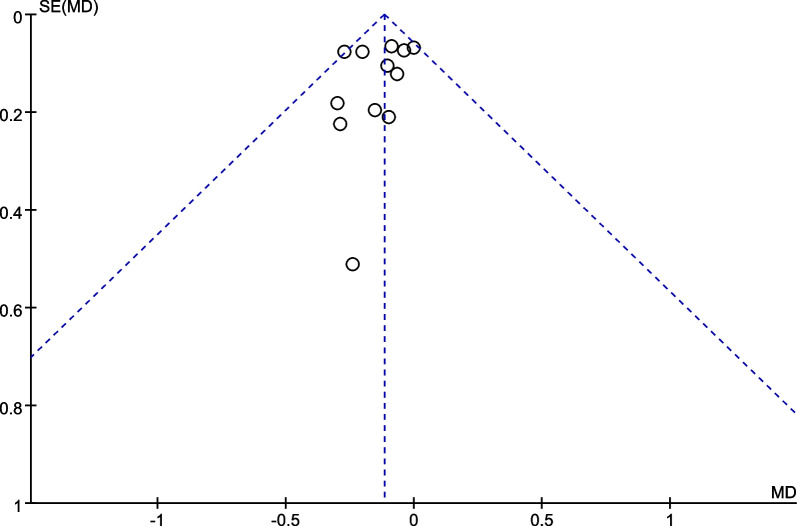
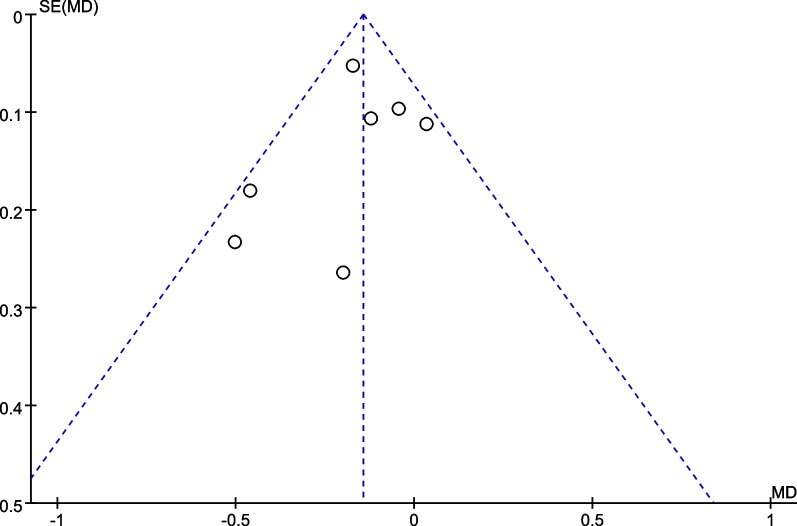
Publication bias
The funnel plots demonstrated the improvement in BCVA at 6 months after stem cell therapy for patients with RP (Fig. 8, P for Begg’s test: 0.170) and STGD (Fig. 9, P for Begg’s test: 0.652). No significant publication bias was detected.
Fig. 8.
The funnel plot for the best-corrected visual acuity improvement for patients with RP at 6 months
Fig. 9.
The funnel plot for the best-corrected visual acuity improvement for patients with STGD at 6 months
Systemic and ocular adverse events
Eleven treated-related ocular adverse events from three studies and no related systemic adverse events were reported for RP patients [15, 30, 35]. One study reported three tractional retinal detachments (RD) [35]. One study with long-term follow-up reported a case that experienced diffuse vitreous hemorrhage and osseous metaplasia in the ciliary body in the third year of follow-up and a case that developed minimal intraocular lens subluxation in the fourth year of follow-up [15]. Another study reported a case that developed choroidal neovascular membrane (CNM) and five cases had epiretinal membrane (ERM) with peripheral tractional RD [30].
