Abstract
Objective
The aim of this study is to analyze the diagnostic value of Quick Sequential Organ Failure Assessment (qSOFA), modified qSOFA, National Early Warning Score (NEWS) and NEWS + Lactate (NEWS + L) scores in the detection of severe community-acquired pneumonia (CAP).
Methods
This research is a retrospective cohort study. Patients admitted to the Emergency Department (ED) with the diagnosis of CAP were divided into severe and mild pneumonia regarding their Pneumonia Severity Index (PSI) scores. The accuracies of lactate, procalcitonin (PCT) values, NEWS and qSOFA scores, as well as score combinations (NEWS + L and qSOFA + PCT) in predicting patients with severe CAP were analyzed.
Results
Median qSOFA value in the severe CAP group (0 [IQR 0–1]) was found to be higher than median qSOFA value (0 [IQR 0-0]) in the mild CAP group (p < 0.001). The rate of qSOFA positivity (qSOFA ≥ 2) was significantly higher in the severe CAP group (17.1%, n = 21) compared to the mild CAP group (1.3%, n = 1) (p < 0.001). Median qSOFA + PCT for the severe CAP group (2 [IQR 1–2]) was higher than the mild CAP group (1 [IQR 0–1]) (p < 0.001). Mean NEWS score for severe CAP (4.95 ± 3.09) was found to be 1.69 (95% CI 0.92–2.46) higher than mean NEWS score of the mild CAP group (3.26 ± 2.39) (p < 0.001). The severe CAP NEWS + L score (6.97 ± 3.71) was higher than the mild CAP NEWS + L score (4.94 ± 2.48) (p < 0.001). Blood lactate level was not significant in the evaluation of severe CAP (p = 0.221). PCT (AUROC = 0.685 [95% CI 0.610–0.760]; p = 0.038), NEWS score (AUROC = 0.658 95% CI [0.582–0.733]; p < 0.001), qSOFA (AUROC = 0.686) were calculated to have adequate accuracy for the detection of severe CAP. [95% CI 0.613–0.759]; p = 0.037), NEWS + L score (AUROC = 0.665 [95% CI 0.589–0.740]; p = 0.038). The qSOFA + PCT score (AUROC = 0.758 [95% 0.691–0.825]; p = 0.034) was also found to be a highly accurate predictor of severe CAP.
Conclusion
In this study, we found a combination of qSOFA and PCT to be the most reliable method of detecting severe CAP.
Keywords: Community-acquired pneumonia, Scoring systems, Procalcitonin, Lactate
1. Introduction
Community-acquired pneumonia (CAP) is a major cause of hospitalizations and deaths globally [1]. It is a serious disorder that impacts 450 millions individuals each year, particularly in the older population, where comorbid disorders are increasingly widespread due to the extension of human life spans and the aging of societies [2]. In many countries of the world, patients with CAP are initially diagnosed in emergency departments (ED). Although a joint decision is made mostly in liaison with many disciplines in the management and treatment of the patient diagnosed with CAP, emergency physicians occupy an indispensable place in order to triage these patients expediently in the first admission, to diagnose them, to isolate them from other patients, to prevent progression and to manage them correctly. Decisions to be made in ED should be fast, accurate and appropriate in terms of effectiveness [3]. A correct triage and prioritization is the first step in making these decisions. Although many triage systems are used to prioritise every patient presenting to the ED, one of the most frequently used triage systems is the National Early Warning Score (NEWS), which provides additional information on mortality rates and intensive care admission rates beyond traditional clinical risk scores [4,5].
ED assessment of patients with CAP consists of history, physical examination, imaging, use of biomarkers, diagnostic and clinical scores. Most of the literature available on CAP prognostic markers cover risk stratification of patients admitted to the hospital in order to estimate the risk of death and to decide on discharge or hospitalization, to determine the most appropriate care for the patients to be admitted [6]. Since severe pneumonia is closely associated with sepsis and mortality, distinguishing between mild and severe pneumonia is critical in addition to hospitalization and discharge judgments [7]. Cultivating this distinction in the emergency department may aid in complying with the requirements of early hydration and antibiotherapy in terms of sepsis, as well as concentrating on the subtle signs of hypoperfusion and organ system dysfunction that accompany severe pneumonia [8]. Therefore, while safe clinical decision support systems or scoring systems enable clinicians to make objective and rapid decisions, they can provide closer follow-up of critical patients in different sites in the ED [9].
