Abstract
Incomplete understanding of the multiple mechanisms underlying the link between ultra-processed foods and cardiometabolic health should not be an excuse for inaction argue Mathilde Touvier and colleagues
The effect of diet on health has historically been considered from a nutrient based perspective—for example, excess total fat, saturated fat, dietary cholesterol, calories, sugar, or salt and lack of dietary fibre, vitamins, and minerals.1 More recently, this approach has been complemented by extensive evidence supporting health effects of dietary patterns (eg, the Mediterranean diet), characterised by various dietary scores such as the Alternative Healthy Eating Index (AHEI), or DASH (Dietary Approaches to Stop Hypertension) diet.2 However, the degree of processing and formulation of foods was not taken into account. For instance, all vegetable soups were considered similar, regardless of whether they were homemade, industrial canned, or industrial dehydrated and contained food additives and flavours.
The potential health effect of food processing and food formulation, beyond their food ingredients, nutrient composition, and energy content, is now being widely researched. An important milestone was the 2009 publication of the NOVA classification,3 which categorises foods according to the type, intensity, and purpose of food processing (box 1). The ultra-processed group includes all foods and drinks made using intense physical or chemical processes or containing cosmetic food additives and other industrial ingredients (eg, artificial flavours, hydrogenated oils, glucose/fructose corn syrup).4 These foods are generally convenient, affordable, highly palatable, and often intensively advertised.
Box 1. Nova classification.
Nova 1: Unprocessed or minimally processed foods
Fresh, dried, grounded, chilled, frozen, pasteurised, or fermented staple foods such as fruits, vegetables, pulses, rice, pasta, eggs, meat, fish, or milk
Nova 2: Processed culinary ingredients
Substances usually extracted from foods, not to be consumed by themselves, but for use in preparing staple foods for consumption such as salt, vegetable oils, butter, and sugar
Nova 3: Processed foods
Canned vegetables with added salt, meat and fish products preserved by salting, cheeses and freshly made unpackaged breads, sugar coated dried fruits, and other products manufactured with the addition of salt, sugar, or other group 2 ingredients
Nova 4: Ultra-processed foods
Food that has undergone intense industrial physical, chemical, or biological processes (eg, hydrogenation, moulding, extruding, preprocessing by frying) or that contains industrial substances not usually found in domestic kitchens (eg, maltodextrin, hydrogenated oils, or modified starches), cosmetic additives (eg, dyes, emulsifiers, artificial sweeteners), or flavouring agents. Examples include carbonated soft drinks, chocolate and energy bars, instant noodles, dehydrated soups, fish and chicken nuggets, powdered or “fortified” meals, and meat substitutes containing substances such as protein isolates or additives that modify colour and flavours.
Prospective studies since 2015 have found associations between consumption of ultra-processed food and altered lipoprotein profiles in children5 and increased risks of obesity,6 type 2 diabetes,7 and cardiovascular diseases8 in adults. Over 70 long term prospective epidemiological studies (some of them reviewed elsewhere9) and a handful of short term interventional studies10 11 have also consistently observed that consuming ultra-processed foods is linked with weight gain and increased risk of various diseases, particularly cardiometabolic conditions. It has also been suggested that these foods meet the criteria to be labelled as addictive substances using the standards set for tobacco products.12
Today, the question is: do we have enough evidence to take concrete action from a government policy and public health standpoint? The ultra-processed food category is broad and heterogeneous, encompassing a wide variety of products and ingredients that may have different effects on health. Although evidence is emerging about the mechanisms whereby ultra-processed foods and their components affect human health, much remains to be unravelled. Given the economic interest in the ultra-processed foods market, some big food companies are advocating for no public action in the meantime, including attempts to conflate the benefits of food processing (such as greater shelf stability, microbiological safety, affordability, and attractive functional and taste properties of foods) with ultra-processing, and promoting a view that there is no or only limited consensus about the relation between food processing and human health.13 14 15
However, we believe that the available evidence justifies certain public health measures to reduce population level exposure. These should be implemented in synergy with measures promoting foods and diets that are minimally processed and have favourable food ingredients and nutritional profiles.
The ultra-processed foods epidemic: how countries differ
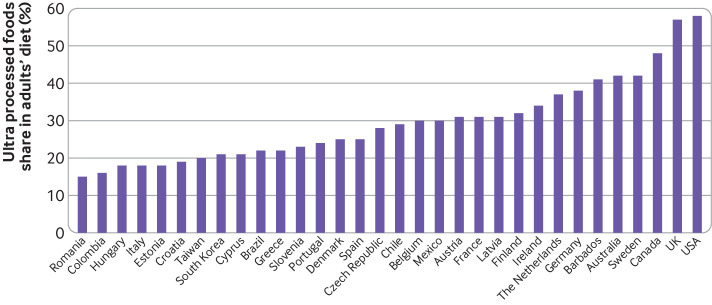
Since the 1990s, sales of ultra-processed foods in most countries have either been increasing (mainly in low and middle income countries) or stayed high. At the same time, data from consumption surveys indicate that the share of ultra-processed foods in diets varies greatly among countries worldwide (fig 1). The highest intake is in the United States (58% of daily energy intake) and the lowest in Colombia (16%).9 16 Intake also varies within Europe, ranging from 15% of total calories consumed by the adult population in Romania to 57% in the UK.17 These variations reflect differences in economic, sociocultural, politico-legal, and commercial factors that structure human behaviour throughout food systems and shape the availably, affordability, desirability, and ultimately consumption of ultra-processed foods.18 Although sales data provide some insights, national surveys of ultra-processed food consumption have not been done in many countries, a key gap for further research.
Fig 1.
Mean proportion of ultra-processed foods in adults’ diet across countries (% energy intake) from nationally representative surveys9 16 17
Evidence on cardiometabolic effects
Several meta-analyses have summarised the accumulating evidence from observational studies linking ultra-processed foods to cardiometabolic health (table 1). Overall, compared with people with low consumption of ultra-processed food, those with the highest consumption have been shown to have higher risks of type 2 diabetes,19 hypertension,21 overweight or obesity,23 cardiovascular and cerebrovascular events,20 26 as well as all-cause22 and cardiovascular25 mortality. Cohort studies have also associated ultra-processed foods with risks of other non-communicable diseases such as several cancers,27 inflammatory bowel disease,28 depression,29 gestational diabetes,30 and chronic kidney disease31 (box 2).
