Abstract
目的
麻醉前超声测量胃窦部横截面积(cross-sectional area, CSA), 观察术前2 h口服碳水化合物300 mL对妇科腹腔镜手术特殊头低臀高仰卧截石体位患者麻醉前胃容量(gastric volume, GV)的影响, 并评估患者发生反流误吸的风险。
方法
选择2020年6月至2021年2月在北京大学国际医院择期行妇科腹腔镜手术特殊头低臀高仰卧截石体位患者80例, 年龄18~65岁, 体重指数18~35 kg/m2, 美国麻醉医师学会(American Society of Anesthesiologists, ASA)分级Ⅰ或Ⅱ级。采用随机数字表法将患者随机分为干预组和对照组, 每组40例。干预组患者手术前一日24:00后禁食, 对于首台手术患者, 手术日5:30口服碳水化合物300 mL; 对于接台手术患者在预计手术开始前2 h口服碳水化合物300 mL。对照组患者于手术前一日24:00后常规禁食禁饮。麻醉前分别在仰卧位和右侧卧位下行胃窦部超声检查。记录仰卧位和右侧卧位下CSA, 计算出两组患者麻醉前GV, 使用Perlas A半定量评级及胃容量/体质量(gastric volume/weight, GV/W)评估患者发生反流误吸的风险, 记录术前口渴感、饥饿感视觉模拟评分(visual analogue scale, VAS)等。
结果
两组共80例患者均完成胃窦部超声评估及测量, 干预组和对照组麻醉前GV分别为(58.8±23.6) mL和(56.3±22.1) mL, GV/W分别为(0.97±0.39) mL/kg和(0.95±0.35) mL/kg, 上述指标两组间差异均无统计学意义(P>0.05)。Perlas A半定量评级: 干预组0级24例(60%), 1级15例(37.5%), 2级1例(2.5%); 对照组0级25例(62.5%), 1级13例(32.5%), 2级2例(5%), 两组评级构成比差异无统计学意义(P>0.05)。两组共3例(干预组1例, 对照组2例)Perlas A半定量评级为2级的患者, 经干预, 均未发生反流误吸。与对照组比较, 干预组术前口渴感、饥饿感VAS明显降低(P<0.05)。
结论
妇科腹腔镜手术特殊头低臀高仰卧截石体位患者术前2 h口服300 mL碳水化合物, 麻醉前胃容量未见增加, 反流误吸风险未见增加, 对患者生理需求的干扰减少, 患者舒适度增加。
Keywords: 胃窦部超声, 胃容量, 术前禁食禁饮, 加速康复外科, 头低臀高体
Abstract
Objective
To investigate the effect of 300 mL carbohydrates intake two hours before sur-gery on the gastric volume (GV) in patients positioning in trendelenburg undergoing gynecological laparoscopic procedures by using gastric antrum sonography, and further assess the risk of reflux aspiration.
Methods
From June 2020 to February 2021, a total of 80 patients, aged 18–65 years, body mass index (BMI) 18–35 kg/m2, falling into American Society of Anesthesiologists (ASA) physical status Ⅰ or Ⅱ, scheduled for gynecological laparoscopic procedures positioning in trendelenburg were recruited and divided into two groups: the observation group (n =40) and the control group (n=40). In the observation group, solid food was restricted after 24:00, the patients were required to take 300 mL carbohydrates two hours before surgery. In the control group, solid food and liquid intake were restricted after 24:00 the night before surgery. The cross-sectional area (CSA) of gastric antrum was measured in supine position and right lateral decubitus position before anesthesia. Primary outcome was gastric volume (GV) in each group. Secondary outcome included Perlas A semi-quantitative grading and gastric volume/weight (GV/W). All the patients received assessment of preoperative feeling of thirsty and hunger with visual analogue scale (VAS).
Results
Complete data were available in eighty patients. GV was (58.8±23.6) mL in the intervention group vs. (56.3±22.1) mL in the control group, GV/W was (0.97±0.39) mL/kg vs. (0.95±0.35) mL/kg, respectively; all the above showed no significant difference between the two groups (P > 0.05). Perlas A semi-quantitative grading showed 0 in 24 patients (60%), 1 in 15 patients (37.5%), 2 in 1 patient (2.5%) in the intervention group and 0 in 25 (62.5%), 1 in 13 (32.5%), 2 in 2 (5%) in the control group, the proportion of Perlas A semi-quantitative grading showed no significant difference between the two groups (P > 0.05). A total of 3 patients (1 in the intervention group and 2 in the control group) with Perlas A semi-quantitative grading 2 were treated with special intervention, no aspiration case was observed in this study. The observation group endured less thirst and hunger (P<0.05).