Although the pneumonia severity index (PSI) is the most commonly used risk stratification tool for differentiating CAP into severe and mild, its calculation involves an extensive range of variables and parameters such as BUN, sodium, partial oxygen pressure, and pH, that might have limited benefit in diagnosis, particularly in the young population, and whose pathologies are infrequent [10]. Furthermore, compared to NEWS-L, a newly introduced clinical score, PSI score has lower area under the receiver operating characteristics for detecting mortality in pneumonia patients [11]. The qSOFA score, which is simpler to calculate and implement in practice than the PSI, has been demonstrated to have a high specificity in identifying mortality, but its poor sensitivity hindered early identification of individuals with high mortality [12]. But nevertheless, while qSOFA is not frequently utilized in the management of CAP, which is a leading cause of sepsis, both this score and the lactate value are used in everyday practice to define and assess the severity of sepsis [13]. A combination of procalcitonin, which is recommended as a way to determine antibiotic durations and to differentiate viral infections from bacterial infections, and qSOFA demonstrated higher diagnostic accuracy in detecting mortality than qSOFA alone [14,15].
The aim of this study is to determine the diagnostic accuracy of the NEWS score qSOFA score, qSOFA + Procalcitonin score, and NEWS + Lactate score in the differentiation of severe and mild CAP.
2. Methods
2.1. Study design and population
This research is a retrospective cohort study which uses patient information accessed from the hospital information management system (HIMS). This study was conducted with the data of patients admitted to the ED of Health Sciences University Istanbul Training and Research Hospital during a 7-month period (September 1, 2018–March 30, 2019). The study included all patients diagnosed with CAP in the emergency department over 18 years of age, regardless of whether they were admitted or discharged. Through HIMS, medical history, physical examination findings, laboratory data, and imaging were utilized to validate the primary ED physician's diagnosis of CAP. Patients excluded from the study were those whose information could not be accessed in HIMS, nosocomial pneumonia was suspected, recent history of hospitalization, immunocompromised, received radiotherapy and or chemotherapy in the last three months, those who had HIV-infection, invasive fungal infection, malaria attack, neuroendocrine tumor, patients with non-infectious systemic inflammation (inhalation injury, pancreatitis, heat stroke, mesenteric ischemia), major/multiple trauma, severe burns, recent major surgery, and those who refused to participate in the study. Institutional Review Board approval was obtained before the study by Health Sciences University Istanbul Training and Research Hospital Ethics Committee (Decision number: 1329). The study was conducted in accordance with the declaration of Helsinki.
2.2. Data collection
The patients' PSI scores and outcome data were recorded by a joint decision by experts from 4 different medical branches (emergency medicine, pulmonology, infectious diseases and intensive care). ICD-10 codes for certain specific diagnoses (J15, J18, J18.9, J22, R05, R07.4) associated with pneumonia were abstracted from the HIMS to monitor patients’ clinical courses. Observation forms, progression notes of the patients admitted to the ED were followed up. Thus, the rates of missing data due to incorrect or incomplete diagnostic codes was minimized.
Demographic characteristics (sex and age) of the patients included in the study, vital signs (blood pressure, pulse, fever, respiratory rate, peripheral oxygen saturation, level of consciousness), presence of pleural effusion on chest X-ray, laboratory test results on admission to ED, comorbid diseases such as cerebrovascular disease (CVD), chronic kidney disease (CKD), neoplastic disease, congestive heart failure (CHF) were recorded. Admission PCT and other laboratory values of the patients were measured, and the PSI score was calculated. The procalcitonin kit was from Roche and was run on a Cobas E instrument (Roche Diagnostics, Rotkreuz, Switzerland). National Committee for Clinical Laboratory Standards (NCCLS) and International Federation of Clinical Chemistry (IFCC) made according to the recommendations [16,17].
In accord with the calculated PSI scores, the patients were divided into two groups as severe CAP (PSI>90) and mild CAP (PSI≤90) [18]. On the other hand, qSOFA scores were obtained with the variables of respiratory rate (>22), systolic blood pressure (<100 mmHg), and clouding of consciousness (GCS<15) [13]. For the calculation of qSOFA + PCT score, procalcitonin was scored as 0, 1, and 2 according to the PCT level obtained on admission (PCT <0.25 = 0; 0.25 < PCT<2=1; PCT>2 = 2) and it was added to the qSOFA score [15].
