Abstract
Background:
As no evidence-based treatment guidelines exist for chronic Achilles tendon rupture (CATR), a systematic review of the literature was performed to compare the different treatment options and recommend a literature-based algorithm.
Methods:
In June 2022, MEDLINE, Embase, and Cochrane Library databases were systematically reviewed based on the PRISMA guidelines. The level of evidence (LOE) and quality of evidence were evaluated, and statistics on clinical outcomes and complications were calculated.
Results:
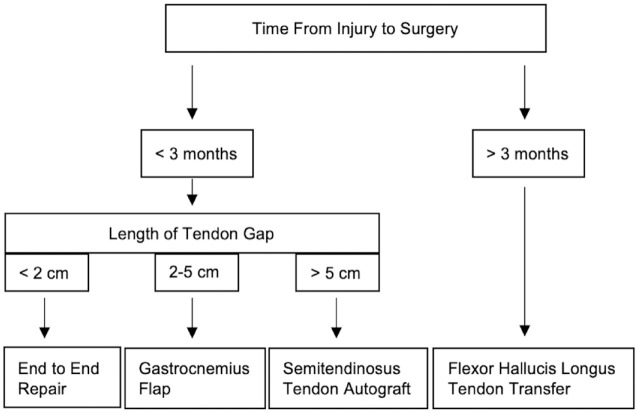
Twenty-seven studies with 614 patients were included. Three studies were LOE III and 25 studies were LOE IV. The mean Achilles tendon rupture score improved from a preoperative weighted mean of 38.8 ± 12.4 to a postoperative score 90.6 ± 4.7. The overall complication rate was 11.4%. Single techniques were used in 23 studies and dual techniques were used in 5 studies. The FHL tendon transfer was the most frequently used technique. We devised an algorithmic approach based on time from injury to surgical intervention and the length of the gap between the tendon stumps: >3 months: FHL transfer; <3 months (a) gap <2 cm, end-to-end repair; (b) gap 2 to 5 cm, gastrocnemius transfer, (c) gap >5 cm, semitendinosus autograft.
Conclusion:
Surgical management of CATR produced improvements in patient-reported outcome scores at midterm follow up, but a high complication rate (11.4%) was noted. Our proposed treatment algorithm may assist in shared decision making for this complex problem.
Keywords: repair, reconstruction, rupture, tear, chronic, Achilles, allograft, autograft, tendon, transfer
Introduction
The Achilles tendon is the most commonly ruptured tendon in the lower limb, affecting 18 in 100 000 people in the United States and Europe. 2 When left untreated for at least 4 weeks, these are classified as chronic or “neglected” Achilles tendon ruptures (CATR). 14 These chronic injuries may cause marked impairment in gait due to gastrocnemius-soleus complex (GSC) altered mechanics and atrophy of muscle over time. 41 Consequently, they are best managed surgically. 38
Numerous surgical techniques have been described to address CATR. Flexor hallucis longus (FHL) transfer is a frequently used tendon transfer technique as it fires in-phase with the Achilles, but is associated with reduced plantarflexion strength of the first ray.13,20 The semitendinosus tendon can be harvested as an autograft as it is a robust, strong tendon that can bridge large gaps between the tendon stumps.7,28 The gastrocnemius tendon is an easily accessible tendon that is in the same line of pull as the Achilles tendon and thus can restore normal ankle biomechanics.8,12 The peroneus brevis tendon is a local, strong graft that can be used to treat CATR but is associated with reduced postoperative eversion strength. 31 Synthetic materials can be used to treat CATR but are associated with a high complication rate.18,19 Dual techniques may provide additional strength and stability but the requirement for additional incisions is associated with an increased risk of wound complications. 10
There is discordance on the optimal surgical treatment for CATR. Given the prevalence of this injury, there is a need to determine the best in class of the surgical treatments described in the literature. 33 We performed a systematic review to evaluate the clinical outcomes, level, and quality of evidence of the surgical techniques for CATR and proposed an algorithmic approach to the treatment of CATR, based on current best available evidence.
Materials and Methods
Search Strategy
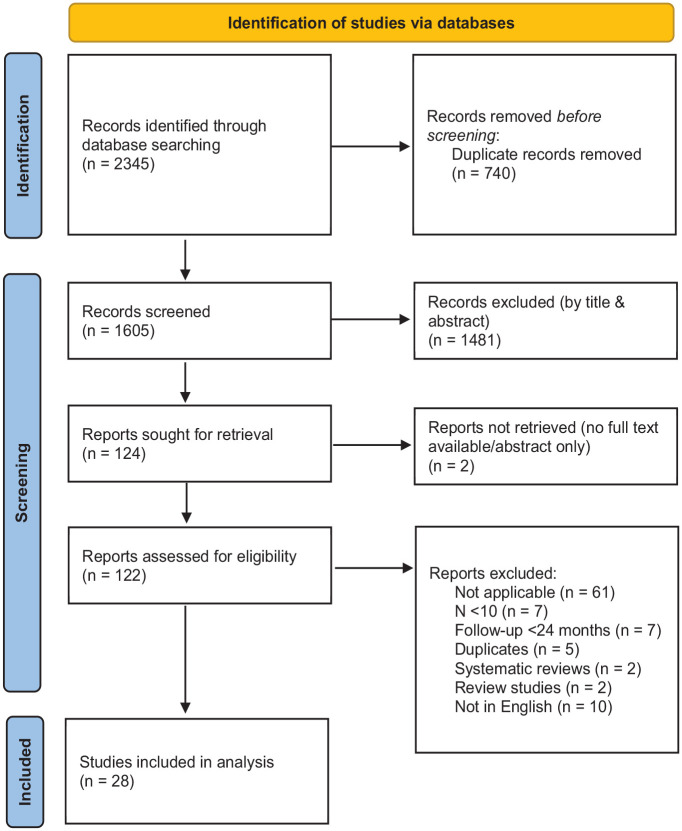
In June 2022, a systematic review of the MEDLINE, Embase, and Cochrane Library databases was performed based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Figure 1). 26 The PRISMA guidelines allow for transparency with respect to the way that researchers conduct a systematic review or meta-analysis including describing the method of search, data selection, and data collection in the manuscript and in a flow chart. The following search terms were used: (((Achilles) and (chronic or neglected or missed) and (surgery or surgical or operation or repair or reconstruction or allograft or autograft or graft))). The inclusion and exclusion criteria are shown in Table 1.
