Abstract
Background:
Rare cases of biconvex hematomas splitting the convexity dura mater were reported and denominated interdural hematoma (IDH). Due to their rarity, little is known about their radiological characteristics, and in most cases, their invasive management with craniotomy and dural membrane excision is unnecessary.
Case Description:
We report here a case of single burr-hole endoscopic evacuation of an IDH and its complete resolution after the 6-month follow-up imaging. The literature review reveals 11 reported cases of IDH. Most of them are male and the mean age is 65 years (range 51–90). Most of the reported IDHs were misdiagnosed as epidural hematoma or meningioma, and therefore, they have been managed invasively through craniotomy with dural excision. Diagnosis of the interdural nature was confirmed macroscopically during surgery in all cases and histology was reported for 6 cases. Image analysis found a double dural beak sign and biconvex shape on coronal planes, subarachnoid space enlargement at the collection extremities, and irregular thick inner wall as common radiological aspects of the IDH.
Conclusion:
IDH is a rarely reported and often misdiagnosed dural hematoma subtype. Its invasive treatment through craniotomy is likely related to its unknown radiological characteristics. We review and raise awareness about potentially unique radiological anatomy that could avoid unnecessary invasive treatment. Moreover, we report the first case of endoscopically evacuated IDH with long-term follow-up imaging showing complete resolution.
Keywords: Dural beak sign, Dural border cells, Endoscopic evacuation, Interdural hematoma, Radiological anatomy, Subdural hematoma
INTRODUCTION
Chronic subdural hematomas (SDHs) are classically described as crescent shape collections following the hemispheric convexity caused by venous bleeding from bridging veins and are commonly managed through burr-hole evacuation.[24,31,38] A widely maintained view is that this occurs in a vascularized bursa-like slit in the subdural space.[50] However, evidence indicates that SDH is actually formed by the accumulation of blood dissecting through the least resistant dural layer, namely, the dural border cell layer.[19,20,28] Consequently, if we do not consider the dural border cell layer as a unique separate meningeal layer, it is reasonable to claim that crescent-shaped SDH is being formed in between the layers of the dura mater rather than in a subdural space.
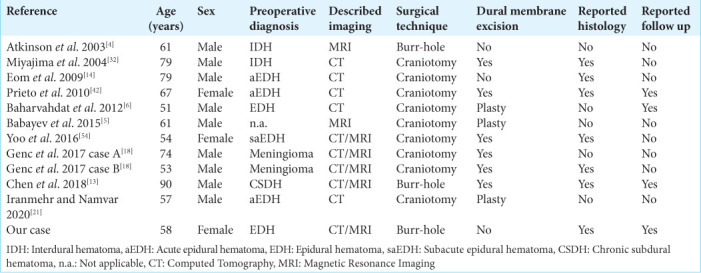
In fact, a minority of all diagnosed SDHs have a biconvex shape with sometimes a very distinct dural beak and 11 cases of such biconvex hematomas were reported in ten publications as being strictly encapsulated between the outer periosteal and the inner thick meningeal layers of the convexity dura mater and named therefore interdural hematoma (IDH) [Table 1].[2,4-6,10,13,14,18,21,30,32,41-43,54] In most of these cases, the collection was misdiagnosed as an epidural hematoma or a meningioma due to its biconvex shape and, therefore, managed invasively through a craniotomy with dural membrane excisions [Table 1].[5,6,14,18,21,32,42,54] The diagnosis of IDH was made intraoperatively after unexpectedly finding a dural layer under the skull and visualizing a thick opaque inner membrane covering the arachnoid membrane confirmed histologically as being of dural origin [Table 1]. Altogether, these observations strongly point to the existence of a convexity subdural/dural hematoma spectrum. Due to the sparse reports in the literature, the radiological semiology of the IDH has not yet been established and there is a lack of consensus about its optimal surgical management.
Table 1:
Patient, operative, and imaging parameters based on the literature review and both reported cases.
Here, we report a case of left convexity IDH that developed following a right subfrontal approach for the resection of a tuberculum sellae meningioma, successfully treated with an endoscopic evacuation. Furthermore, we performed a systematic literature review, with the aim to point out common radiological features that could lead to better identification of this hemorrhagic entity to avoid unneeded aggressive management.
MATERIALS AND METHODS
An electronic literature search in PubMed/MEDLINE, Scopus, Cochrane, and Embase was conducted. The search was done using the term “interdural hematoma.” The literature search strategy was designed to identify all articles in the English language describing cases of adult patients with IDH or cases of biconvex SDH. Moreover, we conducted literature research on the subject of SDH using the term “subdural hematoma” and “subdural hematoma classification(s).” The reference lists in all the identified relevant articles were manually screened for additional relevant references.
RESULTS
Case report
The case is a sexagenarian female operated on for a tuberculum sellae meningioma via a right frontobasal craniotomy with a Simpson grade II resection. The operation was uneventful, and the patient was discharged on postoperative day 5 in stable condition. On the 3-month follow-up, brain magnetic resonance imaging (MRI) revealed a newly formed extra-axial contralateral left convexity hematoma [Figure 1]. It was initially identified as an epidural hematoma by the radiologist; however, after carefully reviewing the images, the diagnosis of IDH was evoked. Endoscopic burr-hole evacuation of SDH was already confirmed in the literature as a safe approach as it gives better direct visual control,[11,22] we, therefore, decided to use the endoscope for this suspected IDH.
