Summary
Increasing awareness of health disparities has led to proposals for a pay-for-equity scheme. Implementing such proposals requires systematic methods of collecting and reporting health outcomes for targeted demographics over time. This lays the foundation for a shift from quality improvement projects (QIPs) to equality improvement projects (EQIPs) that could evaluate adherence to standards and progress toward health equity.
We performed a scoping review on EQIPs to inform a new framework for quality improvement through a health equity lens. Forty studies implemented an intervention after identifying a disparity compared to 149 others which merely identified group differences. Most evaluated race-based differences and were conducted at the institutional level, with representation in both the inpatient and outpatient settings.
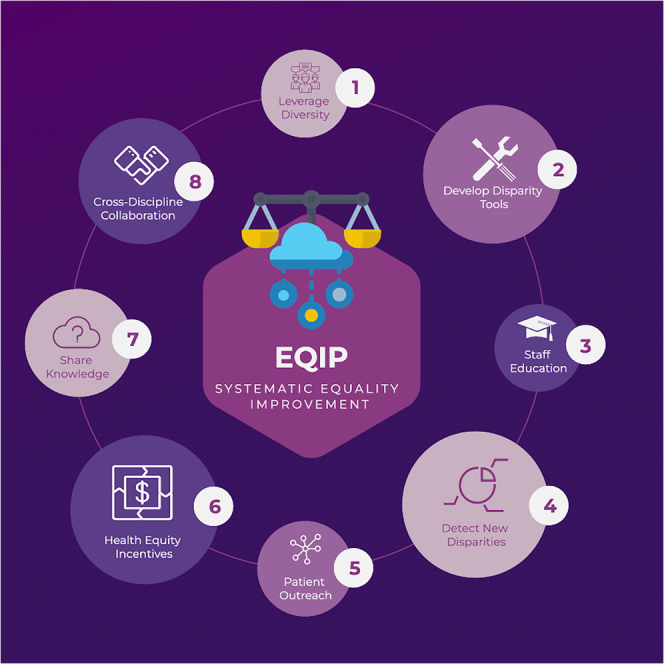
EQIPs that improved equity leveraged multidisciplinary expertise, healthcare staff education, and developed tools to track health outcomes continuously. EQIPs can help bridge the inequality gap and form part of an incentivized systematic equality improvement framework.
Subject areas: Medical science, Medical ethics, Sociology
Graphical abstract
Medical science; Medical ethics; Sociology
From quality improvement to equality improvement projects
Traditional quality improvement projects (QIPs) are a foundational component of healthcare organizations and differ from pure audits significantly (Box 1). They audit the performance of the local clinical practice and evaluate adherence to relevant guidelines, thus offering an essential window into where clinical care is underperforming. It is increasingly recognized that the current health system is failing in one specific aspect, differences in outcomes among demographic groups.1 Health disparities are increasingly reported in the literature, covering many domains and countries where minorities often disproportionately suffer from poorer care and worse overall outcomes.
Box 1. Key Definitions.
| Term | Definition |
|---|---|
| Equality | Equality refers to the state of being equal, especially in status, rights, and opportunities. In a broader context, it is the principle that every individual should have an equal opportunity to make the most of their lives and talents, and that no one should have poorer life chances due to their background or status. |
| Equity | Equity refers to the concept of fairness and justice in economic, political, and social contexts. Unlike equality, which promotes equal treatment for all, equity emphasizes providing resources and opportunities based on individual needs or circumstances to achieve an equal outcome. |
| Quality Metrics | These are metrics shared publicly or reported to government agencies to facilitate comparisons between different organizations. Quality metrics may or may not be associated with quality improvement projects. |
| Audit | An audit is a systematic review or examination of records, operations, processes, or other elements to ensure compliance with established standards, regulations, or laws. |
| Health Equity Audits | These audits are focused on gathering information regarding adherence to guidelines across various groups |
| QIP | These projects utilize rapid cycle improvement efforts, such as PDSA (Plan-Do-Study-Act) cycles, to enhance the quality of services. Typically, this is an internal process and is not disclosed to the public. |
| EQIP | EQIP refers to a systematic evaluation of outcomes across subgroups in response to different interventions. This method is intended to assess the efficiency and effectiveness of interventions across diverse population subgroups. |
QIP: Quality Improvement Projects, EQIP: Equity Quality Improvement Project
The Biden administration has placed health equity at the forefront of its plans for reforming the US health system.2 Recently, the Centers for Medicare and Medicaid (CMS) issued a new initiative that takes a significant step toward tying payments with health equity.3 This proposal focuses on collecting existing core metrics to identify disparities and developing the infrastructure capable of capturing inequities repeatedly. This reform will aim to reduce disparity by tying hospital reimbursement with equity measures and improving disparities in care. This framework will require organizations to start collecting outcome data by subgroups and have the tools to identify root causes, develop a corresponding intervention, and measure a change in the performance of a health system.