Figure 1.
PRISMA diagram.
Table 1.
Inclusion and Exclusion Criteria.
| Inclusion Criteria | Exclusion criteria |
|---|---|
| Patients received surgical correction of CATR | <10 patients |
| Follow-up ≥24 mo | Case reports |
| Published in a peer-reviewed journal | Systematic reviews and meta-analyses |
| Written in English | Review articles |
| Animal studies |
Abbreviation: CATR, chronic Achilles tendon rupture.
We identified 2345 articles, and removing duplicates left 1605 articles to screen by 2 independent reviewers (Figure 1). A senior author was consulted to arbitrate any disagreements that arose. We excluded papers if there were fewer than 10 patients, case reports, meta-analyses, reviews studies, or animal studies, and were left with 28 studies included in our analysis.
Assessment of Level of Evidence and Methodological Quality
The level of evidence (LOE) was evaluated using the criteria published by The Journal of Bone & Joint Surgery. 34 The methodological quality of evidence (QOE) was assessed using the Modified Coleman Methodology Score (MCMS). 5 Two independent reviewers determined the MCMS for each study. Excellent studies had a score between 85 and 100 points, good studies scored between 70 and 84 points, fair studies had a score between 55 and 69 points, and poor studies scored less than 55 points. If any discrepancy existed, the senior author evaluated the available data and a consensus was reached.
Data Extraction and Evaluation
Two independent reviewers independently extracted and assessed the data from each study. Data on patient demographics and the characteristics of the surgical procedure were collected. Subjective outcomes, return to sports data, complications, failures, and reoperations were evaluated for individual treatments and for surgical treatment of CATR overall.
Statistical Analysis
All other statistical analyses were performed using SAS software, version 9.3 (SAS Institute, Inc, Cary NC). Descriptive statistics were calculated for all continuous and categorical variables. Continuous variables were reported as weighted mean and estimated standard deviation, whereas categorical variables were reported as frequencies with percentages.
Results
The search generated 2345 studies (Figure 1). Twenty-eight met the inclusion and exclusion criteria of this systematic review (Table 1). The studies were published between 2002 and 2021 (Table 2).
Table 2.
Summary of Study Characteristics and Outcomes.
| Author | Year | LOE | MCMS | Patients (n) |
Age (y) |
Follow-up (mo) | Technique | Time From Injury to Surgery (wk) | Length of Tendon Gap (cm) | Patient Outcomes | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scores | Pre op. | Post op. | ||||||||||
| Takao et al 44 | 2003 | 4 | 57 | 10 | 51 | 75.1 | Gastrocnemius flap | 16 | AOFAS | 72.6 | 98.1 | |
| Jennings and Sefton 19 | 2002 | 4 | 61 | 16 | 52 | 36 | Polyester tape | 67.2 | Tegner | 2.7 | 1.8 | |
| Elias et al 10 | 2007 | 4 | 54 | 15 | 55.8 | 26.5 | V-Y and FHL transfer | 17.3 | 5.7 | AOFAS | 58.4 | 94.1 |
| VAS | 2.1 | 1.6 | ||||||||||
| Kosanović and Brilej 24 | 2008 | 4 | 54 | 18 | 50 | 67 | Percutaneous suturing of tendon | 7.1 | 5.7 | Tegner | 5.4 | 4.6 |
| Ibrahim 18 | 2009 | 4 | 51 | 14 | 41.6 | LARS | 15 | AOFAS | 48.6 | 85.9 | ||
| Tegner | 2.58 | 1.73 | ||||||||||
| El Shewy et al 8 | 2009 | 4 | 56 | 11 | 34.3 | 89.5 | Gastrocnemius flap | 7.3 | AOFAS | 42.3 | 98.9 | |
| Holz | 66 | 163 | ||||||||||
| Maffulli et al 32 | 2010 | 4 | 55 | 32 | 47.1 | 48.4 | PB transfer | 15.2 | ATRS | 92.5 | ||
| Sarzaeem et al 40 | 2012 | 4 | 53 | 11 | 30 | 25 | ST autograft | 48 | 8.3 | AOFAS | 70 | 92 |
| ATRS | 32 | 89 | ||||||||||
| Khiami et al 21 | 2013 | 4 | 53 | 23 | 52.1 | 24.5 | Free triceps sural aponeurosis | 53.6 | 5.7 | AOFAS | 63.6 | 96.1 |
| Maffulli et al 28 | 2013 | 4 | 65 | 26 | 42 | 98.4 | ST autograft | 15.2 | >6 cm | ATRS | 88 | |
| Maffulli et al 30 | 2013 | 4 | 56 | 28 | 46 | 31.4 | ST autograft | 116 | >6 cm | ATRS | 42 | 86 |
| Esenyel et al 12 | 2014 | 4 | 62 | 10 | 41 | 43.2 | Gastrocnemius flap | 7.6 | AOFAS | 64.8 | 97.8 | |
| El Shazly et al 7 | 2014 | 4 | 60 | 15 | 37.7 | 27 | ST autograft | 13.5 | 4.9 | AOFAS | 32.6 | 90.8 |
| Yasuda et al 47 | 2016 | 4 | 56 | 30 | 52.7 | 33 | Direct repair with scar tissue | 22 | 4.3 | AOFAS | 82.8 | 98.1 |
| ATRS | 92 | |||||||||||
| Ahmad et al 1 | 2016 | 4 | 58 | 32 | 53.3 | 62.3 | FHL transfer and Turndown of proximal, central Achilles | 14.6 | 7.5 | VAS | 6.6 | 1.8 |
| FAAM-Sports | 36.3 | 90.2 | ||||||||||
| Elgohary et al 9 | 2016 | 4 | 56 | 19 | 47 | 29 | FHL transfer and gastrocnemius recession |
