Abstract
The coronavirus disease 2019 (COVID-19) is one of the most severe global health uncertainties to date. Although significant global effort has been put into implementing COVID-19 pandemic control measures such as lockdowns, travel restrictions, and hygiene precautions, the transmission is expected to resurface once these efforts are discontinued. We aimed to determine the prevalence and factors associated with compliance with presidential 53-day lockdown measures in June-July 2021 in northern Uganda. In this cross-sectional study, 587 adult participants (≥18 years old) from northern Uganda were selected using a systematic sampling method. Data collection involved interviewer-administered questionnaires with an internal validity of Cronbach’s α = .72. Socio-demographic characteristics of participants were described, and multivariable modified Poisson regressions were performed to assess prevalence ratios between dependent and selected independent variables, with respective P values at 95% confidence intervals. All analyses were conducted using Stata 17.0. Participants’ compliance with the presidential lockdown directives was high at 88%(95% CI: 85%-90%). Compliance with the presidential directives was more likely among participants who agreed to the lockdown measures [adjusted Prevalence Ratio, aPR = 1.28 (95% CI: 1.10-1.49; P = .001)] compared to those who did not, and more likely among those who were afraid of death from COVID-19 [aPR = 1.08 (95% CI: 1.01-1.15; P = .023)] than those who did not. However, compliance was less likely among males [aPR = 0.91 (95% CI: 0.86-0.97; P = .002)] compared to females, those aged 35 to 44 years [aPR = 0.87 (95% CI: 0.79-0.97; P = .013)] compared to those less 25 years; and unmarried [aPR = 0.89 (95% CI: 0.82-0.97; P = .011)] compared to the married. Compliance with the COVID-19 presidential lockdown measures in northern Uganda was high. The factors associated with compliance were the fear of death and agreement with presidential lockdown measures. However, compliance was less likely among males, unmarried persons, and persons aged 35 to 44. The authors recommend more community engagements, participation, sensitization, mobilization, and simultaneous application of multiple public health approaches to improve compliance and control of COVID-19.
Keywords: COVID-19 lockdown measures, compliance, prevalence, associated factors
What do we already know about this topic?
The lockdown measure was one of the public health approaches to control COVID-19 in Africa.
The degree of lockdown strictness varied from one African country to another.
Lockdown measures prevented an exponential spread of COVID-19 in the African continent.
Lockdown measures had adverse economic, psychosocial, and mental health effects on the African population.
How does this research contribute to the field?
Lockdown measures in Uganda followed a strict stay-home-regulation issued by the President of Uganda.
It was more likely for those who agreed to presidential lockdown directives to comply.
It was more likely for those afraid of death due to COVID-19 to comply with the presidential lockdown measures.
It was less likely for unmarried persons, males, and participants aged 35 to 44 years to comply with the presidential lockdown directives.
Formation of multi-stakeholder COVID-19 taskforces from National to community levels helped to disseminate information on COVID-19 to communities in Uganda.
What are your research’s implications for theory, practice, or policy?
Forming multi-stakeholder COVID-19 taskforces from national to community levels helps to manage and disseminate information on COVID-19 to communities.
Multiple and simultaneous applications of public health approaches are helpful in epidemic control.
The strong leadership at national level and regular information updates during an epidemic are critical for control.
Introduction
The coronavirus disease 2019 (COVID-19) is one of the world’s most significant global uncertainties.1,2 Much effort has gone into implementing COVID-19 pandemic control strategies worldwide around, for example, instituting lockdown measures, travel bans, isolation of confirmed cases and close contacts, social distancing, wearing facemasks, and other hygiene measures. Still, some experts have suggested that the virus will resurface after lifting these measures.2,3
A Global Fund (GF) survey of health facilities in 24 African countries found that 50% of these facilities recorded COVID-19 infections among all categories of health workers between April and September 2020. 4 In the same period, 67% of health facilities reported that 10% of medical staff were absent from duties. 4 Sickness due to COVID-19 or having to quarantine because of exposure to the virus was the primary reason for health staff absenteeism in 19% of these health facilities. 4 Moreover, only 38% of the surveyed health facilities had the four essential personal protective equipment items: facemasks, disinfectants, gloves, and hand sanitizers. 4
As part of the effort to mitigate the impact of COVID-19 on healthcare in Africa, health workers and the general population were advised to adhere to COVID-19 prevention measures. 4 In addition, many African countries implemented lockdown measures at varying degrees of strictness and duration to prevent the exponential spread of the virus. 4
A case in point is Uganda, where a second presidential directive on lockdown measures was placed at a time when there was a resurgence of COVID-19 (June to July 2021), and there was a high community transmission of the virus. At the time of our study (October to November 2021), the country had just eased a presidential order (lockdown measures), which included the implementation of 53-day stay-at-home orders, social distancing, hand hygiene, and mandatory wearing of facemasks when in public. 5
Experts and public health specialists suggest that knowledge, perceptions, compliance, attitudes, behaviors, and practices 5 influence populations’ adherence to these COVID-19 control measures. 5 Also, perceptions, compliance, and practices are interwoven and influence a person’s actions in a period of uncertainty, for example, the COVID-19 pandemic. 5 Thus, the African population should have adequate knowledge of COVID-19 prevention policies to have positive attitudes and appropriate practices that reduce the risk of catching COVID-19. 5
Assessing knowledge, attitudes, perceptions (KAP), and compliance with COVID-19 among the population can aid managers and policymakers in identifying critical gaps in training, policies, and practices that should be addressed. 5 Notably, some African studies have assessed perceptions and compliance with COVID-19 lockdown measures and the use of facemasks among the population.6 -10 They reported adequate COVID-19-related compliance among health workers, but others found significant gaps.6 -8
In mid-2021, community transmission of COVID-19 in Uganda resulted in an exponential spread of the virus across most districts of with resulting public health, economic, and socio-political implications. 11 As the World Health Organization (WHO) recommended, several pandemic response activities were instituted by the government of Uganda to curb the spread of coronavirus disease (COVID-19). 12 These activities included isolation, quarantine, global lockdown measures, movement restrictions, and community containment strategies. 12 that In addition to the lockdown measures, social distancing (SD)/physical distancing (PD), hygiene practices, and wearing facemasks were considered critical non-pharmaceutical public health interventions have proven effective in limiting community transmission of the virus (SARS-CoV-2). 13
The current study determined the prevalence and factors associated with compliance with the presidential directives on COVID-19 lockdown measures among the population of northern Uganda. The findings from this study are significant as they may inform Uganda’s national COVID-19 task force in designing strategies for preventing and controlling prevention the virus as the country is facing many challenges of data scarcity. Information on compliance with infection, prevention, and control (IPC) and Standard Operating Procedures (SOPS) of COVID-19 in northern Uganda are crucial at this pandemic stage as the country is struggling to control the community’s spread of the virus. In addition, understanding factors associated with compliance will be extremely valuable for informing future mitigation strategies and targeted messaging to ensure high compliance with mitigation strategies should Uganda experience a resurgence of COVID-19 or to prepare for future pandemics.
Therefore, this study aimed to determine the prevalence and factors associated with compliance with Uganda’s presidential 53-day lockdown from June to July 2021.
Methods
Study design: We conducted a cross-sectional study in the Acholi subregion of northern Uganda between October and November 2021.