Limitations of QIPs for equality improvement
While QIPs are a valuable tool for assessing healthcare systems, they also exhibit some notable limitations when it comes to ensuring equality. Firstly, although adherence to clinical guidelines is a crucial aspect of quality healthcare, it does not automatically guarantee equity across all patient demographics. Guidelines themselves might lack inclusivity and not account for unique circumstances among different groups. This issue may have multiple causes, including the reality that many of these guidelines are not developed based on representativeness of all ancestral and socio-demographic groups or that symptoms, conditions, and disease may manifest differently across populations, which might inadvertently result in disparities in health outcomes.
Moreover, achieving parity in adherence to guideline-based care is a commendable objective. However, guideline-based care stands alongside many other contributing factors to health inequities. Pathways to health disparities are found at various levels, many ultimately attributable to socio-economic risk factors, including housing, income, education, and environment. Furthermore, because evidence-based guidelines often do not proportionately represent all demographics, responses to standard therapy can vary significantly across diverse groups. This variation underscores a recognized systemic bias in the foundational evidence base for clinical care that could manifest in outcome research but might not be reflected in appropriate variation of benchmark care.
Lastly, the traditional QIP framework tends to prioritize collecting data on proportion of adherence to guidelines across a given provider or group of providers. However, this can misplace emphasis on adherence to a gold standard, which may or may not reflect significant outcome differences between these groups. Ultimately, there is a significant need to recenter improvement projects around patient outcomes first, and evaluating a clinical pathways ability to improve outcomes. Where adherence to a guideline is a reflection of pathway effectiveness; but does not necessarily improve in outcomes, as the guideline may be differentially beneficial across groups. It simply exaggerates an effect size. This approach reveals a gap in the QIP definition and approach, necessitating a shift to a more inclusive and effective model. This model must focus on developing frameworks for implementing, testing, and reporting results from health equity interventions, projects we call EQuality Improvement Projects (EQIPs).4
Current efforts targeting equality improvement
To aid the development of this framework we have characterized previously published studies that undertook QIPs viewed through a health equity lens. We focused on studies that introduced interventions or used a continuous quality improvement framework to reduce health disparities. We then utilized the key lessons from the sum of this body of work to set this in a new framework of systematic equality improvement. The full PubMed search strategy and data processing methodology can be found in the supplemental methods.
Our search yielded 40 studies that actively attempted to reduce health disparity. However, we also identified 149 studies that reported health equity audits but reported a disparity without documenting an intervention and follow-up audit. Of the 40 studies the majority were based in the USA (25/40), with multiple contributions from the UK (4/40) and Australia (4/40). Half were institution based (20/40), where several were conducted regionally (14), and the remaining six reported national coverage. There was a weighting toward the primary care and outpatient setting (23/40), with some representation from the inpatient (14/40) and (3/40) public health domain. Complete characteristics can be found in supplemental methods. Most studies focused on reducing race/ethnicity differences (26/40), and seven focused on sex-based disparities and socioeconomic income. Studies also examined language, visual/hearing impairment, and LGBTQ (lesbian, gay, bisexual, transgender, intersex, queer) disparities.
Designing an EQIP framework
The significant underrepresentation of QIPs in the literature underscores the need for transparently sharing tools and frameworks aimed at improving health equity. Our analysis reveals that less than a quarter of the health equity audits published report active interventions targeted at mitigating these disparities over time. However, among those that did, several reported success in reducing disparities, with several important implications for implementing EQIPs at scale. In the following text we bring together the key lessons from the 40 studies identified previously into a unified framework for improving health equity (Table 1).