16 | 6.8 | AOFAS | 65 | 94 |
| Gedam and Rushnaiwala 15 | 2016 | 3 | 46 | 14 | 45.6 | 30.1 | Gastrocnemius turndown flap and ST autograft | 22 | 5.1 | AOFAS | 64.5 | 96.9 |
| ATRS | 49.4 | 91.4 | ||||||||||
| Guclu et al 16 | 2016 | 3 | 55 | 17 | 33 | 195 | V-Y and fascia turndown | 28 | 6 | AOFAS | 64 | 95 |
| Seker et al 42 | 2016 | 4 | 62 | 21 | 32.1 | 145.3 | Gastrocnemius flap | 8.4 | 6.4 | AOFAS | 33 | 98.5 |
| FADI | 98.9 | |||||||||||
| VAS | 0 | |||||||||||
| Maffulli et al 31 (ST/PB/FHL) | 2018 | 4 | 60 | (21/21/20) | (45.7/45.8/42.7) | (34.1/36.4/35.8) | ST graft, PB transfer, FHL transfer | (15.6/17.2/14.8) | (>6 cm, <6 cm, <6 cm) | ATRS | (50.4/51.3/52.3) | (89.4/89.5/88.9) |
| Lever et al 25 | 2018 | 4 | 57 | 20 | 60 | 73 | FHL transfer | 28 | AOFAS | 94.3 | ||
| ATRS | 83 | |||||||||||
| SF-12 | 47.8 | |||||||||||
| Tegner | 5 | 4 | ||||||||||
| Vega et al 46 | 2018 | 4 | 53 | 22 | 69 | 30.5 | FHL transfer | 6.3 | AOFAS | 55 | 91 | |
| Song et al 43 | 2020 | 4 | 49 | 33 | 36.1 | 53 | ST allograft | 12 | – | AOFAS | 50 | 100 |
| ATRS | 22.5 | 99 | ||||||||||
| Tegner | 1 | 4 | ||||||||||
| VISA-A | 23 | 94 | ||||||||||
| Zou et al 48 | 2021 | 4 | 62 | 19 | 46.7 | 31 | Double-bundle FHL transfer | 14.7 | 5.5 | AOFAS | 52.1 | 97.5 |
| ATRS | 23.3 | 98.3 | ||||||||||
| VISA-A | 23.4 | 95.7 | ||||||||||
| Tsukada et al 45 | 2021 | 4 | 55 | 10 | 51.7 | 36.5 | ST autograft (Slide-locking loop suture - SLLS) |
28.8 | 5.29 | AOFAS | 64.2 | 95 |
| ATRS | 29.8 | 86.2 | ||||||||||
| Fischer et al 13 (FHL/PL) | 2021 | 3 | 52 | 60 (34/26) | 54.82 (57.29/51.58) | 49 | FHL transfer vs plantaris longus augmentation |
30.48 (29.87/31.62) | AOFAS | 87.80 (85.61/90.58) | ||
| VAS-FA | 78.07 (73.66/83.66) | |||||||||||
| SF-12 Phys | 48.21 (46.24/50.71) | |||||||||||
| SF-12 Ment | 54.10 (54.98/52.99) | |||||||||||
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society; ATRS, Achilles tendon rupture score; FAAM, Foot and Ankle Ability Measure; FADI, Foot and Ankle Disability Index; FHL, flexor hallucis longus; LARS, ligament augmentation and reconstruction system; LOE, level of evidence; MCMS; Modified Coleman Methodological Score; PB, peroneus brevis; PL, peroneus longus; SF-12, 12-Item Short Form Health Survey; ST, semitendinosus; VAS, visual analog scale; VISA-A, Victorian Institute Society Australia–Achilles.
Patient Demographics
From the 28 studies, 614 patients with a weighted mean age of 48.0 ± 9.5 (range, 30-69) years underwent surgical correction of CATR. The weighted mean time from injury to surgery was 26.4 ± 22.6 (range, 7.1-116) weeks. The weighted mean postoperative follow-up time was 52.7 ± 38.7 (range, 24.5-195) months. The weighted mean size of the tendon gap was 5.8 ± 1.2 (range, 4-8.3) cm.
LOE and QOE
Three studies were LOE III and 25 studies were LOE IV. The mean MCMS score was 56.0 ± 4.3 of 100 points. Eighteen studies were fair quality and 10 studies were poor quality.
Overall Findings for the Surgical Treatment of CATR
Preoperative American Orthopaedic Foot & Ankle Society (AOFAS) scores increased from a weighted mean of 57.8 ± 13.1 (range, 32.6-82.8) to 94.0 ± 5.1 (range, 78.5-100) postoperatively. Preoperative Achilles total tendon rupture (ATRS) scores increased from a weighted mean of 38.8 ± 12.4 (range, 23.3-52.3) to 90.6 ± 4.7 (range, 83-99) postoperatively. Preoperative Tegner scores increased from a weighted mean of 3.0 ± 1.8 (range, 1-5.4) to 3.4 ± 1.4 (range, 1.7-4.6) postoperatively. Preoperative visual analog scale (VAS) scores decreased from a weighted mean of 5.2 ± 3.2 (range, 2.1-6.6) to 1.2 ± 1.0 (range, 0-1.8) postoperatively.
The return to sport (RTS) was 84.2%.
The complication rate was 11.4%. The 2 most common complications include superficial wound infection and sural nerve hypoesthesia.
Flexor hallucis longus tendon transfer
Seven studies performed flexor hallucis longus (FHL) tendon transfer on 141 patients.13,20,25,31,37,46,48 The decision to perform an FHL transfer was determined by the senior surgeon’s preference. The AOFAS score was the scoring system that was most frequently utilized in 6 studies. The weighted mean preoperative AOFAS score was 54.7 ± 2.7 (range, 52.1-57.5), and the postoperative score was 90.8 ± 7.3 (range, 78.5-97.5). The ATRS score was used in 3 studies. The weighted mean preoperative ATRS score was 38.2 ± 20.5 (range, 23.3-52.3), and postoperative was 89.9 ± 7.7 (range, 83-98.3).
The RTS rate was 81.8%.
The complication rate was 11.3%. The most common complication was surgical wound infection, which was observed in 11 patients (7.8%).