Discussion
Our study was in line with previous systemic reviews which confirmed stem cell therapy was an effective and relatively safe treatment for patients with RP or STGD [16, 43, 44]. This present study, including 21 studies and 496 eyes, was the first to quantitatively assess the improvement of BCVA in patients with RP or STGD who had undergone stem cell therapy. The change of logMAR of STGD patients was significantly improved at 6 and 12 months. However, although the BCVA of RP patients was significantly improved at 6 months, this improvement was no longer significant at 12 months. A study that used RPC cells to treat RP patients showed that vision improvement did not appear at 24 months after stem cell therapy [14]. In addition, another study used hESC-RPE cells to treat STGD patients showed worse BCVA at 60 months after stem cell therapy [37]. The incidence of adverse events after stem cell therapy was low, and most of them were mild ocular adverse events, but the safety of stem cell therapy for patients with RP or STGD requires attention. One study reported the first five cases developed peripheral tractional RD and one case happened CNM [30]. They considered these complications may be attributed to inadvertent preretinal injection of stem cells or reflux of transplanted stem cells from the subretinal space [45]. After modifying the surgical operation, the remaining patients did not have adverse events. Our results showed suprachoroidal space injection showed optimally improved logMAR at 6 months with no serious ocular or systemic adverse events reported, indicating this may be a better administration route of stem cell therapy for RP patients. The standardized surgical procedures were important to the safety of stem cell therapy. These findings suggest that stem cell transplantation is efficient and relatively safe for patients with RP or STGD, but long-term efficacy is uncertain for RP. Weiss et al. indicated that the efficacy of stem cell therapy would be affected by the severity of RP [27]. Meanwhile, the patients with longer disease duration gained less vision improvement, compared to those with shorter duration of RP [35]. In the meta-analysis showing the efficacy of stem cell therapy for RP at 12 months, five in seven studies were advanced RP. Marginally significant improvement was observed in the remaining two studies at 12 months (data not shown) [35, 41].
Stem cells have a strong ability to proliferate and differentiate into many kinds of cells, including RPE cells, PRs, and RGCs. The transplanted stem cells function mainly by secreting neurotrophic factors, replacing the degenerative cells in the host, upregulating anti-apoptotic genes, and forming new functional synapses [46]. In 2016, researchers proposed a new potential mechanism that host and grafted cells could happen material transfer to rescue the host degenerative retina [47], and this mechanism was further verified by subsequent studies [48, 49]. Despite the inspiring results in clinical trials, the exact mechanisms underlying stem cell therapy for IRDs are necessary to explore.
Currently, three common methods are applied to deliver stem cells into the eye: intravitreal injection, subretinal injection, and suprachoroidal injection. Intravitreal injection is a relatively simple and safe procedure, and this method is widely used for treating retinal diseases [50]. However, an intact blood-retinal barrier limited the transport of transplanted stem cells and stem cell-secreted neurotrophic factors [51]. Another serious problem is that the drug can diffuse to nontarget regions such as lens and subretinal space and then trigger fibrous tissue proliferation and lead to RD and ERM [17, 52]. Although some clinical studies have reported the general safety of stem cell therapy for RP patients, this method should be taken into rigorous consideration before being used [15, 35]. Subretinal injection aims to deliver stem cells to the potential space between RPE and PR, which can directly target the retina. Although this method involves a pars plana vitrectomy which may lead RD and vitrectomy-associated complications, the successful use of hESC-RPE in subretinal space has shown its relative safety when carefully using the right techniques [53]. The suprachoroidal space (SCS) is a potential space, between the choroid and sclera. SCS injection is a novel administration route to the posterior segment, which accurately targets the choroid, RPE, and neuroretina, with high bioavailability [54]. Limoli et al. first described the suprachoroidal implantation method of stem cells (they called it the Limoli Retinal Restoration Technique, LRRT) [55–57]. This method allows stem cell-produced growth factors to enter the choroidal blood flow. In this study, the exact mechanism underlying the better efficacy of SCS injection is not clear. One possible explanation is that no ocular adverse events, such as RD and ERM which can impair vision, were reported for the safe SCS injection, compared to intravitreal and subretinal injection. In addition, the accumulation and distribution of drug in the SCS can achieve sustained release [58], which may allow stem cell-derived growth factors to be constantly secreted to the choroid and retina. For those patients who need to inject cell suspension multiply, less invasive SCS inject may be a suitable administration route. For the emerging transplantation of stem cells sheet with the technique of tissue engineering for IRDs, subretinal injection is still the first choice [59].
