Abstract
Background
This review is an update of a rapid review undertaken in 2020 to identify relevant, feasible and effective communication approaches to promote acceptance, uptake and adherence to physical distancing measures for COVID‐19 prevention and control. The rapid review was published when little was known about transmission, treatment or future vaccination, and when physical distancing measures (isolation, quarantine, contact tracing, crowd avoidance, work and school measures) were the cornerstone of public health responses globally.
This updated review includes more recent evidence to extend what we know about effective pandemic public health communication. This includes considerations of changes needed over time to maintain responsiveness to pandemic transmission waves, the (in)equities and variable needs of groups within communities due to the pandemic, and highlights again the critical role of effective communication as integral to the public health response.
Objectives
To update the evidence on the question 'What are relevant, feasible and effective communication approaches to promote acceptance, uptake and adherence to physical distancing measures for COVID‐19 prevention and control?', our primary focus was communication approaches to promote and support acceptance, uptake and adherence to physical distancing.
Secondary objective: to explore and identify key elements of effective communication for physical distancing measures for different (diverse) populations and groups.
Search methods
We searched MEDLINE, Embase and Cochrane Library databases from inception, with searches for this update including the period 1 January 2020 to 18 August 2021. Systematic review and study repositories and grey literature sources were searched in August 2021 and guidelines identified for the eCOVID19 Recommendations Map were screened (November 2021).
Selection criteria
Guidelines or reviews focusing on communication (information, education, reminders, facilitating decision‐making, skills acquisition, supporting behaviour change, support, involvement in decision‐making) related to physical distancing measures for prevention and/or control of COVID‐19 or selected other diseases (sudden acute respiratory syndrome (SARS), Middle East respiratory syndrome (MERS), influenza, Ebola virus disease (EVD) or tuberculosis (TB)) were included. New evidence was added to guidelines, reviews and primary studies included in the 2020 review.
Data collection and analysis
Methods were based on the original rapid review, using methods developed by McMaster University and informed by Cochrane rapid review guidance.
Screening, data extraction, quality assessment and synthesis were conducted by one author and checked by a second author. Synthesis of results was conducted using modified framework analysis, with themes from the original review used as an initial framework.
Main results
This review update includes 68 studies, with 17 guidelines and 20 reviews added to the original 31 studies.
Synthesis identified six major themes, which can be used to inform policy and decision‐making related to planning and implementing communication about a public health emergency and measures to protect the community.
Theme 1: Strengthening public trust and countering misinformation: essential foundations for effective public health communication
Recognising the key role of public trust is essential. Working to build and maintain trust over time underpins the success of public health communications and, therefore, the effectiveness of public health prevention measures.
Theme 2: Two‐way communication: involving communities to improve the dissemination, accessibility and acceptability of information
Two‐way communication (engagement) with the public is needed over the course of a public health emergency: at first, recognition of a health threat (despite uncertainties), and regularly as public health measures are introduced or adjusted. Engagement needs to be embedded at all stages of the response and inform tailoring of communications and implementation of public health measures over time.
Theme 3: Development of and preparation for public communication: target audience, equity and tailoring
Communication and information must be tailored to reach all groups within populations, and explicitly consider existing inequities and the needs of disadvantaged groups, including those who are underserved, vulnerable, from diverse cultural or language groups, or who have lower educational attainment. Awareness that implementing public health measures may magnify existing or emerging inequities is also needed in response planning, enactment and adjustment over time.
Theme 4: Public communication features: content, timing and duration, delivery
Public communication needs to be based on clear, consistent, actionable and timely (up‐to‐date) information about preventive measures, including the benefits (whether for individual, social groupings or wider society), harms (likewise) and rationale for use, and include information about supports available to help follow recommended measures. Communication needs to occur through multiple channels and/or formats to build public trust and reach more of the community.
Theme 5: Supporting behaviour change at individual and population levels
Supporting implementation of public health measures with practical supports and services (e.g. essential supplies, financial support) is critical. Information about available supports must be widely disseminated and well understood. Supports and communication related to them require flexibility and tailoring to explicitly consider community needs, including those of vulnerable groups. Proactively monitoring and countering stigma related to preventive measures (e.g. quarantine) is also necessary to support adherence.
Theme 6: Fostering and sustaining receptiveness and responsiveness to public health communication
Efforts to foster and sustain public receptiveness and responsiveness to public health communication are needed throughout a public health emergency. Trust, acceptance and behaviours change over time, and communication needs to be adaptive and responsive to these changing needs. Ongoing community engagement efforts should inform communication and public health response measures.
Authors' conclusions
Implications for practice
Evidence highlights the critical role of communication throughout a public health emergency. Like any intervention, communication can be done well or poorly, but the consequences of poor communication during a pandemic may mean the difference between life and death.
The approaches to effective communication identified in this review can be used by policymakers and decision‐makers, working closely with communication teams, to plan, implement and adjust public communications over the course of a public health emergency like the COVID‐19 pandemic.
Implications for research
Despite massive growth in research during the COVID‐19 period, gaps in the evidence persist and require high‐quality, meaningful research. This includes investigating the experiences of people at heightened COVID‐19 risk, and identifying barriers to implementing public communication and protective health measures particular to lower‐ and middle‐income countries, and how to overcome these.
Keywords: Humans, Communication, COVID-19, COVID-19/prevention & control, Pandemics, Pandemics/prevention & control, Physical Distancing, Public Health
Plain language summary
How can we communicate better with people and communities about measures which help to prevent and control COVID‐19?
Key messages
‐ During a pandemic, governments and other authorities need to clearly communicate with the public about how people can keep themselves safe. This communication needs to be based on trust and well‐planned. People and communities affected by the pandemic need to be involved in planning and delivering the communication. The communication should reach all people across the community, including those who have trouble reading and writing, people who speak languages other than the community's dominant language, and people who face other types of disadvantage. Clear communication can improve how well people are able to follow measures to keep themselves safe.
‐ This review identified six themes which can guide best‐practice approaches to public health communication during a pandemic. These themes are:
1) Strengthening public trust and countering misinformation;
2) Two‐way communication involving communities so that people have input into how communication can best happen;
3) Development of and preparation for public communication by considering who the audience is and how different people's needs within the community can be met;
4) Public communication features, including how and when messages are delivered to communities;
5) Supporting behaviour change at individual and population levels;
6) Fostering and sustaining receptiveness and responsiveness to public health communication over time.
‐ The review findings can help governments and other authorities make decisions about public health communication during a pandemic. The findings are relevant to COVID‐19 and future public health emergencies. The findings can be applied across different countries and different emergency situations.
‐ Some gaps in the research were found through this review. These included: communication with people who are at higher risk of getting severely sick or dying from COVID‐19; communication in lower‐ and middle‐income countries; and communication in settings known for social inequalities. Further research in these areas may help increase knowledge and improve practices related to pandemic communication.
What are physical distancing measures?
The term 'physical distancing measures' describes ways to reduce the spread of diseases such as COVID‐19 by reducing physical contact between people. Physical distancing measures include contact tracing, avoiding crowds, isolating, quarantine, and measures to reduce transmission in schools and workplaces.
What did we want to find out?
We wanted to find out which ways of communicating with the public are best to increase people's understanding and use of physical distancing measures to protect themselves and limit the spread of COVID‐19 and other similar diseases. We also wanted to find out whether there were ways of communicating that worked better for certain groups in the community, including people who experience disadvantage.
What did we do?
This review is an update of a review conducted in 2020. The 2020 review included primary studies (qualitative and quantitative) and secondary sources (review studies and guidelines).
During the searches for this update, we looked for guidelines or review studies examining communication about physical distancing measures for preventing and/or controlling COVID‐19 or selected other infectious diseases. We compared and summarised the results of included studies and guidelines, together with the findings from the 2020 review.
What did we find?
This review has 68 included studies (guidelines, reviews and primary studies [studies undertaken by researcher(s) which collect original data]). This update added 17 guidelines and 20 reviews (which are considered secondary research) to the original 2020 review.
We identified six main themes related to planning and implementing communication about physical distancing during a pandemic.
These themes can inform policy and decision‐making around pandemic and public health emergency communication. These themes are: 1) Strengthening public trust and countering misinformation; 2) Two‐way communication; 3) Development of and preparation for public communication; 4) Public communication features; 5) Supporting behaviour change at individual and population levels; 6) Fostering and sustaining receptiveness and responsiveness to public health communication.
What are the limitations of the evidence?
This update focused on reviews and guidelines. Typically, these represent the best available evidence but, in this update, were mainly rated as having low or moderate quality. Because of studies' different designs, the quality ratings are not meant to be used as a hierarchy (ranking) of evidence.
A strength of this review is that major themes and findings came from diverse sources, including primary studies, reviews and guidelines. Often, similar findings were reported across different study types, populations and settings. The findings from this updated review also build on those of the 2020 review, adding to the main findings and filling major gaps. Having similar findings across different study types, and adding new information through this update, increases our confidence in the findings even though most of the included studies are of low or moderate quality. However, since searches for new evidence last occurred in 2021, it is likely that further relevant evidence now exists.
How up‐to‐date is this evidence?
This evidence is up‐to‐date until August 2021.
Background
This review update explores the ways in which communication by governments, health organisations, clinicians and community groups have promoted and supported physical distancing to prevent and control COVID‐19. It provides a comprehensive update to a published rapid review that was commissioned by the WHO European Office in 2020 to answer an urgent question: 'What are relevant, feasible and effective communication approaches to promote acceptance, uptake and adherence to physical distancing measures for COVID‐19 prevention and control?' (Ryan 2021a).
Completed in June 2020 (with evidence current up to 1 May 2020), Ryan 2021a was produced against a backdrop of global uncertainty, fear and confusion. Little was known about transmission, treatment or the potential to vaccinate against the new virus. One of the few certainties was that strict physical distancing measures – isolation, quarantine, contact tracing, crowd avoidance, and work and school measures (Iezadi 2021; WHO 2019) – would form the cornerstone of the public health response to COVID‐19. The need to physically distance to reduce the risk of infectious disease transmission has been known since the earliest civilisations (Vitello 2022) and the need for effective public health communication to underpin these actions has not abated. As the findings of this review attest, the role of effective public health communication in supporting the early and ongoing uptake and adherence to physical distancing measures by billions of people around the world was, and remains, vital. As COVID‐19 remains a public health priority and there has been huge growth in research related to COVID‐19 over recent years, it is important that governments, public health agencies and decision‐makers have access to an updated synthesis of available evidence in order to help inform and guide communications related to the pandemic.
This review update identifies and explores relevant and timely evidence on the complex and multi‐layered task of communicating with diverse and disparate audiences about what is known and unknown, and the steps people need to take to reduce risk and protect public health over the course of a pandemic. In doing so, this review update highlights key information and implications for policy‐makers and governments to consider when planning, implementing and revising how and when to enact physical distancing measures for COVID‐19 control over time. These findings can also inform evidence‐based planning and responsiveness to future pandemics and global health crises. As the evidence confirms, the need for clear and effective public communication remains a constant.
Weighing up the evidence over time: what have we learnt
This review update reinforces the original rapid review findings (Ryan 2021a), which underlined the need for:
Clear, accurate and timely public information and actionable messages that are consistently updated.
Information about risk and what people needed to do to minimise risk both in the immediate and longer terms.
Public information conveying consistent messages expressed in clear and understandable language shared via multiple sources and dissemination pathways.
Accessible information tailored to local contexts to enhance reach, relevance and acceptability and to ensure that the needs of diverse, vulnerable and disadvantaged communities are met.
Community engagement to inform tailoring of messages to groups within populations – ensuring appropriateness to local contexts and using community feedback to improve reach and relevance.
Practical support and access to essential services (e.g. food, medicines, financial support) alongside public information and communication in order to enable people to adhere as closely as possible to physical distancing measures.
The 2020 rapid review drew on rapidly emerging information on COVID‐19 alongside evidence from influenza, SARs, MERs and other infectious outbreaks (Ryan 2021a). Since that time, there has been a deluge of COVID‐19 research. This review update, with evidence current up to 18 August 2021, includes 17 new guidelines and 20 new reviews that, taken together, fill several previous evidence gaps and add to our understanding of communication needs, practices and impacts over the short and longer terms.
Key findings in this current review update that build on the previous findings, centre on the need to:
Build and maintain trust in public agencies, which in turn supports individual and community receptiveness and adherence to ongoing public health communications.
Proactively identify and counter misinformation that continues to sow confusion and mistrust, fuel conspiracy theories and undermine/counter public health communications at local and global levels.
Involve communities at all stages of the pandemic response to improve the dissemination, accessibility and acceptability of communications about preventive public health messages.
Monitor changes in attitudes and behaviours over time that influence individual and community willingness and ability to accept and adhere to physical distancing measures.
Deliver consistent, actionable and coordinated public communications that clearly outline what is known and unknown (acknowledging uncertainty) and is responsive to changes over time.
Address multiple equity issues and challenges to ensure information and communication are tailored for and appropriate to diverse audiences, including hard to reach, vulnerable and marginalised groups (see Appendix 1 for comprehensive list).
Actively work to foster and sustain public receptiveness and responsiveness to public health communication over time.
Focus on equity and community engagement
Equity has emerged as a key theme across the WHO’s COVID‐19 key findings and policy briefings (WHO 2023), the Lancet’s Commission on Lessons for the Future of the COVID pandemic (Sachs 2022), the Cochrane Convenes global evidence summit (Cochrane 2020) and the International Red Cross’s Trust, Equity and Local Action ‐ Lessons from the COVID‐19 pandemic to avert the next global crisis (IFRC 2023). The consensus amongst leading health experts, sociologists and economists is that COVID‐19 increased existing inequalities and created additional urgent policy and healthcare issues in need of redress around the world.
It is clear that inequalities influence the degree to which individuals and populations are able to accept and adhere to preventive measures. Accordingly, the importance of public communication that recognises and is designed to counteract inequalities can’t be overstated. This is critical to supporting community‐level uptake of physical distancing measures – particularly as the effects of the pandemic disproportionately affect the poorest and most vulnerable.
In recognition of this, this review update identifies key elements of effective communication for physical distancing measures for diverse populations and groups, and applies a more consistent equity lens across the evidence. It highlights the role of community involvement, feedback and interactive engagement to inform and refine communication approaches, content and delivery over time. It is essential that information, as well as practical supports, are tailored to meet the specific needs of diverse communities, particularly underserved, vulnerable and disadvantaged groups.
