Abstract
The high prevalence of human immunodeficiency virus (HIV) infections has become a devastating public health problem in Indonesia. In response, the government has taken measures to reduce the transmission of HIV and the number of deaths from HIV/acquired immunodeficiency syndrome (AIDS). However, these efforts have not successfully reduced the spread of HIV in Surabaya. In this study, we analyzed the factors that could influence the spread of HIV in Surabaya using a Geographic Information System. We conducted a spatial analysis of HIV/AIDS clusters in Surabaya from 2016 to 2020. Spatial autocorrelation and spatiotemporal analysis were used to identify local HIV clustering. In addition, the Global Moran's I index was applied to detect HIV clustering at the sub-district level. The results showed that HIV mostly occurred among males (683/969; 70.3%) in the economic age group (20–35 years) and that the infection was transmitted mostly through sexual intercourse (942/969; 97.2%). The hotspots were located in Central and Southern Surabaya, including the Genteng, Tegal Sari, Gubeng, and Sawahan sub-sub-districts. Western Surabaya (Benowo and Pakal) was the only hot spot in 2018. In conclusion, the spatial and temporal analysis of HIV, coupled with an assessment of the factors that drive the epidemic, can assist the government to formulate policies and design targeted interventions to prevent and control the epidemic in Surabaya, Indonesia.
Keywords: HIV, Spatial, Temporal, Transmission, Geographic information system
1. Introduction
Human immunodeficiency virus (HIV) affects the immune system and causes a disease called acquired immunodeficiency syndrome (AIDS). HIV infection is increasing year by year [1]. It is becoming a major public health concern in Indonesia and other countries worldwide. Indonesia is one of the countries in Southeast Asia with the highest number of HIV cases. According to the Joint United Nations Program on HIV/AIDS (UNAIDS), 38.4 million people are estimated to live with an HIV infection. New HIV cases are estimated to range from 1.1 million to 2.0 million in the world [2]. In Indonesia, 540,000 people live with HIV infection. The number of new HIV infections increased from 21,511 in 2012 to 41,250 in 2016. However, the number of new HIV infections has decreased sharply since 2010 to 25,000–28,000 cases by 2021 [3]. The rate of HIV transmission by route of infection varies over time. Currently at 89%, sexual transmission is predominant in Indonesia [4].
Geographic information system (GIS) is useful planning tools for public health interventions. In this field, GIS and spatial analysis are powerful tools for understanding, preventing, and treating diseases. As a visual aid, GIS software can be used to map the geographic distribution of diseases, associated risk factors, and services available for the prevention and treatment of diseases. Furthermore, spatial analysis can help identify the risks associated with diseases, epidemic trends over space and time, and disease hotspots [5,6].
The high transmission rate of HIV is a significant health problem. Monitoring the spread of HIV and identifying high-risk areas can provide useful information for planning targeted and improved health services to reduce the spread and improve control of the HIV epidemic. Moreover, these measures are useful for national health policymakers in developing effective intervention strategies and allocating funds and human resources as needed. Understanding the transmission patterns of HIV cases by geography (spatial) and time (temporal) in our targeted areas can be obtained from data analyzed using GIS technology. However, the information on the epidemiological distribution and spatial trends of HIV/AIDS in Surabaya, Indonesia to date is limited.
Thus, in this study, GIS was used to perform spatial and temporal analyses of HIV/AIDS cases in Surabaya, Indonesia. Based on our analysis, we intend to develop HIV/AIDS preventive strategies that can contribute to policymaking in the future. In addition, this study provides information about the factors predicting the spread of HIV and can contribute to the planning for a reduction in the transmission of HIV infection in Surabaya, Indonesia.