In this present study, most RP patients were injected with MSCs. MSCs represent the most frequently studied type of adult stem cells, which are derived from stromal progenitor cells of mesodermal origin [60]. MSCs are found in various parts of the human body, and bone MSCs (BMSCs), adipose tissue-derived MSCs (ADMSCs), and UCMSCs are the three main MSCs used to research IRDs, and they have similar function properties [61, 62]. Several important properties of MSCs include immunomodulation, anti-inflammation, and secretion of neurotrophic factors [60]. Compared to other stem cells, easier isolation from tissues makes MSCs a promising candidate for IRDs. Besides, MSC-derived extracellular vesicles are considered beneficial to retinitis pigmentosa [63]. Our results showed that UCMSCs may be a potential MSCs type for patients with RP. Currently, clinical trials are focused on the transplantation of hESCs-RPE or iPSCs-RPE to treat retinal degeneration [18]. Both ESCs and iPSCs can be successfully differentiated into PRs, RPE cells, and other retinal cells and are seemed a promising way to treat IRDs [64]. In 2012, Schwartz et al. first reported the preliminary results using hESC-RPE to treat two retinal diseases including age-related macular degeneration (AMD) and STGD [65]. Subsequently, a plethora of clinical trials showed inspiring results of hESC for treating RP [11] and STGD [44]. However, ethical concerns limit the use of hESCs; thus, iPSCs are considered a potential alternative to avoid the above problems. In 2006, Takahashi and Yamanaka first discovered iPSCs, which can be derived from embryonic or adult fibroblasts in mouse by introducing four transcription factors [66]. Then, they described this type of stem cells can be obtained from human skin fibroblasts and peripheral blood in 2007 [67]. Like hESCs, iPSCs were soon reported to be able to differentiate into retinal cells in vitro in 2009 [68]. In 2011, milestone study investigated a self-organized 3D optic cup and stratified RPE from mouse iPSCs, creating the research field of retinal organoids [69]. In 2012, Li et al. reported a method to obtain and transplant iPSC-RPE cells into RP mouse model, which was considered a pioneering study on the use of iPSC in the field of retinal diseases [70]. In 2014, RIKEN reported the first clinical trial using autologous iPSCs-RPE to treat a patient with AMD; the vision of this patient was not improved or worsened [71]. Then the first clinical trial using iPSC-retina which was prepared from retinal organoids to treat advanced RP was started by Kobe City Eye Hospital in 2020 [72]. Despite some challenges, scientific researchers spare no effort to pave the way for the practical application of stem cell therapy for patients suffering from retinal degeneration [59, 73].
Some limitations exist in this study. First, we did not evaluate the data from fundus autofluorescence, electroretinogram, and optical coherence tomography, because the sample size was small or these data could not be extracted and synthesized for meta-analysis. Second, subgroup analyses were only performed in RP patients at 6 months after stem cell therapy. Besides, the number of studies in each subgroup was small in subgroup analyses. Third, the definition of serious ocular events differs and lacks standardized criteria.
Conclusions
This study suggests stem cell therapy may be effective and safe for patients with RP or STGD. The long-term vision improvement may be limited for RP patients. Suprachoroidal space injection of stem cells may be a promising administration route for RP patients. Limited by the grade of evidence, large sample sizes and well-designed multi-center randomized controlled trials with long follow-up periods are required in the future.
Acknowledgements
Not applicable.
Author contributions
XC, NX, JL, MZ, and LH designed this study. XC, NX, and JL screened the literature and collected data. XC performed the analysis and drafted the manuscript. LH and MZ supervised this study. All authors read and approved the final manuscript.
