Abstract
Background
Functional dyspepsia (FD) has been a worldwide complaint. More effective therapies are needed with fewer adverse effects than are seen with conventional medications. Acupuncture, as a traditional therapeutic method, has been widely used for functional gastrointestinal disorders in the East. Manual acupuncture and electroacupuncture have been recognized treatments for FD, but to date, no robust evidence has been found for the effectiveness and safety of these interventions in the treatment of this condition.
Objectives
This review was conducted to assess the efficacy and safety of manual acupuncture and electroacupuncture in the treatment of FD.
Search methods
Trials meeting the inclusion criteria were identified through electronic searches of the Cochrane Central Register of Controlled Trials (CENTRAL), MEDLINE, EMBASE, the Allied and Complementary Medicine Database (AMED), Chinese Biology Medicine Disc (CBMdisc), China National Knowledge Infrastructure (CNKI), the Wanfang Database, the VIP Database, and six trial registries. Handsearching was done to screen the reference sections of potential trials and reviews.
Selection criteria
Randomized controlled trials (RCTs) were included if investigators reported efficacy and safety of manual acupuncture or electroacupuncture for patients with FD diagnosed by Rome II or Rome III criteria, compared with medications, blank control, or sham acupuncture.
Data collection and analysis
Data were extracted by independent review authors. Study limitations were assessed by using the tool of The Cochrane Collabration for assessing risk of bias. For dichotomous data, risk ratios (RRs) and 95% confidence intervals (95% CIs) would be applied, and for continuous data, mean differences (MDs) and 95% CIs. A fixed‐effect model was applied in the meta‐analysis, or a descriptive analysis was performed. The quality of evidence for the outcome measure was assessed by the Grading of Recommendations Assessment, Development and Evaluation (GRADE) methods.
Main results
Seven studies were included in the review, involving 542 participants with FD (212 males and 330 females). These studies generally had an unclear risk of bias based on inadequate descriptions of allocation concealment and a high risk of bias based on lack of blinding. None of the studies reported on outcomes of the Functional Digestive Disorder Quality of Life questionnaire (FDDQL), the Satisfaction With Dyspepsia Related Health scale (SODA), the Digestive Health Status Instrument (DHSI), or effective/inefficient rate and symptom recurrence six months from completion of acupuncture treatment.
Four RCTs of acupuncture versus medications (cisapride, domperidone, and itopride) were included in the review. No statistically significant difference was noted in the reduction in FD symptom scores and the frequency of FD attack by manual acupuncture, manual‐electroacupuncture, or electroacupuncture compared with medications. In three trials of acupuncture versus sham acupuncture, all descriptive or quantitative analysis results implied that acupuncture could improve FD symptom scores and scores on the Neck Disability Index (NDI), the 36‐Item Short Form Health Survey (SF‐36), the Self‐Rating Anxiety Scale (SAS), and the Self‐Rating Depression Scale (SDS) more or as significantly as sham acupuncture. With regard to adverse effects, acupuncture was superior to cisapride treatment (one study; all minor events), but no statistically significant difference was reported between acupuncture and sham acupuncture. No adverse effects data were reported in studies examining manual acupuncture versus domperidone, manual‐electroacupuncture versus domperidone, or electroacupuncture versus itopride.
Nevertheless, all evidence was of low or very low quality. The body of evidence identified cannot yet permit a robust conclusion regarding the efficacy and safety of acupuncture for FD.
Authors' conclusions
It remains unknown whether manual acupuncture or electroacupuncture is more effective or safer than other treatments for patients with FD.
Plain language summary
Acupuncture for treating functional dyspepsia
Functional dyspepsia (FD) has been a worldwide gastric disorder. More effective therapies are needed with fewer adverse effects than are seen with conventional medications. In the East, acupuncture has been recognized for a long time as a positive therapy for the treatment of functional gastric disorders. To date, no robust evidence on its efficacy and safety has been found. The evidence obtained has overwhelmingly supported no significance of acupuncture compared with medications and superiority of acupuncture compared with sham acupuncture in FD treatment; however, the low quality of evidence obtained has not permitted a robust conclusion concerning the efficacy and safety of acupuncture in the treatment of FD.
Summary of findings
Summary of findings for the main comparison. Manual acupuncture compared with cisapride for functional dyspepsia.
| Manual acupuncture compared with cisapride for functional dyspepsia | ||||||
| Patient or population: patients with functional dyspepsia Settings: outpatients of Yangqing TCM Hospital in Beijing,China Intervention: manual acupuncture Comparison: cisapride | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| CISAPRIDE | MANUAL ACUPUNCTURE | |||||
| Symptom scores of FD Graded by 4 levels1 | 911 per 10002 | 929 per 1000 (829 to 1000)2 | RR 1.02 (0.91 to 1.16) | 90 (1 study) | ⊕⊝⊝⊝ very low3,4,5 | |
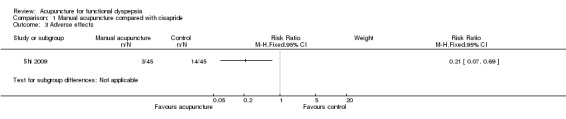
| Adverse effects Discomfort after treatment | 311 per 1000 | 65 per 1000 (22 to 215) | RR 0.21 (0.07 to 0.69) | 90 (1 study) | ⊕⊝⊝⊝ very low3,4 | |
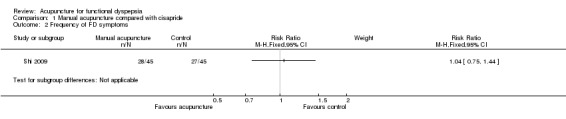
| Frequency of FD symptoms Number of FD attacks per week | 600 per 10006 | 624 per 1000 (450 to 840)6 | RR 1.04 (0.75 to 1.4) | 90 (1 study) | ⊕⊝⊝⊝ very low3,4 | |
| *The basis for the assumed risk (eg, median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
10 points meant no symptoms, 1 point stood for slight symptoms, 2 points indicated moderate symptoms but not sufficient to affect daily life, and 3 points represented symptoms severe enough to affect daily life. Effective rate = (symptom scores after treatment‐symptom scores before treatment)*100%. When equal to or greater than 25%, this meant "effective," equal to or greater than 50% meant "marked effective,; and equal to or greater than 75% meant "healing" effect. "Effective," "marked effective," and "healing" are categorized as "positive effect," and "invalid" as "negative effect." 2Event of FD symptom scores means positive effect. 3Blinding was not easy to conduct because of the heterogeneity of acupuncture and drug control. Also, FD symptom scores at baseline were not reported. Thus, we consider this evidence would be downgraded by 2 levels because of its risk of bias. 4The number of participants was lower than the optimal information sample size, so the quality of evidence was downgraded by 1 level for imprecision. 5FD symptom scores at baseline were not reported 6Event of FD symptom frequency means no FD attacks per week.
Summary of findings 2. Manual acupuncture compared with domperidone for functional dyspepsia.
| Manual acupuncture compared with domperidone for functional dyspepsia | ||||||
| Patient or population: patients with functional dyspepsia Settings: outpatients from People's Hospital of Guangxi Zhuang Autonomous Region, Guangxi Province, China Intervention: manual acupuncture Comparison: domperidone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| DOMPERIDONE | MANUAL ACUPUNCTURE | |||||
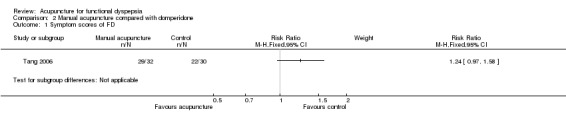
| Symptom scores of FD Graded by 4 levels1 | 733 per 10002 | 909 per 1000 (711 to 1000)2 | RR 1.24 (0.97 to 1.58) | 62 (1 study) | ⊕⊕⊝⊝ low3,4 | |
| *The basis for the assumed risk (eg, median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
10 points meant no symptoms, 1 point stood for slight symptoms, 2 points indicated moderate symptoms but not sufficient to affect daily life, and 3 points represented symptoms severe enough to affect daily life. Effective rate = (symptom scores after treatment‐symptom scores before treatment)*100%. When equal to or greater than 25%, this meant "effective," equal to or greater than 50% meant "marked effective," and equal to or greater than 75% meant "healing" effect. "Effective," "marked effective," and "healing" are categorized as "positive effect," and "invalid" as "negative effect." 2Event of FD symptom scores means positive effect. 3Blinding was probably not done, thus the evidence was downgraded by 1 level. 4The number of participants was lower than the optimal information sample size, so the quality of evidence was downgraded by 1 level for imprecision.
Summary of findings 3. Manual‐electroacupuncture compared with domperidone for functional dyspepsia.
| Manual‐electroacupuncture compared with domperidone for functional dyspepsia | ||||||
| Patient or population: patients with functional dyspepsia Settings: outpatients from Shanghai No. 5 People's Hospital Affiliated to Fudan University, Shanghai, China Intervention: manual‐electroacupuncture Comparison: domperidone | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| DOMPERIDONE | MANUAL‐ELECTROACUPUNCTURE | |||||
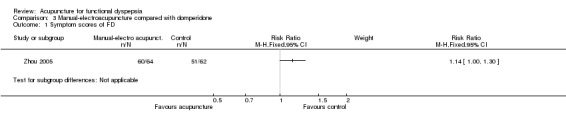
| Symptom scores of FD Graded by 4 levels1 | 823 per 10002 | 938 per 1000 (823 to 1000)2 | RR 1.14 (1 to 1.3) | 126 (1 study) | ⊕⊝⊝⊝ very low3,4 | |
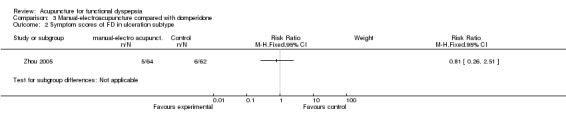
| Symptom scores of ulceration subtype Graded by 4 levels1 | 97 per 10005 | 78 per 1000 (25 to 243)5 | RR 0.81 (0.26 to 2.51) | 126 (1 study) | ⊕⊝⊝⊝ very low3,6 | |
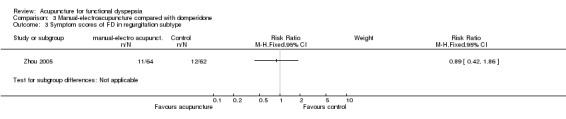
| Symptom scores of regurgitation subtype Graded by 4 levels1 | 32 per 10005 | 29 per 1000 (14 to 60)5 | RR 0.89 (0.42 to 1.86) | 126 (1 study) | ⊕⊝⊝⊝ very low3,6 | |
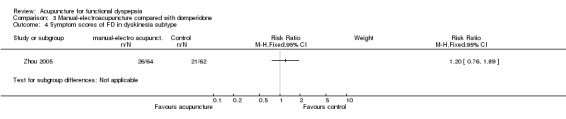
| Symptom scores of dyskinesia subtype Graded by 4 levels1 | 5 | 5 | RR 1.2 (0.76 to 1.89) | 126 (1 study) | ⊕⊝⊝⊝ very low3,6 | |
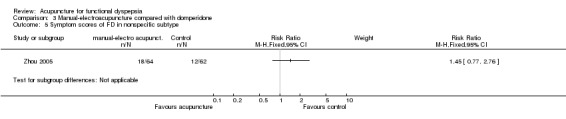
| Symptom scores of nonspecific subtype Graded by 4 levels1 | 5 | 5 | RR 1.45 (0.77 to 2.76) | 126 (1 study) | ⊕⊝⊝⊝ very low3,6 | |
| *The basis for the assumed risk (eg, median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
10 points meant no symptoms, 1 point stood for slight symptoms, 2 points indicated moderate symptoms but not sufficient to affect daily life, and 3 points represented symptoms severe enough to affect daily life. Effective rate = (symptom scores after treatment‐symptom scores before treatment)*100%. When equal to or greater than 25%, this meant "effective," equal to or greater than 50% meant "marked effective," and equal to or greater than 75% meant "healing" effect. "Effective," "marked effective," and "healing" are categorized as "positive effect," and "invalid" as "negative effect." 2Event of FD symptom scores means positive effect. 3Blinding was probably not done. Also, FD symptom scores at baseline were lacking. Thus, the evidence was downgraded by 2 levels. 4FD symptom scores at baseline were omitted. 5Event of FD subtype symptom scores means positive effect. 6The number of participants was lower than the optimal information sample size, so the quality of evidence was downgraded by 1 level for imprecision.
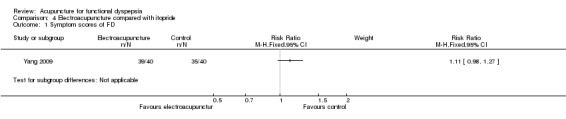
Summary of findings 4. Electroacupuncture compared with itopride for functional dyspepsia.
| Electroacupuncture compared with itopride for functional dyspepsia | ||||||
| Patient or population: patients with functional dyspepsia Settings: outpatients from Wuhan Hospital of Traditional Medicine and Western Medicine, Hubei Province, China Intervention: electroacupuncture Comparison: itopride | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| ITOPRIDE | ELECTROACUPUNCTURE | |||||
| Symptom scores of FD Graded by 4 levels1 | 875 per 10002 | 971 per 1000 (858 to 1000)2 | RR 1.11 (0.98 to 1.27) | 80 (1 study) | ⊕⊕⊝⊝ low3,4 | |
| *The basis for the assumed risk (eg, median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval; RR: Risk ratio. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
10 points meant no symptoms, 1 point stood for slight symptoms, 2 points indicated moderate symptoms but not sufficient to affect daily life, and 3 points represented symptoms severe enough to affect daily life. Effective rate = (symptom scores after treatment‐symptom scores before treatment)*100%. When equal to or greater than 25%, this meant "effective," equal to or greater than 50% meant "marked effective," and equal to or greater than 75% meant "healing" effect. "Effective," "marked effective," and "healing" are categorized as "positive effect," and "invalid" as "negative effect." 2Event of FD symptom scores means positive effect. 3Blinding was probably not done, thus the evidence was downgraded by 1 level. 4The number of participants did not reach the optimal information sample size, thus we consider the evidence to be downgraded by 1 level.
