Abstract
Objective:
This study aimed to estimate the pooled prevalence of myopia among school-age children in Ethiopia.
Methods:
Eligible articles were searched from PubMed, Embase, and Web of Science databases. In addition, Google Scholar and reference lists of the retrieved articles were searched from 30 July 2022 to 02 January 2023. The preferred reporting of items for systematic reviews and meta-analysis was used to report the search results. Microsoft Excel was used to keep the data. The qualities of eligible studies were checked using the Joanna Briggs Institute critical appraisal checklist for prevalence studies. Analysis was held using STATA Version 11. The degree of heterogeneity was checked using I² statistics. The possible sources of heterogeneity were examined using meta-regression and subgroup analyses. The funnel plot and Egger’s test were used to assess the potential publication bias. A correction was made for publication bias using Duval and Twee Die’s trim-and-fill analysis. The systematic review registration number is PROSPERO (#CRD42022330541).
Results:
We identified 21 eligible articles including 20,757 subjects. Of those participants, 10,601 (51.1%) and 10,156 (48.9%) were males and females, respectively. A total of 15,152 (73%) participants were urban residents. The estimated prevalence of myopia among school-age children in Ethiopia was found to be 5.26% (95% confidence interval: 4.09–6.42).
Conclusions:
The prevalence of myopia among school-age children in Ethiopia is considerable, affecting one in 20 school-age children. Therefore, the authors recommend the stakeholders take extra steps to speed up the implementation of the school vision screening program and its integration plan into the existing school nutrition program.
Keywords: Myopia, school children, Ethiopia, prevalence, meta-analysis
Introduction
Refractive errors (REs) happen as a consequence of disparities in axial length with respect to the total refractive power of the eye or refractive power of the cornea and crystalline lens with respect to the axial length of the eye. 1 Lack of exact matching of the axial length and the optical power of the eye during the early years of eye growth results in the development of REs.1,2 Uncorrected RE has been the leading cause of visual impairment (VI) in the world. 3
Myopia, also known as near-sightedness, is a common form of RE where close objects appear clear, but distant objects appear blurry 4 and it is also defined as a spherical equivalent (SE) of ⩽−0.50 diopter (D) on either eye. 5 The condition can be corrected using spectacles, contact lenses, and/or refractive surgery. 6 Unless early innervations are considered, it has a great influence on the public health and socioeconomic well-being 7 of the country because myopia is one of the known causes of VI. Authors believe that if there is no evidence, there is no intervention at all. As of Holden et al., 7 the 2020 estimated prevalence of myopia for each global burden of disease region between 2000 and 2050 were 33.9% and 8.4% globally and in East Africa, respectively.
Justification of this systematic review and meta-analysis
Myopia is considered one of the rising public health issues, especially in individuals who spend considerable amounts of time on near tasks, 8 and recommendations are pinpointed for epidemiological evidence on the theme.5,9 In addition, previously published articles indicated that the prevalence of myopia in Ethiopia varied from 0.02% to 16.05%.10,11 This indicates that evidence on the theme in Ethiopia from individual articles was staggering here and there. Thus, the authors believed that using meta-analysis may provide a comprehensive pooled prevalence of myopia in school-age children in Ethiopia. Furthermore, a larger-scale systematic review and meta-analysis done by Ovenseri-Ogbomo et al. 12 on the prevalence of myopia in African school children included only three previous works to represent myopia in school children in Ethiopia. However, the authors believed that there were missing papers that were ignored by previous publications.12,13 As a result, the authors conducted this review to clear the doubt about the precision of the extent of myopia in school-age children in Ethiopia. Therefore, the authors estimated the pooled prevalence of myopia in school-age children in Ethiopia with the maximum effort to include all the potential papers.
This systematic review and meta-analysis can provide evidence for policymakers and planners to design strategies to reduce the negative consequences of myopia among school-age children in the country.
Objective
To estimate the pooled prevalence of myopia among school-age children in Ethiopia.
Review question: what is the pooled prevalence of myopia in school-age children in Ethiopia?
Methods
This systematic review and meta-analysis was conducted using the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) 2020. 14
Searching strategy
The search addressed the databases such as PubMed, Embase, and Web of Science as a source of information. In addition, Google Scholar and the reference list of the retrieved eligible studies from 30 July 2022 to 02 January 2023. These databases were searched using MeSH (Medical Subject Headings) terms and keywords: (“REs” (All Fields) OR “Myopia” (All Fields) OR “Myopia” (MeSh Terms) OR “Short-sightedness” (MeSh Terms) OR “Near-sightedness” (MeSh Terms) OR “VI” (All Fields) AND “school children” (All Fields) OR “school students” (All Fields) AND “Ethiopia” (All Fields)). In addition, manual searching was done for the reference lists of all the retrieved articles. When the outcome is not clearly specified, the authors contacted the corresponding authors of the suspicious papers for further information. Two of the review members (MML and FK) performed an independent systematic search and screening for the articles from 30 July to 02 January 2023. The PRISMA flowchart was used to show the process of selecting eligible articles.
Eligibility criteria
The participants and outcome for this review were school-age children and myopia, respectively.
Inclusion criteria
This review included studies that explained the refraction technique or not. That was done with the sole aim to increase the representativeness of the study population.
Any degree of myopia (SE of ⩽−0.50 D) was accommodated in this systematic review and meta-analysis.
All studies performed on the theme of myopia, REs, and VI that reported the outcome of interest were considered for this review without restriction based on the sex and residence of study participants.
A cross-sectional study design and survey studies with a clear description of sampling techniques were incorporated in this review.
The articles that were published in the English language were included in the review.
The decision on whether to include the articles in the meta-analysis was made by two independent reviewers (MM and FK). To resolve disagreements between the reviewers, the mean value of the quality score of the studies was taken to reach a consensus.