Funding
This work was supported by the Beijing-Tianjin-Hebei Special Project (Grant Number J200014), Science and Technology Innovation Project of Chinese Academy of Medical Sciences (2019-RC-HL-019), National Key RD Program of China (2020YFC2008200), and the National Natural Science Foundation of China (Grant Number 81670870). The sponsor or funding organization had no role in the design or conduct of this research.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Georgiou M, Fujinami K, Michaelides M. Inherited retinal diseases: therapeutics, clinical trials and end points-a review. Clin Exp Ophthalmol. 2021;49(3):270–288. doi: 10.1111/ceo.13917. [DOI] [PubMed] [Google Scholar]
- 2.Pontikos N, Arno G, Jurkute N, Schiff E, Ba-Abbad R, Malka S, et al. Genetic basis of inherited retinal disease in a molecularly characterized cohort of more than 3000 families from the United Kingdom. Ophthalmology. 2020;127(10):1384–1394. doi: 10.1016/j.ophtha.2020.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Stone EM, Andorf JL, Whitmore SS, DeLuca AP, Giacalone JC, Streb LM, et al. Clinically focused molecular investigation of 1000 consecutive families with inherited retinal disease. Ophthalmology. 2017;124(9):1314–1331. doi: 10.1016/j.ophtha.2017.04.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heath Jeffery RC, Mukhtar SA, McAllister IL, Morgan WH, Mackey DA, Chen FK. Inherited retinal diseases are the most common cause of blindness in the working-age population in Australia. Ophthalmic Genet. 2021;42(4):431–439. doi: 10.1080/13816810.2021.1913610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liew G, Michaelides M, Bunce C. A comparison of the causes of blindness certifications in England and Wales in working age adults (16–64 years), 1999–2000 with 2009–2010. BMJ Open. 2014;4(2):e004015. doi: 10.1136/bmjopen-2013-004015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yioti G, Stefaniotou M, Ziavrou I, Kotsis K, Hyphantis T. Illness perceptions, psychiatric manifestations, and quality of life in patients with inherited retinal dystrophies. Semin Ophthalmol. 2017;32(4):428–437. doi: 10.3109/08820538.2015.1118136. [DOI] [PubMed] [Google Scholar]
- 7.Kessel L, Kjellberg J, Nissen K, Rasmussen A, la Cour M. Childhood-onset retinal dystrophies reduces life-time income by one third—an individual based socio-economic analysis. Ophthalmic Genet. 2022;43(5):602–608. doi: 10.1080/13816810.2022.2089359. [DOI] [PubMed] [Google Scholar]
- 8.Galvin O, Chi G, Brady L, Hippert C, Del Valle RM, Daly A, et al. The impact of inherited retinal diseases in the republic of Ireland (ROI) and the United Kingdom (UK) from a cost-of-illness perspective. Clin Ophthalmol. 2020;14:707–719. doi: 10.2147/OPTH.S241928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gong J, Cheung S, Fasso-Opie A, Galvin O, Moniz LS, Earle D, et al. The impact of inherited retinal diseases in the United States of America (US) and Canada from a cost-of-illness perspective. Clin Ophthalmol. 2021;15:2855–2866. doi: 10.2147/OPTH.S313719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schneider N, Sundaresan Y, Gopalakrishnan P, Beryozkin A, Hanany M, Levanon EY, et al. Inherited retinal diseases: linking genes, disease-causing variants, and relevant therapeutic modalities. Prog Retin Eye Res. 2022;89:101029. doi: 10.1016/j.preteyeres.2021.101029. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y, Tang Z, Gu P. Stem/progenitor cell-based transplantation for retinal degeneration: a review of clinical trials. Cell Death Dis. 2020;11(9):793. doi: 10.1038/s41419-020-02955-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Terrell D, Comander J. Current stem-cell approaches for the treatment of inherited retinal degenerations. Semin Ophthalmol. 2019;34(4):287–292. doi: 10.1080/08820538.2019.1620808. [DOI] [PubMed] [Google Scholar]
- 13.Rao RC, Dedania VS, Johnson MW. Stem cells for retinal disease: a perspective on the promise and perils. Am J Ophthalmol. 2017;179:32–38. doi: 10.1016/j.ajo.2017.04.007. [DOI] [PubMed] [Google Scholar]
- 14.Liu Y, Chen SJ, Li SY, Qu LH, Meng XH, Wang Y, et al. Long-term safety of human retinal progenitor cell transplantation in retinitis pigmentosa patients. Stem Cell Res Ther. 2017;8(1):209. doi: 10.1186/s13287-017-0661-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tuekprakhon A, Sangkitporn S, Trinavarat A, Pawestri AR, Vamvanij V, Ruangchainikom M, et al. Intravitreal autologous mesenchymal stem cell transplantation: a non-randomized phase I clinical trial in patients with retinitis pigmentosa. Stem Cell Res Ther. 2021;12(1):52. doi: 10.1186/s13287-020-02122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Alcalde I, Sánchez-Fernández C, Martín C, De Pablo N, Jemni-Damer N, Guinea GV, et al. Human stem cell transplantation for retinal degenerative diseases: where are we now? Medicina. 2022;58(1):954. doi: 10.3390/medicina58010102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Satarian L, Nourinia R, Safi S, Kanavi MR, Jarughi N, Daftarian N, et al. Intravitreal injection of bone marrow mesenchymal stem cells in patients with advanced retinitis pigmentosa: a safety study. J Ophthalmic Vis Res. 2017;12(1):58–64. doi: 10.4103/2008-322X.200164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Voisin A, Pénaguin A, Gaillard A, Leveziel N. Stem cell therapy in retinal diseases. Neural Regen Res. 2023;18(7):1478–1485. doi: 10.4103/1673-5374.361537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Page MJ, Moher D, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ. 2021;372:n160. doi: 10.1136/bmj.n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.GA Wells BS, D O'Connell, J Peterson, V Welch, M Losos, P Tugwell. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses [Available from: http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 20 August 2023.
