Abstract
Rationale
The coronavirus disease (COVID-19) pandemic exacerbated psychological distress and burnout in frontline healthcare workers. Interventions addressing psychological distress and burnout among these workers are lacking.
Objectives
To determine the feasibility and explore the impact of mobile mindfulness to treat psychological distress and burnout among nurses in frontline COVID-19 units.
Methods
We conducted a pilot randomized trial of 102 nurses working in COVID-19 units at a single hospital between May 2021 and January 2022. Participants were randomized to mobile mindfulness (intervention) or waiting list (control). The primary outcome was feasibility, assessed by comparing rates of randomization, retention, and intervention completion to predefined targets. Secondary outcomes were changes in psychological distress (Patient Health Questionnaire-9, General Anxiety Disorder-7, Perceived Stress Scale-4) and burnout symptoms (Maslach Burnout Inventory) after 1 month.
Results
We randomized 102 of 113 consented individuals (90%, target 80%), and 88 completed follow-up (86%, target 80%). Among 69 intervention participants, 19 completed ⩾1 mindfulness session per week (28%, target 60%), and 13 completed ⩾75% of mindfulness sessions (19%, target 50%). Intervention participants had greater decreases in Patient Health Questionnaire-9 scores than control subjects (difference in differences, −2.21; 95% confidence interval, −3.99, −0.42; P = 0.016), but the Maslach Burnout Inventory depersonalization scores decreased more in the control arm than in the intervention arm (difference in differences, 1.60; 95% confidence interval, 0.18, 3.02; P = 0.027). There were no other changes in emotional distress or burnout symptoms.
Conclusions
This trial of mobile mindfulness in frontline nurses met feasibility targets for randomization and retention, but participants had modest intervention use. Intervention participants had a reduction in depression symptoms, but not in burnout.
Clinical trial registered with www.clinicaltrials.gov (NCT04816708).
Keywords: nursing, burnout, emotional distress, COVID-19
Psychological distress and burnout symptoms are common among nurses (1–3). Before the beginning of the coronavirus disease (COVID-19) pandemic, observational studies estimated the rate of burnout in nurses to be as high as 50%, and nurses reported insomnia, depressive symptoms, and anxiety at significantly higher rates than the general public (4–8). During the COVID-19 pandemic, emotional distress and burnout in nurses have worsened dramatically worldwide, with those nurses caring directly for patients with COVID-19 reporting the highest rates of anxiety, depression, and burnout (9–14). However, proven treatments to mitigate psychological distress and burnout in nurses are lacking.
Mindfulness is a type of mind-body therapy that promotes a practice of nonjudgmental awareness that can alleviate psychological distress by uncoupling emotional reactions and habitual behavior from unpleasant symptoms, thoughts, and emotions (15). Mindfulness has been shown to reduce anxiety and depression symptoms and improve well-being in several different populations and healthcare settings (16, 17). Among nurses, there is also evidence that mindfulness training programs may mitigate burnout symptoms (18, 19). Traditional mindfulness training often relies on in-person, group-based delivery involving multiple hours per week of instruction and home practice. Because healthcare workers account for millions of persons in the United States alone, a more easily accessible alternative approach to delivering mindfulness therapy could be beneficial.
Lift is a monthlong mindfulness program that has been shown to decrease symptoms of psychological distress and improve quality of life among intensive care unit (ICU) survivors (20). As a self-directed program delivered via mobile app, Lift is able to quickly and inexpensively deliver mindfulness therapy to a large number of people at risk for psychological distress and burnout. However, the feasibility and clinical impact of using mobile mindfulness among busy and highly stressed frontline healthcare workers has not been evaluated. Therefore, we conducted a pilot randomized controlled trial whose primary purpose was to assess the feasibility of using the Lift mobile mindfulness program in nurses providing direct care to patients with COVID-19. A secondary goal was to assess the intervention’s clinical impact on psychological distress and burnout symptoms. Portions of this work addressing changes in Patient Health Questionnaire 9-item scale (PHQ-9), Generalized Anxiety Disorder 7-item scale (GAD-7), and Maslach Burnout Inventory (MBI) scores were presented on May 15, 2022, at the American Thoracic Society International Conference (21).
Methods
Study Design, Setting, and Participants
We conducted a pilot randomized waiting list controlled trial between May 2021 and January 2022 in which any nurse who worked in one of four designated COVID-19 units at Duke University Hospital, including a medical/surgical stepdown unit, two ICUs, and the emergency department, was eligible for participation. Exclusion criteria included unreliable access to either a smartphone or a computer with Internet connection, plans to leave current employment within the next 30 days, or active suicidal ideation. Full inclusion and exclusion criteria can be found in the study protocol included in Appendix E1 in the data supplement. The study was approved by the Duke Health Institutional Review Board (protocol 00107657) and was registered at www.clinicaltrials.gov (NCT04816708) before participant recruitment.
