Abstract
Background
Gasping during resuscitation has been reported as a favorable factor for out-of-hospital cardiac arrest. We examined whether gasping during resuscitation is independently associated with favorable neurological outcomes in patients with refractory ventricular fibrillation or pulseless ventricular tachycardia (VF/pVT) undergoing extracorporeal cardiopulmonary resuscitation ECPR.
Methods
Data from a 2014 study on advanced cardiac life support for ventricular fibrillation with extracorporeal circulation in Japan (SAVE-J), which examined the efficacy of ECPR for refractory VF/pVT, were analyzed. The primary endpoint was survival with a 6-month favorable neurological outcome in patients who underwent ECPR with or without gasping during resuscitation. Multivariate logistic regression analysis was performed to evaluate the association between gasping and outcomes.
Results
Of the 454 patients included in the SAVE-J study, data from 212 patients were analyzed in this study after excluding those with missing information and those who did not undergo ECPR. Gasping has been observed in 47 patients during resuscitation; 11 (23.4%) had a favorable neurological outcome at 6 months. Multivariate logistic regression analysis showed that gasping during resuscitation was independently associated with a favorable neurological outcome (odds ratio [OR], 10.58 [95% confidence interval (CI) 3.22–34.74]). The adjusted OR for gasping during emergency medical service transport and on arrival at the hospital was 27.44 (95% CI 5.65–133.41).
Conclusions
Gasping during resuscitation is a favorable factor in patients with refractory VF/pVT. Patients with refractory VF/pVT with continuously preserved gasping during EMS transportation to the hospital are expected to have more favorable outcomes.
Supplementary Information
The online version contains supplementary material available at 10.1186/s40560-023-00692-1.
Keywords: Gasping, Sign of life, Cardiopulmonary resuscitation, Extracorporeal cardiopulmonary resuscitation, Out-of-hospital cardiac arrest
Background
Despite the accumulating knowledge on cardiopulmonary resuscitation (CPR) over the past decade, survival rates with favorable neurological function to discharge from the hospital remain noticeably low in out-of-hospital cardiac arrest (OHCA), which range from 5% to 10% [1, 2]. The prognosis of OHCA in patients who do not respond to the usual advanced cardiac life support (ACLS) is even poorer [3, 4]. For refractory cardiac arrest, in which spontaneous circulation is not restored despite ACLS, extracorporeal CPR (ECPR) is a rescue therapy expected to contribute to improved outcomes by reducing ischemic brain damage and providing time to identify and treat the underlying reversible causes of cardiac arrest [5, 6]. Although the results of a systematic review, including three recent randomized controlled trials on ECPR, suggest a potential benefit of ECPR, the level of evidence remains low [7–10].
Several reports have shown that signs of life during resuscitation are associated with favorable neurological outcomes for patients with OHCA undergoing ECPR [11–14]. Some studies have reported that the presence of gasping, considered a sign of life, predicts the outcome in patients with OHCA [15–18]. However, previous reports on the usefulness of signs of life, including gasping in ECPR cases, have been limited to reports, wherein the criteria for ECPR were unclear or differed between the periods covered within the study [11, 12]. Thus, whether there is an association between the presence of signs of life and outcomes in patients with refractory OHCA undergoing ECPR remains unclear. A multicenter prospective observational study, SAVE-J, was published in 2014 and provides clear criteria for ECPR implementation for refractory ventricular fibrillation or pulseless ventricular tachycardia (VF/pVT) [19]. Patient information on gasping was collected before and on hospital arrival in the SAVE-J study. We believe that using the SAVE-J data with clear criteria for ECPR implementation to examine the value of gasping as a prognostic factor in ECPR will allow for a more focused discussion of case selection for indicating ECPR with less heterogeneity. The primary aim of this study was to examine whether gasping during resuscitation is independently associated with favorable neurological outcomes in patients with refractory VF/pVT undergoing ECPR.
Methods
Study design
Data from the SAVE-J study, which prospectively examined the effect of ECPR on neurological outcomes in patients with refractory OHCA whose initial cardiac rhythm showed VF/pVT between September 8, 2008, and September 30, 2011 [19], were used in this study. Each participating institution was divided into ECPR-performing and non-ECPR-performing institutions, and no randomization was performed. Twenty-two institutions were enrolled in the ECPR group, and 17 institutions in the conventional CPR group. The SAVE-J study collected general prognostic indicators of OHCA and the presence or absence of gasping before and on arrival at the hospital. No information was collected on prehospital advanced airway management in the study. Details of the collective data and resuscitative strategies in the ECPR/CCPR group are available in published data [19].
The SAVE-J study was registered with the University Hospital Medical Information Network Clinical Trials Registry and the Japanese Clinical Trial Registry (registration number: UMIN000001403). This secondary analysis of de-identified data was approved by the Institutional Review Board of Sapporo Medical University Hospital (approval number: 342-163). The requirement for patient consent was waived because of the anonymized data provided in the sub-analysis of the SAVE-J study. The procedures were performed in accordance with the Declaration of Helsinki.