The NEWS score was calculated using respiratory rate (bpm) for (≤8 = 3; 9–11 = 1, 12–20 = 0, 21–24 = 2, ≥25 = 3), oxygen saturation (%) (≤91 = 3, 92–93 = 2, 94–95 = 1, ≥96 = 0), need for oxygen support (yes = 2, no = 0), body temperature (C) (≤35 = 3, 35.1–36 = 1, 36.1–38 = 0, 38.1–39 = 1, ≥39.1 = 2), systolic blood pressure (mmHg) (≤90 = 3, 91–100 = 2, 101–110 = 1, 111–219 = 0, ≥220 = 3) heart rate (bpm) (≤40 = 3, 41–50 = 1, 51–90 = 0, 91–110 = 1, 111–130 = 2, ≥131 = 3) and level of consciousness (AVPU scale, Alert = 0, Verbal = 3, Pain = 3, Unresponsive = 3) [19]. The NEWS + L scores were recorded by adding the numerical value of the blood lactate level to the NEWS score [20].
The diagnostic values of lactate, procalcitonin, qSOFA, qSOFA + PCT, NEWS, and NEWS + L scores in predicting severe CAP were calculated by ROC analysis. Sensitivity, specificity, positive and negative predictive values at the cut-off points where Youden index (or Youden׳s J statistic) was the highest were calculated from ROC analysis.
2.3. Statistical analysis
Statistical Package for Social Sciences (SPSS v27) was used for statistical analysis. Continuous numerical data were given as mean ± standard deviation and median (interquartile range [IQR] 25th–75th), while categorical data were presented as frequency and percentage. The distribution of continuous data was confirmed with the Kolmogorov-Smirnof test and histogram. Comparisons of two independent groups in continuous data showing parametric distribution were performed with Student's t-test, and those with nonparametric distribution were processed with Mann-Whitney U test. Comparison of independent categorical data of the groups was done using the chi-square test. The ROC curve was drawn for the diagnostic valency tests, and the sensitivity, specificity, positive and negative predictive values were calculated for the cut-off values with the highest Youden index for the parameters with statistical significance. P < 0.05 was accepted as the threshold for alpha significance.
3. Results
After excluding 68 patients who did not meet the study's inclusion criteria, the study was completed with data from 199 patients. Among these, 76 (38.2%) of the patients had mild CAP and 123 (61.8%) of them were grouped as severe CAP. Demographic and clinical data of the groups are shown in Table 1. While the median age of the sample was calculated as 75 years (IQR 67–82), it was observed that the median age of the severe CAP group (79 [IQR 70–84]) was significantly higher than the age median of the mild CAP group (70 [IQR 62.25–77]) (p < 0.001, Mann-Whitney U test). The number of women in the mild CAP group was 40 (52.6%), while the number of women in the severe CAP group was 64 (52%) (p = 0.934, Pearson's chi-square test). The demographics, vital signs, and medical history of the study population are summarized in Table 1.
Table 1.
Demographics, vital signs, and medical history of study population.
| Total (n = 199) | Mild Pneumonia (n = 76) | Severe pneumonia (n = 123) | p value | |
|---|---|---|---|---|
| Age (years) | 75 (67–82) | 70 (62.25–77) | 79 (70–84) | <0.001 |
| Gender (female) | 104 (52.3%) | 40 (52.6%) | 64 (52%) | 0.934 |
| SBP (mmHg) | 138.58 ± 27.9 | 139.7 ± 25.61 | 137.89 ± 29.31 | 0.659 |
| DBP (mmHg) | 72.45 ± 13.99 | 72.33 ± 12.95 | 72.53 ± 14.65 | 0.922 |
| Pulse rate (minute) | 98 (87–113) | 94.5 (86–112.75) | 100 (87–114) | 0.376 |
| Peripheric oxygen saturation (%) | 93 (89–96) | 94 (92–96) | 92 (86–95) | <0.001 |
| Temperature (°C) | 37.02 ± 1.08 | 37.04 ± 1.1 | 37 ± 1.06 | 0.846 |
| Respiratory Rate (minute) | 20 (18–24) | 20 (18–20) | 20 (18–24) | <0.001 |
| Urea (mg/dL) | 46 (34–62) | 35.5 (29–46) | 52 (42–83) | <0.001 |
| Nursing Home Resident | 49 (24.6) | 7 (14.3) | 42 (34.1) | <0.001 |
| Neoplasm | 19 (9.5%) | 3 (3.9%) | 16 (13%) | 0.035 |
| Congestive Heart Failure | 47 (23.6%) | 10 (13.2%) | 37 (30.1%) | 0.006 |
| Cerebrovascular Disease | 24 (12.1%) | 5 (6.6%) | 19 (15.4%) | 0.062 |
| Chronic Kidney Disease | 29 (14.6%) | 2 (2.6%) | 27 (22%) | <0.001 |
| Pleural effusion | 48 (24.1%) | 7 (9.2%) | 41 (33.3%) | <0.001 |
| Acidosis | 20 (10.1%) | 1 (1.3%) | 19 (15.4%) | 0.001 |
| Lactate (mmol/L) | 1.64 (1.21–2.24) | 1.53 (1.18–2.04) | 1.67 (1.23–2.35) | 0.221 |
| PCT (ng/mL) | 0.36 (0.23–0.70) | 0.3 (0.05–0.425) | 0.43 (0.3–0.93) | <0.001 |
| Altered mental status | 35 (17.6%) | 1 (1.3%) | 34 (27.6%) | <0.001 |
SBP: Systolic blood pressure; DBP: Diastolic Blood Pressure; PCT: Procalcitonin.
