Abstract
Background
Macular hole (MH) is a full‐thickness defect in the central portion of the retina that causes loss of central vision. According to the usual definition, a large MH has a diameter greater than 400 µm at the narrowest point. For closure of MH, there is evidence that pars plana vitrectomy (PPV) with internal limiting membrane (ILM) peeling achieves better anatomical outcomes than standard PPV. PPV with ILM peeling is currently the standard of care for MH management; however, the failure rate of this technique is higher for large MHs than for smaller MHs. Some studies have shown that the inverted ILM flap technique is superior to conventional ILM peeling for the management of large MHs.
Objectives
To evaluate the clinical effectiveness and safety of pars plana vitrectomy with the inverted internal limiting membrane flap technique versus pars plana vitrectomy with conventional internal limiting membrane peeling for treating large macular holes, including idiopathic, traumatic, and myopic macular holes.
Search methods
The Cochrane Eyes and Vision Information Specialist searched CENTRAL, MEDLINE, Embase, two other databases, and two trials registries on 12 December 2022.
Selection criteria
We included randomized controlled trials (RCTs) that evaluated PPV with ILM peeling versus PPV with inverted ILM flap for treatment of large MHs (with a basal diameter greater than 400 µm at the narrowest point measured by optical coherence tomography) of any type (idiopathic, traumatic, or myopic).
Data collection and analysis
We used standard methodological procedures expected by Cochrane and assessed the certainty of the body of evidence using GRADE.
Main results
We included four RCTs (285 eyes of 275 participants; range per study 24 to 91 eyes). Most participants were women (63%), and of older age (range of means 59.4 to 66 years). Three RCTs were single‐center trials, and the same surgeon performed all surgeries in two RCTs (the third single‐center RCT did not report the number of surgeons). One RCT was a multicenter trial (three sites), and four surgeons performed all surgeries. Two RCTs took place in India, one in Poland, and one in Mexico. Maximum follow‐up ranged from three months (2 RCTs) to 12 months (1 RCT). No RCTs reported conflicts of interest or disclosed financial support. All four RCTs enrolled people with large idiopathic MHs and compared conventional PPV with ILM peeling versus PPV with inverted ILM flap techniques. Variations in technique across the four RCTs were minimal. There was some heterogeneity in interventions: in two RCTs, all participants underwent combined cataract‐PPV surgery, whereas in one RCT, some participants underwent cataract surgery after PPV (the fourth RCT did not mention cataract surgery). The critical outcomes for this review were mean best‐corrected visual acuity (BCVA) and MH closure rates. All four RCTs provided data for meta‐analyses of both critical outcomes. We assessed the risk of bias for both outcomes using the Cochrane risk of bias tool (RoB 2); there were some concerns for risk of bias associated with lack of masking of outcome assessors and selective reporting of outcomes in all RCTs.
All RCTs reported postoperative BCVA values; only one RCT reported the change in BCVA from baseline. Based on evidence from the four RCTs, it is unclear if the inverted ILM flap technique compared with ILM peeling reduces (improves) postoperative BCVA measured on a logarithm of the minimum angle of resolution (logMAR) chart at one month (mean difference [MD] −0.08 logMAR, 95% confidence interval [CI] −0.20 to 0.05; P = 0.23, I2 = 65%; 4 studies, 254 eyes; very low‐certainty evidence), but it may improve BCVA at three months or more (MD −0.17 logMAR, 95% CI −0.23 to −0.10; P < 0.001, I2 = 0%; 4 studies, 276 eyes; low‐certainty evidence). PPV with an inverted ILM flap compared to PPV with ILM peeling probably increases the proportion of eyes achieving MH closure (risk ratio [RR] 1.10, 95% CI 1.02 to 1.18; P = 0.01, I2 = 0%; 4 studies, 276 eyes; moderate‐certainty evidence) and type 1 MH closure (RR 1.31, 95% CI 1.03 to 1.66; P = 0.03, I² = 69%; 4 studies, 276 eyes; moderate‐certainty evidence). One study reported that none of the 38 participants experienced postoperative retinal detachment.
Authors' conclusions
We found low‐certainty evidence from four small RCTs that PPV with the inverted ILM flap technique is superior to PPV with ILM peeling with respect to BCVA gains at three or more months after surgery. We also found moderate‐certainty evidence that the inverted ILM flap technique achieves more overall and type 1 MH closures. There is a need for high‐quality multicenter RCTs to ascertain whether the inverted ILM flap technique is superior to ILM peeling with regard to anatomical and functional outcomes. Investigators should use the standard logMAR charts when measuring BCVA to facilitate comparison across trials.
Keywords: Female; Humans; Male; Cataract; Multicenter Studies as Topic; Myopia; Myopia/surgery; Retina; Retinal Perforations; Retinal Perforations/surgery; Retrospective Studies; Tomography, Optical Coherence; Visual Acuity; Vitrectomy; Vitrectomy/methods
Plain language summary
Is there a difference between pars plana vitrectomy with internal limiting membrane flap and pars plana vitrectomy with internal limiting membrane peeling for large macular holes?
Key messages
1. Pars plana vitrectomy with internal limiting membrane flap technique compared to pars plana vitrectomy with internal limiting membrane peeling for treating macular holes may result in better vision after three or more months. 2. Pars plana vitrectomy with internal limiting membrane flap technique compared to pars plana vitrectomy with internal limiting membrane peeling for treating macular holes probably results in a higher likelihood of macular hole closure 3. There is a need for high‐quality research in this area to confirm these results and measure other effects of the different surgeries.
What is macular hole?
The macula is a small area in the center of the retina (the light‐sensitive layer of cells lining the back of the eye). A macular hole is a gap that opens in the macula. Macular holes vary in size, and can be idiopathic (occurring spontaneously without a specific underlying disease), traumatic (caused by an injury), and myopic (associated with near‐sightedness).
What is pars plana vitrectomy?
Vitrectomy is removal of the vitreous humor (the gel that naturally fills the eye). It is a crucial step to be able to access the retina. The pars plana is part of the eye that does not touch critical internal eye structures such as the retina. In pars plana vitrectomy (PPV), the eye surgeon inserts the surgical instruments through the pars plana to avoid damaging the retina or adjacent eye structures.
What is internal limiting membrane peeling and internal limiting membrane flap?
The internal limiting membrane (ILM) is the innermost layer of the retina. ILM peeling and the ILM flap technique are used to treat macular holes. Peeling refers to complete removal of the ILM from the retina surrounding the macular hole. The ILM flap technique involves separating a portion of the ILM from the retina and inverting it to cover the macular hole.
What did we want to find out?
We wanted to examine whether PPV with the ILM flap technique was better than PPV with ILM peeling for treating large macular holes.
What did we do?
We searched for studies that evaluated PPV with ILM flap versus PPV with ILM peeling for treatment of large macular holes. We compared and summarized the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sizes.
What did we find?
We found four studies that had treated 285 eyes of 275 people diagnosed with large macular holes. The average age of the people taking part was 59.4 years to 66 years. Two studies were conducted in India, one in Poland, and one in Mexico. No studies reported conflicts of interest or financial support.
PPV with ILM flap compared to PPV with ILM peeling may result in better vision and probably increases the likelihood of macular hole closure.
What are the limitations of the evidence?
In three of the four studies, the people measuring the results of the surgery may have known which treatment each study participant had received, and this knowledge may have influenced their assessments. The studies reported the results at different time points after surgery, which may have affected the assessment of vision. There were some differences in the surgeries across the studies; for example, in two studies, all people had cataract surgery combined with PPV.
How up to date is this evidence?
The evidence is current to December 2022.
Summary of findings
Summary of findings 1. Summary of findings.
| Pars plana vitrectomy with internal limiting membrane flap versus pars plana vitrectomy with conventional internal limiting membrane peeling for large macular hole | |||||||
| Patient or population: people with large macular hole Setting: ophthalmology hospital or clinic Intervention: PPV with ILM flap Comparison: PPV with ILM peeling | |||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of eyes (studies) | Certainty of the evidence (GRADE) | Comments | ||
| Assumed risk (PPV with ILM peeling) | Corresponding risk (PPV with ILM flap) | ||||||
| Mean change in BCVA from baseline | No data were available for this outcome. | — | — | — | — | ||
| Mean postoperative BCVA (lower is better) | After 1 month | From 0.66 logMAR to 0.96 logMAR | The mean BCVA was on average 0.08 logMAR lower (95% CI −0.20 to 0.05) | — | 254 (4) | ⊕⊝⊝⊝ Very lowa,b,c | — |
| After ≥ 3 months | From 0.65 logMAR to 0.86 logMAR | The mean BCVA was on average 0.17 logMAR lower (95% CI −0.23 to ‐0.10) | — | 276 (4) | ⊕⊕⊝⊝ Lowa,b | Measurement time points were 3 months (Manasa 2018; Velez‐Montoya 2018), 6 months (Kannan 2018), and 12 months (Michalewska 2010). | |
|
Overall closure of macular hole at end of follow‐up |
858 per 1000 | 944 per 1000 (range 875 to 1000) |
RR 1.10 (95% CI 1.02 to 1.18) |
276 (4) | ⊕⊕⊕⊝ Moderateb | Measurement time points were 3 months (Manasa 2018; Velez‐Montoya 2018), 6 months (Kannan 2018), and 12 months (Michalewska 2010). | |
| Speed of visual acuity improvement | No data were available for this outcome. | — | — | — | — | ||
|
Type 1 macular hole closure at end of follow‐up |
589 per 1000 | 771 per 1000 (606 to 977) |
RR 1.31 (95% CI 1.03 to 1.66) |
276 (4) | ⊕⊕⊕⊝ Moderateb | Measurement time points were 3 months (Manasa 2018; Velez‐Montoya 2018), 6 months (Kannan 2018), and 12 months (Michalewska 2010). | |
|
Postoperative retinal detachment at end of follow‐up |
See comment | — | — | ⊕⊕⊝⊝ Lowd | Velez‐Montoya 2018 reported no retinal detachment in either surgery group. | ||
| *The risk in the intervention group (and its 95% CI) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). BCVA: best‐corrected visual acuity; CI: confidence interval; ILM: internal limiting membrane; logMAR: logarithm of the minimum angle of resolution; MD: mean difference; OCT: optical coherence tomography; PPV: pars plana vitrectomy; RR: risk ratio. | |||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate; the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited; the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect. | |||||||
aDowngraded one level for indirectness (various time points pooled in the analysis). bDowngraded one level for risk of bias concerns. cDowngraded one level for imprecision (wide CI). dDowngraded two levels for imprecision (no events).
Background
Description of the condition
Macular hole (MH) is a vitreoretinal interface disease of the macula that may lead to significant loss of central vision. It is characterized by a full‐thickness defect of the neurosensorial retina at the macula center (Gass 1988; Gattoussi 2019). Anomalous posterior vitreous detachment and persistent vitreoretinal adherence have been implicated in various vitreoretinal interface abnormalities, including idiopathic MH, which was first described in 1988 by Johnson and Gass (Johnson 1988). The pathogenesis of idiopathic MH involves vitreoretinal interface forces and vitreomacular adhesion during the process of posterior vitreous detachment. The dynamic forces of the vitreous constitute both anteroposterior and tangential vectors on the macular layers, and lead to swelling of the middle and outer retinal layers, with elevation and retraction of the inner macular area (Ezra 2001; Tornambe 2003).
Optical coherence tomography (OCT) has confirmed this association and has shown oblique anteroposterior vitreous traction along with intrafoveal microstructural changes early in the process of MH formation (Takahashi 2011). Although hole progression was initially characterized by observation of fundus changes, the current classification is based on OCT findings (Duker 2013).
MH can also be due to mechanical blunt injury to the eye (traumatic MH) or high myopia (myopic MH). Other secondary causes include foveoschisis, macular telangiectasia type 2, exudative age‐related macular degeneration, and surgical trauma (Duker 2013). Reported MH prevalences range from 0.2/1000 in the Blue Mountains of Australia to 3.3/1000 in the Baltimore Eye Survey (Mitchell 1997; Rahmani 1996). One study conducted in Minnesota (USA) found an MH incidence of 7.8 per 100,000 person‐years (McCannel 2009), and another study based on health care claims data in the USA reported a cumulative incidence of 41.1 per 100,000 person‐years (Ali 2017).
Idiopathic MH accounts for an estimated 85% of all MH cases (Duker 2013). It typically presents unilaterally in the sixth or seventh decade of life and occurs more commonly in myopic eyes (Ali 2017; La Cour 2002). Bilateral presentation occurs in 10% to 15% of cases (Lewis 1996; McCannel 2009; Sen 2008). Idiopathic MH affects more women than men, with a female‐to‐male ratio of 3:1 (range 1.2:1 to 7:1; Ali 2017). Traumatic MH mainly occurs in boys and young men following various types of injuries (Budoff 2019).
Up to 50% of all presenting MHs are large MHs (Duker 2013). Although they are relatively common, large MHs remain a surgical challenge. Unsuccessful surgical closure and late reopening after successful closure are more frequent in large MHs compared with smaller MHs (Ip 2002).
Description of the intervention
The internal limiting membrane (ILM) is an acellular transparent structure that forms the internal boundary of the retina, separating it from the vitreous. The ILM is formed by the footplates of Müller cells and is composed of collagen fibers, glycosaminoglycans, laminin, and fibronectin. It plays a role in the early development of the retina and optic nerve. The ILM can also serve as a scaffold for the proliferation of different cells, including myofibroblasts, fibrocytes, and retinal pigment epithelium cells, which play a role in vitreoretinal interface pathologies (Gelman 2015).
ILM peeling is a surgical technique commonly used to treat various vitreoretinal disorders, including: vitreoretinal interface diseases such as vitreomacular traction, MHs, and epiretinal membranes; macular edema in diabetes and retinal vein occlusion; myopic macular retinoschisis; and retinal detachment (Walia 2014).