- 21.Le Q, Chauhan T, Yung M, Tseng CH, Deng SX. Outcomes of limbal stem cell transplant: a meta-analysis. JAMA Ophthalmol. 2020;138(6):660–670. doi: 10.1001/jamaophthalmol.2020.1120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997;13(4):388–391. doi: 10.3928/1081-597X-19970701-16. [DOI] [PubMed] [Google Scholar]
- 23.Beck RW, Moke PS, Turpin AH, Ferris FL, 3rd, SanGiovanni JP, Johnson CA, et al. A computerized method of visual acuity testing: adaptation of the early treatment of diabetic retinopathy study testing protocol. Am J Ophthalmol. 2003;135(2):194–205. doi: 10.1016/s0002-9394(02)01825-1. [DOI] [PubMed] [Google Scholar]
- 24.Siqueira RC, Messias A, Voltarelli JC, Scott IU, Jorge R. Intravitreal injection of autologous bone marrow-derived mononuclear cells for hereditary retinal dystrophy: a phase I trial. Retina. 2011;31(6):1207–1214. doi: 10.1097/IAE.0b013e3181f9c242. [DOI] [PubMed] [Google Scholar]
- 25.Park SS, Bauer G, Abedi M, Pontow S, Panorgias A, Jonnal R, et al. Intravitreal autologous bone marrow CD34+ cell therapy for ischemic and degenerative retinal disorders: preliminary phase 1 clinical trial findings. Invest Ophthalmol Vis Sci. 2014;56(1):81–89. doi: 10.1167/iovs.14-15415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt's macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet. 2015;385(9967):509–516. doi: 10.1016/S0140-6736(14)61376-3. [DOI] [PubMed] [Google Scholar]
- 27.Weiss JN, Levy S. Stem cell ophthalmology treatment study: bone marrow derived stem cells in the treatment of retinitis pigmentosa. Stem Cell Investig. 2018;5:18. doi: 10.21037/sci.2018.04.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oner A, Gonen ZB, Sevim DG, Smim Kahraman N, Unlu M. Suprachoroidal adipose tissue-derived mesenchymal stem cell implantation in patients with dry-type age-related macular degeneration and stargardt's macular dystrophy: 6-month follow-up results of a phase 2 study. Cell Reprogr. 2018;20(6):329–336. doi: 10.1089/cell.2018.0045. [DOI] [PubMed] [Google Scholar]
- 29.Mehat MS, Sundaram V, Ripamonti C, Robson AG, Smith AJ, Borooah S, et al. Transplantation of human embryonic stem cell-derived retinal pigment epithelial cells in macular degeneration. Ophthalmology. 2018;125(11):1765–1775. doi: 10.1016/j.ophtha.2018.04.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Öner A, Gönen Z, Gülmez Sevim D, Sinim Kahraman N, Çetin M, Özkul Y. First-year results of subretinal mesenchymal stem cell implantation in severe retinitis pigmentosa. J Stem Cell Res Ther. 2019;9:954. [Google Scholar]
- 31.Özmert E, Arslan U. Management of retinitis pigmentosa by Wharton's jelly derived mesenchymal stem cells: preliminary clinical results. Stem Cell Res Ther. 2020;11(1):25. doi: 10.1186/s13287-020-1549-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kahraman NS, Oner A. Umbilical cord derived mesenchymal stem cell implantation in retinitis pigmentosa: a 6-month follow-up results of a phase 3 trial. Int J Ophthalmol. 2020;13(9):1423–1429. doi: 10.18240/ijo.2020.09.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Limoli PG, Limoli CSS, Morales MU, Vingolo EM. Mesenchymal stem cell surgery, rescue and regeneration in retinitis pigmentosa: clinical and rehabilitative prognostic aspects. Restor Neurol Neurosci. 2020;38(3):223–237. doi: 10.3233/RNN-190970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhao T, Liang Q, Meng X, Duan P, Wang F, Li S, et al. Intravenous infusion of umbilical cord mesenchymal stem cells maintains and partially improves visual function in patients with advanced retinitis pigmentosa. Stem Cells Dev. 2020;29(16):1029–1037. doi: 10.1089/scd.2020.0037. [DOI] [PubMed] [Google Scholar]
