Abstract
Music therapy (MT) is a common modality that performs a complementary and integrative role along with standard treatments for many pediatric diseases. This article briefly reviewed the effects of MT on children aged 5–11 years old and adolescents with asthma from previous studies, specified its functional target towards asthma symptoms, and sorted out the design and investigation of selected research. Medline/PubMed, Embase, SportDis-cus, Cochrane Library, Teacher Reference Centre, Web of Science, Academic Search Complete, PsycARTICLES, and Scopus were queried for experimental and observational studies published between 1990 and 2021. Then, researchers showed that MT lessened patients’ asthma symptoms, improved medication compliance, pulmonary function, and quality of life, and helped children and their parents manage anxiety and depression. This article may serve as a reference for clinical research for pediatric asthma therapies and lay the foundation for future research on MT and its clinical practice.
Keywords: pediatric asthma, music therapy, breath exercise, sing and play the wind instruments
Introduction
Asthma is the most prevalent chronic respiratory disease; it affects 14% of children worldwide. The management approach for asthma includes pharmacological and non-pharmacological strategies.1,2 According to the latest report on asthma by the Global Initiative for Asthma (GINA),3 asthma can be classified into mild, moderate, and severe (Table 1). The asthma classification should be determined before initiation of pharmacological intervention.2 Airway obstruction, which is a main feature of asthma, may result in functional impairment and lung damage and includes 1) spasm of bronchial smooth muscles, which indicates an abnormal muscle function; 2) mucus secretion, which may plug small airways; and 3) inflammation, which constricts the airways.2 Pharmacological therapy aims to relax the smooth muscles, recover pulmonary function, and decrease inflammation. Guidelines3 show that children diagnosed with asthma may receive regular or long-term medications and that asthma symptoms were controlled in at least 80% of children who received inhaled corticosteroids.4 However, poor adherence may directly affect the therapeutic effect of medication, which should not be ignored. The bitter taste of medications, the inconvenience of using asthma devices, and adverse reactions may be the potential factors that lead to poor medication compliance.5 Therefore, in addition to medication, therapists gradually shift their focus on providing non-pharmacological strategies to improve medication compliance and better control asthma control, such as suitable physical activity. This includes swimming for young people with asthma, which could improve cardiopulmonary fitness and can have a small benefit for asthma control and lung function. Importantly, the breathing exercises recommended in the GINA, including the Buteyko and the Papworth methods, reported improvements in symptoms, quality of life, and psychological measures, voluntary reduction in the use of rescue medication, or engagement of the patient in their health care.
Table 1.
Classification of Asthma by Severity
| Types | |||
|---|---|---|---|
| Mild | Moderate | Severe | |
| Clinical manifestation | Infrequent exacerbations | Exacerbations more than twice a week | Daily wheezing |
| Asymptomatic between exacerbations | Intermittent symptoms between exacerbations; Good exercise tolerance. | Symptoms between exacerbations | |
| Good exercise tolerance | Diminished exercise tolerance | Poor exercise tolerance | |
| Urgent or emergent care not necessary | Urgent or emergent care less than three times a year; decreased mid flows three times a year | Urgent or emergent care more than three times a year | |
| Generally normal peak flows, may have decreased mid flows | Peak flow and FEV1 60%–80%; Generally reversible with bronchodilators | Peak flow and FEV1 less than 60%; May not reverse with bronchodilator; may need steroids to demonstrate reversibility. | |
| Mild asthma is well controlled with low-intensity treatment, ie, as-needed low-dose ICS-formoterol, or low-dose ICS plus as-needed SABA. | Moderate asthma is currently defined as asthma that is well controlled with low- or medium-dose ICS-LABA in either treatment track. | Severe asthma is defined as asthma that remains uncontrolled despite optimized treatment with high-dose ICS-LABA, or that requires high-dose ICS-LABA to prevent it from becoming uncontrolled. Persistent problems with adherence or comorbidities such as chronic rhinosinusitis or obesity, as they need very different treatment compared with if asthma is relatively refractory to high-dose ICS-LABA or even OCS. | |
Abbreviations: FEV1, forced expiratory volume in 1s; SABA, short-acting beta 2 agonist; ICS-LABA, inhaled corticosteroid-long-acting beta2-agonist; OCS, oral corticosteroids.