2. Materials and methods
2.1. Study area
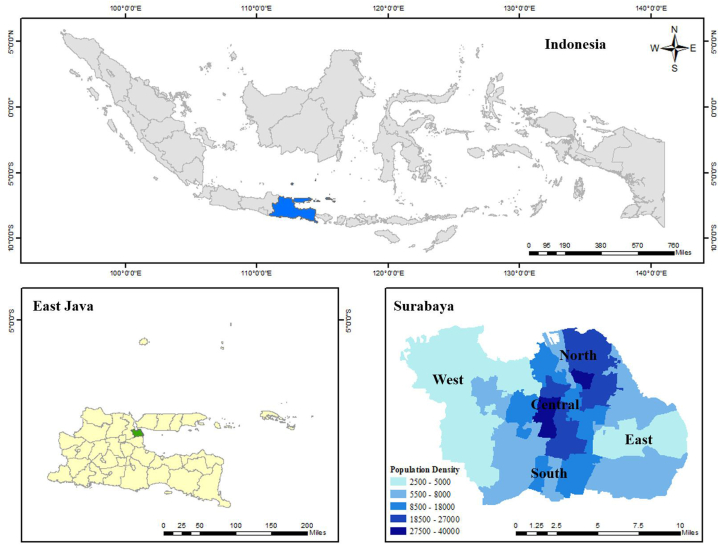
As the largest metropolitan city in Indonesia after Jakarta, Surabaya is the center of economic activities in East Java and its surroundings. Most of the population is engaged in services, industries, and trade, and the city has few green spaces for farming. Many large companies have headquarters in Surabaya [7]. Surabaya had the highest reported number of HIV/AIDS patients, ranking first in East Java. After 2019, approximately 915 people in Surabaya were infected with HIV. Surabaya, has an area of 374.1 km2, a population of approximately 2.87 million and 31 subdistricts with a dense population in the central region. The city lies on the northern and eastern borders of the Madura Strait, while the southern and western borders of this city are Sidoarjo and Gresik, respectively. According to the geographical status quo, Surabaya does not separate its areas, but administratively, it is divided into several sub-districts. This division of the Surabaya area was carried out to manage the administrative regions more easily due to its size, with areas reaching 330 km2. Surabaya area is divided into five regions: Central Surabaya (Bubutan, Genteng, Simokerto, and Tegalsari), Eastern Surabaya (Gubeng, Mulyorejo, Rungkut, Sukolilo, Tambaksari, and Tenggilis Mejoyo), Western Surabaya (Asemrowo, Benowo, Lakarsantri, Pakal, Sambikerep, Sukomanunggal, and Tandes), Northern Surabaya (Bulak, Kenjeran, Krembangan, Pabean Cantian, and Semampir), and Southern Surabaya (Dukuh Pakis, Gayungan, Jambangan, Sawahan, Wiyung, Wonocolo, and Wonokromo). Data on HIV cases per area were obtained (Fig. 1). According to the Indonesian Ministry of Health, East Java is one of the five provinces with the highest number of HIV/AIDS cases between January and March 2021 [8].
Fig. 1.
Location of the study areas in Surabaya, East Java, Indonesia. Map of Indonesia showing Location of East Java which is located in the easternmost of Java Island (A); Surabaya is a city located in East Java Province (B); and population density in each sub-district of Surabaya (C).
2.2. Research participants
Participant health profiles were obtained from the HIV non-governmental organizations in East, West, North, South, and Central Surabaya. Eligible patients were HIV-positive, as determined by three methods: nucleic acid test (NAT), antigen test, and antibody test. Information collected from the organizations included the domicile, sex, age, and route of transmission.
2.3. Data management
All HIV cases collected between 2016 and 2020 were analyzed in this study. To protect patient privacy, all personal information was removed from the database prior to the analysis. All the included cases were geocoded and matched at the district level.
2.4. General spatial autocorrelation
The Global Moran's I index was used to detect HIV clustering at the district level. This is an index that uses values between −1 and 1. The infection distribution was considered to be clustered or to have a positive spatial autocorrelation if Moran's I was more than 0 and the z-value was more than 1.96 at a confidence level of 95%. If Moran's I was less than 0 and the z-value was less than −1.96, the distribution was considered to have a dispersed pattern. In addition, the case distribution was considered random [9,10].
2.5. Local spatial autocorrelation
Previous studies have shown that general spatial autocorrelation can cause changes in the local state. Thus, local spatial autocorrelation was applied to measure the spatial autocorrelation of individual features and to identify spatial patterns across the study area [11,12]. The Getis-Ord Gi* statistic was used to calculate the z-score and p-values. Local clusters with a z-value of more than 1.96 indicate an area as a hot spot since they show high clustering; if the z-value is less than −1.96, the areas are categorized as low clustering (cold spot). ArcGIS 10.3 software (ESRI Inc., Redlands, CA, USA) was used for the spatial analysis and mapping of the case clusters in the examined areas.