The median qSOFA value in the severe CAP group (0 [IQR 0–1]) was higher than the median qSOFA value in the mild CAP group (0 [IQR 0–0]) (p < 0.001, Mann-Whitney U test). The rate of qSOFA positivity, defined as qSOFA ≥ 2, was significantly higher in the severe CAP group (17.1%, n = 21) compared to the mild CAP group (1.3%, n = 1) (p < 0.001, Pearson chi-square test). The median qSOFA + PCT (2 [IQR 1–2]) in the severe pneumonia group was higher than the mild CAP group (1 [IQR 0–1]) (p < 0.001, Mann-Whitney U test). Mean NEWS score of the severe CAP (4.95 ± 3.09) was found to be 1.69 points (95% CI 0.92–2.46) higher than mild CAP group (3.26 ± 2.39) points (p < 0.001, Student's t-test). Likewise, mean NEWS + L score of the patients with severe CAP (6.97 ± 3.71) was higher than the mild CAP group (4.94 ± 2.48) with a mean difference of 2.03 (95% CI 1.17 to 2.90) (p < 0.001, Student's t-test).
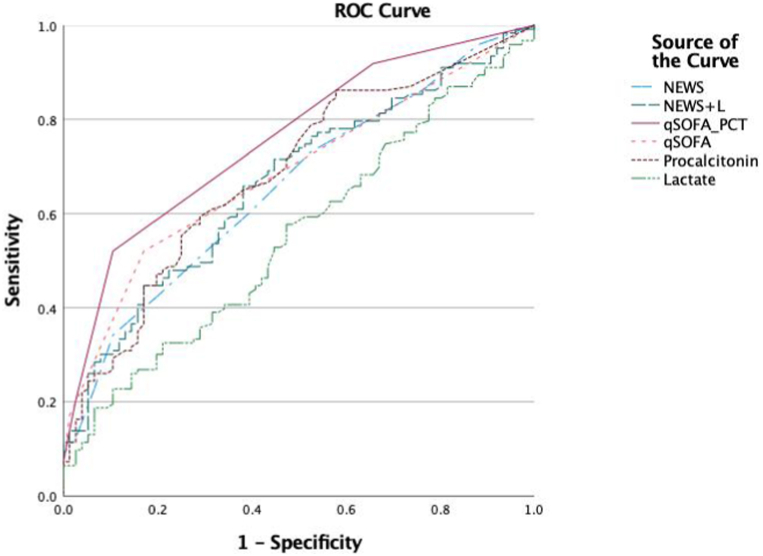
In the light of available clinical and laboratory data, ROC curves were drawn showing the diagnostic value of lactate, procalcitonin, NEWS, NEWS + L, qSOFA and qSOFA + PCT values in the evaluation of severe CAP. Diagnostic values are statistically given in Table 2. It was observed that blood lactate level was not significant in the detection of severe CAP (p = 0.221).
Table 2.
Comparison of scores among mild pneumonia and severe pneumonia groups.
| Total (n = 199) | Mild Pneumonia (n = 76) | Severe pneumonia (n = 123) | p value | |
|---|---|---|---|---|
| qSOFA | 0 (0–1) | 0 (0–0) | 0 (0–1) | <0.001 |
| qSOFA ≥ 2 | 1 (1.3) | 21 (17.1) | <0.001 | |
| qSOFA + PCT | 1 (1–2) | 1 (0–1) | 2 (1–2) | <0.001 |
| NEWS | 4.31 ± 2.95 | 3.26 ± 2.39 | 4.95 ± 3.09 | <0.001 |
| NEWS + L | 6.2 ± 3.44 | 4.94 ± 2.48 | 6.97 ± 3.71 | <0.001 |
qSOFA: Quick Sequential Organ Failure Assessment; PCT: Procalcitonin; qSOFA + PCT: Combination of Procalcitonin and qSOFA; NEWS: National Early Warning Score; NEWS + L: Combination of NEWS and Lactate.
