Abstract
Idiopathic intracranial hypertension (IIH) is characterized by raised intracranial pressure with unknown etiology. The most common neurological manifestations are headache and visual loss. Often, other cranial nerve impairments are also found, most commonly in the VI nerve. Trigeminal neuralgia (TN) is a debilitating condition that is most frequently caused by neurovascular pathology, but TN secondary to IIH is a rare and poorly described topic. Possible explanations of TN in these patients include the distortion of the local anatomy at CN entry zones and fluid displacement causing distortion of the Meckel's cave. In the case below we describe the clinical course of an obese female patient with TN-like pain who underwent a ventriculoperitoneal shunt to treat IIH and experienced complete resolution of both conditions.
Keywords: Idiopathic intracranial hypertension, Trigeminal neuralgia, Ventriculoperitoneal shunt, Meckel's cave
1. Introduction
Trigeminal neuralgia (TN) is a debilitating condition characterized by recurrent painful facial paroxysms [1]. The most common etiology is a compression of the trigeminal nerve root within millimeters of its entry zone into the pons. Approximately 80% of these types of TN cases are caused by compression of an adjacent artery or a vein (most commonly the superior cerebellar artery) [2]. Other conditions that can cause TN include space-occupying lesions such as skull base meningiomas, schwannomas, epidermoid cysts, persistent trigeminal artery, and aneurysms [2]. Multiple sclerosis (MS) is also an established etiology of secondary TN. Patients with MS have a 20-fold increased risk of TN. Aside from a younger age of onset, the clinical features of TN in MS are usually the same as the classical form [[3], [4], [5]].
Idiopathic intracranial hypertension (IIH), formerly known as pseudotumor cerebri is a disease characterized by raised intracranial pressure without a known etiology [6]. Whereas abducens nerve palsies are well recognized in association with isolated IIH (9%–36% of cases), involvement of other cranial nerves has been infrequently described [7]. However, there have been isolated case reports of other cranial nerve impairments in IIH [8]. To our knowledge there are only a few case reports of trigeminal neuralgia associated with IIH [7,9]. In this case report we describe a patient with IIH and classic TN whose symptoms completely resolved after ventriculoperitoneal shunt (VPS) placement.
