Abstract
Background and Objectives
The objective of this study was to determine the relationship between plasma β-amyloid (Aβ), specifically the ratio of 2 Aβ peptides (the Aβ42/Aβ40 ratio, which correlates with increased accumulation of Aβ in the CNS), and late-onset epilepsy (LOE).
Methods
We used Medicare fee-for-service claims codes from 1991 to 2018 to identify cases of LOE among 1,424 Black and White men and women enrolled in the Atherosclerosis Risk in Communities (ARIC) study cohort. The Aβ42/Aβ40 ratio was calculated from plasma samples collected from ARIC participants in 1993–1995 (age 50–71 years) and 2011–2013 (age 67–90 years). We used survival analysis accounting for the competing risk of death to determine the relationship between late-life plasma Aβ42/Aβ40, and its change from midlife to late life, and the subsequent development of epilepsy. We adjusted for demographics, the apolipoprotein e4 genotype, and comorbidities, including stroke, dementia, and head injury. A low plasma ratio of 2 Aβ peptides, the Aβ42/Aβ40 ratio, correlates with low CSF Aβ42/Aβ40 and with increased accumulation of Aβ in the CNS.
Results
Decrease in plasma Aβ42/Aβ40 ratio from midlife to late life, but not an isolated measurement of Aβ42/Aβ40, was associated with development of epilepsy in later life. For every 50% reduction in Aβ42/Aβ40, there was a 2-fold increase in risk of epilepsy (adjusted subhazard ratio 2.30, 95% CI 1.27–4.17).
Discussion
A reduction in plasma Aβ42/Aβ40 is associated with an increased risk of subsequent epilepsy. Our observations provide a further validation of the link between Aβ, hyperexcitable states, and LOE.
Introduction
Aggregations of β-amyloid (Aβ) in the brain are a hallmark of Alzheimer disease (AD). Aβ measured by brain PET with tracer or through the CSF is widely used to classify AD1 and to predict progression to cognitive impairment and dementia.2,3 However, measurements of the CSF are highly invasive, and Aβ-PET is currently prohibitively expensive for use in routine clinical practice. In recent years, Aβ measured from plasma has been found to correlate with CSF levels of Aβ4 and with Aβ in the CNS as measured by PET.5-7 The amyloid precursor molecule is cleaved into peptides of different lengths, with the main final forms the 42-residue length (Aβ42) and 40-residue length (Aβ40). Due to structural differences, these peptides have unique conformational states and can aggregate into plaques in the CNS.8 As plaques deposit in the brain, there is less Aβ in the periphery. In particular, the ratio of the Aβ42 to Aβ40 peptides has become a recognized marker for CNS Aβ. Specifically, a lower Aβ42/Aβ40 ratio in the CSF or plasma is correlated with a higher burden of CNS plaque deposition,5-7 and low plasma and CSF levels are believed to represent increased deposition into insoluble plaques. This biomarker has the potential to be clinically relevant as well. Midlife plasma Aβ42/Aβ40 ratio is associated with later-life cognitive impairment and dementia,9 as was recently demonstrated in the Atherosclerosis Risk in Communities (ARIC) study.10 These findings support the association of a long preclinical period of AD with neuropathologic changes before the first clinical manifestations of memory impairment.
Unexplained new-onset seizures affect more than 100,000 older adults in the United States annually.11 The risk of seizures is elevated in people with AD compared with that in the general population,12 and people with late-onset epilepsy (LOE) are also at an increased risk of subsequent dementia compared with the general population.13,14 One hypothesis for this association is induced hyperexcitability caused by Aβ pathology in the brain.15,16 Two prior studies showed abnormal Aβ in the CSF of cognitively normal persons with unexplained seizures compared with that in healthy controls,17,18 and neuronal hyperexcitability is known to increase Aβ deposition in the brain in animal models.19 However, longitudinal Aβ measurements have not previously been examined in the context of LOE. In this study, we examine measurements of plasma Aβ and longitudinal changes in plasma Aβ and the development of seizures, hypothesizing that a lower plasma Aβ42/Aβ40 ratio and a greater decline over time corresponds to an increased risk of LOE.
Methods
The ARIC study is a longitudinal cohort study, initiated in 1987–1989 in 4 US communities (Forsyth County, NC; Washington County, MD; Jackson, MS; and suburbs of Minneapolis, MN). The ARIC study enrolled 15,792 mostly Black and White men and women, now followed up with 8 study visits (with a ninth visit in progress during this analysis), annual (and since 2011, semiannual) telephone calls, and with continuous hospital discharge and death certificate surveillance. Participants were aged 45–64 years during the first visit (Figure 1).
Figure 1. Timeline of ARIC Visits.
Ages listed are for whole cohort attending each visit. Aβ = β-amyloid; APOE = apolipoprotein; ARIC = Atherosclerosis Risk in Communities; CMS = Centers for Medicare Services.
