Abstract
Background:
Primary Ewing’s sarcoma (ES) arising from cranial bones is an extremely rare entity that accounts for only 1–4% of all ES cases.
Case Description:
A 21-year-old woman presented with ES of the skull affecting the occipital region. The patient underwent surgical excision following radiotherapy and chemotherapy. No recurrence or metastasis occurred over a 10-month follow-up.
Conclusion:
ES reaches adolescents. The mainstay of treatment includes surgical removal of the tumor, followed by radio- and chemotherapy.
Keywords: Ewing sarcoma, Occipital bone, Skull

INTRODUCTION
Ewing’s sarcoma (ES) is a primitive malignant bone tumor that commonly occurs in the long bones of the lower limbs, pelvis, and ribs. Primary ES of the skull is extremely scarce, accounting for only 14% of all cases.[4,8] In the skull, this sarcoma typically affects the frontal, parietal, temporal, ethmoid, orbital, and maxillary bones. To the best of our knowledge, only nine cases of primary occipital ES have been reported in the literature.
Herein, we present the case of a 21-year-old woman harboring primary ES of the occipital region which was successfully treated with radical excision, followed by radiotherapy and chemotherapy.
CASE REPORT
Clinical presentation
A 21-year-old woman was admitted in June 2022 with a history of large progressive swelling over his occipital region, enlarging for a few months. There were no headaches, vomiting, seizures, or loss of vision.
On physical examination, the patient had a large solid, immobile mass over the occipital region, and no focal neurological deficits were observed.
Diagnosis assessment
Computed tomography (CT) of the head revealed a large well-circumscribed extracranial; isodense mass in the occipital region with bony erosion of the adjacent occipital bone [Figures 1-3].
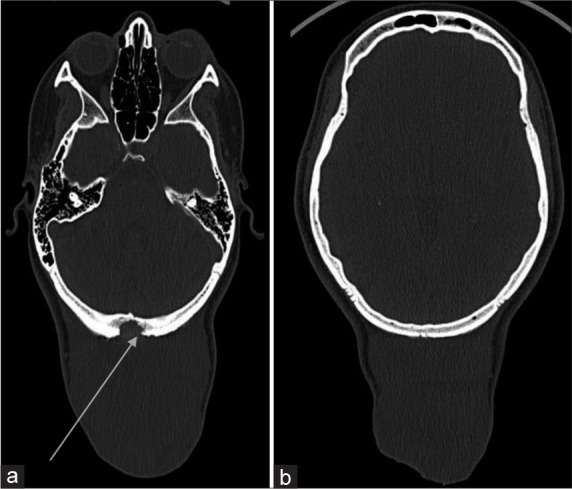
Figure 1:

(a and b) Computed tomography of the head (axial): Showing an extracranial isodense mass lesion of the occipital region (arrow).
Figure 3:
(a and b) Computed tomography of the head with contrast injection (axial bone cuts): Showing a bony erosion (arrow).
Figure 2:

(a and b) Computed tomography of the head with contrast injection (axial): Showing an extracranial isodense mass lesion of the occipital region which was not enhanced after injection.
Therapeutic intervention
After counseling the patient, surgical resection of the tumor was planned. The patient underwent gross total excision of the tumor. A spiculated gross periosteal reaction was observed and the calvarial occipital bone showed erosion. The mass had eroded through the underlying bone but without dura invasion. Methacrylate cranioplasty was performed thereafter [Figure 4]. Histopathological examination revealed that the tumor was an ES.
Figure 4:
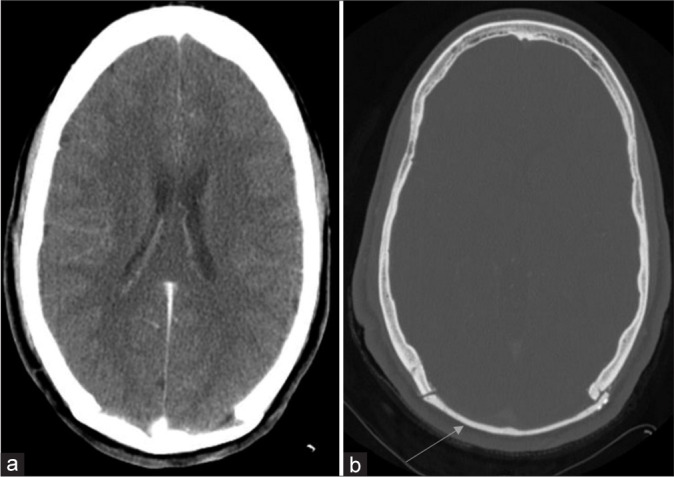
(a and b) Postoperative computed tomography of the head: Showing completely excised tumor with cranioplasty (arrow).
Follow-up
A postoperative CT scan confirmed the complete removal of the tumor [Figure 4]. Based on the diagnosis of ES, the tumor stage was T2, N0, and M0. The patient, then, received postoperative chemotherapy with multiple drugs: Vincristine (1.5 mg/m2 intravenous weekly × 6), cyclophosphamide (1200 mg/m2 intravenous weekly × 6), adriamycin (30 mg/m2 intravenous daily × 2 every month × 6), and actinomycin-D (2 mg/m2 intravenous once every month × 6). For radiotherapy, the patient received 2 Gy/day, 5 days/week for 5 weeks. Ten months after the surgery, the patient remained asymptomatic and tumor-free.
DISCUSSION
In the literature, we have identified nine cases of primary ES of the occipital bone from 1988 to date [Table 1].[1-8] Typically, it occurs in the first two decades of life; however, the youngest patient has been reported to be 16 months old.[8] Interestingly, our study involved the oldest patient in the literature.
Table 1:
A literature review of primary Ewing’s sarcoma of the occipital bone from 1988 to date.

