Graphical Abstract
Graphical abstract.
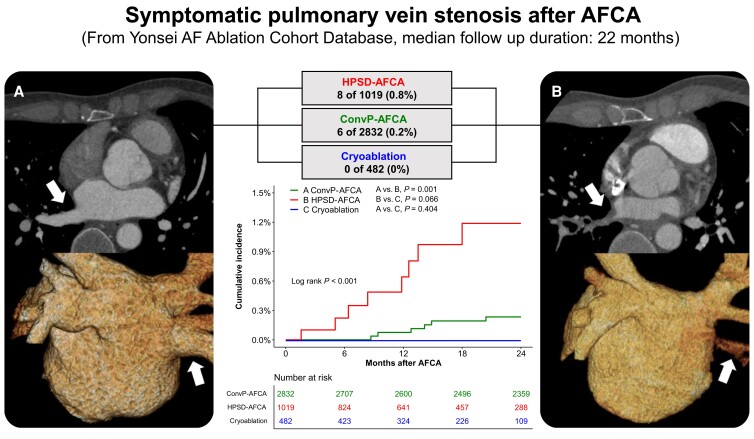
Computed tomography (CT) images of stenotic pulmonary vein before (A) and after atrial fibrillation catheter ablation (AFCA) (B). Kaplan–Meier curves for the cumulative incidence of pulmonary vein stenosis after AFCA. Top arrow of (A) pre-procedural right inferior pulmonary vein (RIPV), bottom arrow of (A) pre-procedural three-dimensional (3D) reconstructed image of RIPV, and arrows of (B) stenotic RIPV after AFCA. AF, atrial fibrillation; ConvP-AFCA, conventional power atrial fibrillation catheter ablation; HPSD, high-power short duration.
What’s new?
In comparison with atrial fibrillation (AF) patients treated with conventional power atrial catheter ablation (ConvP-AFCA), those with high-power short-duration catheter ablation (HPSD-AFCA) more frequently exhibit symptomatic pulmonary vein stenosis (PVS).
Symptomatic pulmonary vein stenosis occurs several months after AFCA, requiring long-term follow-up to monitor whether unexplained signs or symptoms are found.
Pulmonary vein (PV) stenosis (PVS) is a rare condition, and atrial fibrillation (AF) catheter ablation (AFCA) is a well-known cause of acquired PVS.1 The reported incidence of severe PVS or PVS requiring intervention after AFCA has ranged from 0.4% to 0.7% in some studies.2,3 High-power short-duration AFCA (HPSD-AFCA) is now widely accepted owing to its comparable efficacy and safety with conventional power-AFCA (ConvP-AFCA), along with reduced procedure time.4–7 The aim of the present study was to assess the occurrence of PVS according to the type of AFCA.
All patients provided written informed consent for inclusion in the Yonsei AF Ablation Cohort Database (ClinicalTrials.gov Identifier: NCT02138695). Data from 5246 cases in the cohort who underwent AFCA between March 2009 and June 2022 were reviewed. Individuals with AF and rheumatic valvular disease and/or a history of AF surgery were excluded. All patients had pre-procedural three-dimensional (3D) spiral computed tomography (CT). Intracardiac electrograms were recorded using a Prucka CardioLab electrophysiology system, integrated with a 3D electroanatomical mapping system (NavX and CARTO) merged with CT. For ConvP-AFCA, a radiofrequency (RF) power of 30–35 W was used for the anterior side and 25–30 W for ablation of the posterior side of the left atrium (LA) and PVs. For HPSD-AFCA, 50–60 W ablation for 10–15 s was used for the anterior side of the LA and PVs and 40–50 W ablation with a reduced ablation time (<10 s) for the posterior side of the LA and PVs. During the RF procedure, contact force-sensing (CFS) catheters were used at operators’ discretion. All cryoablation procedures were performed using a 28 mm cryoballoon (Arctic Front Advance). Cryoballoon dosing was based on a protocol described in the ICE-T trial.8 If there were remaining PV potentials after cryoablation, 50 W RF touchup ablation was delivered to complete electrical isolation. After discharge, patients visited the clinic regularly or when symptomatic. Those with respiratory symptoms were suspected of PVS and underwent CT, if needed. Symptomatic PVS was defined as PV being reported as occluded by CT and presence of stenotic PV with associated signs or symptoms.