Exclusion criteria
Non-full-text articles, case reports, case series, editorials, and proceedings were excluded from this analysis.
Quality assessment
The quality of the selected article was assessed using Joanna Briggs Institute (JBI) critical appraisal checklist 15 which was prepared for prevalence studies. Using that checklist as a tool, the reviewers (MM, AY, and FK) did an independent review to evaluate the quality of the original articles. Each article was checked for its quality and if it satisfied the necessary criteria outlined on the checklist, a score of one was given for each question. However, the failure to satisfy a criterion scored zero. Then, the risks for biases were classified as high (total score of 0–2), moderate (total score of 3–4), and low (total score of ⩾5) out of nine. Conflicting rates were resolved by taking the mean score of the reviewers’ quality assessment score to reach on consensus.
Data extraction and management
The data extraction and storage were employed using Microsoft Excel. The extraction of each eligible article included the following: Authors name, year of publication, study design, sample size, sex, method of REs assessment (cycloplegic vs non-cycloplegic), the technique of refraction to reach the final decision of the RE (objective vs subjective refraction), the prevalence of myopia, and the response rate. Where the reported prevalence of myopia was not clearly defined, the corresponding author in the published article was contacted for clarification.
Statistical analysis
In this meta-analysis, studies that reported myopia were considered for quantitative synthesis. The analysis was done using STATA V. 11 software. The primary articles included in this meta-analysis were summarized using tables and forest plots. The standard error (SE) of the prevalence of myopia for the original articles was calculated using the formula √(P (100 – P)/N) (where P is the prevalence of myopia in each original article, N is the sample size of a specific study, and √ is the square root). The random effect model was held based on the degree of heterogeneity test (I²) to present the pooled prevalence of myopia in school-age children in Ethiopia. Any observed heterogeneity during analysis is reflected as high (⩾75%), moderate (25%–75%), and low (⩽25%). 16
The possible source (s) of heterogeneity was examined using meta-regression models. The point estimates, the pooled estimates, their 95% confidence intervals, and their corresponding weights were presented using a forest plot.
The potential publication bias was assessed subjectively using a funnel plot and objectively using Begg’s and Egger’s tests at a 5% significance level. 17 Duval and Twee Die’s trim-and-fill analysis was applied to adjust a potential publication bias that was noticed in the test for publication bias.
Subgroup analysis
The subgroup analysis was performed on the prevalence of myopia based on sex, resident year of publication, refraction technique (cycloplegic or non-cycloplegic), and meta-regression output.
Results
Searching results
In this systematic review and meta-analysis, we searched for articles by 02 January 2023 to study the pooled prevalence of myopia among school-age children in Ethiopia. A total of 2100 articles were identified through Pub Med, Embase, Web of Science, and a search engine like Google Scholar, and a check of reference lists of identified articles, accordingly.
A total of 1350 papers remained after the removal of duplicates. Then, authors excluded a total of 1154 based on their titles and 58 based on their abstracts. In addition, about 108 and 3 full-text articles were excluded because they were conducted outside Ethiopia and were meta-analyses, respectively.
In total, 27 full-text studies were assessed for eligibility based on the set criteria. Six articles were found to be ineligible for this meta-analysis because three of them do not fit the target population,18–20 and four articles have not reported the outcome of interest.21–23 A total of 21 articles were included in this systematic review and meta-analysis (Supplemental Figure 1 and Table 1).
Table 1.
Description of original articles included in the study of the pooled prevalence of myopia among school-age children in Ethiopia (n = 21).
| Authors name | Year of publication | Participants resident | Refraction technique | Sample size | Prevalence (95% CI) | Response rate (%) | Risk of bias |
|---|---|---|---|---|---|---|---|
| Bezabih et al. 39 | 2017 | Urban | C | 718 | 1.39 (0.54–2.25) | 89.30 | Moderate |
| Tibebu and Getu 30 | 2000 | Urban | NE | 1134 | 7.41 (5.88–8.93) | 98.10 | Low |
| Jafer and Abonesh 36 | 2010 | Rural | NE | 570 | 2.63 (1.32–3.95) | 96 | Low |
| Mehari and Yimer 25 | 2013 | Rural | NC | 4238 | 5.99 (5.28–6.71) | 77 | Low |
| Abel Sinshaw et al. 26 | 2021 | Urban | C | 601 | 8.49 (6.26–10.71) | 94.80 | Low |
| Hailu et al. 10 | 2020 | Urban | NE | 773 | 1.94 (0.97–2.91) | 94.70 | Low |
| Elias and Kidus 11 | 2022 | Urban | C | 349 | 16.05 (12.20–19.90) | 97 | Low |
| Gashaw et al. 35 | 2020 | Both | NE | 1064 | 1.50 (0.77–2.24) | 100 | Low |
| Tegegne et al. 26 | 2021 | Urban | C | 601 | 8.82 (6.55–11.09) | 94.80 | Moderate |
| Belete et al. 27 | 2016 | Urban | NC | 495 | 11.92 (9.06–14.77) | 99.40 | Low |
| Gessesse and Teshome 34 | 2020 | Urban | NC | 1271 | 6.53 (5.17–7.89) | 89.40 | Low |
| Yared et al. 28 | 2012 | Urban | C | 1852 | 2.97 (2.20–3.74) | 93 | Low |
| Alem and Gebru 33 | 2021 | Urban | NC | 529 | 9.83 (7.29–12.37) | 95.50 | Low |
| Sewunet et al. 29 | 2014 | Both | NE | 420 | 5.48 (3.30–7.65) | 97.20 | Low |
| Dhanesha et al. 32 | 2018 | Urban | C | 1137 | 3.87 (2.75–4.99) | 95.10 | Low |
| Nebiyat et al. 38 | 2015 | Urban | C | 1800 | 1.06 (0.58–1.53) | 99.40 | Low |
| Maru et al. 41 | 2022 | Both | NC | 492 | 9.15 (6.60–11.69) | 97.60 | Moderate |
| Destaye et al. 31 | 2017 | Urban | C and NC | 1287 | 0.78 (0.30–1.26) | 97.50 | Low |
| Ezinne 24 | 2013 | Urban | NE | 313 | 6.07 (3.42–8.72) | NR | Moderate |
| Mehari 37 | 2014 | Both | NE | 735 | 4.63 (3.11–6.14) | NR | Moderate |
| Haile et al. 40 | 2017 | Urban | NE | 378 | 1.85 (1.16–2.54) | NR | Moderate |
NE: not explained; NR: not reported; C: cycloplegic; NC: non-cycloplegic.