ILM removal is preceded by a standard pars plana vitrectomy (PPV). After detachment and removal of the posterior hyaloid, the ILM is typically stained with brilliant blue G (BBG), trypan blue, indocyanine green (ICG), or triamcinolone acetonide, then peeled (Almony 2012). The first step of the peeling process is to create an initial flap of ILM using a sharp instrument (e.g. pick forceps, a bent microvitreoretinal (MVR) blade, or specifically designed vitreoretinal forceps). The flap is then held by forceps and the ILM is peeled, usually in capsulorhexis‐like (circular) fashion (Almony 2012). One Cochrane Review assessed the efficacy of PPV with ILM peeling versus without, and concluded that the ILM peeling group achieved superior rates of MH closure. There was no difference between the groups in visual acuity improvement at six months, but there was a significant improvement at three months in the peeling group, and most people in the no‐peel group had another intervention with ILM peeling (Cornish 2014).
In addition to ILM peeling, the inverted ILM flap technique may be an effective surgical technique for treating large full‐thickness MHs. ILM flap surgery was first described in Michalewska and colleagues, who found that it achieved a better anatomical closure rate (98%) than traditional ILM peeling (88%) for treatment of large idiopathic MHs (diameter exceeding 400 µm) in their randomized controlled trial (Michalewska 2010).
The PPV and ILM staining steps are similar in both procedures. In the flap procedure, the ILM is grasped with special forceps and partially peeled off in a similar circular fashion. The ILM is not detached completely from the retina, but is left attached at the edges of the MH. A peripheral piece of ILM is trimmed with a vitreous cutter or scissors, and the central part of the ILM is left in place. Then, the remnant ILM is gently massaged over the MH from all sides. At this stage, the ILM is inverted, so that the surface normally facing the vitreous body now faces the retinal pigmented epithelium. Once the surgeon has confirmed that the inverted ILM flap is covering the MH, they proceed with fluid‐air exchange (Michalewska 2010).
A modification of the flap technique described in Michalewska 2015 requires peeling only the macular temporal ILM, which is left hinged at the temporal edge of the MH.
How the intervention might work
ILM peeling aims to release the anteroposterior and tangential traction forces exerted on the retina by removing cortical vitreous, residual epiretinal membranes, and ILM. It is also proposed that ILM peeling can induce glial cell proliferation into the MH, thereby enhancing the chances of closure, and leading to improvement of postoperative visual acuity (Almony 2012; Chatziralli 2018).
The inverted ILM flap may further improve outcomes by serving as a scaffold for further glial cell proliferation. One study of an experimental MH model in monkeys treated by the inverted ILM flap showed that ILM flaps produced neurotrophic factors that promote gliosis (Shiode 2017).
Why it is important to do this review
Since the early 2010s, retina surgeons have introduced several new techniques for managing large and refractory MHs. Although conventional MH surgery is usually successful for treating small holes, there is no standard of care for larger holes. There is also debate in the retina community regarding the role of ILM flaps for MH repair. In this review, we used the available evidence to provide a comprehensive comparison of the two most common ILM removal techniques with the aim of guiding clinicians on appropriate surgical management of large MHs.
Objectives
To evaluate the clinical effectiveness and safety of pars plana vitrectomy with the inverted internal limiting membrane flap technique versus pars plana vitrectomy with conventional internal limiting membrane peeling for treating large macular holes, including idiopathic, traumatic, and myopic macular holes.
Methods
Criteria for considering studies for this review
Types of studies
We included only randomized controlled trials (RCTs) in this review. We included all eligible studies irrespective of their publication status.
Types of participants
We included RCTs that enrolled people with large MH (basal diameter greater than 400 µm at the narrowest point, measured by OCT). No eligibility criteria were based on lens status.
Types of interventions
We included RCTs that directly compared ILM peeling with inverted ILM flap following PPV for any type of large MH, including idiopathic, traumatic, and myopic MH.
Types of outcome measures
Reporting of our outcomes of interest was not an inclusion criterion for this review. We included RCTs with a minimal postoperative follow‐up of three months to examine long‐term effects.
Critical outcomes
Best‐corrected visual acuity (BCVA): mean absolute BCVA value or change from baseline, measured on a logarithm of the minimum angle of resolution (logMAR) chart (or equivalent when measured on a decimal or Snellen chart) at one month and three or more months postoperatively. We reported the absolute and change values separately.
Overall closure of MH: proportion of eyes achieving closure of MH, as defined by OCT, at the longest follow‐up time point of each study. We considered both type 1 (closure with no foveal neurosensory defect) and type 2 (closure with foveal neurosensory defect) as successful closure.
Important outcomes
Speed of visual acuity improvement: proportion of eyes achieving the final BCVA (BCVA measured on logMAR chart [or equivalent on decimal or Snellen chart] at longest follow‐up) at one month and three or more months postsurgery (whenever reported before the end of the study). We did not adopt a cut‐off for BCVA, as we aimed to compare how quickly the eyes had achieved their final visual acuity between groups.
Type 1 MH closure: proportion of eyes achieving type 1 MH closure at the longest follow‐up time point of each study.
Postoperative retinal detachment: proportion of eyes with retinal detachment by the longest follow‐up time point of each study. We focused on retinal detachment as the surgical techniques and other adverse events are expected to be similar. We also planned to collect any adverse events reported in the included studies, but no studies reported any other complications or adverse events.
Search methods for identification of studies
Electronic searches
The Cochrane Eyes and Vision Information Specialist consulted with the review authors to develop relevant terms, then searched the following electronic databases for RCTs and controlled clinical trials, applying no restrictions to language or date of publication.
Cochrane Central Register of Controlled Trials (CENTRAL, which contains the Cochrane Eyes and Vision Trials Register; 2022, Issue 12) in the Cochrane Library (searched 12 December 2022; Appendix 1)
MEDLINE Ovid (1946 to 12 December 2022; Appendix 2)
Embase.com (1947 to 12 December 2022; Appendix 3)
PubMed (1948 to 12 December 2022; Appendix 4)
LILACS (Latin American and Caribbean Health Science Information database; 1982 to 12 December 2022; Appendix 5)
US National Institutes of Health Ongoing Trials Register ClinicalTrials.gov (www.clinicaltrials.gov; searched 12 December 2022; Appendix 6)
World Health Organization (WHO) International Clinical Trials Registry Platform (ICTRP; www.who.int/ictrp; searched 12 December 2022; Appendix 7).
Searching other resources
We also searched the reference lists of the studies included in the review for other potential studies. We used Science Citation Index to find studies that had cited the included trials. We did not handsearch conference proceedings or journals specifically for the review.
Data collection and analysis
Selection of studies
Two review authors independently screened the titles and abstracts of the records returned by the searches, categorizing them as 'yes', 'no', or 'maybe'. We obtained the full‐text articles of records labeled 'yes' or 'maybe', and two review authors independently reviewed them to make a final judgment regarding their eligibility. At each stage of the selection process, we resolved any disagreements by discussion or by consulting a third review author where necessary. Review authors were not masked to study authors, institutions, or journals; we corresponded with authors of reports to clarify study eligibility, as appropriate.
In the Characteristics of excluded studies table, we listed all studies excluded at the full‐text review stage and provided a brief justification for their exclusion.
For potentially eligible studies identified from trial registers, we adopted the following approach.
If the study completion date was before December 2019, we searched for all study publications and contacted the investigators to obtain any additional published or unpublished data. We included eligible studies in the review, regardless of whether we could identify a publication.
If the study completion date was in or after December 2019, we documented the study in the Characteristics of ongoing studies table.
Data extraction and management
Two review authors independently extracted data from the studies using an online form developed by Cochrane Eyes and Vision (Covidence 2021). We resolved any discrepancies by discussion. We contacted study authors to request missing outcome data. All data were imported directly into Review Manager Web (RevMan Web; RevMan Web 2020), and one review author checked the accuracy of the data import.
Outcome data
We extracted the following data from each included study for intervention and comparator groups separately.
For the continuous variable (BCVA): mean, standard deviation (SD), and number of participants with outcome data
For dichotomous variables (overall closure of MH, proportion of eyes achieving the final BCVA at different time points, type 1 MH closure, and proportion of eyes with postoperative retinal detachment): number of events and number of eyes with outcome data
For multiarm studies, we extracted only data relevant to our intervention and comparator groups. Whenever two or more study arms per group (intervention or comparator) contributed relevant data, we combined arms using the calculator function in RevMan Web (RevMan Web 2020).
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias of each included study using Cochrane's Risk of Bias tool (RoB 2; Sterne 2019). We applied RoB 2 to assess the two critical outcomes (BCVA and overall closure of MH). We resolved any disagreements by discussion.
RoB 2 covers the following domains.
Bias arising from the randomization process (random sequence generation, allocation concealment): was the sequence of allocation generated using a random procedure, and was the allocation concealed to people recruiting and enrolling participants, and to participants?
Bias introduced by deviations from intended interventions (masking of participants and researchers): were the recipients of care unaware of their assigned intervention? Were the persons providing care unaware of the assigned intervention? Were there any patients who received non‐protocol intervention? Was the analysis appropriate?
Bias in outcome measurement (masking outcome assessors): were persons evaluating outcomes unaware of the assigned intervention?
Bias due to missing outcome data: were the rates of follow‐up and compliance similar in the groups compared? Was the analysis by intention‐to‐treat, and were there any post randomization exclusions?
Bias in selective reporting of outcome data: is there any evidence that some outcomes that were measured were not reported?
We classified each domain as 'low risk of bias', 'high risk of bias' or 'some concerns' (insufficient information or uncertainty of potential for bias). We contacted study authors for clarification of domains with 'some concerns'.
Measures of treatment effect
We calculated the risk ratio (RR) for dichotomous outcomes and the mean difference (MD) for continuous outcomes, with the corresponding 95% confidence interval (CI) for each effect measure. Where possible, we checked for the skewness of continuous data (Altman 1996).
Unit of analysis issues
We expected the included trials would randomize participants, who would each have surgery in one eye. However, one study included 15 (17.4%) bilateral participants (Michalewska 2010). The study authors randomized participants but used the eye as the unit of analysis without considering intrapersonal correlation. We used the data as reported. This approach was conservative, as CIs were wider than they would have been if the potential within‐person correlation was accounted for.
Dealing with missing data
Whenever relevant data were missing from publications or registers, particularly for the critical outcomes, we contacted the study authors to request the missing information. If we did not hear from study authors within two weeks, we proceeded to analyze the available data.
Assessment of heterogeneity
We examined the study characteristics, in particular the type of participants and types of interventions, to decide whether the studies were sufficiently similar to meaningfully combine their outcome data in meta‐analyses.
We examined the forest plots of the effect estimates for consistency across studies, considering the size and direction of effects and the overlap of CIs.
We tested for the presence of statistical heterogeneity with the Chi2 test, considering a P value below 0.1 indicative of significant heterogeneity (Deeks 2021). We calculated the I2 statistic to quantify the percentage of the variability in effect estimates of individual outcomes that was due to heterogeneity rather than sampling error (Higgins 2002), considering I2 values greater than 50% and up to 90% indicative of substantial heterogeneity.
Assessment of reporting biases
Had we included 10 or more trials in a meta‐analysis, we would have constructed funnel plots and tested for asymmetry to assess small study effects, which could be due to publication bias.
Data synthesis
When the I2 value was greater than 75%, or if there was significant clinical heterogeneity, we did not conduct a meta‐analysis. Instead, we presented a tabulated or narrative summary, or both. When the I2 value was less than 75%, and there was no clinical heterogeneity, we combined the effect estimates in a meta‐analysis using a random‐effects model (provided three or more trials contributed data to the outcome). We planned to use a fixed‐effect model for meta‐analyses with fewer than three studies to avoid reporting less robust effect estimates that may result from random‐effects models in situations with very few trials. When the I2 value was greater than 75% but effect estimates were in the same direction, we performed a meta‐analysis of the outcome, but stressed the need for caution in interpreting the results.
Subgroup analysis and investigation of heterogeneity
If there had been a sufficient number of trials with outcome data reported by subgroup (more than 10), we would have compared the effects of treatment in the following subgroups for the two critical outcomes.
-
Etiology
Idiopathic MHs
Traumatic MHs
Myopic MHs
-
Chronicity
Recent MHs (duration of less than six months)
Chronic MHs (duration of six months or more)
Sensitivity analysis
We did not perform a sensitivity analysis based on exclusion of studies at high risk of bias as planned in the protocol. However, we performed a sensitivity analysis for BCVA at three months or more by excluding one study that involved cataract surgery in some participants during the follow‐up period.
Summary of findings and assessment of the certainty of the evidence
We prepared a summary of findings table to present estimated relative and absolute risks. Two review authors independently graded the overall certainty of the evidence for each outcome using the GRADE approach (GRADE 2013). We included the following outcomes in the summary of findings table.
BCVA at one month and three or more months after surgery
Overall closure of MH at the end of follow‐up
Speed of visual acuity improvement
Type 1 MH closure at the end of follow‐up
Postoperative retinal detachment at the end of follow‐up
We applied study‐level risk of bias results for other outcomes that we had not assessed with RoB 2.
Results
Description of studies
Results of the search
We performed the initial database search on 23 November 2021, and then a top‐up search on 12 December 2022. Overall, database searching yielded 3717 records, and the search of clinical trial registries yielded 644 records (Figure 1). After removal of 1331 duplicates, we screened the remaining 3030 records and excluded a further 3001 records based on information in the title and abstract. We obtained the full‐text reports of 29 records (26 studies) for further investigation. We included six reports of four studies (Kannan 2018; Manasa 2018; Michalewska 2010; Velez‐Montoya 2018) and excluded 20 reports of 19 studies (see Characteristics of excluded studies table). There were three potentially eligible ongoing studies; we will assess them when data become available (CTRI/2017/03/008001; CTRI/2017/05/008663; NCT04698226).
1.
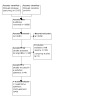
Figure 1: Study flow diagram.
Included studies
Study design
We included four RCTs. Three RCTs were single‐center trials (Kannan 2018; Manasa 2018; Michalewska 2010), and one was conducted at three sites (Velez‐Montoya 2018). Participants were recruited in India (Kannan 2018; Manasa 2018), Poland (Michalewska 2010), and Mexico (Velez‐Montoya 2018). The planned length of follow‐up ranged from three to 12 months. No RCTs reported any conflicts of interest or financial support.