After excluding patients with missing data, the analysis included data from 4333 patients. Among these, 2832 patients received ConvP-AFCA, 1019 underwent HPSD-AFCA, and 482 were treated with cryoablation. The mean age of the overall cohorts was 59.4 ± 12.1 years, 75.1% were male, 64.2% had paroxysmal AF, and 11.7% underwent repeated AFCA more than the re-do procedure. Fourteen cases of symptomatic PVS after AFCA were identified during a median follow-up of 22 months [interquartile range (IQR), 8–50 months]. The incidence rate of symptomatic PVS after AFCA was higher in the ConvP-AFCA group 0.2% (6 of 2832) than in the HPSD-AFCA group and 0.8% (8 of 1019) in the HPSD-AFCA group. The cumulative incidence of symptomatic PVS was significantly higher in the HPSD-AFCA group than that in the ConvP-AFCA group, respectively (log-rank P = 0.001; Graphical abstract). A total of 9.9% of patients in the ConvP-AFCA and 23.9% in the HPSD-AFCA group received RF ablation with a CFS catheter, yet none of them were diagnosed with symptomatic PVS (0 of 524). Additionally, there were no reported cases of symptomatic PVS after cryoablation. The medical records of symptomatic PVS cases were summarized in Table 1 . The median time to diagnosis of PVS from AFCA was 372 days (IQR, 258–427 days). The most common complaints among those with PVS, apart from cough, were haemoptysis and dyspnoea. Pulmonary vein stenosis treatment depended on symptom severity, prioritizing percutaneous procedures over surgery, with stent placement preferred for suitable sizes. About half of symptomatic PVS cases received endovascular or surgical intervention.
Table 1.
Review of symptomatic pulmonary vein stenosis cases after atrial fibrillation catheter ablation
| Case no. | AFCA protocol, type of ablation catheter | Ablation lesion set, RF power | Stenotic PV | Sex, age | Type of AF | AFCA counts | Comorbidity | Time to diagnosis, days | Signs and symptoms |
|---|---|---|---|---|---|---|---|---|---|
| 1 | ConvP-AFCA, Celsius™ | 4 PVI-30 W, POBI, CTI | LSPV | M, 50 | PAF | Re-do | None | 454 | Haemoptysis |
| Management and patient outcome | Observation without worsening symptom | ||||||||
| 2 | ConvP-AFCA, Celsius™ | 4 PVI-30 W, POBI, roof SVC-RA, CTI | RSPV, RIPV | M, 59 | PAF | Re-do | Hypertension, sick sinus | 623 | Dyspnoea on exertion, pleural effusion |
| Management and patient outcome | Percutaneous pulmonary venoplasty * 3 times ((i) RSPV stenosis → RSPV stenting, (ii) RSPV stent restenosis/RIPV stenosis → RSPV/RIPV BA, and (iii) RSPV stent and RIPV restenosis → RSPV BA + RIPV stenting) Chemical and surgical pleurodesis (for persistent effusion despite of venoplasty) |
||||||||
| 3 | ConvP-AFCA, Thermocool™ | RSPV-30 W, SVC-RA, RIGP, LIGP | RSPV | M, 48 | PAF | Tri-do | None | 390 | Haemoptysis |
| Management and patient outcome | Observation without worsening symptom | ||||||||
| 4 | ConvP-AFCA, Thermocool™ | 4 PVI-30 W, CTI | LSPV, LIPV | M, 54 | PAF | De novo | Hypertension | 432 | Dyspnoea on exertion |
| Management and patient outcome | Failed venoplasty due to being unable to pass through the stenotic LSPV | ||||||||