Navigating pandemic fatigue and looking ahead: why this review is important
Communicating clearly with people and populations about why physical distancing measures are needed and how they can adhere to them has been a critical and consistently challenging component of COVID‐19 prevention and control globally. This updated review addresses this identified need for further understanding of effective public health communication approaches. Three years into the pandemic, people’s lives, livelihoods and forbearance have been tested beyond measure. Pandemic fatigue has set in, bringing a fresh set of challenges for effective public health communication.
Late in 2022, WHO Director Tedros Adhanom Ghebreyesus and US President Joe Biden made respective statements that the end of COVID‐19 was in sight (United Nations 2022) and that the pandemic was now over (Berger 2022). In part, these declarations reflected less about actual case numbers and mortality rates and more about the political, economic and social status quo. It is increasingly clear that people, communities and governments across the globe collectively yearn to put COVID‐19 – and the immeasurable losses from illness, isolation, closures and lost opportunities that come with it – firmly out of sight and out of mind.
Universal COVID‐19 fatigue makes the task of public health communication ever more challenging, but no less critical. The evidence in this rapid review update has direct implications for policy‐makers and governments to consider when planning, implementing and revising physical distancing measures for COVID‐19 control over time, and in the real‐world conditions we now find ourselves in. The findings may also have relevance in helping to inform and guide policy‐makers and others when planning communications in relation to future disease outbreaks and public health emergencies.
It adds another important piece to the emerging picture of what worked and what did not in preventing the spread of COVID‐19. The evidence on the role of public health communication in the pages that follow can inform our thinking on critical issues beyond physical distancing measures. It can also shape our response to the ongoing challenges of COVID‐19, and our preparedness for the future global health challenges that lie ahead.
Objectives
This review update builds on the existing rapid review commissioned by WHO to address the question: 'What are relevant, feasible and effective communication approaches to promote acceptance, uptake and adherence to physical distancing measures for COVID‐19 prevention and control?'
Therefore, the primary focus of this review update is communication approaches to promote and support acceptance, uptake and adherence to physical distancing – and not the effects of physical distancing per se.
A secondary objective, introduced in this updated version, is to explore and identify key elements of effective communication for physical distancing measures for different (diverse) populations and groups. This included, where appropriate, differential consideration or analysis of countries according to income levels (e.g. upper and middle income compared with others); or of target groups within populations (e.g. lower socioeconomic status, lower health literacy), underserved groups (e.g. people experiencing homelessness), culturally and ethnically diverse groups (e.g. migrants and refugees), specific age and demographic groups; and included consideration of the prevalence of COVID‐19 within populations over time (e.g. communication during peak times (surge/wave) versus that during lower prevalence periods).
Methods
The original rapid review (Ryan 2021a) and this updated review used methods based closely on rapid response methods developed and used by McMaster University (Wilson 2018) and informed by Cochrane rapid review methods guidance (Garritty 2021; Tricco 2020).
A protocol was developed and made publicly available before the updating process began (Ryan 2021b). Please refer to this for detailed methods, a brief summary of which is provided here. Any changes to the methods from those described in the protocol are noted.
Please also see Table 1 for a list of abbreviations used throughout the review.
1. Abbreviations used in this update.
| AGREE II: Appraisal of Guidelines for Research & Evaluation II tool AMSTAR: A Measurement Tool to Assess Systematic Reviews BAME: Black, Asian and minority ethnic CASP: Critical Appraisal Skills Programme CCM: child contact management CDC: Centres for Disease Control and Prevention CHW: community health worker COI: conflict of interest CT: contact tracing ECE: early care and education ECDC: European Centre for Disease Prevention and Control EEA: European Economic Area ERC: emergency risk communication EU: European Union EVD: Ebola virus disease FAQ: frequently asked questions FTTIS: find, test, trace, isolate, support GL: guideline GOARN: Global Outbreak Alert and Response Network GPS: global positioning system H1N1: H1N1 influenza strain HCW: health care worker HIV: Human Immunodeficiency Virus IFRC: Internation Federation of Red Cross and Red Crescent Societies IHE: institute of higher education LMIC: lower‐ and middle‐ income country MERS: Middle Eastern respiratory syndrome N/A: not applicable NGO: non‐goverment organisation NICE: National Institute for Clinical Excellence NIHR: National Institute for Health Research NPI: non‐pharmaceutical intervention OECD: Organisation for Economic Co‐operation and Development PD: physical distancing PH: public health PHAC: Public Health Agency Canada PHM: public health measures PHSM: public health and social measures PPE: personal protective equipment PTSD: post‐traumatic stress disorder QES: qualitative evidence synthesis QR: quick response RCCE: risk communication and community engagement RCT: randomised controlled trial SAGE: Scientific Advisory Group for Emergencies SARS: Sudden acute respiratory syndrome SES: socioeconomic status SIM: subscriber identity module SMS: short message/ messaging service SPI‐B: Scientific Pandemic Influenza Group on Behaviours SR: systematic review TB: tuberculosis THL: Finnish Institute for Health and Welfare UAE: United Arab Emirates UNICEF: United Nations International Children's Emergency Fund WHO: World Health Organization |
Eligibility criteria for this review update
Types of study design
We had planned to consider eligible studies in two phases (refer to Appendix 2 for details):
Phase 1 (synthesised evidence sources; focusing on COVID‐19, SARS, MERS, influenza, Ebola (EVD), or TB): guidelines (country‐specific, global or regional), systematic reviews (intervention reviews, qualitative syntheses, mixed‐methods reviews).
Phase 2 (primary studies; focusing on COVID‐19 only): single studies on COVID‐19 if there were gaps in the evidence derived from guidelines or reviews (i.e. primary studies that provided new knowledge not found in identified synthesised evidence sources), including observational studies, controlled trials, qualitative studies (any empirical method (i.e. based on observation or measurement of phenomena)), mixed‐methods research.
At the screening stage, we identified a large volume of synthesised evidence (i.e. guidelines, systematic reviews) eligible for inclusion. We, therefore, decided to stop screening at Phase 1 and formulate this update as an overview of synthesised evidence sources.
Population and context
Consistent with the original rapid review (Ryan 2021a), studies focussing on physical distancing measures for prevention and/or control of COVID‐19 or other selected infectious diseases (SARS, MERS, influenza, EBV or TB) were included. We focused on communication to promote physical distancing measures outside healthcare settings, i.e. measures put in place in community settings, including workplaces and schools. All countries were eligible, irrespective of income level or geographic location.
Types of intervention
To be included, studies must have focused on the intersection between communication and physical distancing measures. Communication with individuals, organisations, communities and/or systems was included.
Physical distancing measures (contact tracing, isolation, quarantine, crowd avoidance, school and work measures) were defined based on WHO definitions for pandemic influenza control (WHO 2019); see Table 2 for definitions.
2. Definitions of physical distancing measures considered by this review update.
| Contact tracing | The identification and follow‐up of persons who may have come into contact with an infected person, usually in combination with quarantine of identified contacts. |
| Crowd avoidance | Measures to reduce virus transmission in crowded areas/mass gatherings, including restrictions on gatherings, and approaches for individual distancing in homes, shops, workplaces, public transport and public places. |
| Isolation | Reduction in virus transmission from an ill person to others by confining symptomatic individuals for a defined period either in a special facility or at home. |
| Quarantine | Isolation of individuals who contacted a person with proven or suspected viral illness, or travel history to an affected area, for a defined period after last exposure, with the aim of monitoring them for symptoms and ensuring the early detection of cases. |
| School measures | Closure of schools when virus transmission is observed either in the school or community, or an early planned closure of schools before virus transmission initiates. |
| Work measures, including closures | Measures to reduce virus transmission in the workplace, or on the way to and from work, by decreasing the frequency and length of social interactions. May include closure of workplaces when virus transmission is observed in the workplace, or an early planned closure of workplaces before virus transmission initiates. |
Definitions of physical distancing measures taken from WHO 2019
Communication in the context of physical distancing was defined as that undertaken for one or more of the following purposes (Hill 2011; Kaufman 2017; Ryan 2014):
Information/education.
Reminding.
Facilitating communication or decision‐making.
Enabling communication.
Acquiring skills.
Supporting behaviour change.
Being supported.
Involving the community in decision‐making for the promotion of physical distancing.
The following were excluded:
Methods of enhancing community ownership of non‐pharmaceutical intervention (NPI) measures.
Personal support (e.g. individual psychosocial support).
Strategies for minimising risks/harms to individuals/communities, without a focus on communication of physical distancing measures (e.g. informing individuals about the importance of ‘flu' vaccination in the context of the COVID‐19 pandemic).
Implementation and/or effects of physical distancing measures, without an identifiable communication element (e.g. effectiveness of physical distancing measures themselves).
Modelling of effectiveness scenarios (e.g. effectiveness of quarantine at preventing viral transmission).
Mobile/digital health applications without an explicit focus on physical distancing measures and related communication.
Knowledge of pandemic risks and/or risk perceptions without a focus on physical distancing measures.
Public/consumer information materials on physical distancing.
Types of outcome(s)
We sought qualitative and quantitative data on outcomes for individuals and communities, broadly aligned with the following major categories:
Acceptance;
Uptake;
Adherence;
Feasibility and related outcomes.
Studies were not excluded based on outcomes sought or outcome measures reported.
Search methods for identification of studies
An Information Specialist (AP) designed and ran all searches, which were informed by a content expert, independently peer reviewed and updated from the original 2020 search methods designed to identify all relevant physical distancing measures. Previous keyword choices had been peer‐reviewed by Robin Featherstone (then Information Specialist, Cochrane Evidence Production & Methods Directorate) and Andrew Booth (University of Sheffield).
Electronic databases
For the original rapid review (Ryan 2021a), we searched electronic databases from inception to 1 May 2020. For this review update, we searched the MEDLINE, Embase and the Cochrane Library databases from 1 January 2020 to 18 August 2021:
Cochrane Central Register of Controlled Trials (CENTRAL; 2021, Issue 8), in the Cochrane Library (Appendix 3);
Embase Classic (1947 to 2021 week 33) (Appendix 4); and
MEDLINE via Ovid (1946 to 18 August, 2021) (Appendix 5).
Please refer to Table 3 for all search details.
3. Search activities and dates.
| Database | Date searched |
| CAMARADES COVID‐19 SOLES | 24 Aug 2021 |
| CDC | 24 Aug 2021 |
| Cochrane Library | 18 Aug 2021 |
| Cochrane study Registry COVID‐19 | 24 Aug 2021 |
| ECDC | 24 Aug 2021 |
| Embase Classic + Embase 1947 to 2021 August 18 | 18 Aug 2021 |
| Epistemonikos COVID‐19 | 25 Aug 2021 |
| Google Scholar | 18 – 25 Aug 2021 |
| Health Systems Evidence | 25 Aug 2021 |
| Lit COVID | 25 Aug 2021 |
| Ovid MEDLINE(R) ALL 1946 to August 19, 2021 | 18 Aug 2021 |
| MedRixv | 31 Aug 2021 |
| NICE | 25 Aug 2021 |
| PDQ Evidence | 25 Aug 2021 |
| PubMed | 24 Aug 2021 |
| WHO Global research on COVID‐19 | 31 Aug 2021 |
| Web of Science (citing references) | 1 Sep 2021 |
All records were downloaded to an Endnote library. Duplicates from the previous publication’s search (Ryan 2021a) were removed from the database records. As when undertaking the original review, the Cumulated Index to Nursing and Allied Health Literature (CINAHL) and PsycINFO were assessed before the searches were conducted. Both were judged as not having sufficiently unique references and, so again, were not searched in this update.
Guidelines
The eCOVID19 Recommendations Map (https://covid19.recmap.org/; eCOVID‐19 RecMap) team supplied us with spreadsheets of all the organisational guidelines screened for the COVID‐19 Living Catalogue of Guidelines in November 2021.
Other searches
Reference lists of key studies were searched, together with searches for citing articles about key studies. Key informants were also consulted for additional sources of relevant evidence.
For studies available but not yet peer‐reviewed (e.g. MedRivx), the lack of peer review was noted in the quality assessment. For pre‐prints included in the original review, we checked the publication status and verified the data extracted against any subsequently published peer‐reviewed articles.
We also searched a range of online databases and grey literature (see Table 3). Relevant keywords were chosen for each of the websites. Full search terms and strategies for the online databases and grey literature are available from the authors upon request.
At the time of publication, approximately 24 months had elapsed since running searches for this update. We did not update the searches to identify more recently available evidence as it was beyond our resourcing to do so. This high‐level synthesis draws on a very large volume and range of literature related to COVID‐19 as well as other selected diseases, with the purpose of informing current public health communications and future pandemic preparedness planning. The methods and approach adopted are therefore different to usual Cochrane review methods but tailored to providing a rigorous review of evidence for decision‐makers.
Screening
Decision rules operationalising the selection criteria were developed and refined iteratively by two review authors (RR, CS). One author (RR) screened all titles and abstracts for eligibility. All records identified as potentially relevant were retrieved for full‐text assessment. A second reviewer (CdMM) independently checked 20% of excluded records.
Two review authors (RR, CS) screened all full‐text articles, with discrepancies resolved by discussion to reach consensus.
We handsearched the list of guidelines from eCOVID‐19 RecMap. One author (RR) screened titles, and two authors (RR, CS) screened full‐text copies of all potentially‐relevant guidelines to determine eligibility.
Studies excluded at the full‐text screening phase for this update are reported in Characteristics of excluded studies, with reasons for exclusion. Full‐text studies excluded from the original review are available at opal.latrobe.edu.au/articles/dataset/Studies_excluded_from_Ryan_et_al_2021/20436261.
We did not exclude studies based on the language of the publication. All potentially eligible non‐English language abstracts progressed to full‐text assessment, and methods were translated to determine eligibility, where possible.
As part of Phase 1 screening, included guidelines and reviews were mapped systematically against major themes identified in the original review by a single reviewer (RR) and checked by a second reviewer (CS, BM, CdMM, LS). All six themes were well‐populated with evidence, and major gaps that had been identified in the original review were addressed by the addition of more recent evidence (school and work measures; measures for vulnerable populations including those at heightened risk of severe disease; communications related to alterations of public health measures). Accordingly, screening was halted at Phase 1, and primary studies were not considered further in the review.
Inclusion of ongoing or unpublished studies
We assessed studies identified as pre‐prints in the original rapid review, identifying one (Atchison 2020, cited April 3, 2020) subsequently published in 2021. The published and pre‐print versions were cross‐checked, and while several small changes were identified in the 2021 publication, none affected data extracted from the pre‐print version.