Conclusion
Three hundred mL carbohydrates intake two hours before surgery along with ultrasound guided gastric content monitoring does not increase gastric volume and the risk of reflux aspiration in patients positioning in trendelenburg undergoing gynecological laparoscopic surgery, and is helpful in minimizing disturbance to the patient's physiological needs, therefore leading to better clinical outcome.
Keywords: Gastric ultrasonography, Gastric volume, Fasting, Enhanced recovery surgery, Trendelenburg position
近年来,加速康复外科(enhanced recovery surgery,ERAS)理念在我国外科领域更新迅速,权威文献肯定了ERAS的临床意义,尤其是促进术后康复的效果[1]。饮食管理是ERAS围术期系列管理措施中一项重要内容,2012年ERAS指南提出术前6 h禁食、2 h禁饮新标准[2],但其循证医学证据多来自结直肠手术,来源相对单一,推广到其他特殊体位手术尚需更多临床实践及循证医学证据。妇科腹腔镜手术较开腹结直肠手术的差异主要体现在两方面:其一,建立人工CO2气腹后腹内压增高,膈肌上抬,使胃内压增高,病人发生反流乃至误吸概率大幅增加[3];其二,手术体位为头低臀高仰卧截石体位,受重力作用,胃内容物易反流,更易发生误吸[3-4],有报道此类手术中反流发生率为3%~7%[5-8]。在没有客观可靠的胃容量(gastric volume,GV)评估指标的情况下,缩短妇科腔镜手术患者术前禁食禁饮时间,在麻醉安全方面尚存在顾虑。床旁胃窦部超声判断胃内容物不仅具有无创、快速的特点而且准确、可靠[9-10],能够对反流误吸高风险患者做出筛选[11],提高手术麻醉患者的安全性。本研究旨在通过床旁胃窦部超声技术,评估缩短妇科腔镜手术术前禁饮时间是否增加患者麻醉前GV,是否增加特殊头低臀高仰卧截石体位患者围术期反流误吸风险,验证这类特殊体位的妇科腔镜手术患者术前口服碳水化合物的安全性。
1. 资料与方法
1.1. 研究对象
本研究为前瞻性随机病例对照研究,研究开始前已经北京大学国际医院伦理委员会审查批准(批准文号:YJ2020-013),所有参与研究的患者均签署知情同意书。
选择2020年6月至2021年2月在北京大学国际医院择期行妇科腔镜手术的良性疾病以及早期恶性肿瘤患者80例。入选标准: 年龄18~65岁,美国麻醉医师学会(American Society of Anesthesiologists,ASA)分级为Ⅰ级或Ⅱ级,体重指数(body mass index,BMI)<35 kg/m2。排除标准: 合并幽门梗阻、反流性食管炎、食道裂孔疝、未控制稳定的糖尿病、严重的肝肾功能不全者;有消化道手术史者;近期服用影响胃肠动力药物者;精神障碍不能合作者。
采用随机数字表法,将患者随机分为干预组(n=40)和对照组(n=40)。干预组术前一日24:00后禁食,首台手术患者术日5:30口服碳水化合物[5%(质量分数)葡萄糖溶液]300 mL,接台手术患者在预期手术开始前2小时口服碳水化合物300 mL[12];对照组术前一日24:00后禁食禁饮。
1.2. 麻醉过程
采用盲法,麻醉医生不知道分组情况,对所有患者行口渴感及饥饿感视觉模拟评分(visual analogue scale,VAS),然后使用Phlips CX 50超声仪,选用腹部超声低频探头(频率为2~5 Hz),依次对患者行仰卧位、右侧卧位下胃窦扫描, 超声图像的切面以肝左叶及腹主动脉为内参[9],采用开放轨迹法测量胃窦部位横截面积(cross-sectional area,CSA),记录两种体位下CSA(为减小测量误差,两种体位下所有数据取3次测量的均值)。
麻醉医生再对患者行Perlas A半定量评级[10],评估反流误吸风险,若在仰卧位和右侧卧位下胃窦部位均未发现明显液体记0分,超声示胃窦前后壁接近平行(图 1);仰卧位时胃窦部未发现液体而右侧卧位发现明显液体记1分,超声示胃窦呈扩张态,前后壁变薄有低回声(图 2);两种体位下胃窦部均探测到明显液体记2分。任一体位下发现固体记录固体。根据右侧卧位下预测GV的公式[11][GV(mL)=27.0 + 14.6 × CSA(cm2)-1.28×年龄(岁)]计算GV,进而计算胃容量/体质量(gastric volume/weight,GV/W)。患者Perlas A半定量分级为2分或发现固体或GV/W≥1. 5 mL/kg时,判定患者为反流误吸高风险;当患者Perlas A半定量分级小于2分且GV/W<1.5 mL/kg时,判定患者为反流误吸低风险[11, 13-14]。
图 1.
