Abstract
Premature ovarian insufficiency is a multi-factor gynecological disease that has become a major global health problem. In recent years, several trials have explored the treatment of premature ovarian insufficiency using Chinese herbal medicine and acupuncture, but the efficacy and safety of this combination remains controversial. This systematic review and meta-analysis aimed to comprehensively evaluate the efficacy and safety of combining Chinese herbal medicine with acupuncture to treat premature ovarian insufficiency. From eight different databases, we retrieved randomized controlled trials wherein Chinese herbal medicine and acupuncture had been compared with western medicine in the treatment of premature ovarian insufficiency. The bias risk assessment stipulated by the Cochrane Collaboration's tool was utilized to evaluate the quality of the chosen randomized controlled trials. This meta-analysis was executed with the help of Review Manager 5.3 and Stata 10.0. The quality of evidence was assessed using the Grading of Recommendations, Assessment, Development, and Evaluation framework. A total of 10 randomized controlled trials involving 594 premature ovarian insufficiency patients were included in the analysis. Compared with western medicine, co-treatment with acupuncture and Chinese herbal medicine exhibited a significantly higher total effective rate (relative risk: 1.21; 95% confidence interval: 1.12–1.31; P < 0.01, I2 = 0%), but lower levels of luteinizing hormone (standardized mean difference: −0.57; 95% confidence interval: −1.06, −0.08; P < 0.05, I2 = 80%), follicle-stimulating hormone, and Kupperman index score. Moreover, the combined intervention increased estradiol level in the serum. Overall, the data demonstrate that acupuncture plus Chinese herbal medicine is an efficacious and safe treatment option for POI patients. These findings must be verified by conducting large-scale, multicenter, high-quality, and long-term randomized controlled trials.
Keywords: Chinese herbal medicine, Premature ovarian insufficiency, Meta-analysis, Acupuncture, Review
Highlights
-
•
Patients treated with acupuncture and CHM had a higher total effective rate.
-
•
Patients treated with acupuncture and CHM had lower levels of LH, FSH and KI score.
-
•
Patients treated with acupuncture and CHM had a higher level of E2.
-
•
The occurrence of complications was similar between two groups.
1. Introduction
Premature ovarian insufficiency (POI) is characterized by compromised hormonal and reproductive functions in females under the age of forty. It currently affects approximately 1% of women in the general population, and its incidence is persistently increasing [1]. POI is a gynecological endocrine illness caused by multiple factors, which may be related to socioeconomic status [2], autoimmune disorders [3], or prenatal ethanol exposure [4]. POI makes females more susceptible to multiple health risks, such as infertility [5], lipid disorders, early progression of cardiovascular illnesses [6], osteoporosis [7], psychiatric disorders, and other adverse events [8,9]. Besides, it increases the economical and psychological burden on their families and society [10].
Despite the huge global efforts to manage this disease, no established treatment exists. Hormone replacement therapy (HRT) is recommended for women with POI, especially to treat the symptoms of low estrogen. It alleviates vasomotor and genitourinary symptoms and prevents bone loss and cardiovascular disease. However, the medical history of patients must be strictly assessed before HRT is administered; for example, in breast cancer survivors, HRT is generally contraindicated by the international recommendations. The potential risks associated with HRT have been previously reviewed [1].
Several POI patients have opted for alternative medicine, particularly traditional Chinese medicine (TCM), which has an exceptional concept of the etiology of POI [11]. Chinese herbal medicine (CHM) in combination with acupuncture has been widely used to treatment multiple diseases, including POI [[12], [13], [14], [15]]. Previous systematic meta-analyses have shown that both CHM and acupuncture have positive therapeutic effects on POI [16,17]. A recent meta-analysis indicated that a combination of acupuncture and other treatment options (CHM/western drugs) produces a superior therapeutic effect against POI compared with that produced by CHM or western drugs alone [18]. However, this study had a relatively small sample size and did not distinguish between CHM and western medicine in the control group. Here, we have designed a more rigorous study that interrogates the therapeutic efficacy of combining acupuncture and CHM versus the use of Western drugs in patients with POI. This study identifies complementary therapeutic approaches for POI and can guide its clinical treatment.
2. Material and methods
This review has adopted the guidelines described in Preferred Reporting Items for Systematic Reviews and Meta-Analyses [19]. The PROSPERO registration number is CRD42020190573.
2.1. Data sources and searches
Systematic data searches, without language restrictions for randomized controlled trials (RCTs), were conducted across the Wanfang database, Chinese Scientific Journals Database, PubMed, Chinese BioMedical Database, Web of Science, Embase, China National Knowledge Infrastructure, and Cochrane Library. We examined the efficacy of acupuncture plus CHM versus western drugs for treating patients with POI from the time each database was established to 31 July 2022. We devised a formula for retrieval following the PICOS strategy. The specific retrieval formula for China National Knowledge Infrastructure was “subject = (acupuncture + body acupuncture + electroacupuncture + needling therapy + needle acupuncture) AND (premature ovarian failure + primary ovarian insufficiency + premature ovarian insufficiency + POI + POF) AND (randomization + randomized controlled + random grouping + RCT + clinical research)". The search strategies applied to PubMed have been reported in Supplement Digital. In addition, we manually searched the reference lists of all selected articles to find probably related research.
2.2. Inclusion criteria
We included RCTs that involved patients diagnosed with POI according to a clear diagnostic criterion, such as the guidelines of the European Society of Human Reproduction and Embryology, regardless of their ethnicity or nationality, and wherein they received acupuncture (including needle acupuncture and electroacupuncture) plus CHM, irrespective of the course of treatment, prescription name, dosage form, and dosage. Studies that compared acupuncture plus CHM with western drugs, and those with at least one clear outcome, such as the follicle-stimulating hormone (FSH) level, total effective rate, estradiol (E2) level, luteinizing hormone (LH) level, Kupperman index (KI) score, and the occurrence of complications, were also included.
2.3. Exclusion criteria
Studies involving animal experiments, commentaries, editorials, experience introduction, conference articles, reviews, graduation theses, and case reports were excluded from our analysis. We also excluded duplicate publications, studies whose original data were difficult to obtain, and those with intervention measures such as moxibustion, warm acupuncture, auriculotherapy, acupoint catgut embedding, or auricular acupoint pressing. Besides, articles without a clear outcome index were excluded.
2.4. Data extraction
Using a pre-designed, standardized data retrieval form, H. F. Li and W. J. Chen independently extracted data as follows: first author and year of publication, TCM syndrome differentiation, the number of persons, age, disease duration, interventions and comparisons, treatment duration, and outcomes. The third author (J. X. Zhang) resolved the disagreements between the two reviewers.
2.5. Outcome measures
The primary outcome was the total effective rate, which was assessed according to the Guidance Principle of Clinical Research on New Drug of Traditional Chinese Medicine [20]. For trials that assessed the treatment effect as different classification without total effective rate, we integrated the effective classification into “totally effective” for analysis. The secondary outcomes were serum E2, FSH, and LH levels, KI score, and the incidence of adverse events.