Data collection and analysis
Data extraction and quality assessment
Data were extracted from included studies by one author (RR) and verified by a second author (CS, BM, CdM, LS), including quality assessments. Included studies were appraised using established tools (for guidelines, AGREE II (Brouwers 2010); for systematic reviews, AMSTAR (original tool) (Shea 2007)). Where available from reliable databases, quality ratings were extracted directly, with acknowledgement of the assessment source.
For studies identified from handsearching of eCOVID‐19 RecMap, the eCOVID‐19 Rec Map Critical Appraisal Team critically appraised eligible guidelines independently in duplicate using the AGREE‐II tool. Inter‐rater item differences of 3 points or greater were flagged as a conflict. All conflicts were resolved through discussion with the help of the critical appraisal coordinator, as needed.
We did not contact the study authors to request more information related to missing data. In the protocol, we noted that any such efforts would concentrate on primary research studies (Ryan 2021b). Given that our methods for selecting studies changed during the review, this step was no longer a priority. We did, however, contact authors of forthcoming reviews (protocols) that were judged as eligible for inclusion. We requested access to the review (if completed) and/or information about the likely timing of the full review becoming available.
Review Manager (RevMan) was used to collate and report all elements of the review using a flexible review format. Data tables, once verified, were added to RevMan directly as Appendix 6. Other review information and data was entered into RevMan by one reviewer (RR) and checked for accuracy by a second reviewer (AV, CS).
Data synthesis
Data were systematically extracted and tabulated in the first instance to transparently and consistently present key features and findings of the included evidence, including quality assessments, in a structured way (Campbell 2020). Data were extracted, and findings mapped to each component of the review question (e.g. acceptance, adherence). There was then a second translational step to identify the communication purpose and how this might affect interpretation of the study findings (Campbell 2020).
For the original review, included studies were mapped to each component of the review question and grouped for analysis. In the analysis, we considered population features, intervention characteristics (i.e. characteristics of the communication intervention or issue), and contextual factors or implementation issues. Data were standardised by identifying major thematic categories. We used modified framework analysis (Ritchie 1994) for analysing data in the original review, informed by methods described in Tricco 2017 (primarily Chapter 4). Findings from both qualitative and quantitative research were analysed concurrently, and six themes were identified (see Appendix 7).
These themes provided the guiding framework for synthesising newly identified evidence in this update, allowing for new categories to emerge through the analysis.
The quality of studies informing each section of findings was systematically assembled and presented alongside the thematic findings in all cases. We also identified and discussed any limitations of the assembled evidence and potential biases in the review process.
At the protocol stage (Ryan 2021b), we planned to investigate and identify key elements of effective communication for physical distancing measures for different (diverse) populations and groups. Data on these features (e.g. income levels, population features such as socioeconomic status) were collected and systematically assembled and used to inform the development of themes (e.g. identification of findings related to particular groups at a disadvantage and/or who may require specific consideration related to communication, such as migrants and refugees). We also sought to identify communication approaches targeting individual members of the public and report these separately from community‐level (public health) communication.
At each stage of synthesis (identifying major thematic categories and subcategories of data, analysing the findings and considering other factors such as intervention and population features), we developed clear decision rules to ensure consistency across the author team. Training and support were provided by the original author team members.
A single reviewer (RR), with work checked by a second reviewer (CS, AV), undertook each synthesis step. At least one senior member of the original author team (RR, SH) was involved in the oversight or conduct of the review at all stages of synthesis (for all data) to ensure consistency and accuracy of the data and analyses. In addition, members of the review team provided key input at critical points of the synthesis. For example, input from co‐authors was sought upon preliminary development of the themes for this update. Co‐authors' feedback critically shaped the scope and language of themes and subthemes as well as the structure and order of the findings.
We planned to explore the possibility of quantitative outcomes for statistical analyses. However, none were identified in the data for this update.
Results
Description of studies
Results of the search
Searches of databases and grey literature sources identified 6845 records after deduplication. Screening of titles and abstracts identified 1517 records for full‐text screening. At this stage, the decision was taken to include only synthesised evidence sources (reviews and guidelines) in this review update. As a result, 1355 primary studies were excluded from the full‐text assessment. A total of 162 records were identified as systematic reviews or guidelines for full‐text screening.
Screening of a further 412 records in eCOVID19 RecMap identified 151 guidelines for full‐text assessment.
In total, 313 (162 + 151) reviews and guidelines were assessed for eligibility in full text. Of these, 267 were excluded. Seven studies are outstanding (5 awaiting classification, 2 awaiting translation), with two ongoing at the time of searching and screening; see Figure 1.
1.

PRISMA flow diagram to illustrate our study selection process for this update
The current review update includes 68 studies. Of these, 31 were from the original rapid review (Ryan 2021a). We added 37 new studies (17 guidelines and 20 reviews) in this updated version. One included review was empty (Moya‐Salazar 2021) and so is not reported further.
Of the reviews included, five (1 from the original review (Eaton 2020) and 4 newly included (Berg 2021; Majid 2020; Mobasseri 2020; Noone 2021)) were scoping, rather than systematic, reviews. These were included as it was judged that they contributed relevant, important evidence, for instance, communication issues related to unique population groups (older people Mobasseri 2020), health authorities' considerations of modes for pandemic communication with the public (Berg 2021), or identification of determinants of physical distancing behaviour uptake and adherence related to communication about these measures (e.g. beliefs, knowledge, skills) (Lunn 2020).
Included studies are summarised in data tables (see Appendix 6), reporting all relevant information for each of the included studies as an updated map of evidence addressing the review objectives previously presented in Ryan 2021a. Each study's data table presents the following information:
Study characteristics.
Study findings.
Results of quality assessment.
Mapping and translational steps. These were undertaken as part of the synthesis of results and represent intermediate steps, translating the study findings to communication purpose and the review's objectives.
Disease context
The original rapid review included 31 studies conducted during the COVID‐19 era and those on selected infectious diseases (influenza, SARS, MERS, EBV and TB). All the 17 primary studies (12 cross‐sectional surveys, one randomised controlled trial (RCT), one cohort study and three qualitative studies) focused on COVID‐19. For the 14 systematic reviews and guidelines, synthesised evidence was based on studies of pandemic influenza, particularly related to the 2009 H1N1 pandemic influenza outbreak (n = 7), EVD (2), SARS (2), TB (2) and MERS (1).
Of the 37 systematic reviews and guidelines added to this review update, 31 focussed on COVID‐19; the remaining six drew on research that was not COVID‐19‐specific, but the research was explicitly conducted in the context of the current pandemic outbreak.
Geographic location and income level
Geographically, included studies were spread across the world and from all continents. For details, please refer to Appendix 6.
However, most included studies (48/68) were drawn either exclusively or predominately from high‐income countries (according to World Bank classifications), with only nine from low‐ and middle‐income countries. Of these, several focused on EVD (largely from countries in West Africa; Congo, Guinea, Liberia, Senegal and Sierra Leone) or TB (including Ethiopia, India, Indonesia, Malawi, South Africa, Peru and selected higher‐income countries). Several guidelines and reviews (n = 10) included evidence drawn from several countries across income brackets, and many sought studies or evidence from a range of countries.
Target of communications
In the original review, much of the evidence was directed at the population level and focused on public pandemic risk messaging, including information to the public or specific groups within populations to promote physical distancing measures.
In this update, we again planned to attempt to identify communication approaches targeting individual members of the public and report these separately from community‐level (public health) communication. However, most included studies again dealt with general, community‐level communication (approximately three quarters; 72%). We did find, however, that in newly identified studies, a number (10 guidelines and reviews) focused on communication with specific vulnerable groups. Three guidelines specifically focused on vulnerable groups (ECDC 2020a; ECDC 2020b; WHO 2021), while other guidelines and reviews included a general population scope but specifically identified vulnerable groups within this (PHAC 2021; PHAC 2022; Sopory 2021); or focused on one or more groups requiring tailored communication (e.g. non‐English speaking groups and EVD survivors (Gilmore 2020), vulnerable groups (Cardwell 2021), older adults and/or those with comorbidity or of lower socioeconomic status (Mobasseri 2020; Regmi 2021)). Themes in the data relating specifically to vulnerable groups were identified in our analysis.
In the protocol (Ryan 2021b), we planned to investigate and identify key elements of effective communication for diverse populations and groups, including countries according to income level; target groups within populations (such as those based on socioeconomic levels); health literacy; hard(er)‐to‐reach groups; culturally, linguistically and ethnically diverse groups; and any other relevant features, such as age. We also aimed to identify populations defined by COVID‐19 prevalence over time (e.g. communication during peak times (surge/wave) versus that during lower prevalence periods).
We extracted all such information where available, and identified these groups and information relevant for shifting public health measures in the presence of changing COVID‐19 levels within communities in our analysis. Findings related to these groups were identified naturally in the data. Findings related to specific groups and changing requirements of public health communication over time are reflected throughout the thematic results.
Excluded studies
Studies excluded based on title and abstract screening were checked by a second reviewer: of the 4918 studies excluded at the preliminary screening stage, 984 (20%) were checked by a second reviewer. In total, 10 studies were queried, and half (5) were re‐included in the group of primary studies to be assessed in full text as phase 2 citations (no longer considered eligible for inclusion in this update). These checks indicated a high level of agreement between reviewers about selection decisions, and that potentially‐relevant studies were unlikely to have been mistakenly excluded by a single reviewer conducting title and abstract screening.
Studies excluded at the full‐text screening stage are reported with reasons in Characteristics of excluded studies. Studies were more often excluded because they lacked an identifiable focus on communication; had insufficient intersection between communication and physical distancing measures; focused on clinical/infection control; or were set primarily in health systems or services (non‐community settings).
Studies screened in full text and excluded from the original review are not reported here but are available at: https://opal.latrobe.edu.au/articles/dataset/Studies_excluded_from_Ryan_et_al_2021/20436261.
Quality of included studies
An overview of the quality ratings of included studies (original review and this update) is provided in Table 4, with a more detailed breakdown of ratings provided in Table 5. A detailed quality assessment can be found for each study within the data tables provided in Appendix 6. We report quality assessments of studies contributing data to each theme and subtheme in the results, to convey an indication of the volume, type and quality of the evidence underpinning all findings. However, the quality assessments are not intended to be used as a hierarchy of evidence, as this was neither possible nor appropriate with the mix of included research (i.e. qualitative and quantitative, primary and synthesised evidence sources). Rather, this information on quality is provided with the aim of informing interpretation and implementation of the findings.
4. Overview of included studies and quality ratings (original review and this update).
| Guidelines | Systematic reviews | Primary studies | |
| Original review (Ryan 2021a) | 3 | 11 | 17 |
| Cochrane update | 17 | 20* | 0 |
| Total included | 20 Quality (AGREE II):
|
31* Quality (AMSTAR):
|
17 Quality (design‐specific tools):
|
* One included review was empty (Moya‐Salazar 2021) and was therefore not assessed for quality or considered further in this update.
AMSTAR ratings categorised as follows (scored out of 11): 1‐4 low, 5‐7 moderate, 8+ high‐quality
AGREE II ratings categorised as follows (mean scores across 6 domains): < 40% low, 40 to < 70% moderate, 70%+ high‐quality
5. Included studies and ratings of methodological quality.
| Physical distancing measure | Study ID (type of study) | Quality, assessment tool |
| Contact tracing | Chung 2021(SR)# | Low, AMSTAR |
| Gilmore 2020(SR)#^ | Moderate, AMSTAR | |
| Heuvelings 2018 (SR)* | Moderate, AMSTAR | |
| Khorram‐Manesh 2021(SR)# | Moderate, AMSTAR | |
| Megnin‐Viggars 2020(SR)# | High, AMSTAR | |
| Saurabh 2017 (SR)* | Low, AMSTAR | |
| Szkwarko 2017 (SR)* | Moderate, AMSTAR | |
| Bodas 2020 (survey)# | Low‐moderate | |
| Isolation | WHO 2021(GL)# | Moderate, AGREE II |
| Cardwell 2021(SR)#^ | Moderate, AMSTAR | |
| Chu 2020(SR)#^ | Moderate, AMSTAR | |
| ECDC 2020b(GL)# | Moderate&, AGREE II | |
| ECDC 2020a(GL)# | Low, AGREE II | |
| Mao 2021(SR)# | Moderate, AMSTAR | |
| Mobasseri 2020(scoping review)# | Low, AMSTAR | |
| Regmi 2021(SR)# | Moderate, AMSTAR | |
| Seale 2020(SR)# | Low, AMSTAR | |
| WHO 2020c(GL)# | Moderate, AGREE II | |
| Burnet 2020 (qualitative)# | Moderate, CASP | |
| Burnet 2020a (qualitative)# | Moderate, CASP | |
| Farooq 2020 (survey)# | Low | |
| Qazi 2020 (survey)# | Low | |
| Quarantine | Brooks 2020 (SR)*^ | Low%, AMSTAR |
| Gomez‐Duran 2020(SR)#^ | Moderate, AMSTAR | |
| Lin 2014 (SR)* | Moderate, AMSTAR | |
| Sopory 2021(qualitative, SR)#^ | High, AMSTAR | |
| Webster 2020 (SR)#^ | Moderate, AMSTAR | |
| WHO 2021b(GL)# | Low, AGREE II | |
| Zhu 2020 (survey)# | Moderate | |
| School measures | Brooks 2020a (SR)*^ | Low%, AMSTAR |
| CDC 2022(GL)# | Low, AGREE II | |
| CDC 2022a(GL)# | Low, AGREE II | |
| CDC 2022b(GL)# | Low, AGREE II | |
| DES 2020(GL)# | Low, AGREE II | |
| Work measures | ‐ | ‐ |
| Crowd avoidance, including individual physical distancing measures | ECDC 2020(GL)# | Low, AGREE II |
| NACCHO 2006 (guideline)+* | Moderate, AGREE II | |
| PHAC 2021(GL)# | Low, AGREE II | |
| PHAC 2021a(GL)# | Low, AGREE II | |
| Teasdale 2014 (SR, qualitative)* | Moderate, AMSTAR | |
| Tooher 2013 (SR)* | High, AMSTAR | |
| WHO 2020b(GL)# | Moderate, AGREE II | |
| Eaton 2020 (scoping review)*^ | Low, AMSTAR | |
| Lor 2016 (qualitative)* | Moderate, CASP | |
| Atchison 2020 (survey)# | Moderate | |
| Briscese 2020 (survey)# | Moderate | |
| Clements 2020 (survey)# | Low | |
| Kwok 2020 (survey)# | Low‐moderate | |
| Lohiniva 2020 (qualitative)# | Moderate, CASP | |
| Lunn 2020 (RCT)# | Moderate, CASP | |
| Meier 2020 (survey)# | Low‐moderate | |
| Roy 2020 (survey)# | Low | |
| Zhong 2020 (survey)# | Low | |
| General | Bekele 2020(SR)# | Moderate, AMSTAR |
| Berg 2021(scoping review, rapid)# | Low, AMSTAR | |
| ECDC 2020g (review of guidelines)# | Low, AMSTAR | |
| Gupta 2021(SR)# | Low, AMSTAR | |
| JHCHS 2019 (guideline)* | Moderate, AGREE II | |
| Li 2020(SR)# | Moderate, AMSTAR | |
| Majid 2020(scoping review) #^ | Low, AMSTAR | |
| Noone 2021(scoping review, rapid)# | High, AMSTAR | |
| PHAC 2022(GL)# | Low, AGREE II | |
| Sarria‐Guzman 2021(SR)# | Low, AMSTAR | |
| WHO 2017 (guideline)* | High, AGREE II | |
| WHO 2020(GL)# | Low, AGREE II | |
| WHO 2020a(GL)# | Low, AGREE II | |
| WHO 2021a(GL)# | Low, AGREE II | |
| Lim 2020 (survey)# | Moderate |
# COVID‐19‐specific, #^ included research not COVID‐19‐specific but review conducted explicitly in the context of the current pandemic outbreak, *non‐COVID‐19‐specific study
Bold text indicates new studies added in this update.