2. Case description
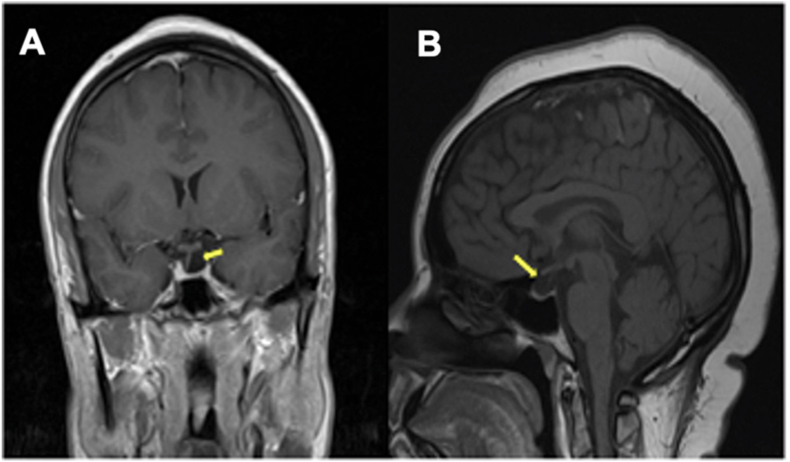
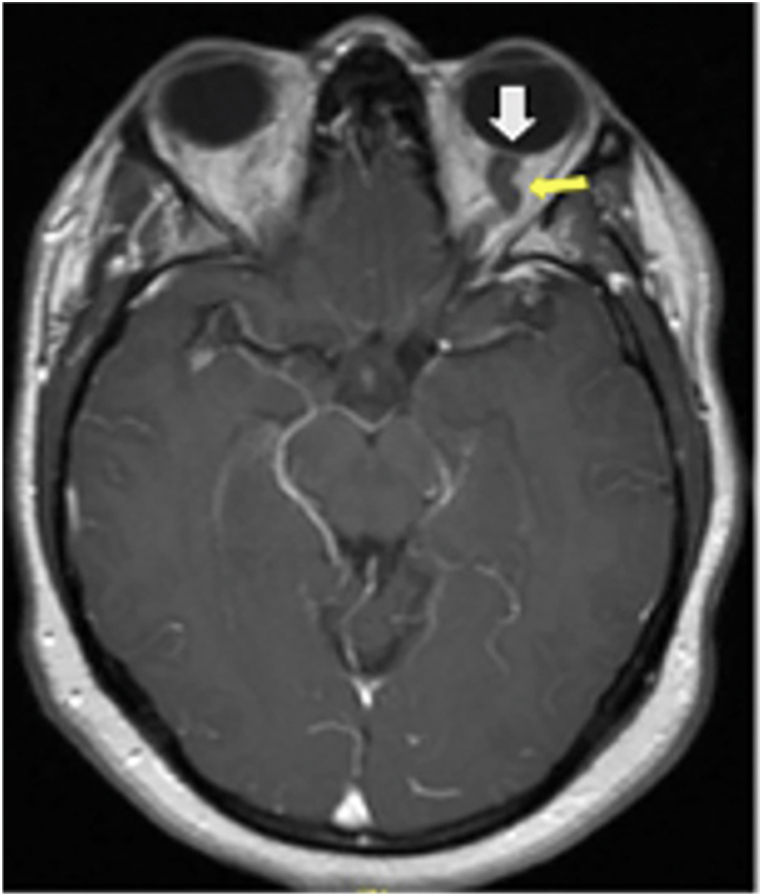
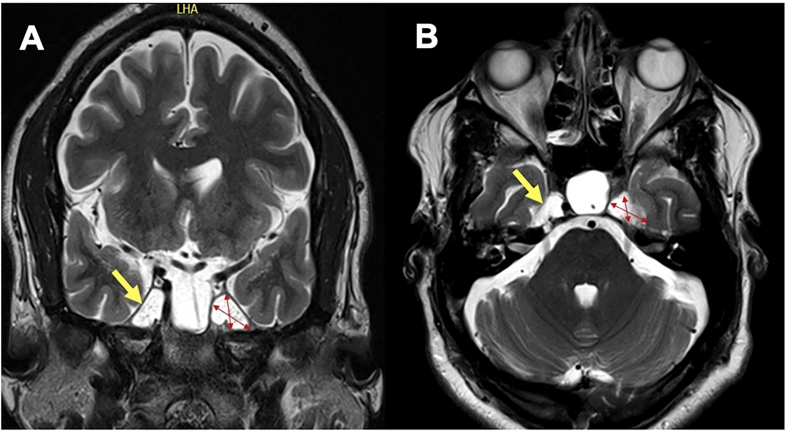
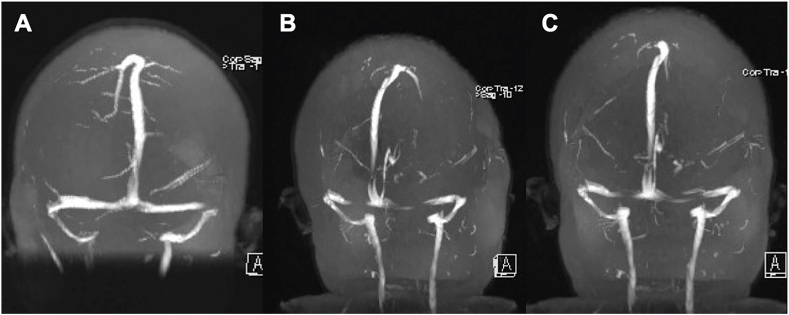
A 34-year-old female patient presented with typical TN right-sided facial pain that had started 7 years prior to her first visit to the author's clinic. The patient described the pain as recurrent and electric shock-like in the V2/V3 distribution, lasting for a few seconds, with increasing severity elicited by brushing teeth, chewing, or talking. In addition to facial pain, the patient complained of intermittent episodes of diplopia, blurred vision, and throbbing headaches. The patient also reported a 30-pound weight gain (BMI = 37.76 Kg/m2) within the previous month associated with a worsening of symptoms. On neurologic examination, the patient was found to have papilledema, full visual fields bilaterally, and intact extraocular movements. Lumbar puncture (LP) demonstrated an opening pressure of 42 cm H2O. A T1-weighted MRI of the brain demonstrated optic nerve tortuosity, flattening of the optic disc, and a partially empty sella (Fig. 1, Fig. 2). T2-weighted images showed a Meckel's cave diameter of 16.6mm × 9.6mm (Fig. 3). No occupying-space lesions were reported. An axial T2-weighted CISS sequence was also assessed to exclude any neurovascular compression. The 3D-TOF-MRA demonstrated apparent bilateral stenosis of the transverse sinus (Fig. 4). The patient was subsequently diagnosed with IIH. Initial treatment with acetazolamide failed to improve her visual deficits. The patient underwent a ventriculoperitoneal shunt procedure for treatment of the IIH and remained on carbamazepine 1200mg daily for trigeminal pain following the procedure. Two weeks after the surgery, at the first postoperative visit, she reported an improvement in visual symptoms and significant relief of her facial pain. Carbamazepine was progressively tapered off, on her 1 month, 3 month, and 6 month follow-up visits. The patient remains medication free one year after her VP shunt placement.