2.6. Quality assessment
Two authors (W. J. Chen and H. F. Li) independently evaluated the bias risk for the selected trials in accordance with the Cochrane Handbook. Briefly, the criteria included: selective reporting, blinding of participants and personnel, random sequence generation, incomplete outcome data, blinding of outcome assessments, and allocation concealment. Each RCT was categorized as high, low, or unclear. Any disagreement was resolved by a third researcher (J. X. Zhang).
2.7. Grading of Recommendations, assessment, development, and evaluation (GRADE)
The quality of evidence was assessed by GRADE, and categorized as very low, low, moderate, or high. The criteria consisted of study design, indirectness of the evidence, inconsistency in the outcomes, and risk of bias, among others.
2.8. Statistical analysis
We executed this meta-analysis with the help of Review Manager (RevMan) (Version 5.3, Copenhagen; The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) and Stata (Version 10.0; Stata Corporation, College Station, TX, USA). For the study results, relative risk (RR) with 95% confidence interval (CI) were utilized as binary variables. Mean differences (MDs) and 95% CIs for the continuous data were computed using some measure evaluation units and methods. Then, the standardized MD (SMD) was calculated. Cochrane's P values and I2 were used to assess heterogeneity among the RCTs. In cases where high heterogeneity existed due to methodological and clinical factors, the random effect model was employed even if I2 was small. Subgroup analysis was carried out, premised on different types of acupuncture. Egger regression tests and funnel plots were executed to assess possible publication bias. Additionally, sensitivity analysis was undertaken by chronologically removing RCTs to test the stability of the primary outcome.
2.9. Ethics and dissemination
No ethical approval was required because this systematic review is based on published studies.
3. Results
3.1. Study selection
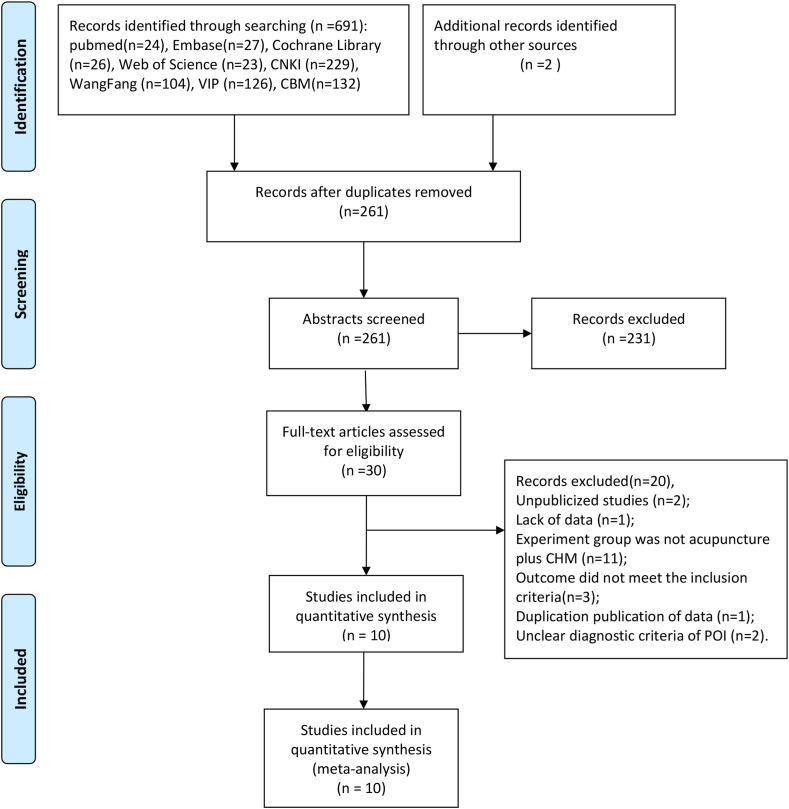
Of 693 relevant studies, only 10 were included in our systematic review [[21], [22], [23], [24], [25], [26], [27], [28], [29], [30]] (Table 1). The search and evaluation procedure is depicted in Fig. 1.
Table 1.
The basic characteristics of the included trials.
| Studies | TCM syndrome differentiation | Sample size (n) | Age (y) | Course of disease | Intervention measures | Duration treatment (mos) | Main outcomes |
|---|---|---|---|---|---|---|---|
| Fang (2016) | Kidney deficiency and liver depression | T: 32 C: 32 |
T: 34.6 ± 4.7 C: 33.8 ± 4.3 |
T: 12.2 ± 3.4 mos C: 13.3 ± 2.8 mos |
T: TCM Decoction + Electroacupuncture C: E + P |
3 | ①②③④⑤⑨ |
| Li (2017) | Kidney deficiency and liver depression | T: 16 C: 16 |
NR | NR | T: TCM Decoction+ Needle acupuncture C: E + P |
3 | ①②③④ |
| Liu (2017) | NR | T: 24 C: 24 |
33.4 ± 3.6 | 10.3 ± 5.9 mos | T: TCM Decoction+ Needle acupuncture C: E + P |
3 | ① |
| Luo (2015) | Kidney deficiency and blood stasis | T: 30 C: 30 |
T: 30.40 ± 9.0 C: 29.34 ± 8.74 |
T: 18.8 ± 6.8 mos C: 17.6 ± 5.9 mos |
T: TCM Decoction + Electroacupuncture C: E + P |
3 | ①②④⑤ |
| Wang (2011) | NR | T: 20 C: 20 |
T: 35.35 ± 9.62 C: 33.54 ± 9.85 |
T: 5.4 ± 3.8 yrs C: 5.0 ± 3.5 yrs |
T: TCM Decoction+ Needle acupuncture C: E + P |
3 | ①②③④ |
| Wu (2016) | Kidney deficiency and liver depression | T: 30 C: 30 |
T: 35.02 ± 4.91 C: 36.67 ± 3.45 |
NR | T: TCM Decoction + Electroacupuncture C: E + P |
3 | ①②③④⑤⑥ |
| Zhang (2014) | NR | T: 29 C: 29 |
NR | NR | T: TCM Decoction + Electroacupuncture C: E + P |
6 | ②④ |
| Zhang (2015) | Kidney deficiency and liver depression | T: 30 C: 30 |
NR | NR | T: TCM Decoction + Electroacupuncture C: E + P |
3 | ① |
| Zhang (2017) | NR | T: 60 C: 60 |
T: 34.5 C: 34.3 |
T: 2.4 yrs C: 2.3 yrs |
T: TCM Decoction+ Needle acupuncture C: E + P |
6 | ①②③④ |
| Wang (2021) | Kidney deficiency and blood stasis | T: 26 C: 26 |
T: 30.22 ± 4.31 C: 30.15 ± 4.23 |
T: 9.44 ± 2.07 mos C: 9.58 ± 2.14 mos |
T: TCM Decoction+ Needle acupuncture C: E + P |
3 | ①②③④⑦⑧ |
Abbreviations: T: trial group; C: control group; NR: not reported; mos: months; yrs: years; E: Estrogen; P: Progesterone; TCM: traditional Chinese medicine. ①: the total effective rate; ②: serum Estradiol (E2) levels; ③: serum luteinizing hormone (LH) levels; ④: serum follicle-stimulating hormone (FSH) levels; ⑤: Kupperman index (KI) score; ⑥: endometrial thickness (ET); ⑦: ovarian volume (OV); ⑧: antral follicle count (AFC); ⑨: adverse events.