| 5 | ConvP-AFCA, Cool Flex™ | 4 PVI-30 W, SVC-RA, CTI | RSPV, RIPV | M, 70 | PAF | De novo | Hypertension, sick sinus | 265 | Haemoptysis |
| Management and patient outcome | Observation without worsening symptom | ||||||||
| 6 | ConvP-AFCA, Cool Flex™ | 4 PVI-30 W, CTI | LSPV, LIPV | F, 24 | PAF | De novo | Congenital (functional single ventricle) | 287 | Chest pain, cough |
| Management and patient outcome | Successful venoplasty by LIPV stenting | ||||||||
| 7 | HPSD-AFCA FlexAbility™ | 4 PVI + LAA PW-60 W, PW-50 W, CTI, SVC-RA | RIPV | F, 59 | PAF | De novo | None | 195 | Dyspnoea on exertion, pleural effusion |
| Management and patient outcome | Surgical wedge resection of the lung (a suspicion of pulmonary veno-infarction as lung malignancy at another hospital) | ||||||||
| 8 | HPSD-AFCA, FlexAbility™ | 4 PVI + LAA PW-60 W, PW-50 W, CTI, SVC-RA | RIPV | F, 78 | PAF | De novo | Chronic kidney disease, coronary artery disease | 48 | Dyspnoea on exertion |
| Management and patient outcome | Observation without worsening symptom | ||||||||
| 9 | HPSD-AFCA, FlexAbility™ | 4 PVI + LAA PW-60 W, PW-50 W, CTI, SVC-RA | RIPV | M, 34 | PAF | De novo | None | 154 | Cough, haemoptysis, chest pain |
| Management and patient outcome | Observation without worsening symptom | ||||||||
| 10 | HPSD-AFCA, FlexAbility™ | 4 PVI + LAA PW-60 W, PW-50 W, CTI, SVC-RA | RIPV | M, 46 | PAF | De novo | None | 255 | Cough, haemoptysis |
| Management and patient outcome | Successful venoplasty by RSPV stenting | ||||||||
| 11 | HPSD-AFCA, FlexAbility™ | 4 PVI + LAA PW-60 W, PW-50 W, CTI, SVC-RA | LIPV | M, 56 | PAF | De novo | None | 412 | Cough, haemoptysis |
| Management and patient outcome | Observation without worsening symptom | ||||||||
| 12 | HPSD-AFCA, FlexAbility™ | 4 PVI + LAA PW-60 W, PW-50 W, postero-inferior LA, CTI, SVC-RA | LIPV, LSPV | M, 33 | PAF | Re-do | None | 383 | Cough, haemoptysis |
| Management and patient outcome | Successful venoplasty by LIPV stenting | ||||||||
| 13 | HPSD-AFCA, FlexAbility™ | 4 PVI + LAA PW-60 W, PW-50 W, CTI, SVC-RA | RIPV | M, 56 | PAF | De novo | Ischaemic stroke | 361 | No symptom, minimal pleural effusion |
| Management and patient outcome | Observation without worsening symptom | ||||||||
| 14 | HPSD-AFCA, FlexAbility™ | 4 PVI + LAA PW-60 W, PW-50 W, LLI, postero-inferior LA | RSPV, RIPV | M, 68 | PeAF | Re-do | Hypertension, diabetes, heart failure, ischaemic stroke | 541 | Dyspnoea on exertion |
| Management and patient outcome | Successful venoplasty by RSPV stenting | ||||||||
AF, atrial fibrillation; BA, balloon angioplasty; ConvP-AFCA, conventional power atrial fibrillation catheter ablation; CTI, cavotricuspid isthmus; CXR, chest X-ray; HPSD, high-power short duration; LAA PW, left atrial appendage posterior wall; LIGP, left inferior ganglion plexus; LIPV, left inferior pulmonary vein; LLI, left lateral isthmus; LSPV, left superior pulmonary vein; PAF, paroxysmal AF; PeAF, persistent atrial fibrillation; PV, pulmonary vein; PW, posterior wall of left atrium; RA, right atrium; RF, radiofrequency; RIGP, right inferior ganglion plexus; RIPV, right inferior pulmonary vein; RSPV, right superior pulmonary vein.