- 35.Wiącek MP, Gosławski W, Grabowicz A, Sobuś A, Kawa MP, Baumert B, et al. Long-term effects of adjuvant intravitreal treatment with autologous bone marrow-derived lineage-negative cells in retinitis pigmentosa. Stem Cells Int. 2021;2021:6631921. doi: 10.1155/2021/6631921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sung Y, Lee MJ, Choi J, Jung SY, Chong SY, Sung JH, et al. Long-term safety and tolerability of subretinal transplantation of embryonic stem cell-derived retinal pigment epithelium in Asian Stargardt disease patients. Br J Ophthalmol. 2021;105(6):829–837. doi: 10.1136/bjophthalmol-2020-316225. [DOI] [PubMed] [Google Scholar]
- 37.Li SY, Liu Y, Wang L, Wang F, Zhao TT, Li QY, et al. A phase I clinical trial of human embryonic stem cell-derived retinal pigment epithelial cells for early-stage Stargardt macular degeneration: 5-years' follow-up. Cell Prolif. 2021;54(9):e13100. doi: 10.1111/cpr.13100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weiss JN, Levy S. Stem cell ophthalmology treatment study (SCOTS): bone marrow-derived stem cells in the treatment of stargardt disease. Medicines. 2021;8(2):10. doi: 10.3390/medicines8020010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nor Khairullah S, Nor Fariza N, Roslin AAZ, Angelina T. Subtenon implantation of Wharton's jelly-derived mesenchymal stromal cells in retinitis pigmentosa. Med J Malaysia. 2022;77(5):564–568. [PubMed] [Google Scholar]
- 40.Fernandes MR, Lojudice FH, Ribeiro LZ, da Cruz NF, Polizelli MU, Cristovam PC, Innocenti F, Morimoto L, Magalhães O, Jr, Sallum JM, Sogayar MC. Transplantation of subretinal stem cell-derived retinal pigment epithelium for stargardt’s disease: a phase I clinical trial. Retina. 2022;17:10–97. doi: 10.1097/IAE.0000000000003655. [DOI] [PubMed] [Google Scholar]
- 41.Oner A, Kahraman NS. Suprachoroidal umbilical cord derived mesenchymal stem cell implantation for the treatment of retinitis pigmentosa in pediatric patients. Am J Stem Cell Res. 2023;5(1):1–7. [Google Scholar]
- 42.Cotrim CC, Vieira Messias AM, Jorge R, Siqueira RC. Intravitreal use of a bone marrow mononuclear fraction (BMMF) containing CD34+ cells in patients with stargardt type macular dystrophy. Stem Cells Int. 2020;2020:8828256. doi: 10.1155/2020/8828256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nair DSR, Thomas BB. Stem cell-based treatment strategies for degenerative diseases of the Retina. Curr Stem Cell Res Ther. 2022;17(3):214–225. doi: 10.2174/1574888X16666210804112104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Moghadam Fard A, Mirshahi R, Naseripour M, Ghasemi FK. Stem cell therapy in stargardt disease: a systematic review. J Ophthalmic Vis Res. 2023;18(3):318–327. doi: 10.18502/jovr.v18i3.13780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oner A, Gonen ZB, Sinim N, Cetin M, Ozkul Y. Subretinal adipose tissue-derived mesenchymal stem cell implantation in advanced stage retinitis pigmentosa: a phase I clinical safety study. Stem Cell Res Ther. 2016;7(1):178. doi: 10.1186/s13287-016-0432-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.He Y, Zhang Y, Liu X, Ghazaryan E, Li Y, Xie J, et al. Recent advances of stem cell therapy for retinitis pigmentosa. Int J Mol Sci. 2014;15(8):14456–14474. doi: 10.3390/ijms150814456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pearson RA, Gonzalez-Cordero A, West EL, Ribeiro JR, Aghaizu N, Goh D, et al. Donor and host photoreceptors engage in material transfer following transplantation of post-mitotic photoreceptor precursors. Nat Commun. 