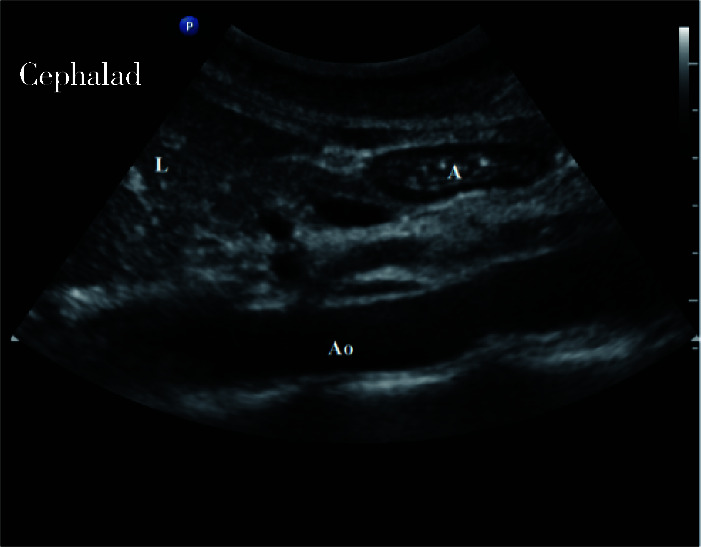
“空胃”胃超声图像
The sonoanatomic image of the stomach when empty stomach with collapsed pylorus
图 2.
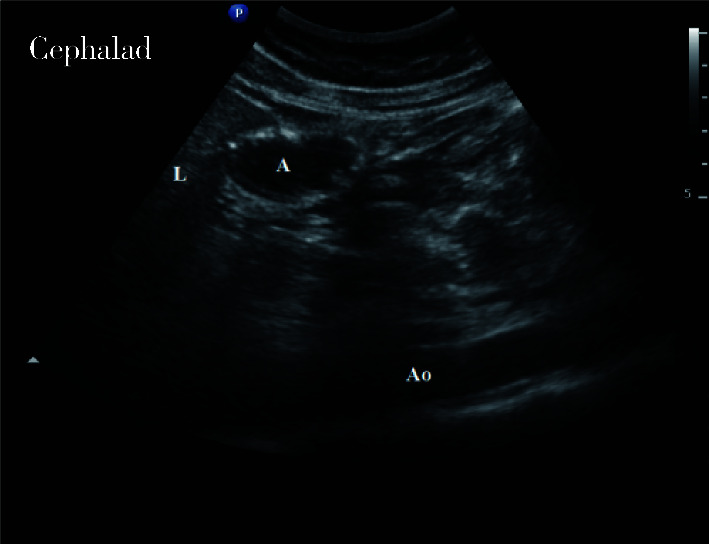
胃内有液体时胃超声图像
The sonoanatomic image of the stomach filled with clear liquids
反流误吸低风险患者,常规麻醉诱导。反流误吸高风险患者,采用快速序贯诱导,面罩吸纯氧3 min,氧流量6 L/min,吸氧去氮后(不予面罩正压通气)静脉注射咪达唑仑0.02 mg/kg,舒芬太尼0.3 μg/kg,丙泊酚2 mg/kg,患者意识消失由助手按压环状软骨,立即静脉注射罗库溴铵1 mg/kg,1 min后使用可视喉镜行气管插管成功后,气囊注气连接麻醉机。置入胃管,抽吸胃内容物。麻醉维持均采用丙泊酚、瑞芬太尼全凭静脉麻醉,维持脑电双频指数(bispectral index,BIS)40~60,间断注射罗库溴铵。术中经过调整麻醉深度及补液后,血压降低超过基础血压20%,给予麻黄碱6 mg/次。手术结束时停止麻醉。
1.3. 观察指标
记录仰卧位和右侧卧位下CSA, 计算出两组患者麻醉前GV,使用Perlas A半定量评级及GV/W评估患者发生反流误吸的风险,记录术前口渴感、饥饿感VAS。
记录诱导前10 min(基础值T0)、插管后5 min(T1)、手术开始后5 min(T2)各时点的平均动脉压和心率。记录术中麻黄碱使用情况、输液量、出血量。术后24 h随访记录患者是否有恶心呕吐、低氧血症等。
1.4. 统计学分析
使用SPSS 20.0软件进行统计分析,以麻醉前GV进行样本量计算,预实验6例常规禁食水患者麻醉前GV为(57±9) mL,研究假设口服碳水化合物增加麻醉前GV为10%(6 mL), 设β=0.2,显著性水准双侧α,两组按1 ∶ 1进行病例分配,计算后样本量为每组35例。考虑到可能的病例脱落,最终每组纳入40例。正态分布的计量资料以x±s表示,组间比较采用独立样本t检验。非正态分布计量资料以M(min,max)表示,组间比较采用Mann-Whitney U非参数检验。计数资料用n(%)表示,组间比较采用χ2检验及Fisher确切概率法。P<0.05为差异有统计学意义。
2. 结果
干预组和对照组共80例患者,均在胃窦部超声评估下完成Perlas A半定量评级和CSA测量。两组患者一般情况差异无统计学意义(表 1)。仰卧位下,干预组和对照组的CSA分别为(378±111) mm2和(384±114) mm2;右侧卧位下,干预组和对照组的CSA分别为(566±173) mm2和(572±163) mm2,GV分别为(58.8±23.6) mL和(56.3±22.1)mL,GV/W分别为(0.97±0.39) mL/kg和(0.95±0.35) mL/kg,上述指标两组间差异均无统计学意义(P>0.05,表 2)。
表 1.
两组患者一般临床资料比较
The demographics of patients in two groups