Enrollment, Randomization, and Data Collection
Potentially eligible participants were provided with a hyperlink via e-mail and/or given a QR code via flyer to download the generic (i.e., no specific content activated) mobile app platform if they were interested in enrollment. A short informational video on the study website (lift.duke.edu/nurse) was also used to assist potential participants. After downloading the app, all participants used it first to provide electronic informed consent and then to complete a baseline questionnaire that confirmed self-reported eligibility, and collected baseline demographic information, psychological distress symptoms, and burnout symptoms. After providing consent and completing the baseline questionnaire, participants were immediately randomized in a two-to-one allocation ratio either to access the Lift intervention or to the waiting list control group. Randomization was stratified by baseline PHQ-9 score (⩾10 representing moderate symptoms of depression vs. <10) and years of experience as a nurse (>5 yr vs. ⩽5 yr) using a within-app dynamic allocation minimization method (22). Randomization to the Lift intervention arm triggered the mobile app platform to display all Lift content for the participant. At 1 month postenrollment, all participants were prompted via the app to complete a final follow-up questionnaire within the app platform that included the same surveys of emotional distress and burnout completed at baseline. Participants randomized to the waiting list were given access to Lift content 1 month after completion of the study period.
Mobile Mindfulness Intervention and Safety Monitoring
The Lift intervention has previously been described (20). Briefly, Lift is a 4-week self-directed mindfulness program that provides unique daily audio and video mindfulness content, as well as tips for integrating mindfulness into a participant’s daily life, within four different weekly themes. Daily reminders from the app prompted participants in the intervention arm to complete their mindfulness sessions and surveys when appropriate. Symptoms of worsening psychological distress were monitored via weekly completion of the PHQ-9 survey within the app. Additional content was automatically displayed for participants whose PHQ-9 score was either very high (⩾20) or had increased in comparison with the previous week’s score. Any participant reporting suicidal ideation at any time during the trial triggered a real-time e-mail alert that notified study staff. In the event of an alert, the participant was contacted immediately by study staff via telephone to ensure their safety and connect them with additional mental health services. Any self-report of suicidal ideation also prompted the app to provide the participant with the telephone number for mental health crisis services.
Outcomes
The primary outcome was the feasibility of using a self-directed app-based platform to address distress symptoms among nurses working in COVID-19 units. Feasibility was assessed by comparison of observed frequencies with a priori specified targets of randomization of consented participants (80%); retention as measured by completion of the postintervention survey (80%); and among participants in the intervention arm, completion of at least one mindfulness audio or video session all 4 weeks of the study period (60%) as well as completion of ⩾75% of all daily mindfulness interventions (50%).
Secondary outcomes were differences in psychological distress and burnout symptom survey scores at 1 month after enrollment and baseline. We assessed depression symptoms via the PHQ-9, a 9-item scale (score range 0 [no distress] to 27 [high distress]) (23), anxiety symptoms with the GAD-7 (range 0 [no distress] to 21 [high distress]) (24), and general stress symptoms with the Perceived Stress Score 4-item scale (PSS-4; range, 0 [no stress] to 16 [high stress]) (25). Burnout symptoms were measured using the MBI, which is generally scored across three domains: Emotional Exhaustion (9 items; range, 0 [no emotional exhaustion] to 54 [high emotional exhaustion]), Personal Accomplishment (8 items; range, 0 [low personal accomplishment] to 48 [high personal accomplishment]), and Depersonalization (5 items; range, 0 [low depersonalization] to 30 [high depersonalization]) (26). Surveys were self-completed by all participants within the app platform. Due to an app programming error, all participants were missing GAD-7 item 3 and MBI Personal Accomplishment item 5. These values were imputed for each individual using each scale’s other items.
Additional outcomes included the frequency of each participant’s app use, intervention completion, and survey completion, which were assessed using standard analytic metrics derived from interrogation of the app platform. We also collected open-ended text feedback on user experience from intervention participants after completion of the study period.
Sample Size
No power calculation was performed for this pilot study. A 100-person sample size was chosen to reflect the pragmatics of recruitment during a short enrollment period while also being large enough to inform the feasibility of a future randomized controlled trial and provide preliminary evidence of the clinical impact of the Lift mobile mindfulness program.
Statistical Methods
Patient characteristics were summarized overall and by arm as median and interquartile range or as count and percent. To assess feasibility, the frequency of app use, intervention completion, and survey completion were calculated using standard analytic metrics derived from interrogation of the app platform. Each survey outcome (PHQ-9, GAD-7, PSS-4, MBI Emotional Exhaustion domain, MBI Personal Accomplishment domain, and MBI Depersonalization domain) was summarized graphically via box plots by group and time.
To estimate the difference in differences (DID) of survey score changes from baseline to 1 month postrandomization between the Lift intervention and control group participants, we used general linear regression models with unstructured covariance for repeated measures over time for each outcome (PHQ-9, GAD-7, PSS-4, MBI Emotional Exhaustion domain, MBI Personal Accomplishment domain, and MBI Depersonalization domain). Models were fit with PROC MIXED (SAS version 9.4; SAS Institute), and coefficients included a common intercept, indicator variables for time (baseline, 1 month postrandomization), and the interaction between treatment group and time. We calculated estimated means and 95% confidence intervals (CIs) for each treatment group and time point, differences between time points, and DID (27). A full statistical analysis plan was finalized before data analysis and can be found in Appendix E2. In post hoc analysis, we evaluated the association between the number of mindfulness sessions completed and the change in psychological distress and burnout scores using Spearman correlation tests.