Figure 1:
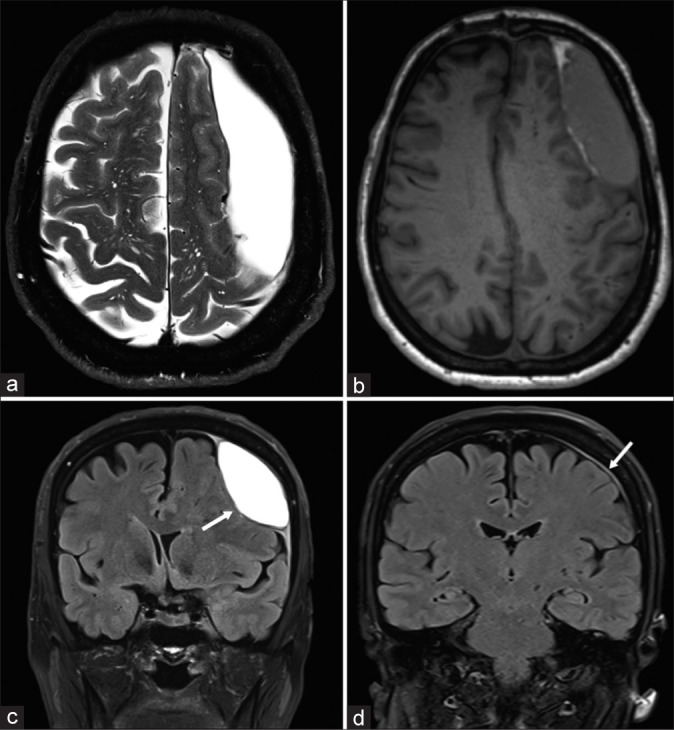
Illustrative case no. 1 of interdural hematoma. (a) Preoperative T2-weighted axial magnetic resonance imaging (MRI); (b) preoperative T1-weighted axial MRI; (c) preoperative T2 fluid attenuated inversion recovery (FLAIR) coronal MRI showing the biconvex lentiform hematoma (white arrow); and (d) 6 months postoperative T2 FLAIR coronal MRI showing the complete resolution of the collection with a slight residual dural thickening (white arrow). Notice the irregular thick inner wall of the hematoma (a). Notice the dural thickening at both dural edges (dural beak sign) indicating dural splitting and the slight subarachnoid space enlargement (c).
Imaging characteristics
On the MRI, the collection was localized over the frontoparietal convexity and was crossing the sutures like a SDH [Figures 1a and b]. It was, however, biconvex on coronal sections and enlarging the subarachnoid space at its dural base like an epidural hematoma [Figure 1c]. Contrary to the epidural and SDH, its inner convexity was irregular on axial images, and a dural tail or dural beak was visible both at its base rostrally and caudally on coronal images [Figures 1a-d]. The outer and inner membranes were enhanced on contrast administration indicating an inflammatory wall. The inner wall was spontaneously hyperintense on T1 sequences suggesting subacute bleeding [Figure 1b]. The content of the collection was isointense on T1 and hyperintense on T2 sequences suggesting old blood of more than 2–3 weeks [Figures 1a and b].
Surgical details
Although the patient was asymptomatic, due to the size of the collection, the midline shift, and its epidural localization, we decided to evacuate the collection. With the aid of neuronavigation (Medtronic Stealth Navigation), a single burr-hole centered on the outer convexity of the hematoma was performed. After drilling the bone, an intact dural membrane was found excluding its epidural origin. After coagulation and incision of the dura, a thin classically looking grayish hematoma membrane was identified. Piercing this membrane resulted in the outflow of a liquid that had a typical chronic blood aspect often described as “motor oil.” After rinsing profusely with saline, the cavity was explored with the help of the neuroendoscope (Karl Storz). An opaque dura-like thick yellowish hemorrhagic membrane was observed under direct vision with irregular darker yellowish spots smoothly in continuity with all of its walls like a proper dural pocket [Figure 2a]. With the help of a micro-blade and forceps, an infracentimetric piece of the inner membrane was sharply dissected and sent for histopathological analysis [Figure 2b]. After widening this incision through the inner membrane, a thin transparent membrane with visible vessels under it was identified as the arachnoid membrane, confirming the interdural anatomical origin of the hematoma [Figure 2b].