Participants
The four RCTs enrolled 275 participants (285 eyes; range per study 24 to 91 eyes). Most participants were women (172/275; 63%) and of older age (range of mean ages 59.4 years to 66 years). All four RCTs enrolled people with large idiopathic MHs. Mean BCVA was comparable between the ILM flap and ILM peeling groups at baseline, ranging from 0.75 logMAR to 1.1 logMAR in the ILM flap group and from 0.79 logMAR to 1.1 logMAR in the ILM peeling group across the trials. The RCTs varied in terms of minimum MH diameter at baseline. Two RCTs included only eyes with a minimum hole diameter greater than 600 μm (Kannan 2018; Manasa 2018), while the other two included eyes with a minimum hole diameter greater than 400 μm (Michalewska 2010; Velez‐Montoya 2018). Kannan 2018 excluded eyes with a minimum hole diameter greater than 1500 μm. All four RCTs excluded people with co‐existing ocular conditions.
Interventions
All four RCTs compared PPV and inverted ILM flap with conventional PPV and ILM peeling. The same surgeon performed all surgeries in two RCTs (Kannan 2018; Michalewska 2010), four surgeons performed the surgeries in the multicenter RCT (Velez‐Montoya 2018), and Manasa 2018 did not report the number of surgeons. Kannan 2018 reported that the surgeon tucked the inverted ILM flap inside the hole, while the other three only described covering the hole with the inverted flap, with no mention of tucking (Manasa 2018; Michalewska 2010; Velez‐Montoya 2018). All RCTs reported ILM staining: Michalewska 2010 used trypan blue stain, while the remaining RCTs used brilliant blue stain. Michalewska 2010 reported only using air as a postoperative tamponade, and the other three RCTs reported using gas tamponade (SF6 or C3F8) at different concentrations. Velez‐Montoya 2018 included a third study arm (free ILM flap), which we did not include in this review. Two RCTs performed cataract removal with implantation of intraocular lens in addition to PPV and ILM techniques in all study participants (Kannan 2018; Velez‐Montoya 2018). Michalewska 2010 reported that six eyes (two in the ILM peeling group and four in the inverted ILM flap group) were already pseudophakic prior to the MH surgery, and did not report any cataract surgery. Michalewska 2010 reported that nine eyes (six in the ILM peeling group and three in the inverted ILM flap group) required phacoemulsification four to 11 months after surgery.
Outcomes
All four RCTs reported our critical outcomes (BCVA and overall closure of MH). Three RCTs reported BCVA at one month, and all four RCT reported BCVA at three or more months. We contacted the authors of the study that had not reported BCVA at one month, and they provided this information (Michalewska 2010). The maximum follow‐up period was three months in Manasa 2018 and Velez‐Montoya 2018, six months in Kannan 2018, and 12 months in Michalewska 2010. Only Kannan 2018 reported change in BCVA from baseline. All four RCTs reported overall rates of MH closure and types of MH closure, but no studies reported the proportion of eyes that achieved final visual acuity. Only Velez‐Montoya 2018 reported the rate of postoperative retinal detachment.
Excluded studies
We excluded 19 studies at full‐text review stage (see Characteristics of excluded studies table). Eight excluded studies had an ineligible study design, one recruited an ineligible patient population, seven examined ineligible interventions, and three examined ineligible comparators.
Risk of bias in included studies
Domain 1: bias arising from the randomization process
Best‐corrected visual acuity, overall closure of macular hole
For both outcomes, we considered three RCTs at low risk of bias as they utilized simple randomization, pulling a ball from a box, or computer‐generated random number tables/envelope techniques for randomization (all acceptable methods), and reported that each allocation was concealed before it was assigned to a participant (Manasa 2018; Michalewska 2010; Velez‐Montoya 2018). However, we had some risk of bias concerns for Kannan 2018 because it did not report the method of allocation concealment.
Domain 2: bias arising from deviations from intended interventions
Best‐corrected visual acuity, overall closure of macular hole
For both outcomes, we judged all four RCTs at low risk of bias in terms of deviation from the intended intervention. Although only Kannan 2018 clearly stated masking of the study participants, lack of masking is unlikely to have caused any deviations. All participants underwent surgical intervention. Surgeons were informed of the assigned technique after randomization and could not be masked thereafter.
Domain 3: bias due to missing outcome data
Best‐corrected visual acuity, overall closure of macular hole
For both outcomes, we considered all four RCTs at low risk of bias regarding missing outcome data. Three RCTs did not mention any missed outcomes or loss to follow‐up (Michalewska 2010; Kannan 2018; Velez‐Montoya 2018). In Manasa 2018, 91/100 (91%) randomized participants were included in the analysis.
Domain 4: bias in outcome measurement
Best‐corrected visual acuity
There were some risk of bias concerns regarding measurement of this outcome for two RCTS because they did not report masking of BCVA assessors (Kannan 2018; Manasa 2018). We judged the other two RCTs at low risk of bias because they reported masking of BCVA assessors (Michalewska 2010; Velez‐Montoya 2018). All RCTs provided sufficient information on the method of BCVA measurements to judge their acceptability.
Overall closure of macular hole
There were some risk of bias concerns regarding measurement of this outcome for three RCTs because they did not report masking of personnel who assessed MH closure (Kannan 2018; Manasa 2018; Michalewska 2010). We judged only Velez‐Montoya 2018 at low risk because it described masking of outcome assessors. All RCTs provided sufficient information on the method of MH closure assessment.
Domain 5: bias in selective reporting of outcome data
Best‐corrected visual acuity
There were some risk of bias concerns regarding selective reporting of BCVA for all four RCTs. Only Kannan 2018 reported improvement in BCVA as an outcome measure. However, BCVA measurements had been made on a Snellen chart and converted to logMAR values, then reported in lines (which could refer to either measurement scale). The other three RCTs did not report BCVA change from baseline; they reported only mean values of measurements at baseline and during follow‐up. Furthermore, Michalewska 2010 reported having measured BCVA at one month, but did not publish the one‐month means. The study authors provided us with these data on request.
Overall closure of macular hole
We considered all four RCTs at low risk of bias regarding completeness of reporting of MH closure rates, as all analyzed and reported the outcome.
Overall assessment of bias
Best‐corrected visual acuity
There were some overall risk of bias concerns for this outcome in all four RCTs, due to lack of masking of outcome assessors and selective reporting of BCVA outcomes in three RCTs (Michalewska 2010; Kannan 2018; Manasa 2018), and due to selective reporting of BCVA measurements in Velez‐Montoya 2018.
Overall closure of macular hole
There were some overall risk of bias concerns for this outcome in three RCTs, mostly due to unclear masking of outcome assessors (Kannan 2018; Manasa 2018; Michalewska 2010). We judged Velez‐Montoya 2018 at low overall risk of bias for this outcome.
Effects of interventions
See: Table 1
See Table 1.
Critical outcomes
Change in best‐corrected visual acuity from baseline
No data were available for this outcome. Kannan 2018 reported change in BCVA from baseline but did not specify a time point. Furthermore, we could not interpret the data because measurements had been made on a Snellen chart and converted to logMAR values, then reported as lines, which could refer to either Snellen lines or lines on standard logMAR charts. The report stated that the difference in change in BCVA from baseline was not statistically significant (1.4 lines for the peeling group versus 2.1 lines for the inverted flap group, P = 0.353). No other RCTs reported change in BCVA from baseline.
Mean best‐corrected visual acuity at one month
No trial reported any statistically or clinically significant difference between groups for baseline BCVA. Three RCTs reported BCVA at 1 month (Kannan 2018; Manasa 2018; Velez‐Montoya 2018), and the authors of Michalewska 2010 provided us with mean one‐month BCVA values for both groups. All four RCTs reported these results after the primary surgery. Meta‐analysis of data from 254 eyes provided very uncertain evidence of the effect of PPV with inverted ILM flap compared to PPV with ILM peeling on mean BCVA at one month (MD −0.08 logMAR, 95% CI −0.20 to 0.05, lower is better; P = 0.23, I2 = 65%; 4 studies; Analysis 1.1, Figure 2). The estimated difference in BCVA (four letters on a logMAR chart) was not clinically relevant. We combined effect estimates in a meta‐analysis despite some heterogeneity (I2 = 65%), as we found no baseline or interventional differences that could explain the heterogeneity. We judged the certainty of evidence for this outcome as very low, downgrading by one level for risk of bias concerns (masking of outcome assessors and selective reporting), one level for inconsistency of effect estimates, and one level for imprecision (wide CI crossing the null value).
1.1. Analysis.

Comparison 1: Pars plana vitrectomy (PPV) with internal limiting membrane (ILM) inverted flap versus PPV with ILM peeling, Outcome 1: Mean logMAR best‐corrected visual acuity (one month)
2.

Figure 2: Forest plot of Analysis 1.1: Mean LogMAR best‐corrected visual acuity (one month).
Mean best‐corrected visual acuity at three or more months
All four trials reported mean BCVA at three or more months: two RCTs reported mean BCVA at three months (Manasa 2018; Velez‐Montoya 2018), one RCT reported mean BCVA at six months (Kannan 2018), and one RCT reported mean BCVA at one year (Michalewska 2010). Meta‐analysis of data from 276 eyes showed that PPV with inverted ILM flap compared to PPV with ILM peeling may reduce (improve) mean logMAR BCVA at three or more months after surgery (MD −0.17 logMAR, 95% CI −0.23 to −0.10; P < 0.001, I2 = 0%; 4 studies; Analysis 1.2, Figure 3). Three RCTs reported the results after the primary surgery. In Michalewska 2010, nine participants underwent cataract surgery four to 11 months after the primary surgery. Therefore, we performed a sensitivity analysis by removing this study, and the result still favored the intervention (MD −0.15 logMAR, 95% CI −0.22 to ‐0.07). We graded the certainty of evidence for this outcome as low, downgrading one level for indirectness (outcomes measured at different time points pooled in the same analysis) and one level for risk of bias concerns (masking of outcome assessors and selective outcome reporting). The test for subgroup differences suggested no differential effects according to time point of outcome measurement from three months to one year postsurgery (P = 0.52; Analysis 1.2, Figure 3).
1.2. Analysis.

Comparison 1: Pars plana vitrectomy (PPV) with internal limiting membrane (ILM) inverted flap versus PPV with ILM peeling, Outcome 2: Mean logMAR best‐corrected visual acuity (three months or more)
3.

Figure 3: Forest plot for Analysis 1.2: Mean LogMAR best‐corrected visual acuity (three or more months).
Overall closure of macular hole
All four RCTs reported the proportions of MH closure in both groups at the end of follow‐up (three months to one year). Meta‐analysis of data from 276 eyes suggested that PPV with inverted ILM flap compared to PPV with ILM peeling probably increases the proportion of MH closure (RR 1.10, 95% CI 1.02 to 1.18; P = 0.01, I2 = 0%; 4 studies; Analysis 1.3; Figure 4). However, the 95% CIs of all four individual effect estimates included 1.0, consistent with no difference in outcome. The certainty of the evidence was moderate; we downgraded one level for risk of bias concerns related to masking of outcome assessors. Although there is some indirectness due to different lengths of follow‐up periods among the studies, it is unlikely to have affected the direction of effect estimates. In addition, external evidence suggests a minimal risk of change in MH surgery anatomical results across different time points after three months (Christmas 1998).
1.3. Analysis.

Comparison 1: Pars plana vitrectomy (PPV) with internal limiting membrane (ILM) inverted flap versus PPV with ILM peeling, Outcome 3: Proportion of eyes achieving closure of macular hole
4.

Figure 4: Forest plot for Analysis 1.3: Proportion of participants achieving closure of macular hole.
Important outcomes
Speed of visual acuity improvement
No RCTs reported the proportion of eyes achieving the final BCVA at one month or at three or more months.
Type 1 macular hole closure
All four RCTs reported the proportion of eyes achieving type 1 MH closure by three or more months. Meta‐analysis of data from 276 eyes showed that PPV with inverted ILM flap compared to PPV with ILM peeling probably increases type 1 closures (RR 1.31, 95% CI 1.03 to 1.66; P = 0.03, I² = 69%; 4 studies; Analysis 1.4, Figure 5). All four RCTs reported the results after the primary surgery. Velez‐Montoya 2018 reported an outlying estimate of type 1 closure. That trial enrolled the fewest participants but was given significant weight in the analysis (27.4%; Figure 5). When we removed Velez‐Montoya 2018 from the meta‐analysis, heterogeneity was reduced and the effect estimate was larger (RR 1.41, 95% CI 1.19 to 1.67; P < 0.001, I² = 15%; 3 studies). The certainty of the evidence was moderate; we downgraded one level for risk of bias concerns related to masking of outcome assessors.
1.4. Analysis.

Comparison 1: Pars plana vitrectomy (PPV) with internal limiting membrane (ILM) inverted flap versus PPV with ILM peeling, Outcome 4: Proportion of eyes achieving type 1 macular hole closure
5.

Figure 5: Forest plot for Analysis 1.4: Proportion of participants achieving type 1 macular hole closure.
Postoperative retinal detachment
Only Velez‐Montoya 2018 reported rates of postoperative retinal detachments: none in either surgery group. The certainty of the evidence for this outcome was low; we downgraded two levels for imprecision of results (no events).
No studies reported any other complications or adverse events.
Discussion
Summary of main results
We identified four completed RCTs that had evaluated PPV with inverted ILM flap versus PPV with conventional ILM peeling for treatment of large MH. After reviewing the available evidence, we summarized our findings in Table 1.
There was some variability among the studies with respect to inclusion criteria (minimal MH diameter), length of follow‐up, and interventions (ILM manipulation, combined phacovitrectomy, use of tamponade); otherwise, the four RCTs were similar in design.
There was low‐certainty evidence that the ILM flap procedure compared to ILM peeling reduced (improved) mean logMAR BCVA at three months or more postoperatively. We found moderate‐certainty evidence that the inverted ILM flap technique achieved higher rates of any closure and of type 1 closure (which accounted for most successful closures) compared to ILM peeling.