Results
Participant Characteristics
Participants were enrolled between May 19, 2021, and December 15, 2021, and followed up until January 31, 2022. The trial was stopped because target enrollment was met. During the trial period, 476 full-time nurses were employed in the four study units and potentially eligible. A total of 133 nurses downloaded the app platform, of whom 102 completed both informed consent and the baseline questionnaire and were randomized to the Lift mindfulness intervention (69 participants) or a waiting list (33 participants) (Figure 1). Baseline characteristics were similar in the two groups (Table 1). Most participants were female (n = 96 [94%]), self-identified as White race (n = 87 [85%]), and self-identified as non-Hispanic ethnicity (n = 94 [92%]). A total of 69 worked the majority of their time in an ICU setting (n = 56 [55%] in the medical ICU and n = 13 [13%] in the surgical ICU).
Figure 1.
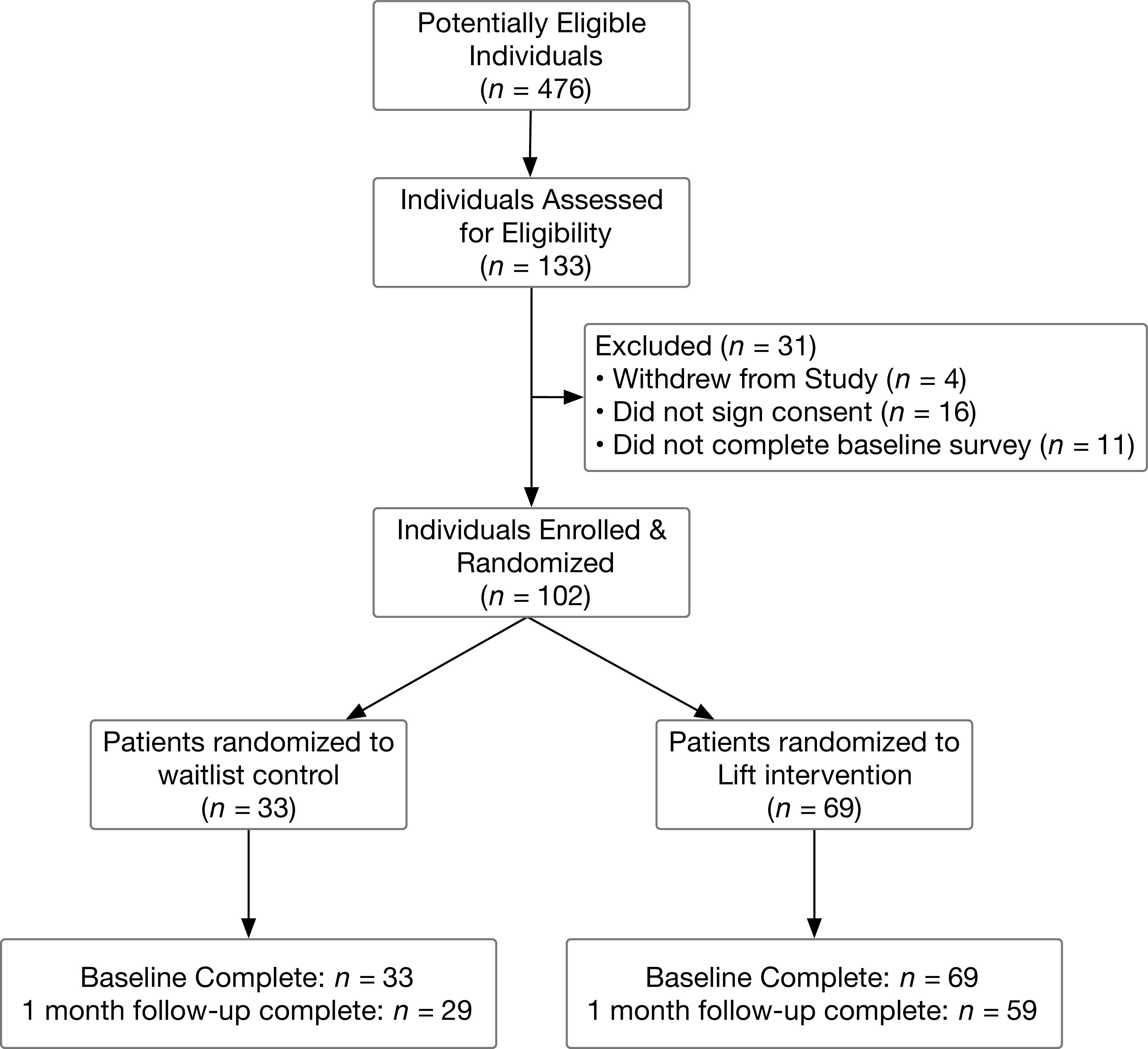
CONSORT (Consolidated Standards of Reporting Trials) diagram.
Table 1.