Summary of findings 5. Acupuncture compared with sham acupuncture for functional dyspepsia.
| Acupuncture compared with sham acupuncture for functional dyspepsia | ||||||
| Patient or population: patients with functional dyspepsia Settings: outpatients from No, 1 Affiliated Hospital of Hunan Universtiy of TCM, the Guan'anmen Hospital of China Academy of Chinese Medicine Science, the Korean Oriental Medicine Clinics Intervention: acupuncture Comparison: sham acupuncture | ||||||
| Outcomes | Illustrative comparative risks* (95% CI) | Relative effect (95% CI) | No. of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | |||||
| SHAM ACUPUNCTURE | ACUPUNCTURE | |||||
| FD symptom scores Graded by 4 levels1 Follow‐up: 1˜3 months | See comment | See comment | Not estimable | 116 (2 studies) | ⊕⊕⊝⊝ low2,3 | |
| FD symptom scores at follow‐up Graded by 4 levels1 Follow‐up: 1˜3 months | See comment | See comment | Not estimable | 116 (2 studies) | ⊕⊕⊝⊝ low2,3 | |
| Nepean Dyspepsia Symptom Index Follow‐up: 0˜1 months | See comment | See comment | Not estimable | 128 (2 studies) | ⊕⊕⊝⊝ low2,3 | |
| Nepean Dyspepsia Life Quality Index Follow‐up: 0˜1 months | See comment | See comment | Not estimable | 128 (2 studies) | ⊕⊕⊝⊝ low2 | |
| Nepean Dyspepsia Symptom Index at follow‐up 1 month Follow‐up: 1 month | Mean Nepean Dyspepsia Symptom Index at follow‐up 1 month in the control groups was 27.69 points | Mean Nepean Dyspepsia Symptom Index at follow‐up 1 month in the intervention groups was 16.63 lower (24.513 to 8.75 lower) | 60 (1 study) | ⊕⊕⊝⊝ low2,3 | ||
| Nepean Dyspepsia Life Quality Index at follow‐up of 1 month Follow‐up: 1 month | Mean Nepean Dyspepsia Life Quality Index at follow‐up of 1 month in the control groups was 82.10 points | Mean Nepean Dyspepsia Life Quality Index at follow‐up 1 month in the intervention groups was 13.64 higher (8.22 to 19.06 higher) | 60 (1 study) | ⊕⊕⊝⊝ low2 | ||
| SF‐36 SF‐36 scale Follow‐up: 1˜3 months | Mean SF‐36 ranged across control groups from 56˜75.53 points | Mean SF‐36 in the intervention groups was 12.18 higher (8.45 to 15.91 higher) | 116 (2 studies) | ⊕⊕⊝⊝ low2,3 | ||
| *The basis for the assumed risk (eg, median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: Confidence interval. | ||||||
| GRADE Working Group grades of evidence. High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||||
10 points meant no symptoms, 1 point stood for slight symptoms, 2 points indicated moderate symptoms but not sufficient to affect daily life, and 3 points represented symptoms severe enough to affect daily life. 2Blinding cannot be confirmed because of the difficulty of the acupuncture operation. Thus, we consider evidence to be downgraded by 1 level. 3The number of participants did not reach the optimal information sample size; thus we consider the evidence to be downgraded by 1 level.
Background
Description of the condition
Functional dyspepsia (FD) is a common complaint regardless of geographic location (Mahadeva 2006). The prevalence of FD diagnosed by Rome I or Rome II criteria has been noted to vary between 11% and 29.2% (Mahadeva 2006). Patients who report one or more of a set of symptoms (bothersome postprandial fullness, early satiation, epigastric pain, and epigastric burning) for three months, with symptom onset at least six months before diagnosis, and who lack indicators of structural disease likely to explain the symptoms (including evidence from upper endoscopy) will be given a diagnosis of FD (Rome III 2006).
The main therapeutic methods used in patients with FD include prokinetic agents, Helicobacter pylori eradication, proton pump inhibitors (PPIs), tricyclic antidepressants (TCAs), histamine type 2 receptor antagonists, and serotonin reuptake inhibitors. However, the efficacy of these approaches remains unsatisfactory because of associated adverse effects. Take prokinetic drugs, for example. Despite early promising results, itopride and mosapride were reported to be no better than placebo in a study in Japan (Holtmann 2006). Less than 60% of patients with FD report improved symptoms with medication, and the efficacy of drug therapy usually varies (Mönkemüller 2006). Also, the adverse effects associated with drugs and the recurrence of symptoms reported by patients have presented challenges for researchers and clinicians.
Scientific observations on the pathophysiology of functional gastrointestinal disorders focus mainly on such items as abnormal motility, inflammation and bacterial flora, visceral hypersensitivity, brain‐gut interactions, genetic predisposition, early family environment, and psychosocial factors (Drossman 2006). This suggests the complicated pathologic mechanisms and the heterogeneity of the disease.
Description of the intervention
Acupuncture is one of the most important therapeutic modalities in traditional Chinese medicine (TCM). Acupuncture uses fine needles that may pierce through specific anatomic points (named 'acupoints') so that certain healing effects are produced (Deng 1997). Acupuncture has been applied for a long time in the treatment of dyspepsia. LI 4 (Hegu) on the Large Intestine Meridian, ST36 (Zu Sanli) on the Stomach Meridian, and CV12 (Zhongwan) are the best known acupoints in the treatment of dyspepsia. Traditional acupuncture commonly includes manual acupuncture; however, in recent decades, electrical acupuncture, in which an electrical stimulator is connected to the acupuncture needle, has been used frequently (Lao 1996). Now, manual acupuncture and electroacupuncture are the most frequently used acupuncture techniques for treatment of this condition.
How the intervention might work
Discomfort or pain or both are requisite symptoms of FD. Research has demonstrated that acupuncture could improve gastric emptying and accommodation to improve the symptoms of FD (Xu 2004). Investigators have further observed that acupuncture to the abdomen can excite sympathetic nerves via spinal reflexes, causing inhibition of gastric motilities; acupuncture of the limbs excites vagus nerves via supraspinal reflexes, causing an increase in gastric motility (Noguchi 2008). Functional neuroimaging studies have revealed that in patients with FD, resting cerebral glycometabolism differs significantly from that in healthy individuals, and the anterior cingulate cortex, insula, thalamus, middle cingulate cortex, and cerebellum might be key regions that determine the severity of symptoms (Zeng 2011); symptom improvement was found to be relevant with deactivation of the primary somatosensory area and the cerebellum as a response to acupuncture stimulation (Zeng 2009).
Why it is important to do this review
Manual acupuncture and electroacupuncture have been recognized treatments for FD in the East, but to date, no robust evidence has shown their effectiveness and safety in the treatment of patients with FD.
Objectives
This review was conducted to assess the efficacy and safety of manual acupuncture and electroacupuncture in the treatment of FD.
Methods
Criteria for considering studies for this review
Types of studies
Only randomized controlled trials (RCTs) reporting clinical assessment were included. Quasi‐RCTs, cross‐over trials, cluster‐randomized trials, and other study designs were excluded. Language restriction was not applied during study selection.
Types of participants
Studies involving participants older than 17 years of age who met Rome II or Rome III diagnostic criteria for FD were included without limitations related to gender or race. Studies involving participants with structural, systemic, or metabolic disease, severe psychiatric sickness, or a history of abdominal operations were excluded.
Types of interventions
Trials involving manual acupuncture or electroacupuncture were included. Also included were studies in which acupuncture techniques and other treatments were provided to the intervention group, as long as all methods except acupuncture therapy were applied to both treatment and control groups. Studies in which any acupuncture techniques were compared with one other or with Chinese herbs were excluded.
Comparisons
Manual acupuncture or electroacupuncture or their combination versus no treatment.
Manual acupuncture or electroacupuncture or their combination versus placebo acupuncture (sham acupuncture, minimal acupuncture, etc.).
Manual acupuncture or electroacupuncture or their combination versus medication.
Types of outcome measures
Primary outcomes
-
Symptomatic improvement in any of the following.
Symptom scores.
Nepean Dyspepsia Index (NDI).
Functional Digestive Disorder Quality of Life questionnaire (FDDQL).
Satisfaction With Dyspepsia Related Health scale (SODA).
Digestive Health Status Instrument (DHSI).
Effective rate, inefficient rate, etc.
No symptom recurrence six months from completion of acupuncture treatment.
Secondary outcomes
Medical Outcome Study Short Form Health Survey (SF‐36).
Self‐Rating Depression Scale (SDS), Self‐Rating Anxiety Scale (SAS).
Adverse events.
Search methods for identification of studies
Trials meeting the inclusion criteria were identified through electronic searches and by handsearching.
Electronic searches
The following bibliographic databases were searched.
The Cochrane Central Register of Controlled Trials (CENTRAL) 2012, Issue 1 (part of The Cochrane Library) (Appendix 1).
MEDLINE (1950 to February 2012) (Appendix 2).
EMBASE (1980 to February 2012) (Appendix 3).
AMED (Allied and Complementary Medicine Database) (1985 to February 2012) (Appendix 4).
CNKI (China National Knowledge Infrastructure) (1999 to February 2012) (Appendix 5).
VIP Database (1999 to February 2012) (Appendix 6).
CBMdisc (Chinese Biology Medicine Disc) (1999 to February 2012) (Appendix 7).
Wanfang Database (1999 to February 2012) (Appendix 8).
Chinese databases were searched back to 1999, the date when the ROME II diagnostic criteria were first used, and when functional dyspepsia was first known by Chinese researchers.
Trial registries were searched using the keywords "functional dyspepsia" and "acupuncture."
ACTR (http://www.actr.org.au/).
BNRR (http://www.nrr.nhs.uk).
Chinese Clinical Trial Register (www.chictr.org).
Clinical Trials (http://www.clinicaltrials.gov),
Trial Central (http://www.trialscentral.org/).
Searching other resources
Handsearching was done to screen reference sections of identified studies for potential trials or reviews.
Data collection and analysis
Selection of studies
Review author Lan L inspected English titles and abstracts identified by the literature search of MEDLINE, EMBASE, AMED, CENTRAL, and several trial registries. Review author Liu ML scanned the Chinese search lists of CBM, CNKI, VIP, and Wanfang databases. When it was not known from titles and abstracts whether a study should be included, copies of trials were requested for further identification. All identified trials were downloaded in full‐text form, and references were inspected to search for potential RCTs of acupuncture for FD. Studies excluded or awaiting classification were recorded in detail, and a third review author (Wu X) checked them randomly.
Data extraction and management
Review authors Liu ML , Zeng F, and Ying L drafted data extraction items and performed a pretest. Disagreement led to consultation with Lan L. Then Zeng F and Ying L independently extracted data into Review Manager software (RevMan 2011). If needed, authors of trials were contacted and were asked to provide incomplete data.
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias in each included trial, involving sequence generation; allocation concealment; blinding of participants, personnel, and outcome assessors; incomplete outcome data; and selective reporting. Consensus was used to resolve disagreements, and a third review author was consulted when disagreement persisted.
The Grading of Recommendations Assessment, Development and Evaluation (GRADE system) was applied to confirm the level of evidence and the strength of the recommendation.
Measures of treatment effect
Meta‐analysis was conducted on the basis of homogeneity of included trials. For dichotomous data, risk ratios (RRs) and 95% confidence intervals (95% CIs) were applied. For continuous data, mean differences (MDs) and 95% CIs were used for analyses.
Dealing with missing data
The problem of missing data was resolved by contacting the original investigators to request the missing information. If data were not obtained, trials with incomplete data involving inclusion criteria would be listed in the Characteristics of studies awaiting classification section, along with a description of the reason, and will be included in updates of this review (Higgins 2011).
Assessment of heterogeneity
The I² statistic was used to assess heterogeneity (Higgins 2003). Values lower than 50% suggested homogeneity; values of 50% or higher were indicative of heterogeneity. However, when values were very close to but lower than 50%, review authors determined whether meta‐analysis would be conducted.
Data synthesis
A fixed‐effect model was applied in the meta‐analysis if heterogeneity did not exist. When inconsistency was noted, causes of heterogeneity were detected first by subgroup analysis. If this did not occur, a random‐effects model was applied. Results obtained by the random‐effects model were interpreted with caution.
Subgroup analysis and investigation of heterogeneity
Subgroup analysis was not performed because of the small number of trials.
Sensitivity analysis
Sensitivity analysis was not conducted because of lack of available data.
Results
Description of studies
Results of the search
A total of 681 citations were retrieved through the literature search. Upon screening of titles, abstracts, and full text, 17 potential studies were found to meet the inclusion criteria, three of which were awaiting classification for lack of full text to confirm study details. One study was awaiting classification because of difficulty associated with getting in touch with the study author and having unclear data explained, and six studies were excluded with reasons. Eventually, seven studies were included. Details can be seen in Figure 1.
1.
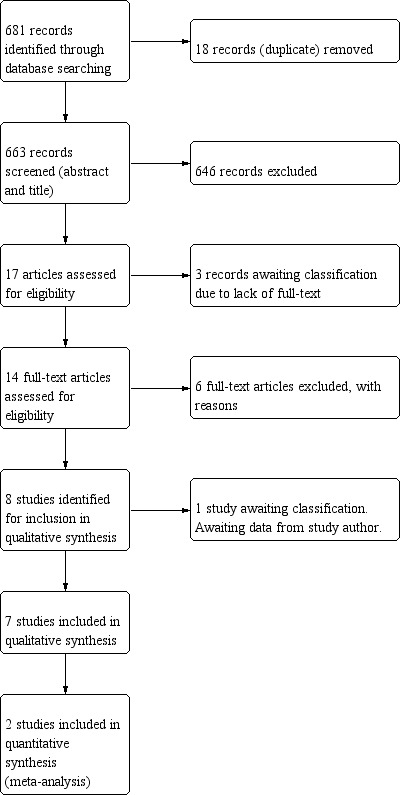
Study flow diagram.
Included studies
External characteristics
Seven RCTs were verified to be included, five of which were fully published papers (Chang 2010; Park 2009; Shi 2009; Tang 2006; Zhou 2005); two studies were unpublished (Jin 2011; Yang 2009). Among the seven trials, five were written in Chinese (Chang 2010; Jin 2011; Shi 2009; Tang 2006; Yang 2009) and two in English (Park 2009; Zhou 2005).