2.6. Ethical considerations
In this study, we ensured the confidentiality of the patient data and respected their privacy. We considered the ethical considerations regarding data sharing and access, including the protection of intellectual property rights and ensuring confidentiality.
3. Results
3.1. Demographic characteristics
A total of 869 HIV cases in Surabaya, identified between 2016 and 2020, were anlyzed. The demographic data of the identified cases are presented in Table 1. As shown in Table 1, the data included the number of new HIV cases by year, region, sex, age, and transmission. In total, there were 114 cases in 2016, 212 cases in 2017, 236 cases in 2018, 229 cases in 2019, and 178 in 2020. HIV cases are widely found in the eastern and southern regions of Surabaya. Most cases were from the southern region, with 37.7% in 2016 and 26.4% in 2020. The percentage of new cases in the Eastern region increased from 18.4% in 2016 to 28% in 2020. Many new HIV cases have emerged in these regions, and HIV-infected male patients are more prevalent than HIV-infected female patients. The highest age group infected by HIV was the 20–35 years old group, accounting for 34.8% of male cases and 10.8% of female cases in 2016 and 33.6% of male cases and 11.2% of female cases in 2020. The HIV cases’ mode of transmission during 2016–2020 was dominated by sexual intercourse and the cases were mostly male. However, owing to the limitations of this study, there were no data that explained their sexual behavior orientation (male-to-male or male-to-female).
Table 1.
Demographic characteristics of the HIV-infected individuals in Surabaya, Indonesia.
| New HIV cases (%) |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2016 | 2017 | 2018 | 2019 | 2020 | ||||||
| Total Cases | 114 | 212 | 236 | 229 | 178 | |||||
| Regions | ||||||||||
| West | 16 (14) | 45 (21.2) | 52 (22) | 52 (22.7) | 30 (16.8) | |||||
| East | 21 (18.4) | 45 (21.2) | 68 (28.8) | 61 (26.6) | 50 (28) | |||||
| South | 43 (37.7) | 55 (25.9) | 55 (23.3) | 53 (23.1) | 47 (26.4) | |||||
| Central | 14 (12.2) | 36 (16.9) | 28 (11.8) | 33 (14.4) | 27 (15.1) | |||||
| North | 20 (17.5) | 31 (14.6) | 33 (13.9) | 30 (13.1) | 24 (13.4) | |||||
| Sex | ||||||||||
| Male | 75 (65.7) | 147 (69.3) | 171 (72.4) | 160 (69.8) | 128 (71.9) | |||||
| Female | 39 (34.2) | 65 (30.6) | 65 (27.5) | 69 (30.1) | 50 (28) | |||||
| Age (years) | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female |
| <14 | 1 (0.87) | 2 (1.73) | 1 (0.47) | 2 (0.94) | 0 (0.00) | 1 (0.42) | 1 (0.43) | 2 (0.87) | 0 (0.00) | 1 (0.55) |
| >55 | 5 (4.34) | 3 (2.6) | 6 (2.83) | 3 (1.41) | 14 (5.9) | 4 (1.7) | 7 (3.1) | 0 (0.00) | 3 (1.7) | 2 (1.11) |
| 14–19 | 0 (0.00) | 2 (1.73) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 0 (0.00) | 10 (5.6) | 0 (0.00) |
| 20–35 | 40 (34.8) | 7 (6.1) | 62 (29.2) | 23 (10.8) | 94 (39.8) | 25 (10.6) | 97 (42.4) | 22 (9.6) | 77 (33.6) | 20 (11.2) |
| 36–55 | 30 (26.1) | 25 (21.7) | 78 (36.8) | 37 (17.5) | 63 (26.7) | 35 (14.8) | 55 (24.1) | 45 (19.6) | 39 (21.8) | 27 (15.1) |
| Transmission | Male | Female | Male | Female | Male | Female | Male | Female | Male | Female |
| Sexual intercourses | 73 (64.04) | 35 (30.70) | 143 (67.45) | 62 (29.25) | 170 (72.03) | 64 (27.12) | 155 (67.69) | 65 (28.38) | 126 (70.79) | 49 (27.53) |
| Injected drugs | 1 (0.88) | 0 (0.00) | 3 (1.42) | 1 (0.47) | 1 (0.42) | 0 (0.00) | 4 (1.75) | 1 (0.44) | 2 (1.12) | 0 (0.00) |
| Perinatal | 1 (0.88) | 4 (3.51) | 1 (0.47) | 2 (0.94) | 0 (0.00) | 1 (0.42) | 1 (0.44) | 3 (1.31) | 0 (0.00) | 1 (0.56) |
| Total | 114 (11.7) | 212 (21.8) | 236 (24.3) | 229 (23.6) | 178 (18.3) | |||||
3.2. Spatial clustering analysis
General spatial autocorrelation analysis was used to analyze HIV cases in Surabaya (Table 2). The Global Moran's analysis indicated a direct autocorrelation between HIV cases from 2016 to 2020. All Global Moran's I values were greater than 0 (p < 0.01), indicating significant annual clustering throughout the study area.