Overall completeness and applicability of evidence
There were no significant differences in baseline or inclusion/exclusion criteria across the four RCTs. Interventions varied among the RCTs, with refinements such as tucking of ILM inside the MH, type of ILM stain, intraocular tamponade, and combined phacovitrectomy versus vitrectomy.
We could not explore the effect of ILM tucking inside the MH, as only one RCT described this technique, with no available direct comparison with the inverted ILM flap without tucking. The potential effect of the inverted ILM flap technique variation is unknown. Concurrent or subsequent cataract surgery is often necessary in people undergoing MH surgery because cataract develops in many eyes following vitrectomy. Notably, Michalewska 2010 reported final BCVA at 12 months' follow‐up, after a minority of participants had undergone phacovitrectomy/subsequent cataract surgery, which raises concerns regarding the effect of postvitrectomy cataract on final BCVA in the remaining participants (Petermeier 2010). Overall, variation in phacovitrectomy/subsequent cataract surgery between the RCTs may have some effects, but the number of participants who had undergone these additional procedures was similar in the two intervention groups, so we judged the effect of this variation on BCVA difference to be minimal. Cataract surgery is not expected to affect MH closure rates (Valmaggia 2021).
The included RCTs addressed functional improvement (BCVA) and anatomical improvement (MH closure), but did not include other objective functional outcomes such as multifocal electroretinogram (except Manasa 2018) or microperimetry. Investigating these outcomes would have provided strong evidence of functional improvement.
Only one RCT reported masking of the outcome assessors; absence of masked outcome assessment was a possible source of bias in the remaining three RCTs. In addition, no RCTs used an independent reading center to evaluate and standardize the assessment of MH closure based on OCT; this is a possible source of heterogeneity within and between the RCTs due to the lack of standard and independent methods of interpreting OCT images.
Another limitation is the small size of the trials: Velez‐Montoya 2018 enrolled only 12 participants in each group, finding similar rates of MH closure. Although there was some heterogeneity among the RCTs regarding mean BCVA at one month and proportions of MH closure types, we conducted meta‐analyses nonetheless, as we identified no significant participant baseline differences among the studies. However, readers should take heterogeneity into account when interpreting the results of our review.
No RCTs included traumatic or myopic MHs, which limits the applicability of our findings to idiopathic MHs.
Quality of the evidence
The certainty of the evidence was very low to moderate. The main reasons for downgrading were indirectness (pooling of results reported at various time points), risk of bias (masking and selective reporting), and imprecision (wide CI including no effect in one RCT, no events in one RCT).
One major limitation in this review is that three out of four RCTs used Snellen rather than a standardized logMAR chart.
Potential biases in the review process
We made a concerted effort to identify and include all the eligible trials in the review by applying a broad search strategy, applying no publication date or language restrictions, and considering not only studies with published outcome data, but also those underway or nearing publication. Nevertheless, we found only four trials eligible for inclusion. We followed the standard Cochrane Review methodology to minimize bias and checked Methodological Expectations of Cochrane Intervention Reviews (MECIR) standards for the reporting of new Cochrane Intervention Reviews. None of the authors has any financial conflicts of interest.
Agreements and disagreements with other studies or reviews
One published meta‐analysis included the same RCTs as this review (Chen 2020). It reported better results for the inverted ILM flap technique in terms of anatomic success (odds ratio (OR) 4.89, 95% CI 2.09 to 11.47; P < 0.001), type 1 closure rate (OR 5.23, 95% CI 2.83 to 9.66; P < 0.00001), postoperative BCVA (weighted mean difference (WMD) 0.17 logMAR, 95% CI 0.11 to 0.24, higher is better; P < 0.001) and mean change of BCVA from baseline (WMD 0.08 logMAR, 95% CI 0.01 to 0.16, higher is better; P = 0.03). Overall, the results are similar to ours, except we also examined BCVA difference after one month of follow‐up, finding very uncertain evidence of little or no effect. In addition, we employed a random‐effects model rather than a fixed‐effect model, we calculated RRs rather than ORs for dichotomous outcomes, and we considered the effect of reporting BCVA at different time points. Chen 2020 calculated the change in BCVA from baseline in three of four RCTs; we did not do this owing to potential errors.
Another meta‐analysis including five RCTs reported a significantly higher overall MH closure rate (OR 3.10, 95% CI 1.25 to 7.66; P = 0.01) and better postoperative BCVA (WMD −0.14 logMAR, 95% CI −0.21 to −0.07, lower is better; P < 0.001) in the inverted ILM flap group compared to the ILM peeling group (Yu 2021). Interestingly, the subgroup meta‐analysis demonstrated better postoperative visual acuity in the inverted ILM flap group at three months (WMD −0.17 logMAR, 95% CI −0.26 to −0.08, lower is better; P < 0.001) but no clear difference at six months (WMD −0.09 logMAR, 95% CI −0.20 to 0.02, lower is better; P = 0.10). Yu 2021 included the same four RCTs as our review in addition to an RCT that evaluated the inverted ILM flap technique versus ILM peeling and subretinal macular fluid aspiration (Iovino 2018); that RCT did not meet our eligibility criteria.
A third meta‐analysis evaluated idiopathic large MHs (two RCTs and two retrospective studies) in their subgroup analysis with at least six months of follow‐up and reported higher closure rates (RR 1.12, 95% CI 1.05 to 1.20; P < 0.001; 362 eyes), but no clear difference in BCVA improvement (MD −0.16 logMAR, 95% CI −0.36 to 0.05, lower is better; P = 0.13) with the inverted ILM flap technique (Marques 2020).
Shen 2020 (four RCTs and four retrospective studies) also showed that the inverted ILM flap technique compared to ILM peeling significantly improved the rate of MH closure (OR 3.95, 95% CI 1.89 to 8.27; P < 0.001) and postoperative visual acuity at three months (MD − 0.16 logMAR, 95% CI − 0.23 to 0.09, lower is better; P < 0.001). However, there was no difference in visual outcomes between the two groups at six months' follow‐up (MD 0.01 logMAR, 95% CI − 0.12 to 0.15; lower is better; P = 0.86), which was consistent with Yu 2021 and Marques 2020. The most important limitation of Marques 2020 and Shen 2020 was the inclusion of retrospective studies in their analysis.
Gu 2018 conducted a single‐arm meta‐analysis for the inverted ILM flap technique in large MHs (161 participants) and reported a pooled MH closure rate of 95% (95% CI 88% to 98%) and a visual acuity improvement rate of 75% (95% CI 62% to 85%). They then pooled the results of four selected reference RCTs on large MHs treated with ICG‐assisted ILM peeling, finding an MH closure rate of 87% (95% CI 79 % to 92%) and a visual acuity improvement rate of 57% (95% CI 46% to 68%). However, the initial analysis included seven case series and only one RCT (Michalewska 2010).
Authors' conclusions
Implications for practice.
We found low‐certainty evidence that the inverted internal limiting membrane (ILM) flap technique compared to ILM peeling for treatment of large macular holes (MHs) improves best‐corrected visual acuity (BCVA) at three or more months after surgery. We downgraded the certainty of the evidence due to concerns associated with unclear masking of outcome assessors, selective reporting of outcomes, and indirectness. We also found moderate‐certainty evidence that the inverted ILM flap technique results in higher overall and type 1 MH closure rates. We downgraded the certainty of the evidence due to some concerns associated with unclear masking of outcome assessors.
Although the inverted ILM flap technique for large MH led to improved anatomical and visual outcomes compared to ILM peeling without a flap, the certainty of evidence was moderate to low. Therefore, further studies are needed to clarify which surgical method provides meaningful improvements.
Implications for research.
High‐quality, multicenter randomized clinical trials are required to ascertain whether the inverted ILM flap technique is superior to ILM peeling in terms of anatomical and functional outcomes, and to provide more precise estimates of the effects on BCVA. Future trials should include participant‐reported outcomes and should measure BCVA with commercially available logarithm of the minimum angle of resolution (logMAR) charts to facilitate comparisons across trials and analyses.
History
Protocol first published: Issue 12, 2021
Risk of bias
Risk of bias for analysis 1.1 Mean logMAR best‐corrected visual acuity (one month).
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Kannan 2018 | Some concerns | The authors stated that "System‐generated random number were used to recruit the patients into two groups," suggesting that randomization were properly performed. In terms of allocation concealment, the author specified in the trial registry that the method of concealment was "an open list of random numbers," suggesting that allocation was not properly concealed. The baseline characteristics in terms of sex, age, minimum diameter, base diameter, and baseline visual acuity were comparable between groups. | Low risk of bias | The authors stated that participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians as previously assigned. Participants were analyzed based on a group that they were previously assigned. | Low risk of bias | Although the authors did not explicitly specified, it is likely that all participants' data were available. | Some concerns | The authors mentioned that "the Snellen visual acuity was converted into a logarithm of the minimum angle of resolution i.e. logMAR for statistical analysis." Such a method of measurement were appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Some concerns | Although there was a pre‐specified analysis plan available in the trial registry, such details did not provide sufficient information to assess consistency in reporting outcomes. However, the authors reported vision change from baseline but did not specify at which time point and the unit of change was in lines, which was not clear. | High risk of bias | The RCT was judged to have a some concern risk of bias in the randomization process, measurement of the outcome and the selection for the reported result. |
| Manasa 2018 | Low risk of bias | The authors mentioned that "Randomization was done using the computer‐generated random number tables and the envelope method." The baseline characteristics were comparable between groups in terms of age, duration, preoperative VA, MLD, and MHI. | Low risk of bias | It is unclear whether or not participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians as previously assigned. It is likely that participants were analyzed based on group that they were previously assigned. | Low risk of bias | Although the number of losses to follow‐up was not explicitly specified, it seems like 9% of all were dropped out. Such number is acceptable. | Some concerns | The authors mentioned that "best‐corrected VA (BCVA) was measured using the standard ETDRS chart and converted to logMAR for statistical analysis." Such a method of measurement was appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Some concerns | There is no pre‐specified analysis plan available to assess. The authors did not report "change in visual acuity" but instead reported the absolute values at the follow up visits, which is of some concerns. | Some concerns | The RCT was judged to have some concerns of bias in some domains. |
| Michalewska 2010 | Low risk of bias | The authors stated that simple randomization was performed. Although the authors did not specify whether or not the allocation sequence was concealed, it is likely that participants was not aware of their treatment allocation before receiving intervention as the ranodmization was performed immediately before surgery. The baseline characteristics in terms of sex, age, preoperative macular hole diameters, preoperative visual acuity, and duration of the macular hole were similar between groups. | Low risk of bias | It is unclear whether or not participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. Although 7 cases in PPV with ILM flap group were accidentally seperated their ILM remnant from the margin of macular hole, it is likely to be occured by chance. Participants were analyzed based on group that they were previously assigned. | Low risk of bias | Although the authors did not explicitly specified, it is likely that all participants' data were available. | Low risk of bias | The authors mentioned that "best‐corrected visual acuity was measured by a "blinded" examiner using Snellen tables." Such a method of measurement was appropriate and applied similarly on both groups. | Some concerns | The authors reported measuring BCVA at 1 month in the methods but did not disclose it in the published article. We communicated with the authors of (Michalewska 2010) and they provided us with BCVA at 1 month for both groups, which was similar. In addition, the authors did not report "change in visual acuity" but instead reported the absolute values at the follow up visits, which is of some concerns. | Some concerns | The RCT was judged to have some concerns in one domain. |
| Velez‐Montoya 2018 | Low risk of bias | The selection of the ILM peeling technique for each individual case was randomized with a simple block randomization technique (3 × 3). None of the surgeons were aware of the ILM peeling technique before the surgery. They only became aware of the appointed technique after randomization. The baseline characteristics of participants across groups were similar in terms of age, time of evolution, and macular hole measurements at baseline. | Low risk of bias | Although the authors did not clearly state whether or not participants were masked throughout the study, it is likely that they were not aware of their treatment assignment. Physicians delivering the interventions were aware of surgery techniques as they could not be masked. However, It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians who were aware of the appointed technique after randomization. The authors did not clearly specified which analysis were used to estimate the effect of assignment, but It is likely that participants were analysed according to their assigned groups. | Low risk of bias | The authors did not mention the number of losses to follow‐up nor evidence that the result was not biased by missing outcome data. However, it is unlikely that losses to follow‐up, if there was any, could be related to participants' health status. | Low risk of bias | The author mentioned that "the assessment of the BCVA in Snellen lines [later converted to its logarithm of the minimum angle of resolution, (logMAR) equivalent for statistical purposes]". Such a method of measurement was applied similarly to both groups. Also, they mentioned that "all BCVA assessments and OCT tests during the follow‐up visits were done by a different physician or technician, who was blinded to the ILM peeling technique and randomization of each patient." | Some concerns | There was no protocol available to compare. The authors did not report "change in visual acuity" but instead reported the absolute values at the follow up visits, which is of some concerns. | Some concerns | The RCT was judged to have some concerns of bias in one domian. |
Risk of bias for analysis 1.2 Mean logMAR best‐corrected visual acuity (three months or more).