Fig. 1.
The inclusion process for the literature.
3.2. Study characteristics
All the chosen RCTs were undertaken in China and published in Chinese. The studies included an aggregate of 594 POI patients, of which 297 received acupuncture in conjunction with CHM and 297 fell in the control cohort. Six studies had described the TCM syndrome differentiation [21,22,24,26,27,29], and the most frequent criterion was kidney deficiency and liver depression, which was used in four trials [21,22,27,29]. The baseline in all RCTs showed no significant difference. Eight RCTs utilized two-arm designs [[21], [22], [23],[25], [26], [27],29,30] while two had three-arm designs [24,28]. All the studies reported treatment duration, which was 3 months in eight studies [[21], [22], [23], [24], [25], [26], [27],29] and 6 months in two [28,30]. Nine trials presented the total effective rate [[21], [22], [23], [24], [25], [26], [27],29,30], eight reported FSH and E2 levels [21,22,[24], [25], [26], [27], [28],30], six reported LH levels [21,22,[25], [26], [27],30], three mentioned the KI score [21,24,27], and only one mentioned adverse events [21]. Besides, only one trial demonstrated follow-up [22], while another mentioned withdrawals and dropouts [28]. The basic characteristics of the included trials were shown in Table 1.
All the studies used a decoction in the experimental group. Five RCTs employed needle acupuncture [22,23,25,26,30], while five applied electroacupuncture [21,24,[27], [28], [29]] (Supplement Table). On the other hand, the control group received hormone therapy with estrogen and progesterone.
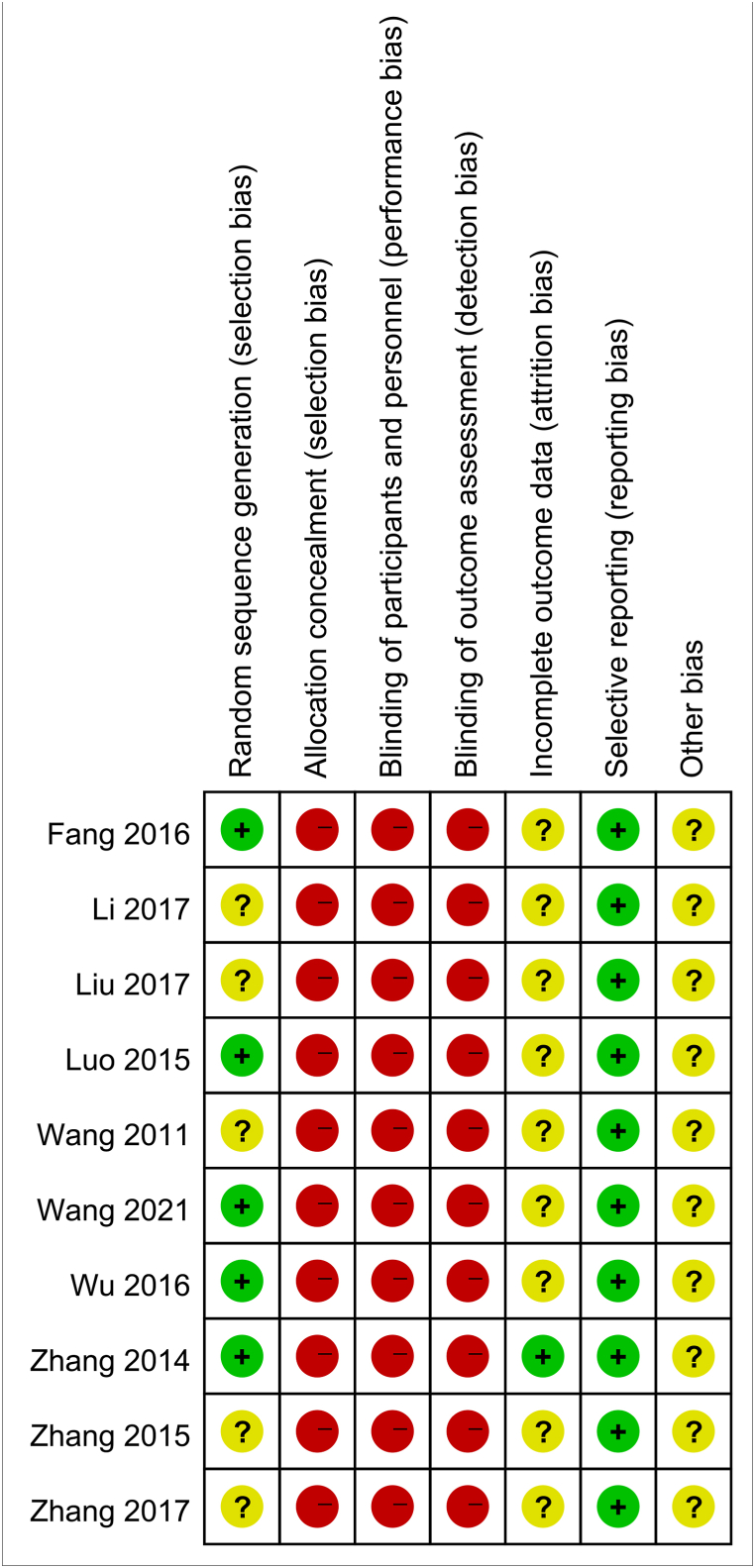
3.3. Risk of bias
Although all the studies were randomized, only four employed the random method (random number table) [21,24,26,27]. None of the included RCTs used any blinding or concealed allocation of investigators and patients. Only one reported the number of dropouts as well as the reasons for them [28]. None employed selective reporting. None of the studies computed the sample size in advance. A summary of the risk of bias is depicted in Fig. 2.
Fig. 2.
The risk of bias for each included study.