Table 1.
Key lessons for Designing EQIPs
| Lesson | Explanation | Reference |
|---|---|---|
| Incentivize and encourage health equity processes. | Pay for equity encourages discovery where organizations should be rewarded for providing good care for all. Successful practices can be used to develop transferable frameworks that can be appropriately incentivized. | 5,6,7,8,9 |
| Develop and share tools to track equity | Develop tools to track outcomes in real-time that can be used to create health equity reports that can unmask previously hidden inequalities between groups. Then publish and open-source these tools. | 10,11,12,13,14,15,16 |
| Engage Systematic Equality improvement | Few disparities can be expected to be abolished in one cycle; therefore, tools must form part of a broader framework that detect disparities and points to corresponding interventions to reduce disparity. | 17,18,19,20,21,22,23 |
| Encourage cross-disciplinary collaboration | Cross-disciplinary projects are more likely to yield understanding of the complex causes of inequity and different teams are well-positioned to generate an appropriate interventions. | 24,25,26,27 |
| Outreach/educating patients | Successful EQIPs used outreach techniques to engage minorities and provide information on their available care. | 28,29,30,31,32,33 |
| Educate staff/provide clear information on disparities | Provide education on disparities that exist and how biases may manifest. Then provide clear information on the disparities within a local context in real-time. | 34,35,36,37,38,39,40 |
| Consider how diversity may affect presentation, treatment, and follow up. | Different groups have varying risk factors, and care delivery should aim to recognize how patients may differ in environment, circumstances, and lifestyle and use these insights to maximize their outcomes. | 41,42,43,44 |
EQIPs: Equality Improvement Projects
Implement and share tools for health equity tracking
The collection of outcome data by subgroups must become a fundamental part of clinical practice to effectively address health disparities. Yet, there are no set standards for acceptable outcome differences between demographic and clinical groups. Further complicating this issue is the fact that quantifying and publishing demographic-based differences in outcomes is not currently mandatory, making it extremely challenging to measure the scope of these disparities accurately.
This concern is particularly valid as the knowledge landscape that informs clinical practice often fails to represent all populations adequately, especially minority groups. Such knowledge imbalance is troublesome as traditional QIPs typically measure success based on adherence to guidelines informed by this potentially skewed literature. Consequently, it is crucial to collect this information regularly, showcasing progress over time and making visible the real-world disparities in healthcare outcomes. Given that audits can be labor-intensive when manual data collection is necessary, leveraging tools that can continuously extract and display outcomes to stakeholders will significantly contribute to scaling health equity. This effort can include developing tools like disparity dashboards, which provide real-time data and insights into health disparities.45
One key challenge to reproducible evaluation and comprehensive tracking is the reluctance or prohibition of recording sensitive attributes, such as race, in many regions, including large parts of Europe. However, the prohibition against the collection of sensitive data need not be an insurmountable barrier to collecting crucial data that inform understanding of disparities. Other factors that can impact clinical outcomes such as socioeconomic status may be a suitable and valuable category informing patterns of health disparity. This crucial data are necessary to accurately assess the impact on vulnerable groups and fully understand the scope of the problem. Therefore, we argue that the collection and reporting of such data should be mandatory and standardized where it is relevant and not prohibited. This will demand transparent and public processes that reassure patients and providers of appropriate management of their data. To safeguard against misuse of sensitive data there must be a strong ethical, legal, and social framework that governs what is beneficial to patients, and what is deemed an invasion of privacy. Significant downstream implications also arise from the failure to collect such data, potentially leading to patient harm. For instance, the lack of comprehensive and representative data could compromise the evaluation of Artificial Intelligence (AI) tools, which may inadvertently encode disparities from routinely collected Electronic Health Record (EHR) data. Hence, addressing these data collection challenges is vital in moving toward a more equitable healthcare system.
Systematic improvement and cross-disciplinary collaboration
The consistent collection and analysis of demographic data are imperative steps toward addressing health disparities and implementing effective policies. However, these efforts should be embedded within a broader framework of systematic equality improvement. This should involve a top-down process, championed by governmental bodies who not only incentivize these endeavors but also invest in the necessary technology to deliver enhanced results.