Outcome Ascertainment
The ARIC study has merged Centers for Medicare and Medicaid Services (CMS) fee-for-service (FFS) claims code data from 1991 to 2018 with participant information. We used a definition of 2 or more epilepsy or seizure-related codes from at least 2 sources (inpatient, outpatient, or carrier files; eTable 1, links.lww.com/WNL/D24), in the first 5 diagnostic positions, to ascertain epilepsy.13,20,21 To identify incident epilepsy, we identified participants with at least 2 years of FFS coverage before the first seizure-related code (excluding those with earlier seizures). Because most participants became eligible for Medicare coverage at age 65 years, we considered only those with first seizure code at age 67 years or later, to allow for a confirmed 2-year seizure-free period.
Plasma Aβ Measurement
A subset of ARIC participants had plasma samples from visit 3 (1993–1995, at which participants with amyloid sampled were 50–71 years of age) and visit 5 (2011–2013, at which participants with amyloid sampled were 67–90 years of age) analyzed for Aβ40 and Aβ42. This subset consisted of 50% participants with prevalent cognitive impairment at visit 5, and 50% participants unimpaired at visit 5, randomly selected across 2 age strata (younger than 80 years and aged 80 years or older). Criteria for cognitive impairment in the ARIC have been previously detailed.22 Procedures for blood sampling in the ARIC have been previously described in detail.23 Whole-blood samples were obtained from fasting participants in EDTA tubes, were stored in an ice bath, and plasma was separated by centrifugation at 4°C. Plasma was stored in −80°C freezers in 1.5-mL tubes. The plasma Aβ assay was performed in 2014 at the Mayo Clinic, Jacksonville, FL, with the INNO-BIA assay (Innogenetics, Ghent, Belgium10). This is a fluorometric bead-based immunoassay that measures peptides Aβ1–42 and Aβ1–40. Bound Aβ fluorescence was detected by a Luminex 200 IS Total System instrument (Luminex Corp, Austin, TX). The same plate was used to quantify plasma Aβ from visit 3 and 5 samples simultaneously for each participant. Then, Aβ40 and Aβ42 concentrations (in picograms per milliliter) were predicted through a logistic regression model by relating the observed fluorescence intensities to a standard curve.10
For analysis, we considered the plasma Aβ42/Aβ40 ratio from visit 5 and change in Aβ42/Aβ40 ratio from visit 3 to visit 5. We hypothesized that lower Aβ42/Aβ40 ratio at visit 5, and a greater decrease in Aβ42/Aβ40 ratio from visit 3 to visit 5, would be associated with LOE. Due to a skewed distribution, we used the base 2 log of the plasma ratio for analysis.10 The use of the base 2 logarithm allows for intuitive comparisons, because each increase by 1 in the log2 ratio is equivalent to a doubling of the raw ratio. Because most participants were younger than 67 years at visit 3, we did not examine visit 3 Aβ measurements in isolation to avoid immortal time bias.
Covariates
Demographic information and blood sample for DNA sequencing for the apolipoprotein E genotype (Taqman) were collected at visit 1. At visit 5, blood pressure was measured 3 times, and the second and third measurements averaged. Medications and medical history were recorded, and blood glucose level, weight, and height measured. We considered participants to have hypertension if they had an averaged systolic blood pressure (of 2 measurements taken at each visit) of ≥140 mm Hg or averaged diastolic blood pressure of ≥90 mm Hg or if they used an antihypertensive agent. We considered participants to have diabetes if they had fasting blood glucose ≥126 mg/dL, nonfasting blood glucose ≥200 mg/dL, or used a diabetic medication or insulin. Body mass index (BMI) was calculated from height and weight. Prevalent stroke was self-reported at visit 1, and incident strokes during subsequent follow-up were recorded from hospital surveillance by computer algorithm and adjudicated by cerebrovascular experts. Dementia was ascertained from in-person neuropsychological testing starting at visit 5 and from telephone testing of the participants, interviews with their informants, and hospital and death certificate surveillance with expert adjudication. Head injury was ascertained from participant self-report, CMS claims codes (eTable 2, links.lww.com/WNL/D24), and ARIC hospitalization surveillance.
Statistical Analysis
We used survival analysis accounting for the competing risk of death24 to determine the association of plasma Aβ42/Aβ40 ratio with development of LOE, using visit 5 as the origin and LOE as the failure. Participants without LOE were censored on December 31, 2018 (last date of available CMS data). The 2 participants younger than 67 years at visit 5, therefore not eligible for CMS Medicare benefits, were excluded from analyses. We adjusted for age, sex, a combined field center-race variable (as is standard in the ARIC due to some centers being primarily monoracial), hypertension, diabetes, APOE genotype, self-reported sleep apnea, BMI, and history of stroke, dementia, and head injury. Stroke, dementia, and head injury were included as time-varying variables.
