Abstract
Objectives:
Endometriosis originating in mesonephric cyst is unusual and with unknown prevalence. Endometriotic lesion in vestigial remnant of wolffian duct (mesonephric cyst) is exceptional. In the extended literature review only three cases have been reported in animal studies, and our case reported here is the first in human beings. We present a case of mesonephric cyst endometrioma in a 37-year-old patient who was referred for severe dysmenorrhea, long duration pelvic and back pain, subfertility, severe dyspareunia, and groin discomfort. The patient underwent laparoscopic removal and we performed a literature review to gain insight about the origin and surgical management of an atypical site endometriosis.
Methods and Procedures:
Case report presentation rests on information obtained from the patient database. We performed the literature review using a Medline search with the keywords: mesonephric cyst endometriosis, atypical location of endometriosis in vestigial remnant in wolffian duct, and Gartner duct cyst endometrioma.
Results:
On physical examination, fullness and tenderness in left adnexa and lateral vaginal wall fullness on left side with restricted mobility of uterus was noted. Based on the examination and imaging the left ovarian cyst and mesonephric cyst were suspected. Surgical exploration revealed the left hemorrhagic cyst with deep infiltrating endometriosis involving left ureter and left uterosacral ligament with mesonephric cyst endometriosis. The review of literature revealed three cases where ectopic endometrial tissue in mesonephric cyst remnant was found in female dogs.
Conclusion:
Mesonephric cyst endometrioma, although rare, can be a representative of extensive endometriosis. This case highlights an importance of careful clinical examination, correlation of patient symptoms with examination and imaging, and successful laparoscopic management of an atypical location endometriotic lesions. We completed the literature review on successful surgical management of such cases.
Keywords: Atypical site endometriosis, Deep infiltrating endometriosis, Endometrioma (chocolate cyst), Endometriosis, Gartner’s duct cyst, Mesonephric cyst, Operative laparoscopic surgery
INTRODUCTION
Endometriosis is defined as the presence of an endometrial gland and/or stroma in an ectopic location. Extragenital-intrapelvic and extragenital-extra pelvic endometriotic lesions spread by lymphatics, blood, or by direct dissemination. The typical cyclical symptoms are present only in 50% patients.1–5 Its pathogenesis is widely argued, and its inconsistent morphology represent a continuity of individual presentations and progressions. With increasing distance from uterus these lesions appear asynchronous with tendency to lose hormonal receptors. More often the distant lesions are independent of hormone stimulation supporting their premalignant potential if undiagnosed for many years. Undiagnosed, late detected, and untreated endometrioma can have premalignant potential.1–3 A mesonephric cyst (Gartner’s duct cyst) is a primitive remnant of the Wolffian duct in females and is benign in nature.4 This case is being reported to provide insight into a very rare location of endometriosis, symptoms correlation with location, its effect on fertility and premalignant potential if undetected for many years. Atypical site endometriosis is associated with diagnostic difficulties even on laparoscopy and missed by the expert on imaging studies.7
We report a case of mesonephric cyst endometrioma after missing it for many years, which was then removed, and complete clearance was obtained at the end of surgery. Only 3 cases have been reported in animal studies.8 We report a case of mesonephric cyst endometrioma as atypical location of endometriosis and its laparoscopic management to provide an insight about the rare presentation.
