Summary:
As plastic surgery procedures become safer and more popular, the number of patients undergoing cosmetic surgery will rise. A recent trend in plastic surgery has been a rise in combining multiple procedures in a single setting. Such an approach has the advantage of lower surgical cost to the patient and affords the patient a reduced downtime from work. Although the complication profile of patients undergoing plastic surgery is well documented, combining procedures prolongs operation time, which has been associated with a significant increase in the risk of complications. Our case report describes a patient who presented with a wrist drop and paraesthesia in the radial nerve distribution 1 day postoperatively after prolonged combined breast reduction and abdominoplasty procedures. The patient was diagnosed with radial nerve neuropraxia through electromyography. She was reassured, treated by an occupational therapist and showed complete recovery within 3 months. Surgeons offering combined procedures for plastic surgery should be aware of the risk of nerve injury associated with prolonged blood pressure cuff monitoring and take precautionary measures to prevent this risk.
The number of plastic surgery procedures performed has been on the rise in recent years.1 This rise has been primarily linked to the popularity and safety of cosmetic surgery.2 More specifically, a recent trend has seen patients requesting combined procedures in a single surgical setting.3 Combining procedures offers the advantage of decreasing patient downtime, which allows patients to undergo all desired procedures in one session, and leads to significant cost savings for patients.4 However, combining procedures prolongs operative duration, which has been associated with a significant increase in the risk of complications.5 As more patients seek to combine cosmetic procedures for the benefits discussed above, continuous assessment of risks and complications of such procedures, specifically those that have not been previously reported in the literature, will be necessary.
CASE REPORT
A 31-year-old mother of four children presented for a “mommy makeover” surgery comprising a bilateral breast reduction and abdominoplasty. She had a body mass index (BMI) of 34 (weight of 95 kg and height of 1.67 cm), with no medical comorbid conditions. She was a nonsmoker, and previous surgical procedures for childbirth were uneventful.
She worked as a general practitioner and requested a combined procedure to accelerate recovery and reduce downtime from work. She underwent routine inverted-T medial pedicle breast reduction combined with a standard abdominoplasty.
An intravenous line was inserted on her left hand, and the right arm was used for blood pressure (BP) monitoring. A 31–40 cm Dura-Cuf BP cuff (Datex-Ohmeda Critikon blood pressure cuffs) was used, and the circle time was set at 3 minutes on the Datex-Ohmeda Aisys CS5 anesthetic machine. Both limbs were placed on arm boards, and padding was applied to cushion the limbs during the procedure. The procedure lasted 6 hours and 4 minutes, and the intraoperative course was uneventful. Upon waking in the recovery room, the patient reported an inability to feel her right upper limb. Inspection of the arm revealed erythema of the mid-arm in the region where the blood pressure cuff was applied. No signs of swelling or compartment syndrome were observed. Both radial and ulnar artery pulsations were intact, with no signs of vascular compromise to the hand. Due to the patient experiencing postoperative drowsiness, a full examination was deferred until she was fully awake.
Upon review the following morning, the patient complained of paraesthesia of her right arm, approximately 4 cm proximal to the elbow joint, with loss of sensation in the radial nerve distribution and inability to extend the wrist, thumb, and fingers. (See Video [online], which was taken 1 day postoperatively after combined breast reduction and abdominoplasty, demonstrating a drop of the right hand with inability to extend the wrist, the thumb, and all four digits as a result of radial nerve palsy.)
Video 1. was taken 1 post-operative day after combined breast reduction and abdominoplasty demonstrating a drop of the right hand with inability to extend the wrist, the thumb, and all four digits as a result of radial nerve palsy.