Interestingly, a significant portion of EQIPs investigated in this study were implemented at the institutional level, implying a potential risk of duplication when these efforts are extrapolated to regional and national scales. To mitigate such redundancy and maximize efficiency, there must be concerted efforts to coordinate between sites, share results transparently, and extract valuable lessons from each intervention. Such collaboration can optimize resources and enable healthcare organizations to learn from each other’s successes and challenges. Furthermore, it is important to recognize that the landscape of health disparities is fluid. This is both in the areas of care disparities and the fact that groups considered as minorities or discriminated against can shift over time due to various factors. While disparities are heavily concentrated in specific groups at present, and efforts should focus on these groups now, the process of detecting and reducing disparities must consider its place in the broader landscape. New technologies, treatments, and health policies can differentially impact different groups, sometimes creating new disparities while addressing others. Therefore, there’s a pressing need for continuous and systematic equality improvement frameworks that can adapt to these evolving landscapes.
In essence, while data collection is a crucial component of addressing health disparities, it must be part of a larger, dynamic strategy of systematic equality improvement. This approach calls for robust governmental support, inter-institutional collaboration, and an understanding of the fluidity of health disparities. Only then can we truly hope to make significant strides in addressing and reducing health disparities on a large scale.
Patient engagement, staff education, and understanding contextual differences
A key strength of EQIPs lies in the priority they accord to patient outreach and education. This patient-centric approach is particularly beneficial for minority groups, who often experience the brunt of health disparities. Patient education efforts help demystify available care options, enabling patients to make informed decisions about their health. Such engagement not only empowers patients but also promotes a shared understanding of health goals, fostering a stronger partnership between patients and healthcare providers.
Simultaneously, educating healthcare staff about the realities of health disparities is crucial. Staff must be aware of how biases, whether explicit or implicit, can potentially compromise the quality of care. By providing clear, real-time information about local disparities, staff members can better understand the context in which they provide care, equipping them to recognize and tackle these biases head-on.
This notion of understanding and addressing health within context extends to the broader EQIP framework. Each patient group has its unique set of risk factors, lifestyle choices, and health beliefs—all of which contribute to their health outcomes. By acknowledging these distinct contexts, healthcare providers can develop personalized care tools and delivery methods that respect and respond to this diversity.
In essence, the intersection of patient education, staff enlightenment, and contextual understanding is a potent formula for prioritizing health equity. EQIPs exemplify this approach, ensuring that care is not only high quality but is also equitable and responsive to the needs of different patient groups.
Limitations
This paper acknowledges several limitations in the current landscape of QIP evaluation and sharing. First and foremost, QIPs are not routinely published, thus the picture we present in this paper may not reflect the entirety of the initiatives undertaken. This lack of transparency obscures a complete understanding of the efforts made in quality improvement. The existing practice of conducting quality improvement in isolation, or “working in a silo,” can lead to significant delays, unnecessary duplication of efforts, and even harm to the patient population. Moreover, this modality hinders the broad-scale recognition of disparities and the development of effective tools to address them.
To achieve health equity, we must encourage a culture that prioritizes the systematic documentation of disparities and the strategies developed to overcome them. Not only does this allow others to identify these disparities in their own contexts, but it also facilitates learning from others’ experiences and leveraging those insights to improve patient care universally.
The recent shift by CMS to provide reimbursement for health equity could represent toward systematizing this process and, over time, foster development of a pool of effective interventions. This article aims to encourage healthcare entities to adopt systematic mechanisms for measuring, improving, and sharing their EQIP successes and failures. By acknowledging and learning from both our successes and our shortcomings, we can work collaboratively toward the goal of health equity for all.
Conclusions
This study underscores the urgent necessity for transparent, continuous measurement of health disparities in clinical practice as part of a more substantial shift toward systematic equality improvement. Integrating tools like disparity dashboards, which continuously display and disseminate changes in health disparities, will be crucial to scaling this framework’s success.45 However, the transition to this new model will necessitate a substantial collective effort within healthcare institutions. It is not sufficient merely to identify disparities—once brought to light, active measures must be taken to reduce these disparities.