CASE REPORT
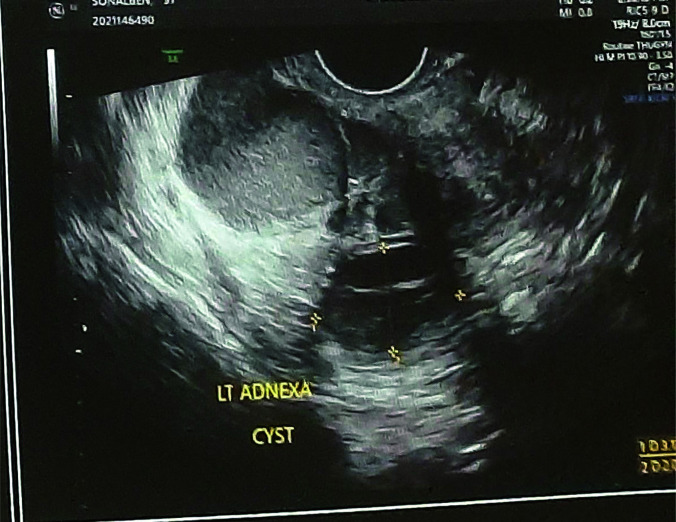
A 37-year-old female presented to the gynecological outpatient department with history of secondary infertility, chronic pelvic pain, cyclical lower backache, dyspareunia, and dysmenorrhea for 3 years. Apart from classical symptoms of endometriosis, she had atypical symptoms of groin discomfort, leg pain and hip discomfort, pain in gluteal region, and symptoms of acid reflux. The onset of menarche was 13 years. She had regular menstrual cycles with normal flow for many years post menarche. She had one spontaneous miscarriage in 2009 which was treated surgically by suction and evacuation. In 2017, she underwent diagnostic hysteroscopy and diagnostic laparoscopy as a part of a subfertility evaluation; findings on laparoscopy were mild congestion of the left tube and the left ovary was adherent in the ovarian fossa. On dye test, there was a free flow of methylene blue from both the tubes. There was no evidence of deep infiltrating endometriosis (uterosacral, retrocervical, rectovaginal septum, and vaginal fornix) at that time. The mesonephric cyst was missed on laparoscopic evaluation because of the location and uncommonness the of lesion. Husband semen parameters were within the normal range. The patient took infertility treatment in the form of ovulation induction in 2017 for many months and she did not conceive. She suffered with pelvic pain, low back pain, and subfertility for 4–5 years without any conclusive diagnosis. On physical examination, she had tenderness and fullness in left fornix and fullness in lateral vaginal wall on left side. Also, uterus mobility was restricted and painful. Transvaginal ultrasound was done which showed well defined left ovarian cyst with septation and of 30 × 30 mm size suggestive of left ovarian simple cyst which appeared adherent to the posterior surface of the uterus. Another cyst of 70 × 70 mm in size with dense echoes and homogenous ground glass appearance adjacent to the above-mentioned cyst was seen arising from the anterolateral aspect of the vagina on the left side and was seen separated from the left ovary suggestive of mesonephric cyst endometrioma (Figure 1). Considering all these findings, patient and her family members were counselled thoroughly about the possibility of the presence of endometriosis and its rare presentation causing all her atypical symptoms.
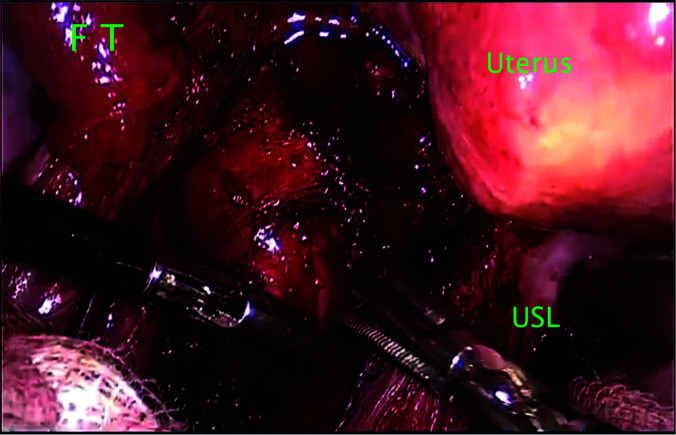
Figure 1.
Laparoscopic image of atypical site endometrioma below the left uterosacral ligament, lateral to fornix and arising from the apex of the vagina depicting the exact location of mesonephric cyst. Abbreviations: USL, uterosacral ligament; FT, fallopian tube.