Figure 2:
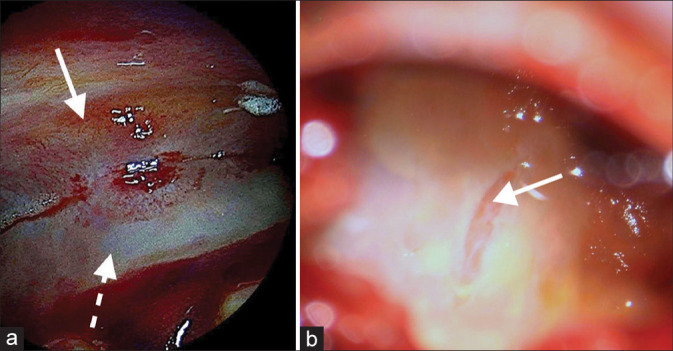
Intracranial, interdural endoscopic pictures taken through a single burr-hole, after hematoma evacuation from case no. 1. (a) Image showing the dural splitting from the inside of the hematoma pocket at the dorsomedial apex (dashed white arrow points to the inner dural layer and solid white arrow to the outer dural layer). (b) Image of the inner wall after dural biopsy, revealing the transparent thin arachnoid membrane (solid white arrow).
Histopathological findings
Histopathological examination confirmed the dural origin of the sampled tissue piece coming from the thick inner membrane of the hematoma. Mature fibroblasts and extracellular collagen were visualized [Figure 3].
Figure 3:
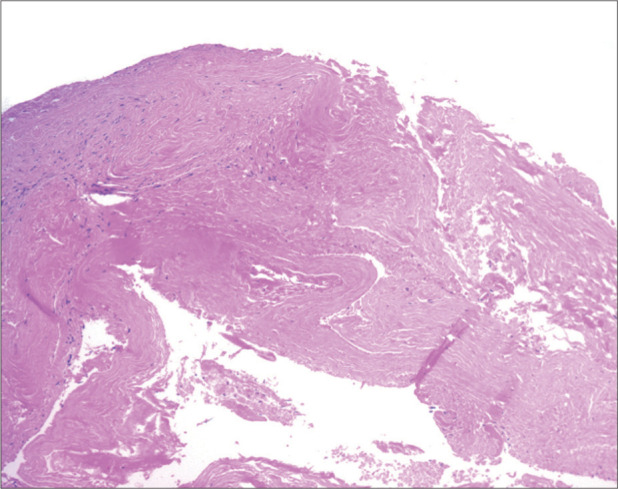
The histological examination of the inner wall showed a dense fibrous tissue, with low cellularity, compatible with dura mater (H&E staining: ×10).
Follow-up
The 6-month follow-up MRI showed complete resolution of the hematoma with no residual collection [Figure 1d]. Clinically, the patient was asymptomatic.
DISCUSSION
We report here a rare case of successfully treated biconvex hematoma splitting the convexity dura compatible with an IDH. The nomenclature of IDH should be used carefully as this diagnosis relies on specific radiological patterns and the confirmation that the inner wall of the hematoma is of dural origin.[4-6,13,14,18,21,32,42,54] After reviewing the literature, we have identified the biconvex shape, the dural beak sign on the coronal plane, as well as the irregular thick inner wall as potential unique radiological characteristics of the IDH [Figure 1]. The IDH is a chimeric radiological entity as it is biconvex like the epidural hematoma but crosses the suture on the rostrocaudal axis like a SDH. The case described, herein, illustrates the important role of minimally invasive approaches for the treatment of IDH, as opposed to most of the reported IDH cases that were managed more invasively through a craniotomy due to the misdiagnosis [Table 1].[4-6,13,14,18,21,32,42,54] Unfortunately, the low number of reported cases and the lack of follow-up imaging precludes the discussion aiming at better recognizing this radiological anatomy, understanding the physiopathology, and defining optimal surgical management.
Physiopathology
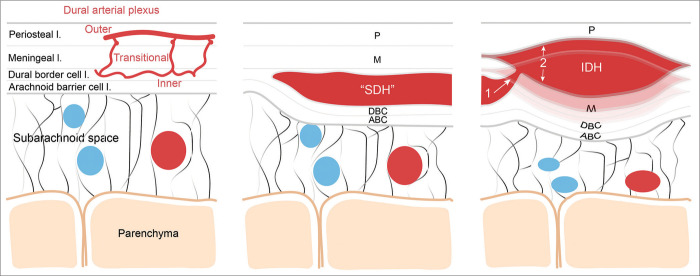
The dura mater has long been considered as an avascular, metabolically rather inactive tissue.[1] However, recent anatomical observations point to a highly rich arterial supply from the meningeal arteries traversing the dural layers from superficial to deep layers and anastomosing with a complex arteriovenous plexus in the deep dural layers.[1,47] In contrary to the general belief, the dura mater at the level of the cranium is composed of three layers, the endosteal or periosteal layer, the meningeal layer, and the deeply sitting border cell layer [Figure 4].[1,19,28,34] All three layers have their respective vascular network: the outer, the transitional and the inner plexus, and the latter having the densest inner capillary network [Figure 4].[47] The dural border cell layer, first described by Nabeshima et al.,[34] is composed of flattened fibroblasts firmly attached to the most superficial arachnoid layer called the barrier cell layer. These cells are loosely attached through tight junctions to the meningeal layer in line with its putative role in matching brain size changes during life [Figure 4].[17,34,40,46] In 1991, Duane Haines et al. carried out electron microscopic and histological investigations of the SDH and concluded that the bursa-like subdural space, as described before, does not exist and proposed that the SDH is actually formed by the accumulation of blood dissecting through the least resistance dural layer, namely, the dural border cell layer [Figure 4].[19,20,28] Consequently, if we do not consider the dural border cell layer as a unique separate meningeal layer, it is reasonable to claim that the SDH is being formed in between the layers of the dura mater rather than in a subdural space [Figure 4].