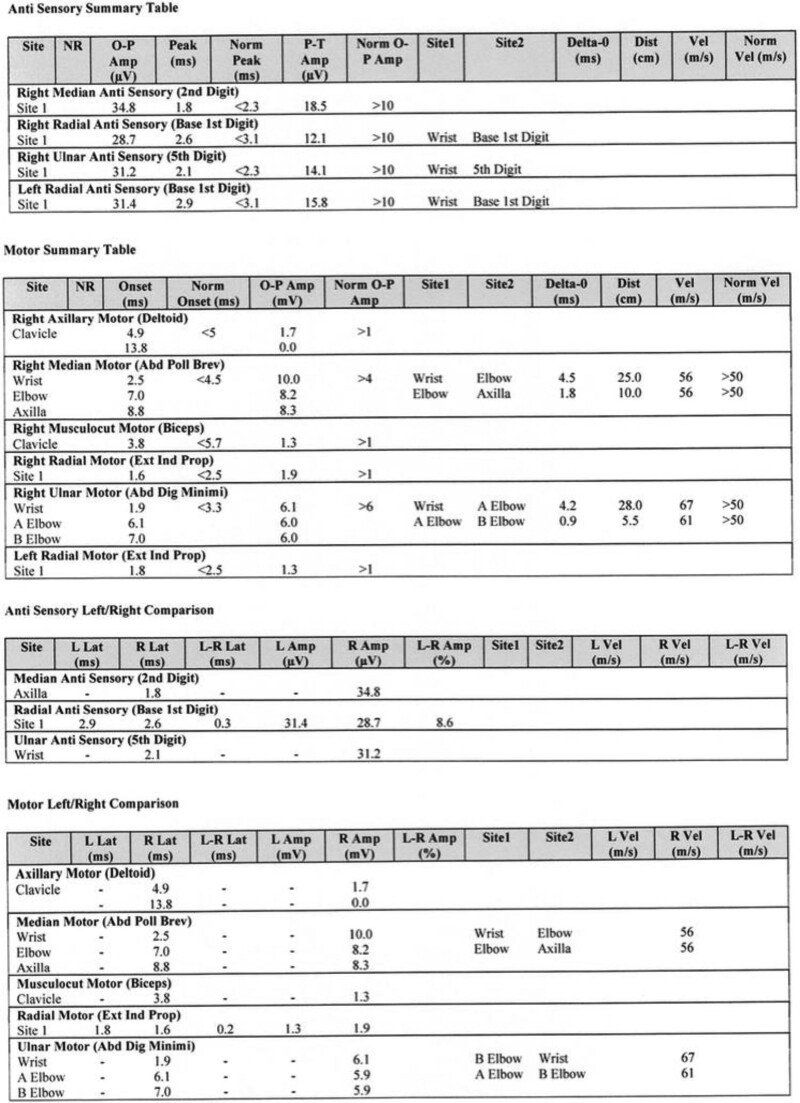
A clinical diagnosis of radial nerve palsy was made, and a neurologist was consulted to perform nerve conduction studies. The results of the nerve conduction and electromyography studies revealed normal latencies, amplitudes, and nerve conduction velocities for all nerves tested (Fig. 1).
Fig. 1.
Nerve conduction studies of the right median and ulnar (motor and sensory), axillary, musculocutaneous, and bilateral radial (motor and sensory) nerves.
The patient was clinically diagnosed with neuropraxia of the right radial nerve and referred to an occupational therapist for further assessment and management. Therapy was initiated before the patient was discharged, and a splint was ordered and applied. The patient was reassured, discharged, and followed up every 2 weeks. She showed remarkable improvement, with full recovery and return to baseline hand function within 3 months.
DISCUSSION
Combining elective breast surgery with abdominoplasty has not been shown to increase the risk of surgical complications compared with single procedures.6 However, the prolonged intraoperative time can predispose patients to nonsurgical complications. We present a case of radial nerve neuropathy induced by blood pressure cuff used for intraoperative monitoring. The risk of this complication can be attributed to the prolonged intraoperative time associated with combined surgical procedures. The patient had a high nerve injury, as evidenced by a wrist drop, indicating the level of the injury to be above the elbow. Clinically, the patient had a blood pressure cuff applied to the right arm with the area of application erythematous upon examination, pointing to the blood pressure cuff as the inciting agent for the injury sustained.
Nerve injuries occurring as a result of blood pressure cuff monitoring are exceedingly rare, but the mechanism could be due to the tourniquet effect, as the blood pressure cuff fills to measure the blood pressure. These injuries have been shown to most commonly affect the ulnar nerve, accounting for 28% of cases, whereas the radial nerve is less frequently affected, accounting for only 3% of reported cases.7 Nerve damage due to tourniquet application has been shown to emerge from either direct nerve compression or ischemia, particularly if it is applied for more than 3 hours.8 Thus, alternating the arm used for monitoring blood pressure and decreasing the circle time for patients undergoing prolonged procedures might help reduce the likelihood of such occurrences. Patient positioning in theater also plays a crucial role in the development of compression injuries. Staging surgical procedures to reduce intraoperative time should also be considered whenever feasible to reduce complications associated with prolonged intraoperative times.