Participant characteristics
| Control (Waiting List) (n = 33) | Intervention (Lift) (n = 69) | Total (N = 102) | |
|---|---|---|---|
| Age at finish date, yr | 26.0 (25.0, 35.0) | 27.0 (25.0, 32.0) | 26.5 (25.0, 32.0) |
| Sex | |||
| Male | 2 (6.1%) | 4 (5.8%) | 6 (5.9%) |
| Female | 31 (93.9%) | 65 (94.2%) | 96 (94.1%) |
| Ethnicity | |||
| Hispanic or Latino | 1 (3.0%) | 7 (10.1%) | 8 (7.8%) |
| Not Hispanic or Latino | 32 (97.0%) | 62 (89.9%) | 94 (92.2%) |
| Race | |||
| American Indian or Alaskan Native | 0 (0.0%) | 1 (1.4%) | 1 (1.0%) |
| Asian | 4 (12.1%) | 3 (4.3%) | 7 (6.9%) |
| Black or African American | 2 (6.1%) | 2 (2.9%) | 4 (3.9%) |
| White | 27 (81.8%) | 60 (87.0%) | 87 (85.3%) |
| Other race | 0 (0.0%) | 3 (4.3%) | 3 (2.9%) |
| Marital status | |||
| Married or live with partner | 18 (54.5%) | 34 (49.3%) | 52 (51.0%) |
| Single | 15 (45.5%) | 35 (50.7%) | 50 (49.0%) |
| Children under 18 | |||
| No | 24 (72.7%) | 61 (88.4%) | 85 (83.3%) |
| Yes | 9 (27.3%) | 8 (11.6%) | 17 (16.7%) |
| Work location | |||
| Emergency department | 10 (30.3%) | 15 (21.7%) | 25 (24.5%) |
| Surgical ICU | 5 (15.2%) | 8 (11.6%) | 13 (12.7%) |
| Medical ICU | 17 (51.5%) | 39 (56.5%) | 56 (54.9%) |
| Medicine stepdown | 1 (3.0%) | 6 (8.7%) | 7 (6.9%) |
| Duke Raleigh Hospital | 0 (0.0%) | 1 (1.4%) | 1 (1.0%) |
| Work shift | |||
| Day shift | 14 (42.4%) | 24 (34.8%) | 38 (37.3%) |
| Night shift | 5 (15.2%) | 13 (18.8%) | 18 (17.6%) |
| Both day and night shifts | 14 (42.4%) | 32 (46.4%) | 46 (45.1%) |
| Number of shifts worked per week | |||
| <9 | 1 (3.0%) | 1 (1.4%) | 2 (2.0%) |
| 9–12 | 15 (45.5%) | 31 (44.9%) | 46 (45.1%) |
| 13–16 | 17 (51.5%) | 34 (49.3%) | 51 (50.0%) |
| >16 | 0 (0.0%) | 3 (4.3%) | 3 (2.9%) |
| Years as nurse | |||
| <1 yr | 8 (24.2%) | 16 (23.2%) | 24 (23.5%) |
| 1–5 yr | 17 (51.5%) | 33 (47.8%) | 50 (49.0%) |
| 6–10 yr | 3 (9.1%) | 9 (13.0%) | 12 (11.8%) |
| >10 yr | 5 (15.2%) | 11 (15.9%) | 16 (15.7%) |
Definition of abbreviation: ICU = intensive care unit.
Values are displayed as median (interquartile range) or number (percent).
Feasibility Outcomes
Of 133 potentially eligible participants who downloaded the app platform, 113 individuals provided informed consent. Of the 113 individuals who provided informed consent, 102 (90%) completed the baseline questionnaire and were randomized, and of the 102 randomized, 88 (86%) completed the follow-up survey 1 month after randomization, both exceeding predefined feasibility targets (Table 2). In the intervention group, 19 (28%) of 69 participants completed at least one mindfulness session in each of the 4 weeks of the Lift program (target, 60%), and 13 (19%) completed >75% of daily mindfulness sessions provided (target, 50%). The mean number of sessions completed per week of the Lift program in the intervention group is shown in Table E1.
Table 2.
Feasibility outcomes
| Feasibility Outcome | A Priori Defined Benchmark | Observed |
|---|---|---|
| Randomization of consented patients | 80% | 90% (102 of 113) |
| Retention | 80% | 86% (88 of 102) |
| Completion of 4 wk of intervention* | 60% | 28% (19 of 69) |
| Completion of ⩾75% of daily sessions | 50% | 19% (13 of 69) |
At least one session per week completed.
Psychological Distress and Burnout Symptoms
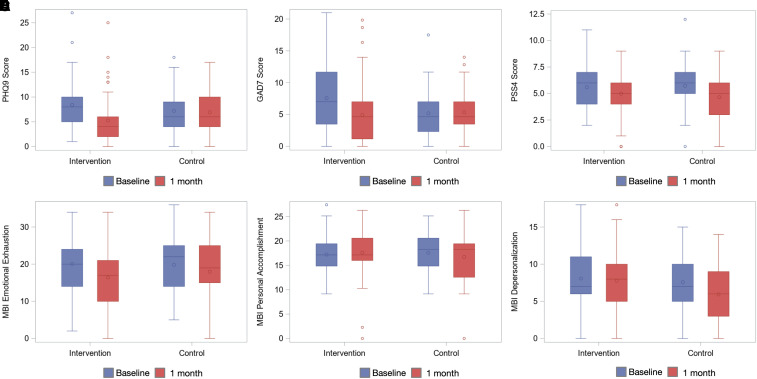
Psychological distress symptom scores (PHQ-9, GAD-7, and PSS-4) and burnout symptom domain scores (MBI Emotional Distress, MBI Personal Accomplishment, and MBI Depersonalization) over time are shown in box plot summaries in Figure 2, and median values and change over time are shown in Table E2. Most participants reported mild to moderate baseline symptoms of depression, anxiety, and perceived stress, as well as high levels of burnout.