Table 1.
Meta-analyses reporting associations between ultra-processed food consumption and cardiometabolic outcomes*
| Study | Risk increase (highest versus lowest exposure categories) |
|---|---|
| Chen et al (2023)19 | Type 2 diabetes (40% higher risk) |
| Yuan et al (2023)20 | Cardiovascular events (35% higher risk) |
| Wang et al (2022)21 | Hypertension (23% higher risk) |
| Taneri et al (2022)22 | All-cause mortality (29% higher risk) |
| Moradi et al (2021)23 | Abdominal obesity (41% higher risk) Overweight (36% higher risk) Obesity(55% higher risk) |
| Lane et al (2021)24 | Metabolic syndrome (81% higher odds) |
| Suksatan et al (2021)25 | Cardiovascular mortality (50% higher risk) Cardiac mortality (66% higher risk) |
When more than one meta-analysis was available for a given outcome, the most recent and complete (in terms of number of prospective studies included) was selected.
Box 2. Geographical location, and methodological characteristics of prospective studies examining association of ultra-processed foods with health outcomes.
Adults
67 prospective cohort studies have been conducted in adults based on the NOVA classification, 48 (70%) of which included more than 10 000 participants and 17 (25%) more than 100 000 participants. These have shown consistent associations with adverse outcomes, including obesity, dyslipidaemia, hypertension, diabetes, cardiovascular and cerebrovascular diseases, chronic kidney disease, Crohn's disease and ulcerative colitis, depression, and all-cause mortality
Geographical distribution: 34 in Europe, 15 in United States and Canada, 9 in Latin America, 5 in Asia, and 4 in other geographical regions
Primary exposure measure: 43 used the percentage of ultra-processed food in the diet by weight or energy; others used servings or absolute grams per day. Assessment was by food frequency questionnaire (43), 24 hour records or recalls (15), or structured dietary history questionnaire (9)
All studies adjusted for socioeconomic and demographic factors; 57 also adjusted for total energy intake and 42 for dietary content of key nutrients or diet quality indexes
Nearly all studies that explored outcomes beyond obesity also accounted for body mass index (52 out of 58 studies)
Children and pregnant women
Nine studies have evaluated cardiometabolic outcomes in children or adolescents and six in pregnant women
High intake of ultra-processed foods during childhood was associated with higher levels of total and low density lipoprotein cholesterol, as well as adiposity
High intake during pregnancy was associated with increased gestational weight gain and blood glucose levels
Some short term randomised controlled trials examining intermediate health markers provide complementary information. One crossover trial allocated participants to an ultra-processed or unprocessed diet for two weeks each and found that the ultra-processed diet led to increased energy intake and weight gain, while the unprocessed diet resulted in lower energy intake and weight loss.10
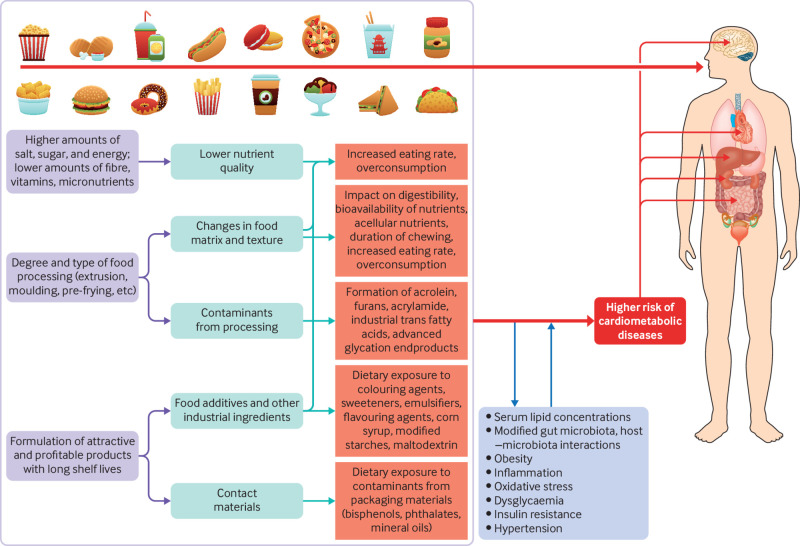
Multifaceted mechanisms beyond nutrient profile
The precise factors associated with disease risk (eg, food ingredients, nutrient profiles, specific additives, contaminants) and their causal mechanisms are not yet fully understood. However, evidence suggests that diets with high and low proportions of ultra-processed foods differ in several aspects that could drive adverse health effects in humans32 (fig 2). Analyses show that the nutrient quality of diets with large amounts of ultra-processed foods are on average poorer, containing more added sugars, refined grains, saturated fat, and sodium, energy density, and less fibre, protein, and micronutrients.16 The food ingredients used in ultra-processed foods are on average of poorer quality, and ultra-processed foods also displace minimally processed, nutritious foods such as fruit, vegetables, legumes, nuts, and seeds from the diet and thereby limit intake of plant based bioactive compounds such as polyphenols.