Fig. 1.
A: Coronal T1-weighted non-enhanced MRI demonstrating a displaced pituitary stalk and partially empty sella. B: Sagittal T1-weighted non-enhanced MRI demonstrating a partially empty sella (yellow arrow).
Fig. 2.
Axial T1-weighted post-GD demonstrating a flattening of the optic disc (white arrow) and a tortuosity of the optic nerve (yellow arrow).
Fig. 3.
A: Coronal T2-weighted MRI demonstrating a symmetrically dilated Meckel cave (yellow arrow). B: Axial T2-weighted MRI showing a mean Meckel's cave diameter of 16.6mm × 9.6mm (two-headed red arrows).
Fig. 4.
A 3D-TOF-MRA demonstrating bilateral stenosis of the transverse sinus.
3. Discussion
The exact etiology of IIH is unknown, and many hypotheses suggest that the etiology stems from retinoids, corticosteroid hormones, increased body mass index, and inflammatory markers [10]. While the exact cause remains elusive, these are strong risk factors associated with IIH. Compromised cerebral venous outflow caused by bilateral transverse dural venous sinus stenosis and a high venous pressure gradient have also been implicated in IIH pathophysiology. Weight loss is a commonly employed non-pharmacologic treatment strategy for reducing intracranial pressure in IIH patients. Medications that reduce CSF production such as acetazolamide are also used. In cases where more conservative measures fail, transverse sinus stenting and ventriculoperitoneal shunt placement can be used with high success rates [[11], [12], [13], [14]]. Visual loss in IIH is thought to be due to increased CSF pressure on the optic nerve in the dura sheath, causing papilledema and compressing neurovascular structures [15,16]. Cranial nerve palsies are also described in the literature, most frequently in the sixth nerve [17,18].
The most common etiology of TN is vascular compression of the trigeminal nerve root, in up 75% of cases caused by the superior cerebellar artery [2]. Carbamazepine is the first line of therapy for typical TN [19]. Patients who do not tolerate pharmacological treatment can be considered for surgery. The current gold standard is microvascular decompression (MVD) which has high success rates and lower chance of recurrence [[20], [21], [22]]. In addition to MVD, other options include gamma knife radiosurgery, glycerol rhizotomy, radiofrequency thermoablation, and percutaneous balloon compression [[23], [24], [25], [26]]. However, the association of trigeminal neuralgia and IIH may prompt a different therapeutic approach.
Davenport et al. described a case of TN in a patient with IIH who improved after repetitive lumbar punctures and concluded that increased intracranial pressure could displace CSF through the basal subarachnoid cisterns, leading to displacement and/or compression of cranial nerves (CN). Compression from this proposed mechanism could cause traction on the CN V nerve root [7]. Caudal displacement of the brainstem from elevated intracranial pressure can also lead to traction on CNs and cause impairment, leading to trigeminal neuralgia like symptoms and extrinsic ocular motility deficits [7]. In a case reported by Arsava et al. a patient presented with facial pain and visual disturbance and was diagnosed with TN and IIH. The patient saw some improvement in facial pain with the initial CSF tap and underwent lumboperitoneal shunt (LPS) placement. However, the patient did not show any additional improvements in facial pain post-LPS. The authors concluded that long-term and untreated TN caused a degree of permanent nerve damage that was unable to be relieved by a reduction in intracranial pressure [27]. In addition to considering other etiologies of IIH and the possible pressure-related manifestation of TN, early diagnosis and treatment are imperative to avoid permanent refractory nerve damage.