3.4. Evaluation of the therapeutic effect
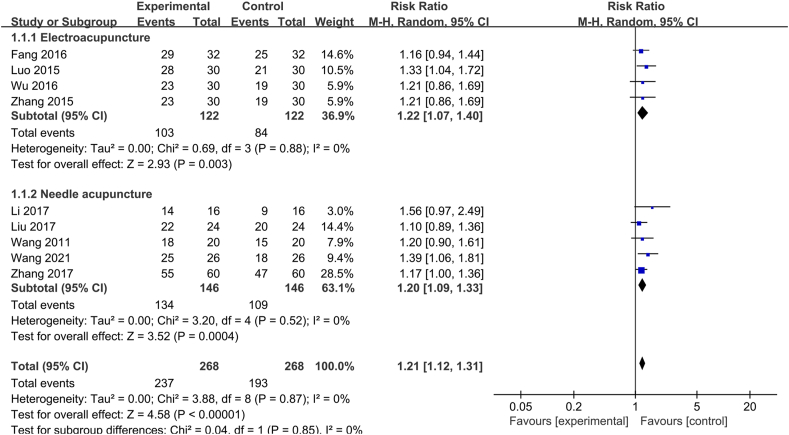
3.4.1. The total effective rate
Nine studies assessed the total effective rate. Our data illustrated that patients who received acupuncture in conjunction with CHM exhibited a higher total effective rate than those treated with western drugs (RR: 1.21; 95% CI: 1.12–1.31; P < 0.01, I2 = 0%, Fig. 3). Similarly, subgroup analysis showed that the acupuncture–CHM combination was associated with a superior total effective rate (Electroacupuncture: RR: 1.22; 95% CI: 1.07–1.40; P < 0.01, I2 = 0%; Needle acupuncture: RR: 1.20; 95% CI: 1.09–1.33; P < 0.01, I2 = 0%, Fig. 3).
Fig. 3.
Forest plot for total effective rate between the acupuncture plus CHM and the western drugs group. (CHM, Chinese herbal medicine).
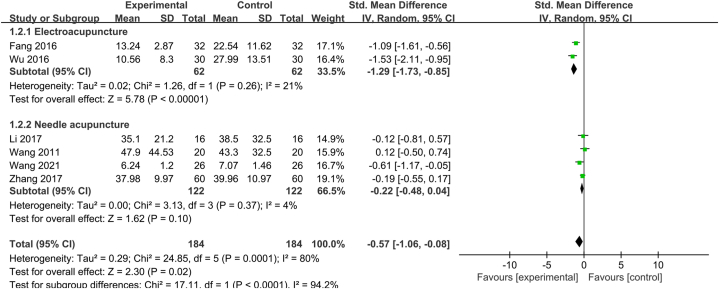
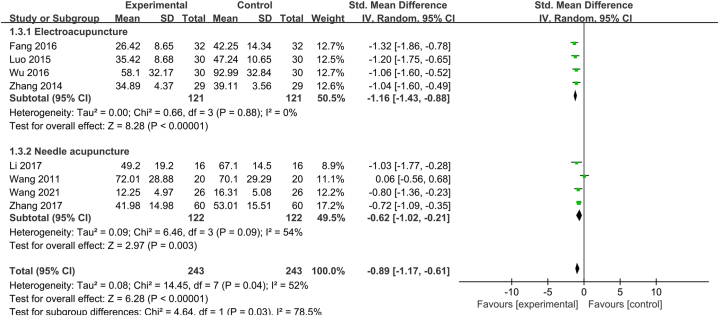
3.4.2. The LH levels
Six trials reported the LH levels. The acupuncture plus CHM group showed significantly lower serum LH levels, with significant heterogeneity (SMD: −0.57; 95% CI: −1.06, −0.08; P < 0.05, I2 = 80%, Fig. 4). Subgroup analysis, which was premised on the distinct forms of acupuncture significantly decreased the heterogeneity.
Fig. 4.
Forest plot for the LH levels between acupuncture plus CHM and western drugs group. (LH, luteinizing hormone; CHM, Chinese herbal medicine).
3.4.3. The FSH levels
Eight studies mentioned the FSH levels. The acupuncture plus CHM group displayed lower serum FSH levels (SMD: −0.89; 95% CI: −1.17, −0.61; P < 0.01, I2 = 52%, Fig. 5), with a 52% heterogeneity, which was not reduced after subgroup analysis.
Fig. 5.
Forest plot for the FSH levels between acupuncture plus CHM and western drugs group. (FSH, follicle-stimulating hormone; CHM, Chinese herbal medicine).
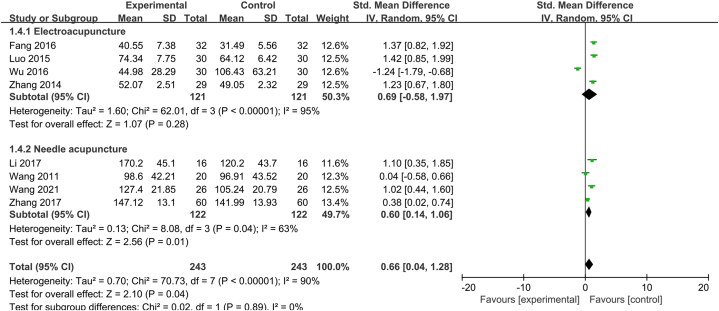
The E2 Levels.
Eight trials reported serum E2 levels, which were significantly higher in the acupuncture plus CHM group (SMD: 0.66; 95% CI: −0.04, 1.28; P < 0.05, I2 = 90%, Fig. 6). Similar, subgroup analysis did not reduce the heterogeneity.
Fig. 6.
Forest plot for the E2 levels between acupuncture plus CHM and western drugs group. (E2, estradiol; CHM, Chinese herbal medicine).
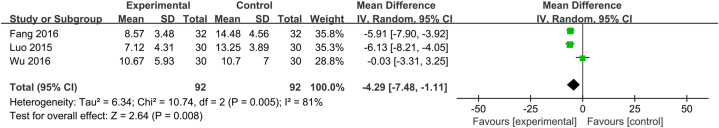
3.4.4. KI score
Three trials assessed the KI score, which was significantly lower in the combined treatment group (MD: −4.29; 95% CI: −7.48, −1.11; P < 0.01, I2 = 81%, Fig. 7).
Fig. 7.
Forest plot for the KI score between acupuncture plus CHM and western drugs group. (KI, Kupperman index; CHM, Chinese herbal medicine).
3.4.5. Adverse events
One study recorded episodes of nausea and vomiting and elevated alanine transaminase (ALT) [21], the occurrence of which was significantly lower occurrence in the acupuncture plus CHM group compared with that in the western medicine group.
However, a definitive conclusion could not be drawn from this study.