| Items | Intervention group (n=40) | Control group (n=40) | Statistical value | P |
| BMI, body mass index; ASA, American Society of Anesthesiologists. | ||||
| Age/years, x±s | 40±10 | 42±10 | t=1.115 | 0.268 |
| Height/cm, x±s | 161±5 | 162±4 | t=1.193 | 0.236 |
| Weight/kg, x±s | 61.4±8.9 | 59.2±8.2 | t=-1.170 | 0.245 |
| BMI/(kg/m2), x±s | 23.8±3.5 | 22.6±3.2 | t=0.340 | 0.113 |
| ASA, Ⅰ/Ⅱ | 15/25 | 22/18 | χ2=2.464 | 0.116 |
| Patients combined diabetes, n (%) | 3 (7.5) | 4 (10) | 1.000 | |
表 2.
两组患者胃超声测量值及Perlas A半定量评级比较
Main ultrasound data and Perlas A grading scale in two groups
| Items | Intervention group (n=40) | Control group (n=40) | Statistical value | P |
| CSA, antral cross-sectional area; RLD, right lateral decubitus position; GV/W, gastric volume /weight. | ||||
| CSA in supine/(mm2), x±s | 378±111 | 384±114 | t=0.263 | 0.793 |
| CSA in RLD/(mm2), x±s | 566±173 | 572±163 | t=0.167 | 0.868 |
| Gastric volume/mL, x±s | 58.8±23.6 | 56.3±22.1 | t=-0.491 | 0.625 |
| GV/W/(mL/kg), x±s | 0.97±0.39 | 0.95±0.35 | t=-0.170 | 0.865 |
| Perlas A grade, n (%) | Z=-0.130 | 0.897 | ||
| 0 | 24 (60) | 25 (62.5) | ||
| 1 | 15 (37.5) | 13 (32.5) | ||
| 2 | 1 (2.5) | 2 (5) | ||
Perlas A半定量评级:干预组0级24例(60.0%),1级15例(37.5%),2级1例(2.5%);对照组0级25例(62.5%),1级13例(32.5%),2级2例(5%),两组评级构成比差异无统计学意义(P>0.05,表 2)。两组共3例Perlas A半定量分级为2级的患者(干预组1例,对照组2例)均进行干预后未发生反流误吸。
与对照组比较,干预组口渴、饥饿感VAS评分明显降低(P<0.05,表 3)。
表 3.