After the placement of a VPS, the patient's TN pain resolved completely. It is likely that her facial pain originated from compression of the CN V entry root zone or at the level of Meckel's cave (MC). The distortion of the local anatomy of the trigeminal nerve can be supported by image findings such as dilatation of MC (Fig. 3). In a retrospective case-control study, Maradesh et al. described a cut-off value of 4.5 mm for the diameter of MC in association with IIH [28,29]. This morphological variation of MC can reflect the accumulation of CSF under high pressure leading to cranial nerve dysfunction.
4. Conclusion
This case report describes a possible association between IIH and TN. The physiopathology of TN manifestation in these patients may involve pressure and damage to CN V from increased ICP. Early detection, diagnosis, and treatment of increased ICP might improve TN symptoms, and prevent further neurologic deterioration.
Author contribution statement
All authors listed have significantly contributed to the investigation, development and writing of this article.
Funding statement
This study received no specific funding or grant.
Data availability statement
The data that has been used is confidential.
Consent form
Informed consent was obtained from the patient. All the authors have approved the manuscript and agree with the submission. There are no conflicts of interest or financial disclosures to declare.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.heliyon.2023.e19756.
Appendix A. Supplementary data
The following is the Supplementary data to this article.
References
- 1.Alobaid A., et al. Rare cause of trigeminal neuralgia: meckel's cave meningocele. Acta Neurochir. 2015;157(7):1183–1186. doi: 10.1007/s00701-015-2434-4. [DOI] [PubMed] [Google Scholar]
- 2.Bašić Kes V., Zadro Matovina L. Accommodation to diagnosis of trigeminal neuralgia. Acta Clin. Croat. 2017;56(1):157–161. doi: 10.20471/acc.2017.56.01.21. [DOI] [PubMed] [Google Scholar]
- 3.Togha M., et al. Prevalence of new-onset migraine in patients with idiopathic intracranial hypertension in comparison to the general population. Iran J Neurol. 2018;17(4):161–166. [PMC free article] [PubMed] [Google Scholar]
- 4.Hoffmann J., et al. European headache federation guideline on idiopathic intracranial hypertension. J. Headache Pain. 2018;19(1):93. doi: 10.1186/s10194-018-0919-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.De Simone R., et al. A clinical comparison of trigeminal neuralgic pain in patients with and without underlying multiple sclerosis. Neurol. Sci. 2005;26(Suppl 2):s150–s151. doi: 10.1007/s10072-005-0431-8. [DOI] [PubMed] [Google Scholar]
- 6.Algahtani H.A., et al. Idiopathic intracranial hypertension. Atypical presentation. Saudi Med. J. 2007;28(5):762–765. [PubMed] [Google Scholar]
- 7.Davenport R.J., Will R.G., Galloway P.J. Isolated intracranial hypertension presenting with trigeminal neuropathy. J. Neurol. Neurosurg. Psychiatry. 1994;57(3):381. doi: 10.1136/jnnp.57.3.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Samara A., et al. Idiopathic intracranial hypertension presenting with isolated unilateral facial nerve palsy: a case report. J. Med. Case Rep. 2019;13(1):94. doi: 10.1186/s13256-019-2060-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panda A., et al. Trigeminal neuralgia due to meckel's cave crowding in the setting of possible idiopathic intracranial hypertension without papilledema. Ann. Indian Acad. Neurol. 2021;24(1):107–109. doi: 10.4103/aian.AIAN_690_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Toscano S., et al. An update on idiopathic intracranial hypertension in adults: a look at pathophysiology, diagnostic approach and management. J. Neurol. 2021;268(9):3249–3268. doi: 10.1007/s00415-020-09943-9. [DOI] [PubMed] [Google Scholar]