In addition, food processing can produce potentially toxic compounds such as furans, heterocyclic amines, polycyclic aromatic hydrocarbons, acrolein, advanced glycation end products, industrial trans-fatty acids, and acrylamide. Ultra-processed foods also generally have a long shelf life, which could result in migration of contaminants such as phthalates, bisphenols, mineral oils, and microplastics from contact packaging.9 Studies have suggested that these contaminants may have carcinogenic properties and increase the risk of cardiovascular disease, obesity, insulin resistance, and type 2 diabetes.33 34
The many food additives (eg, sweeteners, colorants, preservatives, thickeners, and emulsifiers) in ultra-processed foods may also have detrimental effects on health, both through single exposures and cocktail effects. Several studies in animal models and in humans35 36 have suggested deleterious health effects for some of the roughly 330 additives currently approved for use in Europe, for instance through gut microbiome dysbiosis,32 inflammation37 and DNA damage.38
Changes to the food matrix during processing may affect satiety, transit time, digestibility, the absorption kinetics and bioavailability of ingested nutrients (such as the glycaemic response),39 as well as partitioning of energy and nutrients between digestion by the host versus the gut microbiota. In particular, the concept of “acellular nutrients” is gaining ground, identifying starches, sugars, and proteins that have been rendered completely devoid of any natural intact food structure. Such nutrients are rapidly digested and absorbed in the mouth, stomach, and small intestine, leaving little nutrition for microbiota bacteria in the large gut.40 This may also contribute to a faster rate of energy intake than with unprocessed foods,41 although the type of energy source (solid foods or beverages) should be considered.10
Ultra-processed foods are also generally aggressively marketed, with attractive packaging that includes animal and cartoon characters, images, and health related claims. Although studies of the effect of packaging and marketing are limited, they may encourage overconsumption.42
Challenges for regulation
Food processing in general is important for many reasons, including for greater shelf stability, energy extraction, microbiological safety, cost, and functional and taste properties. But there is now consistent and deep evidence for health harms from ultra-processed foods. However, challenges to policy change remain.
Classification
Firstly, ultra-processed foods encompass a large and heterogeneous group of products, and foods within this category are likely to have different health effects depending on their characteristics, including their ingredient and nutrient profiles. Some people have therefore argued for more nuance within the category, based on additional scientific inquiry. To support this, one of us (DM) is part of a group that has developed a system that uses artificial intelligence and machine learning to adapt the NOVA categories into a continuous indicator of food processing.43
Defining which foods are ultra-processed and measuring consumption can be challenging.44 45 For instance, in epidemiological studies that use food frequency questionnaires with broad food categories, it may be difficult to determine whether some items are either processed or ultra-processed (eg, cakes, biscuits), leading to classification biases.
Nevertheless, numerous studies around the world show the value of assessing ultra-processed foods as a group, suggesting that it may not be only specific food ingredients and nutrients, but the interplay between all characteristics of ultra-processed foods that affects health.46 Regulation of ultra-processed foods may require more specificity and granularity in the definition, but the value of the category has been demonstrated by numerous studies including tens of thousands of participants and assessing multiple endpoints through a variety of methods.9
While many of these studies were based on less precise dietary assessment tools, increasing the risk for measurement errors, several included a high level of detail (eg, the NutriNet-Santé cohort study, which used repeated 24 hour records including over 3500 generic food items and commercial names7 8) ensuring a high reliability in identifying ultra-processed foods. Several dietary assessment methods specifically designed to assess consumption of ultra-processed foods are currently being developed,47 48 and a recent guide has been published on best practices to apply NOVA in epidemiological studies, including a clear definition of ultra-processed foods and a three step iterative approach to make categorisation more efficient and transparent.49
Effect of individual components
Despite the fact that many cohort studies have adjusted for key nutrients, food groups, or energy density (box 2), some people claim that it remains uncertain whether a more complete adjustment for these factors would modify the findings and are not convinced that ultra-processed foods have an effect beyond their nutrient profile.50 Evidence suggests, however, that nutritional quality contributes but does not entirely explain the observed poor health outcomes.51 Indeed, mechanistic evidence supporting other causal effects is accumulating (fig 2).
Fig 2.
Summary of potential factors and mechanisms linking ultra-processed food consumption with adverse cardiometabolic outcomes
Although many components of ultra-processed foods (eg, artificial sweeteners such as aspartame, or emulsifiers such as carboxymethylcellulose) have been authorised by international and national bodies as safe for consumption at current levels, the assessments were based on focused metrics from industry-led toxicological studies (eg, cytotoxicity, genotoxicity), not metabolic or chronic disease effects in humans. Growing evidence suggests potential harms of several of these additives in humans, as well as potential “cocktail” effects of multi-additive mixtures and effects on the gut microbiota.35 52 53 54 55
This calls for an urgent re-evaluation of multiple common additives. Nanoparticulate titanium dioxide is an emblematic example. It was authorised and used as an additive for years because it had passed the initial cytotoxicity and genotoxicity tests, but new research exploring its effect on the intestinal microbiota and role in colon carcinogenesis54 led Europe to reverse its conclusions and suspend use of titanium dioxide in food. Industrial trans fats provide another sobering example,56 as well as the growing literature around harms of artificial and “natural” zero and low calorie sweeteners.57 58Future research in this field is critical to help identify key characteristics and compounds of ultra-processed foods that drive their deleterious effects and it is industry’s responsibility to address them, while retaining, as appropriate, the other benefits of food processing for cost, convenience, stability, etc.
Confounding
As for all observational evidence, a degree of residual confounding may be present and partly explains the observed associations with adverse health outcomes. People who eat large amounts of ultra-processed foods may have less healthy lifestyles, including other dietary factors, physical activity, and alcohol or tobacco use, and may also be disadvantaged from being in lower socioeconomic groups. However, the consistency of findings across numerous epidemiological studies in different nations and populations that carefully controlled for dietary, lifestyle, sociodemographic, and economic factors makes it unlikely that residual confounding fully explains all of the observed associations.
Although randomised trials have been small and short term, they have also shown harms of ultra-processed foods, including weight gain, metabolic perturbations, and changes in the gut microbiota (for some additives emblematic of ultra-processed foods).52 53 Long term clinical trials of dietary interventions are not always feasible or ethical, especially when deleterious effects are expected. Triangulation of multiple study designs has previously been used to show causality59 by combining well conducted large scale observational and mechanistic epidemiological studies on long term health outcomes with short term trials studying intermediate metabolic endpoints and with in vivo and in vitro experimental studies.
Appropriate food systems policies
Given the evidence from experimental and epidemiological studies on the harms of ultra-processed foods, it is time for government, public health, and industry actions to reduce exposure to such processed foods, as well as major investment in research to better elucidate the factors and causal mechanisms involved.