Figure 2.
Box-and-whisker plots showing psychological distress and burnout symptoms at baseline and 1 month for control and Lift groups. (A) PHQ-9. (B) GAD-7. (C) PSS-4. (D) Maslach Burnout Inventory (MBI) Emotional Exhaustion domain. (E) MBI Personal Accomplishment domain. (F) MBI Depersonalization domain. GAD-7 = Generalized Anxiety Disorder 7-item scale; PHQ-9 = Patient Health Questionnaire 9-item depression scale; PSS-4 = Perceived Stress Scale 4-item scale.
Change in Psychological Distress and Burnout Scores
Model results indicated significant improvement in PHQ-9 scores for the intervention group participants as compared with the control group (DID, −2.21; 95% CI, −3.99, −0.42; P = 0.016) (Table 3 and Figure E1). However, MBI Depersonalization domain scores showed significantly less improvement for the intervention arm than the control arm (DID, 1.60; 95% CI, 0.18, 3.02; P = 0.03). There were no clinically important group differences over time in GAD-7, PSS-4, MBI Emotional Exhaustion, and MBI Personal Accomplishment.
Table 3.
Psychological distress and burnout symptom score model estimates and difference in differences
| Outcome | Control (Waiting List) |
Intervention (Lift) |
DID | P Value | ||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 1 mo | Difference | Baseline | 1 mo | Difference | |||
| PHQ-9 | 8.01 [7.09, 8.93] | 7.27 [5.75, 8.80] | −0.74 [−2.27, 0.80] | 8.01 [7.09, 8.93] | 5.07 [3.95, 6.19] | −2.94 [−4.07, −1.82] | −2.21 [−3.99, −0.42] | 0.016 |
| GAD-7 | 6.81 [5.87, 7.75] | 6.02 [4.57, 7.47] | −0.79 [−2.29, 0.71] | 6.81 [5.87, 7.75] | 4.62 [3.56, 5.67] | −2.19 [−3.31, −1.07] | −1.40 [−3.11, 0.30] | 0.106 |
| PSS-4 | 5.64 [5.24, 6.03] | 4.66 [3.90, 5.43] | −0.97 [−1.80, −0.15] | 5.64 [5.24, 6.03] | 4.99 [4.45, 5.53] | −0.65 [−1.27, −0.02] | 0.33 [−0.60, 1.26] | 0.487 |
| MBI Emotional Exhaustion | 20.00 [18.54, 21.46] | 17.81 [14.85, 20.76] | −2.19 [−5.14, 0.75] | 20.00 [18.54, 21.46] | 16.49 [14.34, 18.63] | −3.51 [−5.64, −1.39] | −1.32 [−4.81, 2.17] | 0.455 |
| MBI Personal Accomplishment | 17.33 [16.61, 18.06] | 16.70 [14.88, 18.52] | −0.63 [−2.49, 1.22] | 17.33 [16.61, 18.06] | 17.56 [16.27, 18.85] | 0.23 [−1.11, 1.57] | 0.86 [−1.34, 3.06] | 0.439 |
| MBI Depersonalization | 7.91 [7.15, 8.67] | 6.02 [4.80, 7.25] | −1.89 [−3.11, −0.66] | 7.91 [7.15, 8.67] | 7.63 [6.73, 8.52] | −0.29 [−1.19, 0.61] | 1.60 [0.18, 3.02] | 0.027 |
Definition of abbreviations: DID = difference in differences; GAD-7 = Generalized Anxiety Disorder 7-item scale, MBI = Maslach Burnout Inventory; PHQ-9 = Patient Health Questionnaire 9-item depression scale; PSS-4 = Perceived Stress Scale 4-item scale.
Values are presented with estimated means (95% confidence intervals). DID = (T2 − T1 in intervention) − (T2 − T1 in control).
Association of Lift App Use and Psychological Distress and Burnout Scores
In exploratory post hoc analysis, patients in the Lift arm were grouped according to quartile on the basis of the number of mindfulness sessions completed. Median PHQ-9 and GAD-7 scores appeared to decrease with an increasing number of mindfulness sessions completed (Table E3 and Figures E2–E7). However, there was no statistically significant association between the number of mindfulness sessions completed and the change in psychological distress and burnout scores (Table E3).
Discussion
In this pilot randomized controlled trial, a self-directed, mobile app–delivered mindfulness program demonstrated feasibility in recruitment and completion of surveys but had relatively low use by frontline COVID-19 nurses. Nonetheless, those randomized to receive the intervention experienced a significant reduction in depression symptoms relative to the control group. Burnout symptoms were no different by group.
This trial’s findings are important for several reasons. First, they demonstrate the promise of using a highly scalable mobile app–based technology to deliver self-directed therapy to large numbers of healthcare workers quickly. Furthermore, our findings suggest that a brief mobile mindfulness program may provide clinical benefit to address psychological distress symptoms among frontline healthcare workers. This extends past work that successfully tested longer in-person mindfulness programs among healthcare workers (28). The trial results also highlight the difficulty of substantively improving burnout symptoms, which are currently epidemic and undertreated among healthcare workers and with generally higher rates among nurses than among physicians (2, 29, 30).