Semitendinosus Autograft
Six studies performed semitendinosus autografts on 111 patients.7,28,30,31,40,45 The ATRS score was the most commonly utilized scoring system in 5 studies. The weighted mean preoperative ATRS score was 41.2 ± 9.5 (range, 29.8-50.4), and the postoperative score was 87.7 ± 1.6 (range, 86-89.4). The AOFAS score was used in 3 studies, all of which reported preoperative and postoperative scores. The weighted mean preoperative AOFAS score was 52.8 ± 20.1 (range, 32.6-70), and the postoperative score was 92.3 ± 2.2 (range, 90.8-95).
The RTS was 76.7%.
The complication rate was 7.2%. The most common complication was superficial wound infection, which was observed in 4 patients (3.6%).
Gastrocnemius flaps
Four studies utilized turndown gastrocnemius fascial flaps for 52 patients.8,12,42,44 The AOFAS score was the scoring system that was most frequently used in all 4 studies. The weighted mean preoperative AOFAS score was 48.7 ± 18.6 (range, 33-72.6), and the postoperative score was 98.4 ± 0.5 (range, 97.8-98.9).
The RTS rate was 100%.
The complication rate was 11.5%. Three patients (5.8%) developed superficial wound infections, and 3 patients developed wound gapping (5.8%).
Peroneus Brevis transfer
Two studies performed peroneus brevis tendon (PB) transfer on 53 patients.31,32 The ATRS was utilized in both studies. The preoperative ATRS score was 51.3, and the weighted mean postoperative score was 91.3 ± 2.12 (range, 89.5-92.5).
The RTS rate was 76.0%.
The complication rate was 11.3%. Complications included 4 superficial wound infections (7.5%) and 2 cases (3.6%) of hypertrophic scarring.
Synthetic Materials
Two studies utilized synthetic materials, ligament augmentation and reconstruction system (LARS) and polyester tape, to treat CATR for 30 patients total.18,19 The Tegner score was the most commonly utilized scoring system in both studies. The preoperative weighted mean Tegner score was 2.6 ± 0.1 (range, 2.58-2.7), and the postoperative score was 1.8 ± 0.07 (range, 1.7-1.8).
The RTS rate was 100%.
The complication rate was 20.0%. The most common complication was superficial wound infection, which was observed in 4 patients (13.3%). One patient (3.3%) required further surgical intervention to excise tape from the calcaneus.
Other Techniques
Five studies reported single technique procedures that were not used in any of the other studies, operating on 130 patients. These include semitendinosus tendon allograft, 43 percutaneous suturing of the tendon, 24 free triceps sural aponeurosis, 21 direct repair with scar tissue, 47 and plantaris longus augmentation. 13 The AOFAS score was the scoring system that was used most frequently in 4 studies. The weighted mean preoperative AOFAS score was 64.9 ± 16.5 (range, 50.0-82.8), and the postoperative score was 96.5 ± 4.1 (range, 90.6-100). The weighted mean Tegner score was 2.5 ± 3.1 (range, 1.0-5.4) preoperatively and 4.2 ± 0.4 (range, 4.0-4.6) postoperatively.
The RTS rate was 76.7%.
The complication rate was 10.8%. The most common complication was surgical wound complications, which was observed in 7 patients (5.4%). One patient (0.8%) developed septic partial tendon necrosis requiring surgical resection to preserve the tendon.
Dual Techniques
Five studies utilized dual techniques to treat CATR for 97 patients. This included combining V-Y lengthening with a FHL transfer, 10 combining V-Y lengthening with a fascia turndown, 16 combining a turndown of the proximal, central Achilles with a FHL tendon transfer 1 ; combining a FHL transfer with a gastrocnemius recession 9 ; and combining central gastrocnemius turndown flap with semitendinosus augmentation. 15 The AOFAS score was the scoring system that was used most commonly in 4 studies. The weighted mean preoperative AOFAS score was 63.1 ± 3.1 (range, 58.4-65.0), and the postoperative score was 94.9 ± 1.3 (range, 94.0-96.9). The VAS score was used in 2 studies, both of which reported pre- and postoperative scores. The weighted mean preoperative VAS score was 5.2 ± 3.2 (range, 2.1-6.6), and the postoperative score was 1.7 ± 0.14 (range, 1.6-1.8).
The RTS rate was 100%.
The complication rate was 14.4%. The most common complication was superficial wound complications, which was observed in 10 patients (10.3%). Three patients required further surgical intervention.
Discussion
The gold standard operative technique for CATR remains controversial because of low LOE, low QOE, and a multitude of factors influencing each individual case. Several variables have been shown to influence outcomes, not just surgical technique. Chronicity, tendon gap size, gender, and age are all potential predictors of outcome and should be included in any treatment algorithm. We present a simplified algorithm with the current best available evidence and results from our systematic review.
The most commonly used single technique procedure to bridge Achilles tendon gap was the FHL tendon transfer. The muscle belly of the FHL is a highly vascularized region 3 and may provide increased blood supply to the Achilles tendon repair site, which can aid in wound tissue repair. Patients treated with FHL transfer reported improvement in subjective clinical outcome scores and had a low surgical wound complication rate (11.3%). However, there is concern that FHL transfer reduces interphalangeal joint (IPJ) plantarflexion strength of the hallux. 23 This review found that the hallux of the operated leg was weaker than the contralateral leg. The loss of IPJ plantarflexion of the hallux diminishes push off during the stance phase. 6 Nevertheless, a study of 19 patients conducted by Ozer et al 35 found no statistically significant differences in lower extremity strength between the operated leg and the healthy contralateral leg (P > .05). Thus, although IPJ plantarflexion may be reduced, overall function might not be impacted. The mean delay to treatment was 40 weeks, and considering all patients returned to preinjury daily activities, FHL tendon transfers can be considered an appropriate technique for considerably delayed cases. 35
Six studies utilized a semitendinosus tendon autograft. This can be harvested safely, quickly, has a low donor site morbidity, 36 and is less technically demanding than harvesting of other tendons. 28 Additionally, the length of the semitendinosus graft allows it to bridge larger Achilles tendon defects.11,29 This review found that patients who underwent semitendinosus tendon autograft had good functional outcomes at midterm follow-up and the lowest complication rate (7.2%). In cases with a tendon gap greater than 6 cm, this technique showed statistical significance in terms of clinical outcomes (P < .05). 40 One study in this review used a semitendinosus tendon allograft. 43 The semitendinosus allograft has similar beneficial properties to an autograft, without the risks associated with donor site morbidity. However, the relatively few number of studies with adequate sample sizes and follow-up times, together with the potential risks of creep, disease transmission, immunogenic response, cost, and poor incorporation of the graft into the host tissue, reduces our enthusiasm for routine use of this procedure.