Based on the author’s experience, signs or symptoms related to PVS developed several months after AFCA and it was diagnosed at a median of 12 months after the procedure. A previous study reported that PV diameters gradually decreased over 3 months after AFCA.9 In experimental animal studies, histopathological changes after RF ablation progress gradually over >10 weeks.10 Therefore, PVS after AFCA may occur late, requiring long-term follow-up, and, when unexplained signs or symptoms are found, further examination using modalities, such as contrast-enhanced CT, is necessary.
To date, there have been no reports suggesting that HPSD-AFCA is a risk factor causing more PVS than ConvP-AFCA. In a swine model, HPSD ablation resulted in wider lesions compared with standard ablation, which were consistently transmural.11,12 Based on these findings, we speculate that HPSD-AFCA is likely to induce histopathological changes in a broader area of myocardial tissue and may lead to more frequent endovascular contractions compared with ConvP-AFCA. Additionally, there were no instances of symptomatic PVS when using CFS catheter. To assess the relationship between CFS usage and PVS catheter, we require a larger sample size and further evaluation.
Recent experimental studies have reported that very high-power (>70 W), short-duration AFCA is as safe as conventional ablation and is associated with improved efficacy.13–15 However, because these studies only described peri-procedural and short-term complications, questions remain about the potential link between HPSD ablation and long-term complication such as PVS. Further analysis or studies investigating the long-term outcomes of HPSD ablation could potentially provide valuable insights into the relationship between HPSD ablation and PVS.
Acknowledgements
We would like to thank Mr John Martin, Editage, for his linguistic assistance.
Contributor Information
Joongmin Kim, Department of Internal Medicine, Yonsei University Health System, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea.
Daehoon Kim, Department of Internal Medicine, Yonsei University Health System, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea.
Hee Tae Yu, Department of Internal Medicine, Yonsei University Health System, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea.
Tae-Hoon Kim, Department of Internal Medicine, Yonsei University Health System, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea.
Boyoung Joung, Department of Internal Medicine, Yonsei University Health System, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea.
Moon-Hyoung Lee, Department of Internal Medicine, Yonsei University Health System, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea.
Hui-Nam Pak, Department of Internal Medicine, Yonsei University Health System, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Republic of Korea.
Funding
This work was supported by a grant (HI21C0011) from the Ministry of Health and Welfare; a grant (NRF-2020R1A2B5B01001695) from the Basic Science Research Program run by the National Research Foundation of Korea (NRF), which is funded by the Ministry of Science, ICT & Future Planning (MSIP); and a Korea Medical Device Development Fund grant (project number 1711174471; RS-2022-00141473) funded by the Korean government (Ministry of Science and ICT; Ministry of Trade, Industry and Energy; Ministry of Health & Welfare; and a grant [22213MFDS486] from the Ministry of Food and Drug Safety, Republic of Korea).
Data availability
Data are available upon reasonable request; the corresponding authors may provide the data.