Participants
Seven trials included 542 participants with FD—212 males and 330 females. All participants were Chinese and were enrolled as hospital outpatients, except those from the Korean population studied in Park 2009. Participant age was reported to range from 18 years (Shi 2009) to 70 years (Jin 2011). Duration of FD symptoms before recruitment ranged from three months (Tang 2006) to 480 months (Jin 2011). Rome II criteria were used to diagnose FD in three trials (Park 2009; Tang 2006; Zhou 2005), and Rome III criteria were used for the other four trials (Chang 2010; Jin 2011; Shi 2009; Yang 2009).
For the inclusion criteria, the highlight character of included participants in seven studies was absent from organic diseases. Also, two studies described clearly that medication intake was avoided before enrollment or treatment. Yang 2009 instructed participants to refrain from taking any gastrointestinal drugs for at least 15 days before recruitment, and Zhou 2005 demanded that participants withdraw from anticholinergic, anticonvulsant, emetic, or H‐receptor antagonist treatment one week before the start of acupuncture treatment. Additionally, participants in Tang 2006 were required to have symptoms lasting at least one month before enrollment.
Among exclusion criteria, pregnancy was mentioned in four studies (Chang 2010; Jin 2011; Shi 2009; Yang 2009). One study described in the exclusion criteria people with a tendency toward bleeding and those with unconsciousness (Yang 2009).
Interventions
All included trials provided details of baseline comparability, except Zhou 2005 and Shi 2009. Interventions applied included manual acupuncture or electroacupuncture versus oral drugs in four studies (Shi 2009; Tang 2006; Yang 2009; Zhou 2005), and manual acupuncture versus sham acupuncture (puncturing sham acupoints) in three studies (Chang 2010; Jin 2011; Park 2009). Zhou 2005 compared manual acupuncture treatment on CV12, PC6, and LI4 acupoints combined with electroacupuncture on ST36 and SP6 acupoints with domperidone usage of three weeks' duration. Tang 2006 compared four‐week manual acupuncture treatment on ST36, CV12, PC6, LR3, BL15, BL19, BL20, BL21, and ST44 acupoints with four‐week domperidone administration. Yang 2009 compared four‐week electroacupuncture treatment on ST34, ST36, ST40, and ST42 acupoints with four‐week itopride administration. Shi 2009 compared manual acupuncture using mainly ST36, CV12, and PC6 acupoints with cisapride of three weeks' treatment duration. Park 2009 applied two‐week manual acupuncture on LI4, LR3, PC6, SP4, ST36, and CV12 acupoints compared with puncturing on sham acupoints lateral to the aforementioned acupoints. Chang 2010 and Jin 2011 separately compared manual acupuncture on acupoints of the formulae composed of ST32, ST36, ST40, ST42 or ST36, and KI 3, with sham acupuncture on points lateral to the aforesaid acupoints of four weeks' duration. Only Chang 2010 and Jin 2011 reported separately follow‐up assessment one month and three months after interventions were provided.
For acupuncture interventions, therapists in included trials were licensed doctors and were required to perform lifting, thrusting, and rotating manipulations. Needle brands and sizes were clearly described in Park 2009, Chang 2010, and Jin 2011. Although acupoints used were heterogeneous, acupuncture style was traditional Chinese acupuncture, except that of Park 2009, in which acupoints were selected on the basis of traditional Chinese acupuncture theory. "De‐qi" sensations were considered vital for efficacy in traditional Chinese acupuncture. All studies except Park 2009 were required to perform manipulations to a specific depth until "de‐qi" occurred at least three times per week.
For the control interventions, medication was administered orally before three meals per day for a similar treatment duration as acupuncture, and sham acupuncture consisted of puncturing points lateral to acupoints. Co‐interventions of manual acupuncture combined with electroacupuncture were found in Zhou 2005.
No trials reported data on acupuncture versus waiting list for treatment of FD.
Outcome measures
For the primary outcome measures, symptom scores of FD were applied in all included studies, except Park 2009, in which zero points meant no symptoms, one point stood for slight symptoms, two points indicated moderate symptoms but not sufficient to affect daily life, and three points represented symptoms severe enough to affect daily life. Investigators also described how to assess efficacy through symptom scores of FD. Shi 2009 calculated the effective rate (difference/(pretreatment score) *100%), limited effective rate to mean positive effect when it was equal to or greater than 25%, and reported efficacy as effective or invalid. Tang 2006 described that efficacy consisted of four levels: healing (no symptoms and no recurrence one month after treatment), marked effective (symptom scores after treatment decreased by more than two‐thirds), effective (symptom scores after treatment decreased by more than one‐third), and invalid (symptom scores after treatment decreased by less than one‐third). Yang 2009 described four similar levels of efficacy, healing (no symptoms or symptom scores decreased by three points), marked effective (symptom scores after treatment decreased by two points), effective (symptom scores after treatment decreased by one point), and invalid (symptom scores after treatment hardly decreased). Zhou 2005 reported the same efficacy assessment as Yang 2009, except without a "healing" description. Chang 2010 and Jin 2011 reported FD scores for pretreatment, post‐treatment, and follow‐up.
Another primary outcome (NDI) was used to assess efficacy in Park 2009 and Chang 2010. Both trials separately showed two types of NDI scores between groups: Nepean Dyspepsia Symptom Index (NDSI) and Nepean Dyspepsia Life Quality Index (NDLQI).
None of these studies reported on outcomes of the Functional Digestive Disorder Quality of Life questionnaire (FDDQL), the Satisfaction With Dyspepsia Related Health scale (SODA), the Digestive Health Status Instrument (DHSI), effective/inefficient rates, and symptom recurrence six months from completion of acupuncture treatment.
For secondary outcome measures, SF‐36 was used to assess life quality between groups in Chang 2010 and Jin 2011. SAS, SDS, and adverse events were reported in Jin 2011. Additionally, Shi 2009 assessed frequency of FD symptoms between groups; zero points meant no attack, one point indicated one to three attacks per week, two points showed four to six attacks per week, and three points represented attacks every day as well as adverse effects of interventions. Jin 2011 described scores for each FD symptom before and after treatment. Zhou 2005 also reported symptom scores for each subtype diagnosed by Rome II FD criteria and assessed efficacy as totally effective or invalid.
Excluded studies
Six trials were excluded for the following reasons: One study did not clearly state the dyspepsia diagnostic criterion (Paterson 2003); one study was a cross‐over trial (Liu S 2008); one study was a letter to the editors (Beyazit 2010); three studies were quasi‐RCTs in which participants were allocated in terms of visiting time (Chen 2005; Peng 2008; Yang 2009a); three studies were awaiting classification for failure to identify full texts (Cao 2007; Cash 2001; Sun 2006); and one study was excluded because the review authors were unable to get in touch with the study author to have unclear data explained (Zhang 2009b).
Risk of bias in included studies
Results of risk of bias can be seen in Figure 2 and Figure 3. The most frequent bias was noted in blinding. For characteristics of acupuncture manipulations, it is too difficult to conduct blinding for therapists and participants, especially those familiar with acupuncture. Another bias involved lack of comprehensive descriptions of randomization concealment. For the quality of evidence assessment performed using the GRADE system, almost all evidence from outcomes was found to be of low quality (Table 2; Table 4; Table 5) or very low quality (Table 1; Table 3; Table 5).
2.
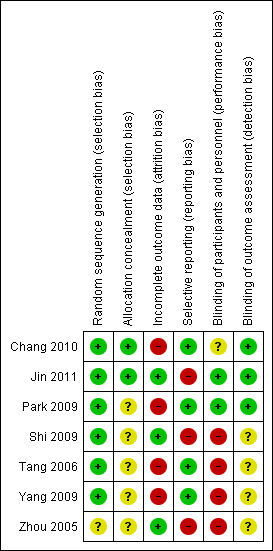
Methodological quality summary: review authors' judgements about each methodological quality item for each included study.
3.
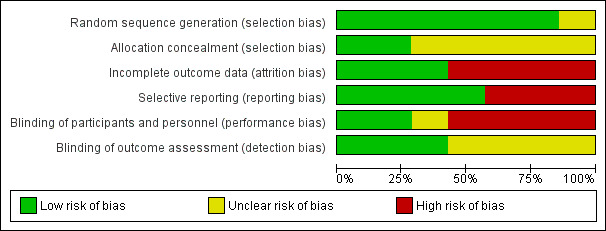
Methodological quality graph: review authors' judgements about each methodological quality item presented as percentages across all included studies.
Allocation
Random sequence generation
Zhou 2005 just briefly mentioned random allocation but neglected to state the random method used and assessed unclear risk of bias. Other included trials described the method of random generation and were determned to have low bias risk.
Random concealment
Central randomization could ensure sequence concealment in Chang 2010; sealed, opaque, and sequentially numbered envelopes were helpful for validating the random unknown in Jin 2011. Other included trials did not describe random concealment and were assessed as having unclear risk of bias.
Blinding
Blinding of participants and personnel
Both Park 2009 and Jin 2011 reported that the same therapist would conduct the manipulations in acupuncture and control groups, and that participants were blinded to the formula. Thus, these trials were assessed as having low risk of bias. Chang 2010 did not offer any explanation of blinding and was assessed to have an unclear risk of bias. As acupuncture was so different from medication, and no details were obtained from the other four included trials, all were assessed as having high risk of bias.
Blinding of outcome assessment
Park 2009, Chang 2010, and Jin 2011 described that assessors were blinded to allocation; therefore these studies were assessed as having low risk of bias. Because they provided no descriptions of blinding, all four of the other trials were assessed as having an unclear risk of bias.
Incomplete outcome data
All included trials were free of incomplete outcome data, except Jin 2011, Shi 2009, and Zhou 2005. Jin 2011 did not provide scores for each FD symptom during the follow‐up period. FD symptom scores at baseline were omitted in Shi 2009 and Zhou 2005.
Selective reporting
Scores for each FD symptom during the follow‐up period were not reported in Jin 2011. Shi 2009 and Zhou 2005 omitted FD symptom scores at baseline and offered just the scores after treatment for interventions. Therefore, selective omission outcomes reporting may have occurred, leading to bias in both studies.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5
1 Acupuncture versus medications
Four studies (358 participants) were included (Shi 2009; Tang 2006; Yang 2009; Zhou 2005). Because of the explicit clinical heterogeneity (inhomogeneous interventions and controls) among included studies, descriptive analysis was conducted. No significance was found for manual acupuncture, electroacupuncture, or manual‐electroacupuncture compared with medications. Additionally, we detected that manual acupuncture would bring about fewer adverse effects than were seen with cisapride. However, evidence of outcomes was of very low quality.
1.1 Manual acupuncture compared with cisapride
Descriptive analysis was performed on the following outcome measures in Shi 2009 (90 participants).
1.1.1 Symptom scores of FD
Effective rate was calculated as the (symptom scores after treatment ‐ symptom scores before treatment) / symptom scores before treatment*100%. When effective rate was greater than or equal to 25%, this meant "effective," greater than or equal to 50% meant "marked effective," and greater than or equal to 75% meant "healing" effect. "Effective," "marked effective," and "healing" were categorized as "positive effect," and "invalid" as "negative effect". Then, the outcome data were transformed as dichotomous data. No significance was detected for manual acupuncture compared with cisapride in improving FD symptom scores (RR 1.02, 95% CI 0.91 to 1.16, very low‐quality evidence).
1.1.2 Frequency of FD symptoms
Frequency of FD symptoms meant the number of attacks per week. On the basis of extracted data, we separated FD symptoms into two groups: positive effect (no attacks per week) and negative effect (RR 1.04, 95% CI 0.75 to 1.44, very low quality evidence). No significance was detected for manual acupuncture compared with cisapride in reducing the frequency of FD attacks.
1.1.3 Adverse effects
The significant finding for adverse effects showed that manual acupuncture may have fewer adverse effects than are seen with cisapride in the treatment of patients with FD (RR 0.21, 95% CI 0.07 to 0.69, very low‐quality evidence).
1.2 Manual acupuncture compared with domperidone
Descriptive analysis was performed for the following outcome measures in Tang 2006 (62 participants).
1.2.1 Symptom scores of FD
FD symptom scores were transformed to dichotomous data, as was described in the aforementioned Section 1.1.1. No significance in FD symptom scores was investigated between manual acupuncture and domperidone (RR 1.24, 95% CI 0.97 to 1.58, low‐quality evidence).
1.2.2 Adverse effects
No adverse effects data were reported in this study, which examined manual acupuncture versus domperidone.
1.3 Manual‐electroacupuncture compared with domperidone
Zhou 2005 (126 participants) compared manual acupuncture combined with electroacupuncture with domperidone medication.
1.3.1 Symptom scores of FD
FD symptom scores were analyzed as described in the aforementioned method in Section 1.1.1 (RR 1.14, 95% CI 1.00 to 1.30, very low‐quality evidence). No significance was detected in FD symptom scores between the manual‐electroacupuncture group and the group treated with domperidone.
1.3.2 Symptom scores of FD subtypes
Symptom scores of FD subtypes were as follows: ulceration subtype: RR 0.81, 95% CI 0.26 to 2.51, very low‐quality evidence; regurgitation subtype: RR 0.89, 95% CI 0.42 to 1.86, very low‐quality evidence; dyskinesia subtype: RR 1.20, 95% CI 0.76 to 1.89, very low‐quality evidence; and nonspecific subtype: RR 1.45, 95% CI 0.77 to 2.76, very low‐quality evidence. No significance was detected in symptom scores of FD subtypes between the manual‐electroacupuncture group and the group given domperidone.
1.3.3 Adverse effects
No adverse effects data were reported in the study examining manual‐electroacupuncture versus domperidone.
1.4 Electroacupuncture compared with itopride
Descriptive analysis was performed for the following outcome measures in Yang 2009 (80 participants).
1.4.1 Symptom scores of FD
FD symptom scores were transformed as dichotomous data as described in the aforementioned method in Section 1.1.1. No significance was investigated in improving FD symptom scores of electroacupuncture compared with itopride (RR 1.11, 95% CI 0.98, 1.27, low‐quality evidence).