Description of articles included in this review
All the included articles were cross-sectional studies. The meta-analysis covered eligible studies from 2000 to 2022. In the identified eligible articles, the lowest sample size used by an article was 313 (n = 313), 24 while the highest sample size used by an article was 4238 (n = 4238). 25 A total of 20,757 participants were involved in this meta-analysis to estimate the pooled prevalence of myopia among school-age children in Ethiopia. Of those participants, 10,601 (51.1%) and 10,156 (48.9%) were males and females, respectively. A total of 15,152 (73%) participants were urban residents, whereas the remaining 5605 (17%) participants were rural residents. The studies were conducted in different corners of the country. Eight studies were conducted in Amhara Region,24,26–31 one study was conducted in Tigray Region, 32 seven studies were conducted in Southern Nations Nationalities and Peoples Region,11,25,33–37 four studies were conducted in Addis Ababa City administration,10,38–40 and a single study was conducted in Benishangul Gumuz Region. 41 A single article was a preprint, 41 whereas all the remaining articles were published. Independent evaluators (MML, FK, and AY) reassessed the quality of the papers before formal analysis. Disagreements were resolved through discussion. The quality of eligible studies was assessed using the JBI 15 checklist that was prepared for the appraisal of prevalence studies. In all, 15 studies (n = 15) were found to have a low-risk bias. The eligible studies considered for the synthesis of this result are documented in Table 1.
Meta-analysis
Prevalence of myopia in school-age children
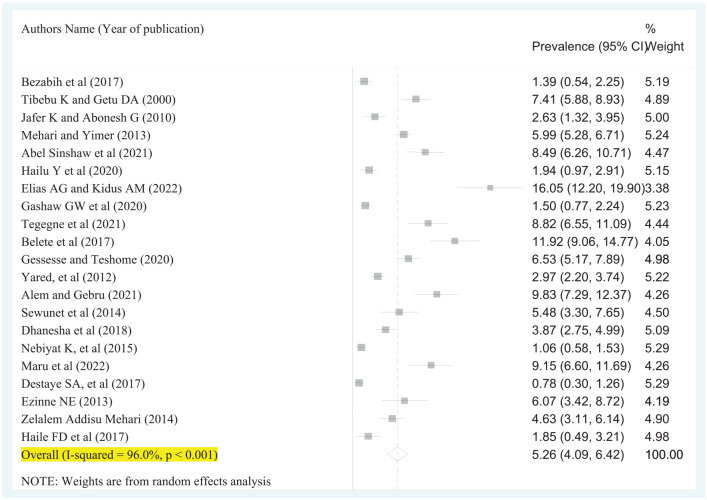
We performed a random effect model to estimate the overall pooled prevalence of myopia in school-age children in Ethiopia due to high heterogeneity (I² = 96.0%; p < 0.001) in the fixed effect model. In this meta-analysis, the pooled prevalence of myopia among the target population was 5.26% (95% CI: 4.09–6.42) (Figure 1).
Figure 1.
Forest plot representing the pooled prevalence of myopia among school-age children in Ethiopia (n = 21).
Of 21 included articles, only eight articles (n = 8) stated the number of myopic males and females.11,26–30,34,39 In this review, the highest proportion of myopia was determined among female school-age children in Ethiopia (3.95%; 95% CI: 2.51–5.39) (Supplemental Figure 2), whereas the burden of myopia was lower among male school-age children (2.91%; 95% CI: 1.73–4.08) (Supplemental Figure 3) based on eight articles.
Publication bias and meta-regression
The publication bias was checked using a funnel plot, Egger’s, and Begg’s tests. The funnel plot showed an asymmetric distribution (Supplemental Figure 4). In addition, Egger’s (p < 0.001) and Begg’s tests (p < 0.001) revealed significant publication bias.
In the meta-regression results, the heterogeneity was explained by sample sizes (p < 0.001), but the heterogeneity was not explained by the years of publication (p = 0.356) (Table 2).
Table 2.
Meta-regression analysis results in the study of pooled prevalence of myopia among school-age children in Ethiopia.
| Variables | Coefficient | p Value |
|---|---|---|
| Sample size | –0.00096 | 0.001 |
| Year of publication | 0.164 | 0.356 |
Furthermore, Duval and Twee Die’s trim-and-fill analysis42,43 was held due to the significant publication bias revealed by Egger’s (p < 0.001) and Begg’s tests (p < 0.001). Finally, the prevalence of myopia among school-age children was 5.26% (95% CI: 4.09–6.42) after correction for potential publication bias.