References
- 1. Pazos-López P. Pulmonary vein stenosis: etiology, diagnosis and management. World J Cardiol 2016;8:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Teunissen C, Velthuis BK, Hassink RJ, van der Heijden JF, Vonken EPA, Clappers Net al. . Incidence of pulmonary vein stenosis after radiofrequency catheter ablation of atrial fibrillation. JACC Clin Electrophysiol 2017;3:589–98. [DOI] [PubMed] [Google Scholar]
- 3. Gupta A, Perera T, Ganesan A, Sullivan T, Lau DH, Roberts-Thomson KCet al. . Complications of catheter ablation of atrial fibrillation: a systematic review. Circ Arrhythm Electrophysiol 2013;6:1082–8. [DOI] [PubMed] [Google Scholar]
- 4. Yavin HD, Leshem E, Shapira-Daniels A, Sroubek J, Barkagan M, Haffajee CIet al. . Impact of high-power short-duration radiofrequency ablation on long-term lesion durability for atrial fibrillation ablation. JACC Clin Electrophysiol 2020;6:973–85. [DOI] [PubMed] [Google Scholar]
- 5. Winkle RA. HPSD ablation for AF high-power short-duration RF ablation for atrial fibrillation: a review. J Cardiovasc Electrophysiol 2021;32:2813–23. [DOI] [PubMed] [Google Scholar]
- 6. Ravi V, Poudyal A, Abid QU, Larsen T, Krishnan K, Sharma PSet al. . High-power short duration vs. conventional radiofrequency ablation of atrial fibrillation: a systematic review and meta-analysis. Europace 2021;23:710–21. [DOI] [PubMed] [Google Scholar]
- 7. Lee AC, Voskoboinik A, Cheung CC, Yogi S, Tseng ZH, Moss JDet al. . A randomized trial of high vs standard power radiofrequency ablation for pulmonary vein isolation: SHORT-AF. JACC Clin Electrophysiol 2023;9:1038–47. [DOI] [PubMed] [Google Scholar]
- 8. Chun KR, Stich M, Fürnkranz A, Bordignon S, Perrotta L, Dugo Det al. . Individualized cryoballoon energy pulmonary vein isolation guided by real-time pulmonary vein recordings, the randomized ICE-T trial. Heart Rhythm 2017;14:495–500. [DOI] [PubMed] [Google Scholar]
- 9. Dill T, Neumann T, Ekinci O, Breidenbach C, John A, Erdogan Aet al. . Pulmonary vein diameter reduction after radiofrequency catheter ablation for paroxysmal atrial fibrillation evaluated by contrast-enhanced three-dimensional magnetic resonance imaging. Circulation 2003;107:845–50. [DOI] [PubMed] [Google Scholar]
- 10. Taylor GW, Kay GN, Zheng X, Bishop S, Ideker RE. Pathological effects of extensive radiofrequency energy applications in the pulmonary veins in dogs. Circulation 2000;101:1736–42. [DOI] [PubMed] [Google Scholar]
- 11. Leshem E, Zilberman I, Tschabrunn CM, Barkagan M, Contreras-Valdes FM, Govari Aet al. . High-power and short-duration ablation for pulmonary vein isolation: biophysical characterization. JACC Clin Electrophysiol 2018;4:467–79. [DOI] [PubMed] [Google Scholar]
- 12. Barkagan M, Contreras-Valdes FM, Leshem E, Buxton AE, Nakagawa H, Anter E. High-power and short-duration ablation for pulmonary vein isolation: safety, efficacy, and long-term durability. J Cardiovasc Electrophysiol 2018;29:1287–96. [DOI] [PubMed] [Google Scholar]
- 13. Heeger C-H, Sano M, Popescu SȘ, Subin B, Feher M, Phan HLet al. . Very high-power short-duration ablation for pulmonary vein isolation utilizing a very-close protocol—the FAST AND FURIOUS PVI study. Europace 2022;25:880–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Popa MA, Bourier F, Lengauer S, Krafft H, Bahlke F, Förschner LVet al. . Safety profile and long-term efficacy of very high-power short-duration (60–70 W) catheter ablation for atrial fibrillation: results of a large comparative analysis. Europace 2022;25:408–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kottmaier M, Popa M, Bourier F, Reents T, Cifuentes J, Semmler Vet al. . Safety and outcome of very high-power short-duration ablation using 70 W for pulmonary vein isolation in patients with paroxysmal atrial fibrillation. Europace 2020;22:388–93. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available upon reasonable request; the corresponding authors may provide the data.