Four studies reported outcomes following the use of gastrocnemius turndown fascial flaps. This procedure uses a strong, local graft fashioned from the proximal tendon stumps to fill the length of the defect. The graft is in the same line of pull as the original tendon, which aims to restore normal ankle biomechanics. 7 The lower skin and wound complication rate in this group is in part due to local anatomy. The fascia cruris is linked to the underlying paratenon from which the Achilles tendon receives its blood supply. In addition, the fascia provides stability to the overlying skin and optimizes perfusion by maintaining arteriole tension. A low bulk graft from the gastrocnemius facilitates closure of the fascia compared to a bulky reconstruction. This preserves normal tension, thus avoiding a potential blood supply reduction to the underlying reconstruction and skin, reducing the chance of wound breakdown. 44 Patients reported good postoperative strength, heel raise, and high return to play rates at final follow-up among this cohort. This demonstrated that gastrocnemius turndown fascial flaps are good options for gaps where end-to-end repair is not possible, but within reach of fascial turndown reconstruction to maintain a functional gastrocnemius-soleus complex.
Two studies used PB tendon transfer. The PB tendon is responsible for 28% of the eversion capacity of the hindfoot, 4 and patients in this review were found to have weakened postoperative eversion strength compared to the contralateral ankle and reported a relatively low RTS rate of 76.0%. This suggests that PB tendon transfer may not be suitable for athletes nor patients with chronic ankle instability.
Synthetic materials were used in 2 studies. Ibrahim et al 18 performed LARS and Jennings et al 19 used polyester tape on their respective patient cohorts. Although patients reported good functional outcomes, a high complication rate (20.0%) due to superficial wound infection was observed, calling into question the safety of these procedures.
Five studies used dual techniques. Combining techniques may provide additional support and strength to the tendon, exhibited by the improvement in postoperative plantarflexion strength. However, using multiple techniques may increase the number and length of incisions, exposing patients to a greater risk of wound complications, as evident by the high wound complication rate (14.4%). The ability to determine superiority between single technique and dual technique procedures cannot be reached in this review because of the marked heterogeneity and the poor quality of evidence in the included studies.
This current review found that surgical management of CATR is associated with relatively high complication rates across surgical interventions (11.4%). There are several reasons that could account for the concerning level of wound complications. Many patients had risk factors associated with poor wound healing, including corticosteroid use, diabetes, hypertension, and smoking. One study found that all patients who were smokers experienced postoperative wound complications. 25 Interestingly, some studies excluded patients with these risk factors from their final cohorts,10,46 which may give an inaccurate representation of the true surgical wound complication rate. Furthermore, the ruptured tendon site is often poorly vascularized initially, which may predispose patients to wound necrosis and dehiscence. 27 Many studies employed open surgical techniques, which are inherently associated with a higher incidence of surgical wound complications compared to minimally invasive techniques. Interestingly, for the 4 studies using endoscopic techniques, there were only 3 complications (4.1%),7,16,17,48 suggesting that patients that underwent minimally invasive repair of CATR may be more resistant to wound breakdown. However, this review cannot justify the use of endoscopic treatment for CATR in lieu of more invasive procedures because of the discrepancies in surgical techniques between 4 studies, the small sample sizes and the poor quality of evidence. After evaluating the different techniques for CATR we are proposing an algorithm that simplifies decision making for the treatment of chronic Achilles tendon ruptures with the current available evidence (Figure 2). This algorithm was devised using the most robust available basic science evidence, available clinical evidence, and the experience of the senior author.
Figure 2.
Chronic Achilles tendon rupture surgical management.
To our knowledge, no other study has taken into consideration how the biology of the GSC responds after that period of time. We divide our algorithm based on the time in which fatty muscle infiltration and decreased soleus muscle volume causes GSC impairment as shown by isokinetic peak torque deficits in the calf muscle and reduced plantar flexion strength. Three months has been the reported cut-off for these effects to occur. 17 We avoid using dual techniques due to an approximate 3% increased risk of wound complications compared to single techniques.
For CATR of less than 3 months with a tendon gap <2 cm, end-to-end repair is recommended with a Krackow technique as it has the highest tensile strength. 39 For gaps between 2 and 5 cm, a low bulk flap from the gastrocnemius provides a strong, easily accessible augmentation in the same line of pull as the original tendon restoring the ankle biomechanics. For gaps >5 cm, a semitendinosus autograft should be considered, as it showed in this systematic review high weighted mean postoperative scores of 92.3 ± 2.2 for AOFAS and 87.7 ± 1.6 for ATRS, as well as a low complication rate of 7.2%, and the advantage of the graft length to bridge larger Achilles tendon defects.
For CATR of more than 3 months, an FHL transfer is the author’s preferred technique as it addresses substitution and augmentation of the atrophied Achilles tendon.22,35 After 3 months, there is a compensatory hypertrophy of the FHL muscle to overcome the GSC deficiency. Because of the vascularity of the FHL muscle, it can compensate to achieve concentric and eccentric contraction strength comparable to the nonoperated side. 35
Limitations
This systematic review has several inherent limitations and/or potential biases. There was significant heterogeneity and inconsistency in the reporting of data with respect to surgical techniques, measurement methods, and postoperative outcome measurements between the included studies, limiting any meaningful cross-sectional analysis. Ten different subjective scoring tools were reported in the included studies (Table 3). In addition, the time between the initial injury and operative treatment varied considerably between studies, with a weighted mean time of 26.4 ± 22.6 weeks. RTS was not widely reported across studies and our results may be a product of sampling and should be interpreted with caution. The criterion was limited to MEDLINE, Embase, and Cochrane Library Database articles published in English. Finally, the LOE of the included studies was graded as low with poor QOE.
Table 3.