两组患者禁食水时间及干渴感、饥饿感VAS比较
Comparison of fasting time and thirst VAS and starvation VAS in two groups
| Items | Intervention group (n=40) | Control group (n=40) | Statistical value | P |
| VAS, visual analogue scale. | ||||
| Fasting for clear liquids/h, x±s | 3.1±1.3 | 12.2±1.9 | t=25.553 | < 0.001 |
| Fasting for solids/h, x±s | 14.8±3.6 | 14.7±2.5 | t=-0.127 | 0.900 |
| Thirst VAS, M (min,max) | 2 (2, 2) | 5 (3, 5) | Z=-7.350 | < 0.001 |
| Starvation VAS, M (min,max) | 1 (0, 2) | 3 (3, 3) | Z=-6.920 | < 0.001 |
两组患者术中各观察时点血压、心率比较差异无统计学意义(P>0.05),术中麻黄碱使用率两组比较差异无统计学意义(P>0.05),术后恶心呕吐发生率两组比较差异无统计学意义(P>0.05,表 4)。术后没有患者出现低氧血症。
表 4.
两组患者术中情况及术后不良反应比较
Intraoperative conditions and complications of the two groups
| Items | Intervention group (n=40) | Control group (n=40) | Statistical value | P |
| MAP, mean arterial pressure; HR, heart rate; PONV, post-operative nausea and vomiting. | ||||
| MAP at T0/mmHg, x±s | 89±9 | 92±9 | t=-1.668 | 0.099 |
| HR at T0/(/min), x±s | 77±12 | 73±12 | t=0.580 | 0.564 |
| MAP at T1/mmHg, x±s | 80±12 | 83±9 | t=-1.114 | 0.269 |
| HR at T1/(/min), x±s | 66±12 | 64±10 | t=0.583 | 0.562 |
| MAP at T2/mmHg, x±s | 78±11 | 79±8 | t=-0.739 | 0.462 |
| HR at T2/(/min), x±s | 64±12 | 63±11 | t=0.517 | 0.607 |
| Surgery time/min, x±s | 126±69 | 104±75 | t=1.350 | 0.181 |
| Anesthesia time/min, x±s | 178±79 | 144±86 | t=1.809 | 0.074 |
| Fluid infusion volume/mL, x±s | 1 208±431 | 1 143±237 | t=0.836 | 0.406 |
| Bleeding volume/mL, x±s | 64±40 | 56±31 | t=0.975 | 0.332 |
| The treatment of ephedrine, n (%) | 5 (12.5) | 7 (17.5) | χ2=0.392 | 0.531 |
| The incidence of PONV, n (%) | 7 (17.5) | 8 (20) | χ2=0.082 | 0.775 |
3. 讨论
择期手术前禁食禁饮目的是减少胃内容物容量和酸度,意在预防麻醉期间反流和误吸,确保患者安全。但长时间禁食禁饮导致患者口渴、饥饿和焦虑等不适[15],还可导致患者出现胰岛素抵抗。ERAS协会2012年修订了术前禁食禁饮指南,缩短(尤其是透明液体)禁饮时间[2]。
尽管如此,目前国内很多医院临床上仍沿用传统标准(术前禁食8~12 h,禁饮4 h)[16]。本研究对照组即沿用传统标准,术前一日24:00后禁食禁饮。平均禁食时间14 h、禁饮时间12 h,口渴、饥饿等不适发生率为38. 75%(31/80),与既往研究报道(42/117)基本一致[17]。而干预组平均禁饮时间3 h,口渴、饥饿VAS评分显著下降,患者舒适度和满意度提升。Tsutsumi等[18]提出,与禁食水相比,术前口服碳水化合物患者有更好的术前心理健康状态,可以改善术前饥饿、口渴不适感等,故在安全前提下改善患者术前禁食禁饮现状必要且迫切。
临床上缺乏客观评估麻醉前GV的方法是不敢缩短禁饮时间的主要原因。本研究通过应用胃窦部超声测量CSA, 证明此方法可以用于麻醉前GV评估,两组患者术前CSA、GV、GV/W及Perlas A半定量评级构成比差异无统计学意义,说明缩短禁饮时间妇科腔镜手术患者麻醉前GV及反流误吸风险未见增加,验证了ERAS禁食禁饮方案在妇科腹腔镜手术特殊体位患者中应用的安全性。
既往研究将Perlas A半定量分级为2分或GV/W大于1.5 mL/kg者列为可能导致反流误吸的“危险胃”[13-14]。本研究共发现3例“危险胃”患者(干预组1例,对照组2例),占比为3.75 %,与既往报道采用此类特殊体位手术反流发生率一致[5-8]。由于在全身麻醉诱导前识别出反流误吸高风险患者,采取了预防干预措施(均采用快速序贯诱导气管插管全身麻醉,诱导后置入胃管引流胃液),故所有患者均未发生反流误吸。进一步分析,这3例“危险胃”患者中有2例患者胃管引流出大于100 mL胃液,而这2例患者BMI均大于30。Shiraishi等[19]指出,相较BMI正常的人,肥胖者即使禁食9 h后胃内残余量仍然很高,故推测本研究中这2例患者胃内残余量高可能与肥胖相关,也提示在临床工作中对反流误吸风险高的特殊人群(如糖尿病、肥胖患者等),麻醉诱导前建议使用胃超声评估GV及反流误吸风险,如果GV/W大于1.5 mL/kg、Perlas A半定量分级2分或胃内有固体物质,可提前采取预防措施,包括麻醉前使用H2受体拮抗与胃肠兴奋的复合制剂减少GV及酸度[20];非困难气道患者全身麻醉采用快速序贯诱导方法;置入胃管排空胃液和空气;准备好吸引设备等。一旦发生反流及早处理,把相关并发症风险降到最低以确保手术正常进行。