Patients
Patients enrolled in the SAVE-J study met the following criteria: (1) VF/pVT on the initial cardiac rhythm; (2) cardiac arrest on hospital arrival with or without pre-hospital restoration of spontaneous circulation (ROSC); (3) less than 45 min from the reception of the emergency call or onset of cardiac arrest to hospital arrival; and (4) no ROSC at least during the 15 min after hospital arrival (or after contact with a doctor), even though conventional CPR was performed. Patients excluded in the SAVE-J study were as follows: (a) those aged ≤ 20 years or ≥ 75 years; (b) poor level of activities of daily living before the onset of cardiac arrest; (c) cardiac arrest etiology of non-cardiac origin (e.g., external factors, such as trauma and drug intoxication, primary cerebral disorders, acute aortic dissection diagnosed before the introduction of ECMO, and terminal phase of cancer); (d) core body temperature of < 30 °C; and (e) no informed consent from the individuals representing patients.
Outcomes
The primary endpoint was survival with a 6-month favorable neurological outcome in patients undergoing ECPR, with or without gasping during resuscitation, evaluated using the cerebral performance category (CPC) [20]. A CPC score of 1–2 and 3–5 was regarded as favorable and unfavorable, respectively. The secondary endpoint was survival with a 6-month favorable neurological outcome in all patients with refractory VF/pVT, regardless of the presence or absence of gasping during resuscitation.
Statistical analysis
Continuous variables are presented as median (interquartile range) and were compared using the Mann–Whitney U test. Categorical variables were compared using Fisher’s exact test. Multivariate logistic regression analysis using stepwise forward variable selection was performed to evaluate the association between gasping and outcomes. The candidate variables for multivariate logistic regression analysis using stepwise forward variable selection were age, sex, incidence of witnessed cardiac arrest, bystander CPR attempts, timing of cardiac arrest, epinephrine administration before arrival, ROSC during transportation, time from cardiac arrest to admission, cardiac rhythm at admission, epinephrine administration after arrival, gasping during resuscitation, therapeutic temperature management, intra-aortic balloon pumping, percutaneous coronary intervention, and time from admission to ECMO pump. All statistical analyses were conducted using SPSS Statistics version 25 (IBM Corp., Armonk, NY, USA) and EZR (Saitama Medical Centre, Jichi Medical University, Saitama, Japan), a graphical user interface for R (R Foundation for Statistical Computing, Vienna, Austria). All the tests were two-sided. A p value < 0.05 was considered statistically significant.
Results
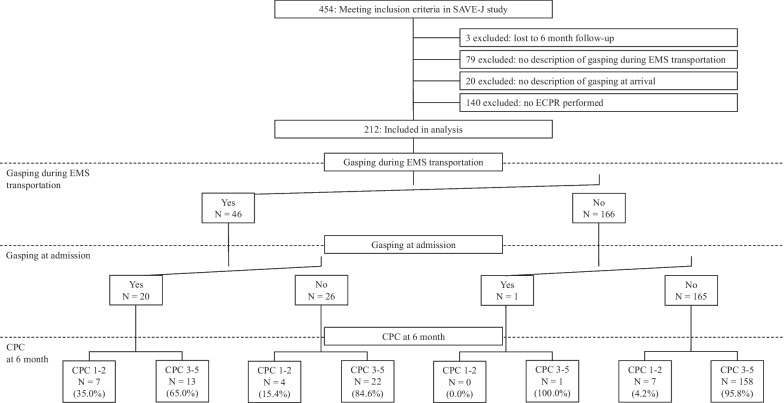
Of the 454 patients included in the SAVE-J study, 212 were enrolled. Three patients with unknown 6-month outcomes, 79 patients with unknown existence of gasping during emergency medical service (EMS) transport, 20 patients with unknown existence of gasping on hospital arrival, and 140 patients who did not undergo ECPR were excluded. Figure 1 shows the outcomes of each of the four groups according to the presence or absence of gasping during EMS transport and on arrival at the hospital. The acquisition rate of favorable neurological outcomes was 35% in patients with gasping during EMS transport and on arrival at the hospital.
Fig. 1.
Patient enrollment, timing of gasping, and outcomes in ECPR group. EMS emergency medical service, ECPR extracorporeal cardiopulmonary resuscitation, CPC cerebral performance category
A comparison of the characteristics of patients with or without gasping during resuscitation is shown in Table 1. Cases with gasping during resuscitation had more patients who developed cardiac arrest during EMS transport, had cardiac arrest rhythm as VF/pVT on hospital arrival, had favorable neurological outcomes, and had 6-month survival. A comparison of the neurological outcomes in patients undergoing ECPR is shown in Additional file 1. The presence of gasping at any time during resuscitation is associated with favorable neurological outcomes.
Table 1.