AMSTAR ratings categorised as follows (scored out of 11): 1‐4 low, 5‐7 moderate, 8+ high‐quality
AGREE II ratings categorised as follows (mean scores across 6 domains): < 40% low, 40 to < 70% moderate, 70%+ high‐quality
&AGREE II overall rating calculated based on mean of 3 domains (1, 3, 6) rather than all 6 domains of the tool
% AMSTAR rating from McMaster Health Forum (via Health Systems Evidence https://www.healthsystemsevidence.org)
The quality of the included studies varied. Half (34/68) of all included studies were rated as of high or moderate quality based on the tools applied. This means that shortcomings in the design and/or conduct of many included studies are present and that findings should be interpreted with recognition that limitations in the assembled research exist.
Results of the synthesis
Themes identified in the framework analysis
From the synthesis of the data, six major themes emerged. These were derived from the six themes originally identified by Ryan 2021a that served as a guiding framework for the synthesis (Appendix 7), but were substantially adapted on the basis of newly included evidence and based on feedback by the wider author team. The ordering of the themes was also modified based on decisions by the team after considering the themes and subthemes emerging from preliminary analysis.
Evidence assembled in this update addressed a number of key knowledge gaps identified in the original review and added significantly to the findings in several key areas. This included the need for ongoing communication over time during a pandemic, particularly to reflect changes to risk and to public health measures; the requirements for tailoring and flexibility of public information and communication; the need to explicitly and carefully consider the needs of vulnerable groups within communities; and the need for systems to support the critical role of community engagement in mounting an effective public health communication response.
Original themes were therefore substantially modified by the inclusion of new findings emerging through the framework analysis. For instance, data previously contributing to and synthesised under a theme of physical distancing measures in schools and workplaces (original theme 6) were judged as aligning to findings within other major themes. A new major theme, on sustaining and maintaining public health communication and behaviour change, emerged with the inclusion of new evidence, and themes were re‐organised to reflect a more intuitive progression of communication purposes ‐ from building public trust through communication, engagement of communities in pandemic response and communications, through to the more specific elements (timing, content and tailoring) of public health communications and the maintenance of these and preventive behaviours over time.
The six major themes emerging from the data with newly‐included evidence are as follows:
Theme 1 Strengthening public trust and countering misinformation: essential foundations for effective public health communication;
Theme 2 Two way‐communication: involving communities to improve the dissemination, accessibility and acceptability of information;
Theme 3 Development of and preparation for public communication: target audience, equity and tailoring;
Theme 4 Public communication features: content, timing and duration, delivery;
Theme 5 Supporting behaviour change at individual and population levels;
Theme 6 Fostering and sustaining receptiveness and responsiveness to public health communication.
Findings of the synthesis
Public information and risk communication during the response to a pandemic are essential and critical components of the public health response to an outbreak. The evidence assembled to date again highlights that communication between authorities and governments and the public can be done well or poorly. To be most effective at promoting uptake of and adherence to protective measures, such as physical distancing measures, communication needs to be based on trust and planned ahead of time, engage communities meaningfully, and incorporate several key features including those related to content, timing, tailoring and reach within communities.
The findings of this update are organised under six major themes, within which subthemes emerging from the evidence are identified. The quality of the evidence on which the findings are based is also provided to aid with interpretation of the findings within each theme.
Theme 1: Strengthening public trust and countering misinformation: essential foundations for effective public health communication
Public trust in the authorities is an essential component of communication.
See Figure 2 for a summary of evidence quality for these findings.
2.
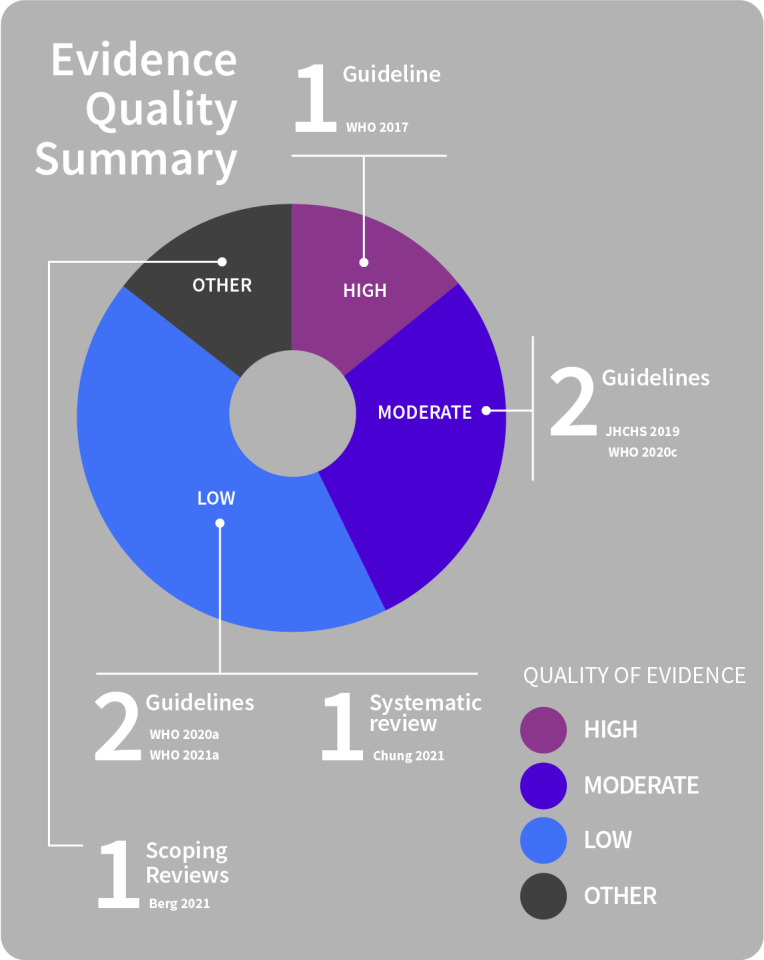
Public trust
Public trust is an essential element of effective communication before, during and after a pandemic outbreak (Berg 2021; JHCHS 2019; WHO 2017). The need to build and maintain public trust is mentioned directly or implied by several of the findings of this review, as it can be built or eroded by the approaches to or consequences of physical distancing or the communication approach taken.
Ideally, public trust in authorities is established and consolidated prior to an outbreak, or prior to introduction of or changes to public health measures (Berg 2021; WHO 2020a; WHO 2021a), but this is not always the case. Governments and authorities need to be mindful that building and maintaining trust amongst the population is essential when planning communication related to a pandemic (Chung 2021; WHO 2020c; WHO 2020a; WHO 2021a), as this is critical for promoting adherence to public health advice and increasing the effectiveness of preventive measures (WHO 2020c).
Facilitators of public trust
See Figure 3 for a summary of evidence quality for these findings.
3.
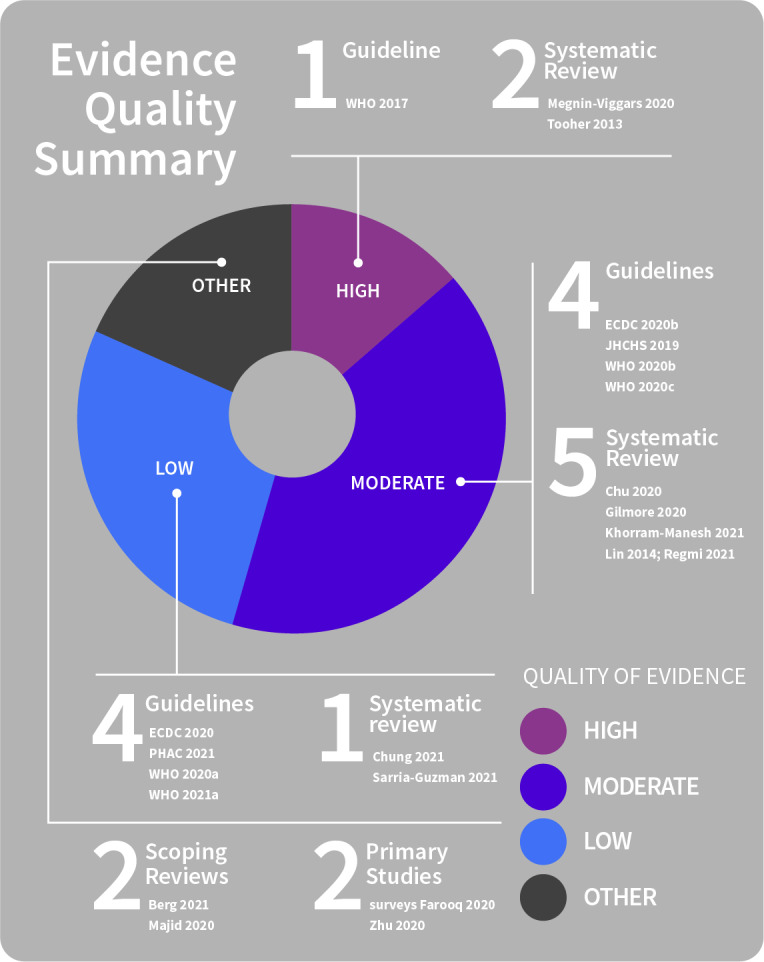
Facilitators of public trust
Several factors positively influence people’s trust of public health messaging and consequently, their adoption of and adherence to preventive behaviours.
Providing clear, timely and consistent (i.e. not conflicting or contradictory) information about risk, physical distancing measures and rationale for the measures that is accessible and disseminated widely through different media and channels helps to build public trust (Berg 2021; Chu 2020; Chung 2021; ECDC 2020b; Farooq 2020; Gilmore 2020; JHCHS 2019; Majid 2020; Megnin‐Viggars 2020; PHAC 2021; Regmi 2021; Sarria‐Guzman 2021; WHO 2017; WHO 2020a; WHO 2020b; WHO 2020c; WHO 2021a).
Findings also show:
Conflicting information from different levels of government, or between governments and authorities, needs to be avoided as this undermines public trust.
Governments and authorities need to regularly communicate epidemiological data to the public to build trust, particularly as measures change over time (WHO 2021a).
To build and sustain trust, communication from the authorities needs to clearly and transparently convey what is known and what is not (uncertainty), as well as the commitment to base decisions on the best available scientific knowledge at any time (ECDC 2020; Majid 2020; PHAC 2021; WHO 2020a; WHO 2020c).
As the pandemic continues, so does uncertainty. Clear, consistent public health communication that acknowledges this can help to mitigate the negative impact of uncertainty, without undermining trust (Chung 2021; Majid 2020; WHO 2020c).
Trust in information sources may also be associated with more accurate knowledge of risk and adoption of protective behaviours (Berg 2021; Regmi 2021; WHO 2021a). Promoting person‐centred, community‐led approaches may increase trust and social cohesion, so improving the feasibility of implementing preventive measures and adherence to them (WHO 2020c; WHO 2021a).
Higher trust in the ability of governments and public officials to work to control a pandemic outbreak and to ensure protection of privacy and personal information are also associated with greater likelihood of the recommended actions (e.g. engagement with contact tracing) being willingly engaged with, and adopted, by the community (Berg 2021; Chung 2021; Farooq 2020; JHCHS 2019; Khorram‐Manesh 2021; Lin 2014; PHAC 2021; WHO 2017; Zhu 2020).
Barriers to public trust
See Figure 4 for a summary of evidence quality for these findings.
4.
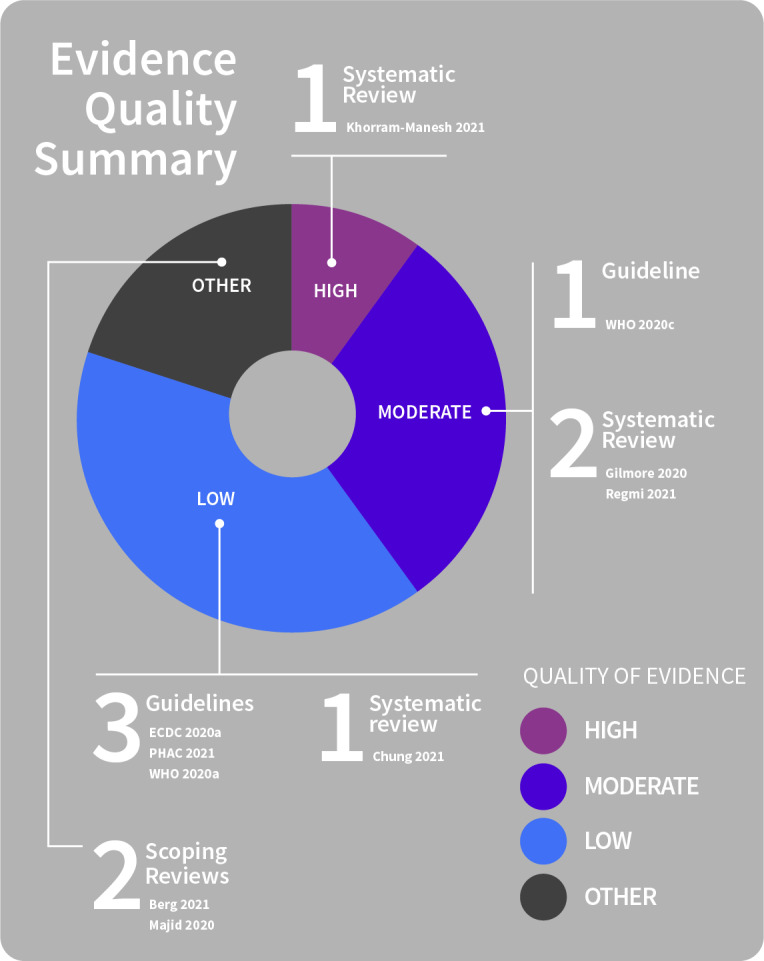
Public trust barriers
In addition to recognised contextual, social, and financial barriers to preventive behaviours, erosion of public trust is also key and can negatively influence people’s uptake of and adherence to preventive messaging and measures. These include conspiracy beliefs or mistrust of government or other organisations (Chung 2021; Gilmore 2020; Megnin‐Viggars 2020; WHO 2020c); mistrust or worries about accuracy of information reported by the media, including social media (Gilmore 2020; Majid 2020); and worsening inequalities, with the pandemic affecting the poorest and most vulnerable disproportionately (ECDC 2020a; WHO 2020c; see Appendix 1 for a comprehensive list of people identified as vulnerable during COVID‐19).