Information and education to allow consumers to identify and limit their consumption of ultra-processed foods is needed. National and international bodies should convene expert groups to generate an operational definition of ultra-processed foods for regulatory purposes—for example, derived from NOVA and specifying a list of processes and ingredients that define ultra-processed foods. Independent academic experts and public health authorities should be involved in this process, through collective expertise. Input from industry can be solicited but should not be binding, and final decisions should be taken without industry involvement or commercial conflicts of interest. The operational definition should then be used for food labelling to facilitate consumer identification of ultra-processed foods in supermarket shelves and online retailing.
Several countries in Latin America already place a warning label on food packaging to help consumers flag ultra-processed foods.60 Various front of pack nutritional labels are used in Europe, with seven using the Nutri-score system. A randomised trial (by a group including BS and MT) found that use of a modified Nutri-score label that included an ultra-processed mark (fig 3) increased objective understanding of the overall nutrient profile and ultra-processing dimension of foods, with downstream effects on purchasing intentions and perceptions of product healthfulness.61 The same group is currently working on scenarios for integration of food processing into the calculation of the Nutri-Score algorithm itself. In the US, a group led by DM has proposed Food Compass as a food rating system combining the food processing classification synergistically with ingredient and nutrient information.62 63
Fig 3.
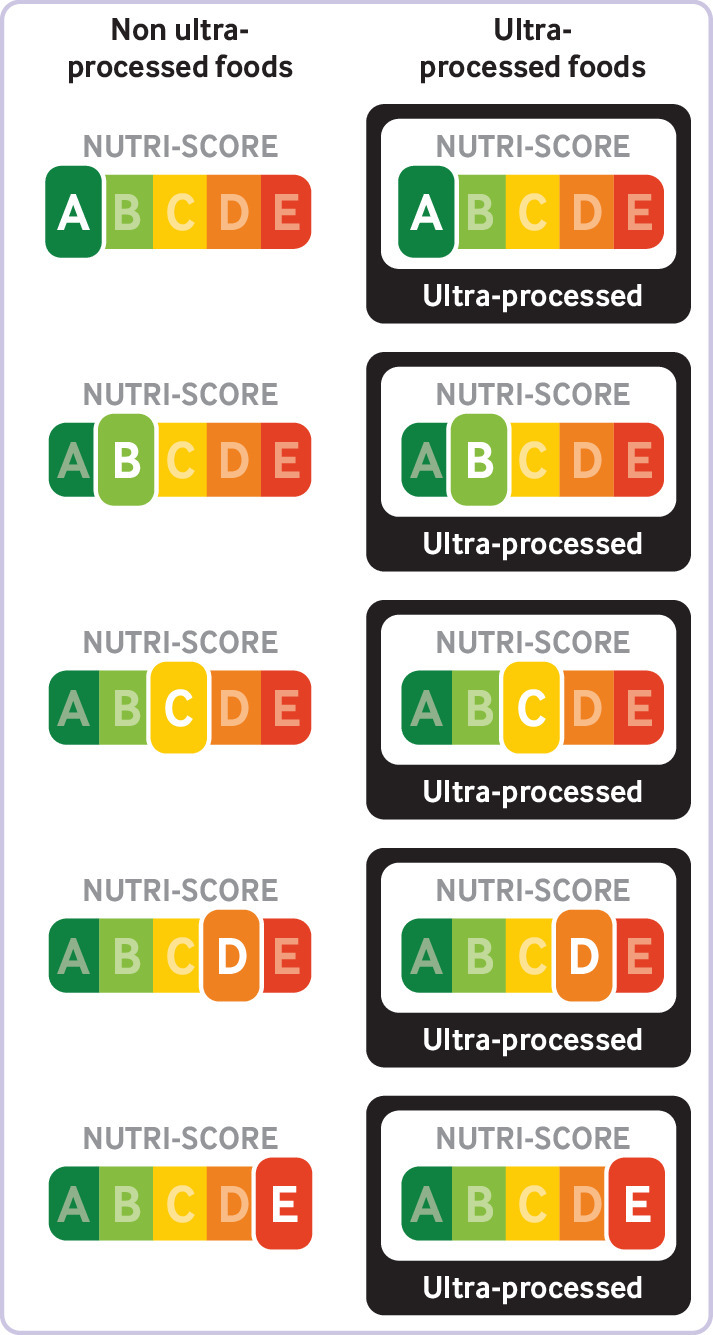
Front-of-pack Nutri-score label adapted to provide information on ultra-processed food
The practical application of these systems as public health tools is a priority for investigation and implementation. In addition to food labelling, national scientific bodies responsible for official dietary guidance should evaluate the evidence for recommendations to limit ultra-processed foods and favour unprocessed or minimally processed foods. These measures will facilitate, at the consumer level, a lowering of ultra-processed food intake by empowering people with better information, further supplemented with food profiling applications (based on barcode scanning, such as Open Food Facts ( https://world.openfoodfacts.org/)) and communication campaigns.
In parallel with consumer education, there is a need to change the environment in which people live and the food supply to which they have access to limit exposure to ultra-processed foods and support informed decision making, free from misleading marketing. This requires policy measures that work ecologically throughout food systems, including through the use of law and regulation, to reduce exposure to ultra-processed foods marketing, protect schools and other learning environments, influence government and employer food procurement policies, and introduce fiscal interventions that target deeper structural and commercial drivers of production, distribution, and promotion of ultra-processed foods.60 64 New government and international policies, standards, and investments are also needed for re-evaluating the public health risks of industrial food additives. Critically, all such decisions should be made free from commercial conflicts of interests.60 65
The food industry is essential to ensure a safe and sufficient food supply, and for providing diets rich in minimally processed or appropriately processed foods. However, the business operating models and financial incentives driving many of today’s largest food corporations and their upstream and downstream supply chains is pushing non-nutritious ultra-processed foods onto consumers using intense, targeted, and highly effective marketing strategies.66 By funding nutrition research and government lobbying, these companies often influence dietary recommendations and food policies, and avoid regulation.67 68
A shift in focus onto the whole food system rather than specific ultra-processed foods is needed. Importantly, regulations and policies that encourage the production of better and less processed foods, increase the availability, accessibility, and affordability of nutritious minimally processed foods, and restrict the ability to market ultra-processed foods are critical to change the current food supply and food environment. Thus, government policies are needed to reward food sector innovations, from farms and manufacturers to retail outlets and restaurants, that replace ultra-processed foods with minimally processed foods.69 Evidence is emerging that the affordability and availability of nutritious, mostly unprocessed or minimally processed, as well as some processed, foods can be increased to be comparable to or even better than ultra-processed foods (box 3).