To examine the change in plasma Aβ42/Aβ40 ratio, we subtracted plasma visit 5 data from visit 3 data; thus, a positive number corresponded to a decrease in plasma Aβ42/Aβ40 ratio from visit 3 to visit 5.
Due to the known relationships between plasma Aβ and dementia10 and between dementia and LOE13,14 we also performed analyses stratified by cognitive diagnosis at visit 5 (normal; MCI or dementia). We used Stata version 16.0 (College Station, TX) for analysis.
Sensitivity Analyses
We performed a sensitivity analysis excluding individuals who developed LOE within 2 years of the last plasma Aβ measurement, in case subclinical seizures preceded the clinical diagnosis of LOE.
Participants who had measurement of plasma Aβ were oversampled for those with mild cognitive impairment and dementia at visit 5. We therefore performed a sensitivity analysis using sampling weights to make our estimates representative of all visit 5 participants (inverse probability weighting [IPW]). Weights were constructed from a base weight representing sampling probability, adjusted for participant refusal.
Standard Protocol Approvals, Registrations, and Patient Consents
All participants provided written informed consent at each visit. Each field center obtained IRB approval.
Data Availability
Deidentified ARIC data are available through the NIH Heart, Lung, and Blood Institute–sponsored Biologic Specimen and Data Repository Information Coordinating Center.
Results
In total, 2,585 participants had plasma Aβ measured from plasma collected at visits 3 and 5. One thousand six hundred fifty-two participants with plasma Aβ measured at visits 3 and 5 also had sufficient FFS coverage for LOE ascertainment; of them, 49 had LOE (Figure 2). Of them, 1,424 had all covariate data available and 33 had LOE with first seizure code after visit 5 and were thus included in the primary analysis. The mean time to first seizure code after visit 5 in those with LOE was 4.4 years (SD 1.6 years). In this subset of ARIC participants with plasma Aβ (which is enriched for those with cognitive impairment, as described earlier), the incidence of LOE was 4.16 (95% CI 2.97–5.82) per 1,000 person-years. Compared with those without LOE, participants with LOE were more likely to have cognitive impairment at visit 5 (p < 0.001; Table 1). Among participants without LOE, visit 5 Aβ42/Aβ40 ratio was lower in those with cognitive impairment or dementia than in those with normal cognition (0.167 vs 0.175, p = 0.029); there was no difference in plasma Aβ42/Aβ40 ratio between those with cognitive impairment or dementia and those with normal cognition in the smaller number with LOE (0.160 vs 0.167, p = 0.710).
Figure 2. Box Plots of Aβ42/Aβ40 Ratio at Visit 3 and Visit 5 in Participants With and Without Late-Onset Epilepsy (LOE).
Aβ = β-amyloid.
Table 1.
ARIC Participant Characteristics at Visit 5
In survival analysis with a mean follow-up of 5.4 years (SD 1.5), plasma Aβ42/Aβ40 ratio at visit 5 was not associated with later development of LOE (p = 0.267; Table 2). However, the change in Aβ42/Aβ40 ratio from visit 3 to visit 5 was associated with LOE, with the decline from visit 3 to visit 5 in Aβ42/Aβ40 ratio associated with a greater risk of developing LOE after visit 5 (Figure 3). A 50% reduction in the Aβ42/Aβ40 ratio from visit 3 to visit 5 corresponded to a 2-fold greater risk of LOE, which persisted after adjusting for the covariates that included stroke, dementia, head injury, and vascular comorbidities (adjusted subhazard ratio [aSHR] 2.30, 95% CI 1.27–4.17; Table 2). The addition of BMI and sleep apnea did not substantially change the relationship between change in plasma Aβ 42/40 ratio and epilepsy (aSHR 2.44, 95% CI 1.26–4.72). Self-reported sleep apnea itself was not independently associated with LOE (aSHR 1.32, 95% CI 0.45–3.88; Table 2).
Table 2.
Hazard of Developing Late-Onset Epilepsy After Visit 5 Associated With Plasma Amyloid Measurements, With Competing Risk of Death
Figure 3. Plasma Aβ42/Aβ40 Ratio at Visit 3 vs Visit 5 in Participants With and Without Late-Onset Epilepsy (LOE), by Comorbidities.
Each participant was characterized as no history of stroke or dementia (top row), prevalent dementia (by visit 5) or incident dementia (after visit 5; middle row), or prevalent stroke (by visit 5) or incident stroke (after visit 5; bottom row). Each plot has the line y = x. A larger decrease in the Aβ42/Aβ40 ratio from visit 3 to visit 5 was associated with LOE. The markers in the upper/left half of the graph represent participants with a higher Aβ42/Aβ40 ratio at visit 3 and a lower Aβ42/Aβ40 ratio at visit 5, while the markers in the lower/right half of the graph represent participants with a lower Aβ42/Aβ40 ratio at visit 3 and a higher Aβ42/Aβ40 ratio at visit 5. Aβ = β-amyloid.