Findings also show:
Public health messaging that includes overstatements or exaggerations, that fosters fear, appeals to authority, repeats myths or misinformation (even where the aim is to counter with factually accurate information), or relies heavily on statistical information is generally less trusted and therefore less effective at promoting adherence to preventive measures (PHAC 2021).
Information that challenges or contradicts misconceptions, and is communicated from a trusted source, may reduce misconceptions if the communication is coherent (Majid 2020; Regmi 2021; WHO 2020a).
Frequent, drastic changes in reporting may be perceived as inaccurate by the public and lead to a loss of trust (Majid 2020), as may the reporting of inaccurate information (Berg 2021; Majid 2020).
Identifying and addressing misinformation
See Figure 5 for a summary of evidence quality for these findings.
5.
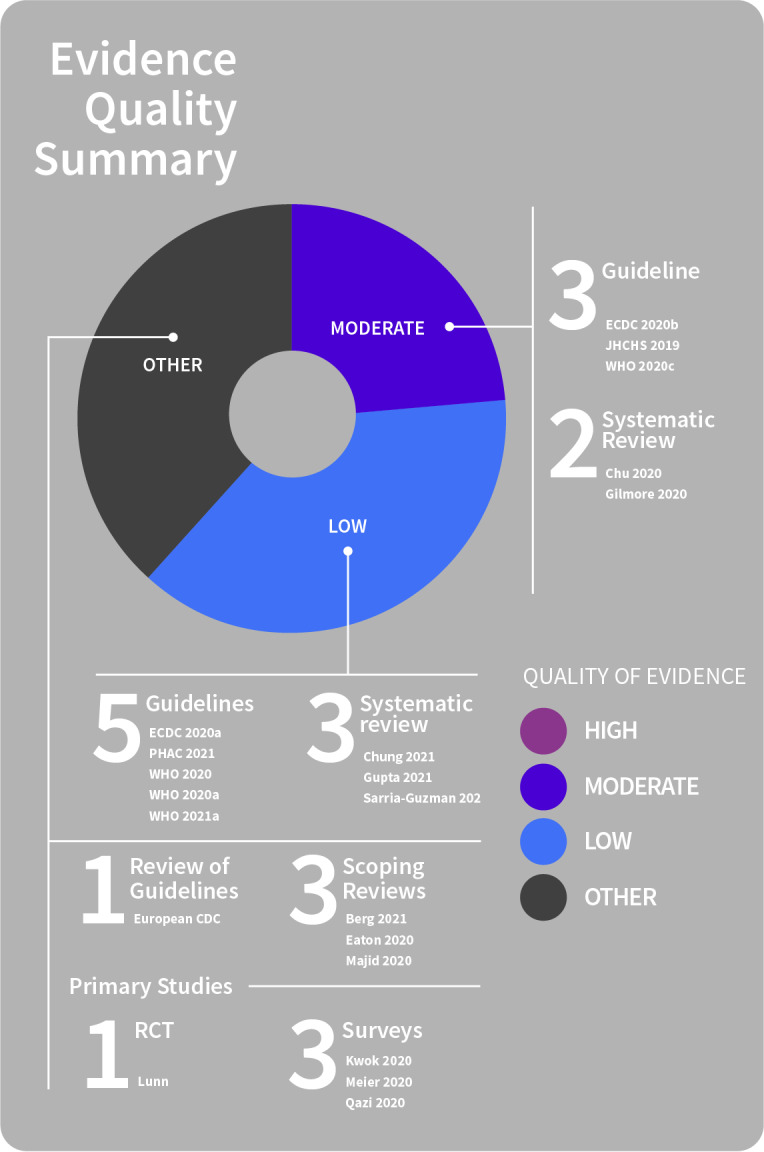
Misinformation
Identifying sources of misinformation
During pandemics, both accurate and inaccurate information spread quickly. It is not yet clear how communities navigate between accurate knowledge that promotes protective behaviours and inaccurate information that does not (Majid 2020).
Commonly accessed information sources may contribute to the spread of misinformation, fears, rumours, and misconceptions about required preventive measures and pandemic risks throughout the general public. This can negatively affect people’s adoption of preventive measures and prevent people from seeking medical care (ECDC 2020b; Gupta 2021; Majid 2020; WHO 2020a).
Misinformation from different sources can circulate alongside accurate information. This may be due to:
a lack of access and availability of accurate information (forcing people to seek alternative, less reliable sources of information);
inadequacy of information from reliable sources to support informed decisions regarding adoption of preventive measures; or
conflicting or contradictory public health messages (Majid 2020; Sarria‐Guzman 2021).
Even where members of the public are knowledgeable about an outbreak, many also actively seek information from diverse sources (Eaton 2020; Kwok 2020; Majid 2020; Meier 2020; Qazi 2020; Sarria‐Guzman 2021). Public access to information sources is a determinant of use. While perceived trustworthiness may also influence frequency of use, high exposure (frequency of use) to a particular information channel does not necessarily correspond with high levels of trust in information received via the channel. For example, use of online sources and social media platforms is high and growing, but trust in these channels is typically low, whereas traditional media and government sources are used less frequently despite being regarded as trustworthy (Kwok 2020; Majid 2020; Qazi 2020; WHO 2020c). Other research suggests that, in some studies, communication by traditional media is seen as alarmist and inaccurate, exaggerating or sensationalising risk information (Berg 2021; Majid 2020).
Some sources, specifically social media, may be more prone to spreading inaccurate information or misinformation about pandemic risks than others. Countering this (misinformation, rumours and contradictory messages) spread via social media remains problematic for health authorities (Berg 2021). Additionally, people may not verify information they receive via social media or their social networks (Berg 2021; Majid 2020; Sarria‐Guzman 2021).
Addressing misinformation
Proactive monitoring for rumours and misinformation is essential. It is critical that health authorities and the media adopt co‐ordinated strategies to identify and counter misinformation, as this may otherwise spread rapidly and negatively affect adherence to preventive measures (Berg 2021; Majid 2020; PHAC 2021; Sarria‐Guzman 2021; WHO 2020; WHO 2020a; WHO 2020c).
Ongoing public health messaging built on clear, accurate, and consistent information is needed to proactively build trust, clarify misconceptions and address misinformation (ECDC 2020b; Gilmore 2020; Majid 2020; PHAC 2021; WHO 2020a; WHO 2020c).
Co‐ordinated management of misinformation and information overload is needed as these may otherwise grow in the absence of available or accessible information or in the presence of conflicting messages (Majid 2020). For example, different health agencies or levels of government might actively work together to address common issues and use consistent messaging.
Providing the right information at the right time, to the right people via trusted, credible channels (e.g. community and faith leaders) is critical in helping to build public understanding and consensus about behaviours, such as physical distancing, to mitigate risk (Chu 2020; ECDC 2020a; Gilmore 2020; Gupta 2021; Majid 2020; PHAC 2021; WHO 2020c; WHO 2021a).
Strengthening the capacity for local and national media to identify and address misinformation may help to ensure consistent messages are communicated (PHAC 2021; WHO 2020c). Building trusted relationships between authorities and the mass media, or authorities engaging effectively with social media, may also build trust (Berg 2021).
Misconceptions may be more common amongst those with less trust of the government or authorities; therefore, community leaders, healthcare providers, the media and government all play an important role in communicating accurate, consistent information about disease and required health protection measures during a pandemic (Chung 2021; Majid 2020; Regmi 2021). Introducing information that contradicts misconceptions may be helpful, but this depends on the source and format of the information and on the level of trust people have in the source. Such information may help to counteract the negative effects of misconceptions on behaviours. However, it requires more cognitive work from people to process information at a higher level to inform their decisions and behaviours. This may delay the adoption of protective behaviours or increase the adoption of ineffective behaviours, lead to information overload and negative emotional states (Majid 2020).
Additionally, putting in place mechanisms to monitor, address misinformation and rumours, and respond to questions or feedback from the public (e.g. mass and social media, hotlines), is important in order to monitor how knowledge, beliefs, practices and behaviours change (Gilmore 2020). Public communication/information needs to be updated after analysis of public risk perceptions and adjusted in response to help promote uptake of public health advice and reduce mental health issues (Gilmore 2020; Regmi 2021; WHO 2020; WHO 2020a; WHO 2020c; WHO 2021a). Part of the role of such a system may be to identify or monitor for areas of uncertainty, inaccuracy or misinformation, as well as common questions in the public realm. This may in turn help to identify opportunities to address misinformation and allow the delivery of tailored communications (WHO 2017; WHO 2020; WHO 2020a; WHO 2021a).
Theme 2: Two‐way‐communication: involving communities to improve the dissemination, accessibility and acceptability of information
Community involvement is key in response planning, dissemination and reach of messages.
See Figure 6 for a summary of evidence quality for these findings.
6.
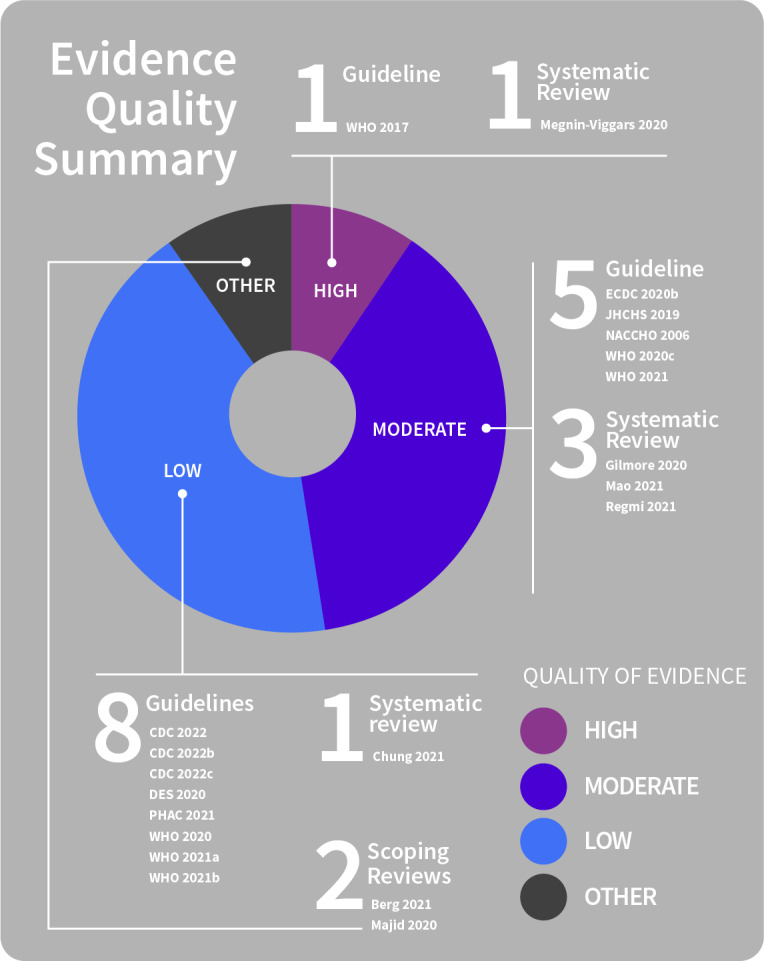
Community involvement in messaging
During a public health emergency, communication of information and advice is a critical public health intervention. The public, healthcare providers and other stakeholders all require trustworthy and accessible (language and literacy level) information to be available in a timely way in order to be able to protect their own and others’ health (PHAC 2021).
Physical distancing uptake, feasibility, acceptability and adherence are influenced by an array of cultural, geographic and economic factors. These include structural features (e.g. social context, living conditions, resources and services), traditions, sociocultural norms, the need for social interaction and access to space. Perceived norms are an important factor but vary across countries, as do other factors such as carer responsibilities (e.g. lower levels of distancing because of caring duties outside the home) (WHO 2020c; WHO 2021b).
Community involvement is needed to address barriers and to promote acceptability and adherence to preventive measures (WHO 2020c; WHO 2021b), and might be based on the two‐way participatory partnership approaches used successfully in past outbreaks (ECDC 2020a; WHO 2020c).
Working with the community is key to understanding local contexts (people’s needs, concerns, attitudes and beliefs, and barriers to implementing measures) and identifying localised solutions (CDC 2022b; Megnin‐Viggars 2020; WHO 2020; WHO 2021). Without community involvement, misinformation, confusion and mistrust can undermine public health efforts (WHO 2020c).
Involving the community helps to ensure an informed and appropriate person‐centred response by:
Gathering information on knowledge and behaviours (e.g. preferred information sources and formats) (CDC 2022b; Megnin‐Viggars 2020; PHAC 2021; Regmi 2021; WHO 2020; WHO 2020a; WHO 2020c; WHO 2021);
Developing (designing) and implementing appropriate messaging related to measures (information, education, communication) (Gilmore 2020); and
Tailoring the supports needed to follow public health measures (PHAC 2021; Regmi 2021).
Community involvement is also critical for identifying the ways people might respond in a crisis that are different from those that were predicted (NACCHO 2006). Community trust is built from sustained two‐way community engagement that is evidence‐based, communicated via trusted sources, and is responsive to community feedback (i.e. monitoring knowledge, beliefs and practices/beliefs and changes over time, and adapting course as needed) (ECDC 2020b; Gilmore 2020; JHCHS 2019; PHAC 2021; WHO 2017; WHO 2020c; WHO 2021a). However, this requires structures and processes to be in place (e.g. participatory governance, mechanisms for involving communities in policy and intervention design). This may be a key consideration for organisations when planning pandemic preparedness processes and structures (WHO 2020c).