It is important to emphasize that we do not conceptualize emotional distress or burnout as shortcomings of the individual or as problems best addressed solely at the individual level. System-level factors, especially poor work environment, have been shown to drive emotional distress and burnout in nurses (31, 32). Interventions and investments to address these system-level factors are urgently needed to combat the nursing burnout crisis in the United States and worldwide (29).
However, although systems-focused interventions may have a greater impact, structural healthcare system changes are slow and expensive (33). At a time when hospitals are reeling from pandemic-related staffing shortages and financial stress, easily accessible and inexpensive app-based interventions could be useful short-term adjuncts to combat burnout and psychological distress while awaiting more long-term structural change. In fact, recent systematic reviews of emotional distress and burnout interventions suggest that a hybrid approach including both individual and systems efforts is likely to be the most effective (34, 35).
We also noted two unexpected findings. First, MBI Depersonalization domain scores, which measure distant or indifferent feelings toward a recipient of care (26), improved more in the control group than in the Lift group. It is unclear if this is a spurious finding driven by the relatively small sample size, an unintentional effect of an intervention designed to enhance self-awareness and reflection, or another phenomenon. This finding is also inconsistent with previously published findings of the impact of mindfulness on burnout in nurses (19) and should be interpreted with caution.
We also noted lower app use among participants in the intervention arm than expected and substantially less than app-based distress therapy trials we have conducted among patients (20, 36). This resulted in a substantial number of participants not receiving the full Lift mobile mindfulness intervention as originally intended. Our post hoc analysis suggested decreasing psychological distress scores with a higher number of mindfulness sessions completed, and past trials have demonstrated a relationship between time spent using the mindfulness app and the magnitude of symptom reduction (20). A future focus on strategies to enhance user engagement could augment the treatment effect observed in our study population.
However, app use and engagement in our trial mirror the observed use of commercially available mental health applications in the public (37) and may more closely reflect how the app would be used in a real-world setting than our a priori defined goals. Because there is no known minimum amount of mindfulness meditation needed to effect changes in emotional and psychological distress (38, 39), our observation of a decrease in PHQ-9 scores despite low participant engagement levels commonly seen with mental health apps may actually enhance the external validity of our trial.
Limitations
This trial has several limitations. First, it was performed at a single healthcare center, which may limit its external validity. Our sample population was predominantly young, White, and female and does not reflect the true diversity of the nursing community at large, which may limit the generalizability of our findings (40). In addition, the generalizability of our findings may be limited by an unclear denominator from which the cohort was drawn, as is often the case in trials targeting healthcare workers, whose nursing personnel rosters are constantly in flux and half of whom work outside the hours during which recruitment typically occurs.
Another significant limitation is that individual-based wellness interventions may be susceptible to selection bias. Those persons who chose to participate in a wellness intervention (or a trial testing the intervention) may form a sample population that is significantly different from the desired study population (41, 42). In our trial, only 133 of 476 potentially eligible nurses downloaded the app, indicating that there may have been a selection bias for participants. However, our recruitment methodology using e-mails and flyers with links for those interested to download the app reflects how mobile mindfulness could pragmatically be delivered to a nursing workforce in a real-world setting and may actually enhance the generalizability of the trial results. Finally, because this was a pilot trial that was not powered to detect a specific difference in outcomes, results regarding clinical impact should be considered exploratory.
Conclusions
Despite lower than expected app use and engagement, a self-directed mobile mindfulness program was feasibly delivered to frontline COVID-19 nurses and reduced depression symptoms, though not burnout, when compared with a control group in this pilot randomized controlled trial. Further efforts to improve app engagement, including incorporating feedback from nurses who participated in this trial, are needed. An efficacy-focused trial to confirm our findings of decreased emotional distress is also warranted. Burnout remains a challenging clinical entity that demands additional attention and innovation in individual- and systems-based interventions.
Acknowledgments
Acknowledgment
The authors thank all the participants; the frontline nurses caring for patients with COVID-19 at our hospital; Allie Frear for her regulatory assistance; and Jennifer McLaughlin, Edward Barber, Edward Holzwarth, and Savita Gupta at Pattern Health.
Footnotes
Supported by a COVID-19 Innovation Award from the School of Medicine, Duke University. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
Author Contributions: Substantial contributions to conception or design of the work: E.H.P. and C.E.C. Acquisition, analysis, or interpretation of data: E.H.P., C.E.C., M.K.O., A.J., and A.P. Drafting of the manuscript: E.H.P., C.E.C., M.K.O., and A.P. Critical revision of the manuscript for important intellectual content: All authors. Statistical analysis: M.K.O., A.J., and A.P. Obtained funding: E.H.P. and C.E.C. Administrative, technical, or material support: L.H. and C.J. Supervision: C.E.C. Accountability: All authors have provided agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. E.H.P. and C.E.C. had full access to all the data and take overall responsibility for the integrity of the data and the accuracy of the data analysis.