Box 3. Are minimally processed diets achievable and affordable?
Cost per calorie of ultra-processed food products is often low, and consumption of some ultra-processed foods such as sugary drinks are consistently higher in disadvantaged socioeconomic classes in many countries.70 However, the socioeconomic profiles of consumers of ultra-processed food differ across countries, and ultra-processed diets are not necessarily cheaper than minimally processed ones. A study based on the data of the Brazilian Household Budget Survey from around 56 000 households found that, regardless of income, diet cost decreased when households better followed national dietary guidance, which included advice on limiting ultra-processed foods.71
Achieving healthy and sustainable diets with minimal amounts of ultra-processed foods at reasonable costs can be difficult currently in some countries where they are ubiquitous. Some countries (Brazil, Ecuador, Peru, Uruguay, Chile, Mexico, France, Belgium, Cataluña, Israel, Malaysia, Zambia, Sri Lanka, Canada) have officially started to promote healthy and affordable non-ultra-processed diets in their official food policies, and provide concrete tools and examples to help citizens in their daily life. For example, the French MangerBouger website proposes weekly ideas of recipes to foster the preparation and consumption of non-to-minimally processed seasonal healthy foods adapted to all budgets and time constraints
The success of other public health measures such as the sugary drink tax in Mexico72 and front-of- package labelling in France shifting consumption from unhealthy to healthy foods,73 suggest similar levers could be used to reduce consumption of ultra-processed foods.
Moving forward
Ultra-processed foods are endemic in our modern societies, making it difficult for many people to shift towards less processed diets within the current food systems. This is especially true for underserved communities where nutritious minimally processed foods are commonly less available, accessible, and affordable.74 Although some ultra-processed foods have proved valuable in meeting the needs of targeted populations (eg, infant formula, clinical oral nutritional supplements), countries of all income levels have shown it is feasible to have a national diet structure with low levels of ultra-processed foods (fig 1).
Scientific efforts must be accelerated through publicly funded research, independent from the food industry, to better identify the specific processes and substances (additives, other industrial ingredients, contaminants from processing or packaging) that contribute to the adverse cardiometabolic effects of ultra-processed foods. Multidisciplinary collaboration is key to success, with approaches combining epidemiology, data science, high quality dietary data collection, toxicology, experimental and interventional research, food technology, as well as public policy, food systems, and social marketing research. Results from this research can guide manufacturers towards innovative, technologically relevant, yet safe and sustainable processes and substances, towards more optimal food processing (but not “ultra-processing”) for health.
Food processing, including at the industrial scale, has enabled humans for millennia to produce safer, more nutritious, and palatable foods. It is essential to healthy and sustainable food systems, and to food security. However, the rise of ultra-processing is leading to serious health harms. It is time to inform consumers about adverse effects of ultra-processed foods consumption and to urge governments to take ambitious and decisive structural measures to enable healthy, less processed foods to be the easiest choice. Everyone’s health is at stake.
Key messages.
Mounting evidence from epidemiological studies links consumption of ultra-processed food to poorer cardiometabolic health
Factors at play (eg, food ingredient profiles, additive mixtures, process or packaging related contaminants) and causal mechanisms are not yet fully understood, but evidence is accumulating beyond nutrient related pathways
Existing evidence is sufficiently strong to warrant immediate public health actions to help citizens identify ultra-processed foods and limit their exposure
Multidisciplinary research, independent of industry, is needed to re-evaluate the safety of food additives and industrially processed ingredients as well as process related contaminants
Fiscal, marketing, and labelling regulations should be used to transform the current food system and facilitate a dietary shift away from ultra-processed foods throughout the population
Contributors and sources: MT and BS are experts in nutritional epidemiology and investigators of the NutriNet-Santé cohort in France, on which large scale studies on food processing and health were based; MLL is a nutritional epidemiologist who has collaborated in many studies evaluating the consumption of ultra-processed foods and its impact on health; DM is a cardiologist and nutrition scientist; PB is an expert in sustainable food systems, nutrition, and public health; and FJ is nutritional epidemiologist. MT and BS drafted the initial version of the manuscript. MLL, DM, PB, and FJ critically reviewed the manuscript and contributed substantially to the writing and revision of the article. All authors approved the final version. MT is the guarantor.
Competing interests: We have read and understood BMJ policy on declaration of interests and have no interests to declare.
Provenance and peer review: Commissioned; externally peer reviewed.
This article is part of a collection proposed by Swiss Re, which also provided funding for the collection, including open access fees. The BMJ commissioned, peer reviewed, edited, and made the decision to publish. Nita Forouhi, Dariush Mozaffarian, and David Ludwig provided advice and guided the selection of topics. The lead editors for the collection were Navjoyt Ladher, Rachael Hinton, and Emma Veitch.