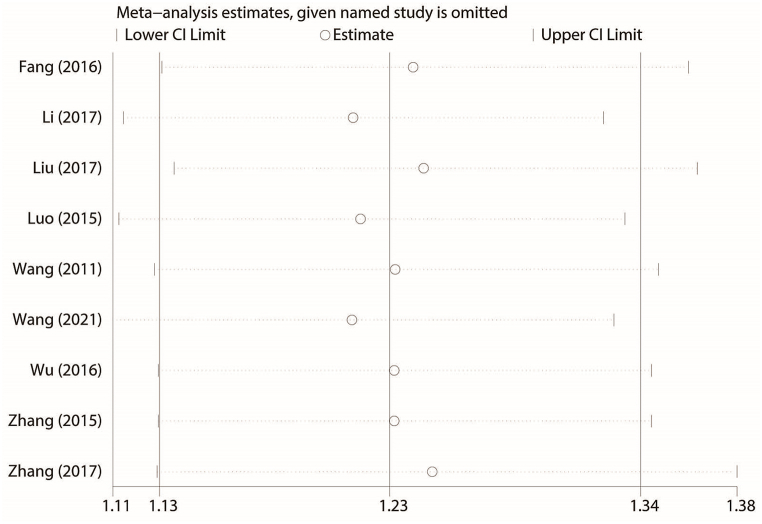
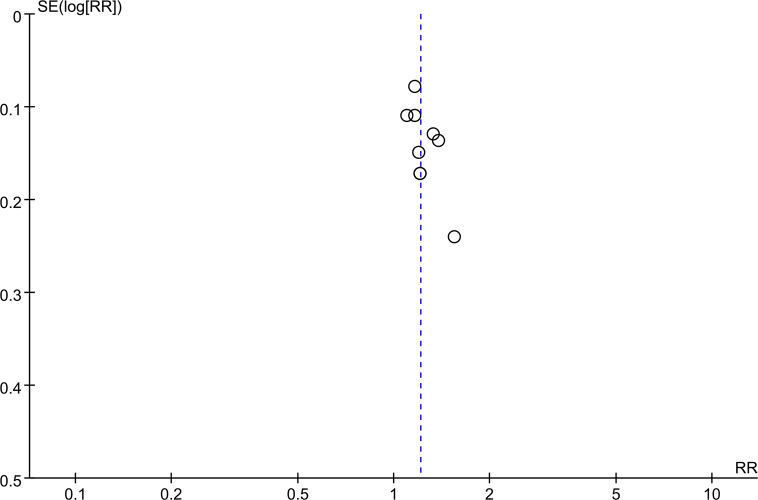
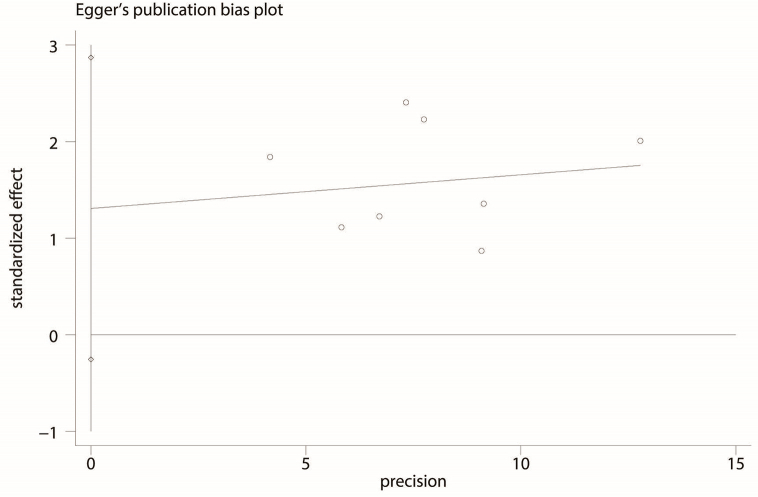
3.5. Publication bias and sensitivity analysis
While the funnel plot for the total effective rate illustrated an asymmetrical distribution (Supplementary Fig. 1), Egger's test illustrated no probable publication bias (P = 0.06, Supplementary Fig. 2). Sensitivity analysis showed unchanged effect estimates, which depicted the robustness of the pooled results (Fig. 8).
Fig. 8.
Sensitivity analysis for the total effective rate.
3.6. GRADE assessment
The quality of evidence was evaluated by using GRADEpro. The quality of chosen RCTs was low, thus the “Risk of bias” was classified as “serious”. Data regarding the serum FSH, LH, and E2 levels, and KI score had high I2 values, so the “Inconsistency” was classified as “serious”. The results of the GRADE assessment for total effective rate were moderate, while the quality for other outcomes was low (Table 2).
Table 2.
Results of GRADE evaluation.
| Outcome | Included studies (n) | Patients (n) | Quality of evidence | Reasons |
|---|---|---|---|---|
| Total effective rate | 9 | 536 | ⨁⨁⨁◯ MODERATE |
“Risk of bias” was downgraded to “serious" |
| Serum LH level | 6 | 368 | ⨁⨁◯◯ LOW |
“Risk of bias” was downgraded to “serious”; “Inconsistency” was downgraded to “serious" |
| Serum FSH level | 8 | 486 | ⨁⨁◯◯ LOW |
“Risk of bias” was downgraded to “serious”; “Inconsistency” was downgraded to “serious" |
| Serum E2 level | 8 | 486 | ⨁⨁◯◯ LOW |
“Risk of bias” was downgraded to “serious”; “Inconsistency” was downgraded to “serious" |
| KI score | 3 | 184 | ⨁⨁◯◯ LOW |
“Risk of bias” was downgraded to “serious”; “Inconsistency” was downgraded to “serious" |
Abbreviations: GRADE, Grading of Recommendations, Assessment, Development, and Evaluation; LH, luteinizing hormone; FSH, follicle-stimulating hormone; E2, Estradiol; KI, Kupperman index.
4. Discussion
4.1. Summary of evidence
This meta-analysis, which included outcomes from 10 RCTs with an aggregate number of 594 POI patients, provides a quantitative estimate of the clinical efficacy and safety of combining acupuncture and CHM to treat POI. The pooled data demonstrated that acupuncture plus CHM had a higher total effective rate than western medicine. The combination therapy yielded better outcomes with regards to serum LH, FSH, and E2 levels, and KI score, without obvious adverse events. Subgroup analysis premised on the different types of acupuncture, such as electroacupuncture and needle acupuncture, was further performed to detect potential sources of heterogeneity. For some outcome measures, the heterogeneity did not decrease significantly, implying that it may originate due to other reasons, including different dosage forms and compositions of the CHM, different diagnostic criteria, or various needling points. However, due to the poor methodology, further studies confirming the beneficial effects and safety of the combination therapy are required.
4.2. Significance of the study
POI is a frustrating gynecological endocrine disease, whose etiology remains unclear. Some studies have associated it with iatrogenic or endogenous factors. Besides limited literature on its optimal management, no existing drug that can halt its progression, a situation that has severely affected the physical and mental health of women [31]. Appropriate HRT plays an imperative part in the management of POI patients with strict indications and contraindications [32]. However, it introduces minor risks of diseases such as breast cancer, cardiovascular disease, stroke, and venous thromboembolism, depending on the type of HRT, duration, and individual health risks [33]. Therefore, many patients have resorted to complementary and alternative medicine for managing POI [34]. Among all the options, a combination of two TCM techniques—CHM and acupuncture—has emerged as a common therapeutic approach for POI in China as well as other Asian countries, even for young survivors of ovarian and breast cancer [20,35,36].