Coincidentally, music therapy (MT), as a new non-pharmacological strategy, could combine breathing exercises or simple physical activities with music and improve medication adherence as well as symptoms, lung function, and regulate mood.2,6–8 This may offer a new approach to asthma treatment in asthma clinical practice.
Indeed, MT is increasingly applied to improve patient health, reduce stress, and distract patients from unpleasant symptoms because it is cheaper than traditional therapies.9,10 It was reported2 that in the comparison of pulmonary function between musicians that played wind instruments and non-musicians, implying that the increased lung capacity is attributed to breathing exercises as well as regular singing training and wind instrument playing. We believe that MT would be effective for patients to manage their asthma, including mood regulation, medication compliance, symptom frequency, and even lung function recovery. Meanwhile, GINA showed that proper breathing exercises and simple physical activities should be encouraged to improve medication adherence as well as symptoms and lung function and regulate mood for pediatric asthma patients. We believe that MT should gradually be getting more attention and application in pediatric asthma therapy due to its safety, convenience, mood effects, low expense, and effective function in physiology and psychology. This is especially true during difficult periods such as COVID-19, when pediatric asthma patients might suffer from more severe symptoms or injury to their lung function due to the limitations of going to the hospital, taking normal therapy, or availability of rehabilitation off-online, with daily nervousness or depression. An acceptable and pleasing therapy method is necessary and important for patients’ recovery.
Although an increasing number of pediatric scientists, researchers, and psychologists focus on MT, most of them are strangers to this field, and there are still few reports regarding the application of MT to pediatric asthma patients and their long-term therapy. Therefore, many researchers interested in MT are confused about its process and mechanism, let alone desire to research MT or apply it to clinics. They may ask questions such as, “What is MT?”, “What kind of music or music activities should be carried on?”, “What would the treatment cycle be?” and “How to assess the effect with valid biotic factors?” Thus, a systematic, concise, and basic review is necessary for readers and researchers from different backgrounds to understand MT.
According to previous research, MT could be successfully used in children aged 5–11 years old and adolescents with mature cognitive and executive abilities to complete the necessary music activity. We briefly summarized the advances and latest developments in MT applied to pediatric asthma patients (children aged 5–11 years old and adolescents) from reviews and research. We determined that MT could regulate mood, alleviate anxiety, ease symptoms, improve medication compliance, and help reduce the dosage of drugs in pediatric asthma patients. We believe this short review will be a significant reference for future research to design and renew MT methods and clinical practice that could be successfully used for pediatric asthma patients, even patients diagnosed with respiratory diseases.
Methods
Search Strategy
We searched for studies published between 1990 and 2021 through Medline/PubMed, Embase, SportDis-cus, Cochrane Library, Teacher Reference Centre, Web of Science, Academic Search Complete, PsycARTICLES, and Scopus. Databases were searched for Randomized Controlled Trials, clinical trials, and observational studies using the following keywords: asthma in pediatrics, MT, complementary therapies, and MT in pediatric asthma.
Subjects
Pediatric asthma patients (children aged 5–11 years old and adolescents).
Content
The diverse applications of MT to pediatric asthma patients and the therapeutic of MT on asthma symptoms, lung function, medication, and emotion adjustment.
Intervention
The musical intervention for patients discussed in this paper is divided into two types. The first is active MT through creating music by singing or playing instruments. There was no difference or preference between different age, gender, or background when choosing an instrument, it was dependent on choice and the arrangement of the music therapist. The second is passive MT, through listening to music. The intensity of MT can vary with the functional role it plays in the whole therapeutic process, with no restrictions on the length, frequency, or duration of the music.
Outcome Measurements
At least one positive effect must be evaluated in each experimental research in this paper.