RESULTS
The patient was taken for operative laparoscopy and removal of endometriotic lesions. The left ovarian cyst was drained, and a cystectomy was done. The peritoneum over the left ureter was excised and the ureter was traced up to the ureteric tunnel. The mesorectum of the left side was dissected with a harmonic scalpel and the rectum was separated from the medial wall of the lesion and the posterior wall of the uterus by sharp dissection with cold scissors. After adhesiolysis a cyst was found arising from the anterolateral wall of the proximal vagina extending towards and abutting rectovaginal space medially. The cyst was related to left ureter and left uterine artery laterally. Cranially it was extending into pararectal space and caudally it was related to the pelvic bone (Figure 2). The cyst was removed by blunt and sharp dissection after lateralization of the ureter. After the removal, the cyst was drained the chocolate material. Apart from this mesonephric cyst there was no evidence of deep infiltrating endometriosis involving rectovaginal septum, vaginal fornix, uterosacral ligaments, and retro cervical region. Histopathology of the ovarian cyst wall showed a simple cyst with no evidence of malignancy. Histopathology of another cyst from vaginal wall showed a mesonephric cyst with endometriotic implants. The postoperative period was uneventful. On the second day following surgery, the patient was discharged with no postoperative symptoms. After the surgery on follow up visits her symptoms of back pain and dyspareunia were relieved completely. Six months after the surgery, the patient conceived naturally.
Figure 2.
Ultrasound image of atypical location endometrioma adjacent to and separated from left ovary, with hemorrhagic cyst in left ovary.
DISCUSSION
Although endometriosis can affect almost any organ or structure, most endometriotic implants are in the pelvic cavity. Many ideas have been put out to describe the pathophysiology of endometriosis, both endometrial and nonendometrial in origin. The implantation theory, which indicates implantation and subsequent growth of retrograde shedding of viable endometrial cells, still is the most widely accepted theory to explain the pathogenesis.1–4 The second theory of in situ development in embryonic Mullerian cells, in which Mullerian cells have the capacity to convert into endometriotic lesions under the influence of estrogen. This theory supports the development of endometriosis in the vestigial remnants of the Wolffian ducts in our case. The benign metastasis through the lymphatics and/or hematogenous spread support the third theory of endometriotic lesions in distant organs like liver and lungs. A nonendometriotic origin concept, also termed as celomic metaplasia includes the transformation of peritoneal tissue to ectopic endometrial tissue via metaplasia.5 Extragenital malignant mixed mesodermal tumors (MMMTs) are extremely rare and have been associated with endometriosis, Wolfian duct remnants, and ovarian cyst adenocarcinoma. Twelve cases have been reported in the literature. With regard to the histogenesis of MMMTs in the extragenital tract or secondary mullerian system, the origin of such lesions could be in (1) endometriosis, (2) coelomic or subcoelomic structures, (3) Mullerian duct remnants, and (4) totipotential endometrial stromal cells with capacity for glandular and stromal differentiation.6
The mesonephric cyst is an embryonic remnant of the mesonephric duct in females and in many cases, it is associated with urinary system developmental abnormalities.4 Anatomically it is above the level of the inferior border of the pubic symphysis. Usually, it is a simple cyst and is lined by nonmucinous cuboidal or columnar epithelium.10 The presence of ectopic endometrium in mesonephric duct remnant has been found in one animal study.9 This finding supports the second concept of endometriosis origin theory. The catamenial nature of the symptoms (occurring between 24 hours before and 72 hours after the onset of menstruation) are present only in 50% of patients, but imaging is fundamental for the evaluation of exact location and size of the lesions.3–5 Transvaginal ultrasound is the most cost-effective imaging modality and should be performed first.1–3 Magnetic resonance imaging offers an added advantage compared to other imaging modalities due to high soft tissue contrast and multiplanar images.3 Mesonephric cyst endometrioma is exceptional.8 Because of enigmatic nature of endometriosis and absence of pathognomonic signs and symptoms the atypically located lesions escape for many years and has a great impact on patient fertility as observed in our case. The patient suffered for 4–5 years without any conclusive diagnosis. Such lesions can have premalignant potential which needs to be discussed with the patient and removal of such lesions can have better prognosis for quality of life and future fertility.6 In advanced stage of endometriosis and deep infiltrating endometriosis cases surgical excision is the ideal therapeutic option for definitive treatment compared to medical management, and comprehensive disease mapping before surgery is necessary to avoid residual disease.5,6
CONCLUSION
Our case report of Mesonephric cyst endometrioma is unique due to the atypical location, thorough surgical exploration and proven extensive pelvic involvement. The goal of conservative operative treatment in advanced stage endometriosis is to remove all implants, dissect all adhesions, relieve pain, restore anatomy, and improve fertility and quality of life. We report the first case of Mesonephric cyst endometrioma in human beings in the literature. Additional unique finding of our case is that the lesion was missed in previous laparoscopic exploration and magnetic resonance imaging done for low back pain. Late diagnosis is common in patients with atypical site endometriosis and is more common in those with extra pelvic disease with a documented delay of an average 4–5 years from the onset of symptoms. Thorough physical examination and correlation of symptoms with imaging remain the paramount important in evaluation and treatment of atypical site endometriosis. Surgical excision of such lesion is the best approach for definitive treatment.