1.4.2 Adverse effects
No adverse effects data were reported in the study examining electroacupuncture versus itopride.
2. Acupuncture versus sham acupuncture
Three studies (184 participants) were included (Chang 2010; Jin 2011; Park 2009).
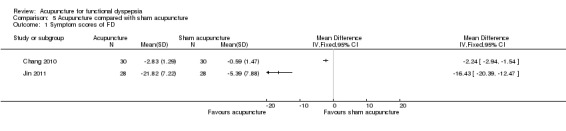
2.1 Symptom scores of FD
Chang 2010 (60 participants) and Jin 2011 (56 participants) reported continuous data, and we applied MDs and 95% CIs to describe them as follows: Chang 2010: MD ‐2.24, 95% CI ‐2.94 to ‐1.54, low‐quality evidence; and Jin 2011: MD ‐16.43, 95% CI ‐20.39 to ‐12.47, low‐quality evidence. Substantial heterogeneity was detected: I² = 98%. Because of the data on FD symptom scores provided, different symptom severity may be the most likely cause of heterogeneity. Therefore, descriptive analysis was performed. Both studies showed that acupuncture can decrease symptom scores of FD more than sham acupuncture can; however, the outcomes were based on low‐quality evidence.
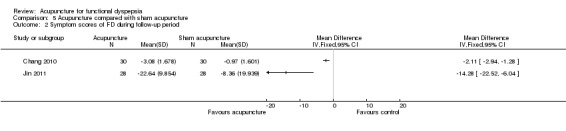
2.2 Symptom scores of FD during the follow‐up period
Heterogeneity was detected (I² = 88%) and may be a result of the length of follow‐up. Descriptive analysis was separately conducted in Chang 2010 (MD ‐2.11, 95% CI ‐2.94 to ‐1.28, low‐quality evidence) and Jin 2011 (MD ‐14.28, 95% CI ‐22.52 to ‐6.04, low‐quality evidence). Both studies suggested that acupuncture would lessen symptom scores of FD during the follow‐up period more significantly, but the evidence was of low quality.
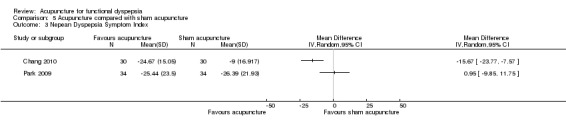
2.3 NDI
2.3.1 NDSI
Substantial heterogeneity of NDSI was investigated by a fixed‐efffect or a random‐effects model: I² = 83% in Chang 2010 and Park 2009 (68 participants); descriptive analysis was conducted. The heterogeneous factors might be due to different symptom severity. Chang 2010 supported that acupuncture could lessen NDSI scores more significantly than sham acupuncture (MD ‐15.67, 95% CI ‐23.77 to ‐7.57, low‐quality evidence). No significance was detected in Park 2009 for acupuncture compared with sham acupuncture in decreasing NDSI (MD 0.95, 95% CI ‐9.85 to 11.7, low‐quality evidence).
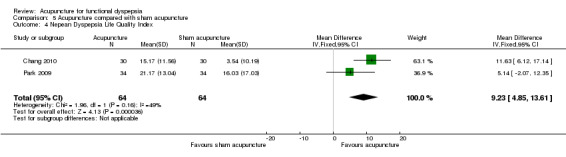
2.3.2 NDLQI
Potential inconsistency of NDLQI was detected under a fixed‐effect or a random‐effects model: I² = 49%. Therefore, we conducted a descriptive analysis. Different symptom severity might be the cause of the heterogeneity. Chang 2010 stood on the side that acupuncture can improve life quality of patients with FD more than sham acupuncture can (MD 11.63, 95% CI 6.12 to 17.14, low‐quality evidence). No significance was found in Park 2009 for acupuncture compared with sham acupuncture in improving quality of life (MD 5.14, 95% CI ‐2.07 to 12.35, low‐quality evidence).
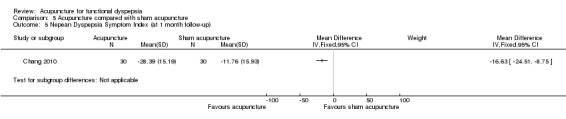
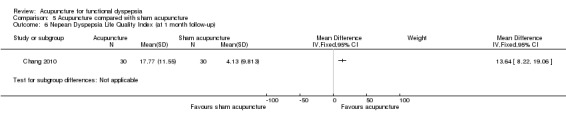
2.3.3 NDI at follow‐up of one month
Chang 2010 provided NDSI during the follow‐up period (MD ‐16.63, 95% CI ‐24.51 to ‐8.75, low‐quality evidence) and NDLQI during the follow‐up period (MD 13.64, 95% CI 8.22 to 19.06, low‐quality evidence). This implied that acupuncture would improve NDI scores at follow‐up of one month more than sham acupuncture would; however, the evidence was of low quality.
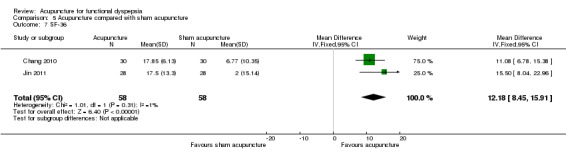
2.4 SF‐36
The I² statistical value of 1% under a fixed‐effect model suggested homogeneity in SF‐36 between Chang 2010 and Jin 2011. Total effect meant that acupuncture can improve life quality of patients with FD more than sham acupuncture can (MD 12.18, 95% CI 8.45 to 15.91, low‐quality evidence).
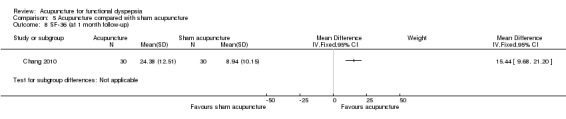
2.5 SF‐36 at follow‐up of one month
Results of Chang 2010 (MD 15.44, 95% CI 9.68 to 21.20, low‐quality evidence) imply that acupuncture could improve life quality more significantly than sham acupuncture at follow‐up of one month.
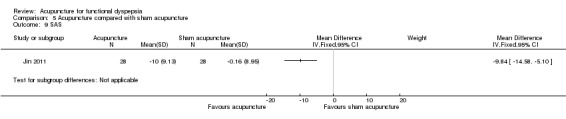
2.6 SAS
Jin 2011 supported that acupuncture could ameliorate the anxiety of patients with FD more than sham acupuncture could (MD ‐9.84, 95% CI ‐14.58 to ‐5.10, low‐quality evidence).
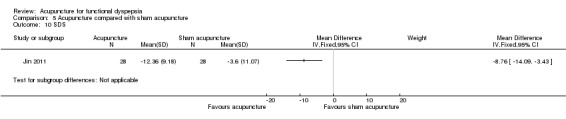
2.7 SDS
Jin 2011 supported the result that acupuncture could also ameliorate depression among patients with FD more than sham acupuncture could (MD ‐8.76, 95% CI ‐14.09 to ‐3.43, low‐quality evidence).
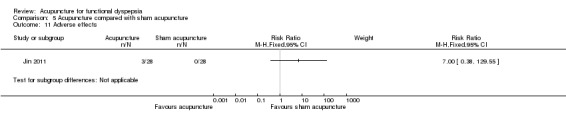
2.8 Adverse effects
In Jin 2011, no significance was found for acupuncture compared with sham acupuncture in reducing adverse effects (RR 7.00, 95% CI 0.38 to 129.55, very low‐quality evidence). Because of the large effect size with very wide confidence intervals, results indicated serious imprecision; attention should be paid to this interpretation.
Discussion
Summary of main results
Seven RCTs were eventually included. The interventions and controls can be roughly divided into two groups: manual acupuncture, electroacupuncture, or manual‐electroacupuncture versus medications (cisapride, domperidone, or itopride); and acupuncture versus sham acupuncture. No comparison between acupuncture and waiting list was included.
Descriptive analysis was applied in all trials of acupuncture versus medications because of the small number of trials and their clinical heterogeneity. No significance was found for acupuncture versus medications in reducing FD symptom scores and frequency of FD attack. In trials of acupuncture versus sham acupuncture, all descriptive or quantitative analysis results implied that acupuncture can improve FD symptom scores, NDI scores, and SF‐36, SAS, and SDS more significantly than sham acupuncture, except that no significance was found in Park 2009 for NDI scores. Results for the follow‐up period of Jin 2011 and Chang 2010 show that acupuncture might improve symptom scores of FD more than sham acupuncture. Additionally, the descriptive analysis of safety in treating FD showed no significance for acupuncture compared with sham acupuncture in reducing adverse effects (Jin 2011), but indicated that it may bring about fewer side effects than the drug cisapride (Shi 2009). It is worth noting that evidence on the above outcomes was of low or even very low quality.
Overall completeness and applicability of evidence
This review involved RCTs on two major acupuncture methods (manual acupuncture and electroacupuncture) for patients meeting Rome II or Rome III diagnostic criteria for FD. Outcome measures included efficacy and safety assessment, involving the most frequently used tools at present, such as FD symptom scores, NDI, SF‐36, SAS, SDS, and so forth. Therefore, results of this review reflect the current situation for acupuncture in FD.
Quality of the evidence
All evidence was assessed to be of low or even very low quality when the GRADE system was used, and the most serious reasons for downgrading included study limitations (blinding) and imprecision (small sample size). The quality of the evidence meant that further research would be very likely to change the estimate of effect, or that we were very uncertain about the estimate. Thus, the body of evidence identified cannot yet allow a robust conclusion regarding the efficacy and safety of acupuncture for FD.
Potential biases in the review process
Some potential biases might be noted during interpretation of the estimate of effect. First, acupuncture manipulation is quite different from the quantitative use of medication. It varies among different therapists or acupuncture techniques, even when the same guidelines are followed. As a result, the heterogeneity of acupuncture manipulations reported in different trials might have an impact on the effect estimate. Second, all seven included trials focused on the Asian style of acupuncture (six Chinese acupuncture trials and one Korean acupuncture trial); Western acupuncture was absent. Regarding differences in acupoint selection, manipulations, and treatment duration and frequency, further review combined with information on different types of acupuncture would be necessary for an update. Third, potentially high risk of bias might be present in the included trials in the following patterns. Neither trial reported details on randomization concealment and calculation of proper sample size. Also, dropout observation was lacking in each study, so it might be impossible to ensure that all participants did not withdraw during the experiment. Follow‐up observation was not brought to the forefront during performance of the experiment.
Agreements and disagreements with other studies or reviews
Two systematic reviews on acupuncture for the treatment of FD were retrieved. In Schneider 2007, clinical trials of acupuncture for functional gastrointestinal disease were included, and only one controlled study (Chen 1998) was available. No significance was detected in Chen 1998 for acupuncture compared with cisapride medication in improving FD symptoms. Another review (Zhu 2008) was different from our review in that RCTs and quasi‐RCTs on acupuncture for FD were included; participants were diagnosed by different international criteria; interventions consisted of acupuncture techniques without limitations; and controls included blank control, modern medications, herbs, and sham acupuncture. Results in Zhu 2008 imply that acupuncture may be superior to medication in improving total scores for FD symptoms. On consideration of the complexity of FD diagnostic criteria and heterogeneity of different acupuncture methods as described in the above reviews, we have set the present criteria in considering studies for inclusion in this review. However, low quality of evidence in three systematic reviews was the same and has resulted in lack of robust evidence on the use of acupuncture for FD. The main reasons for downgrading were risk of bias (unclear description of randomization and its concealment, difficulty of conducting blinding in acupuncture studies), absence of sample size calculations and follow‐up observations, and so forth. Therefore, upgrading the evidence level of acupuncture studies will require continued effort.
Authors' conclusions
Implications for practice.
Given the low or very low quality of evidence obtained, it cannot be concluded whether acupuncture is more effective or safer than other treatments in the treatment of FD.
Implications for research.
Acupuncture, especially the Chinese style of acupuncture, has special characteristics compared with other treatments. Therefore, some consensus must be reached globally to improve the quality of evidence for acupuncture studies. On one hand, for assessment of risk of bias, blinding of therapists is impossible, and even blinding of participants would require great care. Thus, whether current assessment methods for blinding are suitable for acupuncture studies remains controversial. On the other hand, language limitations have impeded comprehensive understanding of CONSORT (Altman 2001) and STRICTA recommendations (MacPherson 2010). Thus, efforts are needed to improve acupuncture publications, especially those on Chinese acupuncture, in accordance with these guidelines.
Acknowledgements
We would like to thank the members of the Upper Gastrointestinal and Pancreatic Disease Group for amendments to the review, and we are grateful to Tang Yong, who completed the primary search for the protocol and amended the review draft.
Appendices
Appendix 1. CENTRAL search strategy
((disturbance$ or disorder$ or difficult$ or dysfunction$ or disease$ or impair$ or condition$ or abnormal$ or illness$ or patholog$ or discomfort$ or hazard$ or damage$ or injur$ or irritab$ or pain$ or distress$ or burning) adj2 postprandial).mp.
indigestion.mp.
(Intestin$ or Digest$ or Gastr$ or gut or epigastr$ or stomach$).mp.
3 and 2
dyspepsia.mp. or exp Dyspepsia/
(epigastric adj2 pain).ti,ab.
(epigastric adj2 burn$).mp.
(Rome adj2 criteria).mp.
or/1,4‐8
exp Acupuncture Therapy/ or exp Acupuncture/ or exp Acupuncture Points/
exp acupressure/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/
acupuncture.mp.
electroacupuncture.mp.
acupoint$.mp.
meridian$.mp.
deqi.mp. [mp=title, original title, abstract, mesh headings, heading words, keyword]
moxibustion$.mp.
or/10‐17
9 and 18
limit 19 to yr="2009 ‐ 2012"
Appendix 2. MEDLINE search strategy
((disturbance$ or disorder$ or difficult$ or dysfunction$ or disease$ or impair$ or condition$ or abnormal$ or illness$ or patholog$ or discomfort$ or hazard$ or damage$ or injur$ or irritab$ or pain$ or distress$ or burning) adj2 postprandial).mp.
indigestion.mp.
(Intestin$ or Digest$ or Gastr$ or gut or epigastr$ or stomach$).mp.