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 1.2.1 Three months | ||||||||||||
| Manasa 2018 | Low risk of bias | The authors mentioned that "Randomization was done using the computer‐generated random number tables and the envelope method." The baseline characteristics were comparable between groups in terms of age, duration, preoperative VA, MLD, and MHI. | Low risk of bias | It is unclear whether or not participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians as previously assigned. It is likely that participants were analyzed based on group that they were previously assigned. | Low risk of bias | Although the number of losses to follow‐up was not explicitly specified, it seems like 9% of all were dropped out. Such number is acceptable. | Some concerns | The authors mentioned that "best‐corrected VA (BCVA) was measured using the standard ETDRS chart and converted to logMAR for statistical analysis." Such a method of measurement was appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Some concerns | There is no pre‐specified analysus plan available to assess. The authors did not report "change in visual acuity" but instead reported the absolute values at the follow up visits, which is of some concerns. | Some concerns | The RCT was judged to have some concerns of bias in some domains. |
| Velez‐Montoya 2018 | Low risk of bias | The selection of the ILM peeling technique for each individual case was randomized with a simple block randomization technique (3 × 3). None of the surgeons were aware of the ILM peeling technique before the surgery. They only became aware of the appointed technique after randomization. The baseline characteristics of participants across groups were similar in terms of age, time of evolution, and macular hole measurements at baseline. | Low risk of bias | Although the authors did not clearly state whether or not participants were masked throughout the study, it is likely that they were not aware of their treatment assignment. Physicians delivering the interventions were aware of surgery techniques as they could not be masked. However, It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians who were aware of the appointed technique after randomization. The authors did not clearly specified which analysis were used to estimate the effect of assignment, but It is likely that participants were analysed according to their assigned groups. | Low risk of bias | The authors did not mention the number of losses to follow‐up nor evidence that the result was not biased by missing outcome data. However, it is unlikely that losses to follow‐up, if there was any, could be related to participants' health status. | Low risk of bias | The author mentioned that "the assessment of the BCVA in Snellen lines [later converted to its logarithm of the minimum angle of resolution, (logMAR) equivalent for statistical purposes]". Such a method of measurement was applied similarly to both groups. Also, they mentioned that "all BCVA assessments and OCT tests during the follow‐up visits were done by a different physician or technician, who was blinded to the ILM peeling technique and randomization of each patient." | Some concerns | There was no protocol available to compare. The authors did not report "change in visual acuity" but instead reported the absolute values at the follow up visits, which is of some concerns. | Some concerns | The RCT was judged to have some concerns of bias in one domians. |
| Subgroup 1.2.2 Six months | ||||||||||||
| Kannan 2018 | Some concerns | The authors stated that "System‐generated random number were used to recruit the patients into two groups," suggesting that randomization were properly performed. In terms of allocation concealment, the author specified in the trial registry that the method of concealment was "an open list of random numbers," suggesting that allocation was not properly concealed. The baseline characteristics in terms of sex, age, minimum diameter, base diameter, and baseline visual acuity were comparable between groups. | Low risk of bias | The authors stated that participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians as previously assigned. Participants were analyzed based on a group that they were previously assigned. | Low risk of bias | Although the authors did not explicitly specified, it is likely that all participants' data were available. | Low risk of bias | The authors mentioned that "the Snellen visual acuity was converted into a logarithm of the minimum angle of resolution i.e. logMAR for statistical analysis." Such a method of measurement were appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Some concerns | Although there was a pre‐specified analysis plan available in the trial registry, such details did not provide sufficient information to assess consistency in reporting outcomes. The authors stated in the trial registry that their visual outcome of interest was "the gain in vision". However, the authors reported vision change from baseline but did not specify at which time point and the unit of change was in lines, which was not clear. | High risk of bias | The RCT was judged to have a some concern risk of bias in the randomization process and the selection for the reported result. |
| Subgroup 1.2.3 One year | ||||||||||||
| Michalewska 2010 | Low risk of bias | The authors stated that simple randomization was performed. Although the authors did not specify whether or not the allocation sequence was concealed, it is likely that participants was not aware of their treatment allocation before receiving intervention as the ranodmization was performed immediately before surgery. The baseline characteristics in terms of sex, age, preoperative macular hole diameters, preoperative visual acuity, and duration of the macular hole were similar between groups. | Low risk of bias | It is unclear whether or not participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. Although 7 cases in PPV with ILM flap group were accidentally seperated their ILM remnant from the margin of macular hole, it is likely to be occured by chance. Participants were analyzed based on group that they were previously assigned. | Low risk of bias | Although the authors did not explicitly specified, it is likely that all participants' data were available. | Low risk of bias | The authors mentioned that "best‐corrected visual acuity was measured by a blinded examiner using Snellen tables." Such a method of measurement was appropriate and applied similarly on both groups. The authors stated that examiners were masked to participants' assigned interventions. | Some concerns | There is no pre‐specified analysus plan available to assess. The authors did not report "change in visual acuity" but instead reported the absolute values at the follow up visits, which is of some concerns. | Some concerns | The RCT was judged to have some concerns of bias in one domain. |
Risk of bias for analysis 1.3 Proportion of eyes achieving closure of macular hole.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Kannan 2018 | Some concerns | The authors stated that "System‐generated random number were used to recruit the patients into two groups," suggesting that randomization were properly performed. In terms of allocation concealment, the author specified in the trial registry that the method of concealment was "an open list of random numbers," suggesting that allocation was not properly concealed. The baseline characteristics in terms of sex, age, minimum diameter, base diameter, and baseline visual acuity were comparable between groups. | Low risk of bias | The authors stated that participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians as previously assigned. Participants were analyzed based on a group that they were previously assigned. | Low risk of bias | Although the authors did not explicitly specified, it is likely that all participants' data were available. | Some concerns | The authors mentioned that "FTMH parameters and indices were gauged with Heidelberg Spectralis Spectral‐Domain Optical Coherence Tomography (SD‐OCT) (Heidelberg Engineering, Inc., Heidelberg, Germany) using high definition 5‐line raster scans and 3‐dimensional 512 × 128 macular cube scans passing through the fovea, before and after the surgery". Such a method of measurement were appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Low risk of bias | The data was analysed in accordance with a pre‐specified analysis plan available in the trial registry. | Some concerns | The RCT was judged to have some concerns of bias in some domains. |
| Manasa 2018 | Low risk of bias | The authors mentioned that "Randomization was done using the computer‐generated random number tables and the envelope method." The baseline characteristics were comparable between groups in terms of age, duration, preoperative VA, MLD, and MHI. | Low risk of bias | It is unclear whether or not participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians as previously assigned. It is likely that participants were analyzed based on group that they were previously assigned. | Low risk of bias | Although the number of losses to follow‐up was not explicitly specified, it seems like 9% of all were dropped out. Such number is acceptable. | Some concerns | The authors mentioned that "Spectral‐domain optical coherence tomography (SDOCT) (Spectralis OCT; Heidelberg Engineering, Heidelberg, Germany) using the radial scan with 125 µm spacing through the center of the hole was used to measure the MLD and to assess postoperative hole closure." Such a method of measurement was appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Low risk of bias | There is no pre‐specified analysis plan available to assess. However, there is low risk for selective reporting. | Some concerns | The RCT was judged to have some concerns of bias in one domain. |
| Michalewska 2010 | Low risk of bias | The authors stated that simple randomization was performed. Although the authors did not specify whether or not the allocation sequence was concealed, it is likely that participants was not aware of their treatment allocation before receiving intervention as the ranodmization was performed immediately before surgery. The baseline characteristics in terms of sex, age, preoperative macular hole diameters, preoperative visual acuity, and duration of the macular hole were similar between groups. | Low risk of bias | It is unclear whether or not participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. Although 7 cases in PPV with ILM flap group were accidentally seperated their ILM remnant from the margin of macular hole, it is likely to be occured by chance. Participants were analyzed based on group that they were previously assigned. | Low risk of bias | Although the authors did not explicitly specified, it is likely that all participants' data were available. | Some concerns | The authors mentioned that "FTMH parameters and indices were gauged with Heidelberg Spectralis Spectral‐Domain Optical Coherence Tomography (SD‐OCT) (Heidelberg Engineering, Inc., Heidelberg, Germany) using high definition 5‐line raster scans and 3‐dimensional 512 × 128 macular cube scans passing through the fovea, before and after the surgery". Such a method of measurement was appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Low risk of bias | There is no pre‐specified analysis plan available to assess. However, there is low risk for selective reporting. | Some concerns | The RCT was judged to have some concerns of bias in one domain. |
| Velez‐Montoya 2018 | Low risk of bias | The selection of the ILM peeling technique for each individual case was randomized with a simple block randomization technique (3 × 3). None of the surgeons were aware of the ILM peeling technique before the surgery. They only became aware of the appointed technique after randomization. The baseline characteristics of participants across groups were similar in terms of age, time of evolution, and macular hole measurements at baseline. | Low risk of bias | Although the authors did not clearly state whether or not participants were masked throughout the study, it is likely that they were not aware of their treatment assignment. Physicians delivering the interventions were aware of surgery techniques as they could not be masked. However, It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians who were aware of the appointed technique after randomization. The authors did not clearly specified which analysis were used to estimate the effect of assignment, but It is likely that participants were analysed according to their assigned groups. | Low risk of bias | The authors did not mention the number of losses to follow‐up nor evidence that the result was not biased by missing outcome data. However, it is unlikely that losses to follow‐up, if there was any, could be related to participants' health status. | Low risk of bias | The author mentioned that "closure of macular hole was measured by optical coherence tomography [OCT (Spectralis HRA‐OCT; Heidelberg Engineering, Heidelberg, Germany); or (Cirrus HD‐OCT, Carl Zeiss Meditec, Dublin CA)]". Such a method of measurement was applied similarly to both groups. Also, they mentioned that "all BCVA assessments and OCT tests during the follow‐up visits were done by a different physician or technician, who was blinded to the ILM peeling technique and randomization of each patient." | Low risk of bias | There was no protocol available to compare. However, there is low risk for selective reporting. | Low risk of bias | The RCT was judged to have low risk of bias in all domains. |
Risk of bias for analysis 1.4 Proportion of eyes achieving type 1 macular hole closure.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 1.4.1 Type 1 | ||||||||||||
| Kannan 2018 | Some concerns | The authors stated that "System‐generated random number were used to recruit the patients into two groups," suggesting that randomization were properly performed. In terms of allocation concealment, the author specified in the trial registry that the method of concealment was "an open list of random numbers," suggesting that allocation was not properly concealed. The baseline characteristics in terms of sex, age, minimum diameter, base diameter, and baseline visual acuity were comparable between groups. | Low risk of bias | The authors stated that participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians as previously assigned. Participants were analyzed based on a group that they were previously assigned. | Low risk of bias | Although the authors did not explicitly specified, it is likely that all participants' data were available. | Some concerns | The authors mentioned that "FTMH parameters and indices were gauged with Heidelberg Spectralis Spectral‐Domain Optical Coherence Tomography (SD‐OCT) (Heidelberg Engineering, Inc., Heidelberg, Germany) using high definition 5‐line raster scans and 3‐dimensional 512 × 128 macular cube scans passing through the fovea, before and after the surgery". Such a method of measurement were appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Low risk of bias | The data was analysed in accordance with a pre‐specified analysis plan available in the trial registry. | Some concerns | The RCT was judged to have some concerns of bias in some domains |
| Manasa 2018 | Low risk of bias | The authors mentioned that "Randomization was done using the computer‐generated random number tables and the envelope method." The baseline characteristics were comparable between groups in terms of age, duration, preoperative VA, MLD, and MHI. | Low risk of bias | It is unclear whether or not participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians as previously assigned. It is likely that participants were analyzed based on group that they were previously assigned. | Low risk of bias | Although the number of losses to follow‐up was not explicitly specified, it seems like 9% of all were dropped out. Such number is acceptable. | Some concerns | The authors mentioned that "Spectral‐domain optical coherence tomography (SDOCT) (Spectralis OCT; Heidelberg Engineering, Heidelberg, Germany) using the radial scan with 125 µm spacing through the center of the hole was used to measure the MLD and to assess postoperative hole closure." Such a method of measurement was appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Low risk of bias | There is no pre‐specified analysis plan available to assess. However, there is low risk for selective reporting. | Some concerns | The RCT was judged to have some concerns of bias in one domain. |
| Michalewska 2010 | Low risk of bias | The authors stated that simple randomization was performed. Although the authors did not specify whether or not the allocation sequence was concealed, it is likely that participants was not aware of their treatment allocation before receiving intervention as the ranodmization was performed immediately before surgery. The baseline characteristics in terms of sex, age, preoperative macular hole diameters, preoperative visual acuity, and duration of the macular hole were similar between groups. | Low risk of bias | It is unclear whether or not participants were masked to their assigned intervention. Carers or people deliverying the interventions couldn't be masked to the participants' intervention due to the trial context. Although 7 cases in PPV with ILM flap group were accidentally seperated their ILM remnant from the margin of macular hole, it is likely to be occured by chance. Participants were analyzed based on group that they were previously assigned. | Low risk of bias | Although the authors did not explicitly specified, it is likely that all participants' data were available. | Some concerns | The authors mentioned that "FTMH parameters and indices were gauged with Heidelberg Spectralis Spectral‐Domain Optical Coherence Tomography (SD‐OCT) (Heidelberg Engineering, Inc., Heidelberg, Germany) using high definition 5‐line raster scans and 3‐dimensional 512 × 128 macular cube scans passing through the fovea, before and after the surgery". Such a method of measurement was appropriate and applied similarly on both groups. However, it is unclear whether or not outcome assessors were aware of the intervention assigned to the participants which is of some concerns. | Low risk of bias | There is no pre‐specified analysis plan available to assess. However, there is low risk for selective reporting. | Some concerns | The RCT was judged to have some concerns of bias in one domain. |
| Velez‐Montoya 2018 | Low risk of bias | The selection of the ILM peeling technique for each individual case was randomized with a simple block randomization technique (3 × 3). None of the surgeons were aware of the ILM peeling technique before the surgery. They only became aware of the appointed technique after randomization. The baseline characteristics of participants across groups were similar in terms of age, time of evolution, and macular hole measurements at baseline. | Low risk of bias | Although the authors did not clearly state whether or not participants were masked throughout the study, it is likely that they were not aware of their treatment assignment. Physicians delivering the interventions were aware of surgery techniques as they could not be masked. However, It is unlikely that there would be deviations from the intended intervention as the intervention is a surgical technique done by physicians who were aware of the appointed technique after randomization. The authors did not clearly specified which analysis were used to estimate the effect of assignment, but It is likely that participants were analysed according to their assigned groups. | Low risk of bias | The authors did not mention the number of losses to follow‐up nor evidence that the result was not biased by missing outcome data. However, it is unlikely that losses to follow‐up, if there was any, could be related to participants' health status. | Low risk of bias | The author mentioned that "closure of macular hole was measured by optical coherence tomography [OCT (Spectralis HRA‐OCT; Heidelberg Engineering, Heidelberg, Germany); or (Cirrus HD‐OCT, Carl Zeiss Meditec, Dublin CA)]". Such a method of measurement was applied similarly to both groups. Also, they mentioned that "all BCVA assessments and OCT tests during the follow‐up visits were done by a different physician or technician, who was blinded to the ILM peeling technique and randomization of each patient." | Low risk of bias | There was no protocol available to compare. However, there is low risk for selective reporting. | Low risk of bias | The RCT was judged to have low risk of bias in all domians. |
Acknowledgements
Cochrane Eyes and Vision US Project (CEV@US) supported the authors in the development of this review. The following people conducted the editorial process for this article.