Study sites and background information of the study area: This study was conducted among adult (≥18 years) community members in northern Uganda. In the outpatient departments (OPDs) of health facilities in Gulu City, Nwoya, Omoro, Lamwo, Kitgum, Agago, Amuru, Pader, and Gulu districts in the Acholi subregion. 14
The Acholi subregion has just emerged from a 20-year-old civil war between the Government of Uganda and the rebel Lord’s Resistance Army (LRA), and the population is in the postwar recovery period. 15
There are nine districts in the Acholi subregion with an estimated population of approximately 2 million. 16 During the study (October to November 2021), Uganda had just eased the second lockdown measures after the second wave of coronavirus disease -19 (COVID-19), 17 and the number of COVID-19 patients had significantly reduced in COVID-19 Treatment Centers (CTUs) in most health facilities in northern Uganda. 17
At the time of our study, Uganda had just adopted a home-based care approach for the management of mild cases of COVID-19. Therefore, reduction in the number of COVID-19 cases in CTUs may not be fully accounted for by patients in communities but rather a general decrease in cases in northern Uganda. However, in both scenarios, health workers were still the frontline workforce, especially nurses, doctors, and laboratory staff, who had to conduct community supervision of cases in the home-based care management approach. 17
In addition, district task forces set up by the Government of Uganda along layers of administrative structures (from national to community levels) to support community management, prevention, and control of COVID-19, met weekly to discuss new developments and strategies. 18
Furthermore, the President of Uganda had announced new work methods in public facilities, where only 30% of staff in public and private organizations were allowed in offices full-time. 18 These COVID-19 control measures were to disrupt day-to-day contact between management, administration, public officials, and the community to end the cycle of physical person-to-person contact to break the transmission cycle of COVID-19. 18
Study participants: The survey was conducted on 587 adult participants who were outpatient attendees or attendants at 24 health facilities (hospitals, health Centre Four (HCIV), and Health Centre Three (HCIII) in 9 districts of the Acholi sub-region in northern Uganda. Only adult community members (18 years and above) who provided written informed consent were recruited to participate in the study. The recruitment and interviews of participants in each health facility were carried out every day for 1 week. Participants who could not speak (due to speech disability or inability to talk and not a language barrier) and were not residents of the Acholi subregion in northern Uganda 6 months before the study were excluded. Interestingly, only 2 potential participants declined to participate in the survey, constituting 2/589(0.34%) of the study population. Thus, the response rate to this study was 587/589(99.7%).
Sample size estimation: The study population’s sample size was calculated using the Raosoft calculator. The computation was based on a 50% response distribution, 5% margin of error, and 95% Confidence Interval (CI). This online software foundation is based on a widely utilized descriptive studies’ sample size estimation formula.19,20 Based on an assumption of a total eligible population size of 50 000 (12.5% of adults above 18 years old in the Acholi subregion that visits health facilities) in 9 districts of the Acholi subregion in 2 months.
Where n = Sample size
N = the population size (50 000 people)
e = margin of error at 5%
Substituting the formula
Add, 10% for non-response, 39.7 + 397 = 437
Based on the above assumptions, the minimum sample size and factoring in a 10% non-response rate is 437. However, by the end of the data collection process, we had interviewed 587 participants.
Sampling technique: A systematic sampling technique of attendants or attendees was used to recruit participants from the 24 selected health facilities’ outpatient departments in the Acholi sub-region. The 24 selected health facilities were estimated to provide outpatient health services to 50 000 people every 2 months. We selected every third attendee or attendant of outpatients’ departments in each chosen health facility for 1 week in 9 districts of the Acholi subregion until the sample size was achieved.21,22
We defined systematic sampling as a probability sampling method where researchers select population members at regular intervals.21,22 We chose this sampling technique because it allowed us to get the desired sample size in the shortest period, reducing the risk of our study team acquiring COVID-19.
In addition, we chose health facilities because it was the most convenient place to receive participants for interviews as most population was still apprehensive about receiving visitors or researchers in their homes or offices, or public places as the Government of Uganda had just eased the lockdown measures, and the population was still in fear of catching the virus.
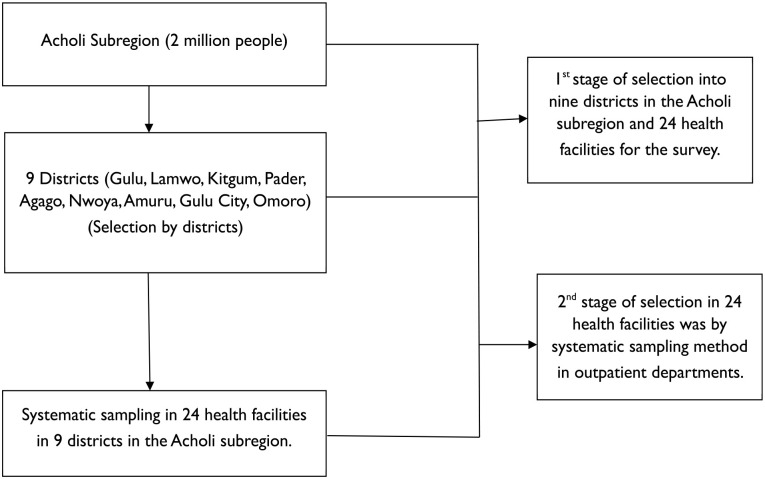
Also, outpatients of health facilities had the required facilities for infection, prevention, and control (IPC) and standard operating procedures (SOPs) that allowed interviewees and interviewers to interact while following COVID-19 standard protocols (Figure 1). Last but most importantly, a systematic sampling method helps to minimize biased samples and poor survey results in addition to eliminating clustered selection with a low probability of contaminating data21,22 which was the ideal situation the research team had to achieve (Figure 1).
Figure 1.
Sampling of participants in 9 districts of the Acholi subregion in northern Uganda.
Data collection procedures: Data collection in each health facility’s OPD was conducted every day for 1 week, beginning at 9:00 am and ending at 6:00 pm. The OPD register was the sampling frame for participants’ selection. Every day at 9:00 am in the OPD of the 24 health facilities, the research team checked the register of attendants and selected every third attendant to seek their consent for an interview. Once the person agreed to be interviewed, the interviewee was taken through a complete consenting process by explaining in detail the protocol, its importance, potential risks, benefits, and usefulness of the research. If a participant agreed to have understood the study, the person was made to sign the consent form, completing the interview process. Those who refused to be interviewed were allowed to proceed with their activities with the assurance that they would not face any penalty based on their position. The team then looked for the next potential participant from the OPD registry and repeated the process throughout the day until there were no more clients. Attendants of selected attendees were also selected similarly, ensuring that there were no repetitions of participants.
Study variables: The dependent variable was compliance with the presidential stay-at-home orders/lockdown measures (the outcome variable). The independent variables were socio-demographic characteristics (age, sex, occupation, marital status, religion, districts, tribes, residences, occupation, level of education, nationality, race, employment status, comorbidities, smoking, alcohol use, and participants’ perceptions on the lockdown measures.
Instruments for data collection: We collected data from participants using a pre-tested questionnaire with an internal validity of Cronbach’s α = .72. The questionnaire was designed in English by the research team to obtain information on COVID-19 after the second wave and lockdown measures in Uganda. The questionnaire had 2 sections: Section A contained information on participants’ socio-demographic characteristics (age, sex, occupation, tribe, religion, district, employment status, race, highest level of education attained, marital status, and habits such as smoking and alcohol use), while section B assessed participants’ perceptions and compliance with the presidential stay-at-home orders/ lockdown measures.
In this, consenting adult persons participated in a face-to-face questionnaire interview, which lasted 30 to 40 min in a nearby quiet of a health facility’s OPD room. Study participants and interviewers followed COVID-19 infection, prevention, and control measures (IPC) and standard operating procedures (SOPS). The face-to-face interview approach was preferred instead of an online approach to reach out to many participants as previous surveys showed that there were very few online and internet users in northern Uganda. 23
Ethical approval: This study was approved by St. Mary’s Hospital Lacor Institutional Research and Ethics Committee (LHIREC No.0192/10/2021). Informed consent was obtained from each adult participant aged ≥18 years. Confidentiality of information of participants was maintained by the research team, with all personal data de-identified and kept under lock and key. The Department of Surgery, Faculty of Medicine of Gulu University, archived the residual data.
Data analysis: Data was analyzed using Stata 17.0, and Microsoft Excel 2019 was used to generate graphs and plots. We performed descriptive analyses of participants’ socio-demographic characteristics and summarized categorical variables as proportions and continuous variables as means, standard deviations, and ranges. We estimated the extent of agreement and compliance with the 53-day lockdown measures using prevalence ratios (PR) at a 95% Confidence Interval (CI). Findings were additionally presented as frequencies, proportions, bar charts, and heat plots. Independent variables selected from related literature on COVID-19 lockdown measures were age, sex, occupation, level of education, employment status, race, nationality, tribes, religion, districts, addresses, comorbidity, smoking and drinking status, marital status, perceptions of COVID-19. While the dependent variable was compliance with the presidential directives on lockdown measures, a binary outcome was defined as participants reporting fidelity to the lockdown measures, recorded as (1) for “yes” and (0) for “no.”