As shown on Table 3, procalcitonin (AUROC = 0.685 [95% CI 0.610–0.760], p = 0.038), NEWS score (AUROC = 0.658 95% CI [0.582–0.733], p < 0.001), qSOFA (AUROC = 0.686 [95% CI 0.613–0.759], p = 0.037), NEWS + L score (AUROC = 0.665 [95% CI 0.589–0.740]; p = 0.038) were found to be sufficient parameters for the detection of severe CAP, whereas qSOFA + PCT score (AUROC = 0.758 [95% 0.691–0.825) ]; p = 0.034) was found to be a strong marker in the detection of severe CAP (Fig. 1). qSOFA + PCT score is found to have significantly higher AUROC values than NEWS + L score (p = 0.001, difference between areas [DBA] 0.093), qSOFA score (p = 0.003, DBA 0.07), NEWS score (p = 0.006, DBA 0.1), PCT value (p = 0.008, DBA 0.072). It was determined that the other scores were not superior to each other in terms of AUROC (p > 0.05 for every comparison).
Table 3.
Diagnostic accuracy of lactate, procalcitonin, NEWS score, NEWS + L score, qSOFA score and qSOFA + PCT score in predicting severe pneumonia.
| AUROC (95% CI) | p | ICF | +LR | -LR | |
|---|---|---|---|---|---|
| Lactate (mmol/L) | 0.552 (0.480–0.622) | 0.221 | |||
| PCT (ng/mL) | 0.685 (0.610–0.760) | 0.038 | 0.38 | 2.05 (1.4–3) | 0.57 (0.44–0.74) |
| NEWS | 0.658 (0.582–0.733) | <0.001 | 6 | 3.24 (1.61–6.52) | 0.74 (0.64–0.86) |
| qSOFA | 0.686 (0.613–0.759) | 0.037 | 1 | 3.04 (1.8–5.13) | 0.58 (0.47–0.72) |
| NEWS + L | 0.665 (0.589–0.740) | 0.038 | 4.5 | 1.56 (1.18–2.05) | 0.54 (0.39–0.76) |
| qSOFA + PCT | 0.758 (0.691–0.825) | 0.034 | 2 | 4.94 (2.51–9.72) | 0.54 (0.44–0.66) |
qSOFA: Quick Sequential Organ Failure Assessment; PCT: Procalcitonin; qSOFA + PCT: Combination of Procalcitonin and qSOFA; NEWS: National Early Warning Score; NEWS + L: Combination of NEWS and Lactate; ICF: Ideal Cut-off Value; + LR: Positive Likelihood Ratio; -LR: Negative Likelihood Ratio; CI: Confidence Interval.
Fig. 1.
ROC curves for lactate, procalcitonin, NEWS, NEWS + L, qSOFA and qSOFA + PCT for diagnostic accuracy in predicting severe pneumonia.
Sensitivity, specificity, positive and negative predictive value data according to the highest Youden index cut-offs of PCT, qSOFA, NEWS, NEWS + L and qSOFA + PCT values are given in Table 4.
Table 4.
Sensitivity, specificity, positive predictive value and negatif predictive value of PCT, qSOFA, NEWS, NEWS + L and qSOFA + PCT at highest Youden index.
| Sensitivity (95% CI) | Specificity (95% CI) | PPV (95% CI) | NPV (95% CI) | |
|---|---|---|---|---|
| PCT≥0.38 | 59.35 (50.1–68.1) | 71.05 (59.5–80.9) | 76.84 (69.38–82.93 | 51.92 (45.5–58.28) |
| qSOFA ≥1 | 52.03 (42.8–61.1) | 82.89 (72.5–90.6) | 83.12 (74.47–89.26) | 51.64 (46.38–56.86) |
| NEWS ≥6 | 34.15 (25.8–43.2) | 89.47 (80.3–95.3) | 84 (72.28–91.36) | 45.64 (41.98–49.35) |
| NEWS + L ≥ 4.5 | 69.92 (61–77.9) | 55.26 (43.4–66.7) | 71.67 (65.76–76.91) | 53.16 (44.77–61.39) |
| qSOFA + PCT≥2 | 52.03 (42.8–61.1) | 89.47 (80.3–95.3) | 88.89 (80.26–94.03) | 53.54 (48.56–58.46) |
qSOFA: Quick Sequential Organ Failure Assessment; PCT: Procalcitonin; qSOFA + PCT: Combination of Procalcitonin and qSOFA; NEWS: National Early Warning Score; NEWS + L: Combination of NEWS and Lactate; PPV: Positive Predictive Value; NPV: Negative Predictive Value; CI: Confidence Interval.