Figure 4:
Schematic representation of the putative pathophysiological mechanisms leading to the formation of the interdural hematoma. Left, schematic illustrating the normal meningeal layer microanatomy including the dural arterial plexus (layer thickness is not scaled). From external to internal meningeal layer: the periosteal layer (P), the meningeal layer (M), the dural border cell layer (DBC), and the arachnoid barrier cell layer (ABC); middle, illustration of the microanatomical localization of the classic subdural hematoma contained by the DBC; Right, the putative mechanism leading to the formation of the IDH through higher pressure blood dissecting more superficially the dural layers from the vascularized inner DBC layer. SDH: Subdural hematoma, IDH: Interdural hematoma.
The precise pathophysiological events leading to the IDH and whether the crescent shape hematoma has any link to the biconvex IDH remains unknown. The accumulation of blood between the border cell and meningeal dural layers from ruptured bridging veins traversing the dura is not the only mechanism responsible for the formation of the crescent shape SDH hematoma.[24,26] Chronic SDH is believed to derive from a prolonged interaction between the dural layers and leaking cerebrospinal fluid (CSF) into the pachymeninges, leading to the hemorrhagic transformation of a hygroma or the slow “chronicization” of subdural blood oozing compatible with degenerative vascular and inflammatory changes of the cerebrovasculature.[24,47] In addition, the chronic healing process of a traumatic SDH including inflammatory events, neovascularization, neomembrane formation, and volumetric growth[13,25,26,35,44,53] may also contribute to this process. An intriguing possibility is that dural splitting observed in cases of IDH is due to accumulating blood with greater pressure continuing toward the superficial periosteal layer, possibly following the dural vascular channels [Figure 4].[13,21,30] Supporting this hypothesis, we found two articles linking the nature of bleeding with the hematoma shape. A more focal shape was associated preferentially with arterial bleeding and a crescent-shaped hematoma was more prevalent in cases of identified venous bleeding.[29,43] The case of IDH we report here gives further support to this idea, since the IDH appeared in the span of a few months, in a patient already operated on and only lightly symptomatic. Thus, biconvex IDH hematoma may start after a small rapid high-pressure arterial bleeding splitting a possibly inflamed/injured dura directly between the periosteal and meningeal layers or forms from the dissection starting at the dural border cell layer to more superficial layers [Figure 4]. It is therefore plausible that the IDH takes first the form of a crescent shape SDH before accumulating bleeding shapes out of the biconvex aspect of the IDH by putting the meningeal dura under tension [Figure 4].
It is of interest to note that a meningeal space between the meningeal and periosteal dura, named the interperiosteodural space, part of the extradural neural axis compartment was anatomically demonstrated at the level of the cavernous sinus and its continuity toward the foramen magnum, at the dural folds of the jugular foramen, and the level of the falx cerebri.[7,9,15,51] A few reports suggest the existence of a transdural passage, and absorption of CSF is observed at the level of the falx cerebri and tentorium.[28,51] This could explain the high physiological prevalence of CSF in subdural collections. In addition, middle meningeal artery embolization leading to hematoma resolution suggests the existence of not yet identified transdural resorption pathways.[47] Whether such interdural space may variably exist among the population at the level of the convexity dura, participating in the formation of the IDH remains to be demonstrated.
Radioanatomical characteristics
As IDH is a rare and most likely underdiagnosed entity, its radiological features are undefined. Small IDH takes rather the form of the described “Chinese dumpling,” while the more extended frontoparietal convexity IDH as reported by Chen et al. and including our case could be described as uniquely chimeric.[13] Indeed, on coronal images, they have a biconvex shape similar to an epidural hematoma, but they cross the cranial sutures like a SDH on axial images [Figure 1]. On the other hand, they have unique characteristics including an irregular inner convexity thick wall easily visualized on axial images and a very distinct dural thickening or double dural beak sign mostly visible on coronal planes indicating dural splitting [Figure 1]. Moreover, contrary to classic SDHs, they enlarge the subarachnoid space on their borders as they push the brain at their convexity away from the arachnoid membrane still attached to the dura by putting the dura under tension similarly to the epidural hematoma instead of smoothly following the convexity surface like a classic subdural collection would do [Figure 1]. These radioanatomical characteristics strongly support the interdural layer anatomical localization of the hematoma. The aforementioned radiological characteristics were confirmed on most MRIs in those cases where additional imaging was performed.[4-6,13,14,18,21,32,35,42]
Attempts were made to subclassify chronic SDH based on its internal radiological anatomy and volumetry at the moment of diagnosis and during its aging with the aim to define predicting factors of its recurrence, among them the Oslo Grading System.[3,8,35-37,48] Radioanatomical analysis of the shape of the SDH was however rarely reported or analyzed and likely explains also why biconvex SDHs and among them, IDH are rarely recognized or reported.[29,43] In addition, some of the previously reported cases and the case of the present work were spotted incidentally on an MRI scan on which the radioanatomical characteristics of the IDH are better defined in comparison to multiplanar computed tomography (CT) scan which remains the gold standard imaging for SDH. Finally, the dural beak sign, probably the most specific radiological characteristic of IDH, is not very defined on CT scan, also likely accounting for the low number of reported cases of IDH.