We then performed a univariable modified Poisson regression to examine the association between the dependent and each independent variable, reporting results as crude prevalence ratios (crude PR) and their respective P values at 95% Confidence Intervals.
All selected independent variables were then entered into a multivariable modified Poisson regression model and regressed to determine factors associated with compliance with the presidential 53-day lockdown measures. Further, after fitting the multivariable regression model, we assessed the collinearity between independent variables using the variance inflation factor (VIF) method. VIF values were all less than 2 (<2), indicating negligible collinearity. We reported results as adjusted Prevalence Ratios (aPR) with their respective P values and 95% Confidence Intervals. A P-value less than .05 was considered statistically significant.
Results
This study was conducted among the adult population in northern Uganda (Figure 1), where we achieved a questionnaire response rate of 587/589 (99.7%). The majority of participants agreed with presidential lockdown (stay-at-home) directives at 86% (95% CI: 84%−89%) and high compliance with the directives at 88% (95% CI: 85%−90%).
As illustrated in Figure 2, most participants agreed to 507/587 (86.4%) and had high compliance 515/587 (88.0%) with the presidential directives on COVID-19 lockdown (stay-at-home) measures in Uganda.
Figure 2.
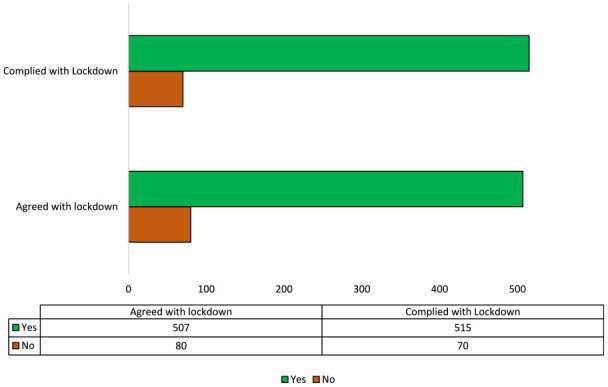
Agreement and compliance with lockdown directives among participants in northern Uganda.
Participants’ Sociodemographic Characteristics
As shown in Table 1, most participants were males 335 (57.1%); 25 to 34 years 180 (30.7%); married 341 (58.9%); Catholics 312 (53.2%); tertiary level of education 261 (44.5%); Acholi 425 (72.9%); health professionals 136 (23.2%); Ugandans 581 (99.0%); did not use alcohol 401 (69.0%); did not smoke cigarettes 545 (94.1%); had no diabetes mellitus 571 (97.3%); no heart diseases 571 (97.3%); no obesity 578 (98.3%); no hypertension 559 (95.2%); no asthma 572 (97.4%); no HIV and AIDS 577 (98.3%) and no other chronic diseases, 542 (92.3%). The mean age of participants was 33.3 years (SD ± 11.1), with a minimum of 18 years and a maximum of 75 years.
Table 1.
Sociodemographic and Health Background Characteristics of Participants.
| Sociodemographic characteristics | N (%) | |
|---|---|---|
| Sex | Female | 252 (42.9) |
| Male | 335 (57.1) | |
| Age in years | <25 | 150 (26.2) |
| 25-34 | 180 (31.4) | |
| 35-44 | 157 (27.4) | |
| >45 | 86 (15.0) | |
| Marital status | Married/Cohabiting | 341 (58.9) |
| Unmarried/Others | 238 (41.1) | |
| Religion | Catholic | 312 (53.2) |
| Protestant | 245 (41.7) | |
| Others | 30 (5.1) | |
| Tribe | Acholi | 425 (72.9) |
| Lango | 41 (7.0) | |
| Others | 117 (20.1) | |
| Districts | Gulu-Omoro | 220 (37.5) |
| Kitgum-Lamwo | 133 (22.7) | |
| Amuru-Nwoya | 92 (15.7) | |
| Agago-Pader | 86 (14.7) | |
| Others | 56 (9.5) | |
| Level of education | Tertiary | 261 (44.5) |
| Secondary | 225 (38.3) | |
| Primary | 64 (10.9) | |
| None | 37 (6.3) | |
| Occupation | Health Professional | 136 (23.2) |
| Agriculture/Self-employed | 115 (19.6) | |
| Employed/Retired | 82 (14.0) | |
| Student/Unemployed | 105 (17.9) | |
| Others | 149 (25.4) | |
| Nationality | Ugandans | 581 (99.0) |
| non-Ugandans | 6 (1.0) | |
| Race | Africans | 586 (99.8) |
| Caucasians | 1 (0.2) | |
| Health background and habits (Yes and No answers) | ||
| Alcohol use | No | 401 (69.0) |
| Smoking status | No | 545 (94.1) |
| Diabetes | No | 571 (97.3) |
| Heart diseases | No | 571 (97.3) |
| Obesity | No | 578 (98.5) |
| Hypertension | No | 559 (95.2) |
| Asthma | No | 572 (97.4) |
| HIV | No | 577 (98.3) |
| Other diseases | No | 542 (92.3) |
| Views of participants on COVID-19 lockdown measures | ||
| Agreed with the lockdown measures | Yes | 507 (86.4%) |
| Availability of major needs | Yes | 157 (26.8%) |
| Availability of food and money | Yes | 127 (21.6%) |
| Desire to prevent the infection from spreading | Yes | 283 (48.2%) |
| Fear of contracting COVID-19 | Yes | 227 (38.7%) |
| The fear of death | Yes | 408 (69.5%) |
Note. Table 1 shows sociodemographic characteristics, health backgrounds, and participants’ views on COVID-19 lockdown measures. Most participants were males 335 (57.1%); in the age group of 25 to 34 years 180 (30.7%); married or cohabiting 341 (58.9%); Catholics 312 (53.2%); had tertiary level of education 261 (44.5%); Acholi by tribe 425 (72.9%); health professionals 136 (23.2%); Ugandans 581 (99.0%); did not use alcohol 401 (69.0%); did not smoke cigarettes 545 (94.1%); had no diabetes mellitus 571 (97.3%); no heart diseases 571 (97.3%); no obesity 578 (98.3%); no hypertension 559 (95.2%); no asthma 572 (97.4%); no HIV and AIDS 577 (98.3%) and no other chronic diseases, 542 (92.3%). Most participants agreed with the lockdown measures 507 (86.4%); availability of major needs 157 (26.8%); availability of food and money 127 (21.6%); desire to prevent the COVID-19 from spreading 283 (48.2%); the fear of contracting COVID-19, 227 (38.7%) and the fear of death, 408 (69.5%).