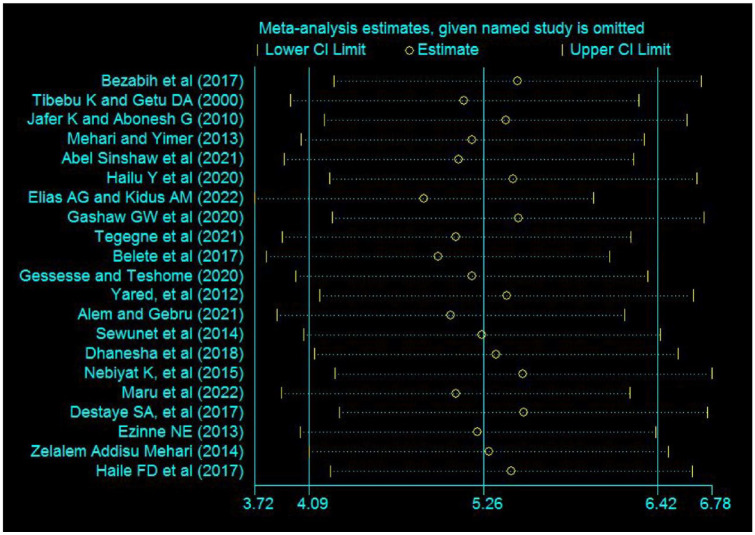
Sensitivity and subgroup analyses
The existence of a single study effect on the pooled prevalence of myopia among school-age children in Ethiopia was checked using meta-influence analysis. No study significantly influenced the pooled prevalence of myopia among school-age children in Ethiopia (Figure 2).
Figure 2.
A forest plot representing the effect of the given named study is omitted from the pooled estimate of myopia among school-age children in Ethiopia.
In a subgroup analysis, the prevalence of myopia among school-age children was 5.40% (95% CI: 3.49–7.41) based on the study’s results that did cycloplegic refraction. The finding of myopia was 8.35% (95% CI: 6.40–10.29) based on the study that applied non-cycloplegic refraction. The prevalence of myopia was 3.79% (95% CI: 2.31–5.26) in studies that did not explain the refraction technique that they used to attain the amount of RE (Table 3).
Table 3.
The subgroup analysis of the pooled prevalence of myopia among school-age children in Ethiopia.
| Variables | Characteristics | Number of studies | Prevalence with 95% CI |
|---|---|---|---|
| Refraction technique | Cycloplegic | 7 | 5.40 (3.49–7.41) |
| Non-cycloplegic | 5 | 8.35 (6.40–10.29) | |
| Not explained | 8 | 3.79 (2.31–5.26) | |
| Both (cycloplegic and non-cycloplegic) | 1 | 0.78 (0.30–1.26) | |
| Year of publication | 2015–2022 | 14 | 5.38 (3.97–6.79) |
| Before 2015 | 7 | 4.94 (3.50–6.38) | |
| Sample size | <1000 | 13 | 6.50 (4.57–8.43) |
| >1000 | 8 | 3.69 (2.09–5.30) | |
| Resident | Urban | 15 | 5.47 (4.07–6.86) |
| Rural | 2 | 4.36 (1.07–7.65) | |
| Both | 4 | 5.03 (1.93–8.13) |
Based on the year of publication, in studies that were conducted prior to 2015, the pooled prevalence of myopia among school-age children was 4.94% (95% CI: 3.50–6.38). However, based on the studies that were done from 2015 to 2022, the estimated prevalence of myopia was 5.38% (95% CI: 3.97–6.79) (Table 3).
Based on the sample size, those studies that included study participants of >1000 indicated the prevalence of myopia as 3.69% (95% CI: 2.09–5.30), while those 13 studies that incorporated study participants of <1000 in combination gave the prevalence of myopia as 6.50% (95% CI: 4.57–8.43) (Table 3).
Based on the resident included studies of participants, the prevalence of myopia among urban, rural, and in studies that include both urban and rural school-age children were 5.47% (95% CI: 4.07–6.86), 4.36% (95% CI: 1.07–7.65), and 5.03% (95% CI: 1.93–8.13), respectively (Table 3).
Discussion
In this study, the pooled prevalence of myopia among school-age children in Ethiopia was 5.26% (95% CI: 4.09–6.42). In terms of sex, the prevalence of myopia was 3.95% (95% CI: 2.51–5.39) and 2.91% (95% CI: 1.73–4.08) among female and male school-age children, respectively. The prevalence of myopia based on the refraction technique was 5.40% (95% CI: 3.40–7.41) and 8.35% (95% CI: 6.40–10.29) for the cycloplegic versus non-cycloplegic category, respectively. The pooled prevalence of myopia for studies conducted before 2015 was 4.94% (95% CI: 3.50–6.38), and it was 5.38% (95% CI: 3.97–6.79) for studies conducted from 2015 to 2022. Based on the sample size that the studies included, the prevalence of myopia was 3.69% (95% CI: 2.08–5.30) and 6.5% (95% CI: 4.57–8.43) for studies that used a sample size of >1000 and <1000, respectively. Interims of residency of the study participants, the prevalence of myopia among school-age children was 5.47% (95% CI: 4.07–6.86), 4.36% (95% CI: 1.07–7.65), and 5.03% (95% CI: 1.93–8.13) for urban, rural, and both, respectively.
In the systematic review and meta-analysis conducted by Naidoo et al. 44 in 2020, uncorrected refractive errors (UREs) account for 20.88% and 12.40% of blindness worldwide and in Eastern sub-Saharan Africa, respectively. The same study revealed that moderate and severe VI due to URE accounts for 53.88% and 48.46% globally and in Eastern sub-Saharan Africa, 44 respectively.
In Ethiopia, the estimated prevalence of blindness and low vision due to URE was 7.8% and 33.4%, respectively. 45 Furthermore, the meta-analyses on the prevalence of REs among school students; the one conducted to estimate VI due to REs among children and adolescents, and the other stated VI among school children in Ethiopia reported 7.36% 13 and 6%, 46 and 6.13%, 47 respectively. However, those findings were based on a limited number of studies. Visually impaired children are three times more likely to fail at least one grade level. 48
As a part of REs, myopia is an emerging public health problem worldwide. 7 Its 2020, 2030, 2040, and 2050 projection in East Africa ranges from 8.4% to 22.7%, 7 indicating nearly 4%–6% additional increment in the prevalence of myopia throughout every decade.