3 and 2
dyspepsia.mp. or exp Dyspepsia/
(epigastric adj2 pain).ti,ab.
(epigastric adj2 burn$).mp.
(Rome adj2 criteria).mp.
or/1,4‐8
exp Acupuncture Therapy/ or exp Acupuncture/ or exp Acupuncture Points/
exp acupressure/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/
acupuncture.mp.
electroacupuncture.mp.
acupoint$.mp.
meridian$.mp.
deqi.mp. [mp=title, abstract, original title, name of substance word, subject heading word, protocol supplementary concept, rare disease supplementary concept, unique identifier]
moxibustion$.mp.
or/10‐17
9 and 18
limit 19 to ed=20090801‐20120107
Appendix 3. EMBASE search strategy
((disturbance$ or disorder$ or difficult$ or dysfunction$ or disease$ or impair$ or condition$ or abnormal$ or illness$ or patholog$ or discomfort$ or hazard$ or damage$ or injur$ or irritab$ or pain$ or distress$ or burning) adj2 postprandial).mp.
indigestion.mp.
(Intestin$ or Digest$ or Gastr$ or gut or epigastr$ or stomach$).mp.
3 and 2
dyspepsia.mp. or exp Dyspepsia/
(epigastric adj2 pain).ti,ab.
(epigastric adj2 burn$).mp.
(Rome adj2 criteria).mp.
or/1,4‐8
exp Acupuncture Therapy/ or exp Acupuncture/ or exp Acupuncture Points/
exp acupressure/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/
acupuncture.mp.
electroacupuncture.mp.
acupoint$.mp.
meridian$.mp.
deqi.mp. [mp=title, abstract, subject headings, heading word, drug trade name, original title, device manufacturer, drug manufacturer, device trade name, keyword]
moxibustion$.mp.
or/10‐17
9 and 18
limit 19 to em=200933‐201202
Appendix 4. AMED search strategy
((disturbance$ or disorder$ or difficult$ or dysfunction$ or disease$ or impair$ or condition$ or abnormal$ or illness$ or patholog$ or discomfort$ or hazard$ or damage$ or injur$ or irritab$ or pain$ or distress$ or burning) adj2 postprandial).mp.
indigestion.mp.
(Intestin$ or Digest$ or Gastr$ or gut or epigastr$ or stomach$).mp.
3 and 2
dyspepsia.mp. or exp Dyspepsia/
(epigastric adj2 pain).ti,ab.
(epigastric adj2 burn$).mp.
(Rome adj2 criteria).mp.
or/1,4‐8
exp Acupuncture Therapy/ or exp Acupuncture/ or exp Acupuncture Points/
exp acupressure/ or exp electroacupuncture/ or exp meridians/ or exp moxibustion/
acupuncture.mp.
electroacupuncture.mp.
acupoint$.mp.
meridian$.mp.
deqi.mp. [mp=title, original title, abstract, mesh headings, heading words, keyword]
moxibustion$.mp.
or/10‐17
9 and 18
limit 19 to yr="2009 ‐ 2012"
Appendix 5. CNKI search strategy
( (关键词 =针灸) or (关键词 =针刺) or (关键词 =电针)) and ( (关键词=消化不良) or (关键词 =功能性消化不良) or (关键词 =烧灼) or (关键词 =食欲不振) or (关键词 =上腹不适) or (关键词 =上腹痛) or (关键词 =腹胀) or (关键词 =早饱) or (关键词 =嗳气) )
Appendix 6. VIP Database search strategy
(K=针灸+K=针刺+K=电针)*(K=消化不良+K =功能性消化不良+K =烧灼+K =食欲不振+K =上腹不适+K =上腹痛+K =腹胀+K =早饱+K =嗳气)
Appendix 7. CBMdisc search strategy
#1 缺省 =消化不良
#2 缺省 =功能性消化不良
#3 缺省 =烧灼
#4 缺省 =食欲不振
#5 缺省 =上腹不适
#6 缺省 =上腹痛
#7 缺省 =腹胀
#8 缺省 =早饱
#9 缺省 =嗳气
#10 #1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9
#11 缺省=针灸
#12 缺省=针刺
#13 缺省=电针
#14 #11 or #12 or #13
#15 #10 and #14
Appendix 8. Wanfang search strategy
针刺and功能性消化不良
Data and analyses
Comparison 1. Manual acupuncture compared with cisapride.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptom scores of FD | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2 Frequency of FD symptoms | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Adverse effects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
1.1. Analysis.
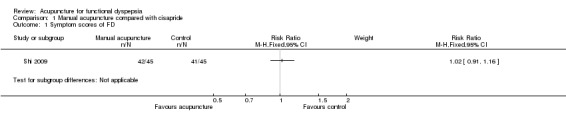
Comparison 1 Manual acupuncture compared with cisapride, Outcome 1 Symptom scores of FD.
1.2. Analysis.
Comparison 1 Manual acupuncture compared with cisapride, Outcome 2 Frequency of FD symptoms.
1.3. Analysis.
Comparison 1 Manual acupuncture compared with cisapride, Outcome 3 Adverse effects.
Comparison 2. Manual acupuncture compared with domperidone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptom scores of FD | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
2.1. Analysis.
Comparison 2 Manual acupuncture compared with domperidone, Outcome 1 Symptom scores of FD.
Comparison 3. Manual‐electroacupuncture compared with domperidone.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptom scores of FD | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 2 Symptom scores of FD in ulceration subtype | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 3 Symptom scores of FD in regurgitation subtype | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 4 Symptom scores of FD in dyskinesia subtype | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only | |
| 5 Symptom scores of FD in nonspecific subtype | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
3.1. Analysis.
Comparison 3 Manual‐electroacupuncture compared with domperidone, Outcome 1 Symptom scores of FD.
3.2. Analysis.
Comparison 3 Manual‐electroacupuncture compared with domperidone, Outcome 2 Symptom scores of FD in ulceration subtype.
3.3. Analysis.
Comparison 3 Manual‐electroacupuncture compared with domperidone, Outcome 3 Symptom scores of FD in regurgitation subtype.
3.4. Analysis.
Comparison 3 Manual‐electroacupuncture compared with domperidone, Outcome 4 Symptom scores of FD in dyskinesia subtype.
3.5. Analysis.
Comparison 3 Manual‐electroacupuncture compared with domperidone, Outcome 5 Symptom scores of FD in nonspecific subtype.
Comparison 4. Electroacupuncture compared with itopride.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptom scores of FD | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
4.1. Analysis.
Comparison 4 Electroacupuncture compared with itopride, Outcome 1 Symptom scores of FD.
Comparison 5. Acupuncture compared with sham acupuncture.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Symptom scores of FD | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 2 Symptom scores of FD during follow‐up period | 2 | Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 3 Nepean Dyspepsia Symptom Index | 2 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4 Nepean Dyspepsia Life Quality Index | 2 | 128 | Mean Difference (IV, Fixed, 95% CI) | 9.23 [4.85, 13.61] |
| 5 Nepean Dyspepsia Symptom Index (at 1 month follow‐up) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 6 Nepean Dyspepsia Life Quality Index (at 1 month follow‐up) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 7 SF‐36 | 2 | 116 | Mean Difference (IV, Fixed, 95% CI) | 12.18 [8.45, 15.91] |
| 8 SF‐36 (at 1 month follow‐up) | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 9 SAS | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 10 SDS | 1 | Mean Difference (IV, Fixed, 95% CI) | Subtotals only | |
| 11 Adverse effects | 1 | Risk Ratio (M‐H, Fixed, 95% CI) | Subtotals only |
5.1. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 1 Symptom scores of FD.
5.2. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 2 Symptom scores of FD during follow‐up period.
5.3. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 3 Nepean Dyspepsia Symptom Index.
5.4. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 4 Nepean Dyspepsia Life Quality Index.
5.5. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 5 Nepean Dyspepsia Symptom Index (at 1 month follow‐up).
5.6. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 6 Nepean Dyspepsia Life Quality Index (at 1 month follow‐up).
5.7. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 7 SF‐36.
5.8. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 8 SF‐36 (at 1 month follow‐up).
5.9. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 9 SAS.
5.10. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 10 SDS.
5.11. Analysis.
Comparison 5 Acupuncture compared with sham acupuncture, Outcome 11 Adverse effects.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Chang 2010.
| Methods | Eligibility criteria: Rome III diagnostic criteria for functional dyspepsia Study duration: 4 weeks Sequence generation: randomization allocation mentioned without details Randomization concealment: not described Blind participants: not described Blind assessors: not described Blind therapists: not described Baseline comparability: Mean and standard deviation (SD) in age, disease course, and FD symptom scores were shown; no significance was found Follow‐up: NDI, SF‐36, and FD symptom scores assessed 1 month after interventions |
|
| Participants | Setting: outpatients from the First Affiliated Hospital of Hunan University of TCM, Changsha City, Hunan Province, China Total number: 60 Male/Female (n/n): 19/41 Mean age (± SD) or age range, years: between 21 and 51 Duration of functional dyspepsia before recruitment: 1.7 to 6.5 years Important inclusion criteria (clearly describe): without organic disease Important exclusion criteria (clearly describe): with pregnancy, lactation, or gestation‐in‐plan |
|
| Interventions |
ACUPUNCTURE GROUP Number allocated to acupuncture: 30 Style of acupuncture: manual acupuncture Needles: sterile needles, gauge 32, length of 25 mm and 40 mm, single‐use, made by Suzhou Medical Appliance Co., Ltd (Jiangsu, China) Numbers and names of points stimulated: a formula of 4 acupoints stimulated involving ST32, ST36, ST40, and ST42 Insertion depth: 0.3 to 0.5 cm Manipulation after insertion: lifting and thrusting while rotating "De‐qi" required or not: yes Duration of treatment (minutes): 30 Frequency of treatment per week: 5 times Total length of treatment period (weeks): 4 Description of therapists' qualifications: no, but participants were treated by TCM doctors CONTROL GROUP Number allocated to control: 30 Style of control: sham acupuncture (puncturing sham acupoints) Needles: sterile needles, gauge 32, length of 25 mm and 40 mm, single‐use, made by Suzhou Medical Appliance Co., Ltd (Jiangsu, China) Numbers and names of points stimulated: a formula of 4 sham acupoints stimulated involving points lateral to ST32, ST36, ST40, and ST42 between Stomach Meridian and Gallbaldder Meridian Insertion depth: 0.3 to 0.5 cm Manipulation after insertion: lifting and thrusting while rotating "De‐qi" required or not: yes Duration of treatment (minutes): 30 Frequency of treatment per week: 5 times Total length of treatment period (weeks): 4 Description of therapists' qualifications: no, but participants were treated by TCM doctors CO‐INTERVENTIONS IN GROUPS: no |
|
| Outcomes |
1. NDI Conclusion from original data: Significance in both groups was reported in scores after treatment versus before treatment, at follow‐up versus before treatment. Significance was found in acupuncture group compared with sham acupuncture group 1.1 Nepean Dyspepsia Symptom Index (NDSI) ACUPUNCTURE GROUP: pretreatment 42.53 ± 16.642; post‐treatment 17.86 ± 12.660;follow‐up 14.14 ± 13.120 CONTROL GROUP: pretreatment 39.45 ± 16.917; post‐treatment 30.45 ± 16.917; follow‐up 27.69 ± 14.707 1.2 Nepean Dyspepsia Life Quality Index (NDLQI) ACUPUNCTURE GROUP: pretreatment 76.43 ± 13.337; post‐treatment 91.60 ± 6.237; follow‐up 94.20 ± 6.706 CONTROL GROUP: pretreatment 77.97 ± 9.813; post‐treatment 81.51 ± 10.522; follow‐up 82.10 ± 9.813 2. Symptom scores of FD How to assess: 0 points: no symptoms; 1 point: slight symptoms; 2 points: moderate symptoms but not sufficient to affect daily life; 3 points: symptoms severe enough to affect daily life Conclusion from original data: Significance in both groups was reported in scores after treatment versus before treatment, at follow‐up versus before treatment. Significance was found in acupuncture group compared with sham acupuncture group ACUPUNCTURE GROUP: pretreatment 4.33 ± 1.446; post‐treatment 1.50 ± 1.036; follow‐up 1.25 ± 1.236 CONTROL GROUP: pretreatment 3.97 ± 1.377; post‐treatment 3.38 ± 1.568;follow‐up 3.00 ± 1.336 3. SF‐36 scale Conclusion from original data: Significance in both groups was reported in scores after treatment versus before treatment, at follow‐up versus before treatment. Significance was found in acupuncture group compared with sham acupuncture group ACUPUNCTURE GROUP: pretreatment 64.19 ± 14.349; post‐treatment 82.04 ± 9.084;follow‐up 88.57 ± 5.691 CONTROL GROUP: pretreatment 68.76 ± 11.264; post‐treatment 75.53 ± 9.082; follow‐up 77.70 ± 8.432 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Sixty patients were divided randomly into two groups" Comment: Central randomization was confirmed upon telephone visit |
| Allocation concealment (selection bias) | Low risk | Quote: no description Comment: It has been confirmed that allocation concealment was performed by another professional team named Chengdu GCP Centre, using specific software, after visiting the main study staff by phone |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: not found Comment: probably no |
| Selective reporting (reporting bias) | Low risk | Quote: not found Comment: probably yes |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Quote: no description Comment: It could not be validated |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: not mentioned Comment: It was replied in a phone visit that outcome assessment was done by people unknown to allocation |
Jin 2011.