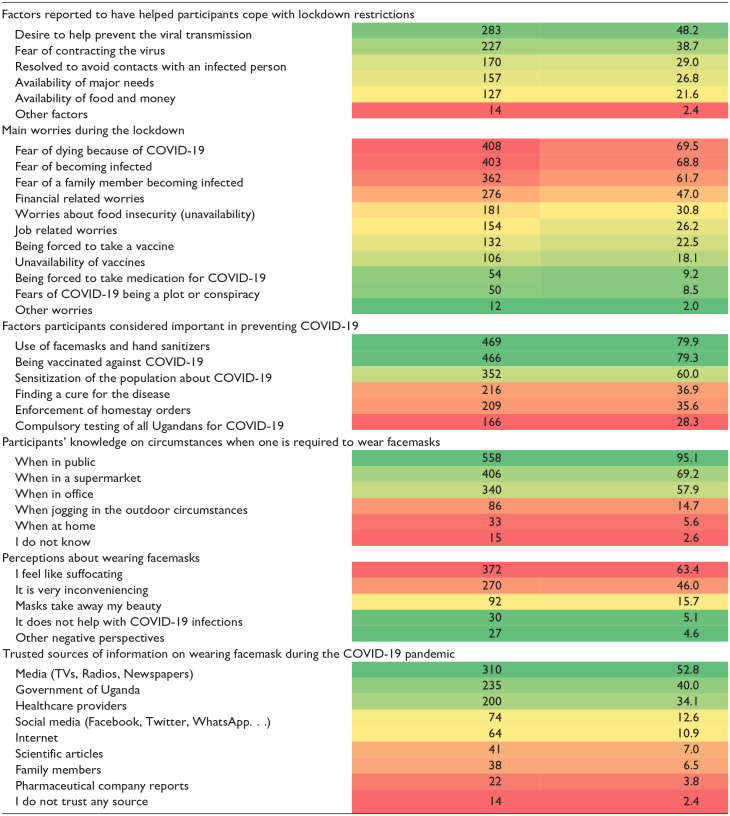
Heat Plot Showing Participants’ Perspectives on COVID-19 Control Measures and Media Sources
Participants’ perceptions of COVID-19 were assessed, and most considered the desire to help prevent the transmission of the virus as the reason they complied with the lockdown measures 283 (48.2%); the main worry during the lockdown was the fear of death from the virus 408 (69.3%); most considered the use of facemasks, hand sanitizers 469 (79.9%) and getting vaccinated 466 (79.3%) as necessary for preventing COVID-19; most considered wearing facemasks when in public as one of the most critical interventions for the control of COVID-19 558 (95.1%); most felt suffocated when wearing facemasks 392 (63.4%) and mass media (TV, Radios, and newspapers) were the most trusted sources of COVID-19 media information on wearing facemasks 310 (52.8%) (Table 2).
Table 2.
Heat Plot Showing Participants’ Perspectives on COVID-19 Control Measures and Media Sources.
| Assessment of participants’ perspectives | People reporting being worried. | |
|---|---|---|
| N = 587 | % | |
| ||
This was a multiple-response question, so the total percentage is >100.
The heat plot table used a traffic coding system with a spectrum of colors between green and red, with green denoting low-denoting-low/good, yellow for medium, and red for high/bad.
A Multivariable Modified Poisson Regression Analyses on Presidential Directives on Lockdown Measures
Participants who agreed with the lockdown measures were 28% more likely to comply with the lockdown measures compared to those who disagreed, aPR = 1.28, 95% CI: 1.10 to 1.49; P = .001. Also, participants who feared death from COVID-19 were 8% more likely to comply with lockdown measures than those who did not aPR = 1.08, 95% CI: 1.01 to 1.15; P = .023. However, compliance was less likely among males, aPR = 0.91, 95% CI: 0.86 to 0.97; P = .002 compared to females; age-group of 35 to 44 years, aPR = 0.87, 95% CI: 0.79 to 0.97 compared to less than 25 years; unmarried participants aPR = 0.89, 95% CI: 0.82 to 0.97; P = .011 compared to married participants (Table 3).
Table 3.
Bivariable and Multivariable Modified Poisson Regression Analysis of Factors Associated With Compliance With the Lockdown Measures in Northern Uganda.
| Independent variables | Crude PR | 95% CI | P value | Adjusted PR | 95% CI | P value | |
|---|---|---|---|---|---|---|---|
| Sociodemographic factors | |||||||
| Sex | Female | 1 | 1 | ||||
| Male | 0.91 | 0.86-0.96 | .001 | 0.91 | 0.86-0.97 | .002* | |
| Age (years) | <25 | 1 | 1 | ||||
| 25-34 | 0.97 | 0.91-1.05 | .457 | 0.94 | 0.85-1.03 | .174 | |
| 35-44 | 0.91 | 0.84-0.99 | .036 | 0.87 | 0.79-0.97 | .013* | |
| >45 | 0.98 | 0.90-1.07 | .637 | 0.91 | 0.82-1.02 | .106 | |
| Marital status | Married/cohabiting | 1 | 1 | ||||
| Unmarried/others | 0.96 | 0.90-1.03 | .249 | 0.89 | 0.82-0.97 | .011* | |
| Level of education | Tertiary | 1 | 1 | ||||
| Secondary | 1.04 | 0.97-1.11 | .310 | 1.02 | 0.95-1.11 | .554 | |
| Primary | 1.11 | 1.03-1.20 | .005 | 1.06 | 0.96-1.17 | .251 | |
| None | 1.01 | 0.88-1.16 | .905 | 1.03 | 0.90-1.18 | .693 | |
| Occupation | Health professional | 1 | 1 | ||||
| Agriculture/self-employed | 1.01 | 0.93-1.10 | .832 | 0.97 | 0.87-1.09 | .643 | |
| Student/unemployed | 1.03 | 0.95-1.112 | .456 | 0.98 | 0.87-1.09 | .663 | |
| Employed/retired | 0.98 | 0.88-1.08 | .662 | 0.99 | 0.90-1.10 | .907 | |
| Others | 0.91 | 0.83-1.00 | .062 | 0.91 | 0.81-1.01 | .087 | |
| Alcohol use | No | 1 | 1 | ||||
| Yes | 0.91 | 0.85-0.98 | .017 | 0.93 | 0.86-1.00 | .063 | |
| Smoking cigarettes | No | 1 | 1 | ||||
| Yes | 0.97 | 0.84-1.12 | .642 | 1.07 | 0.90-1.29 | .44 | |
| Underlying health conditions | |||||||
| Diabetes | No | 1 | 1 | ||||
| Yes | 0.99 | 0.82-1.20 | .948 | 1.06 | 0.83-1.36 | .636 | |
| Heart diseases | No | 1 | 1 | ||||
| Yes | 0.92 | 0.73-1.17 | .497 | 0.89 | 0.70-1.14 | .374 | |
| Obesity | No | 1 | 1 | ||||
| Yes | 1.01 | 0.80-1.28 | .934 | 0.97 | 0.73-1.29 | .842 | |
| Hypertension | No | 1 | 1 | ||||
| Yes | 1.01 | 0.89-1.16 | .826 | 1.03 | 0.92-1.16 | .598 | |
| Asthma | No | 1 | 1 | ||||
| Yes | 0.83 | 0.61-1.13 | .232 | 0.84 | 0.631.13 | .249 | |
| HIV | No | 1 | 1 | ||||
| Yes | 1.02 | 0.83-1.26 | .833 | 0.98 | 0.74-1.30 | .902 | |
| Psychosocial and behavioral factors | |||||||
| Agreed with lockdown measures | No | 1 | 1 | ||||
| Yes | 1.31 | 1.13-1.153 | <.001 | 1.28 | 1.10-1.49 | .001* | |
| Availability of major needs | No | 1 | 1 | ||||
| Yes | 1.02 | 0.95-1.09 | .621 | 1.03 | 0.96-1.11 | .414 | |
| Availability of food and money | No | 1 | 1 | ||||
| Yes | 0.96 | 0.88-1.04 | .280 | 0.97 | 0.89-1.05 | .421 | |
| Desire to prevent infection spread | No | 1 | 1 | ||||
| Yes | 1.07 | 1.01-1.14 | .023 | 1.06 | 0.99-1.12 | .089 | |
| Fear of contracting COVID-19 | No | 1 | 1 | ||||
| Yes | 1.06 | 1.00-1.12 | .054 | 1.02 | 0.97-1.08 | .436 | |
| Fear of death | No | 1 | 1 | ||||
| Yes | 1.11 | 1.041.19 | .003 | 1.08 | 1.01-1.15 | .023* | |
Compliance was defined as participants reporting agreeing with the 53-day lockdown measures.
Note. In Table 3, factors associated with compliance with COVID-19 presidential lockdown measures were those who agreed with the measures aPR = 1.28, 95% CI: 1.10 to 1.49; P = .001 compared to those who did not and likely among those who were afraid of death from COVID-19, aPR = 1.08, 95% CI: 1.01 to 1.15; P = .023 compared to those who did not. However, compliance was less likely among males aPR = 0.91, 95% CI: 0.86 to 0.97; P = .002 compared to females, those aged 35 to 44 years aPR = 0.87, 95% CI: 0.79 to 0.97; P = .013 compared to those less 25 years; and unmarried aPR = 0.89, 95% CI: 0.82 to 0.97; P = .011 compared to the married.
