Abstract
Surgical and interventional repair of thoracoabdominal aortic aneurysms improve survival significantly compared to the natural history of the disease. However, both strategies are associated with a substantial risk of spinal cord ischemia, which has been reported to occur—even in contemporary series by expert centers—in up to 12% of patients, depending on the extent of the disease. Following improved neurological outcomes after staged approaches in extensive clinical and long-term large animal studies, and the description of the “collateral network”, the concept of “Minimally Invasive Staged Segmental Artery Coil Embolization” (MIS2ACE) was introduced by Etz et al. This concept of priming the collateral network in order to improve spinal cord blood supply showed promising experimental and early clinical outcomes, and consequently led to the initiation of the randomized controlled multicenter PAPAartis trial (Paraplegia Prevention in Aortic Aneurysm Repair by Thoracoabdominal Staging). This Keynote Lecture describes the background and rationale for this trial and gives an update on the current status.
Keywords: Thoracoabdominal aortic repair, spinal cord ischemia (SCI), aortic surgery
Introduction
Spinal cord ischemia (SCI) is one of the most devastating complications following surgical or interventional treatment of thoracoabdominal aortic aneurysms (TAAA). It can occur immediately or delayed and it depends strongly on the extent of the TAAA that is being treated, with reports of up to 22% of patients with Crawford type II aneurysms being affected (1-4). A variety of—in some instances counterintuitive or even seemingly contradictory—concepts have been described to prevent SCI including intra- and perioperative cerebrospinal fluid drainage, preservation of an adequate mean arterial pressure, especially in relation to the patient’s preoperative arterial pressure, as well as generous systematic sacrifice and reimplantation of intercostal and lumbar arteries without motor evoked potential (MEP) or somatosensory evoked potential (SSEP) monitoring during surgical repair (3,5). It is well known that a staged repair significantly reduces SCI in TAAA repair (6,7).
Following extensive translational research on preventing SCI in the large animal lab by Dr. Griepp’s group under the lead of Dr. Etz in the late 2000s, the collateral network concept of spinal cord perfusion has been thoroughly investigated (8-12). This culminated in the introduction of the technique of Minimally Invasive Staged Segmental Artery Coil Embolization (MIS2ACE) to combine the advantages of an individualized, selective, staged approached with modern endovascular technologies (13). This Keynote Lecture presents the rationale of the PapaArtis trial (Paraplegia Prevention in Aortic Aneurysm Repair) by MIS2ACE. It is the largest publicly funded randomized controlled international multicenter trial in aortic aneurysm repair so far (14).
SCI in thoracoabdominal aortic repair
In 1986, Dr. Crawford introduced a classification, in which TAAA are divided into four groups depending on the extent of the aneurysm (1). This classification was modified by Dr. Safi in 1998 with an additional fifth group (2). It is well known that patients undergoing surgical repair for TAAA have significantly better survival compared to patients who are not treated surgically (15). Endovascular and open repair techniques show similar survival and rates of SCI; however, the choice of technique may depend on patients’ age and comorbidities (3). With either technique, SCI remains as the major concern. Pathophysiologically, an increase in intracranial pressure leads to decreased spinal cord perfusion pressure, resulting in SCI (5). As SCI does not only occur immediately after the intervention, but also in a delayed manner, a dynamic aspect in spinal cord perfusion can be assumed (16). In addition, it is well known that a staged approach reduces the risk of SCI significantly (6,7). This is based on improved arterial blood supply by a sophistically primed spinal cord collateral network, which—according to current concepts—can be ‘primed’ by arteriogenesis with the development of new arteries, transferring arterial blood from three major inflow sources to the paraspinal (and spinal) microcirculation. The presence of this collateral network led to the concept that a staged approach by preemptive segmental artery coil embolization may prevent SCI (11,12) through priming of the collateral network (by arteriogenesis).
MIS2ACE concept
The technique of MIS2ACE is described in another paper in this special issue of the Annals of Cardiothoracic Surgery. In brief, MIS2ACE is performed under local anesthesia with percutaneous access. Up to seven segmental artery pairs are occluded within one session, depending on the clinical symptoms of the patient during coil embolization. These symptoms may occur as transient back pain. Depending on the number of segmental arteries that need to be occluded, the coil embolization is repeated, with at least five days and a recommended three-week interval between sessions. Patient are closely monitored for the first 72 hours after the intervention to ensure they are maintaining an adequate blood pressure, which needs to be correlated with the preexisting blood pressure.
The “first in man” endovascular preconditioning of the spinal cord collateral network was performed in 2015 (17), followed by the first series of ischemic priming in patients undergoing endovascular TAAA repair (18).