Findings also show:
Two‐way community engagement is most effective if started early, if it is ongoing as information changes, and occurs through multiple channels. This can help to promote better understanding of the sociocultural context in which disease prevention and control efforts are needed (Gilmore 2020; WHO 2020a; WHO 2020c).
Community involvement is needed in all stages of local COVID‐19 responses: planning, design, implementation, monitoring, and evaluation (WHO 2020c; WHO 2021a).
Planning and decision‐making related to introduction or adjustment of public health measures needs to be undertaken collaboratively with local and regional leadership with the aim of balancing community needs and the benefits of measures against potential harms (CDC 2022; CDC 2022a; CDC 2022b; Gilmore 2020; PHAC 2021; WHO 2021a).
If stricter measures are needed, the impact of these need to be balanced against the positive and negative effects for the community, as a whole and for individuals. If measures are lifted, implications for transmission must be well understood, and adequate health systems and measures put in place to minimise risk to vulnerable people (WHO 2021a).
Incorporating community members into planning, response and monitoring activities of pandemic management teams is needed, with plans widely disseminated within communities to promote support (Gilmore 2020; WHO 2020c).
Strengthening and support of authorities for community involvement is needed by providing guidance and tools for best practice community engagement; developing strategies to address stigma/discrimination, pandemic fatigue and to build trust; and by co‐ordinating efforts to manage the infodemic and build health and digital literacy (WHO 2020c). Capacity and local solutions to control the pandemic and mitigate the impacts also need to be supported through mentoring, technical support and resource sharing with local groups. Explicitly recognising local expertise and ensuring it is central to community engagement efforts (building on existing relationships and established trust) is key. Considerations need to include identifying required skills in different contexts (e.g. participatory approaches, facilitation and co‐ordination, data collection/analysis); assessing the need for technical support and capacity building (including training and training resources (adaptable to culture, language, format, accessibility); and strengthening capacity for local and national media to identify and address misinformation (WHO 2020c)).
Additionally, community engagement and dialogue can strengthen alternate channels for communication (e.g. local networks, community leaders). This can improve the reach of important preventive messages, including to groups most affected by the pandemic (e.g. vulnerable and underserved groups)(CDC 2022b; JHCHS 2019; Mao 2021; NACCHO 2006; PHAC 2021; WHO 2017; WHO 2020; WHO 2021). It can also underpin mechanisms for providing meaningful feedback from the community to authorities about the relevance and value of communications in order to improve subsequent communications and information (ECDC 2020; Mao 2021; WHO 2020; WHO 2020a; WHO 2020c; WHO 2021; WHO 2021a) and to monitor knowledge, beliefs and behaviours (Berg 2021; Chung 2021; ECDC 2020b; Gilmore 2020; WHO 2021a), prevention barriers (ECDC 2020b; Majid 2020) and address rumours, misinformation and queries (WHO 2020a).
Promising models might aim to build local capacity by working with community leaders to promote appropriate behaviours, as well as signposting, practical instructions, and linking behaviours to social norms (ECDC 2020b). Disseminating information (including about COVID‐19 prevention and when to seek care), addressing concerns and promoting dialogue on specific needs of groups, such as those with lower literacy, visual, intellectual or other impairments may also be useful (WHO 2021). Community champion schemes, where volunteers are provided with the most recent information (including infographics in community languages) on COVID‐19 to share with their community (Mao 2021), or working with local community networks to build capacity and train local leaders may also be beneficial (WHO 2021a).
Specific settings, such as schools (defined inclusively here to mean kindergarten to high school, early childhood education settings, institutes of higher education), need to engage effectively with their local communities (staff, parents/guardians and other partners (e.g. health centres)) to plan preventive measures, ensure that diverse community needs are taken into account and work collaboratively (with state, tribal, local health and other officials) to implement guidance (CDC 2022; CDC 2022a; CDC 2022b). Ongoing engagement to provide information to diverse groups within school communities, and to ensure ongoing two‐way communication and support mechanisms are in place, adapted as circumstances change, is essential for managing school settings (DES 2020).
Community involvement underpins effective tailoring of measures and communications.
See Figure 7 for a summary of evidence quality for these findings.
7.
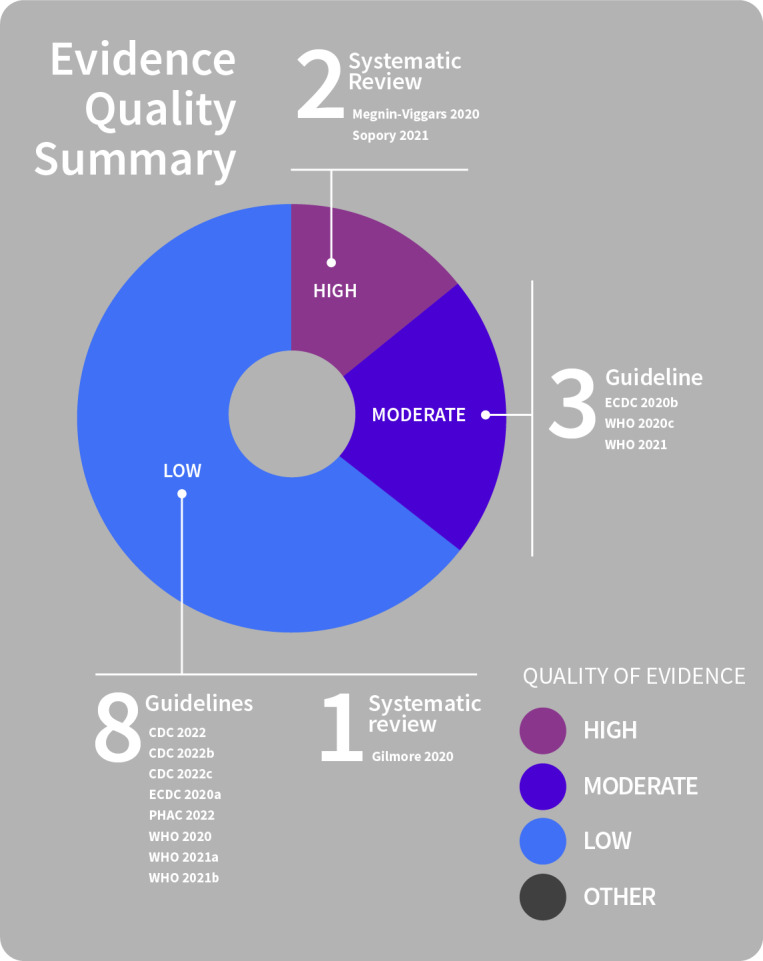
Community involvement in tailoring
Public health measures and the communications related to them must be flexible and responsive over time; calibrated to local setting and context (e.g. intensity of community transmission); reviewed regularly; adapted to the local community; and tailored to the characteristics of the intended audience (e.g. socioeconomic status, gender, age, caregiving responsibilities) (PHAC 2021; WHO 2020).
Interventions to directly control COVID‐19 need to be balanced with strategies to limit short‐ and long‐term impacts on health and socioeconomic well‐being (e.g. those arising from loss of income, loss of services) that might arise from restrictions. Unintended negative impacts of measures need to be identified and managed alongside policies to maintain essential services (healthcare, essential goods, income, human rights) (WHO 2020).
Findings also show:
Communication on preventive measures needs to be developed with communities in whom the measures are to be enacted or adjusted, so promoting uptake of measures that fits with local community needs, including those of diverse groups (CDC 2022; CDC 2022a; CDC 2022b; ECDC 2020b; Megnin‐Viggars 2020; PHAC 2021; WHO 2020c; WHO 2021a). This is critical so that people understand their risk and can access actionable information to make informed decisions about how to reduce their risk (ECDC 2020b; WHO 2020; WHO 2020a).
Key information needs to be conveyed to the community through clear, simple language and messages that encourage information sharing, focus on actionable messages about what people can (rather than what they cannot) do, and emphasise personal responsibility and the role of each person in preventing disease and saving lives (ECDC 2020b; PHAC 2021; WHO 2020; WHO 2021).
Lack of appropriate tailoring can undermine messages and the uptake of or adherence to public health measures. These include lack of contextual/cultural understanding (e.g. social norms, traditions, customs, and beliefs pervasive within the specific context); lack of engagement with appropriate actors; inconsistent and confusing messaging and/or misinformation; lack of trust in government, media and organisations; inadequate training, support structures, resources or incentivisation; unclear responsibilities; and weak infrastructure or broader contextual conflict (e.g. poverty) (ECDC 2020b; Gilmore 2020).
Lack of, or insufficient, tailoring of communications and protective measures can also mean that vulnerable groups are not adequately considered in decision‐making (see Appendix 1 for list of vulnerable groups in the context of COVID‐19). There is a need for recognition and acceptance that imposing quarantine on vulnerable groups (e.g. poor, people experiencing homelessness) requires greater modification of standard processes and awareness that greater harms (psychological, social and financial) are possible (Sopory 2021).
Community engagement may help to identify people who are vulnerable (those with less agency to comply with physical distancing measures) and their range of specific needs (CDC 2022; PHAC 2021; WHO 2020c; WHO 2021). Deliberate efforts to ensure that vulnerable people are represented and engaged throughout the planning, communication and implementation of protective health measures are needed (CDC 2022; CDC 2022a; CDC 2022b; ECDC 2020a; Sopory 2021; WHO 2020c; WHO 2021a). This helps to ensure the acceptability, sustainability and effectiveness of chosen approaches; to avoid unintended effects (harms)(ECDC 2020a); and enable information sharing and feedback on the relevance and value of communications to help address inequalities (ECDC 2020a; PHAC 2021).
Theme 3: Development of and preparation for public communication: target audience, equity and tailoring
Target audience and setting for communications
See Figure 8 for a summary of evidence quality for these findings.
8.
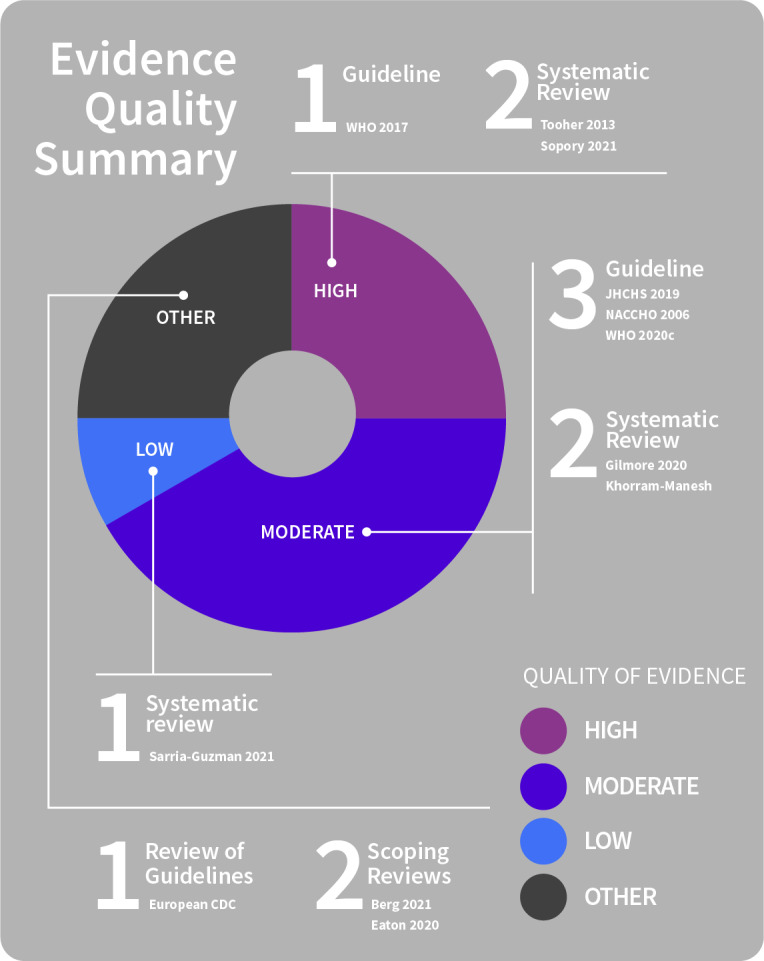
Communication audience and setting
Public communications about physical distancing measures must take into account the context, settings, and different audiences in a population because these factors influence adherence (Berg 2021; Khorram‐Manesh 2021; Sopory 2021). This does not mean that different messages (i.e. saying different things) need to be communicated: rather, it means that communication has to be planned to take into account the complexity of any audience and the groups within one population (Gilmore 2020; Sopory 2021). Decisions about implementing physical distancing measures, and communicating with the public about pandemic health threats and the importance of behavioural mitigation measures need to consider that the strategies themselves and the communications about them (e.g. delivery mode) must be appropriate to context and setting (Berg 2021; ECDC 2020g). Including in communications details specific to communities, such as information about for who, when, where, and how measures are to be implemented are critical elements (Khorram‐Manesh 2021).
Comprehensive risk communication strategies, informed by knowledge of the affected community, are therefore needed, alongside strategic planning efforts to ensure that:
The diverse needs of different groups within a population can be met (Sopory 2021);
Different audiences can be targeted (Eaton 2020; ECDC 2020g; Gilmore 2020; JHCHS 2019; NACCHO 2006; Tooher 2013); and
Information is sufficient to support informed decisions regarding adoption of preventive measures (Sarria‐Guzman 2021).
Example: schools as a setting for pandemic communication
See Figure 9 for a summary of evidence quality for these findings.
9.