Discussion
As COVID-19 spread globally, it was critical to establish regulations on strengthening control and flattening the epidemic curve through measures such as restrictions on movements and physical contact. This study found a high compliance with the presidential directives on COVID-19 lockdown measures among people in northern Uganda between June and July 2021. Compliance with lockdown measures, a “stay-at-home” policy, was 88.0% (Figure 2). The high compliance with prevention and control measures reported in northern Uganda is commendable and may have contributed to the low prevalence of COVID-19 observed throughout the pandemic. 24
In addition, Uganda experienced a much lower COVID-19 prevalence and mortality compared to many countries globally, with achievements that can be partially attributed to the high compliance with the lockdown measures by the population, decisive leadership by Uganda’s President and Ministry of Health, and simultaneous application of multiple public health measures for the control of COVID-19.24 -26 Many scholars suggest that enforcement and compliance with preventive measures such as wearing facemasks, hand hygiene, and physical distancing in a population stabilized the outbreak or halted the viral transmission.24 -27 For example, a halt to the viral transmission was observed in the USA when the State of Arizona enforced the wearing of facemasks and other preventive measures. Cases of COVID-19 reduced by 75% in 1 month. 28
Public health experts and scholars suggest that the Ministry of Health’s mass sensitization, mobilization, and engagement of the Ugandan population on the severe risks posed to the population may have persuaded the people of northern Uganda to comply with the presidential directives. 14 This is consistent with evidence from the rest of Africa, which noted that compliance with lockdown measures contributed to lowering the effective reproduction rate of COVID-19 in many sub-Saharan African countries.7,8
Also, studies from 9 sub-Saharan African countries showed that lockdown measures ranged from the strictest to the most liberal (or none) during the COVID-19 pandemic. 7 For example, there was a general reference to varying degrees of lockdown across sub-Saharan African (SSA) countries, such as total and partial lockdown or tight lockdown and loose lockdown. 8
However, logic and evidence from elsewhere in many countries in sub-Saharan Africa indicate that lockdown measures lowered the effective reproduction rate of the virus,7,8 and geographic containment, travel restrictions, and prohibition of large gatherings inhibited community transmission of the virus in many African countries. 7
In many ways, the relatively more significant percentage of people living in rural areas where there were naturally more physical distances and less population mixing in many sub-Saharan African countries contributed to the prevention of large national epidemic spikes. 7
Our current study finding contrasts with another among participants in supermarkets in central Uganda, which reported low compliance with COVID-19 preventive measures in 2021. 26 Differences in results between the two studies could partly be due to differences in the timing and regions when and where the two studies were conducted. The central Ugandan study was undertaken during the first wave of COVID-19. However, ours was conducted in northern Uganda after the second COVID-19 wave, when there were higher hospitalization and case fatalities than the first wave.29,30 Thus, the higher compliance in our study could have likely been influenced by the experience of witnessing the suffering of loved ones from COVID-19 in the second wave compared to the first, hence committing to the strict stay-at-home measures.
As for differences in the region, a few studies in Uganda showed that compliance with lockdown measures and other non-pharmaceutical measures was higher in northern and eastern Uganda compared to western and central regions of Uganda, a factor that may have been at play in these two studies.28,29 This may partly be due to the need for more lack of confidence and trust in government directives by the population in the significant central region of Uganda because of current and past negative perceptions of the current Government.18,31,32
The need to preserve life was strong among the study population during the second wave of COVID-19 in Uganda. This was evidenced by a strong association between compliance with the lockdown measures and the fear of death (P = .023), whereby other priorities like the lack of major needs had a limited effect on the population (P = .414) (Table 3). Another distinction between the two studies was that the study among supermarket attendees used direct observations to obtain data on participants’ behavior as opposed to this study, which relied on participants’ self-report, which could have resulted in over-reporting of compliance due to pressure to provide a more socially desirable response.
Furthermore, the high compliance reported in our study population could have resulted from the Uganda Government’s use of security forces to strictly enforce COVID-19 control measures in this region.33,34 This controversial intervention was effective in this region that only recently emerged from 20 years of brutal rebel insurgency by the Lord’s Resistance Army (LRA).
Also, we found that compliance with the lockdown measures varied across different groups of people in northern Uganda (Table 3). For example, we found that people who agreed to the lockdown measures or were afraid of death due to COVID-19 were more likely to comply with the presidential lockdown directives than the rest of the population. On the other hand, it was less likely for males, unmarried persons, and age-group of 35 to 44 years, to comply with the presidential directives on lockdown measures (Table 3).
Several researchers have emphasized the importance of a population’s agreement to forego their usual lifestyles, accept constraints, and comply with government epidemic control directives and regulatory measures as critical pillars for effective epidemic and pandemic management.25,26,31,32,35,36
Gender differences in perceptions and compliance with COVID-19 control measures have also been noted in past studies.37,38 Another Ugandan study found that while both males and females recognized the importance of COVID-19 in their households, more than half (52.9%, 54/102) of male participants perceived that they were more likely to die of COVID-19 than their female counterparts, even though most women disagreed with that perception (PR = 1.8, 95% CI: 1.1-2.7). 39 Findings in that Ugandan study that risks perceptions of COVID-19 among women differed from males were worrying as more elderly males in Europe, for example, were the most severely affected. 27
Even though the Ugandan study was exploratory and did not follow the European findings, these observations warrant more worries for Ugandan population. 27 Differences in risk perceptions between females and males on COVID-19 infection have implications on compliance with lockdown measures, infection, prevention, and control (IPC), and standard operating procedures (SOPS) for the control and prevention of COVID-19 in Uganda. 27 We, the authors, were, however, not surprised to find in our study that males were less likely to follow the presidential lockdown directives during the pandemic in northern Uganda (Table 3) as this has often been observed with other health services, including vaccination, HIV testing, reproductive health, antenatal services for their wives, and cancer screening.31,32
Even though compliance levels to lockdown measures varied among countries in the African continent, many sub-Saharan (SSA) countries demonstrated a high level of compliance with avoiding crowded places, observed wearing of facemasks, and regular handwashing during the pandemic. 8 That study finding is consistent with ours, where factors associated with compliance and mitigating practices were having adequate COVID-19-related knowledge and the perceived high risk of contracting the virus except age, marital status (married), and sex (females). 8 On this, some experts argue that differences in compliance rate among sub-Saharan African (SSA) countries and populations may suggest a direct link between varying degrees of the strictness of lockdown measures, sensitization, and education of citizens, especially among the vulnerable groups.7,8
Unlike some studies from SSA, our study found that unmarried participants were less likely to comply with the presidential directives on lockdown measures than married participants (Table 3). Some researchers suggest that married people were more likely to understand better the risks involved with COVID-19 to themselves and their families, and so have considered opinions about protecting themselves and their families. The responsibility to each other and family seems more persuasive to married people to adhere to public health measures to protect themselves and their families from the virus.32 -35,40 One study across several sub-Saharan African countries also found that people with a high-risk perception of contracting COVID-19 infection had higher compliance rates with COVID-19 control measures than others. 8 Likely, the fear of death and the risks of infecting family members may have influenced our study population to comply with the presidential directives on lockdown measures in northern Uganda (Tables 1-3).