As of 25 January 2023, the population of Eastern Africa was greater than 474 million, 49 and Ethiopia is the most populous country in East Africa with a total population of more than 122 million. 49 In Ethiopia, as reported by Addis Standard on 22 October 2022, the 2022–2023 academic year school enrolment was 16.3 million leaving 13 million eligible children out of school 50 (i.e., 29.3 million eligible school-age children in Ethiopia). Also, a manual prepared for school vision screening by the Ministry of Health in 2021 indicated that children under the age of 15 years account for 45% of the total population of the country (i.e., Ethiopia). 48 Studies revealed that school-age children are the most exposed group to myopic RE51,52 due to the greater intensity of near activities.53–57 So, this study estimated the pooled prevalence of myopia among school-age children in Ethiopia.
In this meta-analysis, the pooled prevalence of myopia among school-age children in Ethiopia was 5.26% (95% CI: 4.09–6.42). Based on the current eligible school-age children in Ethiopia, 50 at least 1.5 million school-age children are myopic, which is approximately equal to the total population of Ireland 58 and that of Monterrey City, Mexico. 59 This implies that the burden of myopia among school-age children in Ethiopia is as huge as observing all individuals in those cited areas visually impaired.
The finding of this meta-analysis (5.26%) is consistent with the results of meta-analyses done in children in India in 2018 (5.3%) 60 and Nepal in 2023 (7.1%). 61 It is also in line with the result of a meta-analysis of childhood myopia and myopia in school children in Africa in 2022 (4.7%)12,62 and comparable with the study finding in Ethiopia among school students (5.10%), 13 based on the results of 16 articles. The similarity in the study results may be due to approximate similarities in the study populations specifically their age. However, the result of this review was lower than a meta-analysis result done by Dutheil et al. 56 (31%) and in Indian school children in 2020 (7.5%). 63 The variation of the results may be explained by the difference in the lifestyle routine (e.g. reading, studying, and using electronic materials for near tasks) of the study participants 64 and the difference in genetic predisposition.
On the other hand, the present meta-analysis showed a higher prevalence of myopia when compared with the result of a meta-analysis conducted in the Middle East Region (4%). 65 The difference in the result might be subjected to the exclusion of studies that performed non-cycloplegic refraction in previous work in the Middle East Region.
In this review, the highest proportion of myopia was among female school-age children in Ethiopia (3.95%; 95% CI: 2.51–5.39). On the other hand, the burden of myopia was lower (2.91%; 95% CI: 1.73–4.08) among male school-age children. This finding is comparable with the previous work conducted by Fahimeh et al. 65 (3.5% among males and 4.2% among females aged 15 years or less). The consistency in the results may be due to the inaccessibility of health care, specifically eye care services. However, the sex-based proportion of myopia among school-age children in Ethiopia in the current study is lower than the meta-analysis results in school-age children in Africa. 12 The difference in the study outcome may be due to the variation in ethnicity and race in Africa and within the countries of Africa.
Based on the refraction technique utilized by the included articles, the pooled prevalence of myopia among school-age children was 5.40% (95% CI: 3.40–7.41) in studies that used cycloplegic refraction. However, the finding was raised to 8.35% (95% CI: 6.40–10.29) in studies that performed non-cycloplegic refraction. This finding is reliable with the study done on African school children. 12 The similarity of the findings might be due to similar inclusion criteria regarding the refraction technique utilized by the original articles. In the studies that did not explain the refraction techniques, the pooled prevalence of myopia was 3.79% (95% CI: 2.31–5.26). This result is lower than the finding in studies that explained the refraction technique they used on the way to detect myopia. The authors’ hypothesis that the lower prevalence of myopia in this category might be due to the smaller sample size (approximately 26% of the total population included in this meta-analysis) in the studies that included estimated myopia although there were no reported refraction techniques by previous original articles.
On the other way, based on the year of publication, in the studies that were conducted prior to 2015, the pooled prevalence of myopia was found to be 4.94% (95% CI: 3.50–6.38). Whereas based on the studies that were conducted from 2015 to 2022, the pooled prevalence of myopia was 5.38% (95% CI: 3.97–6.79). According to the most recent studies, the rising prevalence of myopia among school-age children in Ethiopia may be due to the shifting nature of lifestyle culture because of technological advancements 66 and due to increasing urbanization. 67
In the current study, the subgroup analysis based on sample size represents that the pooled estimated of myopia among school-age children in Ethiopia was 3.69% (95% CI: 2.08–5.30), provided that the included studies recruited >1000 participants (more than 66% of contribution to this meta-analysis) while studies in which <1000 participants were involved shown that the prevalence of myopia was 6.50% (95% CI: 4.57–8.43). The represented cut point was not tested formally, and the authors decided to use this arbitrary cut point to see the effect of sample size on the overall prevalence of myopia. Based on the findings, the authors assume that studies that addressed more than 1000 participants may represent their target population better when compared to their counterparts. Because the pooled results of the studies whose sample sizes >1000 have a narrower confidence interval.
In addition, in this meta-analysis, a subgroup analysis was performed for studies that included urban school-age children (N = 15), rural school-age children (N = 2), and studies that included both urban and rural school-age children (N = 4). The estimated prevalence of myopia based on the studies conducted in urban school-age children in rural school-age children, and based on the studies that included both urban and rural school-age children were 5.47% (95% CI: 4.07–6.86), 4.36% (95% CI: 1.07–7.65), and 5.03% (95% CI: 1.93–8.13), respectively. According to this study result, the estimated prevalence of myopia, based on studies conducted among urban school-age children, was higher than the prevalence of myopia that studies conducted on rural school-age children, and those studies results included both rural and urban school-age children. This report may also be due to the shifting nature of lifestyles and increasing urbanization as explained above. Nevertheless, the interpretation of this result also requires caution in the Ethiopian context because school-age children move from rural areas to urban areas most probably due to the inaccessibility of education.