| Methods | Eligibility criteria: Rome III diagnostic criteria for functional dyspepsia Study duration: 4 weeks Sequence generation: randomization number table Randomization concealment: sealed, opaque, and numbered envelopes Blind participants: yes, but not with details Blind assessors: yes, other participants unknown to allocation performed the assessment Blind therapists: no Baseline comparability: Mean and standard deviation (SD) in age, gender, disease course, and FD symptom score were shown; no significance was found Follow‐up: FD symptom score assessed 3 months after interventions |
|
| Participants | Setting: outpatients from the Guan'anmen Hospital of China Academy of Chinese Medical Sciences, Beijing City, China Total number: 56 Male/Female (n/n): 21/35 Mean age (± SD) or age range, years: between 18 and 70 Duration of functional dyspepsia before recruitment: 1.0 to 40.0 years Important inclusion criteria (clearly describe): without organic disease Important exclusion criteria (clearly describe): with pregnancy, lactation, or gestation‐in‐plan |
|
| Interventions |
ACUPUNCTURE GROUP Number allocated to acupuncture: 28 Style of acupuncture: manual acupuncture Needles: sterile needles, gauge 32, length of 25 mm, single‐use, made by Suzhou Medical Appliance Co., Ltd (Jiangsu, China) Numbers and names of points stimulated: a formula of 2 main acupoints stimulated involving ST36 and KI 3 Insertion depth: 1 cun Manipulation after insertion: lifting and thrusting while rotating "De‐qi" required or not: yes Frequency of treatment per week: 3 to 4 times Total length of treatment period (weeks): 4 Description of therapists' qualifications: yes, therapist was the one with 6 years of acupuncture practice CONTROL GROUP Number allocated to control: 28 Style of control: sham acupuncture (puncturing sham acupoints superficially) Needles: sterile needles, gauge 32, length of 25 mm, single‐use, made by Suzhou Medical Appliance Co., Ltd (Jiangsu, China) Numbers and names of points stimulated: a formula of 2 main sham acupoints stimulated involving points lateral to ST36 and KI 3, which were in charge of the same spinal level as ST36 and KI 3 Insertion depth: 2 to 3 mm Manipulation after insertion: lifting and thrusting while rotating "De‐qi" required or not: yes Frequency of treatment per week: 3 to 4 times Total length of treatment period (weeks): 4 Description of therapists' qualifications: yes, therapist was the same one with 6‐year acupuncture practice CO‐INTERVENTIONS IN GROUPS: no |
|
| Outcomes |
1. Symptom scores of FD How to assess: 0 points: no symptoms; 1 point: slight symptoms; 2 points: moderate symptoms but not sufficient to affect daily life; 3 points: symptoms severe enough to affect daily life Conclusion from original data: total scores in each group after treatment versus before treatment decreased significantly, but only total scores in the acupuncture group before treatment versus follow‐up decreased significantly. Significance of total scores in acupuncture group compared with sham acupuncture group was found ACUPUNCTURE GROUP: pretreatment 24.32 ± 8.28, post‐treatment 2.50 ± 3.28, follow‐up 1.68 ± 2.36 CONTROL GROUP: pretreatment 24.79 ± 7.48, post‐treatment 19.4 ± 8.23, follow‐up 16.43 ± 7.41 (pretreatment vs follow‐up: P value > 0.05) Scores for each FD symptom ACUPUNCTURE GROUP Postprandial discomfort: pretreatment 9.00 ± 2.09, post‐treatment 1.57 ± 2.28 Early satiety: pretreatment 9.74 ± 1.91, post‐treatment 0.42 ± 1.43 Epigastric pain: pretreatment 6.81 ± 2.23, post‐treatment 0.48 ± 1.03 Epigastric burning sensation: pretreatment 6.31 ± 2.39, post‐treatment 0.50 ± 1.50 CONTROL GROUP Postprandial discomfort: pretreatment 8.89 ± 2.39, post‐treatment 6.22 ± 2.59 Early satiety: pretreatment 8.43 ± 2.87, post‐treatment 6.05 ± 2.52 Epigastric pain: pretreatment 7.41 ± 3.02, post‐treatment 6.32 ± 3.41 (pretreatment vs post‐treatment: P value > 0.05) Epigastric burning sensation: pretreatment 6.71 ± 2.78, post‐treatment 6.47 ± 3.00 (pretreatment vs post‐treatment: P value > 0.05) 2. SF‐36 scale Conclusion from original data: Scores in acupuncture group after treatment versus before treatment were increased significantly, as were scores of acupuncture group compared with sham acupuncture group ACUPUNCTURE GROUP: pretreatment 52.50 ± 13.94, post‐treatment 70.00 ± 12.549 CONTROL GROUP: pretreatment 54.00 ± 16.41, post‐treatment 56 ± 13.42 (pretreatment vs post‐treatment: P value > 0.05) 3. SDS Conclusion from original data: Scores in acupuncture group after treatment versus before treatment were decreased significantly, as were scores of acupuncture group compared with sham acupuncture group ACUPUNCTURE GROUP: pretreatment 57.96 ± 9.55, post‐treatment 45.60 ± 8.75 CONTROL GROUP: pretreatment 57.60 ± 11.84, post‐treatment 54 ± 10.08 (pretreatment vs post‐treatment: P value > 0.01) 4. SAS Conclusion from original data: Scores in acupuncture group after treatment versus before treatment were decreased significantly, as were scores of acupuncture group compared with sham acupuncture group ACUPUNCTURE GROUP: pretreatment 52.30 ± 10.48, post‐treatment 42.3 ± 6.22 CONTROL GROUP: pretreatment 52.36 ± 9.67, post‐treatment 52.2 ± 7.98 (pretreatment vs post‐treatment: P value > 0.05) 5. Adverse effects ACUPUNCTURE GROUP: 3 cases of numb feeling for 3 to 7 days CONTROL GROUP: 0 cases |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "patients were divided randomly into two groups in the way of randomization number table" Comment: probably done for allocation concealment description |
| Allocation concealment (selection bias) | Low risk | Quote: "allocation concealment was done by sealed, opaque and sequentially numbered envelopes" Comment: probably done |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: Scores of all FD symptoms during the follow‐up period are not shown Comment: probably yes |
| Selective reporting (reporting bias) | High risk | Quote: Scores of all FD symptoms during the follow‐up period were not reported Comment: probably no |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "therapist was the same one conducting the acupuncture in treatment and control groups, patients were blinded to the formula, and statisticians were not involved into the study" Comment: The therapist was not blinded; acupoints and sham acupoints are adjacent to each other, so probably blinding or participants was performed; this was probably done to blind statisticians |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "other participants but therapist who were unknown the allocation did the assessment" Comment: probably done |
Park 2009.
| Methods | Eligibility criteria: Rome II diagnostic criteria for functional dyspepsia Study duration: 2 weeks Sequence generation: block randomization mentioned without details Randomization concealment: not described Blind participants: participants except the doctor conducting acupuncture blinded, including investigators, participants, and study monitors Blind assessors: yes, but without details Blind therapists: not blinded Baseline comparability: No significance in mean age, gender, weight, height, severity of dyspepsia symptoms, scores for quality of life, and treatment surmise was found |
|
| Participants | Setting: patients from the Korean Oriental Medicine Clinics, South Korea Total number: 68 Male/Female (n/n): 14/54 Mean age (± SD) or age range, years: between 20 and 60 Duration of functional dyspepsia before recruitment: not described Important inclusion criteria (clearly describe): without organic disease Important exclusion criteria (clearly describe): with organic disease |
|
| Interventions |
ACUPUNCTURE GROUP Number allocated to acupuncture: 34 Style of acupuncture: manual acupuncture Needles: sterile needles (diameter 0.25 mm, length 30 mm; made by Dongbang Acupuncture Inc., Seoul, South Korea) Numbers and names of points stimulated: a formula of 6 acupoints stimulated involving LI4, LR3, PC6, SP4, ST36, and CV12 Insertion depth: 1.0 at LI4, LR3, PC6, and SP4; 2.5 cm at ST36 and CV12 Manipulation after insertion: rotate 90 degrees clockwise 3 times "De‐qi" required or not: not described Duration of treatment (minutes): 15 Frequency of treatment per week: 3 times Total length of treatment period (weeks): 2 Description of therapists' qualification: yes, the therapist was a licensed doctor CONTROL GROUP Number allocated to control: 34 Style of control: sham acupuncture (puncturing sham acupoints) Needles: sterile needles (diameter 0.25 mm, length 30 mm; made by Dongbang Acupuncture Inc., Seoul, South Korea) Numbers and names of points stimulated: 6 sham acupoints stimulated involving points of 10 mm to 20 mm away from LI4, LR3, PC6, SP4, ST36, and CV12 Manipulation: performance done by the same doctor for the acupuncture group Duration of treatment (minutes): 15 Frequency of treatment per week: 3 times Total length of treatment period (weeks): 2 Description of therapists' qualifications: yes, the therapist was a licensed doctor CO‐INTERVENTIONS IN GROUPS: no |
|
| Outcomes |
1. NDI Conclusion from original data: Dyspepsia symptoms and life quality of participants with FD were significantly improved in both groups, but no significance was found between the 2 groups 1.1 Nepean Dyspepsia Symptom Index (NDSI) ACUPUNCTURE GROUP: pretreatment 59.59 ± 22.03; post‐treatment 34.15 ± 24.74 CONTROL GROUP: pretreatment 55.71 ± 22.94; post‐treatment 29.32 ± 20.76 1.2 Nepean Dyspepsia Life Quality Index (NDLQI) ACUPUNCTURE GROUP: pretreatment 67.10 ± 15.06; post‐treatment 88.27 ± 7.65 CONTROL GROUP: pretreatment 70.47 ± 19.66; post‐treatment 86.50 ± 9.78 |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "Subjects were allocated into either the classical acupoints (CA) group or the non defined points (NP) group by block randomization" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote: no description Comment: cannot be identified for the moment |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: not found Comment: probably no |
| Selective reporting (reporting bias) | Low risk | Quote: not found Comment: probably yes |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Quote: "A licensed doctor performed the acupuncture; other study participants, including investigators, patients, and study monitors, were blinded. The protocol forbade the doctor performing the acupuncture to give information of the treatment regimens to patients or other participants" Comment: probably done |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Quote: "A licensed doctor performed the acupuncture; other study participants, including investigators, patients, and study monitors, were blinded. The protocol forbade the doctor performing the acupuncture to give information of the treatment regimens to patients or other participants" Comment: probably done |
Shi 2009.
| Methods | Eligibility criteria: Rome III diagnostic criteria for functional dyspepsia Study duration: 3 weeks Sequence generation: random number table Randomization concealment: not described Blind participants: not described Blind assessors: not described Blind therapists: not described Baseline comparability: It was described that no significance in gender, age, disease course, and FD symptoms was found, but details of FD symptoms at baseline were not offered Follow‐up: no |
|
| Participants | Setting: outpatients of Yanqing TCM Hospital in Beijing, China Total number: 90 Male/Female (n/n): 45/45 Mean age (± SD) or age range, years: between 18 and 66 Duration of functional dyspepsia before recruitment: 3 to 5 years Important inclusion criteria (clearly describe): without hypertension and organic disease Important exclusion criteria (clearly describe): with ulcer or organic disorders under gastroscopy; pregnancy, lactation or gestation‐in‐plan |
|
| Interventions |
ACUPUNCTURE GROUP Number allocated to acupuncture: 45 Style of acupuncture: manual acupuncture Numbers and names of points stimulated: a formula of 3 acupoints stimulated involving ST36 (bilateral), CV12, and PC6 (bilateral), adding LR3, LR13, LR14, and SP6 on consideration of TCM syndrome differentiations Insertion depth: 1 to 1.5 cun Manipulation after insertion: lifting and thrusting while rotating "De‐qi" required or not: yes Duration of treatment (minutes): 30 Frequency of treatment per week: 5 times Total length of treatment period (weeks): 3 Description of therapists' qualifications: no, but participants were treated by TCM doctors CONTROL GROUP Number allocated to control: 45 Style of control: orally Names of medications (if drugs, describe drug names): cisapride Dose of medication per intake: 5 mg before meals Frequency of medication per day: 3 times Total length of treatment period (weeks): 3 Description of co‐medications: no CO‐INTERVENTIONS IN GROUPS: no |
|
| Outcomes |
1. Symptom scores of FD after treatment How to assess: 0 points: no symptoms (acupuncture 27 cases, control 26 cases); 1 point: slight symptoms (acupuncture 9 cases, control 10 cases); 2 points: moderate symptoms but not sufficient to affect daily life (acupuncture 5 cases, control 4 cases); 3 points: symptoms severe enough to affect daily life (acupuncture 4 cases, control 5 cases) Effective rate = (symptom scores after treatment‐symptom scores before treatment)*100%. When equal to or greater than 25%, this meant "effective," equal to or greater than 50% meant "marked effective," and equal to or greater than 75% meant "healing" effect. "Effective," "marked effective," and "healing" are categorized as "positive effect," and "invalid" as "negative effect" Positive effect (acupuncture 42 cases, control 41 cases); negative effect (acupuncture 3 cases, control 4 cases) Conclusion from original data: No significance was found between acupuncture and control groups 2. Frequency of symptoms How to assess: 0 points: no attack (acupuncture 28 cases, control 27 cases); 1 point: 1 to 3 attacks per week (acupuncture 10 cases, control 9 cases); 2 points: 4 to 6 attacks per week (acupuncture 5 cases, control 6 cases); 3 points: attacks every day (acupuncture 2 cases, control 3 cases) Conclusion from original data: No significance was found between acupuncture and control groups 3. Adverse effects Acupuncture: 2 cases of subcutaneous hematoma and 1 case of vesicle (adverse effect rate 6.7%) Control: 11 cases of slight dizziness and 3 cases of diarrhea or borborygmus (adverse effect rate 31.1%) |
|
| Notes | Details of FD symptoms at baseline were not described clearly in this trial, only the results after treatment was obtained. Also details of randomization and blinding were not described clearly Weak points: too simply descriptive about baseline and study design |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random number table" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote: not described Comment: cannot be confirmed |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: FD symptoms at baseline not described Comment: probably yes |
| Selective reporting (reporting bias) | High risk | Quote: FD symptoms at baseline not reported Comment: probably no |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: not described Comment: Heterogeneity between acupuncture and drugs could result in performance bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: not mentioned whether outcome assessment was done in blinding way Comment: cannot be confirmed |
Tang 2006.