Table 2.
General spatial autocorrelation results (by year) of HIV cases in Surabaya.
| Year | Moran's I | z Value | p-values |
|---|---|---|---|
| 2016 | 0.09 | 0.94 | <0.01 |
| 2017 | 0.26 | 2.20 | <0.01 |
| 2018 | 0.05 | 0.64 | <0.01 |
| 2019 | 0.10 | 1.02 | <0.01 |
| 2020 | 0.17 | 1.57 | <0.01 |
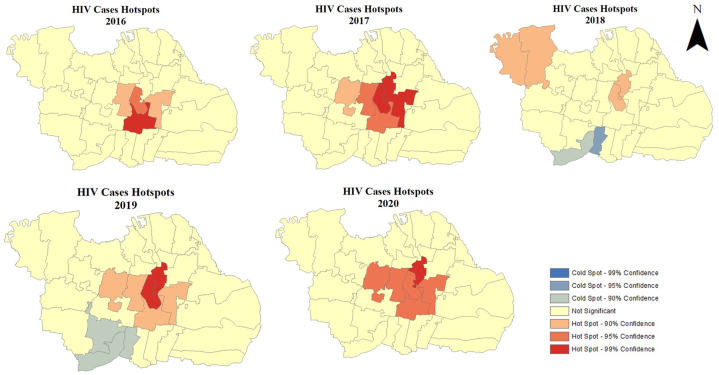
In this study, the spatial autocorrelation analysis showed statistically significant “hot spots'’ and “cold spots” and the results from the steps demonstrated areas with a particular risk or concentrated need and the characteristics of the cases inside and outside of the clusters [5]. As shown in Fig. 2, the annual distribution of hot/cold spots was identified from local spatial autocorrelation, showing that hot spots were mostly found in Central Surabaya, specifically in the Genteng, Tegalsari, and Gubeng sub-districts with a 99% confidence level. However, in 2018, an identified change in a hot spot was found in the Western Surabaya (Pakal and Benowo sub-districts). Cold spots appeared in Southern Surabaya, including the Karang Pilang, Jambangan, and Wiyung subdistricts, in 2018 and 2019. The hotspot analysis revealed consistent patterns in 2016, 2017, 2019, and 2020.
Fig. 2.
Hot and cold spot of HIV cases in Surabaya, Indonesia from 2016 to 2020.