Generally, myopia is an increasing burden in Ethiopia affecting more than 1.5 million school-age children. This implies that at least 1.5 million of the school-age children in Ethiopia may have impairment in their future lives and may become dependent on others due to the possible complications and irregularities from the rising burden of myopia. In addition, the finding of the present study implies the prevalence of myopia is more common among female school-age children when compared to that of male school-age children. Also, according to this study, the prevalence of myopia based on non-cycloplegic refraction seems overestimated because it is not the recommended refraction technique for the young population in whom the REs can be affected potentially by accommodation. Therefore, the interpretation of the result based on this technique needs caution. As a result, the authors recommend future researchers follow the gold standard approach (i.e., cycloplegic refraction) to investigate the prevalence of myopia in children, provided that using a large sample size as much as possible and encourages emphasis on the population who are perusable at risk.
The strength of this study is that it estimated the pooled prevalence of myopia among school-age children in Ethiopia. So, it will be an additional input for policymakers and planners and as baseline evidence to execute trends in myopia epidemiology and to establish an early intervention program for school-age children in Ethiopia.
However, the limitation of this study is that it did not report the prevalence of high myopia and the factors that manipulate myopia. In addition, this study included papers that did not declare the method of refraction that they applied to detect myopia.
Conclusion
The prevalence of myopia among school-age children in Ethiopia is considerable, affecting one in 20 school-age children. The analysis is essential to guide future eye health care, the intervention, clinical management, and the betterment of the implementation of the school vision screening program. Therefore, the authors recommend the stakeholders take extra steps to speed up the implementation of the school vision screening program and its integration plan into the existing school nutrition program.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121231200105 for Prevalence of myopia in school-age children in Ethiopia: A systematic review and meta-analysis by Merkineh Markos Lorato, Ali Yimer and Fassikaw Kebede Bizueneh in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121231200105 for Prevalence of myopia in school-age children in Ethiopia: A systematic review and meta-analysis by Merkineh Markos Lorato, Ali Yimer and Fassikaw Kebede Bizueneh in SAGE Open Medicine
Supplemental material, sj-docx-3-smo-10.1177_20503121231200105 for Prevalence of myopia in school-age children in Ethiopia: A systematic review and meta-analysis by Merkineh Markos Lorato, Ali Yimer and Fassikaw Kebede Bizueneh in SAGE Open Medicine
Supplemental material, sj-docx-4-smo-10.1177_20503121231200105 for Prevalence of myopia in school-age children in Ethiopia: A systematic review and meta-analysis by Merkineh Markos Lorato, Ali Yimer and Fassikaw Kebede Bizueneh in SAGE Open Medicine
Acknowledgments
Researchers who involved in the papers included this meta-analysis.
Footnotes
Authors’ contributions: MML: the conception of the research protocol, analysis, and drafting of the manuscript. AY and FK: designing methods and analysis techniques and reviewing the manuscript. All the authors have read and approved the manuscript.
Availability of data and materials: All relevant data are within the manuscript and on its supplementary materials.
Consent for publication: Not applicable.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethics and consent to participate: Ethics approval and consent are not required.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Merkineh Markos Lorato  https://orcid.org/0000-0003-1422-9837
https://orcid.org/0000-0003-1422-9837
Fassikaw Kebede Bizueneh  https://orcid.org/0000-0002-6117-5272
https://orcid.org/0000-0002-6117-5272
Supplemental material: Supplemental material for this article is available online.
References
- 1. Wallman J, Winawer J. Homeostasis of eye growth and the question of myopia. Neuron 2004; 43(4): 447–468. [DOI] [PubMed] [Google Scholar]
- 2. Smith EL. Spectacle lenses and emmetropization: the role of optical defocus in regulating ocular development. Optom Vis Sci 1998; 75(6): 388–398. [DOI] [PubMed] [Google Scholar]
- 3. Flaxman SR, Bourne RRA, Resnikoff S, et al. Global causes of blindness and distance vision impairment 1990–2020: a systematic review and meta-analysis. Lancet Glob Health 2017; 5: e1221–e1234. [DOI] [PubMed] [Google Scholar]
- 4. Bethesda National Institutes of Health: National Eye Institute. Myopia 2020; 20892–3655(301): 496–5248. [Google Scholar]
- 5. WHO. The impact of myopia and high myopia: report of the joint world health organization–Brien Holden vision institute global scientific meeting on myopia. Sydney, Australia: University of New South Wales, 2015. [Google Scholar]
- 6. Leo SW, Young TL. An evidence-based update on myopia and interventions to retard its progression. JAAPOS 2011; 15(2): 181–189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016; 123(5): 1036–1042. [DOI] [PubMed] [Google Scholar]
- 8. Saw SM, Chua WH, Hong CY, et al. Nearwork in early-onset myopia. Invest Ophthalmol Vis Sci 2002; 43(2): 332–339. [PubMed] [Google Scholar]
- 9. Grzybowski A, Kanclerz P, Tsubota K, et al. A review on the epidemiology of myopia in school children worldwide. BMC Ophthalmol 2020; 20: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hailu Y, Hiko D, Shaweno T. Prevalence of visual impairment and associated factors in primary schoolchildren in Addis Ababa, Central Ethiopia. Clin Ophthalmol 2020; 14: 767–774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Gebru EA, Mekonnen KA. Prevalence and factors associated with myopia in high school students in Hawassa City, South Ethiopia. Clin Optom 2022; 14: 35–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ovenseri-Ogbomo G, Osuagwu UL, Ekpenyong BN, et al. Systematic review and meta-analysis of myopia prevalence in African school children. PloS One 2022; 17(2): e0263335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Sume BW, Seyoum G. Prevalence of refractive errors among school students in Ethiopia: a systematic review and meta-analysis. SAGE Open Med 2022; 10: 205031212211270. [Google Scholar]