Surgical management
The optimal surgical management of IDHs is unknown. Likely related to its biconvex shape, more than half of the reported IDH cases, especially the small ones putting the dural layers under tension, were misdiagnosed as an epidural hematoma or a solid tumor and, therefore, managed invasively through a craniotomy [Table 1].[5,6,14,18,21,32,42,54] Only three cases including the one reported here were managed surgically through burr holes [Table 1].[4,13] Compared to the classic SDH, its propensity for recurrence is unknown and, in most cases, an invasive dural resection or dural membrane suturing was performed with the aim to reduce recurrence [Table 1].[4-6,13,14,18,21,32,42,54] Dural suturing was performed in three cases and dural wall excision was performed in five cases [Table 1]. The case reported by Chen et al. is an example of the utilization of such a dural resection resolving a recurrent IDH.[13] However, similarly to chronic SDH for which membranectomy is debated, no conclusion can be made on the necessity of such an aggressive surgical management as for most of the IDH cases less than half of them reported postoperative imaging and outcome [Table 1].[23,45,52] For the case reported here, we observed a complete resolution at the 6-month follow-up after endoscopic assisted single burr-hole evacuation with complete brain re-expansion [Figure 1c]. Evacuating the proinflammatory blood collection strictly encapsulated in the pachymeninges certainly could promote both vascularized dural layers to rapidly fuse again and account for its complete resolution after a few months. In comparison, complete resolution of chronic SDHs and brain re-expansion are reported to take several months to a year.[12,39] This difference could also be related to the prolonged contact between the proinflammatory blood and the dural border cell – arachnoid barrier cell junction leading to dural border cell proliferation, neovascularizations, and solidification of these membranes slowing down brain re-expansion in cases of chronic SDH formed in between the dural border cell layer.[13,16,17,27,46,49]
CONCLUSION
The evident radioanatomical heterogeneity in the shape of the SDH argues against its simple monotype definition. Accumulating observations strongly suggest the existence of a convexity “dural” hematoma spectrum based on its shape, likely related to the amount of dural splitting caused by the hematoma. Early laboratory SDH models pointed out the splitting of the dural border cell layer as a pathophysiological mechanism for the crescent shape SDH.[17,19,46,47,33] In addition, recent evidence showing the existence of blood collections splitting the convexity dura and having unique radiological anatomy strongly supports the existence of an IDH differing from the crescent shape SDH.[4-6,13,14,18,21,32,42,54] IDH is likely formed when bleeding from a dural vascular plexus splits the dura more superficially in two distinct thick layers progressively putting under tension the meningeal dural layer shaping out a biconvex hematoma [Figure 4].[13,21,30] IDH should be kept in the differential diagnosis in cases of convexity collection combining a thick irregular inner wall on axial images with subarachnoid space enlargement at its anterior and posterior apex, and biconvex shape associated with a double dural beak sign on coronal images [Figure 1]. Endoscopic single burr- or two burr-hole craniostomy evacuations of IDH is a safe procedure and it is associated with rapid and complete resolution in a few months. This rapid postoperative resolution of the IDH may be related to its encapsulated localization between the thick meningeal and periosteal dural layers keeping it from triggering inflammatory responses in contact with the dural border cell layer avoiding osmotic volumetric growth and neovascularization characterizing chronic recurrent SDHs. Raising awareness about the unique radiological anatomy of the IDH will help to better identify it and to better understand its nature and prognosis in case of surgery. Future studies exploring the prevalence of the biconvex dural hematoma, putatively compatible with an IDH, would bring additional insights.
Ethics
All procedures performed were in accordance with the 1964 Helsinki Declaration and its later amendments.
Footnotes
How to cite this article: Kiss-Bodolay D, Papadimitriou K, Hedjoudje A, Duc C, Vargas MI, Kiss JZ, et al. The interdural hematoma: A subtype of convexity subdural/dural hematoma with specific radioanatomical characteristics. Surg Neurol Int 2023;14:316.
Contributor Information
Daniel Kiss-Bodolay, Email: daniel.kiss.b@gmail.com.
Kyriakos Papadimitriou, Email: kpapademetriou1@gmail.com.
Abderrahmane Hedjoudje, Email: a.hedjoudje@gmail.com.
Christophe Duc, Email: christophe.duc@hotmail.ch.
Maria Isabel Vargas, Email: maria.i.vargas@hcuge.ch.
Jozsef Zoltan Kiss, Email: jozsef.kiss@unige.ch.
Karl Schaller, Email: karl.schaller@hcuge.ch.