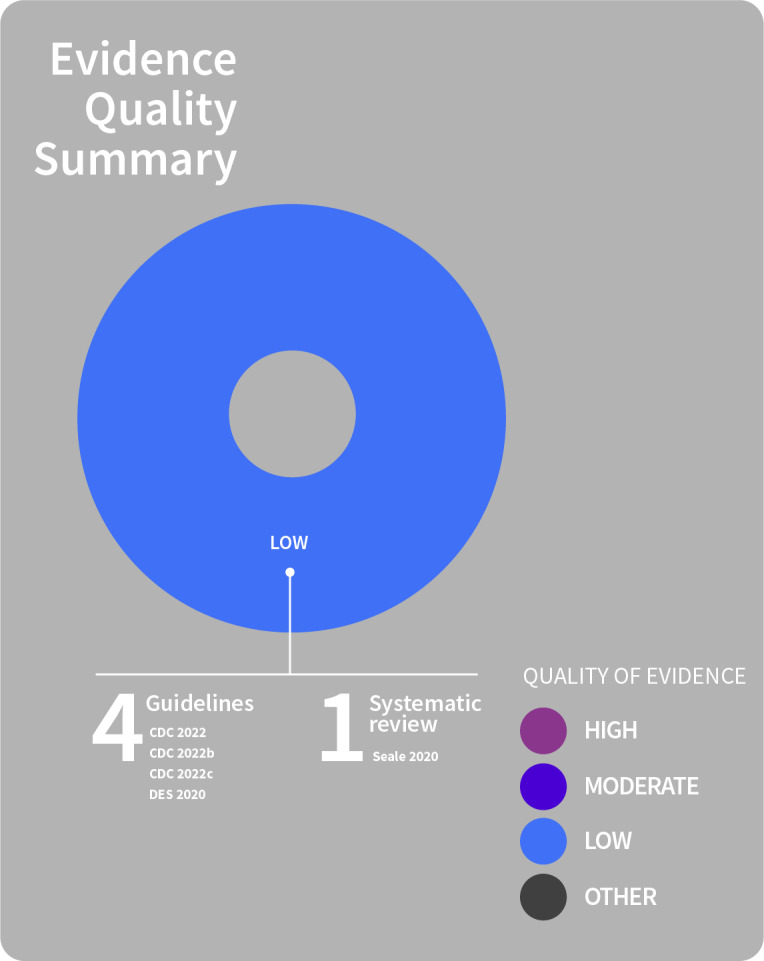
School settings for pandemic communication
To support safety within schools, a significant shift is required behaviourally, with all members of the community playing their part to keep everyone safe (e.g. respecting physical distancing practices and minimising social contact). A clear rationale for the measures needs to be widely communicated from schools to the school community, so that people understand the reasons for the measures and the risks involved. Key public health advice messages conveying clear and actionable information need to be communicated and reinforced throughout the school community so that people are aware of what to do to protect themselves and others, of the need to adhere to measures as schools re‐open, and of the need to continue to observe preventive measures, including as measures change, to support schools to stay open (CDC 2022a; DES 2020; Seale 2020).
There is a need for frequent, easy‐to‐understand communication and training for staff (CDC 2022a; CDC 2022b). Communication from schools to families and to staff is required, using clear, accessible communication materials and channels; in a language, literacy level and format that accommodates diverse audiences, including staff members, families and children, people with disabilities, and those with limited proficiency in the dominant community language (CDC 2022; CDC 2022a; CDC 2022b).
In schools and early childhood education services, in particular, layered preventive approaches (i.e. multi‐faceted measures such as physical distancing together with mask wearing and good ventilation) may be needed to keep students and staff safe, as physical distancing may not always be possible. Information about these measures and their role in protecting the health of students and staff needs to be clearly communicated within schools and to the wider school community (CDC 2022; CDC 2022a). The benefits and importance for students of in‐person learning mean that safely returning to classrooms is a priority. Implementing layered prevention strategies is therefore key to protecting all, rather than excluding students from in‐person learning (CDC 2022a).
Implementation of layered preventive approaches needs to be developed and supported with an understanding of the community’s needs (CDC 2022; CDC 2022a). Each school district and school needs to have a plan in place to protect students, teachers, staff and families (CDC 2022; CDC 2022a) that considers social and behavioural factors that might influence transmission risk and the feasibility of different prevention strategies in the school community (CDC 2022a).
Such plans might include:
Signage in highly visible locations, and communication with students and staff (via social media and email) to inform them of prevention strategies, including physical distancing (CDC 2022b);
Physical markers to remind cohorts or individuals to maintain an appropriate distance in communal areas (e.g. tape on floor, wall signs)(CDC 2022);
Behavioural techniques such as modelling and reinforcing desired behaviours, and using approaches such as picture schedules, timers, visual cues, and positive reinforcement to help children to adjust (CDC 2022). Staff and students could also be provided with virtual training on prevention strategies, policies and procedures (CDC 2022b).
A range of support is needed to assist schools to implement prevention strategies and communicate effectively about them. This might include strategies such as staff training, age‐appropriate information posters with key health messages, and communication guidance. For students, parents and school communities, support might include information provided via different channels; and, for schools more broadly, might include strategies such as a webpage for transparent information sharing, or an educational department team to support schools with information and requests (DES 2020).
A staff member or office should be given responsibility for responding to COVID‐19 concerns and notifying teachers, staff and families of students who were close contacts as soon as possible after notification of a positive case (CDC 2022a; CDC 2022b). Schools need to encourage families to monitor children for symptoms of an infectious illness and report new cases to the school and to public health authorities (CDC 2022a; CDC 2022b). Schools also need to provide information about when people should stay home and when they can safely return (CDC 2022; CDC 2022a; CDC 2022b).
The ongoing nature of the pandemic means that schools need to be flexible and prepared to provide continuity of learning and teaching, as a contingency for future closures. This includes being prepared to communicate with students, teachers and staff, and to promote communication between them, should the need arise in response to public health advice (DES 2020).
Tailoring of communications
See Figure 10 for a summary of evidence quality for these findings.
10.
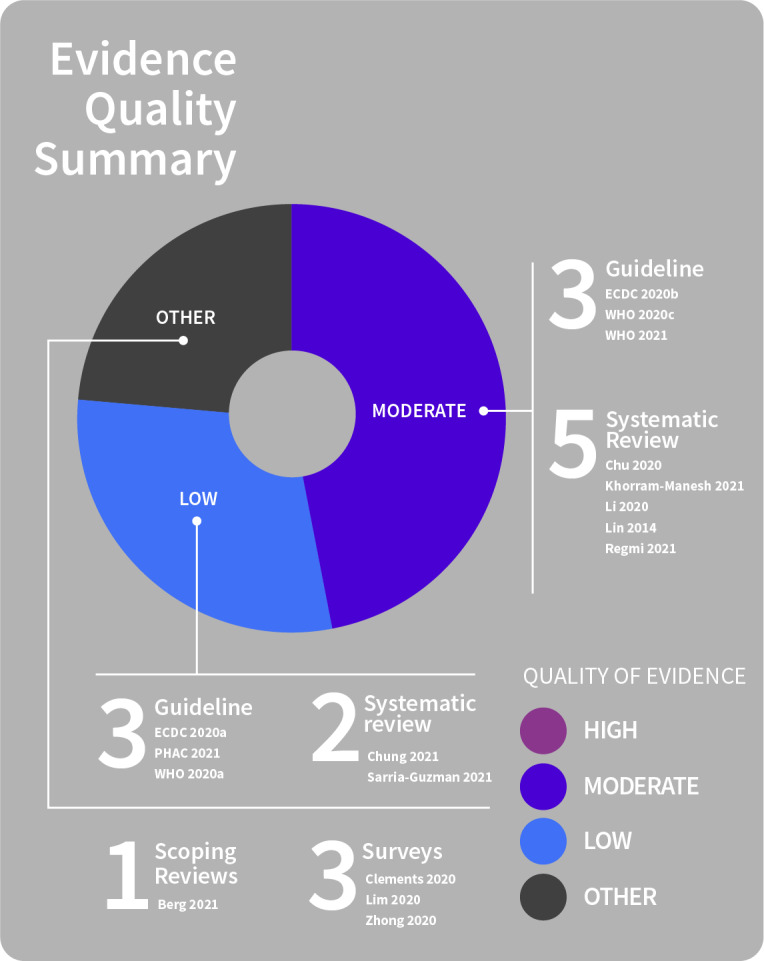
Communication tailoring
Tailoring of public health communications plays a critical role in reaching and informing more of the community, including those for whom information access may be unequal (Berg 2021; ECDC 2020a; Khorram‐Manesh 2021; PHAC 2021; Sarria‐Guzman 2021; WHO 2021). Clear, structured communication of reliable health information can also be tailored to people experiencing information overload and to manage the infodemic, and to build digital health literacy (Lim 2020; WHO 2020c).
Recognising population groups who are more likely to be non‐adherent to preventive measures can help public health policy‐makers to identify target populations for pandemic prevention and education efforts. Public health education may be more effective if it targets groups more at risk of low knowledge and risky behaviour (Clements 2020; Lin 2014; Sarria‐Guzman 2021).
Acceptance, uptake, and adherence to physical distancing measures are also determined by personal characteristics such as socioeconomic status, ethnicity, culture, age, and gender (e.g. men tend to leave the house to socialise more often than women; risk may be more common in those with fewer resources) (Berg 2021; Lim 2020; WHO 2020c). Surveys undertaken during the COVID‐19 pandemic, for example, indicate that knowledge, attitudes, and preventive practices towards COVID‐19 may be lower amongst younger people (up to 29 years) and amongst those with lower incomes (Clements 2020; Zhong 2020). Public health communication strategies that specifically target particular groups may therefore help to provide actionable information that people can use to protect their health (Berg 2021; Li 2020). Collaboration between health authorities and communities, using trusted spokespeople, may help improve the tailoring and accessibility of communications (Berg 2021; PHAC 2021).
Findings also show:
Particular groups within the community may lack adequate knowledge about emerging diseases and that the information provided to them may be inadequate to meet their needs. Therefore, there is a need for communication strategies and information that are specifically tailored to target different groups (Berg 2021; Li 2020; PHAC 2021; Regmi 2021; Sarria‐Guzman 2021).
Tailoring might include developing communication campaigns collaboratively with community members, altering the communication mode (e.g. community radio, mailouts, posters), and considering whether messaging from familiar or trusted individuals (e.g. Elders, First Nations physicians) may be appropriate (PHAC 2021).
Information delivery needs to be adjusted (e.g. sign language for people with disabilities or visual communication (e.g. infographics) for people with low literacy) (ECDC 2020b; WHO 2021) to ensure accessibility (ECDC 2020b), provided via a range of formats, follow accessibility standards (written in clear, non‐technical language)(Berg 2021; Chung 2021; WHO 2020a; WHO 2020c), and be disseminated through several channels (mass media, digital, written) (ECDC 2020b; PHAC 2021). Communicators must also be appropriately skilled and trained (Berg 2021; PHAC 2021; WHO 2020a).
Pretesting tailored messages for acceptability and accuracy of understanding is needed with members of the intended audience, with awareness that some people within the community may not be able to access or use standard resources (PHAC 2021). Working to ensure that messages are both appropriate (acceptable) and effective (accurately understood) (Chu 2020; ECDC 2020a; WHO 2020c), is key (see also theme 2 on community engagement).
General equity considerations in communication
See Figure 11 for a summary of evidence quality for these findings.
11.
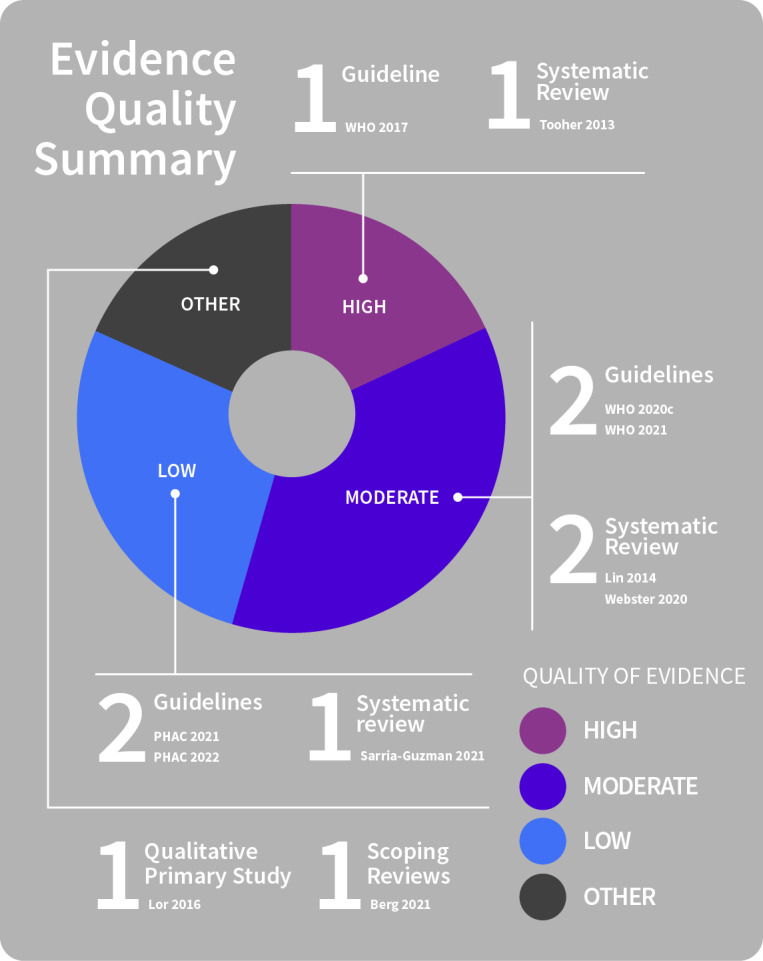
Equity in communication
Several factors influence community awareness of public health messages related to a pandemic, which, in turn, influences acceptance, uptake and adherence (Lin 2014; Lor 2016; Webster 2020). Public health communications intending to inform populations about pandemic disease and physical distancing measures need to take account of such factors to ensure that communication is as equitable and achieves as much reach as possible within communities. The need to communicate comprehensively and clearly to a population, as well as to specific groups within the community, arises because knowledge and adoption of preventive behaviours are not evenly distributed. In doing so, the groundwork is laid to help to ensure the greatest possible uptake of and adherence to preventive measures and so mount a consistent pandemic response (Berg 2021; Lin 2014; Lor 2016; PHAC 2021; WHO 2021).
Many inequalities exist and can importantly influence acceptance, uptake, and adherence to preventive measures and the correct use of measures (PHAC 2021). Some are structural or societal inequalities, which need to be addressed through political or societal decisions to support physical distancing measures, such as the provision of financial support to those unable to work, particularly for those from disadvantaged or vulnerable groups. However, the importance of public communication which deliberately recognises and plans to counteract inequalities cannot be overstated, as this is critical for community‐level uptake of physical distancing measures, and the effects of the pandemic thus far are known to disproportionately affect the poorest and most vulnerable (Sarria‐Guzman 2021; WHO 2020c; WHO 2021).
Communications must also be designed and adapted to reach those groups who are less likely or less able to take up preventive measures, or who are less likely to be reached by traditional public health communications, so that information and communication inequalities are not amplified (Berg 2021; PHAC 2021; PHAC 2022; Tooher 2013; WHO 2017).