Sign‐off Editors (final editorial decision): Dr Tianjing Li (University of Colorado Anschutz Medical Campus, Aurora, CO), Dr Gianni Virgilli (Queen's University Belfast, Belfast, Northern Ireland)
Managing Editor and Assistant Managing Editors (selected peer reviewers, collated peer‐reviewer comments): Anupa Shah (Queen's University Belfast, Belfast, Northern Ireland); Louis Leslie (University of Colorado Anschutz Medical Campus, Aurora, CO), Genie Han (Johns Hopkins University, Baltimore, MA)
Methodologist (provided methodological and editorial guidance to authors, edited the article): Alison Su‐Hsun Liu and Sueko Ng (University of Colorado Anschutz Medical Campus, Aurora, CO)
Information Specialist: Lori Rosman (Johns Hopkins University, Baltimore, MA)
Copy Editor: Julia Turner, Cochrane Central Production Service
Peer reviewers: two reviewers who wish to remain anonymous
Appendices
Appendix 1. CENTRAL search strategy
#1 MeSH descriptor: [Retinal Perforations] explode all trees #2 (macula* near/3 hole*) #3 (retina* near/3 hole*) #4 #1 OR #2 OR #3 #5 MeSH descriptor: [Vitrectomy] explode all trees #6 MeSH descriptor: [Vitreoretinal Surgery] explode all trees #7 vitrect* #8 (vitre* AND surg*) #9 PPV #10 (ILM OR (internal near/2 limit* near/2 membrane*)) AND (flap* OR peel*) #11 #7 OR #8 OR #9 OR #10 #12 #4 AND #11
Appendix 2. MEDLINE Ovid search strategy
1. Randomized Controlled Trial.pt. 2. Controlled Clinical Trial.pt. 3. (randomized or randomised).ab,ti. 4. placebo.ab,ti. 5. drug therapy.fs. 6. randomly.ab,ti. 7. trial.ab,ti. 8. groups.ab,ti. 9. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 10. exp animals/ not humans.sh. 11. 9 not 10 12. exp Retinal Perforations/ 13. (macula* adj3 hole*).tw. 14. (retina* adj3 hole*).tw. 15. 12 or 13 or 14 16. exp Vitrectomy/ 17. exp Vitreoretinal Surgery/ 18. vitrect*.tw. 19. (vitre* and surg*).tw. 20. PPV.tw. 21. ((ILM or (internal adj2 limit* adj2 membrane*)) and (flap* or peel*)).tw. 22. 16 or 17 or 18 or 19 or 20 or 21 23. 15 and 22 24. 11 and 23
The search filter for trials at the beginning of the MEDLINE strategy is from the published paper by Glanville 2006.
Appendix 3. Embase.com search strategy
#1 'randomized controlled trial'/exp #2 'randomisation'/exp #3 'double blind procedure'/exp #4 'single blind procedure'/exp #5 random*:ab,ti #6 #1 OR #2 OR #3 OR #4 OR #5 #7 'animal'/exp OR 'animal experiment'/exp #8 'human'/exp #9 #7 AND #8 #10 #7 NOT #9 #11 #6 NOT #10 #12 'clinical trial'/exp #13 (clin* NEAR/3 trial*):ab,ti #14 ((singl* OR doubl* OR trebl* OR tripl*) NEAR/3 (blind* OR mask*)):ab,ti #15 'placebo'/exp #16 placebo*:ab,ti #17 random*:ab,ti #18 'experimental design'/exp #19 'crossover procedure'/exp #20 'control group'/exp #21 'latin square design'/exp #22 #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 #23 #22 NOT #10 #24 #23 NOT #11 #25 'comparative study'/exp #26 'evaluation'/exp #27 'prospective study'/exp #28 control*:ab,ti OR prospectiv*:ab,ti OR volunteer*:ab,ti #29 #25 OR #26 OR #27 OR #28 #30 #29 NOT #10 #31 #30 NOT (#11 OR #23) #32 #11 OR #24 OR #31 #33 'retina tear'/exp #34 (macula* NEAR/3 hole*):ab,ti,kw #35 (retina* NEAR/3 hole*):ab,ti,kw #36 #33 OR #34 OR #35 #37 'vitreoretinal surgery'/exp #38 vitrect*:ab,ti,kw #39 (vitre* AND surg*):ab,ti,kw #40 ppv:ab,ti,kw #41 (ilm:ab,ti,kw OR ((internal NEAR/2 limit* NEAR/2 membrane*):ab,ti,kw)) AND (flap*:ab,ti,kw OR peel*:ab,ti,kw) #42 #37 OR #38 OR #39 OR #40 OR #41 #43 #36 AND #42 #44 #32 AND #43
Appendix 4. PubMed search strategy
1. ((randomized controlled trial[pt]) OR (controlled clinical trial[pt]) OR (randomised[tiab] OR randomized[tiab]) OR (placebo[tiab]) OR (drug therapy[sh]) OR (randomly[tiab]) OR (trial[tiab]) OR (groups[tiab])) NOT (animals[mh] NOT humans[mh]) 2. (macula*[tw] OR retina*[tw]) AND hole*[tw] 3. (vitrect*[tw] OR PPV[tw]) 4. (vitre*[tw] AND surg*[tw]) 5. (ILM[tw] OR (internal[tw] AND limit*[tw] AND membrane*[tw])) AND (flap*[tw] OR peel*[tw]) 6. #3 OR #4 OR #5 7. #1 AND #2 AND #6 8. Medline[sb] 9. #7 NOT #8
Appendix 5. LILACS search strategy
(MH:C11.768.740$ OR (macula$ AND hole$) OR (retina$ AND hole$)) AND (vitrect$ OR MH:E04.540.960$ OR PPV$ OR (vitre$ AND surg$) OR MH:E04.540.980$ OR (ILM AND (flap$ OR peel$)) OR ((internal AND limit$ AND membrane$) AND (flap$ OR peel$)))
Appendix 6. ClinicalTrials.gov search strategy
("macular hole" OR "retinal hole") AND (vitrectomy OR PPV OR "vitreous surgery" OR "vitreoretinal surgery" OR ((ILM OR "internal limiting membrane") AND (flap or peeling)))
Appendix 7. WHO ICTRP search strategy
macular hole AND vitrectomy OR macular hole AND PPV OR macular hole AND surgery OR macular hole AND ILM OR macular hole AND peeling
retinal hole AND vitrectomy OR retinal hole AND PPV OR retinal hole AND surgery OR retinal hole AND ILM OR retinal hole AND peeling
macular hole AND internal limiting membrane OR retinal hole AND internal limiting membrane
Data and analyses
Comparison 1. Pars plana vitrectomy (PPV) with internal limiting membrane (ILM) inverted flap versus PPV with ILM peeling.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1.1 Mean logMAR best‐corrected visual acuity (one month) | 4 | 254 | Mean Difference (IV, Random, 95% CI) | ‐0.08 [‐0.20, 0.05] |
| 1.2 Mean logMAR best‐corrected visual acuity (three months or more) | 4 | 276 | Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.23, ‐0.10] |
| 1.2.1 Three months | 2 | 115 | Mean Difference (IV, Random, 95% CI) | ‐0.17 [‐0.26, ‐0.07] |
| 1.2.2 Six months | 1 | 60 | Mean Difference (IV, Random, 95% CI) | ‐0.12 [‐0.23, ‐0.01] |
| 1.2.3 One year | 1 | 101 | Mean Difference (IV, Random, 95% CI) | ‐0.22 [‐0.35, ‐0.09] |
| 1.3 Proportion of eyes achieving closure of macular hole | 4 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 1.10 [1.02, 1.18] |
| 1.4 Proportion of eyes achieving type 1 macular hole closure | 4 | Risk Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 1.4.1 Type 1 | 4 | 276 | Risk Ratio (M‐H, Random, 95% CI) | 1.31 [1.03, 1.66] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Kannan 2018.
| Study characteristics | |
| Methods |
Study design: single‐center parallel‐group RCT Number randomized
Exclusions after randomization: none reported Losses to follow‐up
Unit of analysis: participant (1 eye per participant) Number analyzed
Handling of missing data: NR Sample size calculation: "The type 1 closure rate obtained by Michalewska et al., i.e. 69% in ILM peeling group and 96% in ILM flap group, was used as reference (Michalewska 2010). By keeping the power of the study as 80% and the confidence interval as 95%, a sample of 60 subjects (30 in each arm) was calculated." |
| Participants |
Country: India Mean age
Gender
Mean preoperative BCVA in logMAR
Mean preoperative MH index in mm
Mean preoperative MH minimum diameter in mm
Mean preoperative MH base diameter in μm
Pseudophakia status
Inclusion criteria
Exclusion criteria
Types of MH in the study: idiopathic Equivalence of baseline characteristics: yes: sex, age, minimum diameter, base diameter, and baseline visual acuity were comparable between groups. |
| Interventions |
Intervention: PPV with ILM inverted flap (type of inverted flap technique: tucking) Control: PPV with ILM peeling Cointerventions: "In both groups, phacoemulsification with implantation of intraocular lens was followed by core vitrectomy and induction of posterior vitreous detachment." Follow‐up
Type of tamponade: SF6 Number of surgeons performing surgeries: 1 |
| Outcomes |
Primary outcomes
Secondary outcomes
Safety outcomes: no postoperative complications or adverse events were reported. Time points of measurement: day 1, 2 weeks, 1 month, 6 months |
| Notes |
Publication type: published article Funding sources: none reported Disclosures of interest: "The authors declare that they have no competing interests" Trial registry: CTRI/2017/11/010474 Study period: NR Subgroup analyses: no Publication language: English |
Manasa 2018.
| Study characteristics | |
| Methods |
Study design: single‐center parallel‐group RCT Number randomized:
Exclusions after randomization: no Losses to follow‐up
Unit of analysis: participant (1 eye per participant) Number analyzed
Handling of missing data: complete‐case analysis Sample size calculation: NR |
| Participants |
Country: India Mean age
Gender
Mean preoperative BCVA in logMAR
Mean preoperative MH index in mm
Mean preoperative MH minimum diameter in mm
Mean preoperative MH base diameter in μm (SD)
Pseudophakia status
Inclusion criteria
Exclusion criteria
Types of MH in the study: idiopathic Equivalence of baseline characteristics: yes: age, duration, preoperative visual acuity, minimum linear diameter, and MH index were comparable between groups. |
| Interventions |
Intervention: PPV with ILM inverted flap (type of inverted flap technique: the ILM flap was inverted and placed over the hole with a soft‐tipped cannula or a diamond‐dusted membrane scraper) Control: PPV with ILM peeling Cointerventions: NR Follow‐up
Type of tamponade: 20% SF6 with air was left in the vitreous cavity. Postoperatively, face‐down positioning was prescribed for 3 days. Number of surgeons performing surgeries: NR |
| Outcomes |
Primary outcomes
Secondary outcomes
Safety outcomes: no postoperative complications or adverse events were reported. Time points of measurement: 1 week, 1 month, 3 months |
| Notes |
Publication type: published article Funding sources: none reported Disclosures of interest: "The authors declare that they have no competing interests." Trial registry: none reported Study period: NR Subgroup analyses: no Publication language: English |
Michalewska 2010.
| Study characteristics | |
| Methods |
Study design: single‐center parallel‐group RCT Number randomized
Exclusions after randomization: no Losses to follow‐up: none reported Unit of analysis: eye Number analyzed
Handling of missing data: NR Sample size calculation: NR |
| Participants |
Country: Poland Mean age
Gender
Mean preoperative BCVA in logMAR
Mean preoperative MH index in mm
Mean preoperative MH minimum diameter in mm
Mean preoperative MH base diameter in μm
Pseudophakia status
Inclusion criteria
Exclusion criteria
Types of MH in the study: idiopathic Equivalence of baseline characteristics: yes: sex, age, minimum diameter, base diameter, and visual acuity were comparable between groups. |
| Interventions |
Intervention: PPV with ILM inverted flap (type of inverted flap technique: manipulated over the hole) Control: PPV with ILM peeling Cointerventions: "Cataract surgery in 9 patients (6 in group 1 and 3 in group 2) was performed during the time of this study (4–11 months after surgery)." Follow‐up
Type of tamponade: air Number of surgeons performing surgeries: 1 |
| Outcomes |
Primary outcomes
Secondary outcomes: not specified Safety outcomes: no postoperative complications or adverse events were reported. Time points of measurement: 1 week, 1 month, 3 months, 6 months, 12 months |
| Notes |
Publication type: published article Funding sources: none reported Disclosures of interest: "The author(s) have no proprietary or commercial interest in any materials discussed in this article." Trial registry: none reported Study period: NR Subgroup analyses: no Publication language: English |
Velez‐Montoya 2018.