2016;7:13029. doi: 10.1038/ncomms13029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ortin-Martinez A, Yan NE, Tsai ELS, Comanita L, Gurdita A, Tachibana N, et al. Photoreceptor nanotubes mediate the in vivo exchange of intracellular material. Embo j. 2021;40(22):e107264. doi: 10.15252/embj.2020107264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kalargyrou AA, Basche M, Hare A, West EL, Smith AJ, Ali RR, et al. Nanotube-like processes facilitate material transfer between photoreceptors. EMBO Rep. 2021;22(11):e53732. doi: 10.15252/embr.202153732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Avery RL, Bakri SJ, Blumenkranz MS, Brucker AJ, Cunningham ET, Jr, D'Amico DJ, Dugel PU, Flynn HW, Jr, Freund KB, Haller JA, Jumper JM. Intravitreal injection technique and monitoring: updated guidelines of an expert panel. Retina. 2014;1(34):S1–8. doi: 10.1097/IAE.0000000000000399. [DOI] [PubMed] [Google Scholar]
- 51.Kim YC, Chiang B, Wu X, Prausnitz MR. Ocular delivery of macromolecules. J Control Release. 2014;190:172–181. doi: 10.1016/j.jconrel.2014.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kim JY, You YS, Kim SH, Kwon OW. Epiretinal membrane formation after intravitreal autologous stem cell implantation in a retinitis pigmentosa patient. Retin Cases Brief Rep. 2017;11(3):227–231. doi: 10.1097/ICB.0000000000000327. [DOI] [PubMed] [Google Scholar]
- 53.Peng Y, Tang L, Zhou Y. Subretinal injection: a review on the novel route of therapeutic delivery for vitreoretinal diseases. Ophthalmic Res. 2017;58(4):217–226. doi: 10.1159/000479157. [DOI] [PubMed] [Google Scholar]
- 54.Chiang B, Jung JH, Prausnitz MR. The suprachoroidal space as a route of administration to the posterior segment of the eye. Adv Drug Deliv Rev. 2018;126:58–66. doi: 10.1016/j.addr.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Limoli PG, Vingolo EM, Morales MU, Nebbioso M, Limoli C. Preliminary study on electrophysiological changes after cellular autograft in age-related macular degeneration. Medicine. 2014;93(29):e355. doi: 10.1097/MD.0000000000000355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Limoli PG, Limoli C, Vingolo EM, Scalinci SZ, Nebbioso M. Cell surgery and growth factors in dry age-related macular degeneration: visual prognosis and morphological study. Oncotarget. 2016;7(30):46913–46923. doi: 10.18632/oncotarget.10442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Limoli PG, Vingolo EM, Limoli C, Scalinci SZ, Nebbioso M. Regenerative therapy by suprachoroidal cell autograft in dry age-related macular degeneration: preliminary in vivo report. JoVE J Vis Exp. 2018;132:e56469. doi: 10.3791/56469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Robinson MR, Lee SS, Kim H, Kim S, Lutz RJ, Galban C, et al. A rabbit model for assessing the ocular barriers to the transscleral delivery of triamcinolone acetonide. Exp Eye Res. 2006;82(3):479–487. doi: 10.1016/j.exer.2005.08.007. [DOI] [PubMed] [Google Scholar]
- 59.Jin ZB, Gao ML, Deng WL, Wu KC, Sugita S, Mandai M, et al. Stemming retinal regeneration with pluripotent stem cells. Prog Retin Eye Res. 2019;69:38–56. doi: 10.1016/j.preteyeres.2018.11.003. [DOI] [PubMed] [Google Scholar]