After stratifying by cognitive status at visit 5, in the 778 participants with normal cognition at visit 5, there were 13 cases of LOE after visit 5. The relationship between change in plasma Aβ42/Aβ40 ratio and LOE had similar magnitude to that in the whole sample, but the 95% CI included 1 (aSHR 2.34, 95% CI 0.88–6.27). In the 643 participants with MCI or dementia at visit 5, the relationship persisted (aSHR 2.24, 95% CI 1.02–4.98). Analyses additionally stratified as MCI only and dementia only at visit 5 are in eTable 3, links.lww.com/WNL/D24; the relationship between change in plasma Aβ42/Aβ40 ratio and LOE was strongest in the 78 participants with dementia at visit 5.
In the sensitivity analysis excluding the 2 participants whose first seizure-related code occurred within 2 years of the last Aβ measurement, the relationship between change in plasma Aβ42/Aβ40 ratio and LOE persisted, with adjusted SHR 2.63 (95% CI 1.44–4.82).
In the sensitivity analysis using IPW for representation of the full cohort at visit 5, the relationship between change in plasma Aβ42/Aβ40 ratio persisted (aSHR 2.99, 95% CI 1.43–6.29). In this sensitivity analysis, stratifying by cognitive status at visit 5 found that change in plasma Aβ42/Aβ40 ratio was associated with LOE in participants both with and without dementia (Table 3). In the IPW sensitivity analysis, among individuals with normal cognition at visit 5, the relationship between change in plasma Aβ42/Aβ40 ratio and LOE persisted even after adjusting for incident dementia after visit 5 (which occurred in 200 individuals; aSHR 3.00, 95% CI 1.37–6.57, p = 0.006).
Table 3.
Hazard of Developing Late-Onset Epilepsy After Visit 5 Associated With Plasma Amyloid Measurements, With Competing Risk of Death

Discussion
We found that a reduction in the plasma Aβ42/Aβ40 ratio from midlife to later life was positively associated with the risk of developing LOE in later life. This research aligns with prior studies that found increased prevalence of “pathologic” Aβ in the CSF of nondemented people with LOE compared with that in healthy controls.17,18 Our findings are also supported by the relationships observed in other studies between plasma Aβ42/Aβ40 ratio and dementia10,25 and between LOE and dementia.14,26-28 In the ARIC study, high visit 3 and visit 5 Aβ42/Aβ40 ratios (in all participants) were each associated with a lower risk of cognitive impairment compared with higher Aβ42/Aβ40 ratios.10 Each doubling of visit 3 Aβ42/Aβ40 ratio was associated with a 37% reduction in risk of later cognitive impairment, and each doubling of visit 5 Aβ42/Aβ40 ratio was associated with a 23% reduction in the risk of cognitive impairment.
As outlined earlier, low Aβ42/Aβ40 ratio in the CSF or plasma is correlated with high CNS Aβ plaque burden5-7 because low plasma and CSF levels are believed to represent deposition into insoluble plaques and less freely circulating Aβ. CNS Aβ is implicated in synaptic dysfunction in AD and may lead to an increase of excitatory synaptic transmission at low concentrations.29 Animal studies provide many possible explanations for the relationship between CNS Aβ and induced hyperexcitability. For example, transgenic mouse models of AD demonstrate that animals with increased brain Aβ have epileptiform spiking activity and seizures.30 Aβ may also alter synaptic transmission, reduce interneuron GABAergic activity, and alter the normal slow-wave oscillations in the brain.31-34 In humans, an investigation of autosomal dominant early-onset AD families with identified genetic variants found that those with a duplication of the amyloid precursor protein, which is associated with overproduction of Aβ, had the highest rates of clinical seizures (occurring in 81% of individuals).35 Prior studies have identified lower CSF Aβ and higher CSF tau in persons with normal cognition and unexplained LOE compared with healthy controls without seizures along with higher rates of progression to dementia in those with unexplained seizures.17,18 Retrospective studies of people with AD have found increased rates of adult-onset epilepsy in the 5 years preceding cognitive symptoms36 and have also found that those with epileptiform activity have faster cognitive decline than do those without.37 This study adds to this growing body of evidence that there may be shared pathophysiology between neurodegenerative disorders and unexplained LOE.
Of interest, we did not find a relationship between a single measurement of Aβ42/Aβ40 ratio in later life and LOE; rather, the change from midlife to later life was associated with later development of LOE. This may suggest that the rate or duration of Aβ accumulation in the brain has an effect on hyperexcitability; additional studies are needed to support this conclusion.