| Methods | Eligibility criteria: Rome II diagnostic criteria for functional dyspepsia Study duration: 4 weeks Sequence generation: random number table Randomization concealment: not described Blind participants: not described Blind assessors: not described Blind therapists: not described Baseline comparability: yes, no significance in gender, age, FD course, and FD symptoms was found between groups Follow‐up: no |
|
| Participants | Setting: outpatients from People's Hospital of Guangxi Zhuang Autonomous Region, Guangxi Province, China Total number: 62 Male/Female (n/n): 29/33 Mean age (± SD) or age range, years: 38.2 ± 11.3 in acupuncture group and 36.7 ± 12.8 in control group Duration of functional dyspepsia before recruitment: 3 to 108 months Important inclusion criteria (clearly describe): symptoms lasting for at least 1 month before enrollment Important exclusion criteria (clearly describe): organic disease under gastroscopy |
|
| Interventions |
ACUPUNCTURE GROUP Number allocated to acupuncture: 32 Style of acupuncture: manual acupuncture Numbers and names of points stimulated: a formula of 9 acupoints bilaterally stimulated involving ST36, CV12, PC6, LR3, BL15, BL19, BL20, BL21, and ST44 Insertion depth: 1 cun Manipulation after insertion: lifting and thrusting while rotating "De‐qi" required or not: yes Duration of treatment (minutes): 30 Frequency of treatment per week: 7 times Total length of treatment period (weeks): 4 (actually 30 days) Description of therapists' qualifications: no, but participants were treated by TCM doctors in the outpatient department CONTROL GROUP Number allocated to control: 30 Style of control: orally Names of medications (if drugs, describe drug names): domperidone Dose of medication per intake: 10 mg before meals Frequency of medication per day: 3 times Total length of treatment period (weeks): 4 Description of co‐medications: yes, required that participants not take drugs for gastro discomfort CO‐INTERVENTIONS IN GROUPS: no |
|
| Outcomes |
Symptom scores of FD How to assess: 0 points: no symptoms; 1 point: slight symptoms; 2 points: moderate symptoms but not sufficient to affect daily life; 3 points: symptoms severe enough to affect daily life Conclusion from original data: Significance was found in each group pretreatment and post‐treatment and between 2 groups Healing: no symptoms and no recurrence 1 month after treatment (acupuncture 12 cases, control 4 cases); marked effective: symptom scores after treatment decreased by more than two‐thirds (acupuncture 10 cases, control 6 cases); effective: symptom scores after treatment decreased by more than one‐third (acupuncture 7 cases, control 12 cases); invalid: symptom scores after treatment decreased by less than one‐third (acupuncture 3 cases, control 8 cases) ACUPUNCUTURE GROUP: pretreatment 12.5 ± 3.8, post‐treatment 7.3 ± 3.2 (pretreatment vs post‐treatment: P value < 0.01) CONTROL GROUP: pretreatment 11.7 ± 3.4, post‐treatment 7.8 ± 2.2 (pretreatment vs post‐treatment: P value < 0.01) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random number table" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote: not described Comment: cannot be confirmed at present |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: not found Comment: probably no |
| Selective reporting (reporting bias) | Low risk | Quote: not found Comment: probably yes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: not described Comment: Heterogeneity between acupuncture and drugs could result in performance bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: not mentioned whether outcome assessment was done in blinding way Comment: cannot be confirmed |
Yang 2009.
| Methods | Eligibility criteria: Rome III diagnostic criteria for functional dyspepsia Study duration: 4 weeks Sequence generation: random number table Randomization concealment: not described Blind participants: not described Blind assessors: not described Blind therapists: not described Baseline comparability: yes, no significance in gender, age, FD course, and FD symptoms between groups was found Follow‐up: no |
|
| Participants | Setting: outpatients from Wuhan Hospital of Traditional Medicine and Western Medicine, Hubei Province, China Total number: 80 Male/Female (n/n): 39/41 Mean age (± SD) or age range, years: 46.2 ± 11.7 in acupuncture group and 45.9 ± 12.1 in control group Duration of functional dyspepsia before recruitment: 14.5 ± 7.8 months in acupuncture group and 14.7 ± 7.6 months in control group Important inclusion criteria (clearly describe): absent from any gastrointestinal drugs at least 15 days before recruitment Important exclusion criteria (clearly describe): any contraindication listed in the catalogue of control drug itopride; pregnancy; tendency toward bleeding; unconsciousness |
|
| Interventions |
ACUPUNCTURE GROUP Number allocated to acupuncture: 40 Style of acupuncture: electroacupuncture with 2 Hz/100 Hz Numbers and names of points stimulated: a formula of 4 acupoints bilaterally stimulated involving ST34, ST36, ST40, and ST42 Insertion depth: not described Manipulation after insertion: manipulations performed until "de‐qi" occurred "De‐qi" required or not: yes Duration of treatment (minutes): 30 Frequency of treatment per week: 5 times Total length of treatment period (weeks): 4 Description of therapists' qualifications: no CONTROL GROUP Number allocated to control: 40 Style of control: orally Names of medications (if drugs, describe drug names): itopride tablet Dose of medication per intake: 50 mg before meals Frequency of medication per day: 3 times Total length of treatment period (weeks): 4 (actually 20 treatment days) Description of co‐medications: no CO‐INTERVENTIONS IN GROUPS: no |
|
| Outcomes |
Symptom scores of FD (P value < 0.05 when acupuncture was compared with control after treatment) How to assess: 0 points: no symptoms; 1 point: slight symptoms; 2 points: moderate symptoms but not sufficient to affect daily life; 3 points: symptoms severe enough to affect daily life Conclusion from original data: Significance was found in each group pretreatment and post‐treatment and between 2 groups Healing: no symptoms or symptom scores decreased by 3 points (acupuncture 22 cases, control 12 cases); marked effective: symptom scores after treatment decreased by 2 points (acupuncture 11 cases, control 15 cases); effective: symptom scores after treatment decreased by 1 point (acupuncture 6 cases, control 8 cases); invalid: symptom scores after treatment hardly decreased (acupuncture 1 case, control 5 cases) ACUPUNCTURE GROUP: pretreatment 10.21 ± 2.81, post‐treatment 5.78 ± 2.01 (pretreatment vs post‐treatment: P value < 0.01) CONTROL GROUP: pretreatment 10.09 ± 2.95, post‐treatment 6.69 ± 1.99 (pretreatment vs post‐treatment: P value < 0.01) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Quote: "random number table" Comment: probably done |
| Allocation concealment (selection bias) | Unclear risk | Quote: not described Comment: cannot be confirmed |
| Incomplete outcome data (attrition bias) All outcomes | High risk | Quote: not found Comment: probably no |
| Selective reporting (reporting bias) | Low risk | Quote: not found Comment: probably yes |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: not described Comment: Heterogeneity between acupuncture and drugs could result in performance bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: not mentioned whether outcome assessment was done in blinding way Comment: cannot be confirmed |
Zhou 2005.
| Methods | Eligibility criteria: Rome II diagnostic criteria for functional dyspepsia Study duration: 3 weeks Sequence generation: unclear, mentioned just "randomly" in the trial Randomization concealment: not described Blind participants: not described Blind assessors: not described Blind therapists: not described Baseline comparability: It was described that comparability between groups can be seen in baseline values for gender, age, and FD course, but no descriptions of baseline comparability of FD symptoms were reported Follow‐up: no |
|
| Participants | Setting: Shanghai No. 5 People's Hospital Affiliated to Fudan University, Shanghai, China Total number: 126 Male/Female (n/n): 45/81 Mean age (± SD) or age range, years: cannot be extracted directly Duration of functional dyspepsia before recruitment: not mentioned Important inclusion criteria (clearly describe): medication affecting the observation such as anticholinergic, anticonvulsant, emetic, H2‐receptor antagonist had to be withdrawn 1 week before acupuncture treatment Important exclusion criteria (clearly describe): participants with gastrointestinal cancer, peptic ulceration, cholecystitis gallstones, pancreatic disease, diabetes, and hyperthyroidism. All participants had to receive gastroscopy and X‐ray 4 weeks before treatment to exclude organic disorders |
|
| Interventions |
ACUPUNCTURE GROUP Number allocated to acupuncture: 64 Style of acupuncture: manual acupuncture combined with electroacupuncture Numbers and names of points stimulated: a formula of 5 acupoints stimulated involving CV12, ST36 (bilateral), PC6 (bilateral), SP6 (bilateral), and LI4 (bilateral) Insertion depth: not mentioned Manipulation after insertion: Reinforcement and reduction of manipulations were performed until "de‐qi." Then needles on ST36 and SP6 were connected with G6805 electro apparatus for 20 minutes "De‐qi" required or not: yes Duration of treatment (minutes): at least 20 Frequency of treatment per week: 7 times Total length of treatment period (weeks): 3 Description of therapists' qualifications: no, but acupuncture treatments were conducted in the hospital CONTROL GROUP Number allocated to control: 62 Style of control: orally Names of medications (if drugs, describe drug names): domperidone Dose of medication per intake: 10 mg before meals Frequency of medication per day: 3 times Total length of treatment period (weeks): 3 Description of co‐medications: not mentioned CO‐INTERVENTIONS IN GROUPS: manual acupuncture combined electroacupuncture |
|
| Outcomes |
1. Symptom scores of FD How to assess: 0 points: no symptoms; 1 point: mild but not obvious sensations; 2 points: slightly severe symptoms but not sufficient to affect daily life; 3 points: symptoms severe enough to affect daily life Conclusion from original data: Total effective rate in acupuncture group showed significant difference from that of control group (Chi² = 3.97, P < 0.05) Marked effective: Symptom scores after treatment decreased by 2 points (acupuncture 38 cases, control 22 cases); effective: Symptom scores after treatment decreased by 1 point (acupuncture 22 cases, control 29 cases); invalid: Symptom scores after treatment hardly decreased (acupuncture 4 cases, control 11 cases) 2. Efficacy assessment about subtypes of FD by symptom scores Conclusion from original data: Compared with medication group, no significance of the number of total effective cases showed in ulceration, regurgitation and dyskinesia subtypes, except nonspecific subtype ACUPUNCTURE GROUP Total effective: 5 cases of ulceration subtype, 11 cases of regurgitation subtype, 26 cases of dyskinesia subtype, 18 cases of nonspecific subtype Invalid: 2 cases of ulceration subtype, 2 cases of regurgitation subtype, 0 cases of dyskinesia subtype, 0 cases of nonspecific subtype MEDICATION GROUP Total effective: 6 cases of ulceration subtype, 12 cases of regurgitation subtype, 21 cases of dyskinesia subtype, 12 cases of nonspecific subtype Invalid: 3 cases of ulceration subtype, 0 cases of regurgitation subtype, 3 cases of dyskinesia subtype, 5 cases of nonspecific subtype |
|
| Notes | FD symptom description before treatment was lacking. Therefore, baseline FD symptoms in 2 groups cannot be known, whether comparable or not | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Quote: mentioned just "randomly" in the description Comment: cannot be confirmed so far |
| Allocation concealment (selection bias) | Unclear risk | Quote: not described Comment: cannot be identified |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Quote: Lack of FD symptom description before treatment Comment: probably yes |
| Selective reporting (reporting bias) | High risk | Quote: Lack of FD symptom description before treatment Comment: probably no |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Quote: not described Comment: Heterogeneity between acupuncture and drugs could result in performance bias |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Quote: not mentioned whether outcome assessment was done in blinding way Comment: cannot be confirmed for the moment |
Abbreviations: FD: functional dyspepsia. NDI: Nepean Dyspepsia Index. NDLQI: Nepean Dyspepsia Life Quality Index. NDSI: Nepean Dyspepsia Symptom Index. SD: standard deviation. SF‐36: 36‐Item Short‐Form Health Survey. TCM: traditional Chinese medicine.
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Beyazit 2010 | Was a letter to the editors |
| Chen 2005 | The trial was a quasi‐RCT in which participants were allocated as the visiting time |
| Liu S 2008 | The trial was excluded because of its cross‐over trial design |
| Paterson 2003 | FD diagnostic criteria were not known from the description |
| Peng 2008 | The trial was a quasi‐RCT in which participants were allocated as the visiting time |
| Yang 2009a | The trial was a quasi‐RCT in which participants were allocated as the visiting time |
Characteristics of studies awaiting assessment [ordered by study ID]
Cao 2007.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Full text cannot be obtained, so details of the trial cannot be had |
Cash 2001.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Full text cannot be obtained, so details of the trial cannot be had |
Sun 2006.
| Methods | |
| Participants | |
| Interventions | |
| Outcomes | |
| Notes | Full text cannot be obtained, so details of the trial cannot be had |
Zhang 2009b.