References
- 1. Mozaffarian D, Rosenberg I, Uauy R. History of modern nutrition science-implications for current research, dietary guidelines, and food policy. BMJ 2018;361:k2392. 10.1136/bmj.k2392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Schulze MB, Martínez-González MA, Fung TT, Lichtenstein AH, Forouhi NG. Food based dietary patterns and chronic disease prevention. BMJ 2018;361:k2396. 10.1136/bmj.k2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Monteiro CA. Nutrition and health. The issue is not food, nor nutrients, so much as processing. Public Health Nutr 2009;12:729-31. 10.1017/S1368980009005291. [DOI] [PubMed] [Google Scholar]
- 4.Monteiro CA, Cannon G, Lawrence M, da Costa Louzada ML, Pereira Machado P. Ultra-processed foods, diet quality, and health using the NOVA classification system. 2019. https://www.fao.org/3/ca5644en/ca5644en.pdf
- 5. Rauber F, Campagnolo PD, Hoffman DJ, Vitolo MR. Consumption of ultra-processed food products and its effects on children’s lipid profiles: a longitudinal study. Nutr Metab Cardiovasc Dis 2015;25:116-22. 10.1016/j.numecd.2014.08.001. [DOI] [PubMed] [Google Scholar]
- 6. Mendonça RD, Pimenta AM, Gea A, et al. Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. Am J Clin Nutr 2016;104:1433-40. 10.3945/ajcn.116.135004. [DOI] [PubMed] [Google Scholar]
- 7. Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultraprocessed food consumption and risk of type 2 diabetes among participants of the NutriNet-Santé prospective cohort. JAMA Intern Med 2020;180:283-91. 10.1001/jamainternmed.2019.5942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultra-processed food intake and risk of cardiovascular disease: prospective cohort study (NutriNet-Santé). BMJ 2019;365:l1451. 10.1136/bmj.l1451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Srour B, Kordahi MC, Bonazzi E, Deschasaux-Tanguy M, Touvier M, Chassaing B. Ultra-processed foods and human health: from epidemiological evidence to mechanistic insights. Lancet Gastroenterol Hepatol 2022;7:1128-40. 10.1016/S2468-1253(22)00169-8. [DOI] [PubMed] [Google Scholar]
- 10. Hall KD, Ayuketah A, Brychta R, et al. Ultra-processed diets cause excess calorie intake and weight gain: an inpatient randomized controlled trial of ad libitum food intake. Cell Metab 2019;30:67-77.e3. 10.1016/j.cmet.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Sartorelli DS, Crivellenti LC, Baroni NF, et al. Effectiveness of a minimally processed food-based nutritional counselling intervention on weight gain in overweight pregnant women: a randomized controlled trial. Eur J Nutr 2023;62:443-54. 10.1007/s00394-022-02995-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Gearhardt AN, DiFeliceantonio AG. Highly processed foods can be considered addictive substances based on established scientific criteria. Addiction 2023;118:589-98. 10.1111/add.16065. [DOI] [PubMed] [Google Scholar]
- 13. Capozzi F, Magkos F, Fava F, et al. A multidisciplinary perspective of ultra-processed foods and associated food processing technologies: a view of the sustainable road ahead. Nutrients 2021;13:3948. 10.3390/nu13113948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Food Drink Europe. Position paper: scientific critique of ‘ultra-processed foods’ classifications. 2023. https://www.fooddrinkeurope.eu/wp-content/uploads/2023/01/FoodDrinkEurope-position-paper-ultra-processed-foods.pdf
- 15. Monteiro CA, Jaime PC. Brazilian food guide attacked. Now, overwhelming support for the guide in Brazil and worldwide. World Nutrition 2020;11:94-9. 10.26596/wn.202011494-99. [DOI] [Google Scholar]
- 16. Martini D, Godos J, Bonaccio M, Vitaglione P, Grosso G. Ultra-processed foods and nutritional dietary profile: a meta-analysis of nationally representative samples. Nutrients 2021;13:3390. 10.3390/nu13103390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Mertens E, Colizzi C, Peñalvo JL. Ultra-processed food consumption in adults across Europe. Eur J Nutr 2022;61:1521-39. 10.1007/s00394-021-02733-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Baker P, Machado P, Santos T, et al. Ultra-processed foods and the nutrition transition: Global, regional and national trends, food systems transformations and political economy drivers. Obes Rev 2020;21:e13126. 10.1111/obr.13126. https://onlinelibrary.wiley.com/doi/10.1111/obr.13126. [DOI] [PubMed] [Google Scholar]
- 19. Chen Z, Khandpur N, Desjardins C, et al. Ultra-processed food consumption and risk of type 2 diabetes: three large prospective U.S cohort studies. Diabetes Care 2023;46:1335-44. 10.2337/dc22-1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Yuan L, Hu H, Li T, et al. Dose-response meta-analysis of ultra-processed food with the risk of cardiovascular events and all-cause mortality: evidence from prospective cohort studies. Food Funct 2023;14:2586-96. 10.1039/D2FO02628G. [DOI] [PubMed] [Google Scholar]
- 21. Wang M, Du X, Huang W, Xu Y. Ultra-processed foods consumption increases the risk of hypertension in adults: a systematic review and meta-analysis. Am J Hypertens 2022;35:892-901. 10.1093/ajh/hpac069. [DOI] [PubMed] [Google Scholar]
- 22. Taneri PE, Wehrli F, Roa-Díaz ZM, et al. Association between ultra-processed food intake and all-cause mortality: a systematic review and meta-analysis. Am J Epidemiol 2022;191:1323-35. 10.1093/aje/kwac039. [DOI] [PubMed] [Google Scholar]
- 23. Moradi S, Entezari MH, Mohammadi H, et al. Ultra-processed food consumption and adult obesity risk: a systematic review and dose-response meta-analysis. Crit Rev Food Sci Nutr 2023;63:249-60. 10.1080/10408398.2021.1946005 [DOI] [PubMed] [Google Scholar]
- 24. Lane MM, Davis JA, Beattie S, et al. Ultraprocessed food and chronic noncommunicable diseases: A systematic review and meta-analysis of 43 observational studies. Obes Rev 2021;22:e13146. 10.1111/obr.13146 [DOI] [PubMed] [Google Scholar]