Comparison between patients who underwent ECPR with and without gasping during resuscitation
| Presence of gasping during resuscitation | Absence of gasping during resuscitation | p value | |
|---|---|---|---|
| n = 47 | n = 165 | ||
| Age (years), median [IQR] | 58 [48, 65] | 59 [48, 64] | 0.678 |
| Sex (female), n (%) | 5 (10.6) | 14 (8.5) | 0.772 |
| Witnessed cardiac arrest, n (%) | 39 (83.0) | 118 (71.5) | 0.133 |
| Bystander CPR attempt, n (%) | 0.123 | ||
| Yes | 28 (59.6) | 78 (47.3) | |
| No | 18 (38.3) | 86 (52.1) | |
| Unknown | 1 (2.1) | 1 (0.6) | |
| Occurrence of cardiac arrest during EMS activity, n (%) | 4 (8.5) | 3 (1.8) | 0.045 |
| Epinephrine administration before hospital arrival, n (%) | 0.879 | ||
| Yes | 22 (46.8) | 76 (46.1) | |
| No | 24 (51.1) | 81 (49.1) | |
| Unknown | 1 (2.1) | 8 (4.8) | |
| ROSC during EMS transportation, n (%) | 0.643 | ||
| Yes | 11 (23.4) | 29 (17.6) | |
| No | 34 (72.3) | 127 (77.0) | |
| Unknown | 2 (4.3) | 9 (5.5) | |
| Time from cardiac arrest to admission, median [IQR] | 33 [23, 41] | 31 [26, 38] | 0.951 |
| Cardiac rhythm at admission, n (%) | 0.002 | ||
| VF of pulseless VT | 38 (80.9) | 86 (52.1) | |
| PEA | 4 (8.5) | 38 (23.0) | |
| Asystole | 5 (10.6) | 41 (24.8) | |
| Epinephrine administration after hospital arrival, n (%) | 0.542 | ||
| Yes | 40 (85.1) | 128 (77.6) | |
| No | 7 (14.9) | 36 (21.8) | |
| Unknown | 0 (0.0) | 1 (0.6) | |
| Time from arrival to ECMO pump on, median [IQR] | 22 [17, 37] | 23 [17, 33] | 0.869 |
| Outcome at 6 months | |||
| CPC 1–2, n (%) | 11 (23.4) | 7 (4.2) | < 0.001 |
| Survival, n (%) | 15 (31.9) | 23 (13.9) | 0.009 |
IQR interquartile range, CPR cardiopulmonary resuscitation, ROSC return of spontaneous circulation, EMS emergency medical service, VF ventricular fibrillation, VT ventricular tachycardia, PEA pulseless electrical activity, ECMO extracorporeal membrane oxygenation, CPC cerebral performance
Association between neurological outcome and gasping in patients undergoing ECPR
Multivariate logistic regression analysis showed that gasping during resuscitation was independently associated with a favorable neurological outcome (odds ratio [OR], 10.58 [95% confidence interval (CI) 3.22–34.74]), after adjusting for age, ROSC during EMS transportation, and therapeutic temperature management (Table 2). Table 3 shows the unadjusted and adjusted ORs of favorable neurological outcomes with gasping during EMS transportation and/or on hospital arrival, with no gasping as the reference. The adjusted ORs for the presence of gasping either during EMS transport or on arrival at the hospital, or both, were 4.97 (95% CI 1.11–22.39) and 27.44 (95% CI 5.65–133.41), respectively.
Table 2.
Logistic regression analysis of prognostic factors for favorable neurological outcomes in ECPR patients
| Variables | Unadjusted OR (95% CI) | p value | Adjusted OR (95% CI) | p value |
|---|---|---|---|---|
| n = 212 | n = 207* | |||
| Age (years) | 0.95 (0.91–0.99) | 0.006 | 0.93 (0.89–0.97) | 0.002 |
| Female sex | 4.95 (1.54–15.87) | 0.007 | ||
| witnessed cardiac arrest | 1.25 (0.39–3.97) | 0.707 | ||
| Bystander CPR attempt | ||||
| Yes | 3.50 (1.10–11.10) | 0.034 | ||
| No | 1.00 (Ref.) | 0.030 | ||
| Unknown | 25.00 (1.31–475.97) | 0.032 | ||
| Occurrence of cardiac arrest during EMS activity | 1.84 (0.21–16.21) | 0.582 | ||
| Epinephrine administration before hospital arrival | ||||
| Yes | 1.59 (0.58–4.36) | 0.367 | ||
| No | 1.00 (Ref.) | 0.642 | ||
| Unknown | 1.75 (0.19–16.05) | 0.621 | ||
| ROSC during transportation | ||||
| Yes | 0.25 (0.03–1.95) | 0.186 | 0.17 (0.02–1.74) | 0.135 |
| No | 1.00 (Ref.) | 0.240 | 1.00 (Ref.) | 0.041 |
| Unknown | 2.16 (0.43–10.95) | 0.351 | 8.13 (1.02–64.67) | 0.048 |
| Time from cardiac arrest to admission | 0.96 (0.92–1.01) | 0.104 | ||
| Cardiac rhythm at admission | ||||
| VF of pulseless VT | 1.00 (Ref.) | 0.372 | ||
| PEA | 0.34 (0.07–1.53) | 0.160 | ||
| Asystole | 0.00 (0.00-) | 0.997 | ||
| Epinephrine administration after hospital arrival | ||||
| Yes | 1.31 (0.36–4.74) | 0.683 | ||
| No | 1.00 (Ref.) | 0.920 | ||
| Unknown | 0.00 (0.00-) | 1.000 | ||
| Gasping during resuscitation | 6.90 (2.50–19.02) | < 0.001 | 10.58 (3.22–34.74) | < 0.001 |
| Therapeutic temperature management | ||||
| Yes | 1.00 (Ref.) | 1.000 | 1.00 (Ref.) | 1.000 |
| No | 0.00 (0.00–) | 0.997 | 0.00 (0.00–) | 0.997 |
| Unknown | 0.00 (0.00–) | 1.000 | 0.00 (0.00–) | 1.000 |
| Intra-aortic balloon pumping | ||||
| Yes | 1.99 (0.44–9.02) | 0.374 | ||
| No | 1.00 (Ref.) | 0.673 | ||
| Unknown | 0.00 (0.00–) | 0.999 | ||
| Percutaneous coronary intervention | ||||
| Yes | 0.66 (0.24–1.80) | 0.414 | ||
| No | 1.00 (Ref.) | 0.486 | ||
| Unknown | 2.30 (0.23–22.63) | 0.475 | ||
| Time from admission to ECMO pump ona | 0.98 (0.95–1.03) | 0.436 | ||
Multivariate logistic analysis by replacing the variable "Therapeutic temperature management" with "Bystander CPR attempt" were also performed. The statistical significance of "Gasping during resuscitation" was similar. The result is shown in Additional file 10
ECPR extracorporeal cardiopulmonary resuscitation, OR odds ratio, CI confidence interval, CPR cardiopulmonary resuscitation, EMS emergency medical service, ROSC return of spontaneous circulation, VF ventricular fibrillation, VT ventricular tachycardia, PEA pulseless electrical activity, ECMO extracorporeal membrane oxygenation, Ref. reference
aFive data points were missing from admission to ECMO pump onset; thus, the multivariate analysis included 207 participants
Table 3.