Result
The primary literature search identified 458 citations. After removing duplicate citations and scattered contents, 125 unique citations were selected to further screening. Seven studies that focused on pediatric asthma and MT were ultimately chosen for our review for further analysis and summary. Exclusions occurred because of small sample sizes, trials without randomization, or unconvincing results. The included studies were heterogeneous in terms of MT methodology but covered the latest research results in MT applied to pediatric asthma patients. The interventions varied from passive MT (listening to relaxation music, progressive muscle relaxation with background music) to active MT (breathing exercises, singing, and/or playing wind instruments). MT was applied to children in both in and outpatient settings. Patients from experimental and control groups may receive different feedback from different music methods, periods, and environments. The basic and effective information from the results of each reference is shown in Table 2.
Table 2.
The Main Information of Appraised Studies
| References | Number and Age of Subjects | Music Therapy Method | Detail Information in Therapy Method | Times | Effect Targets | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Relieves Symptom | Improves Medication Compliance | Improves Medication Use | Improves Lung Function | Improves Quality of Life | Regulates Mood | |||||
| Wade2 | 9 (7–14 years old) | Listening to music Singing | Music assisted relaxation/15 min Vocal exercises and singing/15 min | 4 weeks (twice a week) | × | × | × | √ | √ | √ |
| Loewy6 | 173 (9–11 years old) | Listening to music Playing instruments Improvisation | Music-assisted relaxation Breathing exercises total: 30 min |
6 months (once a week) | √ | √ | √ | √ | √ | √ |
| Eley11 | 27 (5–18 years old) | Listening to music Playing instruments Singing | Music-assisted relaxation Breathing exercises 1st: 60 min; 2nd: 90 min |
6 months (once a week) | √ | × | × | √ | √ | √ |
| Andrew7 | 30 (5–16 years old) | Playing wind instruments | Playing the flute, clarinet, or cornet Breathing exercises and games total: 30 min |
1 months (once a week) | √ | × | √ | √ | × | × |
| Lucia12 | 18 (7–14 years old) | Playing wind instruments | Practice wind instruments/1 h | 1 months (twice a week) | √ | × | × | × | √ | √ |
| Lehrer8 | 10 (18 years old) | Listening to music | Music-assisted relaxation/1 h | 4 months (every day) | √ | × | × | √ | × | × |
| Janiszewski13 | 96 (18–23 years old) | Music-assisted breathing exercises | Breathing exercises/1 h | 1 years (every day) | × | × | × | √ | × | √ |
Notes: √, MT has a positive effect on this aspect; ×, Research did not discussed or mentioned.
Relieves Symptoms
Asthma exacerbation is accompanied by chest tightness, dyspnea, cough, and other symptoms. Prior to this, patients often experience symptoms such as nasal obstruction, sneezing, eye itchiness, and even dyspnea and hypoxemia. Loewy6 recruited 173 children and divided them into three groups based on therapeutic modalities applied to them, such as listening to music, playing instruments, and breathing exercises. The results showed that MT could relieve symptoms, such as cough and chest tightness, and reduce the number of hospitalizations, absences from classes, and ER visits. Eley11 also reported that the severity of symptoms in 27 children decreased after MT. In their research, MT consisted of playing wind instruments and singing. Andrew,7 who used the same musical measure for his patients, also found that playing wind instruments could significantly relieve symptoms and improve patients’ sleep. Researchers8,12 have reported that MT could decrease the frequency of pediatric asthma exacerbation and improve sleep quality in pediatric asthma patients 7–18 years old.
Ameliorates Medication Compliance
Children diagnosed with asthma may require medication (Table 3), such as pills and aerosols, to prevent disease progression. Pills with bitter or acidic taste may result in rejection or reluctance to take medications. Meanwhile, parents and children may not properly use aerosol medications, which would affect both compliance and function. Andrew’s research7 found that after playing wind instruments, the inhalation technique improved, and there was less dependence on reliever medications. Loewy6 also reported that after MT, parents were less anxious about their children’s medication compliance. Although the mechanism is unclear, it might be related to the patient’s positive emotions or the recovery of lung function following MT.
Table 3.