This article has a data supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Zhang YY, Han WL, Qin W, Yin HX, Zhang CF, Kong C, et al. Extent of compassion satisfaction, compassion fatigue and burnout in nursing: a meta-analysis. J Nurs Manag . 2018;26:810–819. doi: 10.1111/jonm.12589. [DOI] [PubMed] [Google Scholar]
- 2. Shechter A, Diaz F, Moise N, Anstey DE, Ye S, Agarwal S, et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen Hosp Psychiatry . 2020;66:1–8. doi: 10.1016/j.genhosppsych.2020.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sinsky CA, Brown RL, Stillman MJ, Linzer M. COVID-related stress and work intentions in a sample of US health care workers. Mayo Clin Proc Innov Qual Outcomes . 2021;5:1165–1173. doi: 10.1016/j.mayocpiqo.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Maharaj S, Lees T, Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. Int J Environ Res Public Health . 2018;16:61. doi: 10.3390/ijerph16010061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Letvak S, Ruhm CJ, McCoy T. Depression in hospital-employed nurses. Clin Nurse Spec . 2012;26:177–182. doi: 10.1097/NUR.0b013e3182503ef0. [DOI] [PubMed] [Google Scholar]
- 6. Huang CY, Chen CJ, Lee YF, Yeh HC, Kuo JC, Lai HL. Effects of individual characteristics on insomnia severity trajectory among nurses: a prospective longitudinal study. J Nurs Manag . 2019;27:1640–1647. doi: 10.1111/jonm.12851. [DOI] [PubMed] [Google Scholar]
- 7. Huang CL, Wu MP, Ho CH, Wang JJ. Risks of treated anxiety, depression, and insomnia among nurses: a nationwide longitudinal cohort study. PLoS One . 2018;13:e0204224. doi: 10.1371/journal.pone.0204224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Zangaro GA, Dulko D, Sullivan D, Weatherspoon D, White KM, Hall VP, et al. Systematic review of burnout in US nurses. Nurs Clin North Am . 2022;57:1–20. doi: 10.1016/j.cnur.2021.11.001. [DOI] [PubMed] [Google Scholar]
- 9.Manzano García G, Ayala Calvo JC. The threat of COVID-19 and its influence on nursing staff burnout. J Adv Nurs. 2021;77:832–844. doi: 10.1111/jan.14642. [DOI] [PubMed] [Google Scholar]
- 10. Morgantini LA, Naha U, Wang H, Francavilla S, Acar Ö, Flores JM, et al. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: a rapid turnaround global survey. PLoS One . 2020;15:e0238217. doi: 10.1371/journal.pone.0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ross J. The exacerbation of burnout during COVID-19: a major concern for nurse safety. J Perianesth Nurs . 2020;35:439–440. doi: 10.1016/j.jopan.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hu D, Kong Y, Li W, Han Q, Zhang X, Zhu LX, et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: a large-scale cross-sectional study. EClinicalMedicine . 2020;24:100424. doi: 10.1016/j.eclinm.2020.100424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Witkoski Stimpfel A, Ghazal L, Goldsamt L, Vaughan Dickson V. Individual and work factors associated with psychosocial health of registered nurses during the Covid-19 pandemic: a mixed methods study. J Occup Environ Med . 2022;64:515–524. doi: 10.1097/JOM.0000000000002495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Guttormson JL, Calkins K, McAndrew N, Fitzgerald J, Losurdo H, Loonsfoot D. Critical care nurse burnout, moral distress, and mental health during the COVID-19 pandemic: a United States survey. Heart Lung . 2022;55:127–133. doi: 10.1016/j.hrtlng.2022.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Creswell JD. Mindfulness interventions. Annu Rev Psychol . 2017;68:491–516. doi: 10.1146/annurev-psych-042716-051139. [DOI] [PubMed] [Google Scholar]
- 16. Hofmann SG, Gómez AF. Mindfulness-based interventions for anxiety and depression. Psychiatr Clin North Am . 2017;40:739–749. doi: 10.1016/j.psc.2017.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Goldberg SB, Tucker RP, Greene PA, Davidson RJ, Wampold BE, Kearney DJ, et al. Mindfulness-based interventions for psychiatric disorders: a systematic review and meta-analysis. Clin Psychol Rev . 2018;59:52–60. doi: 10.1016/j.cpr.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Guillaumie L, Boiral O, Champagne J. A mixed-methods systematic review of the effects of mindfulness on nurses. J Adv Nurs . 2017;73:1017–1034. doi: 10.1111/jan.13176. [DOI] [PubMed] [Google Scholar]
- 19. Suleiman-Martos N, Gomez-Urquiza JL, Aguayo-Estremera R, Cañadas-De La Fuente GA, De La Fuente-Solana EI, Albendín-García L. The effect of mindfulness training on burnout syndrome in nursing: a systematic review and meta-analysis. J Adv Nurs . 2020;76:1124–1140. doi: 10.1111/jan.14318. [DOI] [PubMed] [Google Scholar]