| Study characteristics | |
| Methods |
Study design: multicenter parallel‐group RCT Number randomized
Exclusions after randomization: no Losses to follow‐up: NR Unit of analysis: participant (1 eye per participant) Number analyzed
Handling of missing data: NR Sample size calculation: NR |
| Participants |
Country: Mexico Mean age
Gender
Mean preoperative BCVA in logMAR
Mean preoperative MH index in mm
Mean preoperative MH minimum diameter in mm
Mean preoperative MH base diameter in μm
Pseudophakia status: all eyes were phakic prior to the surgery in both groups Inclusion criteria
Exclusion criteria
Types of MH in the study: idiopathic Equivalence of baseline characteristics: "There was no difference in age and time of evolution among groups (p= 0.58)"; " There were no differences in the MH closure rate between groups." |
| Interventions |
Intervention 1: PPV with ILM inverted flap (type of inverted flap technique: manipulated over the hole) Intervention 2: PPV with ILM free‐flap technique (not included in review) Control: PPV with ILM peeling Cointerventions: "Cataract surgery in all cases (combined with vitrectomy)" Follow‐up
Type of tamponade: none reported Number of surgeons performing surgeries: 4 surgeons in 3 centers. |
| Outcomes |
Primary outcomes
Secondary outcomes
Safety outcomes: no cases of retinal detachment in any group Time points of measurement: baseline, 1 month, 3 months |
| Notes |
Publication type: published article Funding sources: "There were no funds allocated to the realization of this research." Disclosures of interest: no conflicts of interest Trial registry: none reported Study period: 1 January 2016 to 1 January 2017 Subgroup analyses: no Publication language: English |
BCVA: best corrected visual acuity; ETDRS: early treatment diabetic retinopathy study; FTMH: full‐thickness macular hole; ILM: internal limiting membrane; logMAR: logarithm of the minimum angle of resolution; mfERG: multifocal electroretinogram; MH: macular hole; NR: not reported; OCT: optical coherence tomography; PPV: pars plana vitrectomy; RCT: randomized controlled trial; SD: standard deviation.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agrawal 2022 | Ineligible intervention. |
| ARVO 2016 | Ineligible comparator. |
| Babu 2020 | Ineligible intervention. |
| Bottoni 2020 | Ineligible study design. |
| Cacciamani 2020 | Ineligible comparator. |
| Casini 2017 | Ineligible intervention. |
| D'aloisio 2021 | Ineligible patient population. |
| Deng 2018 | Ineligible study design. |
| Ehrhardt 2022 | Ineligible intervention. |
| Freeman 1997 | Ineligible comparator. |
| Huang 2019 | Ineligible intervention. |
| Iovino 2018 | Ineligible intervention. |
| Iwasaki 2019 | Ineligible study design. |
| Karalezli 2021 | Ineligible study design. |
| Mete 2016 | Ineligible study design. |
| Mete 2017 | Ineligible study design. |
| NCT03020459 | Ineligible intervention. |
| Nerome 2002 | Ineligible study design. |
| Peralta 2019 | Ineligible study design. |
Characteristics of ongoing studies [ordered by study ID]
CTRI/2017/03/008001.
| Study name | Comparison between standard surgical technique versus newer technique for large holes in the centre of the retina: a prospective randomised control trial |
| Methods |
Study design: single‐center parallel‐group RCT Number randomized: 102 in total Exclusions after randomization: none reported Unit of analysis: NR Handling of missing data: NR |
| Participants |
Country: India Inclusion criteria
Exclusion criteria
Types of MH in the study: idiopathic |
| Interventions |
Intervention: PPV with ILM inverted flap (type of inverted flap technique: NR) Control: PPV with ILM peeling Planned follow‐up: 12 months Type of tamponade: SF6 |
| Outcomes |
Primary outcomes
Secondary outcomes
Time points of outcome measurement: 12 months |
| Starting date | 3 September 2017 |
| Contact information | Prabu Baskaran, Aravind Eye Hospital. Email: prabubaskaran@gmail.com |
| Notes | Sponsorship source: Aravind Eye Hospital, Cuddalore Main Road, Thavalakuppam, Pondicherry 605007, India |
CTRI/2017/05/008663.
| Study name | Comparative study between the conventional surgery versus a new surgical technique for treatment of macular holes |
| Methods |
Study design: single‐center parallel‐group RCT Number randomized
Exclusions after randomization: none reported Unit of analysis: none reported Handling of missing data: NR |
| Participants |
Country: India Inclusion criteria
Exclusion criteria
Types of MH in the study: idiopathic |
| Interventions |
Intervention: PPV with ILM inverted flap (type of inverted flap technique: NR) Control: PPV with ILM peeling Planned follow‐up: 1 week, 1 month, 3 months Type of tamponade: NR |
| Outcomes |
Primary outcomes
Secondary outcomes
Time points of outcome measurement: 1 week, 1 month, 3 months |
| Starting date | 1 April 2016 to 1 June 2018 (estimated) |
| Contact information | Manasa S. Centre for Ophthalmic Sciences, All India Institute Of Medical Sciences. Email: sendtomanasa@gmail.com |
| Notes | Sponsorship source: Dr Rajendra Prasad: Centre for Ophthalmic Sciences; All: India Institute of Medical Sciences, Ansari Nagar New Delhi, India |
NCT04698226.
| Study name | |
| Methods |
Study design: single‐center parallel‐group RCT Number randomized: 60 in total Exclusions after randomization: none reported Unit of analysis: NR Handling of missing data: NR |
| Participants |
Country: Czechia Inclusion criteria
Exclusion criteria
Types of MH in the study: Idiopathic |
| Interventions |
Intervention: PPV with ILM inverted flap (type of inverted flap technique: "Flower petal" type) Control: PPV with ILM peeling Planned follow‐up: 6 months Type of tamponade: SF6 |
| Outcomes |
Primary outcomes
Secondary outcomes
Time points of outcome measurement: 3 months (perioperative complications), 6 months |
| Starting date | NR |
| Contact information | Martin Pencak. Faculty Hospital Kralovske Vinohrady. Email: pencak@volny.cz |
| Notes | Sponsorship source: Faculty Hospital Kralovske Vinohrady |
BCVA: best‐corrected visual acuity; ERG: electroretinogram; FTMH: full‐thickness macular hole; ILM: internal limiting membrane; IOL: intraocular lens; MH: macular hole; NR: not reported; OCT: optical coherence tomography; PPV: pars plana vitrectomy; RCT: randomized controlled trial; SD: standard deviation; SD‐OCT: spectral domain optical coherence tomography.
Differences between protocol and review
Our review contains the following differences with respect to the protocol (Ghoraba 2021).
We used a random‐effects model for all meta‐analyses regardless of the number of trials, as we expected some heterogeneity across trials.
While the protocol stated "if both absolute and change values are present, we will prioritise the change"; we decided to analyze the absolute and change values separately because all included trials reported the absolute value, but only few of them reported the change value.
For type of macular hole (MH) measured by proportion of eyes achieving MH closure‐the important outcome, we used type 1 closure as a surrogate anatomic outcome of closure with retinal preservation instead of presenting type 1 and type 2 closure as independent outcomes.
We performed a post‐hoc sensitivity analysis for BCVA at three months or more because cataract surgery was performed during the follow‐up period in one study.
Contributions of authors
Designing the review: HG, Amir A, IK, KM, AM Co‐ordinating the review: TR Designing electronic search strategies: Lori Rosman, Cochrane Eyes and Vision Screening search results: HG, TR, WM Organizing retrieval of papers: TR Screening retrieved papers against inclusion criteria: HG, TR, WM Appraising quality of papers: HG, TR, BP Extracting data from papers: HG, TR, BP Writing to authors of papers for additional information: TR Providing additional data about papers: TR Obtaining and screening data on unpublished studies: TR Entering data into RevMan Web: HG, TR Analysis of data: TR Providing a methodological perspective: TR Providing a clinical perspective: HG, WM, IR, KM, QN Providing a policy perspective: HG, KM, CY Writing the review: HG, TR, Amir A, IK, WM, BP, KM, CY, AM, Amira A Providing general advice on the review: TR, QN
All authors read and approved the final version of the review.
Sources of support
Internal sources
-
None, Other
No internal source of support
External sources
-
National Eye Institute, National Institutes of Health, USA
Cochrane Eyes and Vision US Project, supported by grant UG1EY020522 (PI: Tianjing Li, MD, MHS, PhD)
-
Public Health Agency, UK
This protocol was supported by the HSC Research and Development (R&D) Division of the Public Health Agency which funds the Cochrane Eyes and Vision editorial base at Queen's University Belfast, Belfast, Northern Ireland.
-
Queen's University Belfast, UK
Gianni Virgili, Co‐ordinating Editor for Cochrane Eyes and Vision's work is funded by the Centre for Public Health, Queen's University Belfast, Belfast, Northern Ireland.
Declarations of interest
HG: reports involvement in a retrospective study evaluating the studied technique for traumatic macular holes in Magrabi Eye Hospital, Tanta, Egypt. TR: declares no conflicts of interest. Amir A: declares no conflicts of interest. IK: declares no conflicts of interest. WM: reports working as an Ophthalmologist at the Department of Ophthalmology at Kobe University, Kobe, Japan. BP: declares no conflicts of interest. KM: declares no conflicts of interest. CY: declares no conflicts of interest. AM: declares no conflicts of interest. Amira A: declares no conflicts of interest. QN: declares no conflicts of interest.
New
References
References to studies included in this review
Kannan 2018 {published data only}
- CTRI/2017/11/010474. Inverted Internal limiting membrane (ILM) flap technique versus ILM peeling for treatment of large macular holes: a randomised control trial. trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2017/11/010474 (first received 13 November 2017).
- Kannan NB, Kohli P, Parida H, Adenuga OO, Ramasamy K. Comparative study of inverted internal limiting membrane (ILM) flap and ILM peeling technique in large macular holes: a randomized-control trial. BMC ophthalmology 2018;18(1):177. [DOI] [PMC free article] [PubMed] [Google Scholar]
Manasa 2018 {published data only}
- Manasa S, Kakkar P, Kumar A, Chandra P, Kumar V, Ravani R. Comparative evaluation of standard ILM peel with inverted ILM flap technique in large macular holes: a prospective, randomized study. Ophthalmic Surgery Lasers and Imaging Retina 2018;49(4):236‐40. [DOI] [PubMed] [Google Scholar]
Michalewska 2010 {published data only}
- Michalewska Z, Michalewski J, Adelman RA, Nawrocki J. Inverted internal limiting membrane flap technique for large macular holes. Ophthalmology 2010;117(10):2018‐25. [DOI] [PubMed] [Google Scholar]
Velez‐Montoya 2018 {published data only}
- Avila Joor, Ramirez-Estudillo A, Morales-Canton V, Hernandez-Da Mota S, Bejar F, Velez-Montoya R. Assessment of three different surgical ILM peeling techniques for the treatment of complicated macular holes. Investigative Ophthalmology & Visual Science 2017;58(8):2832. [Google Scholar]
- Velez-Montoya R, Ramirez-Estudillo JA, de Liano Cs-G, Bejar-Cornejo F, Sanchez-Ramos J, Guerrero-Naranjo JL, et al. Inverted ILM flap, free ILM flap and conventional ILM peeling for large macular holes. International Journal of Retina and Vitreous 2018;4(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
Agrawal 2022 {published data only}
- Agrawal V, Jindal K, Dhakad Y, Rathore P, Khilnani K. Multilayered inverted internal limiting membrane flap technique versus standard internal limiting membrane peeling for large macular holes: a comparative study. Indian Journal of Ophthalmology 2022;70(3):909-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
ARVO 2016 {published data only}
- Comparison of inverted flap and subretinal aspiration technique in full thickness macular hole surgery. Conference: 2016 Annual Meeting of the Association for Research in Vision and Ophthalmology, 2016 May 1-5; Seattle (WA). Investigative Ophthalmology & Visual Science 2016;(12):1100.
Babu 2020 {published data only}
- Babu N, Kohli P, Ramachandran NO, Adenuga OO, Ahuja A, Ramasamy K. Comparison of platelet-rich plasma and inverted internal limiting membrane flap for the management of large macular holes: a pilot study. Indian Journal of Ophthalmology 2020;68(5):880‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bottoni 2020 {published data only}
- Bottoni F, Parrulli S, Mete M, D'Agostino I, Cereda M, Cigada M, et al. Large idiopathic macular hole surgery: remodelling of outer retinal layers after traditional internal limiting membrane peeling or inverted flap technique. Ophthalmologica 2020;243(5):334-41. [DOI] [PubMed] [Google Scholar]
Cacciamani 2020 {published data only}
- Cacciamani A, Gelso A, Di Nicola M, Scarinci F, Ripandelli G, Costagliola C, et al. Inverted ILM-flap techniques variants for macular hole surgery: randomized clinical trial to compare retinal sensitivity and fixation stability. Scientific Reports 2020;10(1):15832. [DOI] [PMC free article] [PubMed] [Google Scholar]
Casini 2017 {published data only}
- Casini G, Mura M, Figus M, Loiudice P, Peiretti E, De Cillà S, et al. Inverted internal limiting membrane flap technique for macular hole surgery without extra manipulation of the flap. Retina 2017;37(11):2138‐44. [DOI] [PubMed] [Google Scholar]
D'aloisio 2021 {published data only}
- D'aloisio R, Carpineto P, Aharrh-Gnama A, Iafigliola C, Cerino L, Di Nicola M, et al. Early vascular and functional changes after vitreoretinal surgery: a comparison between the macular hole and epiretinal membrane. Diagnostics 2021;11(6):1031. [DOI] [PMC free article] [PubMed] [Google Scholar]
Deng 2018 {published data only}
- Deng J, Sun WT, Lei CL, Chai F, Wang SM, Wang LP. Comparison between internal limiting membrane covering and internal limiting membrane peeling for giant macular hole. International Eye Science 2018;18(12):2199-203. [Google Scholar]
Ehrhardt 2022 {published data only}
- Ehrhardt A, Delpuech M, Luc A, Zessler A, Pastor G, Angioi-Duprez K, et al. Dissociated optic nerve fiber layer appearance after macular hole surgery: a randomized controlled trial comparing the temporal inverted internal limiting membrane flap technique with conventional peeling. Ophthalmology Retina 2023;7(3):227-35. [DOI: 10.1016/j.oret.2022.09.002] [DOI] [PubMed]
- NCT03287102. Macular hole surgery with temporal inverted internal limiting membrane flap (MARTIAL). clinicaltrials.gov/study/NCT03287102 (first received 19 September 2017).