Initial Asthma Medication Treatment
| Object | Presenting Symptoms | Pharmacotherapy |
|---|---|---|
| Children aged 6–11 years | Infrequent asthma symptoms, eg, less than twice a month and no risk factors for exacerbations | Low-dose ICS taken whenever SABA is taken in combination or separate inhalers An alternative option is daily maintenance low-dose ICS with as-needed SABA |
| Asthma symptoms or need for reliever twice a month or more, but less than daily | Low-dose ICS plus as-needed SABA. Other options include daily LTRA (less effective than ICS), or taking ICS whenever SABA is taken in combination or separate inhalers. Consider likely adherence with maintenance treatment if reliever is SABA. | |
| Troublesome asthma symptoms most days (eg, 4–5 days/week); or waking due to asthma once a week or more, especially if any risk factors exist | Low-dose ICS-LABA plus as needed SABA, OR Medium-dose ICS plus as-needed SABA, OR Very-low-dose ICS-formoterol maintenance and reliever. Other options include daily low-dose ICS and LTRA, plus as-needed SABA. | |
| Initial asthma presentation is with severely uncontrolled asthma, or with an acute exacerbation | Start regular maintenance treatment with medium-dose ICS-LABA plus as-needed SABA or low-dose ICS-formoterol maintenance and reliever (MART). A short course of OCS may also be needed. | |
| Adolescents | Infrequent asthma symptoms, eg, less than twice a month and no risk factors for exacerbations, including no exacerbations in the last 12 months | As-needed low-dose ICS formoterol |
| Asthma symptoms or need for reliever twice a month or more | As-needed low-dose ICS formoterol | |
| Troublesome asthma symptoms most days (eg, 4–5 days/week); or waking due to asthma once a week or more, especially if any risk factors exist | Low-dose ICS formoterol maintenance and reliever therapy | |
| Severely uncontrolled asthma, or with an acute exacerbation | Medium-dose ICS formoterol maintenance and reliever therapy (MART). A short course of oral corticosteroids may also be needed. |
Abbreviations: ICS, inhaled corticosteroid; SABA, short-acting beta 2 agonist; LTRA, leuko triene receptor antagonist; ICS-LABA, inhaled corticosteroid-long-acting beta 2-agonist; OCS, oral corticosteroids.
Improves Pulmonary Function
Pulmonary function, defined as the lung’s respiratory function, should be clinically tested in patients who have pulmonary disease and in patients with dyspnea or those who require surgery.14 It was reported that subjects’ lung function was either maintained or improved after singing. When the lung function of musicians and non-musicians were compared, musicians had better lung function due to playing wind instruments and practicing singing for several years. It is implied that the increased lung capacity could be attributed to breathing and regular exercises.2 Loewy6 proved that MT could positively affect pulmonary function, while pediatric asthma management significantly improved in the MT group compared with the control group. Moreover, Eley11 and Wade2 also demonstrated that singing could maintain or increase peak expiratory flow (PEF) in pediatric asthma patients. Janiszewski13 reported that the forced expiratory volume in 1s (FEV1 and forced vital capacity (FVC) of 18 years old pediatric asthma patients improved after performing music-assisted breathing exercises. To observe the effects of medication and whether patients’ symptoms could be relieved, doctors recommend testing for PEF, which patients and parents can perform at home. Research2,6–8 has reported improved PEF after MT. It may be further proven that MT might exert a significant impact on asthma therapy and will be a potential mechanism related to the satisfactory consequences of MT. The pulmonary function test and the effect of MT on the Pulmonary function index are showed in Table 4.
Table 4.
Pulmonary Function Index and the Effects of MT
| Index | Definition | Abnormal Level | References/Effect of MT | |||||
|---|---|---|---|---|---|---|---|---|
| Wade2 | Loewy6 | Andrew7 | Lehrer8 | Eley11 | Janiszewski13 | |||
| FVC | Forced vital capacity | >normal value * 80% | × | FVC scores has no changed | × | FVC scores increase (from 88.6% to 93.7%) | FVC scores increase, but changes in detail was not discussed. | FVC scores increase, but changes in detail was not discussed. |
| FEV1 | Forced expiratory volume in 1s | × | FEV1 scores increase (from 81% to 85%) | × | FEV1 scores increase (from 73.5% to 79.1%) | FEV1 scores increase but changes in detail was not discussed | FEV1 scores increase, but changes in detail was not discussed | |
| FEV1% (FEV1/FVC) | Forced expiratory ratio in 1s | × | FEV1% scores increase (from 89% to 97%) | × | FEV1% scores increase (from 66.7% to 68.5%) | × | × | |
| PEF | Peak expiratory flow | PEF scores increased after singing, but changes in detail was not discussed. | PEF scores increase (from 61% to 66%). | PEF scores increase (from 77% to 96%). | × | × | × | |
| MEF25 | Maximal expiratory flow with 25% expiration | × | × | × | × | × | × | |
| MEF50 | Maximal expiratory flow with 50% expiration | × | × | × | × | × | × | |
| MEF75 | Maximal expiratory flow with 75% expiration | × | × | × | × | × | × | |
Notes: *Normal values obtained from patient data, including height, weight, age, gender; ×, Research did not discussed or mentioned.