Footnotes
Acknowledgement: Our grateful thanks to our surgical team and nursing staff of the hospital to help us at every point in taking care of the patient from preoperative to postoperative journey and completing this case report.
Conflict of interests: The authors report no declarations of interest.
Disclosure: none.
Funding source/financial support: none.
Informed consent: The authors declare that the patient's written informed consent was acquired before this case report and any associated photographs were published. All identifying information have been removed and ultrasound images were entirely anonymized.
Contributor Information
Ripal Madnani, Department of Reproductive Medicine and Infertility, First IVF Clinic, Dubai Healthcare City, Dubai, UAE. (Dr. Madnani).
Sandip Sonara, Department of Minimal Invasive Gynecological Surgery, Parikh Super Specialty Hospital, Ahmedabad, Gujarat, India. (Dr. Sonara).
References:
- 1. Dunselman GAJ, Vermeulen N, Becker C, et al. ESHRE guideline: management of women with endometriosis. Hum Reprod. 2014;29(3):400–412. [DOI] [PubMed] [Google Scholar]
- 2. Andres MP, et al. Extra pelvic endometriosis: a systematic review. J Minim Invasive Gynecol. 2020;27(2):373–389. [DOI] [PubMed] [Google Scholar]
- 3. Chamíe LP, Ribeiro DMFR, Tiferes DA, de Macedo Neto AC, Serafini PC. Atypical sites of deeply infiltrative endometriosis: clinical characteristics and imaging findings. Radiographics. 2018;38(1):309–328. [DOI] [PubMed] [Google Scholar]
- 4. Singh A, Shree S, Mishra V, Radhakrishnan G. Müllerian duct cyst misdiagnosed as ovarian cyst: a rare case report. Int J Reprod Contracept Obstet Gynecol. 2016;5(4):1260–1262. [Google Scholar]
- 5. Nezhat CH, Hincapie M, Gojayev A, Katz A. Suburethral endometriosis as clinical finding of extensive disease. CRSLS. 2022;9(1):e2021.00080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sampson JA. The development of the implantation theory for the origin of peritoneal endometriosis. Am J Obstet Gynecol. 1940;40(4):549–557. [Google Scholar]
- 7. Solis OG, Bui HX, Malfetano JH, Ross JS. Extragenital primary mixed malignant mesodermal tumor. Gynecol Oncol. 1991;43(2):182–185. [DOI] [PubMed] [Google Scholar]
- 8. Andrade MT, de Freitas CV, Câmara SF, Vieira JJ. Umbilical nodule with cyclical bleeding: a case report and literature review of atypical endometriosis. Case Rep Obstet Gynecol. 2016;2016:7401409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bartel C, Berghold P, Walter I. Ectopic endometrial tissue in mesonephric duct remnants in bitches. Reprod Domest Anim. 2011;46(6):950–956. [DOI] [PubMed] [Google Scholar]
- 10. Radswiki T, Yap J, Baba Y, et al. Gartner duct cyst. Reference article. Available at: 10.53347/rID-12523 Accessed November 25, 2022. [DOI] [Google Scholar]