Radial nerve compression injuries often occur when the arm is placed against a rigid surface.9 Adequate padding of all pressure points and regularly checking areas at risk for compression injuries should be carried out during the course of the operation. Obesity has been implicated as one of the risk factors for tourniquet-induced neurological injuries due to loss of some pressure into the subcutaneous tissues during monitoring, thus requiring higher pressures which predisposes these patients to nerve injuries.10 Choosing the correct pressure cuff becomes a crucial consideration when treating patients with a high BMI. Deferring elective surgery in patients presenting with a high BMI undergoing prolonged surgery should also be considered until the patient has lost weight.
Although devastating in nature, the majority of nerve compression injury cases have a satisfactory clinical course with full recovery achieved. In a recent systematic review, 89.7% of patients who presented with similar tourniquet-related nerve injuries experienced full recovery.11 In a case similar to ours reporting a patient who had a radial nerve injury secondary to blood pressure cuff, complete recovery was achieved in 3 months.12 Support and reassurance should be offered to patients presenting with this type of injury, and referral to the occupational therapist should be done early.
CONCLUSIONS
We report a case of radial nerve compressive neuropathy caused by a blood pressure-monitoring cuff in a patient undergoing prolonged elective combined breast reduction and standard abdominoplasty procedures. Compressive neuropathy secondary to the use of a blood pressure-monitoring cuff is rarely encountered in clinical practice. Raising awareness and reporting on this etiology in patients undergoing prolonged cosmetic and plastic surgery procedures will help address factors associated with its development and aid in its prevention.
DISCLOSURE
The author has no financial interest to declare in relation to the content of this article.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.Gelidan AG. Seasonal rise in plastic surgery during Ramadan: a cross-sectional survey. Plast Reconstr Surg Global Open. 2022;10:e4397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rohrich RJ. The increasing popularity of cosmetic surgery procedures: a look at statistics in plastic surgery. Plast Reconstr Surg. 2000;106:1363–1366. [DOI] [PubMed] [Google Scholar]
- 3.Stevens WG, Vath SD, Stoker DA. “Extreme” cosmetic surgery: a retrospective study of morbidity in patients undergoing combined procedures. Aesthetic Surg J. 2004;24:314–318. [DOI] [PubMed] [Google Scholar]
- 4.Pitanguy I, Ceravolo MP. Our experience with combined procedures in aesthetic plastic surgery. Plast Reconstr Surg. 1983;71:56–65. [DOI] [PubMed] [Google Scholar]
- 5.Cheng H, Clymer JW, Chen BP, et al. Prolonged operative duration is associated with complications: a systematic review and meta-analysis. J Surg Res. 2018;229:134–144. [DOI] [PubMed] [Google Scholar]
- 6.Stevens WG, Cohen R, Vath SD, et al. Is it safe to combine abdominoplasty with elective breast surgery? A review of 151 consecutive cases. Plast Reconstr Surg. 2006;118:207–212; discussion 213–214. [DOI] [PubMed] [Google Scholar]
- 7.Lin CC, Jawan B, de Villa MV, et al. Blood pressure cuff compression injury of the radial nerve. J Clin Anesth. 2001;13:306–308. [DOI] [PubMed] [Google Scholar]
- 8.Jolly D, Chrisos H, Kaufman-Goldberg T, et al. Median nerve neuropathy following radial forearm free flap phalloplasty: a case report. Plast Reconstr Surg Global Open. 2020;8:e3027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Winfree CJ, Kline D. Intraoperative positioning nerve injuries. Surg Neurol. 2005;63:5–18. [DOI] [PubMed] [Google Scholar]
- 10.Graham B, Breault MJ, McEwen JA, et al. Perineural pressures under the pneumatic Tourniquet in the upper extremity. J Hand Surg. 1992;17:262–266. [DOI] [PubMed] [Google Scholar]
- 11.Chang J, Bhandari L, Messana J, et al. Management of tourniquet-related nerve injury (TRNI): a systematic review. Cureus. 2022;14:e27685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kim YS, Kwak KH, Hong JG. Radial nerve injury due to automatic blood pressure monitoring: a case report. Korean J Anesthesiol. 2009;57:217–220. [DOI] [PubMed] [Google Scholar]