One important caveat is that animal studies also show that seizures increase Aβ. Indeed, in humans, patients with childhood-onset epilepsy have a higher amyloid burden in adulthood than do healthy controls.38 Thus, it is possible that early subclinical seizures in people who would go on to develop clinically recognized LOE actually occurred first, increasing Aβ deposition in the CNS. However, our findings persisted after adjusting for diagnosis of dementia, suggesting that people with LOE may also have decreased peripheral Aβ and increased CNS Aβ. In addition, in our sensitivity analysis excluding participants whose first clinical seizure diagnosis occurred within 2 years of the last Aβ measurement, this association persisted. Given the abovementioned considerations, there is most likely a bidirectional relationship between Aβ and seizures in susceptible persons.
Because plasma Aβ42/Aβ40 ratio is associated with cognitive impairment and dementia and because seizures are elevated in clinically diagnosed dementia (and even preceding recognition of dementia36), it is possible that our observed association is driven solely by these relationships. However, we adjusted our models for development of dementia, which did not alter the findings. Stratified analysis of the subset of participants without dementia or MCI at visit 5 included a smaller number of participants who developed LOE, but the magnitude of the relationship was similar across participants with and without cognitive impairment and the whole study population. In addition, the IPW sensitivity analyses accounting for the oversampling of cognitively impaired participants in the amyloid measurement subset did show the relationship between change in amyloid and LOE in individuals with normal cognition at visit 5, including after adjustment for incident dementia.
Other limitations of this study include the reliance on CMS codes for identification of LOE and therefore the potential for misclassification errors and the lack of information about seizure type, frequency, or severity. This and similar definitions of LOE have been validated against a gold standard of chart review, with sensitivities and specificities of 85%–97%.39,40 In addition, the number of participants with measurement of plasma Aβ and LOE is small; however, the incidence of LOE in this sample is similar to the expected incidence from prior population studies,11,21 with the known increased incidence of LOE in dementia20,41 (because 50% of the participants with plasma Aβ measurement had cognitive impairment at visit 5). In addition, Aβ was measured in 2014 before widespread adoption of newer techniques now used to measure Aβ (single-molecule array and mass spectrometry42,43). These weaknesses are balanced with the strengths of this study; in particular, the use of multiple measurements of plasma Aβ from samples acquired before first clinical recognition of seizures and the diversity of the ARIC cohort. Future studies of plasma and CSF Aβ and brain imaging and more detailed clinical information about seizure types and frequencies would be of great importance to further define this relationship.
A reduction in plasma Aβ42/Aβ40 ratio from midlife to later life, but not the Aβ42/Aβ40 ratio in later life alone, was associated with LOE. Our observations provide a further validation of the link between Aβ, hyperexcitable states, and LOE.
Acknowledgment
The authors thank the staff and participants of the ARIC study for their important contributions.
Glossary
- AD
Alzheimer disease
- ARIC
Atherosclerosis Risk in Communities
- aSHR
adjusted subhazard ratio
- Aβ
amyloid
- BMI
body mass index
- CMS
Centers for Medicare and Medicaid Services
- FFS
fee-for-service
- IPW
inverse probability weighting
- LOE
late-onset epilepsy
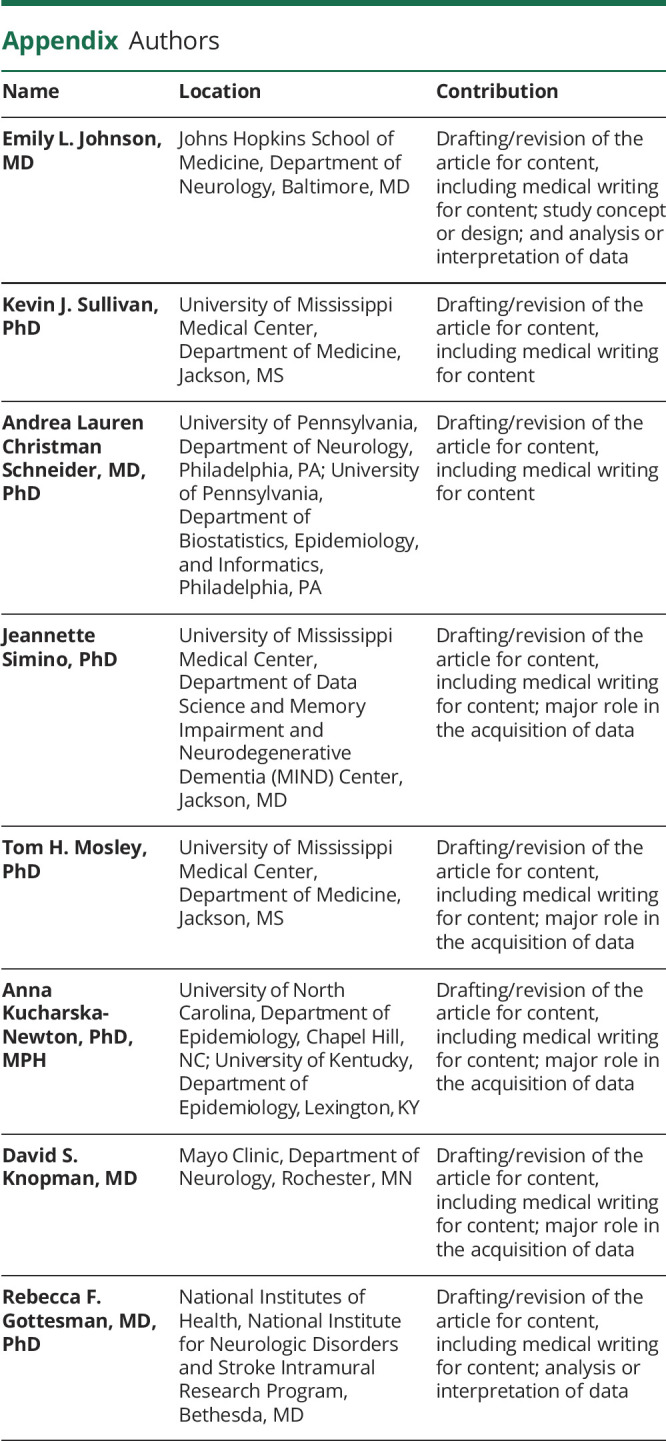
Appendix. Authors
Footnotes
Editorial, page 551
Study Funding