Odds ratios of neurological outcomes according to the recognition timing of gasping based on the absence of gasping in ECPR patients
| Unadjusted OR (95% CI) | p value | Adjusted OR (95%CI) | p value | |
|---|---|---|---|---|
| n = 212 | n = 207a | |||
| Without gasping during resuscitation | 1.00 (Ref.) | < .001 | 1.00 (Ref.) | < .001 |
| With gasping either during EMS transport or on hospital arrival | 3.93 (1.07–14.46) | 0.040 | 4.97 (1.11–22.39) | 0.037 |
| With gasping both during EMS transport and on hospital arrival | 12.15 (3.70–39.97) | < .001 | 27.44 (5.65–133.41) | < .001 |
ECPR extracorporeal cardiopulmonary resuscitation, EMS emergency medical service, OR odds ratio, CI confidence interval, Ref. reference
aFive data points were missing from admission to ECMO pump onset; thus, the multivariate analysis included 207 participants
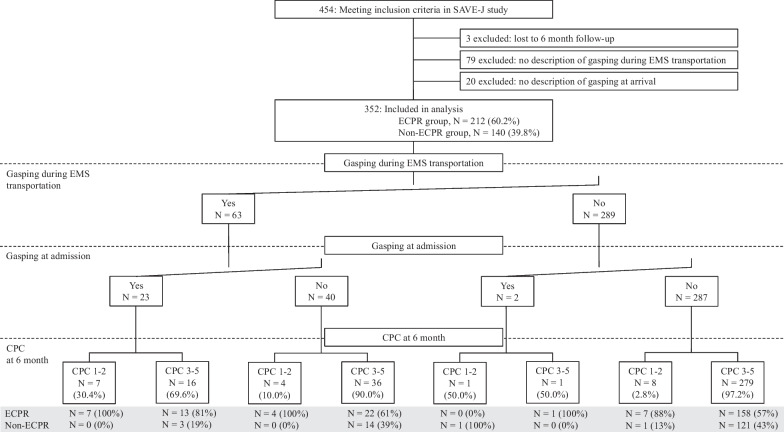
Presence or absence of gasping and neurological outcome in all refractory VF/pVT cases
In total, 352 patients were included in the analysis after excluding three patients with unknown outcomes at 6 months, 79 patients with or without gasping during EMS transport, and 20 patients with or without gassing on arrival at the hospital (Fig. 2). A comparison of the characteristics of cases with or without gasping during resuscitation in all refractory VF/pVT cases is shown in Additional file 2, while the favorable and unfavorable neurological outcomes are shown in Additional file 3. Cases with gasping during resuscitation had more bystander CPR attempts, patients with cardiac arrest during EMS transport, cardiac arrest rhythm as VF/pVT on hospital arrival, favorable neurological outcomes, and 6-month survival. The presence of gasping at any time of resuscitation was associated with a favorable neurological outcome, similar to the case in the ECPR group.
Fig. 2.
Patient enrollment, timing of gasping, and outcomes across all patients. EMS emergency medical service, ECPR extracorporeal cardiopulmonary resuscitation, CPC cerebral performance category
Multivariate logistic regression analysis showed that gasping during resuscitation was independently associated with a favorable neurological outcome (OR 7.01 [95% CI 2.10–23.40]), after adjusting for age, female sex, cardiac arrest rhythm at admission, and therapeutic temperature management (Table 4). The odds of acquisition of favorable neurologic outcome with the existence of gasping both during EMS transport and on hospital arrival was 12.77 (95% CI 3.01–54.25) (Additional file 4).
Table 4.