- 25. Suksatan W, Moradi S, Naeini F, et al. Ultra-processed food consumption and adult mortality risk: a systematic review and dose-response meta-analysis of 207,291 participants. Nutrients 2021;14:174. 10.3390/nu14010174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Pagliai G, Dinu M, Madarena MP, Bonaccio M, Iacoviello L, Sofi F. Consumption of ultra-processed foods and health status: a systematic review and meta-analysis. Br J Nutr 2021;125:308-18. 10.1017/S0007114520002688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kliemann N, Rauber F, Bertazzi Levy R, et al. Food processing and cancer risk in Europe: results from the prospective EPIC cohort study. Lancet Planet Health 2023;7:e219-32. 10.1016/S2542-5196(23)00021-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Narula N, Chang NH, Mohammad D, Wong ECL, Ananthakrishnan AN, Chan SSM, et al. Food processing and risk of inflammatory bowel disease: a systematic review and meta-analysis. Clin Gastroenterol Hepatol 2023;S1542-3565(23)00071-X [DOI] [PubMed]
- 29. Gómez-Donoso C, Sánchez-Villegas A, Martínez-González MA, et al. Ultra-processed food consumption and the incidence of depression in a Mediterranean cohort: the SUN Project. Eur J Nutr 2020;59:1093-103. 10.1007/s00394-019-01970-1. [DOI] [PubMed] [Google Scholar]
- 30. Leone A, Martínez-González MÁ, Craig W, Fresán U, Gómez-Donoso C, Bes-Rastrollo M. Pre-gestational consumption of ultra-processed foods and risk of gestational diabetes in a Mediterranean cohort. The SUN Project. Nutrients 2021;13:2202. 10.3390/nu13072202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Du S, Kim H, Crews DC, White K, Rebholz CM. Association between ultraprocessed food consumption and risk of incident CKD: a prospective cohort study. Am J Kidney Dis 2022;80:589-598.e1. 10.1053/j.ajkd.2022.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Juul F, Vaidean G, Parekh N. Ultra-processed foods and cardiovascular diseases: potential mechanisms of action. Adv Nutr 2021;12:1673-80. 10.1093/advances/nmab049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vafeiadi M, Myridakis A, Roumeliotaki T, et al. Association of early life exposure to phthalates with obesity and cardiometabolic traits in childhood: sex specific associations. Front Public Health 2018;6:327. 10.3389/fpubh.2018.00327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhang Y, Huang M, Zhuang P, et al. Exposure to acrylamide and the risk of cardiovascular diseases in the National Health and Nutrition Examination Survey 2003-2006. Environ Int 2018;117:154-63. 10.1016/j.envint.2018.04.047. [DOI] [PubMed] [Google Scholar]
- 35. Debras C, Chazelas E, Sellem L, et al. Artificial sweeteners and risk of cardiovascular diseases: results from the prospective NutriNet-Santé cohort. BMJ 2022;378:e071204. 10.1136/bmj-2022-071204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Srour B, Chazelas E, Fezeu LK, et al. Nitrites, nitrates, and cardiovascular outcomes: are we living “la vie en rose” with pink processed meats? J Am Heart Assoc 2022;11:e027627. 10.1161/JAHA.122.027627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Basson AR, Rodriguez-Palacios A, Cominelli F. Artificial sweeteners: history and new concepts on inflammation. Front Nutr 2021;8:746247. 10.3389/fnut.2021.746247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Alleva R, Borghi B, Santarelli L, et al. In vitro effect of aspartame in angiogenesis induction. Toxicol In Vitro 2011;25:286-93. 10.1016/j.tiv.2010.09.002. [DOI] [PubMed] [Google Scholar]
- 39. Fardet A. Minimally processed foods are more satiating and less hyperglycemic than ultra-processed foods: a preliminary study with 98 ready-to-eat foods. Food Funct 2016;7:2338-46. 10.1039/C6FO00107F. [DOI] [PubMed] [Google Scholar]
- 40. Spreadbury I. Comparison with ancestral diets suggests dense acellular carbohydrates promote an inflammatory microbiota, and may be the primary dietary cause of leptin resistance and obesity. Diabetes Metab Syndr Obes 2012;5:175-89. 10.2147/DMSO.S33473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Forde CG, Mars M, de Graaf K. Ultra-processing or oral processing? A role for energy density and eating rate in moderating energy intake from processed foods. Curr Dev Nutr 2020;4:a019. 10.1093/cdn/nzaa019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Adams J, Hofman K, Moubarac JC, Thow AM. Public health response to ultra-processed food and drinks. BMJ 2020;369:m2391. 10.1136/bmj.m2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Menichetti G, Ravandi B, Mozaffarian D, Barabási AL. Machine learning prediction of the degree of food processing. Nat Commun 2023;14:2312. 10.1038/s41467-023-37457-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Astrup A, Monteiro CA. Does the concept of “ultra-processed foods” help inform dietary guidelines, beyond conventional classification systems? NO. Am J Clin Nutr 2022;116:1482-8. 10.1093/ajcn/nqac123. [DOI] [PubMed] [Google Scholar]
- 45. Braesco V, Souchon I, Sauvant P, et al. Ultra-processed foods: how functional is the NOVA system? Eur J Clin Nutr 2022;76:1245-53. 10.1038/s41430-022-01099-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Monteiro CA, Astrup A. Does the concept of “ultra-processed foods” help inform dietary guidelines, beyond conventional classification systems? YES. Am J Clin Nutr 2022;116:1476-81. 10.1093/ajcn/nqac122. [DOI] [PubMed] [Google Scholar]
- 47. Martinez-Perez C, Daimiel L, Climent-Mainar C, et al. Integrative development of a short screening questionnaire of highly processed food consumption (sQ-HPF). Int J Behav Nutr Phys Act 2022;19:6. 10.1186/s12966-021-01240-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Sarbagili-Shabat C, Zelber-Sagi S, Fliss Isakov N, Ron Y, Hirsch A, Maharshak N. Development and validation of processed foods questionnaire (PFQ) in adult inflammatory bowel diseases patients. Eur J Clin Nutr 2020;74:1653-60. 10.1038/s41430-020-0632-5. [DOI] [PubMed] [Google Scholar]
- 49. Martinez-Steele E, Khandpur N, Batis C, et al. Best practices for applying the Nova food classification system. Nat Food 2023;4:445-8. 10.1038/s43016-023-00779-w. [DOI] [PubMed] [Google Scholar]