In the CHM, the pathogenesis and etiology of POI are often associated with blood stasis and kidney deficiency, which influence each other [37]. Hence, treatment via CHM aims to regulate hormone levels and improve ovarian function by improving blood circulation and tonifying the kidney. Both clinical and animal studies have illustrated that Chinese activating blood herbs and nourishing kidney herbs that are used to relieve POI symptoms, such as Chinese Yam, Dodder, and prepared Radix rehmanniae, exert phytoestrogen-like effects [38,39]. They can regulate or enhance immune functions and improve ovarian blood flow, thus regulating reproduction [[40], [41], [42], [43]]. These herbs can also promote follicle growth through the phosphoinositide 3-kinase/Akt signaling pathway [44].
On the other hand, two different but widely used types of acupuncture — electroacupuncture and needle acupuncture— have been shown to enhance ovarian blood flow, regulate the reproductive endocrine system, and improve ovarian function in women with POI [45]; [46]. The three most frequently utilized acupoints are Guanyuan (RN4), Sanyinjiao (SP6), and Zigong (EX-CA1), while the most employed meridians are the Ren Meridian, the Spleen Meridian of Foot-Taiyinand, and the Bladder Meridian of Foot-Taiyang. Most of the acupoints are distributed in the lower limbs, lumbar region, abdomen, and chest. A study found that acupuncture achieves the same therapeutic effect as estrogen in the treatment of POI, and might be acting by upregulating gene and protein expression in the phosphoinositide 3-kinase/Akt/mammalian target of rapamycin signaling pathway [47]. Moreover, electroacupuncture pretreatment exerted a certain protective effect on ovarian health in rats with POI by upregulating ovarian granular cells and inhibiting the expression of Bcl-2 and Bax [48]. Although acupuncture can produce noticeable and rapid effects without causing an adverse reaction, it is restricted by its action span and area [49].
Dating back to an ancient Chinese practice mentioned in Huangdi's Internal Classic (Huang Di Nei Jing), the combination of acupuncture and CHM is a comprehensive therapeutic option for preventing and treating diseases [14], [50]. “when disease forms, acupuncture can be used to treat its outside and CHM to treat its inside” is one of the most important classical quotes in TCM. Acupuncture and CHM act via different mechanisms. While acupuncture can relieve pain, regulate qi and blood, and treat meridian diseases, CHM can tonify qi, nourish yin, and effectively treat Zangfu diseases [51]. By affecting signaling pathways, acupuncture and CHM can play a regulatory role and produce a synergistic curative effect, lengthening the duration of efficacy, minimizing the side effects, and shortening the course of treatment, especially in POI patients who respond poorly to acupuncture or CHM alone. The use of acupuncture and herbs can treat hormonal disorders, creating a conducive environment for conceiving and maintaining pregnancy [52]. Besides, the combined treatment option could improve ovarian function in rats with a decreased ovarian reserve. The treatments might be preventing or delaying apoptosis of follicular granulosa cells, slowing follicular atresia, and positively regulating follicular development in rats [53].
In summary, the acupuncture–CHM combination may innovate and optimize the treatment pattern, offering more options and broadening the scope of treatment for POI.
4.3. Limitation
While we have expansively analyzed and evaluated all the selected RCTs, this study was inevitably associated with some shortcomings. First, the selected RCTs had low quality since they employed unclear blinding methods, attrition bias, selective bias, and allocation concealment. Secondly, despite undertaking an unbiased literature search with no language restriction, all the RCTs chosen for this review were performed in China and published in Chinese with no relevant foreign experiments, which potentially contributes to a bias and negatively impacts their representativeness. Thirdly, only a few RCTs employed long-term follow-up, implying that the long-term safety of the interventions is unclear. Fourth, though the intervention and control cohorts were stringently integrated into this meta-analysis, high or moderate heterogeneity still existed, likely due to the different ingredients of CHM and the diverse acupuncture operations performed in the studies. Thus, the lack of high-quality RCTs inevitably impeded the robust assessment of the efficacy of the intervention, which impacted the stability and accuracy of the evaluation test.
5. Conclusion
To summarize, the results of our meta-analysis illustrated that the use of acupuncture in conjunction with CHM is a safe and efficacious therapeutic option for patients with POI. Nevertheless, since the quality of the selected RCTs is relatively low, further studies investigating follow-up and adverse events are needed to confirm these findings. Well-designed, large-sample, and multicenter clinical studies are required in the future to investigate the efficacy of acupuncture combined with CHM for treating POI, and to derive a scientific, objective, and reliable conclusion.
Funding
This study was supported by grants from National Natural Science Foundation of China (82004405), Zhejiang Province Traditional Chinese Medicine Science and Technology Project (Grant NO. 2021ZB299, 2023ZL366).
Author contribution statement
Hui-fang Li; Wen-jun Chen: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper. Jin-xia Zhang: Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
Thank for Zhang-feng Feng and Yang Yi for helping with this study. We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Abbreviations
- ALT
alanine transaminase
- CHM
Chinese herbal medicine
- CI
confidence interval
- E2
estradiol
- EX-CA1
Zigong
- FSH
follicle-stimulating hormone
- GRADE
Grading of Recommendations, Assessment, Development, and Evaluation
- HRT
hormone replacement therapy
- KI
Kupperman index
- LH
luteinizing hormone
- MD
mean difference
- POI
premature ovarian insufficiency
- RCT
randomized controlled trial
- RevMan
Review Manager
- RR
relative risk
- SMD
standardized mean difference
- RN4
Guanyuan
- SP6
Sanyinjiao
- TCM
traditional Chinese medicine
Appendix A. Supplementary data
The following is/are the supplementary data to this article:
References
- 1.Webber L., Davies M., Anderson R., Bartlett J., Braat D., Cartwright B., et al. ESHRE Guideline: management of women with premature ovarian insufficiency. Hum. Reprod. (Oxf.) 2016;31:926–937. doi: 10.1093/humrep/dew027. [DOI] [PubMed] [Google Scholar]