- 11.Gordon W., Abraham M. Contralateral approach to transverse-sigmoid sinus stenting. Intervent Neuroradiol. 2020;26(5):658–663. doi: 10.1177/1591019920954940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Larson A., et al. Reductions in bilateral transverse sinus pressure gradients with unilateral transverse venous sinus stenting for idiopathic intracranial hypertension. J. Neurointerventional Surg. 2021;13(2):187–190. doi: 10.1136/neurintsurg-2020-016170. [DOI] [PubMed] [Google Scholar]
- 13.Abubaker K., et al. Idiopathic intracranial hypertension: lumboperitoneal shunts versus ventriculoperitoneal shunts--case series and literature review. Br. J. Neurosurg. 2011;25(1):94–99. doi: 10.3109/02688697.2010.544781. [DOI] [PubMed] [Google Scholar]
- 14.Bynke G., et al. Ventriculoperitoneal shunting for idiopathic intracranial hypertension. Neurology. 2004;63(7):1314–1316. doi: 10.1212/01.wnl.0000140699.43019.48. [DOI] [PubMed] [Google Scholar]
- 15.McGeeney B.E., Friedman D.I. Pseudotumor cerebri pathophysiology. Headache. 2014;54(3):445–458. doi: 10.1111/head.12291. [DOI] [PubMed] [Google Scholar]
- 16.Schirmer C.M., Hedges T.R., 3rd Mechanisms of visual loss in papilledema. Neurosurg. Focus. 2007;23(5):E5. doi: 10.3171/FOC-07/11/E5. [DOI] [PubMed] [Google Scholar]
- 17.Patton N., Beatty S., Lloyd I.C. Bilateral sixth and fourth cranial nerve palsies in idiopathic intracranial hypertension. J. R. Soc. Med. 2000;93(2):80–81. doi: 10.1177/014107680009300210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ding D., et al. Rapid recovery of bilateral abducens nerve palsies after venous sinus stenting for idiopathic intracranial hypertension. J. Neurol. Sci. 2015;357(1–2):335–337. doi: 10.1016/j.jns.2015.07.047. [DOI] [PubMed] [Google Scholar]
- 19.Bendtsen L., et al. European Academy of Neurology guideline on trigeminal neuralgia. Eur. J. Neurol. 2019;26(6):831–849. doi: 10.1111/ene.13950. [DOI] [PubMed] [Google Scholar]
- 20.Xia L., et al. Effectiveness and safety of microvascular decompression surgery for treatment of trigeminal neuralgia: a systematic review. J. Craniofac. Surg. 2014;25(4):1413–1417. doi: 10.1097/SCS.0000000000000984. [DOI] [PubMed] [Google Scholar]
- 21.Paulo D.L., et al. Microvascular decompression for trigeminal neuralgia in patients with multiple sclerosis: predictors of treatment success. World Neurosurg. 2020;136:e165–e170. doi: 10.1016/j.wneu.2019.12.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Liu J., et al. Long-term retrospective analysis of microvascular decompression in patients with recurrent trigeminal neuralgia. Front. Neurol. 2020;11 doi: 10.3389/fneur.2020.584224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gambeta E., Chichorro J.G., Zamponi G.W. Trigeminal neuralgia: an overview from pathophysiology to pharmacological treatments. Mol. Pain. 2020;16 doi: 10.1177/1744806920901890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Obermann M. Recent advances in understanding/managing trigeminal neuralgia. F1000Res. 2019;8 doi: 10.12688/f1000research.16092.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Obermann M. Treatment options in trigeminal neuralgia. Ther Adv Neurol Disord. 2010;3(2):107–115. doi: 10.1177/1756285609359317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bick S.K.B., Eskandar E.N. Surgical treatment of trigeminal neuralgia. Neurosurg. Clin. 2017;28(3):429–438. doi: 10.1016/j.nec.2017.02.009. [DOI] [PubMed] [Google Scholar]
- 27.Arsava E.M., et al. Electrophysiological evidence of trigeminal neuropathy in pseudotumor cerebri. J. Neurol. 2002;249(11):1601–1602. doi: 10.1007/s00415-002-0866-2. [DOI] [PubMed] [Google Scholar]
- 28.Kamali A., et al. Indentation and transverse diameter of the Meckel cave: imaging markers to diagnose idiopathic intracranial hypertension. AJNR Am J Neuroradiol. 2020;41(8):1487–1494. doi: 10.3174/ajnr.A6682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Marashdeh W.M., Al Qaralleh M.A., Hdeeb A.H. Quantitative parameters for diagnosis of idiopathic intracranial hypertension on brain MRI. Eur J Radiol Open. 2021;8 doi: 10.1016/j.ejro.2021.100371. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that has been used is confidential.