In contrast to our cross-sectional findings, another Ugandan study 27 noted like the UK, 41 that compliance levels of the population to SOPs drastically declined over the years of the pandemic, which was depicted by increasing numbers of COVID-19 cases and deaths at community level. 42 This finding was not unexpected, as many instances of COVID-19 in Ugandan communities remained unreported due to the constrained SARS-CoV-2 testing capacity of the healthcare system and the introduction of a home-based care management system during the pandemic. Still, the overall prevalence of COVID-19 remained low throughout the pandemic in Uganda.42,43
In this study, we described compliance as being established guidelines, presidential directives 44 or specifications, or the process of becoming or having regard for lockdown measures, IPC, and SOPs on COVID-19. Similarly, community compliance was defined as attachment or commitment to a cause, directives, 44 and belief as interpreted in the community and, in this case, the COVID-19 IPC and SOP guidelines and lockdown measures put in place by the Government of Uganda/presidential directives. 44
Inconsistent with our study findings, experience from other countries brings to light some of the major challenges in communication, behaviors, and beliefs of the population during the COVID-19 lockdown period. 45 For example, cultural beliefs in Iran, certain religious beliefs and behaviors caused people to pay less attention to health issues during the COVID-19 pandemic. 45 Fatalism, and unfaithfulness to health problems were part of these beliefs and behaviors in which participants were being labeled fastidious and foppish by colleagues if health guidelines were observed. 45 Some participants’ beliefs were rooted in the religion because most followers of Islam believed that life and death were in the hands of God and our behaviors did not affect the time of our death. 45 So, they did not need to observe health norms including guidelines in the management of the pandemic. 45
Also, other beliefs were rooted in the culture and socialization of the people because, in Iranian society, non-observance of health issues was considered being courageous and its observance was considered being fearful, and those who observed health guidelines were labeled cowards. 45
In addition, the belief that the destiny of people’s lives was predetermined was prevalent among their participants. 45
This was challenging information to deal with because individual rights and will were taken away by this religious belief. Also, in Iranian society, those who observed health guidelines were stigmatized as being fastidious and cowards by those around them, and this played a role in non-observance of health rules during the COVID-19 pandemic. 45
Another in-depth research results from Iran showed that various individual, socio-cultural, economic, and structural factors influenced the non-observance of health advice during the COVID-19 pandemic including low numbers of preventive behaviors among people in high-risk jobs. 46 Personality traits, including carelessness, impatience, laziness, risk-taking, and frustration were among the individual factors that led to the negligence of warnings and non-observance of health guidelines during the pandemic. 46 Several studies have shown that personality traits can be effective in neglecting healthy behaviors, even those recommended by the country’s health Ministry. 46
The lack of self-efficacy was another contributing individual factor for not observing the health rules during the COVID-19 in Iran. 46 Hence, many people found themselves unable to observe health norms. 46
Furthermore, a survey in Canada by Blendon et al 47 found that the absence of medical treatment during quarantine and lockdowns were cited by many participants as a problem during the COVID-19. 47 Other participants’ personal concerns including fears and anxiety about having COVID-19 and their family were consistent with prior studies on SARS and Ebola.48 -52 Other studies conducted by Wu et al, 53 and Zheng et al, 54 found that most participants were concerned about the spread of COVID-19, which impacted their quality of life.
In our study, there was a high compliance to lockdown measures, and this was strictly enforced by Ugandan security forces.42 -44 Our study, however, did not explore what happened in families of people who had COVID-19 patients. However, experience from other countries such as Iran provide an insight to the challenges faced by such families. For example, one study, Lebni et al, explored through experiences of COVID-19 victims’ families who were being rejected by others due to societal stigma. 55 It is reported that during the epidemic, stigma, followed by social isolation rises as a result of people’s fear and anxiety about a sickness with an unknown source and a potentially lethal conclusion. 56
Several studies found that stigma and rejection were common during the COVID-19 pandemic.57 -59 According to findings of Kim’s study, nurses experienced social rejection and avoidance as a result of their direct interaction with COVID-19 patients. 60 The COVID-19 pandemic, according to Bhattacharya et al, had resulted in societal stigma and discriminatory conduct among patients and their relatives. 61 So, in addition to people with COVID-19 being rejected by society, their families and carers were also shunned. 61 This rejection, which stems from the patient’s fear of the disease and death, as well as the high prevalence of rumors and conspiracy theories, persisted even after the patient healed or died.55,61 While victims’ families needed help from family connections more than ever at that time, they were being rejected, which made the process of adjusting to the death of relatives more challenging. 55
As part of a broader interest to determine the challenges experienced during the lockdown and stay-at-home policy, a study by Ahmadi et al, described experiences in Iran. 62 The study results showed the helplessness and limitations of staying-at-home and inability to do things in life and there were other challenges that people faced and resulted in chronic fatigue. 62 In another by Rahmatinejad et al, boredom and loneliness generated by prolonged quarantine caused by getting infected made patients bothered. 63 In the Iheduru—Anderson study in 2020, nurses also experienced burnout and helplessness due to prolonged illness and difficult working conditions. 64 Helplessness was referred to the situation in which people became disappointed with any improvement in their affairs and any controls over them and led to frustration and despair. 62 This was the case for COVID-19 patients, who got tired of the vague and uncertain situation in which they found themselves. 62
In one of the studies, we conducted recently, we found that there were limited access to information to many people during the lockdown period. 18 This experience was similarly observed among refugees in Iran. 65 The limited access to information resources and incomplete knowledge about COVID-19 was one of the interesting findings of their study. 65 Another study by Fouad et al among Syrian refugees in Lebanon showed that refugees had little knowledge of COVID-19. 66 Yücel also stated in his research that during the COVID-19 pandemic, Syrian refugees in Turkey were ignored by the media and this issue further aggravated information inequalities. 67
In another situation, Afghan women were deprived of access to information due to insufficient literacy to study and resources such as television, etc., and this deprivation made them very vulnerable during COVID-19 period because it deprived them of sufficient knowledge and awareness. 65 In addition, many participants had incomplete and little information about COVID-19 and how to prevent and treat it. 65 Therefore, it was necessary to educate women and to provide conditions for them to have access to various information about COVID-19.
Finally, despite the high poverty levels, and severe economic hardships posed by the national lockdown during the COVID-19 pandemic on citizens of Uganda, compliance with the presidential lockdown measures 44 and other non-pharmaceutical interventions varied across different regions. There was high compliance with the presidential directives on lockdown measures and a low prevalence of COVID-19 in northern Uganda from the time when a 53 day-national-lockdown was instituted in June-July 2021.
Strengths of This Study
This study has several strengths, which we highlight here. We had a large sample size of 587 participants, which allows for generalizing our findings to similar contexts. In addition, we included compliance measures that reflect a variety of critical behaviors for reducing COVID-19 transmission in Uganda.
Also, our wide range of compliance predictors revealed significant socio-demographic differences in between-person and within-person correlations relevant for consideration in epidemic control. Finally, the timing of the study after the second wave and lockdown measures provides valuable insights for future epidemic control in similar contexts.
Limitations of This Study
Being a cross-sectional study, the result of our research may have been skewed by unobserved confounding. In addition, we relied on self-reported compliance, which has the risk of social desirability and recall biases, which may result in over-reporting compliance. Furthermore, we only used data from the adult population which may not reflect adolescent opinions and views who are the majority in the general population of Uganda. Finally, most of our participants had secondary or tertiary education, which does not accurately reflect the demographics of northern Uganda’s general population.
Conclusion
Compliance with the presidential lockdown directives during the COVID-19 pandemic in northern Uganda was high. The factors associated with compliance include the fear of death and agreement with COVID-19 presidential lockdown directives. However, compliance was less likely among males, unmarried persons, and participants aged 35 to 44 years. The authors recommend more engagement, participation, sensitization, and mobilization of communities and the simultaneous application of multiple public health approaches to improve compliance to control COVID-19.
Future studies should target actors in community engagement strategy for mobilizing communities for health promotions in Uganda, including the village health teams (VHTs).
Supplemental Material
Supplemental material, sj-docx-1-inq-10.1177_00469580231201258 for Prevalence and Factors Associated With Compliance With COVID-19 Presidential Lockdown Measures: A Cross-Sectional Study by Emmanuel Olal, David Mukunya, Johnson Nyeko Oloya, Steven Baguma, Christopher Okot, Nelson Onira Alema, Denis Acullu, Denish Omoya Ochula, Pamela Okot Atim, Patrick Olwedo Odong, Godfrey Smart Okot, Francis Pebalo Pebolo, Freddy Wathum Drinkwater Oyat, Eric Nzirakaindi Ikoona, Judith Aloyo and David Lagoro Kitara in INQUIRY: The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
We’d like to thank the administration of health facilities in the region for the information obtained. We recognize Dr. Mukunya David and Dr. Emmanuel Olal for conducting a comprehensive data analysis. Financial support from UMA Acholi branch members, which enabled the team to conduct this study successfully, is most appreciated.