本研究存在一定局限性,理论上术前口服碳水化合物可减少术中低血压发生率及缩血管药物使用的频度,本研究两组患者术中各观察时点血压、心率及缩血管药物使用频度比较差异无统计学意义,可能与样本量有限相关,术前口服碳水化合物对围术期循环影响尚待进一步研究;另外,研究人群排除了血糖未控制稳定的糖尿病患者和近期服用影响胃肠动力的药物的患者,而这些高危患者可能更有胃超声筛查价值,术前口服碳水化合物对这些特殊患者GV的影响有待进一步观察。
综上所述,本研究通过引入胃窦部超声这种直接客观监测GV的方法,证明妇科腹腔镜手术特殊头低臀高仰卧截石体位患者术前2 h口服300 mL碳水化合物,麻醉前GV未见增加,反流误吸风险未见增加,对患者生理需求的干扰减少,患者舒适度增加。
Funding Statement
北京大学国际医院科研基金(YN2018ZD03)
Supported by Peking University International Hospital Research Grant (YN2018ZD03)
References
- 1.Nelson G, Kiyang LN, Crumley ET, et al. Implementation of enhanced recovery after surgery (eras) across a provincial healthcare system: The ERAS Alberta colorectal surgery experience. World J Surg. 2016;40(5):1092–1103. doi: 10.1007/s00268-016-3472-7. [Nelson G, Kiyang LN, Crumley ET, et al. Implementation of enhanced recovery after surgery (eras) across a provincial healthcare system: The ERAS Alberta colorectal surgery experience[J]. World J Surg, 2016, 40(5): 1092-1103.] [DOI] [PubMed] [Google Scholar]
- 2.Nygren J, Thacker J, Carli F, et al. Guidelines for perioperative care in elective rectal /pelvic surgery: Enhanced recovery after surgery (ERAS) society recommendations. Clin Nutr. 2012;31(6):801–816. doi: 10.1016/j.clnu.2012.08.012. [Nygren J, Thacker J, Carli F, et al. Guidelines for perioperative care in elective rectal /pelvic surgery: Enhanced recovery after surgery (ERAS) society recommendations[J]. Clin Nutr, 2012, 31(6): 801-816.] [DOI] [PubMed] [Google Scholar]
- 3.赵 国胜, 马 晓玲. 妇科腹腔镜手术对生理的影响及麻醉处理. https://www.cnki.com.cn/Article/CJFDTOTAL-ZWZX200712008.htm. 中国误诊学杂志. 2007;7(12):3. [赵国胜, 马晓玲. 妇科腹腔镜手术对生理的影响及麻醉处理[J]. 中国误诊学杂志, 2007, 7(12): 3.] [Google Scholar]
- 4.Park YT, Nogami M, Okano S. Influence of trendelenburg position and pneumoperitoneum treatment on gastroesophageal reflux in dogs. Pol J Vet Sci. 2017;20(4):823–826. doi: 10.1515/pjvs-2017-0104. [Park YT, Nogami M, Okano S. Influence of trendelenburg position and pneumoperitoneum treatment on gastroesophageal reflux in dogs[J]. Pol J Vet Sci, 2017, 20(4): 823-826.] [DOI] [PubMed] [Google Scholar]
- 5.文 亚杰, 吴 昌彬, 林 金坤, et al. 全麻下妇科腹腔镜手术患者胃食管反流的发生喉罩和气管导管通气下的比较. 中华麻醉学杂志. 2005;25(11):814–816. doi: 10.3760/j.issn:0254-1416.2005.11.004. [文亚杰, 吴昌彬, 林金坤, 等. 全麻下妇科腹腔镜手术患者胃食管反流的发生喉罩和气管导管通气下的比较[J]. 中华麻醉学杂志, 2005, 25(11): 814-816.] [DOI] [Google Scholar]
- 6.Roberts CJ, Goodman NW. Gastro-oesophageal reflux during elective laparoscopy. Anaesthesia. 2010;45(12):1009–1011. doi: 10.1111/j.1365-2044.1990.tb14875.x. [Roberts CJ, Goodman NW. Gastro-oesophageal reflux during elective laparoscopy[J]. Anaesthesia, 2010, 45(12): 1009-1011.] [DOI] [PubMed] [Google Scholar]