4. Discussion
Recent guidelines recommend using the PSI as a clinical prediction rule in addition to the physician's clinical assessment in CAP [21]. In particular, there are many studies on the scoring of the severity of CAP, indicating that these scales are more successful in deciding which patients should be hospitalized and which would course better with outpatient follow-up rather than deciding on the appropriate treatment methods for the patients [22]. The results of our study revealed that the qSOFA + PCT score detected severe pneumonia more effectively than the NEWS + lactate score, the NEWS score, lactate values, and procalcitonin values.
The PSI score, which is recommended to be used in diagnostic process of CAP, includes 20 parameters including patients' demographic data, comorbidities, vital parameters, findings on physical examination, blood test results, and imaging interpretations [23]. In this study, PSI variables such as age, nursing home residence, chronic kidney disease, pleural effusion, altered mental status, respiratory rate, acidosis, peripheral oxygen saturation, neoplastic disease, congestive heart failure, cerebrovascular disease were found to be significantly different between severe and mild patients with CAP. On the other hand, no significant difference was observed between the groups in terms of gender, body temperature, SBP, pulse rate. In addition, urea and PCT values which are not covered by PSI were also significantly higher in severe patients.
Combining biomarkers with the qSOFA score was thought to potentially increase its ability to predict the risk of mortality from sepsis, especially after the usability and accuracy of this rapid screening were controversial debate topics [15]. In a study associating the qSOFA score with mortality in patients with CAP, the area under the ROC curve was found to be 0.70 (95% CI, 0.66–0.74), and the poor sensitivity of qSOFA did not result in a strong recommendation because of its limitations in early identification of mortality in patients with pneumonia [12]. Although patients with severe pneumonia were associated with the qSOFA score not with mortality in this study, it was found to be 0.686 (95% CI, 0.613–0.759), similar to the literature, and qSOFA per se was considered insufficient for the detection of severe pneumonia.
In this study, the predictions of PCT values in addition to qSOFA and the combination of qSOFA + PCT in differentiating severe patients were examined. A significant difference was detected in these three values in severe patients, but qSOFA combined with PCT was found to be the best marker, especially in terms of specificity, in the detection of severe CAP. A combination of qSOFA's ability to detect sepsis, which is one of the most closely correlated factors with death in any infection, and procalcitonin data, one of the best laboratory tests for detecting infection severity among those used in daily practice, may explain why qSOFA + PCT scores outperformed the other scores in our study. Although scarce data are available on CAP, it has been postulated in the literature that this combination is used to estimate mortality in sepsis patients and the combination had a positive contribution on sensitivity [15]. In studies on the predictive power of SOFA and PCT in CAP patients in the ED, SOFA was found to be superior to PCT and a combination was recommended. Of note, most studies using risk scores for sepsis and CAP find combinations of scores and biomarkers stronger.
In addition, most patients with CAP are critically ill, who are commonly present to the ED. In recent years, there are studies in which NEWS is found superior to many scores in predicting ICU admission in patients with CAP [24]. Therefore, NEWS, which is used in critically ill patients in ED in recent years and lactate value, which is frequently used in critical patients, together with their combination, NEWS-lactate (NEWS-L), were also evaluated in this study [20,25].
In this study, it was shown that blood lactate level was not significant in the detection of severe CAP. The combination of both NEWS and NEWS-L has proven to be significant in severe patients [20]. Similar to the findings in the literature, although the NEWS-L combination was more sensitive in predicting severe CAP, it was not as strong as the qSOFA and PCT combination. As there was no statistically significant difference between NEWS scores and qSOFA scores for diagnostic accuracy according to the area under the receiver operating characteristics, procalcitonin's superiority over lactate can be attributed to the difference in detecting severe CAP.
5. Limitations
Single-center observational design is a major limitation of the study, which prevents generalizability of the findings. Likewise, exclusion of patients younger than 18 years of age and certain specific patient groups such as those with nosocomial pneumonia should be taken into account before extrapolating the findings to the general population.