The EQIP framework offers a promising path toward this goal, fundamentally redefining the objectives of traditional QIPs. Instead of focusing solely on overall improvements in healthcare, EQIPs emphasize the need for tailoring care to the unique needs and circumstances of diverse patient groups. This focus aims to systematically address and reduce disparities in healthcare outcomes, providing truly equitable care. To accomplish this, transparency and data sharing must become the norm in healthcare. The current restricted view of health disparities significantly hampers our ability to deliver quality care for all. As we strive to enhance healthcare outcomes for every demographic group, we must remember that equity is an ongoing pursuit, as yet, requiring continuous monitoring, assessment, and intervention. Together, we can transform the landscape of healthcare, ensuring quality and equity go hand in hand.
Acknowledgments
Author contributions
J.G. and L.A.C. conceived the study. J.G. and M.G. processed the data and carried out the data analysis. All authors participated in the discussion and interpretation of the results. J.G. wrote the initial draft. All authors critically revised the manuscript for intellectual content, approved the final version, and met the ICMJE criteria for authorship. J.G. is the guarantor of the study. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Declaration of interests
L.A.C. is funded by the National Institute of Health through the NIBIB R01 017215. All authors declare no financial relationships with any organizations that might have an interest in the submitted work in the previous three years, and no other relationships or activities that could appear to have influenced the submitted work.
Footnotes
Supplemental information can be found online at https://doi.org/10.1016/j.isci.2023.107924.
Supplemental information
Data and code availability
The supplementary methods contain full details on the methods and data used to inform this perspective piece.
References
- 1.Chin M.H. Creating the Business Case for Achieving Health Equity. J. Gen. Intern. Med. 2016;31:792–796. doi: 10.1007/s11606-016-3604-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.davidmcclintock . Epstein Becker & Green, P.C.; 2023. Biden Administration Prioritizes Health Equity in Proposed Reforms to Medicare Managed Care.https://www.ebglaw.com/insights/biden-administration-prioritizes-health-equity-in-proposed-reforms-to-medicare-managed-care/ [Google Scholar]
- 3.CMS Medicare Program; Contract Year 2024 Policy and Technical Changes to the Medicare Advantage Program, Medicare Prescription Drug Benefit Program, Medicare Cost Plan Program, Medicare Parts A, B, C, and D Overpayment Provisions of the Affordable Care Act and Programs of All-Inclusive Care for the Elderly; Health Information Technology Standards and Implementation Specifications. 2022. https://www.federalregister.gov/documents/2022/12/27/2022-26956/medicare-program-contract-year-2024-policy-and-technical-changes-to-the-medicare-advantage-program Federal Register.
- 4.Brooks D., Douglas M., Aggarwal N., Prabhakaran S., Holden K., Mack D. Developing a framework for integrating health equity into the learning health system. Learn. Health Syst. 2017;1:e10029. doi: 10.1002/lrh2.10029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Siegel B., Sears V., Bretsch J.K., Wilson M., Jones K.C., Mead H., Hasnain-Wynia R., Ayala R.K., Bhalla R., Cornue C.M., et al. A Quality Improvement Framework for Equity in Cardiovascular Care: Results of a National Collaborative. J. Healthc. Qual. 2012;34:32–42. doi: 10.1111/j.1945-1474.2011.00196.x. [DOI] [PubMed] [Google Scholar]
- 6.Bhalla R., Schechter C.B., Strelnick A.H., Deb N., Meissner P., Currie B.P. Pay for performance improves quality across demographic groups. Qual. Manag. Health Care. 2013;22:199–209. doi: 10.1097/QMH.0b013e31829a6b4f. [DOI] [PubMed] [Google Scholar]