Outcome Measures Used in the Included Studies.
| Outcome Measures | Studies, n (%) |
|---|---|
| AOFAS | 21 (75.0) |
| ATRS | 11 (39.3) |
| Tegner Score | 5 (17.9) |
| VAS | 3 (10.7) |
| SF-12 | 2 (7.1) |
| VISA-A | 2 (7.1) |
| VAS-FA | 1 (3.6) |
| FAAM | 1 (3.6) |
| FADI | 1 (3.6) |
| Holz | 1 (3.6) |
Abbreviations: AOFAS, American Orthopaedic Foot & Ankle Society; ATRS, Achilles tendon rupture score; FAAM, Foot And Ankle Ability Measure; FADI, Foot and Ankle Disability Index; VAS, Visual Analog Scale; SF-12, 12-Item Short Form Health Survey; VISA-A, Victorian Institute Society Australia–Achilles.
Conclusion
Surgical management of CATR produced improvements in patient-reported outcome scores at midterm follow up, but a relatively high overall complication rate of 11.4% was noted. This systematic review found that no evidence-based treatment guidelines exist for CATR. The literature in this review consists mostly of studies of “fair” quality, with some of “poor” quality. Thus, future studies of higher QOE and LOE with improved data reporting and focused on specific risk factors are warranted to determine in which cases a particular technique would be suitable for CATR. We therefore proposed an algorithmic approach based on the current literature to aid in surgical planning and discussions for CATR.
Supplemental Material
Supplemental material, sj-pdf-1-fao-10.1177_24730114231200491 for Surgical Management of Chronic Achilles Tendon Ruptures: A Systematic Review and Proposed Treatment Algorithm by Mohammad T. Azam, James J. Butler, Matthew. B. Weiss, Hugo A. Ubillus, Noah Kirschner, Nathaniel P. Mercer and John G. Kennedy in Foot & Ankle Orthopaedics
Acknowledgments
This research study was done with collaboration from Yoshiharu Shimozono, MD.
Footnotes
Ethical Approval: Ethical approval was not sought for the present study because this is a systematic review of previously published articles where no PHI data was obtained and recorded.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: John G. Kennedy, MD, MCh, MMSc, FFSEM, FRCS(Orth), would like to acknowledge Mr. and Mrs. Michael J. Levitt for their research support.
ORCID iDs: Mohammad T. Azam BS,  https://orcid.org/0000-0003-0184-1330
https://orcid.org/0000-0003-0184-1330
Matthew. B. Weiss, BS,  https://orcid.org/0000-0001-6127-7626
https://orcid.org/0000-0001-6127-7626
Hugo A. Ubillus, MD,  https://orcid.org/0000-0002-4369-0289
https://orcid.org/0000-0002-4369-0289
Noah Kirschner, MD,  https://orcid.org/0000-0001-8828-6645
https://orcid.org/0000-0001-8828-6645
Nathaniel P. Mercer, MD,  https://orcid.org/0000-0002-2502-9294
https://orcid.org/0000-0002-2502-9294
John G. Kennedy, MD, MCh, MMSc, FFSEM, FRCS(Orth),  https://orcid.org/0000-0002-7258-6528
https://orcid.org/0000-0002-7258-6528
References
- 1. Ahmad J, Jones K, Raikin SM. Treatment of chronic Achilles tendon ruptures with large defects. Foot Ankle Spec. 2016;9(5):400-408. doi: 10.1177/1938640016640895 [DOI] [PubMed] [Google Scholar]
- 2. Badalihan A, Aihemaiti A, Shawutali N, et al. Outcome of a one-stage tensile stress surgical technique and early postoperative rehabilitation in the treatment of neglected Achilles tendon rupture. J Foot Ankle Surg. 2015;54(2):153-159. doi: 10.1053/j.jfas.2014.12.002 [DOI] [PubMed] [Google Scholar]
- 3. Carr AJ, Norris SH. The blood supply of the calcaneal tendon. J Bone Joint Surg Br. 1989;71(1):100-101. doi: 10.1302/0301-620X.71B1.2914976 [DOI] [PubMed] [Google Scholar]
- 4. Clarke HD, Kitaoka HB, Ehman RL. Peroneal tendon injuries. Foot Ankle Int. 1998;19(5):280-288. doi: 10.1177/107110079801900503 [DOI] [PubMed] [Google Scholar]
- 5. Coleman BD, Khan KM, Maffulli N, Cook JL, Wark JD. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports. 2000;10(1):2-11. doi: 10.1034/j.1600-0838.2000.010001002.x [DOI] [PubMed] [Google Scholar]
- 6. Coull R, Flavin R, Stephens MM. Flexor hallucis longus tendon transfer: evaluation of postoperative morbidity. Foot Ankle Int. 2003;24(12):931-934. doi: 10.1177/107110070302401211 [DOI] [PubMed] [Google Scholar]
- 7. El Shazly O, Abou El Soud MM, El Mikkawy DME, El Ganzoury I, Ibrahim AM. Endoscopic-assisted Achilles tendon reconstruction with free hamstring tendon autograft for chronic rupture of Achilles tendon: clinical and isokinetic evaluation. Arthroscopy. 2014;30(5):622-628. doi: 10.1016/j.arthro.2014.02.019 [DOI] [PubMed] [Google Scholar]
- 8. El Shewy MT, El Barbary HM, Abdel-Ghani H. Repair of chronic rupture of the Achilles tendon using 2 intratendinous flaps from the proximal gastrocnemius-soleus complex. Am J Sports Med. 2009;37(8):1570-1577. doi: 10.1177/0363546509333009 [DOI] [PubMed] [Google Scholar]
- 9. Elgohary HEA, Elmoghazy NA, Abd Ellatif MS. Combined flexor hallucis longus tendon transfer and gastrocnemius recession for reconstruction of gapped chronic Achilles tendon ruptures. Injury. 2016;47(12):2833-2837. doi: 10.1016/j.injury.2016.10.029 [DOI] [PubMed] [Google Scholar]