The Atherosclerosis Risk in Communities study has been funded in whole or in part with Federal funds from the National Heart, Lung, and Blood Institute, NIH, Department of Health and Human Services, under Contract nos (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700004I, and HHSN268201700005I). Neurocognitive data are obtained by grants U01 HL096812, U01 HL096814, U01 HL096899, U01 HL096902, and U01 HL096917 from the National Heart, Lung, and Blood Institute, with funding also provided by the National Institute of Neurologic Disorders and Stroke. This study was also supported by K23 AG063899 (E.L. Johnson), from the National Institute on Aging.
Disclosure
E.L. Johnson reports no disclosures relevant to this manuscript. A. Kucharska-Newton, and K.J. Sullivan report no disclosures relevant to this manuscript. A.L.C. Schneider was supported by the National Institute of Neurological Disorders and Stroke K23 NS123340. J. Simino reports no disclosures relevant to this manuscript. D.S. Knopman reports serving on a Data Safety Monitoring Board for the Dominantly Inherited Alzheimer Network (DIAN) study. He serves on a Data Safety Monitoring Board for a tau therapeutic for Biogen but receives no personal compensation. He is an investigator in clinical trials sponsored by Lilly Pharmaceuticals and the University of Southern California. He serves as a consultant for Samus Therapeutics, Third Rock, Roche, and Alzeca Biosciences but receives no personal compensation. T.H. Mosley reports no disclosures relevant to this manuscript. R.F. Gottesman was supported by the National Institute of Neurologic Disorders and Stroke intramural research program. Go to Neurology.org/N for full disclosures.
References
- 1.Jack CR, Bennett DA, Blennow K, et al. NIA-AA Research Framework: toward a biological definition of Alzheimer's disease. Alzheimers Dement. 2018;14(4):535-562. doi. 10.1016/J.JALZ.2018.02.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jack CR, Knopman DS, Jagust WJ, et al. Hypothetical model of dynamic biomarkers of the Alzheimer's pathological cascade. Lancet Neurol. 2010;9(1):119-128. doi. 10.1016/S1474-4422(09)70299-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Albert M, Zhu Y, Moghekar A, et al. Predicting progression from normal cognition to mild cognitive impairment for individuals at 5 years. Brain. 2018;141(3):877-887. doi. 10.1093/brain/awx365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goudey B, Fung BJ, Schieber C, Faux NG. A blood-based signature of cerebrospinal fluid Aβ1–42 status. Sci Rep. 2019;9(1):4163. doi. 10.1038/s41598-018-37149-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Doecke JD, Pérez-Grijalba V, Fandos N, et al. Total Aβ42/Aβ40 ratio in plasma predicts amyloid-PET status, independent of clinical AD diagnosis. Neurology. 2020;94(15):e1580-e1591. doi. 10.1212/WNL.0000000000009240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fandos N, Pérez-Grijalba V, Pesini P, et al. Plasma amyloid β 42/40 ratios as biomarkers for amyloid β cerebral deposition in cognitively normal individuals. Alzheimers Dement (Amst). 2017;8:179-187. doi. 10.1016/j.dadm.2017.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schindler SE, Bollinger JG, Ovod V, et al. High-precision plasma β-amyloid 42/40 predicts current and future brain amyloidosis. Neurology. 2019;93(17):e1647-e1659. doi. 10.1212/WNL.0000000000008081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chen GF, Xu TH, Yan Y, et al. Amyloid beta: structure, biology and structure-based therapeutic development. Acta Pharmacol Sin. 2017;38(9):1205-1235. doi: 10.1038/aps.2017.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Graff-Radford NR, Crook JE, Lucas J, et al. Association of low plasma Aβ42/Aβ40 ratios with increased imminent risk for mild cognitive impairment and Alzheimer disease. Arch Neurol. 2007;64(3):354. doi. 10.1001/archneur.64.3.354 [DOI] [PubMed] [Google Scholar]
- 10.Sullivan KJ, Blackshear C, Simino J, et al. Association of midlife plasma amyloid-β levels with cognitive impairment in late life. Neurology. 2021;97(11):e1123-e1131. doi. 10.1212/WNL.0000000000012482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Faught E, Richman J, Martin R, et al. Incidence and prevalence of epilepsy among older U.S. Medicare beneficiaries. Neurology. 2012;78(7):448-453. doi. 10.1212/WNL.0b013e3182477edc [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Born HA. Seizures in Alzheimer's disease. Neuroscience. 2015;286:251-263. doi. 10.1016/j.neuroscience.2014.11.051 [DOI] [PubMed] [Google Scholar]