Jean-Yves Fournier, Email: jean-yves.fournier@hopitalvs.ch.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The author(s) confirms that there was no use of Artificial Intelligence (AI)-Assisted Technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Adeeb N, Mortazavi MM, Tubbs RS, Cohen-Gadol AA. The cranial dura mater: A review of its history, embryology, and anatomy. Childs Nerv Syst. 2012;28:827–37. doi: 10.1007/s00381-012-1744-6. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal A. Bilateral biconvex frontal chronic subdural hematoma mimicking extradural hematoma. J Surg Tech Case Rep. 2010;2:90–1. doi: 10.4103/2006-8808.73625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alves JL, Santiago JG, Costa G, Pinto AM. A standardized classification for subdural hematomas-I. Am J Forensic Med Pathol. 2016;37:174–8. doi: 10.1097/PAF.0000000000000255. [DOI] [PubMed] [Google Scholar]
- 4.Atkinson JL, Lane JI, Aksamit AJ. MRI depiction of chronic intradural (subdural) hematoma in evolution. J Magn Reson Imaging. 2003;17:484–6. doi: 10.1002/jmri.10275. [DOI] [PubMed] [Google Scholar]
- 5.Babayev R, Ekşi MŞ. A blackhole over brain: Interdural hematoma-a challenging diagnosis. Neurol Neurochir Pol. 2015;49:189–92. doi: 10.1016/j.pjnns.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 6.Baharvahdat H, Etemadrezaie H, Zabihyan S, Dashti S, Ganjeifar B. Acute interdural hematoma mimicking epidural hematoma: A case report. Turk Neurosurg. 2012;22:368–70. doi: 10.5137/1019-5149.JTN.3556-10.2. [DOI] [PubMed] [Google Scholar]
- 7.Bartoli A, Kotowski M, Pereira VM, Schaller K. Acute spinal epidural hematoma and cranial interdural hematoma due to a rupture of a posterior communicating artery aneurysm: Case report. Neurosurgery. 2011;69:E1000–4. doi: 10.1227/NEU.0b013e318223bc0c. discussion E1004. [DOI] [PubMed] [Google Scholar]
- 8.Bechstein M, McDonough R, Fiehler J, Zanolini U, Rai H, Siddiqui A, et al. Radiological evaluation criteria for chronic subdural hematomas: Review of the literature. Clin Neuroradiol. 2022;32:923–9. doi: 10.1007/s00062-022-01138-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bernard F, Zemmoura I, Cottier JP, Fournier HD, Terrier LM, Velut S. The interperiosteodural concept applied to the jugular foramen and its compartmentalization. J Neurosurg. 2018;129:770–8. doi: 10.3171/2017.1.JNS161890. [DOI] [PubMed] [Google Scholar]
- 10.Braun J, Borovich B, Guilburd JN, Zaaroor M, Feinsod M, Grushkiewicz I. Acute subdural hematoma mimicking epidural hematoma on CT. AJNR Am J Neuroradiol. 1987;8:171–3. [PMC free article] [PubMed] [Google Scholar]
- 11.Cai Q, Guo Q, Zhang F, Sun D, Zhang W, Ji B, et al. Evacuation of chronic and subacute subdural hematoma via transcranial neuroendoscopic approach. Neuropsychiatr Dis Treat. 2019;15:385–90. doi: 10.2147/NDT.S193548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang CL, Sim JL, Delgardo MW, Ruan DT, Connolly ES., Jr Predicting chronic subdural hematoma resolution and time to resolution following surgical evacuation. Front Neurol. 2020;11:677. doi: 10.3389/fneur.2020.00677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen KT, Huang HC, Lin YJ, Chen MH, Hsieh TC. The relationship between hematoma and pachymeninges in an interdural hematoma: Diagnosis and surgical strategy. World Neurosurg. 2018;110:492–8.e3. doi: 10.1016/j.wneu.2017.11.040. [DOI] [PubMed] [Google Scholar]
- 14.Eom KS, Kim TY, Park JT. Contralateral acute interdural haematoma occurring after burr hole drainage of chronic subdural haematoma. Br J Neurosurg. 2009;23:213–5. doi: 10.1080/02688690802429202. [DOI] [PubMed] [Google Scholar]
- 15.François P, Travers N, Lescanne E, Arbeille B, Jan M, Velut S. The interperiosteo-dural concept applied to the perisellar compartment: A microanatomical and electron microscopic study. J Neurosurg. 2010;113:1045–52. doi: 10.3171/2010.1.JNS081701. [DOI] [PubMed] [Google Scholar]
- 16.Friede RL. Incidence and distribution of neomembranes of dura mater. J Neurol Neurosurg Psychiatry. 1971;34:439–46. doi: 10.1136/jnnp.34.4.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Friede RL, Schachenmayr W. The origin ofsubdural neomembranes. II. Fine structural of neomembranes. Am J Pathol. 1978;92:69–84. [PMC free article] [PubMed] [Google Scholar]