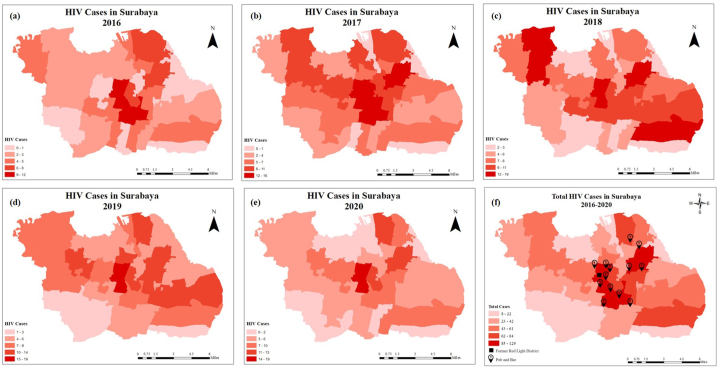
Fig. 3 shows that the geographic distribution of HIV cases can be divided into five classifications: 0–2, 3–6, 7–10, 11–13, and 14–19 years. The number of HIV cases varies according to the geographic location. For example, the highest number of HIV cases was observed in Southern Surabaya, followed by several other subdistricts, including Sawahan, in 2016, 2019, and 2020. In contrast to 2018, a high trend was observed in Eastern, Western, and Southern Surabaya, specifically in Sawahan, Tambaksari, Rungkut, and Benowo. As shown in the figure below, the largest clusters of HIV cases (trends during 2016–2020) were mostly found in Central Surabaya, specifically in the Genteng, Tegalsari, and Gubeng subdistricts.
Fig. 3.
Geographic distribution of HIV cases in Surabaya, Indonesia from 2016 (a) to 2020 (e) and location of former red light district in Surabaya (f).
4. Discussion
Surabaya, the capital city of the East Java Province, Indonesia, has the highest HIV prevalence among all the cities in the country. According to the Indonesian Ministry of Health, more than 300 new HIV cases were likely to be reported in Surabaya in 2021. Using a GIS with insufficient data has made it possible to extrapolate and fill spatial gaps. However, complex spatiotemporal trends in HIV/AIDS prevalence and projections are relatively easy to predict using GIS [13]. Spatial interpolation of the GIS data revealed spatial patterns and growing trends in HIV cases in Surabaya over the past two decades (Fig. 2, Fig. 3). GIS analysis of sentinel surveillance data from antenatal clinics allowed us to analyze HIV/AIDS incidence rates using more sophisticated forecasting software, which will help us model and estimate disease progression in the Surabaya area.
Based on demographic characteristics, Table 1 shows the increase in detected HIV/AIDS cases among age groups with temporally different behaviors. The prevalence of HIV/AIDS was higher in the two age groups of 20–35 years and 36–55 years. Males of 20–35 years of age were most frequently infected. The prevalence of HIV infected cases caused by sexual behavior and injected drugs was higher in the younger age groups rather than in the older age groups. These findings correspond to the research data collected from the US regions where HIV cases transmitted through risky sexual intercourses occurred increasingly in the 35–44 years old group (11%), 25–34 years old group (13%) and 18–24 years old group (18%). Further, injection drug users (people with injecting drugs, PWID) are at risk of acquiring HIV if they use a syringe used previously by someone else. Similarly, individuals aged 30–39 years (40%), 25–29 years (44%), and 18–24 years (48%) were reported to share needles in the US; PWID without HIV in the US who used any injection equipment after someone else were aged 30–39 years (67%), 25–29 years (71%), and 18–24 years (72%) [14].
The largest HIV case clusters were identified in the subdistricts of Central Surabaya, which are HIV hotspots. Since these sub-districts have central business areas, where many office buildings, governmental offices, shopping districts, hangout spots, parks, hotels, pubs, bars, and red light districts are present, the density of populations with HIV is higher in these regions, as is the risk of transmission. In addition, males constitute the majority of the population at risk for HIV infection. According to previous studies, urban gay scenes constructed around bars, clubs, sex venues, and other common locations of queer sociality clearly belong to this category [15]. According to the gay community website in Surabaya (as a reference on GAYa Nusantara), most of their hangout spots were also located in the central region of Surabaya (Pataya, Calfor, Taman Eden, Taman Bungkul, Irian Barat, Kembang Kuning, etc.) [16]. However, as shown in Table 1, there was a high number of new HIV cases in Southern and Eastern Surabaya during the same period. In contrast to the geographical distribution of HIV cases, some areas with a high prevalence of HIV infection were not considered hotspots in the present study. The hotspots in Southern Surabaya were Sawahan and Wonokromo, as they were former areas for red light district. Sawahan was the largest red light district (called “Dolly”) in Southeast Asia, which is the epicenter of HIV cases in Surabaya. However, the mayor of Surabaya closed the red light district in 2014 [[17], [18], [19]]. In line with the demographic characteristics, people practicing sexual intercourse have a higher risk of HIV infection than the perinatal and injection drug routes of transmission [20,21]. The patterns of hotspots across areas gradually became significant and consistent in this analysis.