- 14. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021; 372: n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Munn Z, Moola S, Lisy K, et al. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc 2015; 13(3): 147–153. [DOI] [PubMed] [Google Scholar]
- 16. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med 2002; 21(11): 1539–1558. [DOI] [PubMed] [Google Scholar]
- 17. Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol 2001; 54(10): 1046–1055. [DOI] [PubMed] [Google Scholar]
- 18. Besufikad B, Hailemichael W, Tilahun L, et al. Refractive errors and associated factors among patients visiting BoruMeda Hospital’s secondary eye unit in Dessie Town, South Wollo Zone, Ethiopia. BMC Ophthalmol 2022; 22: 312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Berhane MA, Demilew KZ, Assem AS. Myopia: an increasing problem for medical students at the University of Gondar. Clin Ophthalmol 2022; 16: 1529–1539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Assefa NL, Admas AW, Adimasu NF. Prevalence and associated factors of visual impairment among adults at Debre Berhan town, north Shewa, Ethiopia. BMC Ophthalmol 2020; 20(1): 316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Abayo G, Gessesse GW, Asaminew T. Prevalence and pattern of ocular morbidity among school children in southern Ethiopia. Ethiop J Health Sci 2021; 31(4): 831–836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Zelalem M, Abebe Y, Adamu Y, et al. Prevalence of visual impairment among school children in three primary schools of Sekela Woreda, Amhara regional state, north-west Ethiopia. SAGE Open Med 2019; 7: 2050312119849769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Merrie YA, Tegegne MM, Munaw MB, et al. Prevalence and associated factors of visual impairment among school-age children in Bahir Dar city, northwest Ethiopia. Clin Optom 2019; 11: 135–143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ezinne NE. Prevalence of refractive error among school children in Meseret General Primary School Gondar town north west Ethiopia. J Health Vis Sci 2013; 15(1): 23–29. [Google Scholar]
- 25. Mehari AZ, Yimer AW. Prevalence of refractive errors among schoolchildren in rural central Ethiopia. Clin Exp Optom 2013; 96(1): 65–69. [DOI] [PubMed] [Google Scholar]
- 26. Tegegne MM, Assem AS, Merie YA. Prevalence and associated factors of amblyopia among school age children at Bahir Dar City, northwest Ethiopia: a community-based cross-sectional study. Clin Optom 2021; 13: 143–153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Belete GT, Anbesse DH, Tsegaye AT, et al. Prevalence and associated factors of myopia among high school students in Gondar town, northwest Ethiopia, 2016. Clin Optom 2016; 9: 11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yared AW, Belaynew WT, Destaye S, et al. Prevalence of refractive errors among school children in Gondar town, northwest Ethiopia. Middle East Afri J Ophthalmol 2012; 19(4): 372–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Sewunet SA, Ketema KA, Gedefaw M. Uncorrected refractive error and associated factors among primary school children in Debre Markos district, northwest Ethiopia. BMC Ophthalmol 2014; 14: 95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Kassa T, Alene GD. Prevalence of refractive errors in pre-school and school children of Debarki and Kola Diba towns, north-western Ethiopia. Ethio J Health Dev 2000; 17(2): 117–124. [Google Scholar]
- 31. Haile WA, Ayanaw T, Alemayehu DG, et al. Prevalence and types of amblyopia among primary school children in Gondar town, northwest Ethiopia. J Ophthalmol 2017; 2(3): 1–6. [Google Scholar]
- 32. Dhanesha U, Polack S, Bastawrous A, et al. Prevalence and causes of visual impairment among schoolchildren in Mekelle, Ethiopia. Cogent Med 2018; 5(1): 1554832. [Google Scholar]
- 33. Alem KD, Gebru EA. A cross-sectional analysis of refractive error prevalence and associated factors among elementary school children in Hawassa, Ethiopia. J Intern Med Res 2021; 49(3): 300060521998894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gessesse SA, Teshome AW. Prevalence of myopia among secondary school students in Welkite town: south-western Ethiopia. BMC Ophthalmol 2020; 20: 176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Woldeamanuel GG, Biru MD, Geta TG, et al. Visual impairment and associated factors among primary school children in Gurage zone, southern Ethiopia. Afri Health Sci 2020; 20(1): 533–542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Kedir J, Girma A. Prevalence of refractive error and visual impairment among rural school-age children of Goro district, Gurage zone, Ethiopia. Ethiop J Health Sci 2014; 24(4): 353–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Mehari ZA. Pattern of childhood ocular morbidity in rural eye hospital, central Ethiopia. BMC Ophthalmol 2014; 14: 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Nebiyat K, Alemayehu W, Tigist SW. Refractive errors among school children in Addis Ababa, Ethiopia. J Ophthalmol East Cent South Afr 2015; 19(2): 57–62. [Google Scholar]
- 39. Bezabih L, Abebe TW, Fite RO. Prevalence and factors associated with childhood visual impairment in Ethiopia. Clin Ophthalmol 2017; 11: 1941–1948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Darge HF, Shibru G, Mulugeta A, et al. The prevalence of visual acuity impairment among school children at Arada Subcity primary schools in Addis Ababa, Ethiopia. J Ophthalmol 2017; 2017: 9326108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Maru L, Yitayew M, Getu D, et al. Visual impairment and associated factors among randomly selected secondary school students of Assosa zone, north west Ethiopia. Res Square 2022: 1–17. [Google Scholar]