Logistic regression analysis of prognostic factors for favorable neurological outcomes in all patients
| Variables | Unadjusted OR (95% CI) | p value | Adjusted OR (95% CI) | p value |
|---|---|---|---|---|
| n = 352 | n = 352 | |||
| Age (years) | 0.94 (0.91–0.98) | 0.001 | 0.94 (0.90–0.99) | 0.009 |
| Female sex | 3.76 (1.35–10.42) | 0.011 | 6.71 (1.42–31.74) | 0.016 |
| Witnessed cardiac arrest | ||||
| Yes | 1.34 (0.44–4.12) | 0.611 | ||
| No | 1.00 (Ref.) | 0.879 | ||
| Unknown | 0.00 (0.00-) | 1.000 | ||
| Bystander CPR attempt | ||||
| Yes | 5.12 (1.66–15.76) | 0.004 | ||
| No | 1.00 (Ref.) | 0.016 | ||
| Unknown | 5.84 (0.58–58.45) | 0.133 | ||
| Timing of cardiac arrest | ||||
| Before EMS arrival at scene | 2.13 (0.25–) | 0.488 | ||
| After EMS contact | 1.00 (Ref.) | 0.786 | ||
| Unknown | 0.00 (0.00–) | 1.000 | ||
| Epinephrine administration before hospital arrival | ||||
| Yes | 1.68 (0.64–4.36) | 0.290 | ||
| No | 1.00 (Ref.) | 0.360 | ||
| Unknown | 2.83 (0.55–14.46) | 0.212 | ||
| ROSC during transportation | ||||
| Yes | 0.82 (0.23–2.91) | 0.755 | ||
| No | 1.00 (Ref.) | 0.951 | ||
| Unknown | 1.00 (0.22–4.60) | 0.996 | ||
| Time from cardiac arrest to admission | 0.96 (0.91–1.00) | 0.048 | ||
| Cardiac rhythm at admission | ||||
| VF of pulseless VT | 1.00 (Ref.) | 0.157 | 1.00 (Ref.) | 0.958 |
| PEA | 0.25 (0.06–1.09) | 0.064 | 0.63 (0.12–3.26) | 0.578 |
| Asystole | 0.00 (0.00–) | 0.996 | 0.00 (0.00–) | 0.996 |
| Unknown | 4.53 (0.39–52.60) | 0.227 | Infa | 0.995 |
| Epinephrine administration after hospital arrival | ||||
| Yes | 0.52 (0.17–1.65) | 0.267 | ||
| No | 1.00 (Ref.) | 0.245 | ||
| Unknown | 2.50 (0.22–28.13) | 0.458 | ||
| Gasping during resuscitation | 7.90 (3.08–20.25) | < 0.001 | 7.01 (2.10–23.40) | 0.002 |
| ECPR | 6.40 (1.46–28.04) | 0.014 | ||
| Therapeutic temperature management | ||||
| Yes | 1.00 (Ref.) | 1.000 | 1.00 (Ref.) | 1.000 |
| No | 0.00 (0.00–) | 0.995 | 0.00 (0.00–) | 0.993 |
| Unknown | 0.00 (0.00–) | 0.998 | 0.00 (0.00–) | 0.997 |
| Intra-aortic balloon pumping | ||||
| Yes | 4.72 (1.35–) | 0.015 | ||
| No | 1.00 (Ref.) | 0.052 | ||
| Unknown | 0.00 (0.00–) | 0.998 | ||
| Percutaneous coronary intervention | ||||
| Yes | 1.23 (0.48–3.16) | 0.665 | ||
| No | 1.00 (Ref.) | 0.348 | ||
| Unknown | 0.26 (0.03–2.05) | 0.201 | ||
ECPR extracorporeal cardiopulmonary resuscitation, OR odds ratio, CI confidence interval, CPR cardiopulmonary resuscitation, ROSC return of spontaneous circulation, VF ventricular fibrillation, VT ventricular tachycardia, PEA pulseless electrical activity, Ref reference, Inf infinite
aThe odds ratio was infinite, and the confidence interval could not be calculated
Of the 140 patients with refractory VF/pVT without ECPR, only two patients (1.4%) had favorable neurological outcomes (Additional file 5). Only one of the 18 patients with gasping during resuscitation had a favorable neurological outcome (Additional file 6). Additional files 7 and 8 show the comparison of neurological outcomes and logistic regression analysis results for the neurological outcomes of patients who did not undergo ECPR. Moreover, in comparing ECPR and non-ECPR in patients with gasping during resuscitation, 23.4% and 5.6% had favorable neurological outcomes in the ECPR and non-ECPR groups, respectively (p = 0.155, Additional file 9).
Discussion
In patients with refractory VF/VT, the presence of gasping during resuscitation was an independent prognostic factor for better neurological outcomes at 6 months after onset. Patients who gasped both times during EMS activity and on hospital arrival, indicating continuous presentation of gasping, had a better neurological outcome than those with only one or the other.