- 10. Elias I, Besser M, Nazarian LN, Raikin SM. Reconstruction for missed or neglected Achilles tendon rupture with V-Y lengthening and flexor hallucis longus tendon transfer through one incision. Foot Ankle Int. 2007;28(12):1238-1248. doi: 10.3113/FAI.2007.1238 [DOI] [PubMed] [Google Scholar]
- 11. Ellison P, Mason LW, Molloy A. Chronic Achilles tendon rupture reconstructed using hamstring tendon autograft. Foot (Edinb). 2016;26:41-44. doi: 10.1016/j.foot.2015.09.007 [DOI] [PubMed] [Google Scholar]
- 12. Esenyel CZ, Tekin C, Cakar M, et al. Surgical treatment of the neglected Achilles tendon rupture with Hyalonect. J Am Podiatr Med Assoc. 2014;104(5):434-443. doi: 10.7547/0003-0538-104.5.434 [DOI] [PubMed] [Google Scholar]
- 13. Fischer S, Kutscher R, Gramlich Y, Klug A, Hoffmann R, Manegold S. Secondary reconstruction of chronic Achilles tendon rupture: flexor hallucis longus transfer versus plantaris longus augmentation. Int Orthop. 2021;45(9):2323-2330. doi: 10.1007/s00264-021-05128-9 [DOI] [PubMed] [Google Scholar]
- 14. Flint JH, Wade AM, Giuliani J, Rue JP. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2014;42(1):235-241. doi: 10.1177/0363546513490656 [DOI] [PubMed] [Google Scholar]
- 15. Gedam PN, Rushnaiwala FM. Endoscopy-assisted Achilles tendon reconstruction with a central turndown flap and semitendinosus augmentation. Foot Ankle Int. 2016;37(12):1333-1342. doi: 10.1177/1071100716666365 [DOI] [PubMed] [Google Scholar]
- 16. Guclu B, Basat HC, Yildirim T, Bozduman O, Us AK. Long-term results of chronic Achilles tendon ruptures repaired with V-Y tendon plasty and fascia turndown. Foot Ankle Int. 2016;37(7):737-742. doi: 10.1177/1071100716642753 [DOI] [PubMed] [Google Scholar]
- 17. Heikkinen J, Lantto I, Flinkkila T, et al. Soleus atrophy is common after the nonsurgical treatment of acute Achilles tendon ruptures: a randomized clinical trial comparing surgical and nonsurgical functional treatments. Am J Sports Med. 2017;45(6):1395-1404. doi: 10.1177/0363546517694610 [DOI] [PubMed] [Google Scholar]
- 18. Ibrahim SAR. Surgical treatment of chronic Achilles tendon rupture. J Foot Ankle Surg. 2009;48(3):340-346. doi: 10.1053/j.jfas.2009.02.007 [DOI] [PubMed] [Google Scholar]
- 19. Jennings AG, Sefton GK. Chronic rupture of tendo Achillis. Long-term results of operative management using polyester tape. J Bone Joint Surg Br. 2002;84(3):361-363. doi: 10.1302/0301-620x.84b3.11559 [DOI] [PubMed] [Google Scholar]
- 20. Khalid MA, Weiss WM, Iloanya M, Panchbhavi VK. Dual purpose use of flexor hallucis longus tendon for management of chronic Achilles tendon ruptures. Foot Ankle Spec. 2019;12(4):345-349. doi: 10.1177/1938640018803695 [DOI] [PubMed] [Google Scholar]
- 21. Khiami F, Di Schino M, Sariali E, Cao D, Rolland E, Catonné Y. Treatment of chronic Achilles tendon rupture by shortening suture and free sural triceps aponeurosis graft. Orthop Traumatol Surg Res. 2013;99(5):585-591. doi: 10.1016/j.otsr.2013.03.021 [DOI] [PubMed] [Google Scholar]
- 22. Kim JY, Lee I, Seo K, Jung W, Kim B. FHL tendon transfer in diabetics for treatment of non-healing plantar heel ulcers. Foot Ankle Int. 2010;31(6):480-485. doi: 10.3113/FAI.2010.0480 [DOI] [PubMed] [Google Scholar]
- 23. Kirane YM, Michelson JD, Sharkey NA. Contribution of the flexor hallucis longus to loading of the first metatarsal and first metatarsophalangeal joint. Foot Ankle Int. 2008;29(4):367-377. doi: 10.3113/FAI.2008.0367 [DOI] [PubMed] [Google Scholar]
- 24. Kosanović M, Brilej D. Chronic rupture of Achilles tendon: is the percutaneous suture technique effective? Arch Orthop Trauma Surg. 2008;128(2):211-216. doi: 10.1007/s00402-007-0514-5 [DOI] [PubMed] [Google Scholar]
- 25. Lever CJ, Bosman HA, Robinson AHN. The functional and dynamometer-tested results of transtendinous flexor hallucis longus transfer for neglected ruptures of the Achilles tendon at six years’ follow-up. Bone Joint J. 2018;100-B(5):584-589. doi: 10.1302/0301-620X.100B5.BJJ-2017-1053.R1 [DOI] [PubMed] [Google Scholar]
- 26. Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Maffulli N, Ajis A, Longo UG, Denaro V. Chronic rupture of tendo Achillis. Foot Ankle Clin. 2007;12(4):583-596, vi. doi: 10.1016/j.fcl.2007.07.007 [DOI] [PubMed] [Google Scholar]
- 28. Maffulli N, Del Buono A, Spiezia F, Maffulli GD, Longo UG, Denaro V. Less-invasive semitendinosus tendon graft augmentation for the reconstruction of chronic tears of the Achilles tendon. Am J Sports Med. 2013;41(4):865-871. doi: 10.1177/0363546512473819 [DOI] [PubMed] [Google Scholar]
- 29. Maffulli N, Longo UG, Gougoulias N, Denaro V. Ipsilateral free semitendinosus tendon graft transfer for reconstruction of chronic tears of the Achilles tendon. BMC Musculoskelet Disord. 2008;9:100. doi: 10.1186/1471-2474-9-100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Maffulli N, Loppini M, Longo UG, Maffulli GD, Denaro V. Minimally invasive reconstruction of chronic Achilles tendon ruptures using the ipsilateral free semitendinosus tendon graft and interference screw fixation. Am J Sports Med. 2013;41(5):1100-1107. doi: 10.1177/0363546513479017 [DOI] [PubMed] [Google Scholar]