- 20. Cox CE, Hough CL, Jones DM, Ungar A, Reagan W, Key MD, et al. Effects of mindfulness training programmes delivered by a self-directed mobile app and by telephone compared with an education programme for survivors of critical illness: a pilot randomised clinical trial. Thorax . 2019;74:33–42. doi: 10.1136/thoraxjnl-2017-211264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Pratt EH, Cox CE, Olsen MK, Parish A, Jan A. Mobile mindfulness intervention to reduce emotional distress and burnout in frontline healthcare workers: the LIFT-HCW pilot RCT [abstract] Am J Respir Crit Care Med . 2022;205:A1537. [Google Scholar]
- 22.Han B, Enas NH, McEntegart D. Randomization by minimization for unbalanced treatment allocation. Stat Med. 2009;28:3329–3346. doi: 10.1002/sim.3710. [DOI] [PubMed] [Google Scholar]
- 23. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med . 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med . 2006;166:1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 25. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav . 1983;24:385–396. [PubMed] [Google Scholar]
- 26. Maslach C, Schaufeli WB, Leiter MP. Job burnout. Annu Rev Psychol . 2001;52:397–422. doi: 10.1146/annurev.psych.52.1.397. [DOI] [PubMed] [Google Scholar]
- 27.Fitzmaurice GMLN, Ware JH. Applied longitudinal analysis. Hoboken, NJ: John Wiley & Sons; 2012. [Google Scholar]
- 28. Krasner MS, Epstein RM, Beckman H, Suchman AL, Chapman B, Mooney CJ, et al. Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA . 2009;302:1284–1293. doi: 10.1001/jama.2009.1384. [DOI] [PubMed] [Google Scholar]
- 29. Murthy VH. Confronting health worker burnout and well-being. N Engl J Med . 2022;387:577–579. doi: 10.1056/NEJMp2207252. [DOI] [PubMed] [Google Scholar]
- 30. Sexton JB, Adair KC, Proulx J, Profit J, Cui X, Bae J, et al. Emotional exhaustion among US health care workers before and during the COVID-19 pandemic, 2019-2021. JAMA Netw Open . 2022;5:e2232748. doi: 10.1001/jamanetworkopen.2022.32748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Brooks Carthon JM, Hatfield L, Brom H, Houton M, Kelly-Hellyer E, Schlak A, et al. System-level improvements in work environments lead to lower nurse burnout and higher patient satisfaction. J Nurs Care Qual . 2021;36:7–13. doi: 10.1097/NCQ.0000000000000475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Gensimore MM, Maduro RS, Morgan MK, McGee GW, Zimbro KS. The effect of nurse practice environment on retention and quality of care via burnout, work characteristics, and resilience: a moderated mediation model. J Nurs Adm . 2020;50:546–553. doi: 10.1097/NNA.0000000000000932. [DOI] [PubMed] [Google Scholar]
- 33. Rotenstein LS, Zhao Z, Mata DA, Guille C, Sen S. Substantial overlap between factors predicting symptoms of depression and burnout among medical interns. J Gen Intern Med . 2021;36:240–242. doi: 10.1007/s11606-020-05664-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. West CP, Dyrbye LN, Erwin PJ, Shanafelt TD. Interventions to prevent and reduce physician burnout: a systematic review and meta-analysis. Lancet . 2016;388:2272–2281. doi: 10.1016/S0140-6736(16)31279-X. [DOI] [PubMed] [Google Scholar]
- 35. Romppanen J, Häggman-Laitila A. Interventions for nurses’ well-being at work: a quantitative systematic review. J Adv Nurs . 2017;73:1555–1569. doi: 10.1111/jan.13210. [DOI] [PubMed] [Google Scholar]
- 36. Cox CE, Kelleher SA, Parish A, Olsen MK, Bermejo S, Dempsey K, et al. Feasibility of mobile app-based coping skills training for cardiorespiratory failure survivors: the blueprint pilot randomized controlled trial. Ann Am Thorac Soc . 2023;20:861–871. doi: 10.1513/AnnalsATS.202210-890OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Baumel A, Muench F, Edan S, Kane JM. Objective user engagement with mental health apps: systematic search and panel-based usage analysis. J Med Internet Res . 2019;21:e14567. doi: 10.2196/14567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Shapiro DA, Barkham M, Rees A, Hardy GE, Reynolds S, Startup M. Effects of treatment duration and severity of depression on the effectiveness of cognitive-behavioral and psychodynamic-interpersonal psychotherapy. J Consult Clin Psychol . 1994;62:522–534. doi: 10.1037/0022-006x.62.3.522. [DOI] [PubMed] [Google Scholar]
- 39. Carmody J, Baer RA. How long does a mindfulness-based stress reduction program need to be? A review of class contact hours and effect sizes for psychological distress. J Clin Psychol . 2009;65:627–638. doi: 10.1002/jclp.20555. [DOI] [PubMed] [Google Scholar]
- 40.U.S. Census Bureau. 2022. https://www.census.gov/nssrn
- 41. Jones D, Molitor D, Reif J. What do workplace wellness programs do? Evidence from the Illinois Workplace Wellness Study. Q J Econ . 2019;134:1747–1791. doi: 10.1093/qje/qjz023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Reif J, Chan D, Jones D, Payne L, Molitor D. Effects of a workplace wellness program on employee health, health beliefs, and medical use: a randomized clinical trial. JAMA Intern Med . 2020;180:952–960. doi: 10.1001/jamainternmed.2020.1321. [DOI] [PMC free article] [PubMed] [Google Scholar]