In studies comparing ECPR and conventional CPR in patients with an initial VF/pVT rhythm, the outcomes of the ECPR group were generally favorable [8, 10, 19]. However, it is inconclusive whether ECPR should be performed in all refractory cardiac arrests with VF/pVT and if ROSC cannot be achieved before hospital arrival. The ARREST trial demonstrated the usefulness of ECPR in patients who could not obtain ROSC even after three defibrillation shocks, whose body morphology could accommodate ECMO, and whose estimated time to the emergency department was shorter than 30 min [10]. Although the neurological outcome at 6 months was promising (40%), the trial only included patients who required at least three defibrillation shocks and did not show the usefulness of ECPR on patients with refractory VF/pVT who did not obtain ROSC after 1–2 defibrillation shocks and were converted cardiac rhythm to PEA/asystole. The INCEPTION trial investigated whether ECPR could be compared with conventional CPR in patients with refractory VF/pVT who had witnessed and failed to obtain ROSC at 15 min ACLS [8]. As the neurological outcome for patients undergoing ECPR for the initial cardiac rhythm of VF/pVT and with witnessed onset was 20% (including approximately 26% of patients who did not receive ECPR), this could be lower in patients with early waveform VF/pVT without witnessed onset, even if ECPR is performed. The SAVE-J study targeted the initial cardiac rhythm of VF/pVT, cardiac arrest on arrival at the hospital, and no ROSC even after 15 min of ACLS after arrival [19]. Although the rate of obtaining a favorable neurological outcome for ECPR was 12.3% in the SAVE-J study, our results suggest a 23% chance of a favorable neurological outcome when gasping is observed during resuscitation, which may be a realistic strategy, including the implementation of ECPR. The initial cardiac rhythm of VF/pVT is considered an adequate adaptable indicator of ECPR, and we provide the additional finding that gasping during resuscitation increases the probability of acquiring favorable neurological outcomes.
To date, studies on the signs of life have focused on their presence or absence [11–14, 17]. However, in reality, these studies regarded cases with signs of life observed during ambulance transport as the same phenomenon, whether the sign of life was observed at the beginning and disappeared shortly during transport or it was observed continuously during transport. In the present study, gasping data were available during EMS transport and on arrival at the hospital. The OR for favorable neurological outcomes was 27.44 higher in patients with gasping at both times. Gasping at two different times may potentially suggest that gasping continuously exists during resuscitation. Continuous gasping expression suggests that CPR was consistently effective during resuscitation and generated sufficient cerebral blood flow to produce respiration. Thus, the present study demonstrates that continuous gasping expression is more relevant to favorable outcomes than gasping expression at a certain point. In addition, the relationship between the timing of emerging signs of life and outcomes should be examined in the future.
The SAVE-J study also provided data on cases, where ECPR was not performed for refractory VF/pVT [19]. Analysis of the usefulness of gasping during resuscitation in all refractory VF/pVT cases, including patients who did not undergo ECPR, showed that gasping during resuscitation was significantly associated with a favorable neurological outcome. Thus, gasping during resuscitation is a favorable factor in refractory VF/pVT, with or without ECPR. When ECPR was not introduced in patients with refractory VF/pVT with gasping, the acquisition rate of favorable neurological outcomes was 5.6%, compared with 23.4% in the ECPR implementation group (Additional file 9). Although ECPR appears to improve outcomes, more cases need to be included. In the future, the accumulation of outcomes in patients with refractory VF/pVT and gasping during resuscitation, with and without ECPR, will clarify whether gasping should be included in the criteria for ECPR implementation.
The present study had several limitations. First, the cases analyzed in the present study were from 2008 to 2011, making them somewhat older. Second, the number of patients with favorable neurological outcomes was relatively low at 18 (8.5%). This may have caused bias in the present analysis. Third, although a potential prognostic factor for OHCA is prehospital airway management [21], the information was not collected in the SAVE-J study [19] and, therefore, could not be included in the analysis. Fourth, in the multivariate analysis of neurologic outcomes (Table 2), "Therapeutic temperature management," which was not significantly different in the univariate analysis, was selected by the stepwise forward variable selection method. This was presumably included in the stepwise variable selection method because of its increased predictive (discriminative) power when combined with other variables. All patients in the favorable neurological outcome group received "Therapeutic temperature management," and those who did not receive "Therapeutic temperature management" were included only in the unfavorable neurological outcome group (Additional file 1). Thus, while it remains a presumption, the inclusion of "Therapeutic temperature management" as a variable in the multivariate logistic regression analysis may have been valuable in enhancing the predictive power and, consequently, selected for its contribution to the discrimination of outcomes. The forced entry of a variable (bystander CPR attempt), which was significantly different in the univariate analysis, instead of "Therapeutic temperature management," did not change the prognostic advantage of gasping (Additional file 10).
Conclusion
Gasping during resuscitation is favorable in patients with refractory VF/pVT. Patients with refractory VF/pVT with continuously preserved gasping during EMS transportation to the hospital are expected to have more favorable outcomes.
Supplementary Information
Additional file 1: Comparison of baseline characteristics according to neurological outcomes of ECPR patients.
Additional file 2: Comparison of patients with or without gasping during resuscitation.
Additional file 3: Comparison of baseline characteristics by neurological outcome in all patients.
Additional file 4: Odds ratios of neurological outcomes according to the recognition time of gasping based on the absence of gasping in all patients.