- 7.孙 晓黎, 李 洁, 王 振元, et al. 引流型喉罩对头低位腹腔镜手术反流误吸的影响. https://www.cnki.com.cn/Article/CJFDTOTAL-LCMZ201308026.htm. 临床麻醉学杂志. 2013;29(8):2. [孙晓黎, 李洁, 王振元, 等. 引流型喉罩对头低位腹腔镜手术反流误吸的影响[J]. 临床麻醉学杂志, 2013, 29(8): 2.] [Google Scholar]
- 8.Ho B, Skinner HJ, Mahajan RP. Gastro-oesophageal reflux during day case gynaecological laparoscopy under positive pressure ventilation: Laryngeal mask vs. tracheal intubation. Anaesthesia. 2015;53(9):921–924. doi: 10.1046/j.1365-2044.1998.00461.x. [Ho B, Skinner HJ, Mahajan RP. Gastro-oesophageal reflux during day case gynaecological laparoscopy under positive pressure ventilation: Laryngeal mask vs. tracheal intubation[J]. Anaesthesia, 2015, 53(9): 921-924.] [DOI] [PubMed] [Google Scholar]
- 9.Bouvet L, Mazoit JX, Chassard D, et al. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume. Anesthesiology. 2011;114(5):1086–1092. doi: 10.1097/ALN.0b013e31820dee48. [Bouvet L, Mazoit JX, Chassard D, et al. Clinical assessment of the ultrasonographic measurement of antral area for estimating preoperative gastric content and volume[J]. Anesthesiology, 2011, 114(5): 1086-1092.] [DOI] [PubMed] [Google Scholar]
- 10.Perlas A, Davis L, Khan M, et al. Gastric sonography in the fasted surgical patient: A prospective descriptive study. Anesth Analg. 2011;113(1):93–97. doi: 10.1213/ANE.0b013e31821b98c0. [Perlas A, Davis L, Khan M, et al. Gastric sonography in the fasted surgical patient: A prospective descriptive study[J]. Anesth Analg, 2011, 113(1): 93-97.] [DOI] [PubMed] [Google Scholar]
- 11.Perlas A, Mitsakakis N, Liu L, et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination. Anesth Analg. 2013;116(2):357–363. doi: 10.1213/ANE.0b013e318274fc19. [Perlas A, Mitsakakis N, Liu L, et al. Validation of a mathematical model for ultrasound assessment of gastric volume by gastroscopic examination[J]. Anesth Analg, 2013, 116(2): 357-363.] [DOI] [PubMed] [Google Scholar]
- 12.中华医学会妇产科学分会加速康复外科协作组 妇科手术加速康复的中国专家共识. https://www.cnki.com.cn/Article/CJFDTOTAL-SDZY202106001.htm. 中华妇产科杂志. 2019;54(2):7. [中华医学会妇产科学分会加速康复外科协作组. 妇科手术加速康复的中国专家共识[J]. 中华妇产科杂志, 2019, 54(2): 7.] [Google Scholar]
- 13.Putte VD, Perlas A. Ultrasound assessment of gastric content and volume. Br J Anaesth. 2014;113(1):12–22. doi: 10.1093/bja/aeu151. [Putte VD, Perlas A. Ultrasound assessment of gastric content and volume[J]. Br J Anaesth, 2014, 113(1): 12-22.] [DOI] [PubMed] [Google Scholar]