According to the hotspot analysis, areas with a high number of HIV cases were not considered hotspots if their surrounding areas had a low trend. Thus, the areas were neutral for this reason. Examples of such areas in southern Surabaya were Jambangan, Karangpilang, and Wiyung, which had a low prevalence of HIV despite being located close to a hotspot, Sawahan. Mulyorejo and Gunung Anyar (Eastern Surabaya) were considered neutral areas because they had no HIV cases and were located far from highly infected areas. In contrast, cold spots, such as Karang Pilang, Jambangan, and Wiyung sub-districts, were safe areas because the number of HIV cases in these areas was low. They were also surrounded by another cold spot, Lakarsantri, which exhibited a similar trend.
5. Limitation of this study
This study focused on spatial and temporal analyses of HIV cases across the Surabaya area from 2016 to 2020. In this study, we did not correlate the results with other demographic factors, such as marital status and education. Therefore, the findings of this study must be considered based on these limitations.
6. Conclusion
In this study, we analyzed the spatial and temporal transmission of HIV in Surabaya, Indonesia and identified risk factors for transmission, such as sex and age. The results revealed a correlation between HIV transmission and sexual behavior, as well as with the geographical features. This study found hotspots for HIV transmission in Central and Southern Surabaya, which are surrounded by hangout spots, pubs, bars, and red light districts, with sexual transmission being the most common route. The identified hotspots and risk factors for HIV transmission can be useful for policymaking and HIV program management. Future interventions should focus on high-risk areas or groups. The study also suggested cooperation with the Surabaya Public Health Office in providing regular HIV testing at hotspots, especially at pubs and bars. Continuous monitoring of identified hotspots is required to reduce the number of HIV cases in Surabaya. Overall, this study provides important insights into the transmission of HIV in Surabaya, which can assist in reducing the spread of HIV infection in the region.
Author contribution statement
Siti Qamariyah Khairunisa, Aussie Tahta Maharani: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper. Budi Utomo, Dia Bitari Mei Yuana, Afif Nurul Hidayati: Performed the experiments; Contributed reagents, materials, analysis tools or data. Nasronudin, Ilham Harlan Amarullah: Conceived and designed the experiments; Analyzed and interpreted the data.
Data availability statement
Data included in article/supplementary material/referenced in article.
Declaration of competing interest
The authors declare no conflict of interest.
Acknowledgments
The authors would like to express their appreciation to all the research participants and staff at the Institute of Tropical Disease, Universitas Airlangga. Sincere gratitude is extended to The Indonesian Ministry of Education, Culture, Research, and Technology for facilitating this study.
Contributor Information
Nasronudin, Email: nasronudin@fk.unair.ac.id.
Ilham Harlan Amarullah, Email: amarullah@staf.unair.ac.id.