Footnotes
Authors’ Contributions: DLK, JNO, JA, SB, and FWDO designed the study—JA, JNO, POA, FWDO, and DLK supervised data collection. EO, DM, and DLK conducted data analysis and interpretation. SB, CO, POA, NOA, DA, JNO, DOO, POO, GSO, FPP, ENI, FWDO, JA, EO, DM, and DLK wrote and revised the manuscript. All Authors approved the manuscript.
Availability of Data and Materials: All datasets supporting this article’s conclusion are within this article and are accessible by a reasonable request to the corresponding author.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Most funding for this study was contributions from individual research members of the Uganda Medical Association (UMA) Acholi branch.
Ethics Approval and Consent to Participate: St. Mary’s Lacor Hospital Institutional and Ethics Committee approved this study (LHIREC No.0192/10/2021). In addition, the study was conducted following relevant institutional guidelines and regulations. We obtained written informed consent from each participant of this study.
ORCID iD: David Lagoro Kitara  https://orcid.org/0000-0001-7282-5026
https://orcid.org/0000-0001-7282-5026
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Finney Rutten LJ, Zhu X, Leppin AL, et al. Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. Mayo Clin Proc. 2021;96(3):699-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ba MF, Faye A, Kane B, et al. Factors associated with COVID-19 vaccine hesitancy in Senegal: a mixed study. Hum Vaccin Immunother. 2022;18(5):2060020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hao R, Zhang Y, Cao Z, et al. Control strategies and their effects on the COVID-19 pandemic in 2020 in representative countries. J Biosaf Biosecur. 2021;3(2):76-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. The Global Fund. The Global Fund to Fight AIDS, Tuberculosis and Malaria. GLOBAL HEALTH CAMPUS Chemin du Pommier 40 1218 Grand-Saconnex Geneva, Switzerland. 2021. https://theglobalfund.org. [Google Scholar]
- 5. Xinhua. Uganda enforces mandatory wearing of face masks. XINHUANET. 2021. Error! Hyperlink reference not valid. Accessed November 4, 2021. http://www.xinhuanet.com/english/2020-05/07/c_139035998.htm.
- 6. Nwagbara UI, Osual EC, Chireshe R, et al. Knowledge, attitude, perception, and preventative practices towards COVID-19 in sub-Saharan Africa: A scoping review. PLoS One. 2021;16(4):e0249853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Haider N, Osman AY, Gadzekpo A, et al. Lockdown measures in response to COVID-19 in nine sub-Saharan African countries. BMJ Glob Health. 2020;5:e003319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Nwaeze O, Langsi R, Osuagwu UL, et al. Factors affecting willingness to comply with public health measures during the pandemic among sub-Sahara Africans. Afr Health Sci. 2021;21(4):1629-1639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. ECA. COVID-19 for Africa: Lockdown exit strategies. 2020. Accessed August 23, 2022. https://www.uneca.org/covid-19-africa-lockdown-exit-strategies.
- 10. Alaran AJ, Badmos AO, Bouaddi O, et al. Decisive or impulsive? Re-examining Africa’s lockdown response to COVID-19. Trop Med Health. 2022;50:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Altare C, Kostandova N, OKeeffe J, et al. COVID-19 epidemiology and changes in health service utilization in Uganda’s refugee settlements during the first year of the pandemic. BMC Public Health. 2022;22:1927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Qian M, Jiang J. COVID-19 and social distancing. J Public Health. 2022;30(1):259-261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chiu NC, Chi H, Tai YL, et al. Impact of wearing masks, hand hygiene, and social distancing on influenza, enterovirus, and all-cause pneumonia during the Coronavirus pandemic: retrospective national epidemiological surveillance study. J Med Internet Res. 2020;22(8):e21257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Uganda Bureau of Statistics (UBOS). Uganda Bureau of Statistics. Ubos.org. 2021. Accessed July 24, 2022. https://www.ubos.org.
- 15. Denis AA, Collines A, Frederick ME, Gazda S, Kitara DL. Is there a line between internal displacement and environmental and Dietary factors in the onset of nodding syndrome in northern Uganda? A clinical observational study design. J Pharma Med Res. 2017;3(9):34-48. [Google Scholar]
- 16. Uganda Bureau of Statistics (UBOS). Uganda Bureau of Statistics. Ubos.org. 2019. Accessed August 25, 2022. https://www.ubos.org.
- 17. Oloya JN, Baguma S, Oyat FWD, Ikoona EN, Aloyo J, Kitara DL, et al. Is it COVID-19 vaccine hesitancy or inquisitiveness? Factors associated with COVID-19 vaccine acceptance among the adult population in Northern Uganda. A cross-sectional study. Research Square. 2022. doi: 10.21203/rs.3.rs-1824057/v1. [DOI] [Google Scholar]
- 18. Ikoona EN, Acullu D, Nyeko JO, Aloyo J, Oyat FWD, Kitara DL, et al. COVID-19 pandemic, challenges, and opportunities in northern Uganda; Community overview and perspectives: a qualitative study using informant interviews. Adv J Virol Epidem Pand Dis. 2022;7(1):63-71. [Google Scholar]
- 19. Scott A, Smith TMF. Estimation in multi-stage surveys. J Am Stat Assoc. 1969;64:830-840. [Google Scholar]
- 20. Sathian B, Sreedharan J, Baboo SN, Sharan K, Abhilash ES, Rajesh E. Relevance of sample size determination in medical research. Nepal J Epidemiol. 2010;1(1):4-10. [Google Scholar]
- 21. Thomas L. Systematic Sampling | A Step-by-Step Guide with Examples. Scribbr. 2022. Accessed May 15, 2022. https://www.scribbr.com/methodology/systematic-sampling/.
- 22. Mahmutovic J. What is Systematic Sampling? Pros, Cons, and Examples. SurveyLegend. 2023. Accessed June17, 2022. https://www.surveylegend.com/sampling/systematic-sampling/.
- 23. Gillwald A, Mothobi O, Ndiwalana A, Tusubira T. The State of ICT in Uganda. Research ICT Africa. 2019. Accessed July 17, 2022. https://researchictafrica.net/2019_after-access-the-state-of-ict-in-uganda/.
- 24. Kitara DL, Ikoona EN. COVID-19 pandemic, Uganda’s Story. Pan Afr Med J. 2020;35:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kitara DL, Ikoona EN. Proposed strategies for easing COVID-19 lockdown measures in Africa. Pan Afr Med J. 2020;36(179):179. doi: 10.11604/pamj.2020.36.179.24194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ikoona EN, Kitara DL. A proposed framework to limit post-lockdown community transmission of COVID-19 in Africa. Pan Afr Med J. 2021;38:303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mugambe RK, Ssekamatte T, Kisaka S, et al. Extent of compliance with COVID-19 prevention and control guidelines among supermarkets in Kampala capital city and Mukono Municipality, Uganda. PLoS One. 2021;16(10):e0258840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kasozi KI, MacLeod E, Ssempijja F, et al. Misconceptions on COVID-19 risk among Ugandan men: results from a rapid exploratory survey, April 2020. Front Public Health. 2020;8:416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Elayeete S, Nampeera R, Nsubuga EJ, et al. Comparative epidemiologic analysis of COVID-19 patients during the first and second waves of COVID-19 in Uganda. IJID regions. 2022;3:160-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bongomin F, Fleischer B, Olum R, et al. High mortality during the second wave of the coronavirus disease 2019 (COVID-19) pandemic in Uganda: experience from a national referral COVID-19 treatment unit. Open Forum Infect Dis. 2021;8(11):ofab530. doi: 10.1093/ofid/ofab530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Okot C, Baguma S, Onira NA, Aloyo J, Ikoona EN, Kitara DL, et al. Characteristics of the COVID-19 patients treated at Gulu Regional Referral Hospital, Northern Uganda: a cross-sectional study. J Infect Dis Ther. 2022;S1:004. [Google Scholar]
- 32. Baguma S, Okot C, Alema NO, et al. Factors associated with mortality among the COVID-19 patients treated at Gulu Regional Referral Hospital: A retrospective study. Front Public Health. 2022;10:841906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Human Rights Watch (HRW). Uganda: Authorities weaponize COVID-19 for repression. Investigate killings, end arbitrary detention, allow peaceful gatherings. 2021. https://www.hrw.org/news/2020/11/20/uganda-authorities-weaponize-covid-19-repression.