- 18.Genc A, Yilmaz MB, Egemen E, Yilmaz M, Sav AM. Interdural hematomas: An update of literature. J Neurosurg Sci. 2017;61:101–6. doi: 10.23736/S0390-5616.16.03238-0. [DOI] [PubMed] [Google Scholar]
- 19.Haines DE, Harkey HL, Al-Mefty O The. “subdural” space: A new look at an outdated concept. Neurosurgery. 1993;32:111–20. doi: 10.1227/00006123-199301000-00017. [DOI] [PubMed] [Google Scholar]
- 20.Haines DE. On the question of a subdural space. Anat Rec. 1991;230:3–21. doi: 10.1002/ar.1092300103. [DOI] [PubMed] [Google Scholar]
- 21.Iranmehr A, Namvar M. Traumatic acute convexity interdural hematoma: A case report and literature review. Br J Neurosurg. 2020;37:337–9. doi: 10.1080/02688697.2020.1749985. [DOI] [PubMed] [Google Scholar]
- 22.Kawasaki T, Kurosaki Y, Fukuda H, Kinosada M, Ishibashi R, Handa A, et al. Flexible endoscopically assisted evacuation of acute and subacute subdural hematoma through a small craniotomy: Preliminary results. Acta Neurochir (Wien) 2018;160:241–8. doi: 10.1007/s00701-017-3399-2. [DOI] [PubMed] [Google Scholar]
- 23.Kim JH, Kang DS, Kim JH, Kong MH, Song KY. Chronic subdural hematoma treated by small or large craniotomy with membranectomy as the initial treatment. J Korean Neurosurg Soc. 2011;50:103–8. doi: 10.3340/jkns.2011.50.2.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kolias AG, Chari A, Santarius T, Hutchinson PJ. Chronic subdural haematoma: Modern management and emerging therapies. Nat Rev Neurol. 2014;10:570–8. doi: 10.1038/nrneurol.2014.163. [DOI] [PubMed] [Google Scholar]
- 25.Lee KS, Bae WK, Doh JW, Bae HG, Yun IG. Origin of chronic subdural haematoma and relation to traumatic subdural lesions. Brain Inj. 1998;12:901–10. doi: 10.1080/026990598121972. [DOI] [PubMed] [Google Scholar]
- 26.Lee KS. History of chronic subdural hematoma. Korean J Neurotrauma. 2015;11:27–34. doi: 10.13004/kjnt.2015.11.2.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Liu H, Yan R, Xie F, Richard SA. Hematoma cavity separation and neomembrane thickness are potential triggers of recurrence of chronic subdural hematoma. BMC Surg. 2022;22:236. doi: 10.1186/s12893-022-01687-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mack J, Squier W, Eastman JT. Anatomy and development of the meninges: Implications for subdural collections and CSF circulation. Pediatr Radiol. 2009;39:200–10. doi: 10.1007/s00247-008-1084-6. [DOI] [PubMed] [Google Scholar]
- 29.Maxeiner H, Wolff M. Pure subdural hematomas: A postmortem analysis of their form and bleeding points. Neurosurgery. 2007;61(1 Suppl):267–72. doi: 10.1227/01.neu.0000279222.76375.d4. discussion 272-3. [DOI] [PubMed] [Google Scholar]
- 30.Miki S, Fujita K, Katayama W, Sato M, Kamezaki T, Matsumura A, et al. Encapsulated acute subdural hematoma mimicking acute epidural hematoma on computed tomography. Neurol Med Chir (Tokyo) 2012;52:826–8. doi: 10.2176/nmc.52.826. [DOI] [PubMed] [Google Scholar]
- 31.Miller JD, Nader R. Acute subdural hematoma from bridging vein rupture: A potential mechanism for growth. J Neurosurg. 2014;120:1378–84. doi: 10.3171/2013.10.JNS13272. [DOI] [PubMed] [Google Scholar]
- 32.Miyajima K, Hayashi N, Kurimoto M, Kuwayama N, Hirashima Y, Endo S. Idiopathic interdural hematoma looking like a “Chinese dumpling”--case report. Neurol Med Chir. 2004;44:75–6. doi: 10.2176/nmc.44.75. [DOI] [PubMed] [Google Scholar]
- 33.Moshayedi P, Liebeskind DS. Middle meningeal artery embolization in chronic subdural hematoma: Implications of pathophysiology in trial design. Front Neurol. 2020;11:923. doi: 10.3389/fneur.2020.00923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nabeshima S, Reese TS, Landis DM, Brightman MW. Junctions in the meninges and marginal glia. J Comp Neurol. 1975;164:127–69. doi: 10.1002/cne.901640202. [DOI] [PubMed] [Google Scholar]
- 35.Nagahori T, Nishijima M, Takaku A. Histological study of the outer membrane of chronic subdural hematoma: Possible mechanism for expansion of hematoma cavity. No Shinkei Geka. 1993;21:697–701. [PubMed] [Google Scholar]