PAPAartis trial
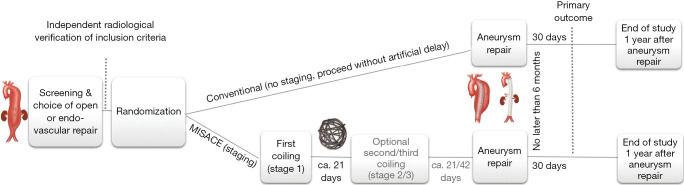
As the MIS2ACE concept showed promising results, the PapaArtis trial was initiated, striving for ‘Level A’ evidence. The trial received funding from the European Union’s (EU) Horizon 2020 research and innovation programme under grant agreement No. 733203 and from the German Research Foundation under grant agreement ET 127/2-1. Until now, it is the largest publicly funded randomized controlled trial in aortic surgery. The trial has been registered with clincaltrials.gov (NCT03434314) and a detailed trial protocol was published in 2019 (14). Trial duration was initially set for five years with 500 participants and 31 recruiting centers in nine countries across Europe and the United States (Figure 1). The coronavirus disease (COVID) pandemic, however, led to a dramatic shortage in intensive care unit (ICU) capacity throughout Europe basically putting all major surgical trials on hold for two years. Following expert reviewer’s advice, the trial duration was therefore recently officially extended by the EU and the German Research Foundation. The trial pathway is depicted in Figure 2.
Figure 1.
List of participating centers. MISACE, Minimally Invasive Staged Segmental Artery Coil Embolization; ca., circa.
Figure 2.
Participant timeline. CH, Switzerland; DE, Germany; FR, France; IT, Italy; NL, Netherlands; PL, Poland; SE, Sweden; UK, United Kingdom; US, Unites States of America.
Patient preoperative data showed excellent representation of “real world” aneurysm extent data with 55% and 50% of stage II TAAA in the surgical and control arm, respectively. So far, no SCI has been reported during MIS2ACE procedures performed in this trial. Patients are assessed with detailed neurological investigations including the modified Rankin Scale-9Q (19), the Montreal Cognitive Assessment (MoCA) (20) and Barthel-Index (21). A first interim analysis is expected in the fourth quarter of 2023.
Conclusions
The PAPAartis trial is a prospective, randomized, multicenter international trial to assess the outcome of selective staged segmental artery coil embolization prior to open and endovascular TAAA repair to prevent SCI and ultimately permanent paraplegia. Initial results and experimental studies are promising and strongly suggest that with this concept, SCI can be significantly reduced in patients undergoing open or endovascular treatment for various thoracoabdominal aortic pathologies.
Video.
Rationale of the PAPAartis trial.
Acknowledgments
Funding: None.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.Crawford ES, Crawford JL, Safi HJ, et al. Thoracoabdominal aortic aneurysms: preoperative and intraoperative factors determining immediate and long-term results of operations in 605 patients. J Vasc Surg 1986;3:389-404. 10.1067/mva.1986.avs0030389 [DOI] [PubMed] [Google Scholar]
- 2.Safi HJ, Winnerkvist A, Miller CC, 3rd, et al. Effect of extended cross-clamp time during thoracoabdominal aortic aneurysm repair. Ann Thorac Surg 1998;66:1204-9. 10.1016/s0003-4975(98)00781-4 [DOI] [PubMed] [Google Scholar]
- 3.Greenberg RK, Lu Q, Roselli EE, et al. Contemporary analysis of descending thoracic and thoracoabdominal aneurysm repair: a comparison of endovascular and open techniques. Circulation 2008;118:808-17. 10.1161/CIRCULATIONAHA.108.769695 [DOI] [PubMed] [Google Scholar]
- 4.Conrad MF, Crawford RS, Davison JK, et al. Thoracoabdominal aneurysm repair: a 20-year perspective. Ann Thorac Surg 2007;83:S856-61; discussion S890-2. 10.1016/j.athoracsur.2006.10.096 [DOI] [PubMed] [Google Scholar]
- 5.Etz CD, Weigang E, Hartert M, et al. Contemporary spinal cord protection during thoracic and thoracoabdominal aortic surgery and endovascular aortic repair: a position paper of the vascular domain of the European Association for Cardio-Thoracic Surgery†. Eur J Cardiothorac Surg 2015;47:943-57. 10.1093/ejcts/ezv142 [DOI] [PubMed] [Google Scholar]
- 6.Etz CD, Zoli S, Mueller CS, et al. Staged repair significantly reduces paraplegia rate after extensive thoracoabdominal aortic aneurysm repair. J Thorac Cardiovasc Surg 2010;139:1464-72. 10.1016/j.jtcvs.2010.02.037 [DOI] [PubMed] [Google Scholar]