- 2.Lim Y.M., Jeong K., Lee S.R., Chung H.W., Lee W. Association between premature ovarian insufficiency, early menopause, socioeconomic status in a nationally representative sample from Korea. Maturitas. 2019;121:22–27. doi: 10.1016/j.maturitas.2018.12.004. [DOI] [PubMed] [Google Scholar]
- 3.Sharif K., Watad A., Bridgewood C., Kanduc D., Amital H., Shoenfeld Y. Clinical endocrinology & metabolism; 2019. Insights into the Autoimmune Aspect of Premature Ovarian Insufficiency. Best Practice & Research. [DOI] [PubMed] [Google Scholar]
- 4.Ni Y., Xu D., Lv F., Wan Y., Fan G., Zou W., et al. Prenatal ethanol exposure induces susceptibility to premature ovarian insufficiency. J. Endocrinol. 2019 doi: 10.1530/JOE-19-0063. [DOI] [PubMed] [Google Scholar]
- 5.Tao X.Y., Zuo A.Z., Wang J.Q., Tao F.B. Effect of primary ovarian insufficiency and early natural menopause on mortality: a meta-analysis. Climacteric : the journal of the International Menopause Society. 2016;19:27–36. doi: 10.3109/13697137.2015.1094784. [DOI] [PubMed] [Google Scholar]
- 6.Podfigurna A., Meczekalski B. Cardiovascular health in patients with premature ovarian insufficiency. Management of long-term consequences. Przeglad menopauzalny = Menopause review. 2018;17:109–111. doi: 10.5114/pm.2018.78551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goh M., Nguyen H.H. Identifying and addressing osteoporosis knowledge gaps in women with premature ovarian insufficiency and early menopause. A mixed-methods study. 2019;91:498–507. doi: 10.1111/cen.14049. [DOI] [PubMed] [Google Scholar]
- 8.Whitcomb B.W., Purdue-Smithe A., Hankinson S.E., Manson J.E., Rosner B.A., Bertone-Johnson E.R. Menstrual cycle characteristics in adolescence and early adulthood are associated with risk of early natural menopause. J. Clin. Endocrinol. Metab. 2018;103:3909–3918. doi: 10.1210/jc.2018-01110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Podfigurna-Stopa A., Czyzyk A., Grymowicz M., Smolarczyk R., Katulski K., Czajkowski K., et al. Premature ovarian insufficiency: the context of long-term effects. J. Endocrinol. Invest. 2016;39:983–990. doi: 10.1007/s40618-016-0467-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Domniz N., Meirow D. Premature ovarian insufficiency and autoimmune diseases. Best Pract. Res. Clin. Obstet. Gynaecol. 2019;60:42–55. doi: 10.1016/j.bpobgyn.2019.07.008. [DOI] [PubMed] [Google Scholar]
- 11.Wang Y.R., Zhang L.M. Advances in TCM research on premature ovarian insufficiency. Journal of Qiannan Medical College for Nationalities. 2019;32:100–103. [Google Scholar]
- 12.Xia L.J., Xia Y.B. Clinical research and the effect mechanism on premature ovarian failure treated with acupuncture in recent 20 years. Chin. Acupunct. Moxibustion. 2018;38:565–570. doi: 10.13703/j.0255-2930.2018.05.031. [DOI] [PubMed] [Google Scholar]
- 13.Xu F.H., Hou Y.N., Ge P.L., Chen H.Z. Characteristic treatment of traditional Chinese medicine on premature ovarian failure. Journal of Liaoning University of Traditional Chinese Medicine. 2020;22:25–28. [Google Scholar]
- 14.Zhou S., Dong L., He Y., Xiao H. Acupuncture plus herbal medicine for alzheimer's disease: a systematic review and meta-analysis. Am. J. Chin. Med. 2017;45:1327–1344. doi: 10.1142/S0192415X17500732. [DOI] [PubMed] [Google Scholar]
- 15.Matsumoto-Miyazaki J., Ushikoshi H., Miyata S., Miyazaki N., Nawa T., Okada H., et al. Acupuncture and traditional herbal medicine therapy prevent deliriumin patients with cardiovascular disease in intensive care units. Am. J. Chin. Med. 2017;45:255–268. doi: 10.1142/S0192415X17500161. [DOI] [PubMed] [Google Scholar]
- 16.Li H.F., Shen Q.H., Chen W.J., Chen W.M. Efficacy of traditional Chinese medicine tonifying kidney (bushen) and activating blood (huoxue) prescription for premature ovarian insufficiency: a systematic review and meta-analysis. Evidence-Based complementary and alternative medicine : eCAM. 2020;2020:1789304. doi: 10.1155/2020/1789304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang J., Huang X., Liu Y., He Y., Yu H. A comparison of the effects of Chinese non-pharmaceutical therapies for premature ovarian failure: a PRISMA-compliant systematic review and network meta-analysis. Medicine. 2020;99 doi: 10.1097/MD.0000000000020958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geng X., Cong P.W., Ni F.M., Cao R. Clinical meta-analysis of treating premature ovarian failure by medicine and acupuncture. Chinese Archives of Traditional Chinese Medicine. 2017;35:1295–1298. [Google Scholar]
- 19.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J. Clin. Epidemiol. 2009;62:1006–1012. doi: 10.1016/j.jclinepi.2009.06.005. [DOI] [PubMed] [Google Scholar]
- 20.Xy Z. China Medical Science and Technology Press; Beijing: 2002. Guidance Principle of Clinical Research on New Drug of Traditional Chinese Medicine (Trial) pp. 379–383. [Google Scholar]
- 21.Fang Q.X., Zou P., Chen R.X. Clinical study on treatment of 32 cases of POF of kidney deficiency and liver stagnation syndrome by bushen shugan formula combined with electroacupuncture. Shandong J. Tradit. Chin. Med. 2016;35:294–296. [Google Scholar]
- 22.Li L.L. Clinical study on the treatment of premature ovarian failure infertility with acupuncture and Chinese. medicine Asia-Pacific Traditional Medicine. 2017;13:124–126. [Google Scholar]
- 23.Liu H.T. Effect of combination of acupuncture and Chinese herbal medicine on premature ovarian failure. Electronic Journal of Practical Gynecologic Endocrinology. 2017;4:49–50. [Google Scholar]
- 24.Luo J.J., Li H., Liu D.Z. Clinical observation on 30 cases of premature ovarian failure treated with electroacupuncture combined with Bushen Huoxue recipe. Guiding Journal of Traditional Chinese Medicine and Pharmacy. 2015;21:46–48. [Google Scholar]
- 25.Wang H.M., Li L., Mi H.R. Clinical study of acupuncture combined with nourishing blood and tonifying kidney formula in treating premature ovarian failure. Journal of Hebei Traditional Chinese Medicine and Pharmacology. 2011;26:28–29. [Google Scholar]
- 26.Wang Y Y., Shi X.H. The clinical efficacy of kidney-tonifying and blood-activating prescription combined with acupuncture for the patients with premature ovarian insufficiency. CHINA MEDICINE AND PHARMACY. 2021;11:5. [Google Scholar]
- 27.Wu Y., Liu J.H., Huang L.L., Zhu Y.M., Zhao Y. Clinical observation of Xiantu Heche recipe combined with electroacupuncture in the treatment of premature ovarian failure with kidney deficiency and liver stagnation syndrome. Shanghai J. Tradit. Chin. Med. 2016;50:59–62. [Google Scholar]