- 13.Johnson EL, Krauss GL, Kucharska-Newton A, et al. Dementia in late-onset epilepsy. Neurology. 2020;95(24):e3248-e3256. doi. 10.1212/wnl.0000000000011080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Keret O, Hoang TD, Xia F, Rosen HJ, Yaffe K. Association of late-onset unprovoked seizures of unknown etiology with the risk of developing dementia in older veterans. JAMA Neurol. 2020;94158:1-6. doi. 10.1001/jamaneurol.2020.0187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Romoli M, Sen A, Parnetti L, Calabresi P, Costa C. Amyloid-β: a potential link between epilepsy and cognitive decline; Nat Rev Neurol. 2021;17(8):469-485. doi. 10.1038/s41582-021-00505-9. [DOI] [PubMed] [Google Scholar]
- 16.Minkeviciene R, Rheims S, Dobszay MB, et al. Amyloid beta-induced neuronal hyperexcitability triggers progressive epilepsy. J Neurosci. 2009;29(11):3453-3462. doi. 10.1523/JNEUROSCI.5215-08.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Costa C, Romoli M, Liguori C, et al. Alzheimer's disease and late-onset epilepsy of unknown origin: two faces of beta amyloid pathology. Neurobiol Aging. 2019;73:61-67. doi. 10.1016/J.NEUROBIOLAGING.2018.09.006 [DOI] [PubMed] [Google Scholar]
- 18.Fernandes M, Manfredi N, Aluisantonio L, et al. Cognitive functioning, cerebrospinal fluid Alzheimer's disease biomarkers and cerebral glucose metabolism in late-onset epilepsy of unknown aetiology: a prospective study. Eur J Neurosci. 2022;9:1-13. doi. 10.1111/EJN.15734 [DOI] [PubMed] [Google Scholar]
- 19.Cirrito JR, Yamada KA, Finn MB, et al. Synaptic activity regulates interstitial fluid amyloid-beta levels in vivo. Neuron. 2005;48(6):913-922. doi. 10.1016/J.NEURON.2005.10.028 [DOI] [PubMed] [Google Scholar]
- 20.Johnson EL, Krauss GL, Lee AK, et al. Association between midlife risk factors and late-onset epilepsy. JAMA Neurol. 2018;75(11):1375-1382. doi. 10.1001/jamaneurol.2018.1935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Choi H, Pack A, Elkind MSV, Longstreth WT, Ton TGN, Onchiri F. Predictors of incident epilepsy in older adults: the Cardiovascular Health Study. Neurology. 2017;88(9):870-877. doi. 10.1212/WNL.0000000000003662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schneider ALC, Richey Sharrett A, Gottesman RF, et al. Normative data for 8 neuropsychological tests in older blacks and whites from the atherosclerosis risk in communities (ARIC) study. Alzheimer Dis Assoc Disord. 2015;29:32-44. doi. 10.1097/WAD.0000000000000042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Papp AC, Hatzakis H, Bracey A, Wu KK. ARIC hemostasis study–I. Development of a blood collection and processing system suitable for multicenter hemostatic studies. Thromb Haemost. 1989;61(1):15-19. doi. 10.1055/s-0038-1646519 [DOI] [PubMed] [Google Scholar]
- 24.Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496-509. doi. 10.1080/01621459.1999.10474144 [DOI] [Google Scholar]
- 25.Palmqvist S, Janelidze S, Stomrud E, et al. Performance of fully automated plasma assays as screening tests for Alzheimer disease–related β-amyloid status. JAMA Neurol. 2019;76(9):1060-1069. doi. 10.1001/JAMANEUROL.2019.1632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Keret O, Hoang TD, Xia F, Rosen HJ, Yaffe K. Association of new idiopathic seizures with development of dementia in older veterens. Alzheimers Dement. 2019;15(7):P1193. [Google Scholar]
- 27.Stefanidou M, Beiser AS, Himali JJ, et al. Bi-directional association between epilepsy and dementia: the Framingham Heart Study. Neurology. 2020;95(24):e3241-e3247. doi. 10.1212/WNL.0000000000011077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schnier C, Duncan S, Wilkinson T, Mbizvo GK, Chin RFM. A nationwide, retrospective, data-linkage, cohort study of epilepsy and incident dementia. Neurology. 2020;95(12):e1686-e1693. doi. 10.1212/WNL.0000000000010358 [DOI] [PubMed] [Google Scholar]