- 7.Hamilton F.L., Bottle A., Vamos E.P., Curcin V., Ng A., Molokhia M., Majeed A., Millett C. Impact of a Pay-for-Performance Incentive Scheme on Age, Sex, and Socioeconomic Disparities in Diabetes Management in UK Primary Care. J. Ambul. Care Manag. 2010;33:336–349. doi: 10.1097/JAC.0b013e3181f68f1d. [DOI] [PubMed] [Google Scholar]
- 8.Manning S.E., Blinn A.M., Selk S.C., Silva C.F., Stetler K., Stone S.L., Yazdy M.M., Bharel M. The Massachusetts Racial Equity Data Road Map: Data as a Tool Toward Ending Structural Racism. J. Publ. Health Manag. Pract. 2022;28:S58–S65. doi: 10.1097/PHH.0000000000001428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McConnell K.J., Charlesworth C.J., Meath T.H.A., George R.M., Kim H. Oregon’s Emphasis On Equity Shows Signs Of Early Success For Black And American Indian Medicaid Enrollees. Health Aff. 2018;37:386–393. doi: 10.1377/hlthaff.2017.1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park J., Arunachalam R., Silenzio V., Singh V.K. Fairness in Mobile Phone-Based Mental Health Assessment Algorithms: Exploratory Study. JMIR Form. Res. 2022;6:e34366. doi: 10.2196/34366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Siegel B., Bear D., Andres E., Mead H. Measuring equity: an index of health care disparities. Qual. Manag. Health Care. 2009;18:84–90. doi: 10.1097/01.QMH.0000349973.61836.41. [DOI] [PubMed] [Google Scholar]
- 12.Cykert S., Eng E., Manning M.A., Robertson L.B., Heron D.E., Jones N.S., Schaal J.C., Lightfoot A., Zhou H., Yongue C., Gizlice Z. A Multi-faceted Intervention Aimed at Black-White Disparities in the Treatment of Early Stage Cancers: The ACCURE Pragmatic Quality Improvement trial. J. Natl. Med. Assoc. 2020;112:468–477. doi: 10.1016/j.jnma.2019.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Badrick E., Hull S., Mathur R., Shajahan S., Boomla K., Bremner S., Robson J. Health equity audits in general practice: a strategy to reduce health inequalities. Prim. Health Care Res. Dev. 2014;15:80–95. doi: 10.1017/S1463423612000606. [DOI] [PubMed] [Google Scholar]
- 14.Maharaj V., Rahman F., Adamson L. Tackling child health inequalities due to deprivation: using health equity audit to improve and monitor access to a community paediatric service. Child Care Health Dev. 2014;40:223–230. doi: 10.1111/cch.12011. [DOI] [PubMed] [Google Scholar]
- 15.Martinez E.M., Carr D.T., Mullan P.C., Rogers L.E., Howlett-Holley W.L., McGehee C.A., Mangum C.D., Godambe S.A. Improving Equity of Care for Patients with Limited English Proficiency Using Quality Improvement Methodology. Pediatr. Qual. Saf. 2021;6:e486. doi: 10.1097/pq9.0000000000000486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Impact of Quality Improvement Efforts on Race and Sex Disparities in Hemodialysis | Health Disparities | JAMA | JAMA Network. https://jamanetwork.com/journals/jama/fullarticle/196047 [DOI] [PubMed]
- 17.Obaid M., Igawa T., Maxwell A., Murray Y.L., Rahman A., Aboudi D., Olivo K., Roeder T., Valdes-Greene R., Brumberg H., et al. “Liquid Gold” Lactation Bundle and Breastfeeding Rates in Racially Diverse Mothers of Extremely Low-Birth-Weight Infants. Breastfeed. Med. 2021;16:463–470. doi: 10.1089/bfm.2020.0322. [DOI] [PubMed] [Google Scholar]
- 18.Balicer R.D., Shadmi E., Lieberman N., Greenberg-Dotan S., Goldfracht M., Jana L., Cohen A.D., Regev-Rosenberg S., Jacobson O. Reducing Health Disparities: Strategy Planning and Implementation in Israel’s Largest Health Care Organization. Health Serv. Res. 2011;46:1281–1299. doi: 10.1111/j.1475-6773.2011.01247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Du X., Patel A., Li X., Wu Y., Turnbull F., Gao R. Treatment and outcomes of acute coronary syndromes in women: An analysis of a multicenter quality improvement Chinese study. Int. J. Cardiol. 2017;241:19–24. doi: 10.1016/j.ijcard.2017.03.090. [DOI] [PubMed] [Google Scholar]
- 20.Edmond K.M., Tung S., McAuley K., Strobel N., McAullay D. Improving developmental care in primary practice for disadvantaged children. Arch. Dis. Child. 2019;104:372–380. doi: 10.1136/archdischild-2018-315164. [DOI] [PubMed] [Google Scholar]