- 7.Maurel B, Delclaux N, Sobocinski J, et al. The impact of early pelvic and lower limb reperfusion and attentive peri-operative management on the incidence of spinal cord ischemia during thoracoabdominal aortic aneurysm endovascular repair. Eur J Vasc Endovasc Surg 2015;49:248-54. 10.1016/j.ejvs.2014.11.017 [DOI] [PubMed] [Google Scholar]
- 8.Etz CD, Homann TM, Luehr M, et al. Spinal cord blood flow and ischemic injury after experimental sacrifice of thoracic and abdominal segmental arteries. Eur J Cardiothorac Surg 2008;33:1030-8. 10.1016/j.ejcts.2008.01.069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Etz CD, Homann TM, Plestis KA, et al. Spinal cord perfusion after extensive segmental artery sacrifice: can paraplegia be prevented? Eur J Cardiothorac Surg 2007;31:643-8. 10.1016/j.ejcts.2007.01.023 [DOI] [PubMed] [Google Scholar]
- 10.Geisbüsch S, Stefanovic A, Koruth JS, et al. Endovascular coil embolization of segmental arteries prevents paraplegia after subsequent thoracoabdominal aneurysm repair: an experimental model. J Thorac Cardiovasc Surg 2014;147:220-6. 10.1016/j.jtcvs.2013.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Etz CD, Kari FA, Mueller CS, et al. The collateral network concept: remodeling of the arterial collateral network after experimental segmental artery sacrifice. J Thorac Cardiovasc Surg 2011;141:1029-36. 10.1016/j.jtcvs.2010.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Etz CD, Kari FA, Mueller CS, et al. The collateral network concept: a reassessment of the anatomy of spinal cord perfusion. J Thorac Cardiovasc Surg 2011;141:1020-8. 10.1016/j.jtcvs.2010.06.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Luehr M, Salameh A, Haunschild J, et al. Minimally invasive segmental artery coil embolization for preconditioning of the spinal cord collateral network before one-stage descending and thoracoabdominal aneurysm repair. Innovations (Phila) 2014;9:60-5. 10.1097/IMI.0000000000000038 [DOI] [PubMed] [Google Scholar]
- 14.Petroff D, Czerny M, Kölbel T, et al. Paraplegia prevention in aortic aneurysm repair by thoracoabdominal staging with 'minimally invasive staged segmental artery coil embolisation' (MIS2ACE): trial protocol for a randomised controlled multicentre trial. BMJ Open 2019;9:e025488. 10.1136/bmjopen-2018-025488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller CC, 3rd, Porat EE, Estrera AL, et al. Number needed to treat: analyzing of the effectiveness of thoracoabdominal aortic repair. Eur J Vasc Endovasc Surg 2004;28:154-7. 10.1016/j.ejvs.2004.03.004 [DOI] [PubMed] [Google Scholar]
- 16.Etz CD, Luehr M, Kari FA, et al. Paraplegia after extensive thoracic and thoracoabdominal aortic aneurysm repair: does critical spinal cord ischemia occur postoperatively? J Thorac Cardiovasc Surg 2008;135:324-30. 10.1016/j.jtcvs.2007.11.002 [DOI] [PubMed] [Google Scholar]
- 17.Etz CD, Debus ES, Mohr FW, et al. First-in-man endovascular preconditioning of the paraspinal collateral network by segmental artery coil embolization to prevent ischemic spinal cord injury. J Thorac Cardiovasc Surg 2015;149:1074-9. 10.1016/j.jtcvs.2014.12.025 [DOI] [PubMed] [Google Scholar]
- 18.Branzan D, Etz CD, Moche M, et al. Ischaemic preconditioning of the spinal cord to prevent spinal cord ischaemia during endovascular repair of thoracoabdominal aortic aneurysm: first clinical experience. EuroIntervention 2018;14:828-35. 10.4244/EIJ-D-18-00200 [DOI] [PubMed] [Google Scholar]
- 19.Patel N, Rao VA, Heilman-Espinoza ER, et al. Simple and reliable determination of the modified rankin scale score in neurosurgical and neurological patients: the mRS-9Q. Neurosurgery 2012;71:971-5; discussion 975. 10.1227/NEU.0b013e31826a8a56 [DOI] [PubMed] [Google Scholar]
- 20.Davis DH, Creavin ST, Yip JL, et al. Montreal Cognitive Assessment for the diagnosis of Alzheimer's disease and other dementias. Cochrane Database Syst Rev 2015;2015:CD010775. 10.1002/14651858.CD010775.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mahoney FI, Barthel DW. Functional evaluation: the barthel index. Md State Med J 1965;14:61-5. [PubMed] [Google Scholar]