Radiologically, CT scans and magnetic resonance imaging (MRI) provide information about the size, extent, and brain/ dura involvement. In general, a CT scan has documented ES as an iso-hyperdense mass that enhances after contrast injection, delineating the bone involvement. On MRI, the mass is hypo-to isointense on T1W and iso-or hyperintense on T2W, with heterogeneous enhancement following contrast injection. Therapeutic options include surgical removal of the tumor, radiotherapy, and multi-drug chemotherapy.
Regarding surgical treatment, tumor resection should be as radical as possible. The previous reports showed that long-term survival can be expected in ES, provided that the tumor is radically removed followed by radio- and chemotherapy.
CONCLUSION
ES of the occipital region of the skull is an extremely rare location. It reaches adolescents and radical surgical resection is the mainstay of treatment. Adjuvant radiotherapy and chemotherapy has been shown to improve patient survival.
Footnotes
How to cite this article: Elmi SM, Mouhssani M, Ontsi Obame F, Imbunhe N, El Asri AC, Gazzaz M. Primary Ewing’s sarcoma of the occipital bone: A case report and review of the literature. Surg Neurol Int 2023;14:309.
Contributor Information
Saad Moussa Elmi, Email: saad.elmi@yahoo.com.
Mohamed Mouhssani, Email: simomouha00@gmail.com.
Fresnel Lutèce Ontsi Obame, Email: ontsiobamef1@gmail.com.
Napoleão Imbunhe, Email: imbunhe@gmail.com.
Abad Cherif El Asri, Email: abad20031@hotmail.com.
Miloudi Gazzaz, Email: gmiloneuro@yahoo.fr.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Desai KI, Nadkarni TD, Goel A, Muzumdar DP, Naresh KN, Nair CN. Primary Ewing’s sarcoma of the cranium. Neurosurgery. 2000;46:62–8. discussion 68-9. [PubMed] [Google Scholar]
- 2.Freeman MP, Currie CM, Gray GF, Jr, Kaye JJ. Ewing sarcoma of the skull with an unusual pattern of reactive sclerosis: MR characteristics. J Comput Assist Tomogr. 1988;12:143–6. [PubMed] [Google Scholar]
- 3.Garg A, Ahmad FU, Suri A, Mahapatra AK, Mehta VS, Atri S, et al. Primary Ewing’s sarcoma of the occipital bone presenting as hydrocephalus and blindness. Pediatr Neurosurg. 2007;43:170–3. doi: 10.1159/000098397. [DOI] [PubMed] [Google Scholar]
- 4.Hollody K, Kardos M, Grexa E, Meszaros I. Ewing’s sarcoma in the occipital bone. Case report. Acta Paediatr Hung. 1992;32:371–8. [PubMed] [Google Scholar]
- 5.Tournut P, Turjman F, Laharotte JC, Froment JC, Gharbi S, Duquesnel J. Primary Ewing’s sarcoma of the skull presenting as an acute surgical emergency. Childs Nerv Syst. 1994;10:193–4. doi: 10.1007/BF00301090. [DOI] [PubMed] [Google Scholar]
- 6.Yamashita Y, Kumabe T, Kobayashi T, Abiko H, Seki H, Yoshimoto T. Ewing’s sarcoma at the occipital bone presenting as acute epidural hematoma: A case report. No Shinkei Geka. 1997;25:567–71. [PubMed] [Google Scholar]
- 7.Yasuda T, Inagaki T, Yamanouchi Y, Kawamoto K, Kohdera U, Kawasaki H, et al. A case of primary Ewing’s sarcoma of the occipital bone presenting with obstructive hydrocephalus. Childs Nerv Syst. 2003;19:792–9. doi: 10.1007/s00381-003-0816-z. [DOI] [PubMed] [Google Scholar]
- 8.Zenke K, Hatakeyama T, Hashimoto H, Sasaki S, Manabe K. Primary Ewing’s sarcoma of the occipital bone--case report. Neurol Med Chir (Tokyo) 1994;34:246–50. doi: 10.2176/nmc.34.246. [DOI] [PubMed] [Google Scholar]