- 42. Shi L, Lin L. The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Medicine (Baltimore) 2019; 98(23): e15987. DOI: 10.1097/MD.0000000000015987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Duval S, Tweedie R. Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 2000; 56(2): 455–463. [DOI] [PubMed] [Google Scholar]
- 44. Naidoo K, Kempen JH, Gichuhi S, et al. Prevalence and causes of vision loss in sub-Saharan Africa in 2015: magnitude, temporal trends and projections. Br J Ophthalmol 2020; 104: 1658–1668. [DOI] [PubMed] [Google Scholar]
- 45. Berhane Y, Worku A, Bejiga A. National survey on blindness, low vision and trachoma in Ethiopia. Ethiop J Health Dev 2007; 21: 204–210. [Google Scholar]
- 46. Atlaw D, Shiferaw Z, Sahiledengele B, et al. Prevalence of visual impairment due to refractive error among children and adolescents in Ethiopia: a systematic review and meta-analysis. PLoS One 2022; 17(8): e0271313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Awoke N, Tekalign T, Teshome Guta M, et al. Visual impairment in Ethiopia: systematic review and meta-analysis. Br J Vis Impair 2022. DOI: 10.1177/02646196221145358. [DOI] [Google Scholar]
- 48. Ethiopian Ministry of Health. The National school eye health manual for teachers. Guidline (2021, accessed 2 January 2021). [Google Scholar]
- 49. Worldometer. Eastern Africa population, 2023, https://www.worldometers.info/world-population/eastern-africa-population/#:~:text=The%20current%20population%20of%20Eastern,among%20subregions%20ranked%20by%20Population
- 50. Addis Standard. Analysis: parents struggle with rising cost of education as wars, natural disasters force 13m out of schools in Ethiopia, 2022. [Google Scholar]
- 51. Ding X, Morgan IG, Hu Y, et al. Exposure to the life of a school child rather than age determines myopic shifts in refraction in school children. Invest Ophthalmol Vis Sci 2022; 63(3): 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Liu L, Jiang D, Li C, et al. Relationship between myopia progression and school entrance age: a 2.5-year longitudinal study. J Ophthalmol 2021; 2021: 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Mukazhanova A, Aldasheva N, Iskakbayeva J, et al. Prevalence of refractive errors and risk factors for myopia among schoolchildren of Almaty, Kazakhstan: a cross-sectional study. PLoS One 2022; 17(6): e0269474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Sun JT, An M, Yan XB, et al. Prevalence and related factors for myopia in school-aged children in Qingdao. J Ophthalmol 2018; 2018: 9781987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Guo L, Yang J, Mai J, et al. Prevalence and associated factors of myopia among primary and middle school-aged students: a school-based study in Guangzhou. Eye 2016; 30: 796–804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Dutheil F, Oueslati T, Delamarre L, et al. Myopia and nearwork: a systematic review and meta-analysis. Int J Environ Res Public Health 2023; 20: 875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Vagge A, Desideri LF, Nucci P, et al. Prevention of progression in myopia: a systematic review. Diseases 2018; 6: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Clark D. Estimated population of the Republic of Ireland from 2002 to 2022, 2022. [Google Scholar]
- 59. Macrotrends. Monterrey, Mexico metro area population 1950–2023, 2023. https://www.macrotrends.net/cities/21853/mexico-city/population
- 60. Sheeladevi S, Seelam B, Nukella PB, et al. Prevalence of refractive errors in children in India: a systematic review. Clin Exp Optom 2018; 101(4): 495–503. [DOI] [PubMed] [Google Scholar]
- 61. Bist J, Kandel H, Paudel N, et al. Prevalence of refractive errors in Nepalese children and adults: a systematic review with meta-analysis. Clin Exp Optom 2023; 106(2): 119–132. [DOI] [PubMed] [Google Scholar]
- 62. Kobia-Acquah E, Flitcroft DI, Akowuah PK, et al. Regional variations and temporal trends of childhood myopia prevalence in Africa: a systematic review and meta-analysis. Ophthalmic Physiol Opt 2022; 42: 1232–1252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Agarwal D, Saxena R, Gupta V, et al. Prevalence of myopia in Indian school children: meta-analysis of last four decades. PLoS One 2020; 15(10): e0240750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Theophanous C, Modjtahedi BS, Batech M, et al. Myopia prevalence and risk factors in children. Clin Ophthalmol 2018; 12: 1581–1587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Khoshhal F, Hashemi H, Hooshmand E, et al. The prevalence of refractive errors in the middle east: a systematic review and meta-analysis. Int Ophthalmol 2020; 40: 1571–1586. [DOI] [PubMed] [Google Scholar]
- 66. Verkicharla PK, Das AV. Technology and myopia. Community Eye Health J 2019; 32(105): 59–60. [PMC free article] [PubMed] [Google Scholar]
- 67. Chen X, Ye G, Zhong Y, et al. Prevalence, incidence, and risk factors for myopia among urban and rural children in southern China: protocol for a school-based cohort study. BMJ Open Ophthalmol 2021; 11(11): e049846. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121231200105 for Prevalence of myopia in school-age children in Ethiopia: A systematic review and meta-analysis by Merkineh Markos Lorato, Ali Yimer and Fassikaw Kebede Bizueneh in SAGE Open Medicine
Supplemental material, sj-docx-2-smo-10.1177_20503121231200105 for Prevalence of myopia in school-age children in Ethiopia: A systematic review and meta-analysis by Merkineh Markos Lorato, Ali Yimer and Fassikaw Kebede Bizueneh in SAGE Open Medicine
Supplemental material, sj-docx-3-smo-10.1177_20503121231200105 for Prevalence of myopia in school-age children in Ethiopia: A systematic review and meta-analysis by Merkineh Markos Lorato, Ali Yimer and Fassikaw Kebede Bizueneh in SAGE Open Medicine
Supplemental material, sj-docx-4-smo-10.1177_20503121231200105 for Prevalence of myopia in school-age children in Ethiopia: A systematic review and meta-analysis by Merkineh Markos Lorato, Ali Yimer and Fassikaw Kebede Bizueneh in SAGE Open Medicine