- 50. Valicente VM, Peng CH, Pacheco KN, et al. Ultraprocessed foods and obesity risk: a critical review of reported mechanisms. Adv Nutr 2023;14:718-38. 10.1016/j.advnut.2023.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Dicken SJ, Batterham RL. The role of diet quality in mediating the association between ultra-processed food intake, obesity and health-related outcomes: a review of prospective cohort studies. Nutrients 2021;14:23. 10.3390/nu14010023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Chassaing B, Compher C, Bonhomme B, et al. Randomized controlled-feeding study of dietary emulsifier carboxymethylcellulose reveals detrimental impacts on the gut microbiota and metabolome. Gastroenterology 2022;162:743-56. 10.1053/j.gastro.2021.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Suez J, Cohen Y, Valdés-Mas R, et al. Personalized microbiome-driven effects of non-nutritive sweeteners on human glucose tolerance. Cell 2022;185:3307-3328.e19. 10.1016/j.cell.2022.07.016. [DOI] [PubMed] [Google Scholar]
- 54. Bettini S, Boutet-Robinet E, Cartier C, et al. Food-grade TiO2 impairs intestinal and systemic immune homeostasis, initiates preneoplastic lesions and promotes aberrant crypt development in the rat colon. Sci Rep 2017;7:40373. 10.1038/srep40373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Srour B, Chazelas E, Druesne-Pecollo N, et al. Dietary exposure to nitrites and nitrates in association with type 2 diabetes risk: Results from the NutriNet-Santé population-based cohort study. PLoS Med 2023;20:e1004149. 10.1371/journal.pmed.1004149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Wendeu-Foyet G, Bellicha A, Chajès V, et al. Different types of industry-produced and ruminant trans fatty acid intake and risk of type 2 diabetes: findings from the NutriNet-Santé prospective cohort. Diabetes Care 2023;46:321-30. 10.2337/dc22-0900. [DOI] [PubMed] [Google Scholar]
- 57.WHO. Health effects of the use of non-sugar sweeteners: a systematic review and meta-analysis. 2022. https://www.who.int/publications/i/item/9789240046429
- 58. Riboli E, Beland FA, Lachenmeier DW, et al. Carcinogenicity of aspartame, methyleugenol, and isoeugenol. Lancet Oncol 2023;24:848-50. 10.1016/S1470-2045(23)00341-8 [DOI] [PubMed] [Google Scholar]
- 59. Samet JM, Chiu WA, Cogliano V, et al. The IARC Monographs. Updated procedures for modern and transparent evidence synthesis in cancer hazard identification. J Natl Cancer Inst 2020;112:30-7. 10.1093/jnci/djz169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Popkin BM, Barquera S, Corvalan C, et al. Towards unified and impactful policies to reduce ultra-processed food consumption and promote healthier eating. Lancet Diabetes Endocrinol 2021;9:462-70. 10.1016/S2213-8587(21)00078-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Srour B, Hercberg S, Galan P, et al. Effect of a new graphically modified Nutri-Score on the objective understanding of foods’ nutrient profile and ultraprocessing: a randomised controlled trial. BMJ Nutr Prev Health 2023;6:108-18. 10.1136/bmjnph-2022-000599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Mozaffarian D, El-Abbadi NH, O’Hearn M, et al. Food Compass is a nutrient profiling system using expanded characteristics for assessing healthfulness of foods. Nat Food 2021;2:809-18. 10.1038/s43016-021-00381-y. [DOI] [PubMed] [Google Scholar]
- 63. O’Hearn M, Erndt-Marino J, Gerber S, et al. Validation of Food Compass with a healthy diet, cardiometabolic health, and mortality among U.S. adults, 1999-2018. Nat Commun 2022;13:7066. 10.1038/s41467-022-34195-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Northcott T, Lawrence M, Parker C, Baker P. Ecological regulation for healthy and sustainable food systems: responding to the global rise of ultra-processed foods. Agric Hum Values 2023 https://link.springer.com/10.1007/s10460-022-10412-4
- 65. Gilmore AB, Fabbri A, Baum F, et al. Defining and conceptualising the commercial determinants of health. Lancet 2023;401:1194-213. 10.1016/S0140-6736(23)00013-2. [DOI] [PubMed] [Google Scholar]
- 66. Swinburn BA, Kraak VI, Allender S, et al. The global syndemic of obesity, undernutrition, and climate change: the Lancet Commission report. Lancet 2019;393:791-846. 10.1016/S0140-6736(18)32822-8. [DOI] [PubMed] [Google Scholar]
- 67. Chartres N, Fabbri A, Bero LA. Association of industry sponsorship with outcomes of nutrition studies: a systematic review and meta-analysis. JAMA Intern Med 2016;176:1769-77. 10.1001/jamainternmed.2016.6721. [DOI] [PubMed] [Google Scholar]
- 68. Monteiro CA, Lawrence M, Millett C, et al. The need to reshape global food processing: a call to the United Nations Food Systems Summit. BMJ Glob Health 2021;6:e006885. 10.1136/bmjgh-2021-006885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Task Force on Hunger, Nutrition, and Health. Ambitious, actionable recommendations to end hunger, advance nutrition, and improve health in the United States. 2022. https://informingwhc.org/2022-task-force-report/
- 70. Chatelan A, Rouche M, Kelly C, et al. Tax on sugary drinks and trends in daily soda consumption by family affluence: an international repeated cross-sectional survey among European adolescents. Am J Clin Nutr 2023;117:576-85. 10.1016/j.ajcnut.2023.01.011. [DOI] [PubMed] [Google Scholar]
- 71. Maia EG, Passos CMD, Granado FS, Levy RB, Claro RM. Replacing ultra-processed foods with fresh foods to meet the dietary recomendations: a matter of cost? Cad Saude Publica 2022;37(Suppl 1):e00107220. 10.1590/0102-311x00107220. [DOI] [PubMed] [Google Scholar]
- 72.World Health Organization. Tackling NCDs: ‘best buys’ and other recommended interventions for the prevention and control of noncommunicable diseases. 2017. https://apps.who.int/iris/handle/10665/259232
- 73.EU Scientists and Health Professionals for Nutri-Score. Why the European commission must choose the Nutri-Score nutritional label – a public health tool based on rigorous scientific evidence – as the mandatory nutrition label for Europe. 2023; https://nutriscore-europe.com/wp-content/uploads/2023/01/NS_rapport-EU-V10_230202.pdf
- 74.Herforth A, Bai Y, Venkat A, Mahrt K, Ebel A, Masters W. Cost and affordability of healthy diets across and within countries. FAO, 2020. https://www.fao.org/documents/card/en/c/cb2431en