- 29.Cuevas ME, Haensgen H, Sepúlveda FJ, et al. Soluble Aβ 1-40 peptide increases excitatory neurotransmission and induces epileptiform activity in hippocampal neurons. J Alzheimers Dis. 2011;23(4):673-687. doi. 10.3233/JAD-2011-091717 [DOI] [PubMed] [Google Scholar]
- 30.Gureviciene I, Ishchenko I, Ziyatdinova S, et al. Characterization of epileptic spiking associated with brain amyloidosis in APP/PS1 mice. Front Neurol. 2019;10:1151. doi. 10.3389/fneur.2019.01151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vossel KA, Tartaglia MC, Nygaard HB, Zeman AZ, Miller BL. Epileptic activity in Alzheimer's disease: causes and clinical relevance. Lancet Neurol. 2017;16(4):311-322. doi. 10.1016/S1474-4422(17)30044-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Cheng A, Wang J, Ghena N, et al. SIRT3 haploinsufficiency aggravates loss of GABAergic interneurons and neuronal network hyperexcitability in an Alzheimer's disease model. J Neurosci. 2020;40(3):694-709. doi. 10.1523/JNEUROSCI.1446-19.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yin J, Reiman EM, Beach TG, et al. Effect of ApoE isoforms on mitochondria in Alzheimer disease. Neurology. 2020;94(23):e2404-e2411. doi. 10.1212/WNL.0000000000009582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lee YF, Gerashchenko D, Timofeev I, Bacskai BJ, Kastanenka KV. Slow wave sleep is a promising intervention target for Alzheimer's disease. Front Neurosci. 2020;14:705. doi. 10.3389/FNINS.2020.00705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Zarea A, Charbonnier C, Rovelet-Lecrux A, et al. Seizures in dominantly inherited Alzheimer disease. Neurology. 2016;87(9):912-919. doi. 10.1212/WNL.0000000000003048 [DOI] [PubMed] [Google Scholar]
- 36.Difrancesco JC, Tremolizzo L, Polonia V, et al. Adult-onset epilepsy in presymptomatic Alzheimer's disease: a retrospective study. J Alzheimers Dis. 2017;60(4):1267-1274. doi. 10.3233/JAD-170392 [DOI] [PubMed] [Google Scholar]
- 37.Vossel KA, Beagle AJ, Rabinovici GD, et al. Seizures and epileptiform activity in the early stages of Alzheimer disease. JAMA Neurol. 2013;70(9):1158. doi. 10.1001/jamaneurol.2013.136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Joutsa J, Rinne JO, Hermann B, et al. Association between childhood-onset epilepsy and amyloid burden 5 decades later. JAMA Neurol. 2017;74(5):583. doi. 10.1001/jamaneurol.2016.6091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Moura LMVR, Price M, Cole AJ, Hoch DB, Hsu J. Accuracy of claims-based algorithms for epilepsy research: revealing the unseen performance of claims-based studies. Epilepsia. 2017;58(4):683-691. doi. 10.1111/epi.13691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reid AY, Germaine-Smith StC, Liu M, et al. Development and validation of a case definition for epilepsy for use with administrative health data. Epilepsy Res. 2012;102(3):173-179. doi. 10.1016/J.EPLEPSYRES.2012.05.009 [DOI] [PubMed] [Google Scholar]
- 41.Subota A, Pham T, Jetté N, Sauro K, Lorenzetti D, Holroyd-Leduc J. The association between dementia and epilepsy: a systematic review and meta-analysis. Epilepsia. 2017;58(6):962-972. doi. 10.1111/epi.13744 [DOI] [PubMed] [Google Scholar]
- 42.Janelidze S, Palmqvist S, Leuzy A, et al. Detecting amyloid positivity in early Alzheimer's disease using combinations of plasma Aβ42/Aβ40 and p-tau. Alzheimers Dement. 2022;18(2):283-293. doi. 10.1002/ALZ.12395 [DOI] [PubMed] [Google Scholar]
- 43.Chong JR, Ashton NJ, Karikari TK, et al. Blood-based high sensitivity measurements of beta-amyloid and phosphorylated tau as biomarkers of Alzheimer's disease: a focused review on recent advances. J Neurol Neurosurg Psychiatry. 2021;92:1231-1241. doi. 10.1136/jnnp-2021-327370 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Deidentified ARIC data are available through the NIH Heart, Lung, and Blood Institute–sponsored Biologic Specimen and Data Repository Information Coordinating Center.