- 34. Kamusiime W. Continuous stricter enforcement of the anti-COVID 19 measures. 2021. Accessed May 16, 2022. https://www.upf.go.ug.
- 35. van Loenhout JAF, Vanderplanken K, Scheen B, Van den Broucke S, Aujoulat I. Determinants of adherence to COVID-19 measures among the Belgian population: an application of the protection motivation theory. Arch Public Health. 2021;79:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ayouni I, Maatoug J, Dhouib W, et al. Effective public health measures to mitigate the spread of COVID-19: a systematic review. BMC Public Health. 2021;21(1):1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Carmen N. Do women and men have a coronavirus risk gap? Forbes. 2020. Accessed April 17, 2020. https://www.forbes.com/sites/carmenniethammer/2020/03/06/do-women-and-men-have-a-coronavirus-risk-gap/#21013e7f6826.
- 38. Nshakira-Rukundo E, Whitehead A. Changing perceptions about COVID-19 risk and adherence to preventive strategies in Uganda: Evidence from an online mixed-methods survey. Sci Afr. 2021;14:e01049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Elrha. Compliance to the COVID-19 guidelines in Uganda: Insights from a multisite study in 13 refugee settlements. 2021. [Google Scholar]
- 40. Aloyo J, Acullu D, Oyat FWD, Obalim L, Ikoona EN, Kitara DL, et al. Distinct characteristics of the COVID-19 among children and young adolescents treated at Gulu Regional Referral Hospital; Northern Uganda: A cross-sectional study. J Infect Dis Ther. 2022;10(S1):1000004. [Google Scholar]
- 41. Wright L, Steptoe A, Fancourt D. Patterns of compliance with COVID-19 preventive behaviours: a latent class analysis of 20 000 UK adults. J Epidemiol Community Health. 2022;76:247-253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Migisha R, Kwesiga B, Mirembe BB, et al. Early cases of SARS-CoV-2 infection in Uganda: epidemiology and lessons learned from risk-based testing approaches - March-April 2020. Global Health. 2020;16(1):114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. James E, Wanume B, Musaba MW, et al. Characteristics, treatment outcomes and experiences of COVID-19 patients under home-based care in Kapelebyong district in Uganda: a mixed-methods study. Trop Med Health. 2022;50:93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. The Independent. Uganda’s emergency response to the COVID-19 pandemic. H.E.-SPEECH-ON-COVID-19-RESPONSE-AS-30-JULY. 2021. https://www.independent.co.ug.
- 45. SoleimanvandiAzar N, Irandoost SF, Ahmadi S, et al. Explaining the reasons for not maintaining the health guidelines to prevent COVID-19 in high-risk jobs: a qualitative study in Iran. BMC Public Health. 2021;21:848. doi: 10.1186/s12889-021-10889-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yoosefi Lebni J, Irandoost SF, Xosravi T, et al. Explaining the problems faced by Iranian housewives during the COVID-19 quarantine period, and their adaption strategies: a qualitative study. Womens Health. 2021;17:17455065211063291. doi: 10.1177/17455065211063291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Blendon RJ, Benson JM, DesRoches CM, Raleigh E, Taylor-Clark K. The public’s response to severe acute respiratory syndrome in Toronto and the United States. Clin Infect Dis. 2004;38(7):925-931. [DOI] [PubMed] [Google Scholar]
- 48. Maunder R, Hunter J, Vincent L. The immediate psychological and occupational impact of the 2003 SARS outbreak in a teaching hospital. CMAJ. 2003;168(10):1245-1251. [PMC free article] [PubMed] [Google Scholar]
- 49. Bai Y, Lin C-C, Lin C-Y, Chen JY, Chue CM, Chou P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr Serv. 2004;55(9):1055-1057. [DOI] [PubMed] [Google Scholar]
- 50. Cava MA, Fay KE, Beanlands HJ, McCay EA, Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005;22(5):398-406. [DOI] [PubMed] [Google Scholar]
- 51. Jeong H, Yim HW, Song Y-J, et al. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health. 2016;38:e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10(7):1206-1212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Y-t WU, Zhang C, Liu H. Perinatal Depression of Women Along With 2019 Novel Coronavirus Breakout in China. World Health Organization; 2020. [Google Scholar]
- 54. Zheng X, Tao G, Huang P. Self-reported depression of cancer patients under 2019 novel coronavirus pandemic. https://ssrn.com/abstract=3555252
- 55. Yoosefi Lebni J, Irandoost SF, Safari H, et al. Lived experiences and challenges of the families of COVID-19 victims: A qualitative phenomenological study in Tehran, Iran. Inquiry. 2022;59:469580221081405. doi: 10.1177/00469580221081405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Abdelhafiz AS, Alorabi M. Social stigma: the hidden threat of COVID-19. Front Public Health. 2020;8:429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Kahambing JGS, Edilo SR. Stigma, exclusion, and mental health during COVID19: 2 cases from the Philippines. Asian J Psychiatr. 2020;54:102292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Sotgiu G, Dobler CC. Social stigma in the time of coronavirus disease 2019. Eur Respir J. 2020;56(2):2002461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Grover S, Singh P, Sahoo S, Mehra A. Stigma related to COVID-19 infection: are the health care workers stigmatizing their own colleagues? Asian J Psychiatr. 2020;53:102381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kim Y. Nurses’ experiences of care for patients with Middle East respiratory syndrome-coronavirus in South Korea. Am J Infect Control. 2018;46(7):781-787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Bhattacharya P, Banerjee D, Rao TS. The “untold” side of COVID-19: social stigma and its consequences in India. Indian J Psychol Med. 2020;42(4):382-386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ahmadi S, Irandoost SF, Ahmadi A, Yoosefi Lebni J, Mohammadi Gharehghani MA, Baba Safari N. Explaining experiences, challenges and adaptation strategies in COVID-19 patients: a qualitative study in Iran. Front Public Health. 2022;9:778026. doi: 10.3389/fpubh.2021.778026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Rahmatinejad P, Yazdi M, Khosravi Z, Shahisadrabadi F. Lived experience of patients with coronavirus (COVID-19): a phenomenological study. J Res Psychol Health. 2020;14:7-86. doi: 10.52547/rph.14.1.71 [DOI] [Google Scholar]
- 64. Iheduru-Anderson K. Reflections on the lived experience of working with limited personal protective equipment during the covid-19 crisis. Nurs Inq. 2021;28:e12382. doi: 10.1111/nin.12382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Yoosefi Lebni J, Enayat H, Irandoost SF, Dehghan AA. Exploring the challenges of Afghan refugee women facing COVID-19: a qualitative study in Iran. Front Public Health. 2022;10:838965. doi: 10.3389/fpubh.2022.838965. 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Fouad FM, McCall SJ, Ayoub H, Abu-Raddad LJ, Mumtaz GR. Vulnerability of Syrian refugees in Lebanon to COVID-19: quantitative insights. Confl Health. 2021;15(1):6. doi: 10.1186/s13031-021-00349-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Yücel A. Symbolic annihilation of Syrian refugees by Turkish news media during the COVID-19 pandemic. Int J Equity Health. 2021;20:137-211. doi: 10.1186/s12939-021-01472-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-inq-10.1177_00469580231201258 for Prevalence and Factors Associated With Compliance With COVID-19 Presidential Lockdown Measures: A Cross-Sectional Study by Emmanuel Olal, David Mukunya, Johnson Nyeko Oloya, Steven Baguma, Christopher Okot, Nelson Onira Alema, Denis Acullu, Denish Omoya Ochula, Pamela Okot Atim, Patrick Olwedo Odong, Godfrey Smart Okot, Francis Pebalo Pebolo, Freddy Wathum Drinkwater Oyat, Eric Nzirakaindi Ikoona, Judith Aloyo and David Lagoro Kitara in INQUIRY: The Journal of Health Care Organization, Provision, and Financing