6. Conclusion
In this study, we found a combination of qSOFA and PCT to be a more reliable and specific method of detecting severe CAP than other scores we studied. This combination could to be used in EDs to detect severe CAP patients quickly and accurately.
Author contribution statement
Tolgahan Güleç: Conceived and designed the experiments; Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper. Sarper Yılmaz; Özgür Karcıoğlu: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper. Rohat Ak: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper. Ali Cankut Tatlıparmak: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Data availability statement
Data will be made available on request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Contributor Information
Tolgahan Güleç, Email: gulectolgahan@gmail.com.
Sarper Yılmaz, Email: sarperyilmaz08@gmail.com.
Rohat Ak, Email: rohatakmd@gmail.com.
Ali Cankut Tatlıparmak, Email: alicankut@gmail.com.
Özgür Karcıoğlu, Email: okarcioglu@gmail.com.
References
- 1.Aliberti S., Dela Cruz C.S., Amati F., Sotgiu G., Restrepo M.I. Community-acquired pneumonia. Lancet. 2021;398:906–919. doi: 10.1016/S0140-6736(21)00630-9. [DOI] [PubMed] [Google Scholar]
- 2.Manikam L., Lakhanpaul M. Epidemiology of community acquired pneumonia. Paediatr. Child Health. 2012;22:299–306. doi: 10.1016/j.paed.2012.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moran G. Approaches to treatment of community-acquired pneumonia in the emergency department and the appropriate role of fluoroquinolones. J. Emerg. Med. 2006;30:377–387. doi: 10.1016/j.jemermed.2005.07.009. [DOI] [PubMed] [Google Scholar]
- 4.Ustaalioğlu İ., Ak R., Öztürk T.C., Koçak M., Onur Ö. Investigation of the usability of the REMS, RAPS, and MPM II0 scoring systems in the prediction of short-term and longterm mortality in patients presenting to the emergency department triage. Ir. J. Med. Sci. 2022 Jun 16 doi: 10.1007/s11845-022-03063-1. [DOI] [PubMed] [Google Scholar]
- 5.Lee Y.S., Choi J.W., Park Y.H., Chung C., Park D.I., Lee J.E., Lee H.S., Moon J.Y. Evaluation of the efficacy of the National Early Warning Score in predicting in-hospital mortality via the risk stratification. J. Crit. Care. 2018;47:222–226. doi: 10.1016/j.jcrc.2018.07.011. [DOI] [PubMed] [Google Scholar]
- 6.Speiser J.L., Karvellas C.J., Shumilak G., Sligl W.I., Mirzanejad Y., Gurka D., Kumar A., Kumar A. Institutional Review Boards (IRB) of the Cooperative Antimicrobial Therapy of Septic Shock (CATSS) Database Research Group, Predicting in-hospital mortality in pneumonia-associated septic shock patients using a classification and regression tree: a nested cohort study. J Intensive Care. 2018;6:66. doi: 10.1186/s40560-018-0335-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rider A.C., Frazee B.W. Community-acquired pneumonia. Emerg. Med. Clin. 2018;36:665–683. doi: 10.1016/j.emc.2018.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Laterre P.-F., Garber G., Levy H., Wunderink R., Kinasewitz G.T., Sollet J.-P., Maki D.G., Bates B., Yan S.C.B., Dhainaut J.-F. PROWESS Clinical Evaluation Committee, Severe community-acquired pneumonia as a cause of severe sepsis: data from the PROWESS study. Crit. Care Med. 2005;33:952–961. doi: 10.1097/01.ccm.0000162381.24074.d7. [DOI] [PubMed] [Google Scholar]
- 9.Kılıç M., Ak R., Alışkan H. The utility of hemoglobin, albumin, lymphocyte and platelet (HALP) score in predicting mortality among COVID-19 patients: a preliminary study. Signa Vitae. 2023;19(1):143–147. doi: 10.22514/sv.2022.080. [DOI] [Google Scholar]
- 10.Chen J.-H., Chang S.-S., Liu J.J., Chan R.-C., Wu J.-Y., Wang W.-C., Lee S.-H., Lee C.-C. Comparison of clinical characteristics and performance of pneumonia severity score and CURB-65 among younger adults, elderly and very old subjects. Thorax. 2010;65:971–977. doi: 10.1136/thx.2009.129627. [DOI] [PubMed] [Google Scholar]
- 11.Jo S., Jeong T., Lee J.B., Jin Y., Yoon J., Park B. Validation of modified early warning score using serum lactate level in community-acquired pneumonia patients. The National Early Warning Score-Lactate score. Am. J. Emerg. Med. 2016;34:536–541. doi: 10.1016/j.ajem.2015.12.067. [DOI] [PubMed] [Google Scholar]