Additional file 5: Patient enrollment, timing, and outcomes in the non-ECPR group. EMS, emergency medical service; ECPR, extracorporeal cardiopulmonary resuscitation; CPC, cerebral performance category
Additional file 6: Comparison of patients with or without gasping during resuscitation who did not undergo ECPR
Additional file 7: Comparison of baseline characteristics by neurological outcomes in patients without ECPR.
Additional file 8: Logistic regression analysis of prognostic factors for favorable neurological outcomes in patients without ECPR.
Additional file 9: Comparison between ECPR and non-ECPR in patients who gasped during resuscitation.
Additional file 10: Logistic regression analysis of prognostic factors for favorable neurological outcomes in ECPR patients (Usage of "Bystander CPR attempt" instead of "Therapeutic temperature management" as variable).
Acknowledgements
We would like to thank all the SAVE-J investigators, staff, and participants for their contributions. We also thank Editage (www.editage.com) for English language editing.
Abbreviations
- ACLS
Advanced cardiac life support
- CI
Confidence interval
- CPC
Cerebral performance category
- CPR
Cardiopulmonary resuscitation
- ECPR
Extracorporeal CPR
- EMS
Emergency medical service
- OHCA
Out-of-hospital cardiac arrest
- OR
Odd ratio
- pVT
Pulseless ventricular tachycardia
- ROSC
Restoration of spontaneous circulation
- SAVE-J
Study on advanced cardiac life support for ventricular fibrillation with extracorporeal circulation in Japan
- VF
Ventricular fibrillation
Author contributions
SN and NB contributed to the conceptualization of the study. TS, NM, KN, YT, YA, and TA contributed to the study concept, study design and completion, data collection, and data management for the SAVE-J study. HO performed statistical analyses. KS, SU, NK, and MH contributed to the interpretation of data. EN, YA, and TS provided guidance for the entire study. SN drafted the manuscript, and NB reviewed and edited the manuscript. All authors have read and approved the final manuscript.
Funding
None.
Availability of data and materials
The data sets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The SAVE-J study was registered with the University Hospital Medical Information Network Clinical Trials Registry and the Japanese Clinical Trial Registry (registration number: UMIN000001403). This secondary analysis of de-identified data was approved by the Institutional Review Board of Sapporo Medical University Hospital (approval number: 342-163). The requirement for patient consent was waived because of the anonymized data provided in the sub-analysis of the SAVE-J study. The procedures were performed in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
TS reports the grant from the Ministry of Health, Labour, and Welfare, Japan. All other authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Tsao CW, Aday AW, Almarzooq ZI, Alonso A, Beaton AZ, Bittencourt MS, et al. Heart disease and stroke Statistics-2022 update: a report from the American Heart Association. Circulation. 2022;145:e153–639. doi: 10.1161/CIR.0000000000001052. [DOI] [PubMed] [Google Scholar]
- 2.Japan Resuscitation Council [introduction]. JRC guidelines for resuscitation 2020. Tokyo: Igaku Shoin; 2021. p. 2–8 [in Japanese].
- 3.Grunau B, Puyat J, Wong H, Scheuermeyer FX, Reynolds JC, Kawano T, et al. Gains of continuing resuscitation in refractory out-of-hospital cardiac arrest: a model-based analysis to identify deaths due to intra-arrest prognostication. Prehosp Emerg Care. 2018;22:198–207. doi: 10.1080/10903127.2017.1356412. [DOI] [PubMed] [Google Scholar]
- 4.Reynolds JC, Grunau BE, Rittenberger JC, Sawyer KN, Kurz MC, Callaway CW. Association between duration of resuscitation and favorable outcome after out-of-hospital cardiac arrest: implications for prolonging or terminating resuscitation. Circulation. 2016;134:2084–2094. doi: 10.1161/CIRCULATIONAHA.116.023309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Inoue A, Hifumi T, Sakamoto T, Okamoto H, Kunikata J, Yokoi H, et al. Extracorporeal cardiopulmonary resuscitation in adult patients with out-of-hospital cardiac arrest: a retrospective large cohort multicenter study in Japan. Crit Care. 2022;26:129. doi: 10.1186/s13054-022-03998-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmberg MJ, Geri G, Wiberg S, Guerguerian AM, Donnino MW, Nolan JP, et al. Extracorporeal cardiopulmonary resuscitation for cardiac arrest: a systematic review. Resuscitation. 2018;131:91–100. doi: 10.1016/j.resuscitation.2018.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holmberg MJ, Granfeldt A, Guerguerian AM, Sandroni C, Hsu CH, Gardner RM, et al. Extracorporeal cardiopulmonary resuscitation for cardiac arrest: an updated systematic review. Resuscitation. 2023;182:109665. doi: 10.1016/j.resuscitation.2022.12.003. [DOI] [PubMed] [Google Scholar]
- 8.Suverein MM, Delnoij TSR, Lorusso R, Brandon Bravo Bruinsma GJ, Otterspoor L, Elzo Kraemer CV, et al. Early extracorporeal CPR for refractory out-of-hospital cardiac arrest. N Engl J Med. 2023;388:299–309. doi: 10.1056/NEJMoa2204511. [DOI] [PubMed] [Google Scholar]