- 60.Ng TK, Fortino VR, Pelaez D, Cheung HS. Progress of mesenchymal stem cell therapy for neural and retinal diseases. World J Stem Cells. 2014;6(2):111–119. doi: 10.4252/wjsc.v6.i2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hosseini Shabanan S, Seyedmirzaei H, Barnea A, Hanaei S, Rezaei N. Stem cell transplantation as a progressing treatment for retinitis pigmentosa. Cell Tissue Res. 2022;387(2):177–205. doi: 10.1007/s00441-021-03551-3. [DOI] [PubMed] [Google Scholar]
- 62.Strioga M, Viswanathan S, Darinskas A, Slaby O, Michalek J. Same or not the same? Comparison of adipose tissue-derived versus bone marrow-derived mesenchymal stem and stromal cells. Stem Cells Dev. 2012;21(14):2724–2752. doi: 10.1089/scd.2011.0722. [DOI] [PubMed] [Google Scholar]
- 63.Zhang J, Li P, Zhao G, He S, Xu D, Jiang W, et al. Mesenchymal stem cell-derived extracellular vesicles protect retina in a mouse model of retinitis pigmentosa by anti-inflammation through miR-146a-Nr4a3 axis. Stem Cell Res Ther. 2022;13(1):394. doi: 10.1186/s13287-022-03100-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Bacci GM, Becherucci V, Marziali E, Sodi A, Bambi F, Caputo R. Treatment of inherited retinal dystrophies with somatic cell therapy medicinal product: a review. Life. 2022;12(5):708. doi: 10.3390/life12050708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Schwartz SD, Hubschman JP, Heilwell G, Franco-Cardenas V, Pan CK, Ostrick RM, et al. Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet. 2012;379(9817):713–720. doi: 10.1016/S0140-6736(12)60028-2. [DOI] [PubMed] [Google Scholar]
- 66.Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126(4):663–676. doi: 10.1016/j.cell.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 67.Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131(5):861–872. doi: 10.1016/j.cell.2007.11.019. [DOI] [PubMed] [Google Scholar]
- 68.Hirami Y, Osakada F, Takahashi K, Okita K, Yamanaka S, Ikeda H, et al. Generation of retinal cells from mouse and human induced pluripotent stem cells. Neurosci Lett. 2009;458(3):126–131. doi: 10.1016/j.neulet.2009.04.035. [DOI] [PubMed] [Google Scholar]
- 69.Eiraku M, Takata N, Ishibashi H, Kawada M, Sakakura E, Okuda S, et al. Self-organizing optic-cup morphogenesis in three-dimensional culture. Nature. 2011;472(7341):51–56. doi: 10.1038/nature09941. [DOI] [PubMed] [Google Scholar]
- 70.Li Y, Tsai YT, Hsu CW, Erol D, Yang J, Wu WH, et al. Long-term safety and efficacy of human-induced pluripotent stem cell (iPS) grafts in a preclinical model of retinitis pigmentosa. Mol Med. 2012;18(1):1312–1319. doi: 10.2119/molmed.2012.00242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Mandai M, Watanabe A, Kurimoto Y, Hirami Y, Morinaga C, Daimon T, et al. Autologous induced stem-cell-derived retinal cells for macular degeneration. N Engl J Med. 2017;376(11):1038–1046. doi: 10.1056/NEJMoa1608368. [DOI] [PubMed] [Google Scholar]
- 72.Yasuo K. Safety study using allogenic iPSC-retinal sheets for patients with retinitis pigmentosa (iRERP). https://jrct.niph.go.jp/en-latest-detail/jRCTa050200027. Accessed 11 Sept 2023.
- 73.Maeda T, Mandai M, Sugita S, Kime C, Takahashi M. Strategies of pluripotent stem cell-based therapy for retinal degeneration: update and challenges. Trends Mol Med. 2022;28(5):388–404. doi: 10.1016/j.molmed.2022.03.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.