- 21.Fox P., Porter P.G., Lob S.H., Boer J.H., Rocha D.A., Adelson J.W. Improving asthma-related health outcomes among low-income, multiethnic, school-aged children: results of a demonstration project that combined continuous quality improvement and community health worker strategies. Pediatrics. 2007;120:e902–e911. doi: 10.1542/peds.2006-1805. [DOI] [PubMed] [Google Scholar]
- 22.Glover J., Lynn C., Holzman J.B.W., Germone M., Talmi A. Working toward Socially Responsive Recruitment Practices of Psychology Interns in an Academic Medical Center. J. Pediatr. Psychol. 2022;47:1110–1124. doi: 10.1093/jpepsy/jsac063. [DOI] [PubMed] [Google Scholar]
- 23.Nietert P.J., Ornstein S.M., Jenkins R.G., Roylance L.F., Dickerson L.M., Feifer C. The effect of ethnicity on outcomes in a practice-based trial to improve cardiovascular disease prevention. Int. J. Equity Health. 2004;3:12. doi: 10.1186/1475-9276-3-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wahl T.S., Goss L.E., Morris M.S., Gullick A.A., Richman J.S., Kennedy G.D., Cannon J.A., Vickers S.M., Knight S.J., Simmons J.W., Chu D.I. Enhanced Recovery After Surgery (ERAS) Eliminates Racial Disparities in Postoperative Length of Stay After Colorectal Surgery. Ann. Surg. 2018;268:1026–1035. doi: 10.1097/SLA.0000000000002307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gianelis K.A., Butler J.M. Improving equitable access to inclusive sexual healthcare in a small urban college health setting. Nurs. Forum. 2022;57:686–693. doi: 10.1111/nuf.12708. [DOI] [PubMed] [Google Scholar]
- 26.Haynes E., Hohnen H., Katzenellenbogen J.M., Scalley B.D., Thompson S.C. Knowledge translation lessons from an audit of Aboriginal Australians with acute coronary syndrome presenting to a regional hospital. SAGE Open Med. 2016;4 doi: 10.1177/2050312116661114. 2050312116661114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mahotière T., Ocepek-Welikson K., Daley M.B., Byssainthe J.P. A Program to reduce the disparity in the rate of biennial lipid profiles between african-american and white medicare beneficiaries with diabetes mellitus in new york city. J. Community Health. 2006;31:263–288. doi: 10.1007/s10900-006-9015-7. [DOI] [PubMed] [Google Scholar]
- 28.Knutson J., Butler J. Providing Equitable Postpartum Breastfeeding Support at an Urban Academic Hospital. Nurs. Womens Health. 2022;26:184–193. doi: 10.1016/j.nwh.2022.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Austad K., Juarez M., Shryer H., Moratoya C., Rohloff P. Obstetric care navigation: results of a quality improvement project to provide accompaniment to women for facility-based maternity care in rural Guatemala. BMJ Qual. Saf. 2020;29:169–178. doi: 10.1136/bmjqs-2019-009524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ashing-Giwa K.T. Enhancing physical well-being and overall quality of life among underserved Latina-American cervical cancer survivors: feasibility study. J. Cancer Surviv. 2008;2:215–223. doi: 10.1007/s11764-008-0061-2. [DOI] [PubMed] [Google Scholar]
- 31.Gallaher C., Herrmann S., Hunter L., Wilkins A. The St Thomas’ Hospital Emergency Department Homeless Health Initiative: improving the quality, safety and equity of healthcare provided for homeless patients attending the ED. BMJ Open Qual. 2020;9:e000820. doi: 10.1136/bmjoq-2019-000820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ir P., Horemans D., Souk N., Van Damme W. Using targeted vouchers and health equity funds to improve access to skilled birth attendants for poor women: a case study in three rural health districts in Cambodia. BMC Pregnancy Childbirth. 2010;10:1. doi: 10.1186/1471-2393-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jenkins C., McNary S., Carlson B.A., King M.G., Hossler C.L., Magwood G., Zheng D., Hendrix K., Beck L.S., Linnen F., et al. Reducing Disparities for African Americans with Diabetes: Progress Made by the REACH 2010 Charleston and Georgetown Diabetes Coalition. Public Health Rep. 2004;119:322–330. doi: 10.1016/j.phr.2004.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Scalley B., Gee A., Katzenellenbogen J.M., Gilles M., Jegasothy E., Thompson S.C. Improving the management of acute coronary syndrome for Aboriginal and non-Aboriginal patients in a regional hospital. Aust. N. Z. J. Public Health. 2016;40:529–534. doi: 10.1111/1753-6405.12550. [DOI] [PubMed] [Google Scholar]