- 36.Nakaguchi H, Tanishima T, Yoshimasu N. Factors in the natural history of chronic subdural hematomas that influence their postoperative recurrence. J Neurosurg. 2001;95:256–62. doi: 10.3171/jns.2001.95.2.0256. [DOI] [PubMed] [Google Scholar]
- 37.Nomura S, Kashiwagi S, Fujisawa H, Ito H, Nakamura K. Characterization of local hyperfibrinolysis in chronic subdural hematomas by SDS-PAGE and immunoblot. J Neurosurg. 1994;81:910–13. doi: 10.3171/jns.1994.81.6.0910. [DOI] [PubMed] [Google Scholar]
- 38.Nouri A, Gondar R, Schaller K, Meling T. Chronic Subdural Hematoma (cSDH): A review of the current state of the art. Brain Spine. 2021;1:100300. doi: 10.1016/j.bas.2021.100300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Nunta-Aree S, Paruang T, Sitthinamsuwan B. Timing of brain expansion and recurrence after surgery of chronic subdural hematoma. J Med Assoc Thai. 2017;100:S59–64. [Google Scholar]
- 40.Orlin JR, Osen KK, Hovig T. Subdural compartment in pig: A morphologic study with blood and horseradish peroxidase infused subdurally. Anat Rec. 1991;230:22–37. doi: 10.1002/ar.1092300104. [DOI] [PubMed] [Google Scholar]
- 41.Park SS, Shin WR, Kim HJ, Kwon CY. Encapsulated unresolved subdural hematoma mimicking acute epidural hematoma: A case report. Korean J Neurotrauma. 2014;10:142–5. doi: 10.13004/kjnt.2014.10.2.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Prieto R, Pascual JM, Subhi-Issa I, Yus M. Acute epidural-like appearance of an encapsulated solid non-organized chronic subdural hematoma. Neurol Med Chir (Tokyo) 2010;50:990–4. doi: 10.2176/nmc.50.990. [DOI] [PubMed] [Google Scholar]
- 43.Radcliffe WB, Guinto FC, Jr, Adcock DF, Krigman MR. Subdural hematoma shape: A new look at an old concept. Am J Roentgenol. 1972;115:72–7. doi: 10.2214/ajr.115.1.72. [DOI] [PubMed] [Google Scholar]
- 44.Sahyouni R, Goshtasbi K, Mahmoodi A, Tran DK, Chen JW. Chronic subdural hematoma: A historical and clinical perspective. World Neurosurg. 2017;108:948–53. doi: 10.1016/j.wneu.2017.09.064. [DOI] [PubMed] [Google Scholar]
- 45.Sahyouni R, Mahboubi H, Tran P, Roufail JS, Chen JW. Membranectomy in chronic subdural hematoma: Meta-analysis. World Neurosurg. 2017;104:418–29. doi: 10.1016/j.wneu.2017.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Schachenmayr W, Friede RL. The origin of subdural neomembranes. I. Fine structure of the dura-arachnoid interface in man. Am J Pathol. 1978;92:53–68. [PMC free article] [PubMed] [Google Scholar]
- 47.Shapiro M, Walker M, Carroll KT, Levitt MR, Raz E, Nossek E, et al. Neuroanatomy of cranial dural vessels: Implications for subdural hematoma embolization. J Neurointerv Surg. 2021;13:471–7. doi: 10.1136/neurintsurg-2020-016798. [DOI] [PubMed] [Google Scholar]
- 48.Stanišic M, Pripp AH. A reliable grading system for prediction of chronic subdural Hematoma recurrence requiring reoperation after initial burr-hole surgery. Neurosurgery. 2017;81:752–60. doi: 10.1093/neuros/nyx090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Tanaka Y, Ohno K. Chronic subdural hematoma-an up-to-date concept. J Med Dent Sci. 2013;60:55–61. [PubMed] [Google Scholar]
- 50.Talbert DG. The subdural myth: Space or place? Anat Physiol. 2016;6:1000242. [Google Scholar]
- 51.Tsutsumi S, Ono H, Ishii H, Yasumoto Y. Interdural high signal on CISS sequence: An alternative CSF pathway? Childs Nerv Syst. 2019;35:487–91. doi: 10.1007/s00381-018-04044-5. [DOI] [PubMed] [Google Scholar]
- 52.Unterhofer C, Freyschlag CF, Thomé C, Ortler M. Opening the internal hematoma membrane does not alter the recurrence rate of chronic subdural hematomas: A prospective randomized trial. World Neurosurg. 2016;92:31–6. doi: 10.1016/j.wneu.2016.04.081. [DOI] [PubMed] [Google Scholar]
- 53.Yamashima T, Yamamoto S. Clinicopathological study of acute subdural haematoma in the chronic healing stage. Clinical, histological and ultrastructural comparisons with chronic subdural haematoma. Neurochirurgia (Stuttg) 1984;27:98–105. doi: 10.1055/s-2008-1053668. [DOI] [PubMed] [Google Scholar]
- 54.Yoo M, Kim JS, Jin SC, Lee SI. Idiopathic interdural hematoma in adult: A case report. NMC Case Rep J. 2016;3:103–5. doi: 10.2176/nmccrj.cr.2015-0293. [DOI] [PMC free article] [PubMed] [Google Scholar]