Freeman 1997 {published data only}
- Freeman WR, Azen SP, Kim JW, el-Haig W, Mishell DR 3rd, Bailey I. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes: results of a multicentered randomized clinical trial. The Vitrectomy for Treatment of Macular Hole Study Group. Archives of Ophthalmology 1997;115(5):11-21. [DOI] [PubMed] [Google Scholar]
Huang 2019 {published data only}
- Huang H, Wang Y, Ke R, Zhang X. Therapeutic effect of two methods of internal limiting membrane dissection on MHCI < 0.7 idiopathic macular hole. International Eye Science 2019;19(7):1170‐3. [Google Scholar]
Iovino 2018 {published data only}
- Iovino C, Caminiti G, Miccoli M, Nasini F, Casini G, Peiretti E. Comparison of inverted flap and subretinal aspiration technique in full-thickness macular hole surgery: a randomized controlled study. European Journal of Ophthalmology 2018;28(3):324‐8. [DOI] [PubMed] [Google Scholar]
Iwasaki 2019 {published data only}
- Iwasaki M, Kinoshita T, Miyamoto H, Imaizumi H. Influence of inverted internal limiting membrane flap technique on the outer retinal layer structures after a large macular hole surgery. Retina 2019;39(8):1470‐7. [DOI] [PubMed] [Google Scholar]
Karalezli 2021 {published data only}
- Karalezli A, Kaderli S T, Sul S. Macular microvasculature differences in patients with macular hole after vitrectomy with internal limiting membrane removal or single-layered temporal inverted flap technique. Eye 2021;35(10):2746-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mete 2016 {published data only}
- Mete M, Alfano A, Guerriero M, Pertile G. Inverted ILM flap and complete ILM removal in the surgery of myopic macular holes: a comparative study. Ophthalmologica 2016;236:2-3. [Google Scholar]
Mete 2017 {published data only}
- Mete M, Alfano A, Guerriero M, Prigione G, Sartore M, Polito A, et al. Inverted internal limiting membrane flap technique versus complete internal limiting membrane removal in myopic macular hole surgery. Retina 2017;37(10):1923-30. [DOI] [PubMed] [Google Scholar]
NCT03020459 {published data only}
- NCT03020459. Internal limiting membrane peeling-reposition to treat idiopathic macular holes. clinicaltrials.gov/show/NCT03020459 (first received 13 January 2017).
Nerome 2002 {published data only}
- Nerome K, Matsumura S, Hatano T, Kayo M. Results of surgery for idiopathic macular hole. Folia Ophthalmologica Japonica 2002;53(2):130-5. [Google Scholar]
Peralta 2019 {published data only}
- Peralta Iturburu F, Garcia-Arumi C, Bove Alvarez M, Garcia-Arumi J. Comparison of anatomical and visual outcomes between idiopathic and myopic macular holes using the internal limiting membrane or inverted internal limiting membrane flap technique. Journal of Ophthalmology 2019 [eCollection 2019]:6723824. [DOI] [PMC free article] [PubMed]
References to ongoing studies
CTRI/2017/03/008001 {published data only}
- CTRI/2017/03/008001. Comparison between standard surgical technique versus newer technique for large holes in the centre of the retina: a prospective randomised control trial. trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2017/03/008001 (first received 3 March 2017).
CTRI/2017/05/008663 {published data only}
- CTRI/2017/05/008663. Comparative study between the conventional surgery versus a new surgical technique for treatment of macular holes. trialsearch.who.int/Trial2.aspx?TrialID=CTRI/2017/05/008663 (first received 25 May 2017).
NCT04698226 {published data only}
- NCT04698226. ILM peeling versus inverted flap technique for treatment of macular hole: near visual acuity outcomes. clinicaltrials.gov/ct2/show/NCT04698226 (first received 6 January 2021).
Additional references
Ali 2017
- Ferhina SA, Joshua DS, Taylor SB, Sarah A, Jay MS. Incidence of and risk factors for developing idiopathic macular hole among a diverse group of patients throughout the United States. JAMA Ophthalmology 2017;135(4):299-305. [DOI] [PMC free article] [PubMed] [Google Scholar]
Almony 2012
- Almony A, Nudleman E, Shah GK, Blinder KJ, Eliott DB, Mittra RA, et al. Techniques, rationale, and outcomes of internal limiting membrane peeling. Retina 2012;32(5):877-91. [DOI] [PubMed] [Google Scholar]
Altman 1996
- Altman DG, Bland JM. Detecting skewness from summary information. BMJ 1996;313(7066):1200. [DOI] [PMC free article] [PubMed] [Google Scholar]
Budoff 2019
- Budoff F, Bhagat N, Zarbin MA. Traumatic macular hole: diagnosis, natural history, and management. Journal of Ophthalmology 2019;2019:5837832. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chatziralli 2018
- Chatziralli IP, Theodossiadis PG, Steel DH. Internal limiting membrane peeling in macular hole surgery; why, when, and how? Retina 2018;38(5):870-82. [DOI] [PubMed] [Google Scholar]
Chen 2020
- Chen G, Tzekov R, Jiang F, Mao S, Tong Y, Li W. Inverted ILM flap technique versus conventional ILM peeling for idiopathic large macular holes: a meta-analysis of randomized controlled trials. PLOS One 2020;15(7):e0236431. [DOI] [PMC free article] [PubMed] [Google Scholar]
Christmas 1998
- Christmas NJ, Smiddy WE, Flynn HW Jr. Reopening of macular holes after initially successful repair. Ophthalmology 1998;105(10):1835-8. [PMID: ] [DOI] [PubMed] [Google Scholar]
Cornish 2014
- Cornish KS, Lois N, Scott NW, Burr J, Cook J, Boachie C, et al. Vitrectomy with internal limiting membrane peeling versus no peeling for idiopathic full-thickness macular hole. Ophthalmology 2014;121(3):649-55. [DOI] [PubMed] [Google Scholar]
Covidence 2021 [Computer program]
- Covidence. Melbourne, Australia: Veritas Health Innovation, accessed 27 July 2021. Available at www.covidence.org.
Deeks 2021
- Deeks JJ, Higgins JP, Altman DG, editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Duker 2013
- Duker JS, Kaiser PK, Binder S, Smet MD, Gaudric A, Reichel E, et al. The International Vitreomacular Traction Study Group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 2013;120(12):2611-9. [DOI] [PubMed] [Google Scholar]
Ezra 2001
- Ezra E. Idiopathic full thickness macular hole: natural history and pathogenesis. British Journal of Ophthalmology 2001;85(1):102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gass 1988
- Gass JD. Idiopathic senile macular hole. Its early stages and pathogenesis. Archives of Ophthalmology 1988;106(5):629-39. [DOI] [PubMed] [Google Scholar]
Gattoussi 2019
- Gattoussi S, Buitendijk GH, Peto T, Leung I, Schmitz-Valckenberg S, Oishi A, et al. The European eye epidemiology spectral-domain optical coherence tomography classification of macular diseases for epidemiological studies. Acta Ophthalmologica 2019;97(4):364-71. [DOI] [PubMed] [Google Scholar]
Gelman 2015
- Gelman R, Stevenson W, Ponce CP, Agarwal D, Christoforidis JB. Retinal damage induced by internal limiting membrane removal. Journal of Ophthalmology 2015;2015:939748. [DOI] [PMC free article] [PubMed] [Google Scholar]
Glanville 2006
- Glanville JM, Lefebvre C, Miles JN, Camosso-Stefinovic J. How to identify randomized controlled trials in MEDLINE: ten years on. Journal of the Medical Library Association 2006;94(2):130-6. [PMC free article] [PubMed] [Google Scholar]
GRADE 2013
- Schünemann H, Brożek J, Guyatt G, Oxman A, editor(s). Handbook for grading the quality of evidence and the strength of recommendations using the GRADE approach (updated October 2013). GRADE Working Group, 2013. Available from gdt.guidelinedevelopment.org/app/handbook/handbook.html.
Gu 2018
- Gu C, Qiu Q. Inverted internal limiting membrane flap technique for large macular holes: a systematic review and single-arm meta-analysis. Graefe's Archive for Clinical and Experimental Ophthalmology 2018;256(6):1041-9. [DOI] [PubMed] [Google Scholar]
Higgins 2002
- Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Statistics in Medicine 2002;21(11):1539-58. [DOI] [PubMed] [Google Scholar]
Iovino 2018
- Iovino C, Caminiti G, Miccoli M, Nasini F, Casini G, Peiretti E. Comparison of inverted flap and subretinal aspiration technique in full-thickness macular hole surgery: a randomized controlled study. European Journal of Ophthalmology 2018;28(3):324-8. [DOI] [PubMed] [Google Scholar]
Ip 2002
- Ip MS, Baker BJ, Duker JS, Reichel E, Baumal CR, Gangnon R, et al. Anatomical outcomes of surgery for idiopathic macular hole as determined by optical coherence tomography. Archives of Ophthalmology 2002;1(1):29-35. [DOI] [PubMed] [Google Scholar]
Johnson 1988
- Johnson RN, Gass JD. Idiopathic macular holes: observations, stages of formation, and implications for surgical intervention. Ophthalmology 1988;95(7):917-24. [DOI] [PubMed] [Google Scholar]
La Cour 2002
- La Cour M, Friis J. Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmologica Scandinavica 2002;80(6):579-87. [DOI] [PubMed] [Google Scholar]
Lewis 1996
- Lewis ML, Cohen SM, Smiddy WE, Gass JD. Bilaterality of idiopathic macular holes. Graefe's Archive for Clinical and Experimental Ophthalmology 1996;234(4):241-5. [DOI] [PubMed] [Google Scholar]
Marques 2020
- Marques RE, Sousa DC, Leal I, Faria MY, Marques-Neves C. Complete ILM peeling versus inverted flap technique for macular hole surgery: a meta-analysis. Ophthalmic Surgery, Lasers & Imaging Retina 2020;51(3):187-A2. [DOI] [PubMed] [Google Scholar]
McCannel 2009
- McCannel CA, Ensminger JL, Diehl NN, Hodge DN. Population-based incidence of macular holes. Ophthalmology 2009;116(7):1366-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Michalewska 2015
- Michalewska Z, Michalewski J, Dulczewska-Cichecka K, Adelman RA, Nawrocki J. Temporal inverted internal limiting membrane flap technique versus classic inverted internal limiting membrane flap technique: a comparative study. Retina 2015;35(9):1844-50. [DOI] [PubMed] [Google Scholar]
Mitchell 1997
- Mitchell P, Smith W, Chey T, Wang JJ, Chang A. Prevalence and associations of epiretinal membranes. The Blue Mountain Eye Study, Australia. Ophthalmology 1997;104(6):1033-40. [DOI] [PubMed] [Google Scholar]
Petermeier 2010
- Petermeier K, Szurman P, Bartz-Schmidt UK, Gekeler F. Pathophysiology of cataract formation after vitrectomy [Pathophysiologie der Katarakt-Entwicklung nach Vitrektomie ]. Klin Monbl Augenheilkd 2010;227(3):175-80. [DOI: 10.1055/s-0029-1245271] [DOI] [PubMed] [Google Scholar]
Rahmani 1996
- Rahmani B, Tielsch JM, Katz J, Gottsch J, Quigley H, Javitt J, et al. The cause-specific prevalence of visual impairment in an urban population: the Baltimore Eye Survey. Ophthalmology 1996;103(11):1721-6. [DOI] [PubMed] [Google Scholar]
RevMan Web 2020 [Computer program]
- Review Manager Web (RevMan Web). Version 4.12.0. The Cochrane Collaboration, 2022. Available at revman.cochrane.org.
Sen 2008
- Sen P, Bhargava A, Vijaya L, George R. Prevalence of idiopathic macular hole in adult rural and urban south Indian population. Clinical and Experimental Ophthalmology 2008;36(3):257-60. [DOI] [PubMed] [Google Scholar]
Shen 2020
- Shen Y, Lin X, Zhang L, Wu M. Comparative efficacy evaluation of inverted internal limiting membrane flap technique and internal limiting membrane peeling in large macular holes: a systematic review and meta-analysis. BMC Ophthalmology 2020;20(1):14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shiode 2017
- Shiode Y, Morizane Y, Matoba R, Hirano M, Doi S, Toshima S, et al. The role of inverted internal limiting membrane flap in macular hole closure. Investigative Ophthalmology & Visual Science 2017;58(11):4847-55. [DOI] [PubMed] [Google Scholar]
Sterne 2019
- Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:I4898. [DOI] [PubMed] [Google Scholar]
Takahashi 2011
- Takahashi A, Nagaoka T, Yoshida A. Stage 1-A macular hole: a prospective spectral-domain optical coherence tomography study. Retina 2011;31(1):127-47. [DOI] [PubMed] [Google Scholar]
Tornambe 2003
- Tornambe PE. Macular hole genesis: the hydration theory. Retina 2003;23(3):421-4. [DOI] [PubMed] [Google Scholar]
Valmaggia 2021
- Valmaggia C, Kostadinov F, Lang C, Guber J. Comparative study of combined vitrectomy with phacoemulsification versus vitrectomy alone for primary full-thickness macular hole repair. BMC Ophthalmology 2021;21(1):174. [DOI: 10.1186/s12886-021-01918-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Walia 2014
- Walia HS, Shah GK, Hariprasad SM. ILM peeling a vital intervention for many vitreoretinal disorders. Ophthalmic Surgery, Lasers and Imaging Retina 2014;45(2):92-6. [DOI] [PubMed] [Google Scholar]
Yu 2021
- Yu JG, Wang J, Xiang Y. Inverted internal limiting membrane flap technique versus internal limiting membrane peeling for large macular holes: a meta-analysis of randomized controlled trials. Ophthalmic Research 2021;64(5):713-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Ghoraba 2021
- Ghoraba H, Abdelkarem AA, Akhavanrezayat A, Matsumiya W, Karaca I, Mishra K, et al. Pars plana vitrectomy with internal limiting membrane flap versus pars plana vitrectomy with conventional internal limiting membrane peeling for large macular hole. Cochrane Database of Systematic Reviews 2021, Issue 12. Art. No: CD015031. [DOI: 10.1002/14651858.CD015031] [DOI] [PMC free article] [PubMed] [Google Scholar]