- 35.Arrington L.A., Edie A.H., Sewell C.A., Carter B.M. Launching the Reduction of Peripartum Racial/Ethnic Disparities Bundle: A Quality Improvement Project. J. Midwifery Wom. Health. 2021;66:526–533. doi: 10.1111/jmwh.13235. [DOI] [PubMed] [Google Scholar]
- 36.Burkitt K.H., Rodriguez K.L., Mor M.K., Fine M.J., Clark W.J., Macpherson D.S., Mannozzi C.M., Muldoon M.F., Long J.A., Hausmann L.R.M. Evaluation of a collaborative VA network initiative to reduce racial disparities in blood pressure control among veterans with severe hypertension. Health. 2021;8(Suppl 1):100485. doi: 10.1016/j.hjdsi.2020.100485. [DOI] [PubMed] [Google Scholar]
- 37.Furness B.W., Goldhammer H., Montalvo W., Gagnon K., Bifulco L., Lentine D., Anderson D. Transforming Primary Care for Lesbian, Gay, Bisexual, and Transgender People: A Collaborative Quality Improvement Initiative. Ann. Fam. Med. 2020;18:292–302. doi: 10.1370/afm.2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hoenig M.P., Mann A., Pavlakis M. Removal of the Black race coefficient from the estimated glomerular filtration equation improves transplant eligibility for Black patients at a single center. Clin. Transplant. 2022;36:e14467. doi: 10.1111/ctr.14467. [DOI] [PubMed] [Google Scholar]
- 39.Isgrò V., Sultana J., Fontana A., Ientile V., Alecci U., Scoglio R., Magliozzo F., Scondotto S., Caramori G., Cazzola M., Trifirò G. Gender differences in COPD management in a Sicilian general practice setting: a cohort study evaluating the impact of educational interventions. ERJ Open Res. 2020;6:00279-2020. doi: 10.1183/23120541.00279-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McDonald N., Little N., Grierson R., Weldon E. Sex and Gender Equity in Prehospital Electrocardiogram Acquisition. Prehospital Disaster Med. 2022;37:1–7. doi: 10.1017/S1049023X2200036X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Tilley B.C., Mainous A.G., Amorrortu R.P., McKee M.D., Smith D.W., Li R., DeSantis S.M., Vernon S.W., Koch G., Ford M.E., et al. Using increased trust in medical researchers to increase minority recruitment: The RECRUIT cluster randomized clinical trial. Contemp. Clin. Trials. 2021;109:106519. doi: 10.1016/j.cct.2021.106519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bryant P.K. Congestive heart failure performance-improvement project: special needs for special patients. Lippincott's Case Manag. 2002;7:152–162. doi: 10.1097/00129234-200207000-00005. [DOI] [PubMed] [Google Scholar]
- 43.Burgess C.P., Bailie R.S., Connors C.M., Chenhall R.D., McDermott R.A., O’Dea K., Gunabarra C., Matthews H.L., Esterman A.J. Early identification and preventive care for elevated cardiovascular disease risk within a remote Australian Aboriginal primary health care service. BMC Health Serv. Res. 2011;11:24. doi: 10.1186/1472-6963-11-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Nnorom O., Sappong-Kumankumah A., Olaiya O.R., Burnett M., Akor N., Shi N., Wright P., Gebreyesus A., Gebremikael L., Lofters A. Afrocentric screening program for breast, colorectal, and cervical cancer among immigrant patients in Ontario. Can. Fam. Physician. 2021;67:843–849. doi: 10.46747/cfp.6711843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Martino S.C., Mathews M., Beckett M.K., Agniel D., Hambarsoomian K., Scholle S.H., Collins S., Quigley D.D., Darabidian B., Elliott M.N. Development of a Medicare plan dashboard to promote health equity. Am. J. Manag. Care. 2023;29:e91–e95. doi: 10.37765/ajmc.2023.89335. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The supplementary methods contain full details on the methods and data used to inform this perspective piece.