| Methods | Eligibility criteria: Rome III diagnostic criteria for functional dyspepsia Study duration: 4 weeks Sequence generation: random number table Randomization concealment: not described Blind participants: not described Blind assessors: not described Blind therapists: not described Baseline comparability: yes, baseline comparability between groups can be seen in gender, age, FD course, and FD symptoms Follow‐up: no |
| Participants | Setting: Traditional Chinese Medicine Hospital of Wuhan, Hubei Province, China Total number: 48 Male/Female (n/n): 27/21 Mean age (± SD) or age range, years: 35.70 ± 11.43 in acupuncture group and 35.23 ± 11.25 in control group Duration of functional dyspepsia before recruitment: 18.40 ± 12.72 months in acupuncture group and 18.17 ± 13.54 months in control group Important inclusion criteria (clearly describe): no entry to other clinical trials when recruitment; absent from any gastrointestinal drugs at least 15 days before recruitment Important exclusion criteria (clearly describe): any contraindication listed in the catalogue of control drug itopride; pregnancy; tendency toward bleeding; unconsciousness |
| Interventions |
ACUPUNCTURE GROUP Number allocated to acupuncture: 24 Style of acupuncture: electroacupuncture with 2 Hz/100 Hz Numbers and names of points stimulated: a formula of 3 acupoints stimulated involving CV12, ST36 (lateral), and BL21 (bilateral) Insertion depth: not described clearly Manipulation after insertion: rotating, lifting, and thrusting until "de‐qi" "De‐qi" required or not: yes Duration of treatment (minutes): 30 Frequency of treatment per week: 5 times Total length of treatment period (weeks): 4 Description of therapists' qualifications: No, but the acupuncture treatment was performed in the outpatent department CONTROL GROUP Number allocated to control: 24 Style of control: orally Names of medications (if drugs, describe drug names): itopride tablet Dose of medication per intake: 50 mg before meals Frequency of medication per day: 3 times Total length of treatment period (weeks): 4 (actually 20 treatment days). Description of co‐medications: no CO‐INTERVENTIONS IN GROUPS: no |
| Outcomes |
1. Symptom scores of FD How to assess: 0 points: no symptoms; 1 point: slight symptoms; 2 points: moderate symptoms but not sufficient to affect daily life; 3 points: symptoms severe enough to affect daily life Conclusion from original data: Significance was found in acupuncture group compared with control group Healing: no symptoms or symptom scores decreased by 3 points (acupuncture 14 cases, control 10 cases); marked effective: symptom scores after treatment decreased by 2 points (acupuncture 5 cases, control 7 cases); effective: symptom scores after treatment decreased by 1 point (acupuncture 3 cases, control 2 cases); invalid: symptom scores after treatment hardly decreased (acupuncture 2 cases, control 5 cases) Scores for each FD symptom ACUPUNCTURE GROUP Postprandial discomfort: pretreatment 2.00 ± 0.63, post‐treatment 0.85 ± 0.47(pretreatment vs post‐treatment: P value < 0.01) Early satiety: pretreatment 1.98 ± 0.50, post‐treatment 0.75 ± 0.36 (P value < 0.05) Epigastric pain: pretreatment 1.92 ± 0.44, post‐treatment 0.72 ± 0.35 (P value < 0.05) Epigastric burning sensation: pretreatment 1.47 ± 0.49, post‐treatment 1.42 ± 0.48 (P value > 0.05) CONTROL GROUP Postprandial discomfort: pretreatment 2.02 ± 0.68, post‐treatment 0.87 ± 0.37 (pretreatment vs post‐treatment: P value < 0.05) Early satiety: pretreatment 1.96 ± 0.52, post‐treatment 1.07 ± 0.49 (P value > 0.05) Epigastric pain: pretreatment 1.95 ± 0.51, post‐treatment 1.02 ± 0.47 (P value > 0.05) Epigastric burning sensation: pretreatment 1.51 ± 0.52, post‐treatment 1.39 ± 0.44 (P value > 0.05) 2. SF‐36 scale Conclusion from original data: No significance was found between acupuncture and control groups. Life quality in acupuncture group was improved for each item. However, items except for physiologic performance in the control group showed no significance ACUPUNCTURE GROUP Physiologic function: pretreatment 90.39 ± 9.17, post‐treatment 94.32 ± 7.09 (pretreatment vs post‐treatment: P value < 0.05) Physiologic performance: pretreatment 55.37 ± 12.26, post‐treatment 75.89 ± 20.98 (P value < 0.05) Body pain: pretreatment 60.27 ± 23.80, post‐treatment 81.32 ± 20.74 (P value < 0.01) General health: pretreatment 64.38 ± 15.31, post‐treatment 82.31 ± 15.78 (P value < 0.05) Vitality: pretreatment 69.33 ± 13.01, post‐treatment 82.72 ± 15.03 (P value < 0.05) Social function: pretreatment 64.33 ± 15.08, post‐treatment 85.74 ± 15.10 (P value < 0.05) Role‐emotion: pretreatment 49.88 ± 23.20, post‐treatment 79.99 ± 23.94 (P value < 0.01) Mental health: pretreatment 73.32 ± 15.03, post‐treatment 80.77 ± 18.02 (P value < 0.05) CONTROL GROUP Physiologic function: pretreatment 91.17 ± 7.02, post‐treatment 92.08 ± 7.04 (pretreatment vs post‐treatment:P value > 0.05) Physiologic performance: pretreatment 58.67 ± 19.99, post‐treatment 59.76 ± 20.00 (P value < 0.05) Body pain: pretreatment 56.72 ± 13.43, post‐treatment 57.23 ± 13.55 (P value > 0.05) General health: pretreatment 68.10 ± 14.76, post‐treatment 70.20 ± 15.01 (P value > 0.05) Vitality: pretreatment 68.03 ± 12.21, post‐treatment 71.23 ± 12.84 (P value > 0.05) Social function: pretreatment 66.00 ± 14.17, post‐treatment 68.01 ± 14.99 (P value > 0.05) Role‐emotion: pretreatment 51.00 ± 19.12, post‐treatment 53.27 ± 19.78 (P value > 0.05) Mental health: pretreatment 75.13 ± 13.60, post‐treatment 76.32 ± 14.00 (P value > 0.05) |
| Notes | With MD data transformation, SF‐36 results were unclear and required explanation; however, we could not get in touch with the study author |
Differences between protocol and review
No significant differences have been noted between the protocol and the review.
Contributions of authors
Lan Lei, Liu Mailan, and Wu Xi obtained copies of trials and selected the identified trials.
Lan Lei, Zeng Fang, Ying Li, and Liu Mailan extracted data and assessed the risk of bias of included trials.
Lan Lei and Liu Guanjian performed analyses of data.
Lan Lei and Zeng Fang were responsible for the draft of the review.
Lan Lei and Liang Fan‐rong were responsible for submitting the systematic review and updating it.
Sources of support
Internal sources
-
National Basic Research Program of China (973 Program) No.2012CB518501, China.
supported by The Ministry of Science and Technology of the People's Republic of China
-
National Basic Research Program of China (973 Program) No. 2006CB504501, China.
Supported by The Ministry of Science and Technology of the People's Republic of China
External sources
No sources of support supplied
Declarations of interest
Ling Ying, one author of this review, once participated in an included trial of acupuncture for FD. Therefore, Ling Ying did not take part in the data selection and analysis process.
New
References
References to studies included in this review
Chang 2010 {published and unpublished data}
- Chang XR, Lan L, Yan J, Wang XJ, Chen HM. Efficacy of acupuncture at Foot‐Yangming Meridian in the treatment of patients with functional dyspepsia: an analysis of 30 cases. World Chinese Journal of Digestology 2010;18(8):839‐44. [DOI: 10.3969/j.issn.1009-3079.2010.08.017] [DOI] [Google Scholar]
Jin 2011 {published and unpublished data}
- Jin Y. Efficacy of acupuncture in the treatment of patients with functional dyspepsia. Unpublished medicine master dissertation. Beijing University of Chinese Medicine. 2011.
Park 2009 {published and unpublished data}
- Park YC, Kang W, Choi SM, Son CG. Evaluation of manual acupuncture at classical and nondefined points for treatment of functional dyspepsia: a randomized‐controlled trial. Journal of Alternative and Complementary Medicine 2009;15(8):879‐84. [DOI: 10.1089/acm.2008.0369] [DOI] [PubMed] [Google Scholar]
Shi 2009 {published and unpublished data}
- Shi H, Zhang J, Guo H. Clinical observation of acupuncture for 90 cases of patients with functional dyspepsia. Beijing Journal of Traditional Chinese Medicine 2009;28(9):732‐3. [Google Scholar]
Tang 2006 {published and unpublished data}
- Tang S, Xu Z, Tang P, Liang L. Acupuncture for functional dyspepsia: a randomised controlled trial. Journal of Sichuan Traditional Chinese Medicine 2006;24(4):101‐2. [Google Scholar]
Yang 2009 {published and unpublished data}
- Yang M. EIectroacupuncture treatment of functionaI dyspepsia from a cIinical research. Unpublished medicine master dissertation, Hubei University of TCM. 2009.
Zhou 2005 {published and unpublished data}
- Zhou Y, Zheng JG. Clinical observation on acupuncture treatment of functional dyspepsia. Journal of Acupuncture and Tuina Science 2005;3(2):20‐2. [DOI: 10.1007/BF02845366] [DOI] [Google Scholar]
References to studies excluded from this review
Beyazit 2010 {published and unpublished data}
- Beyazit Y, Kekilli M, Purnak T. Effects of transcutaneous electrical acu‐stimulation in patients with functional dyspepsia. Alimentary Pharmacology and Therapeutics 2010;31(9):961‐8. [DOI] [PubMed] [Google Scholar]
Chen 2005 {published and unpublished data}
- Chen JY, Pan F, Xu JJ, Zhan CE. Effects of acupuncture on the gastric motility in patients with functional dyspepsia. Chinese Journal of Integrated Traditional and Western Medicine 2005;25(10):880‐2. [PubMed] [Google Scholar]
Liu S 2008 {published and unpublished data}
- Liu S, Peng S, Hou X, Ke M, Chen JD. Transcutaneous electroacupuncture improves dyspeptic symptoms and increases high frequency heart rate variability in patients with functional dyspepsia. Neurogastroenterology and Motility 2008;20(11):1204‐11. [DOI] [PubMed] [Google Scholar]
Paterson 2003 {published and unpublished data}
- Paterson C, Ewings P, Brazier JE, Britten N. Treating dyspepsia with acupuncture and homeopathy: reflections on a pilot study by researchers, practitioners and participants. Complementary Therapies in Medicine 2003;11(2):78‐84. [DOI] [PubMed] [Google Scholar]
Peng 2008 {published and unpublished data}
- Peng SF, Yang JY, Shi ZH. Electroacupuncture improves gastric motility, autonomic nerve activity and psychological state in patients with functional dyspepsia. World Chinese Journal of Digestology 2008;16(36):4105‐9. [Google Scholar]
Yang 2009a {published and unpublished data}
- Yang M, Zhang H, Zou R. Effects of acupuncture on the gastric motility in patients with functional dyspepsia. Chinese Journal of Rehabilitation 2009;24(2):100‐2. [Google Scholar]
References to studies awaiting assessment
Cao 2007 {published and unpublished data}
- Cao J, Qu F, Zhou J. Improvement of gastric movement in patients with functional dyspepsia, treated with acupuncture. International Journal of Clinical Acupuncture 2007;16(1):23‐6. [Google Scholar]
Cash 2001 {published and unpublished data}
- Cash BD, Schoenfeld P. Alternative medical therapies for dyspepsia: a systematic review of randomized trials. In: Johnson DA, Katz PO, Castell DO editor(s). Dyspepsia. Philadelphia, PA: American College of Physicians ‐ American Society of Internal Medicine, 2001:159‐75. [Google Scholar]
Sun 2006 {published and unpublished data}
- Sun D, Cao J. Observation of the therapeutic effect of acupuncture on 58 cases of functional dyspepsia. International Journal of Clinical Acupuncture 2006;15(3):169‐72. [Google Scholar]
Zhang 2009b {published and unpublished data}
- Zhang W. The cIinical observation of Shu Mu with eIectroacupuncture treatment on functionaI dyspepsia. Unpublished medicine master dissertation, Hubei University of TCM. 2009.
Additional references
Altman 2001
- Altman DG, Schulz KF, Moher D, Egger M, Davidoff F, Elbourne D, et al. The revised CONSORT statement for reporting randomized trials: explanation and elaboration. Annals of Internal Medicine 2001;134(8):663‐94. [DOI] [PubMed] [Google Scholar]
Chen 1998
- Chen R, Kang M. Observation on frequency spectrum of electrogastrogram (EGG) in acupuncture treatment of functional dyspepsia. Journal of Traditional Chinese Medicine 1998;18:184‐7. [PubMed] [Google Scholar]
Deng 1997
- Deng L, Gan Y, He S, Ji X, Li Y, Wang R, et al. Chinese Acupuncture and Moxibustion. Vol. 54, Beijing: Foreign Languages Press, 1997:71‐4. [Google Scholar]
Drossman 2006
- Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology 2006;130:1377–90. [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta‐analyses. BMJ 2003;327:557‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Holtmann 2006
- Holtmann G, Talley NJ, Liebregts T, Adam B, Parow C. A placebo controlled trial of itopride in functional dyspepsia. New England Journal of Medicine 2006;354:832‐40. [DOI] [PubMed] [Google Scholar]
Lao 1996
- Lao L. Acupuncture techniques and devices. Journal of Alternative and Complementary Medicine 1996;2:23–5. [DOI] [PubMed] [Google Scholar]
MacPherson 2010
- MacPherson H, Altman DG, Hammerschlag R, Youping L, Taixiang W, White A, et al. Revised standards for reporting interventions in clinical trials of acupuncture (STRICTA): extending the CONSORT statement. Journal of Evidence‐Based Medicine 2010;3(3):140‐55. [PUBMED: 21349059] [DOI] [PubMed] [Google Scholar]
Mahadeva 2006
- Mahadeva S, Goh KL. Epidemiology of functional dyspepsia: a global perspective. World Journal of Gastroenterology 2006;12(17):2661‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mönkemüller 2006
- Mönkemüller K, Malfertheiner P. Drug treatment of functional dyspepsia. World Journal of Gastroenterology 2006;12(17):2694‐700. [DOI] [PMC free article] [PubMed] [Google Scholar]
Noguchi 2008
- Noguchi E. Mechanism of reflex regulation of the gastroduodenal function by acupuncture. Evidence‐based Complementary and Alternative Medicine 2008;5(3):251‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan 2011 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.1. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2011.
Rome III 2006
- Rome III Diagnostic Criteria for Functional Gastrointestinal Disorders. http://www.romecriteria.org/assets/pdf/19_RomeIII_apA_885‐898.pdf (accessed 7 July 2014).
Schneider 2007
- Schneider A, Streitberger K, Joos S. Acupuncture treatment in gastrointestinal diseases: a systematic review. World Journal of Gastroenterology 2007;13(25):3417‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Xu 2004
- Xu S, Zha H, Hou X, Gao Z, Zhang Y, Chen JD, et al. Electroacupuncture accelerates solid gastric emptying in patients with functional dyspepsia. Gastroenterology 2004;126:A‐437. [DOI] [PubMed] [Google Scholar]
Zeng 2009
- Zeng F, Song WZ, Liu XG, Xie HJ, Tang Y, Shan BC, et al. Brain areas involved in acupuncture treatment on functional dyspepsia patients: a PET‐CT study. Neuroscience Letters 2009;456(1):6‐10. [DOI] [PubMed] [Google Scholar]
Zeng 2011
- Zeng F, Qin W, Liang F, Liu J, Tang Y, Liu X, et al. Abnormal resting brain activity in patients with functional dyspepsia is related to symptom severity. Gastroenterology 2011;141(2):499‐506. [DOI] [PubMed] [Google Scholar]
Zhu 2008
- Zhu H. Acupuncture for functional dyspepsia: a systematic review. Unpublished medicine master dissertation. Chengdu University of TCM. 2008.