Improves Quality of Life
Pediatric asthma patients often require long-term medications and frequent hospitalizations. Hence, parents restrict their children from performing physical exercises such as running, swimming, and playing, which are common activities during childhood.15 Therefore, music may play a pivotal role in replacing physical activities while improving patients’ mood and pulmonary function.16,17
Studies have shown that students with asthma who played wind instruments and sang have a more favorable attitude towards their condition than those who do not participate in musical activities. Accordingly, these patients’ asthma exacerbations decreased.2,12 Loewy6 pointed out that children’s cognition and perception improved compared to the control group. Additionally, breathing and retraining programs have remarkably improved the quality of life in patients whose asthma is not adequately controlled by pharmacological methods. Furthermore, Eley11 reported that participants from their research expressed interest and enjoyment in activities that may help them comply with medication while being able to relax.
Psychological and Emotional Management
Research revealed that various MT for pediatric asthma patients might result in several benefits, including improvement in psychological well-being, emotional regulation,6 acquisition of knowledge regarding asthma,11 and management of panic and anxiety during asthma exacerbation,12,13 which is helpful for pediatric asthma patients and their parents.
Discussion and Future Directions
Pediatric asthma patients should attract more attention from the public. We found that a number of MT research focused on other diseases such as autism,18,19 neonatal treatment,20,21 emotional regulation,22,23 and mood disorders,24,25 suggesting MT can have a positive therapeutic impact. However, there has been little research on MT for pediatric asthma patients. We collected and arranged relevant information in this review regarding the application of MT to pediatric asthma patients to illustrate that MT has been proven to improve asthma symptoms, medication compliance, and pulmonary function and helps to manage anxiety and depression in pediatric asthma patients.
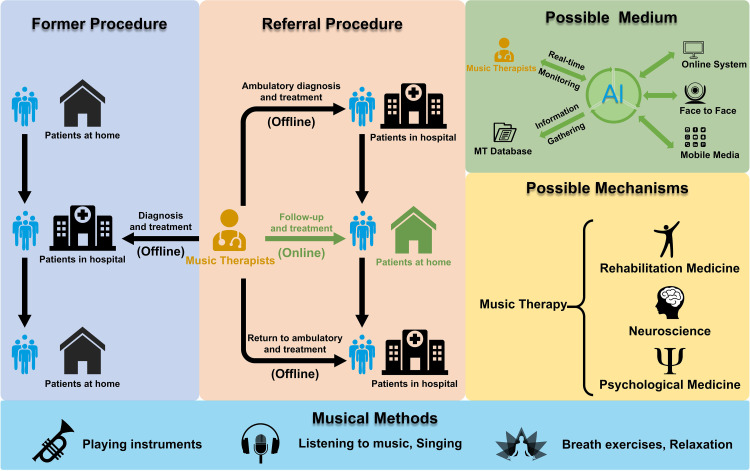
The world faced a tremendous challenge and is engulfed by one of the most widespread and severe public health crises in decades, as COVID-19 has become the leading cause of death internationally from 2019–2022.26 People are particularly vulnerable to feel negative emotions such as fear and anxiety. This is experienced by doctors and nurses working with patients27 and non-healthcare workers, who all experience different levels of psychological distress and depression.28 MT may be applied in these situations to improve mood and reduce stress, and it may also become an important auxiliary therapy following surgery or pharmacological therapy. Due to COVID-19, pediatric asthma patients in China have a decreased frequency of hospital visits. Thus, exploring how to apply MT online or combine the online and off-online models can be widely promoted (Figure 1). This can benefit pediatric asthma patients in remote areas and those with emotional problems and experiencing physical pain or discomfort. Meanwhile, artificial intelligence technology(AIT) is gaining popularity among the public. If we could develop related software to support MT in pediatric asthma control, patients may benefit from the technology with immediate feedback, biotic parameter estimation, and diverse music experience during the immersive therapeutic atmosphere. Future research should focus on the technological evolution of MT and its potential function mechanism—for example, the relationship between MT and brain science and MT and psychology.