- 14.Gola W, Domagala M, Cugowski A. Ultrasound assessment of gastric emptying and the risk of aspiration of gastric contents in the perioperative period. Anaesthesiol Intensive Ther. 2018;50(4):297–302. doi: 10.5603/AIT.a2018.0029. [Gola W, Domagala M, Cugowski A. Ultrasound assessment of gastric emptying and the risk of aspiration of gastric contents in the perioperative period[J]. Anaesthesiol Intensive Ther, 2018, 50(4): 297-302.] [DOI] [PubMed] [Google Scholar]
- 15.Tosun B, Yava A, Acikel C. Evaluating the effects of preoperative fasting and fluid limitation. Int J Nurs Pract. 2014;21(2):156–165. doi: 10.1111/ijn.12239. [Tosun B, Yava A, Acikel C. Evaluating the effects of preoperative fasting and fluid limitation[J]. Int J Nurs Pract, 2014, 21(2): 156-165.] [DOI] [PubMed] [Google Scholar]
- 16.吕 毅. 围术期处理. 北京: 人民卫生出版社; 2018. p. 92. [吕毅. 围术期处理[M]. 北京: 人民卫生出版社, 2018: 92.] [Google Scholar]
- 17.Gustafsson UO, Hausel J, Thorell A, et al. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery. Arch Surg. 2011;146(5):571–577. doi: 10.1001/archsurg.2010.309. [Gustafsson UO, Hausel J, Thorell A, et al. Adherence to the enhanced recovery after surgery protocol and outcomes after colorectal cancer surgery[J]. Arch Surg, 2011, 146(5): 571-577.] [DOI] [PubMed] [Google Scholar]
- 18.Tsutsumi R, Kakuta N, Kadota T, et al. Effects of oral carbohydrate with amino acid solution on the metabolic status of patients in the preoperative period: A randomized, prospective clinical trial. J Anesth. 2016;30(5):842–849. doi: 10.1007/s00540-016-2217-y. [Tsutsumi R, Kakuta N, Kadota T, et al. Effects of oral carbohydrate with amino acid solution on the metabolic status of patients in the preoperative period: A randomized, prospective clinical trial[J]. J Anesth, 2016, 30(5): 842-849.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shiraishi T, Kurosaki D, Nakamura M, et al. Gastric fluid volume change after oral rehydration solution intake in morbidly obese and normal controls: A magnetic resonance imaging-based analysis. Anesth Analg. 2017;124(4):1174–1178. doi: 10.1213/ANE.0000000000001886. [Shiraishi T, Kurosaki D, Nakamura M, et al. Gastric fluid volume change after oral rehydration solution intake in morbidly obese and normal controls: A magnetic resonance imaging-based analysis[J]. Anesth Analg, 2017, 124(4): 1174-1178.] [DOI] [PubMed] [Google Scholar]
- 20.Fawcett WJ, Thomas M. Pre-operative fasting in adults and children: Clinical practice and guidelines. Anaesthesia. 2019;74(1):83–88. doi: 10.1111/anae.14500. [Fawcett WJ, Thomas M. Pre-operative fasting in adults and children: Clinical practice and guidelines[J]. Anaesthesia, 2019, 74(1): 83-88.] [DOI] [PubMed] [Google Scholar]