- 31. Maffulli N, Oliva F, Maffulli GD, Buono AD, Gougoulias N. Surgical management of chronic Achilles tendon ruptures using less invasive techniques. Foot Ankle Surg. 2018;24(2):164-170. doi: 10.1016/j.fas.2017.02.002 [DOI] [PubMed] [Google Scholar]
- 32. Maffulli N, Spiezia F, Longo UG, Denaro V. Less-invasive reconstruction of chronic Achilles tendon ruptures using a peroneus brevis tendon transfer. Am J Sports Med. 2010;38(11):2304-2312. doi: 10.1177/0363546510376619 [DOI] [PubMed] [Google Scholar]
- 33. Maffulli N, Via AG, Oliva F. Chronic Achilles tendon rupture. Open Orthop J. 2017;11:660-669. doi: 10.2174/1874325001711010660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Marx RG, Wilson SM, Swiontkowski MF. Updating the assignment of levels of evidence. J Bone Joint Surg Am. 2015;97(1):1-2. doi: 10.2106/JBJS.N.01112 [DOI] [PubMed] [Google Scholar]
- 35. Ozer H, Ergisi Y, Harput G, Senol MS, Baltaci G. Short-term results of flexor hallucis longus transfer in delayed and neglected Achilles tendon repair. J Foot Ankle Surg. 2018;57(5):1042-1047. doi: 10.1053/j.jfas.2018.03.005 [DOI] [PubMed] [Google Scholar]
- 36. Papandrea P, Vulpiani MC, Ferretti A, Conteduca F. Regeneration of the semitendinosus tendon harvested for anterior cruciate ligament reconstruction. Evaluation using ultrasonography. Am J Sports Med. 2000;28(4):556-561. doi: 10.1177/03635465000280041901 [DOI] [PubMed] [Google Scholar]
- 37. Pendse A, Kankate R. Reconstruction of chronic Achilles tendon ruptures in elderly patients, with vascularized flexor hallucis longus tendon transfer using single incision technique. Acta Orthop Belg. 2019;85(1):137-143. [PubMed] [Google Scholar]
- 38. Reddy SS, Pedowitz DI, Parekh SG, Omar IM, Wapner KL. Surgical treatment for chronic disease and disorders of the Achilles tendon. J Am Acad Orthop Surg. 2009;17(1):3-14. doi: 10.5435/00124635-200901000-00002 [DOI] [PubMed] [Google Scholar]
- 39. Sadoghi P, Rosso C, Valderrabano V, Leithner A, Vavken P. Initial Achilles tendon repair strength—synthesized biomechanical data from 196 cadaver repairs. Int Orthop. 2012;36(9):1947-1951. doi: 10.1007/s00264-012-1533-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Sarzaeem MM, Lemraski MMB, Safdari F. Chronic Achilles tendon rupture reconstruction using a free semitendinosus tendon graft transfer. Knee Surg Sports Traumatol Arthrosc. 2012;20(7):1386-1391. doi: 10.1007/s00167-011-1703-x [DOI] [PubMed] [Google Scholar]
- 41. Schweitzer KM, Dekker TJ, Adams SB. Chronic Achilles ruptures: reconstructive options. J Am Acad Orthop Surg. 2018;26(21):753-763. doi: 10.5435/JAAOS-D-17-00158 [DOI] [PubMed] [Google Scholar]
- 42. Seker A, Kara A, Armagan R, Oc Y, Varol A, Sezer HB. Reconstruction of neglected Achilles tendon ruptures with gastrocnemius flaps: excellent results in long-term follow-up. Arch Orthop Trauma Surg. 2016;136(10):1417-1423. doi: 10.1007/s00402-016-2506-9 [DOI] [PubMed] [Google Scholar]
- 43. Song YJ, Chen G, Jia SH, Xu WB, Hua YH. Good outcomes at mid-term following the reconstruction of chronic Achilles tendon rupture with semitendinosus allograft. Knee Surg Sports Traumatol Arthrosc. 2020;28(5):1619-1624. doi: 10.1007/s00167-018-5113-1 [DOI] [PubMed] [Google Scholar]
- 44. Takao M, Ochi M, Naito K, Uchio Y, Matsusaki M, Oae K. Repair of neglected Achilles tendon rupture using gastrocnemius fascial flaps. Arch Orthop Trauma Surg. 2003;123(9):471-474. doi: 10.1007/s00402-002-0443-2 [DOI] [PubMed] [Google Scholar]
- 45. Tsukada K, Yasui Y, Kubo M, et al. Operative outcome of side-locking loop suture technique accompanied by autologous semitendinosus tendon grafting for chronic rupture of Achilles tendon. Foot Ankle Orthop. 2021;6(2):24730114211003540. doi: 10.1177/24730114211003541 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Vega J, Vilá J, Batista J, Malagelada F, Dalmau-Pastor M. Endoscopic flexor hallucis longus transfer for chronic noninsertional Achilles tendon rupture. Foot Ankle Int. 2018;39(12):1464-1472. doi: 10.1177/1071100718793172 [DOI] [PubMed] [Google Scholar]
- 47. Yasuda T, Shima H, Mori K, Kizawa M, Neo M. Direct repair of chronic Achilles tendon ruptures using scar tissue located between the tendon stumps. J Bone Joint Surg Am. 2016;98(14):1168-1175. doi: 10.2106/JBJS.15.00865 [DOI] [PubMed] [Google Scholar]
- 48. Zou Y, Li X, Wang L, Tan C, Zhu Y. Endoscopically assisted, minimally invasive reconstruction for chronic Achilles tendon rupture with a double-bundle flexor hallucis longus. Orthop J Sports Med. 2021;9(3):2325967120979990. doi: 10.1177/2325967120979990 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-fao-10.1177_24730114231200491 for Surgical Management of Chronic Achilles Tendon Ruptures: A Systematic Review and Proposed Treatment Algorithm by Mohammad T. Azam, James J. Butler, Matthew. B. Weiss, Hugo A. Ubillus, Noah Kirschner, Nathaniel P. Mercer and John G. Kennedy in Foot & Ankle Orthopaedics