Figure 1.
Clinical referral procedures and future research directions of MT.
We hope our manuscript will be a suitable reference for related researchers to understand the basic information for MT and future studies to explore the effective and innovative MT models and methods that could be applied to pediatric asthma control and even other pediatric diseases.
Conclusion
MT is effective for physiology and psychology and has been increasingly applied for pediatric asthma therapy. MT may improve a child’s asthma symptoms, medication compliance, and pulmonary function and help children and their parents manage their mental health. Future research should focus on the technological evolution of this method and model MT and its potential functional mechanism.
Acknowledgments
The authors thank the Daiji Jiang for his support to our study, especially in the analysis and interpretation of references to our manuscript.
Funding Statement
This research received no external funding.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare no conflict of interest.
References
- 1.Azmeh R, Greydanus DE, Agana MG, et al. Update in pediatric asthma: selected issues. Dis Mon. 2020;66:100886. [DOI] [PubMed] [Google Scholar]
- 2.Leanne MW. A comparison of the effects of vocal exercises/singing versus music-assisted relaxation on peak expiratory flow rates of children with asthma. Music Ther Perspect. 2002;20:31–37. doi: 10.1093/mtp/20.1.31 [DOI] [Google Scholar]
- 3.Global strategy for asthma management and prevention; 2023. Available from: www.ginasthma.org. Accessed September 25, 2023.
- 4.Lasmar L, Camargos P, Champs NS, et al. Adherence rate to inhaled corticosteroids and their impact on asthma control. Allergy. 2009;64:784–789. doi: 10.1111/j.1398-9995.2008.01877.x [DOI] [PubMed] [Google Scholar]
- 5.Haktanir AM, Phipatanakul W. Severe asthma in children: evaluation and management. Allergol Int. 2019;68:150–157. doi: 10.1016/j.alit.2018.11.007 [DOI] [PubMed] [Google Scholar]
- 6.Loewy J, Goldsmith C, Deshpande S, et al. Music therapy in pediatric asthma improves pulmonary function while reducing hospitalizations. J Asthma. 2021;58:674–682. doi: 10.1080/02770903.2020.1712725 [DOI] [PubMed] [Google Scholar]
- 7.Andrew W. Bronchial boogie. Community Pract. 2006;79:78–79. [PubMed] [Google Scholar]
- 8.Lehrer PM, Hochron SM, Mayne T, et al. Relaxation and music therapies for asthma among patients prestabilized on asthma medication. J Behav Med. 1994;17:1–24. doi: 10.1007/BF01856879 [DOI] [PubMed] [Google Scholar]
- 9.Antonakopoulou S. Music Therapy for Improving Premature Infants’ Well-Being and Communication Skills and Enhancing Mother-Infant Bonding: A Case Study. Finland: University of Jyväskylä; 2016. [Google Scholar]
- 10.Kehl SM, La Marca-Ghaemmaghami P, Haller M, et al. Creative music therapy with premature infants and their parents: a mixed-method pilot study on parents’ anxiety, stress and depressive symptoms and parent-infant attachment. Int J Environ Res Public Health. 2020;18(1):265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eley R, Gorman D. Didgeridoo playing and singing to support asthma management in Aboriginal Australians. J Rural Health. 2010;26:100–104. doi: 10.1111/j.1748-0361.2009.00256.x [DOI] [PubMed] [Google Scholar]
- 12.Lucia R. Effects of playing a musical wind instrument in asthmatic teenagers. J Asthma. 1994;31:375–385. doi: 10.3109/02770909409061317 [DOI] [PubMed] [Google Scholar]