- 12.Jiang J., Yang J., Jin Y., Cao J., Lu Y. Role of qSOFA in predicting mortality of pneumonia: a systematic review and meta-analysis. Medicine (Baltim.) 2018;97 doi: 10.1097/MD.0000000000012634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singer M., Deutschman C.S., Seymour C.W., Shankar-Hari M., Annane D., Bauer M., Bellomo R., Bernard G.R., Chiche J.-D., Coopersmith C.M., Hotchkiss R.S., Levy M.M., Marshall J.C., Martin G.S., Opal S.M., Rubenfeld G.D., van der Poll T., Vincent J.-L., Angus D.C. The third international consensus definitions for sepsis and septic shock (Sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Berg P., Lindhardt B.Ø. The role of procalcitonin in adult patients with community-acquired pneumonia--a systematic review. Dan Med J. 2012;59:A4357. [PubMed] [Google Scholar]
- 15.Yu H., Nie L., Liu A., Wu K., Hsein Y.-C., Yen D.W., Lee M.-T.G., Lee C.-C. Combining procalcitonin with the qSOFA and sepsis mortality prediction. Medicine (Baltim.) 2019;98 doi: 10.1097/MD.0000000000015981. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Clinical and Laboratory Standards Institute . Defining, Establishing and Verifying Reference Intervals in the Clinical Laboratory: Approved Guideline, 3. Clinical and Laboratory Standards Institute; Wayne, Pa: 2010. [Google Scholar]
- 17.International Federation of Clinical Chemistry (IFCC), Scientific Committee Clinical section, expert panel on theory of reference values, and international committee for standardization in haematology (ICSH), standing committee on reference values. Approved recommendation (1986) on the theory of reference values. Part 1. The concept of reference values. J. Clin. Chem. Clin. Biochem. 1987;25(5):337–342. [PubMed] [Google Scholar]
- 18.Steinberg D.I. ACP Journal Club. Review: risk prediction scales have different strengths and weaknesses for predicting mortality in community-acquired pneumonia. Ann. Intern. Med. 2011;154:JC4–12. doi: 10.7326/0003-4819-154-8-201104190-02012. [DOI] [PubMed] [Google Scholar]
- 19.Almutary A., Althunayyan S., Alenazi K., Alqahtani A., Alotaibi B., Ahmed M., Osman I.S., Kakpuri A., Alanazi A., Arafat M., Al-Mutairi A., Bashraheel F., Almazroua F. National early warning score (NEWS) as prognostic triage tool for septic patients. Infect. Drug Resist. 2020;13:3843–3851. doi: 10.2147/IDR.S275390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dundar Z.D., Kocak S., Girisgin A.S. Lactate and NEWS-L are fair predictors of mortality in critically ill geriatric emergency department patients. Am. J. Emerg. Med. 2020;38:217–221. doi: 10.1016/j.ajem.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 21.Metlay J.P., Waterer G.W., Long A.C., Anzueto A., Brozek J., Crothers K., Cooley L.A., Dean N.C., Fine M.J., Flanders S.A., Griffin M.R., Metersky M.L., Musher D.M., Restrepo M.I., Whitney C.G. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American thoracic society and infectious diseases society of America. Am. J. Respir. Crit. Care Med. 2019;200:e45. doi: 10.1164/rccm.201908-1581ST. –e67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Loke Y.K., Kwok C.S., Niruban A., Myint P.K. Value of severity scales in predicting mortality from community-acquired pneumonia: systematic review and meta-analysis. Thorax. 2010;65:884–890. doi: 10.1136/thx.2009.134072. [DOI] [PubMed] [Google Scholar]
- 23.Ticona J.H., Zaccone V.M., McFarlane I.M. Community-acquired pneumonia: a focused review. Am J Med Case Rep. 2021;9:45–52. doi: 10.12691/ajmcr-9-1-12. [DOI] [Google Scholar]
- 24.Lv C., Chen Y., Shi W., Pan T., Deng J., Xu J. Comparison of different scoring systems for prediction of mortality and ICU admission in elderly CAP population. Clin. Interv. Aging. 2021;16:1917–1929. doi: 10.2147/CIA.S335315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Evans L., Rhodes A., Alhazzani W., et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit. Care Med. 2021;49 doi: 10.1097/CCM.0000000000005337. e1063–e1143. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.