- 9.Belohlavek J, Smalcova J, Rob D, Franek O, Smid O, Pokorna M, et al. Effect of intra-arrest transport, extracorporeal cardiopulmonary resuscitation, and immediate invasive assessment and treatment on functional neurologic outcome in refractory out-of-hospital cardiac arrest: a randomized clinical trial. JAMA. 2022;327:737–747. doi: 10.1001/jama.2022.1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yannopoulos D, Bartos J, Raveendran G, Walser E, Connett J, Murray TA, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396:1807–1816. doi: 10.1016/S0140-6736(20)32338-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Debaty G, Lamhaut L, Aubert R, Nicol M, Sanchez C, Chavanon O, et al. Prognostic value of signs of life throughout cardiopulmonary resuscitation for refractory out-of-hospital cardiac arrest. Resuscitation. 2021;162:163–170. doi: 10.1016/j.resuscitation.2021.02.022. [DOI] [PubMed] [Google Scholar]
- 12.Bunya N, Ohnishi H, Wada K, Kakizaki R, Kasai T, Nagano N, et al. Gasping during refractory out-of-hospital cardiac arrest is a prognostic marker for favourable neurological outcome following extracorporeal cardiopulmonary resuscitation: a retrospective study. Ann Intensive Care. 2020;10:112. doi: 10.1186/s13613-020-00730-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Okamoto N, Bunya N, Kakizaki R, Nishikawa R, Nagano N, Kokubu N, et al. Cases of prolonged cardiac arrest with preserved gasping successfully resuscitated with ECPR. Am J Emerg Med. 2022;60(227):e1–3. doi: 10.1016/j.ajem.2022.07.019. [DOI] [PubMed] [Google Scholar]
- 14.Bunya N, Wada K, Yamaoka A, Kakizaki R, Katayama Y, Kasai T, et al. The prognostic value of agonal respiration in refractory cardiac arrest: a case series of non-shockable cardiac arrest successfully resuscitated through extracorporeal cardiopulmonary resuscitation. Acute Med Surg. 2019;6:197–200. doi: 10.1002/ams2.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bobrow BJ, Zuercher M, Ewy GA, Clark L, Chikani V, Donahue D, et al. Gasping during cardiac arrest in humans is frequent and associated with improved survival. Circulation. 2008;118:2550–2554. doi: 10.1161/CIRCULATIONAHA.108.799940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhao L, Li C, Liu B, Wang M, Shao R, Fang Y. The association of gasping and outcome, in out of hospital cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2015;97:7–12. doi: 10.1016/j.resuscitation.2015.09.377. [DOI] [PubMed] [Google Scholar]
- 17.Debaty G, Labarere J, Frascone RJ, Wayne MA, Swor RA, Mahoney BD, et al. Long-term prognostic value of gasping during out-of-hospital cardiac arrest. J Am Coll Cardiol. 2017;70:1467–1476. doi: 10.1016/j.jacc.2017.07.782. [DOI] [PubMed] [Google Scholar]
- 18.Knor J, Seblova J, Skulec R, Seblova D, Malek J. The presence of gasping predicts long-term survival in out-of-hospital cardiac arrest patients. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2018;162:32–35. doi: 10.5507/bp.2017.053. [DOI] [PubMed] [Google Scholar]
- 19.Sakamoto T, Morimura N, Nagao K, Asai Y, Yokota H, Nara S, et al. Extracorporeal cardiopulmonary resuscitation versus conventional cardiopulmonary resuscitation in adults with out-of-hospital cardiac arrest: a prospective observational study. Resuscitation. 2014;85:762–768. doi: 10.1016/j.resuscitation.2014.01.031. [DOI] [PubMed] [Google Scholar]
- 20.Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett PJ, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. A statement for health professionals from a task force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Circulation. 1991;84:960–975. doi: 10.1161/01.CIR.84.2.960. [DOI] [PubMed] [Google Scholar]
- 21.Hasegawa K, Hiraide A, Chang Y, Brown DF. Association of prehospital advanced airway management with neurological outcome and survival in patients with out-of-hospital cardiac arrest. JAMA. 2013;309:257–266. doi: 10.1001/jama.2012.187612. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Comparison of baseline characteristics according to neurological outcomes of ECPR patients.
Additional file 2: Comparison of patients with or without gasping during resuscitation.
Additional file 3: Comparison of baseline characteristics by neurological outcome in all patients.
Additional file 4: Odds ratios of neurological outcomes according to the recognition time of gasping based on the absence of gasping in all patients.
Additional file 5: Patient enrollment, timing, and outcomes in the non-ECPR group. EMS, emergency medical service; ECPR, extracorporeal cardiopulmonary resuscitation; CPC, cerebral performance category
Additional file 6: Comparison of patients with or without gasping during resuscitation who did not undergo ECPR
Additional file 7: Comparison of baseline characteristics by neurological outcomes in patients without ECPR.
Additional file 8: Logistic regression analysis of prognostic factors for favorable neurological outcomes in patients without ECPR.
Additional file 9: Comparison between ECPR and non-ECPR in patients who gasped during resuscitation.
Additional file 10: Logistic regression analysis of prognostic factors for favorable neurological outcomes in ECPR patients (Usage of "Bystander CPR attempt" instead of "Therapeutic temperature management" as variable).
Data Availability Statement
The data sets during and/or analyzed during the current study are available from the corresponding author on reasonable request.