- 13.Janiszewski M, Kronenberger M, Drózd B. Studies on the use of music therapy as a form of breathing exercise in bronchial asthma. Pol Merkur Lekarski. 1996;1:32–33. [PubMed] [Google Scholar]
- 14.Ruppel GL, Enright PL. Pulmonary function testing. Respir Care. 2012;57:165–175. doi: 10.4187/respcare.01640 [DOI] [PubMed] [Google Scholar]
- 15.Tandon PS, Sasser T, Gonzalez ES, et al. Physical activity, screen time, and sleep in children with ADHD. J Phys Act Health. 2019;16:416–422. doi: 10.1123/jpah.2018-0215 [DOI] [PubMed] [Google Scholar]
- 16.Hill WT, Palmer JA. Affective response to a set of new musical stimuli. Psychol Rep. 2010;106:581–588. doi: 10.2466/pr0.106.2.581-588 [DOI] [PubMed] [Google Scholar]
- 17.Vuilleumier P, Trost W. Music and emotions: from enchantment to entrainment. Ann N Y Acad Sci. 2015;1337:212–222. doi: 10.1111/nyas.12676 [DOI] [PubMed] [Google Scholar]
- 18.Sharda M, Silani G, Specht K, et al. Music therapy for children with autism: investigating social behaviour through music. Lancet Child Adolesc Health. 2019;3:759–761. doi: 10.1016/S2352-4642(19)30265-2 [DOI] [PubMed] [Google Scholar]
- 19.Sharda M, Tuerk C, Chowdhury R, et al. Music improves social communication and auditory-motor connectivity in children with autism. Transl Psychiatry. 2018;8:231. doi: 10.1038/s41398-018-0287-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yue W, Han X, Luo J, et al. Effect of music therapy on preterm infants in neonatal intensive care unit: systematic review and meta-analysis of randomized controlled trials. J Adv Nurs. 2021;77:635–652. doi: 10.1111/jan.14630 [DOI] [PubMed] [Google Scholar]
- 21.Liang S, Zhang J, Liu Y, et al. The effect of neonatal touch and music therapy on the recovery of neurological function in full-term children with moderate to severe asphyxia. Chin Med Pharm. 2019;2019:1. [Google Scholar]
- 22.Duffy B, Fuller R. Role of music therapy in social skills development in children with moderate intellectual disability. J Appl Res Intellectual Disabilities. 2010;13:77–89. doi: 10.1046/j.1468-3148.2000.00011.x [DOI] [Google Scholar]
- 23.Shi ZM, Lin GH, Xie Q. Effects of music therapy on mood, language, behavior, and social skills in children with autism: a meta-analysis - ScienceDirect. Chin Nurs Res. 2016;3:137–141. doi: 10.1016/j.cnre.2016.06.018 [DOI] [Google Scholar]
- 24.Rushing J, Capilouto G, Dressler EV, et al. Active music therapy following acute stroke: a single-arm repeated measures study. J Music Ther. 2022;59:36–61. doi: 10.1093/jmt/thab017 [DOI] [PubMed] [Google Scholar]
- 25.Arezina CH. Music therapy in pediatrics: clinical indications for the treatment of functional symptoms. Funct Sympt Pediat Dis. 2014;2014:417–424. [Google Scholar]
- 26.Izda V, Jeffries MA, Sawalha AH. COVID-19: a review of therapeutic strategies and vaccine candidates. Clin Immunol. 2021;222:108634. doi: 10.1016/j.clim.2020.108634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dincer B, Inangil D. The effect of Emotional Freedom Techniques on nurses’ stress, anxiety, and burnout levels during the COVID-19 pandemic: a randomized controlled trial. Explore. 2021;17:109–114. doi: 10.1016/j.explore.2020.11.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lebel C, MacKinnon A, Bagshawe M, et al. Elevated depression and anxiety symptoms among pregnant individuals during the COVID-19 pandemic. J Affect Disord. 2020;277:5–13. doi: 10.1016/j.jad.2020.07.126 [DOI] [PMC free article] [PubMed] [Google Scholar]