References
- 1.Who . 2022. HIV/AIDS.https://www.who.int/health-topics/hiv-aids#tab=tab_1 [Google Scholar]
- 2.UNAIDS. Global H.I.V., AIDS statistics . 2021. HIV Were Women and Girls.https://www.unaids.org/en/resources/fact-sheet#:~:text=People%20living%20with%20HIV&text=36.7%20million%20%5B32.3%20million-41.9 [Google Scholar]
- 3.UNAIDS . 2022. HIV and AIDS Estimates Indonesia; p. 2021.https://www.unaids.org/en/regionscountries/countries/indonesia [Google Scholar]
- 4.Kemenkes R.I. Infodatin HIV dan, AIDS (2020), kementeri, kesehat. Republik indones. (2020) Infodatin, HIV.pdf. kemkes.go.id. 2020;1–8 [Google Scholar]
- 5.Boyda D.C., Holzman S.B., Berman A., Grabowski M.K., Chang L.W. Geographic information systems, spatial analysis, and HIV in Africa: a scoping review. PLoS One. 2019;14 doi: 10.1371/JOURNAL.PONE.0216388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Geanuracos C.G., Cunningham S.D., Weiss G., Forte D., Reid L.M.H., Ellen J.M. Use of geographic information systems for planning HIV prevention interventions for high-risk youths. Am. J. Publ. Health. 2007;97:1974–1981. doi: 10.2105/AJPH.2005.076851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Urban Development Center Database, Profile of Surabaya. 2022. http://perkotaan.bpiw.pu.go.id/v2/kota-besar/39#:∼:text=Kota Surabaya adalah ibu kota,sebelah barat laut Denpasar%2C Bali [Google Scholar]
- 8.Kementerian kesehatan republik Indonesia, laporan perkembangan HIV AIDS & penyakit lnfeksi menular seksual (PIMS) triwulan I tahun 2021. Kementeri. Kesehat. Republik Indones. 2021;4247608:613–614. https://siha.kemkes.go.id/portal/perkembangan-kasus-hiv-aids_pims# (2021) 4247608. [Google Scholar]
- 9.Moran P.A.P. Notes on continuous stochastic phenomena. Biometrika. 1950;37:17–23. doi: 10.2307/2332142. [DOI] [PubMed] [Google Scholar]
- 10.Tobler W.R. A computer movie simulating urban growth in the Detroit region. Econ. Geogr. 1970;46:234–240. doi: 10.2307/143141. [DOI] [Google Scholar]
- 11.Getis A., Ord J.K. The analysis of spatial association by use of distance statistics. Geogr. Anal. 1992;24:189–206. doi: 10.1111/j.1538-4632.1992.tb00261.x. [DOI] [Google Scholar]
- 12.Ord J.K., Getis A. Local spatial autocorrelation statistics: distributional issues and an application. Geogr. Anal. 1995;27:286–306. doi: 10.1111/j.1538-4632.1995.tb00912.x. [DOI] [Google Scholar]
- 13.Kalipeni E., Zulu L. Using GIS to model and forecast HIV/AIDS rates in africa, 1986–2010. Prof. Geogr. 2008;60:33–53. doi: 10.1080/00330120701724061. [DOI] [Google Scholar]
- 14.Centers for Disease Control and Prevention (Cdc) Estimated HIV incidence and prevalence in the United States, 2010–2015. HIV surveill. suppl. Rep. 2018;23 http://www.cdc.gov/hiv/library/reports/hiv-2018 [Google Scholar]
- 15.Payne R. Queer Sp. Centres Peripher; 2007. Gay Scene, Queer Grid; p. 1.http://www.dab.uts.edu.au/conferences/queer_space/proceedings/online_payne.pdf 6. [Google Scholar]
- 16.Nusantara Gaya. 2023. Encourage People to Be Proud of Their Sexuality.https://gayanusantara.or.id/info-lgbtiq/tempat-ngeber/surabaya/ [Google Scholar]
- 17.B.N Indonesia. Dolly-Jarak localization is officially closed. 2014 https://www.bbc.com/indonesia/berita_indonesia/2014/06/140618_dolly_jarak_tutup [Google Scholar]
- 18.Lau K.A., Wang B., Saksena N.K. Emerging trends of HIV epidemiology in Asia. AIDS Rev. 2007;9:218–229. https://pubmed.ncbi.nlm.nih.gov/18219365/ [PubMed] [Google Scholar]
- 19.Kotaki T., Khairunisa S.Q., Sukartiningrum S.D., Arfijanto M.V., Utsumi T., Normalina I., Handajani R., Widiyanti P., Rusli M., Rahayu R.P., Lusida M.I., Hayashi Y., Nasronudin N., Kameoka M. High prevalence of HIV-1 CRF01-AE viruses among female commercial sex workers residing in Surabaya, Indonesia. PLoS One. 2013;8 doi: 10.1371/journal.pone.0082645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nasronudin N. HIV/AIDS prevalence in Surabaya, Indonesia. Folia Med. Indones. 2003;44:2008. [Google Scholar]
- 21.Pisani E., Dadun D., Sucahya P.K., Kamil O., Jazan S. Sexual behavior among injection drug users in 3 Indonesian cities carries a high potential for HIV spread to noninjectors. J. Acquir. Immune Defic. Syndr. 2003;34:403–406. doi: 10.1097/00126334-200312010-00007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data included in article/supplementary material/referenced in article.