- 28.Zhang C.K., Qin Y.A., Zhao Q., Lan Q., Luo Y.Y. Effect of combination of acupuncture and hormone sequential therapy on serum FSH. E2 on premature ovarian failure patients Asia-Pacific Traditional Medicine. 2014;10:76–77. [Google Scholar]
- 29.Zhang D.Y. Clinical study on treatment of premature ovarian failure of kidney deficiency and liver depression with compound Chinese medicine and acupuncture for kidney deficiency and liver depression. Asia-Pacific Traditional Medicine. 2015 [Google Scholar]
- 30.Zhang Y., Zhang Q. Clinical observation on treatment of premature ovarian failure by acupuncture and Chinese herbal medicine. Journal of Practical Traditional Chinese Medicine. 2017;33:889–890. [Google Scholar]
- 31.Tsiligiannis S., Panay N., Stevenson J.C. Premature ovarian insufficiency and long-term health consequences. Curr. Vasc. Pharmacol. 2019;17:604–609. doi: 10.2174/1570161117666190122101611. [DOI] [PubMed] [Google Scholar]
- 32.Sullivan S.D., Sarrel P.M., Nelson L.M. Hormone replacement therapy in young women with primary ovarian insufficiency and early menopause. Fertil. Steril. 2016;106:1588–1599. doi: 10.1016/j.fertnstert.2016.09.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saul H., Gursul D., Cassidy S., Vinogradova Y. Risk of breast cancer with HRT depends on therapy type and duration. Br. Med. J. Int. Ed. 2022;376:o485. doi: 10.1136/bmj.o485. [DOI] [PubMed] [Google Scholar]
- 34.Posadzki P., Lee M.S., Moon T.W., Choi T.Y., Park T.Y., Ernst E. Prevalence of complementary and alternative medicine (CAM) use by menopausal women: a systematic review of surveys. Maturitas. 2013;75:34–43. doi: 10.1016/j.maturitas.2013.02.005. [DOI] [PubMed] [Google Scholar]
- 35.Ma K., Yuan Y., Zhang H.X. [Clinical efficacy of Bushen Culuan Decoction in treating infertility due to premature ovarian insufficiency] Zhongguo Zhong yao za zhi = Zhongguo zhongyao zazhi = China journal of Chinese materia medica. 2019;44:1075–1079. doi: 10.19540/j.cnki.cjcmm.20181225.005. [DOI] [PubMed] [Google Scholar]
- 36.Zhang J.W., Liu Y.S., Deng R., Guo Y.B., Yan B., Chen P.D., et al. Observation on therapeutic effect of "Tiaoren Tongdu acupuncture" on premature ovarian insufficiency of kidney deficiency. Zhongguo zhen jiu = Chinese acupuncture & moxibustion. 2019;39:579–582. doi: 10.13703/j.0255-2930.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 37.Zhang Y., Liu Y., Wang H., Wang P.J. Professor Wang's experience in treating early-onset ovarian insufficiency by kidney-tonifying and blood-activating therapy. Nei Mongol Journal of Traditional Chinese Medicine. 2020;39:70–72. [Google Scholar]
- 38.Sun L. Phytoestrogens of traditional Chinese medicine for bushen huoxue huayu. Chinese Journal of Gerontology. 2019;39:4875–4880. [Google Scholar]
- 39.Zhao L., Zheng H., Xu Y., Lin N. Research progress in phytoestrogens of traditional Chinese medicine. China J. Chin. Mater. Med. 2017;42:3474–3487. doi: 10.19540/j.cnki.cjcmm.2017.0135. [DOI] [PubMed] [Google Scholar]
- 40.Zhang R., Shu X. Experimental study on the effect of Chinese herbal compound tonifying kidney and activating blood on osteoblasts. Chin. J. Pathophysiol. 2003:49–52. [Google Scholar]
- 41.Zhou X., Chen Y. Summary of mechanism of treating diminished ovarian reserve with traditional Chinese medicine of tonifying kidney and activating blood. Chinese Journal of Traditional Medical Science and Technology. 2014;21:345–346. [Google Scholar]
- 42.Liu H., Xiao Y., Li L., Qi P. The influencen of Bushen Huoxue Prescription on follicular granulosa cell apoptosis of premature ovarian failure (POF) mice. Chin. J. Inf. Tradit. Chin. Med. 2015;22:47–50. [Google Scholar]
- 43.Zhao H., Shan Y., Ma Z., Yu M., Gong B. A network pharmacology approach to explore active compounds and pharmacological mechanisms of epimedium for treatment of premature ovarian insufficiency. Drug Des. Dev. Ther. 2019;13:2997–3007. doi: 10.2147/DDDT.S207823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Long X. Chengdu University of Traditional Chinese Medicine; 2015. Effect of Tonifying Kidney and Activating Blood Method on the GTW Serum Cultivated Rat Ovary Granulosa Cell in Vitro Based on PI3K/AKT Signaling Pathway. [Google Scholar]
- 45.Wang L.M., Zhang Y.C., Jia H.L. Research advances in the mechanism of acupuncture treatment for premature ovarian failure in recent 10 years. Shanghai Journal of Acupuncture and Moxibustion. 2017;36:361–364. [Google Scholar]
- 46.Li X.T., Fang Y.G., Shang J., Guo X.C. Ideas and exploration on acupuncture treatment of premature ovarian failure. China Journal of Traditional Chinese Medicine and Pharmacy. 2016;31:3170–3172. [Google Scholar]
- 47.Zhang Y.M., Yu B., Chen J., Zhao Z.S. Effects of acupuncture on PI3K/Akt/mTOR signaling pathway in rats. with premature ovarian failure Chinese Acupuncture & Moxibustion. 2015;35:53–58. [PubMed] [Google Scholar]
- 48.Wang W., Wang Y., Wu J., Yang L., Liu Z. Protective effects of electroacupuncture pretreatment on ovarian in rats with premature ovarian insufficiency. Chin. Acupunct. Moxibustion. 2018;38:405–411. doi: 10.13703/j.0255-2930.2018.04.016. [DOI] [PubMed] [Google Scholar]
- 49.Ernst E., Lee M.S., Choi T.Y. Acupuncture in obstetrics and gynecology: an overview of systematic reviews. Am. J. Chin. Med. 2011;39:423–431. doi: 10.1142/S0192415X11008920. [DOI] [PubMed] [Google Scholar]
- 50.Yan J., Miao Z.W., Lu J., Ge F., Yu L.H., Shang W.B. vol. 2019. 2019. (Acupuncture Plus Chinese Herbal Medicine for Irritable Bowel Syndrome with Diarrhea: A Systematic Review and Meta-Analysis). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wang W.M., Wang X.B., Zhao J. Preliminary study of acupuncture combined with TCM medication in the prevention and treatment of POI. Journal of Clinical Acupuncture and Moxibustion. 2020;36:84–88. [Google Scholar]
- 52.Jiang D., Li L., Wan S., Meng F. Acupuncture and Chinese herbal medicine effects on assisted reproductive technology: six cases and their clinical significance. Med. Acupunct. 2019;31:395–406. doi: 10.1089/acu.2019.1338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Zhang H., Chen M., Zhang Y.C., Jin S.Z. Effcet of acupuncture combined with Chinese herbs on apoptotic factors of ovarian cells and reproductive hormone in rats of decreased ovarian reserve. Henan Traditional Chinese Medicine. 2019;39:1193–1196. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.