Equity issues for specific population groups
As well as general equity considerations, there are several imbalances commonly identified in the literature (underserved and vulnerable populations, those speaking languages other than the community’s dominant language, people with lower educational levels and those for whom physical distancing may be particularly difficult to reconcile with cultural practices). Such inequities need to be explicitly recognised and addressed when planning and implementing physical distancing measures (PHAC 2021; WHO 2020c).
Underserved and vulnerable populations
See Figure 12 for a summary of evidence quality for these findings.
12.
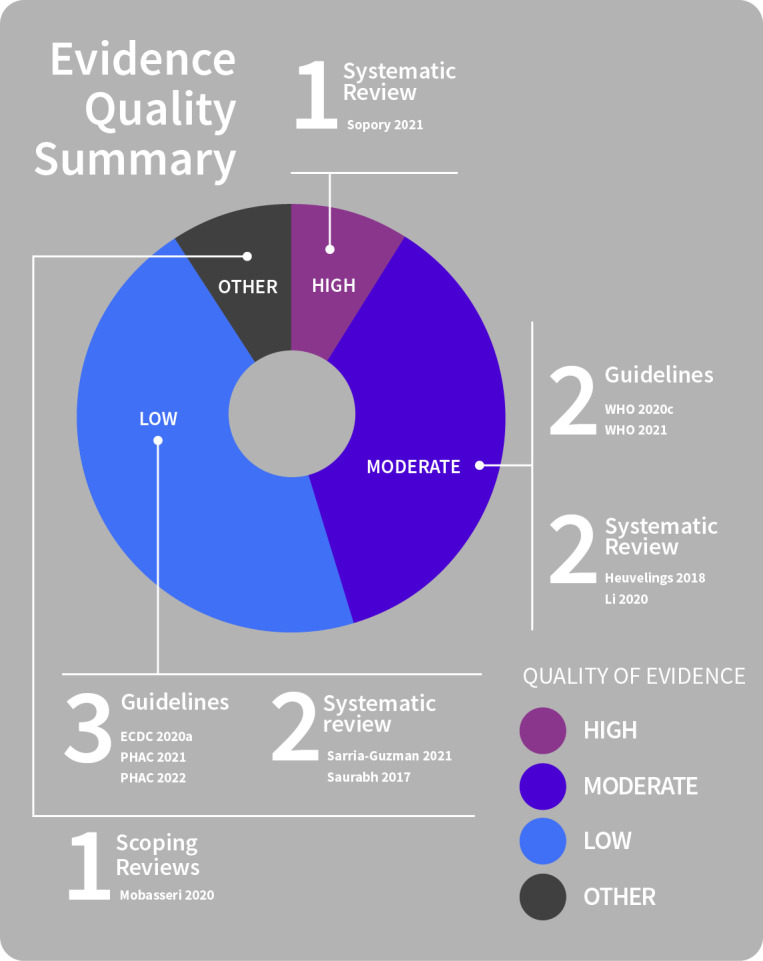
Equity: underserved and vulnerable populations
There is a need for policy responses that actively recognise, and address, the challenges particular to specific groups within the population, and that allow a more comprehensive approach to addressing shared challenges and needs (ECDC 2020a; Mobasseri 2020; Sarria‐Guzman 2021; Sopory 2021). Public health communication planning that includes consideration of diverse audiences and how to reach groups not easily engaged through traditional communication channels is more likely to reach more of the community. This includes prioritising communication and support for those who are most vulnerable and who have different needs to the general public. Public health communication approaches may need to be more flexible to meet these needs (ECDC 2020a; Li 2020; PHAC 2021; PHAC 2022; Sopory 2021; WHO 2020c; WHO 2021).
Public health messages need to be developed with mindfulness that there are people in the community who may not be able to access or use standard resources (ECDC 2020a; PHAC 2021; WHO 2020c). As an example, contact tracing for underserved groups may be improved by using community health workers from the same migrant community, or peers amongst people who use drugs, and is likely to be both highly acceptable and feasible to implement (Heuvelings 2018). While contact tracing has enormous potential to reduce disease cases, successful implementation relies on trust and the provision of appropriate (culturally‐sensitive) messages (Saurabh 2017). Similarly, use of contact tracing apps or other digital technologies needs to be based on consideration that people within the population have differential access to devices to support app usage (e.g. older devices may not run, older people may not have access to or familiarity with the technology, neither Internet access nor digital literacy are uniform across the community) and that this can further marginalise vulnerable people within the community (e.g. those who are older, poorer or in remote regions, those with auditory or visual impairment who cannot access all online materials) (ECDC 2020a; Khorram‐Manesh 2021; Mobasseri 2020; Sarria‐Guzman 2021; WHO 2020c; WHO 2021).
Public health information must be appropriate and accessible, at suitable literacy and comprehension levels for people with intellectual disability or cognitive impairment, and adapted for communication through multiple channels to ensure that people with disabilities receive adequate public health information and services to protect their health (WHO 2021).
For people with disability, mechanisms to enable communication with health professionals to raise concerns or questions about protective measures is needed, and appropriate monitoring processes need to be in place so that people with disabilities who may not be able to voice their concerns during isolation are protected from harm (WHO 2021).
Cultural barriers
See Figure 13 for a summary of evidence quality for these findings.
13.
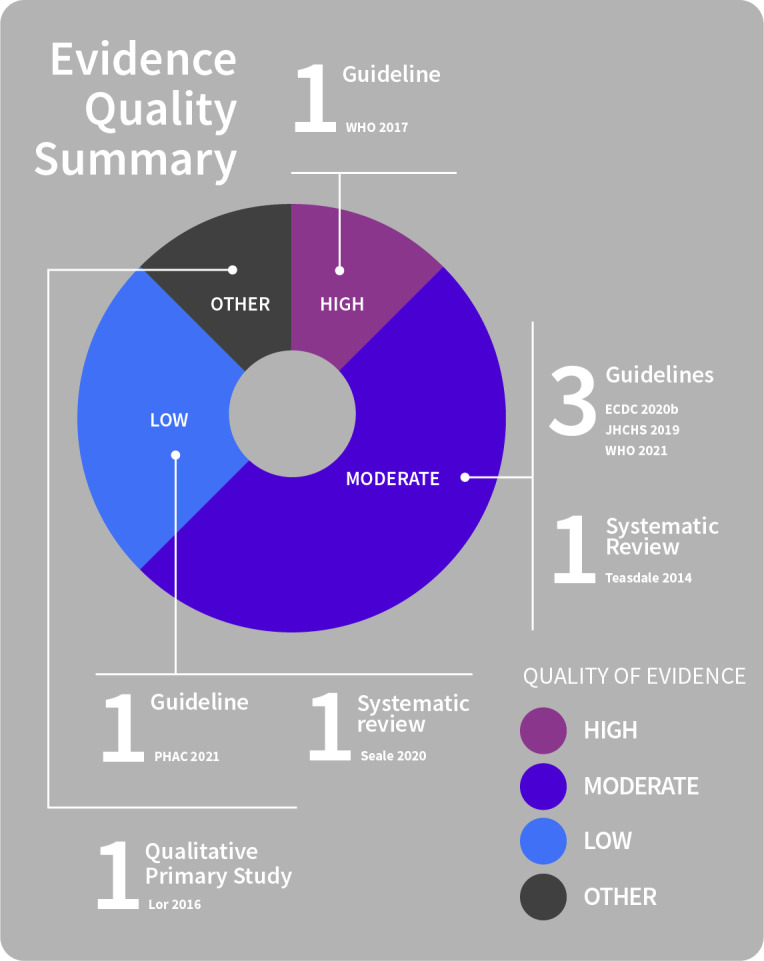
Equity: cultural barriers
Physical distancing for most people within a community is challenging, due to limitations on contact with family, friends, and others. Within some households and some cultural groups, physical distancing may be particularly unacceptable due to the limitations placed on interactions regarded as both socially and culturally necessary. This might include caring for sick family members or funeral duties (Lor 2016; Seale 2020; Teasdale 2014).
Remote islands and isolated communities (e.g. First Nations, Inuit and Metis communities) have additional issues to consider and require tailored approaches to reduce risk and to communicate about these (e.g. tailored based on culture, geography, social determinants of health). For instance, remote communities may not be exposed to the same level of communications as urban areas (PHAC 2021.)
Disseminating actionable information on physical distancing measures, and on coping strategies and support services available may support acceptance, uptake and adherence to measures, but such information needs to be culturally appropriate (ECDC 2020b; WHO 2021). Community involvement may help to identify factors such as cultural and literacy needs of diverse population groups (e.g. people housed within migrant and refugee centres; people in remote areas) and in developing appropriate and accessible public health messaging (ECDC 2020b; JHCHS 2019; Lor 2016; PHAC 2021; WHO 2017). Ideally, such messages should also be pretested for cultural appropriateness (PHAC 2021).
Community languages
See Figure 14 for a summary of evidence quality for these findings.
14.
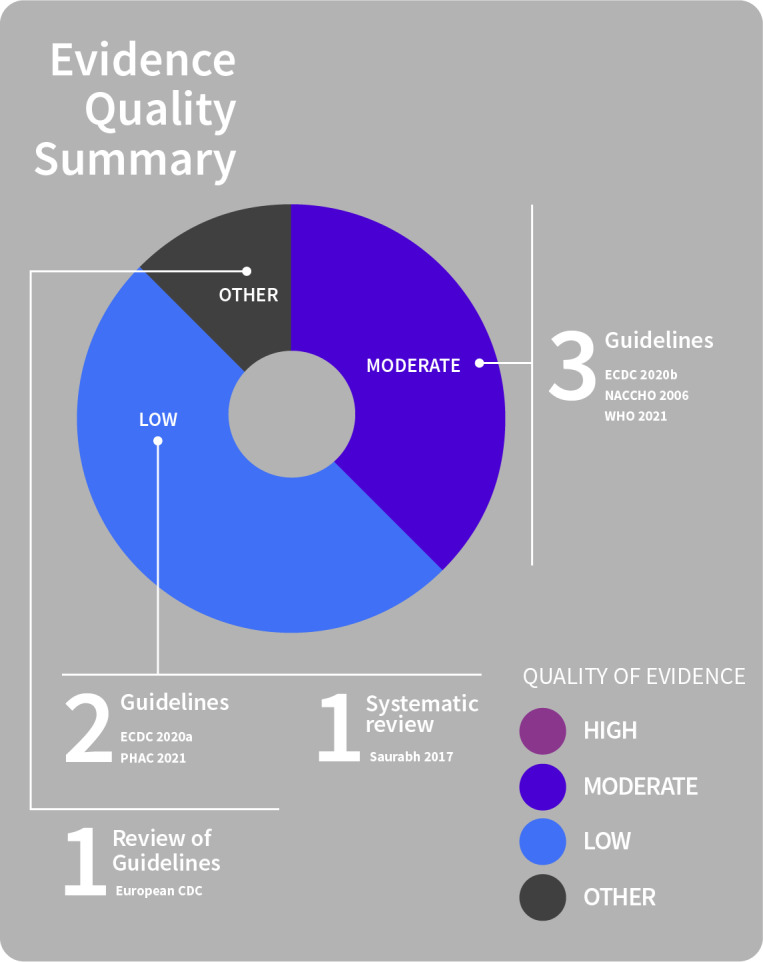
Equity: community languages
Ensuring that information is communicated in a non‐technical language, in the main languages within a population, is imperative, as is translation to official and Indigenous community languages. Planning how to target different audiences, such as those speaking minority languages, including languages understood by irregular migrants is also critical (ECDC 2020a; ECDC 2020b; ECDC 2020g; NACCHO 2006; PHAC 2021; WHO 2021). Lack of readily available information in people’s own languages may otherwise increase fear and anxiety (ECDC 2020b).
Engaging and educating communities (including via community leaders, religious groups and mass media) to promote awareness of accurate, accessible information in affected communities may be key to improving acceptance and uptake of behavioural measures (ECDC 2020b; NACCHO 2006; Saurabh 2017).
Educational inequality
See Figure 15 for a summary of evidence quality for these findings.
15.
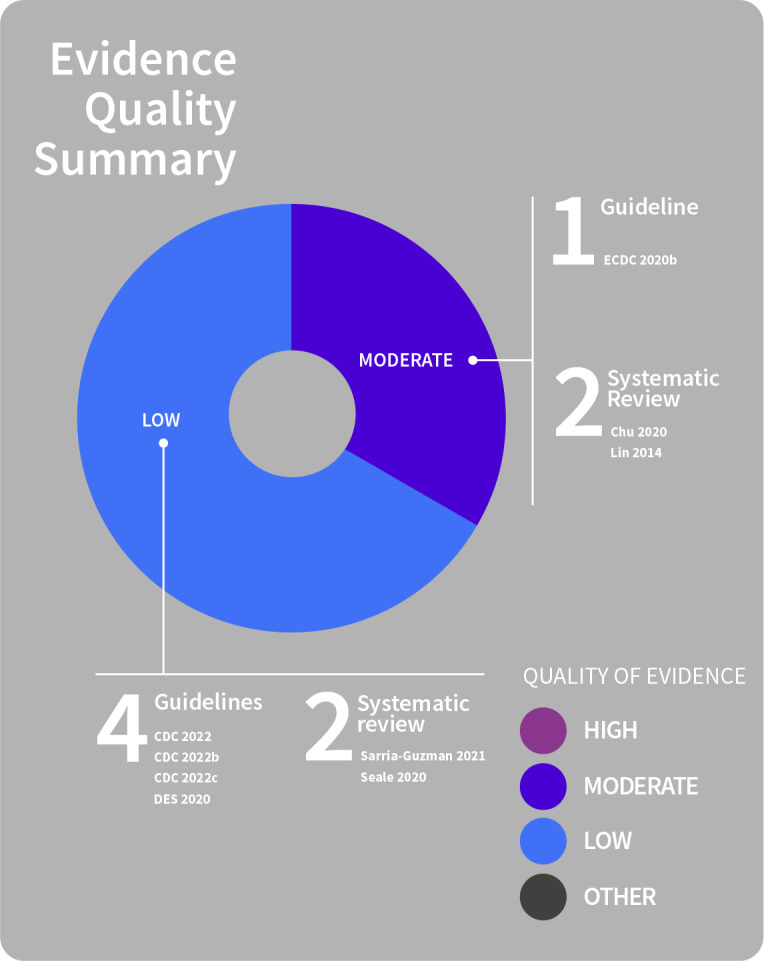
Equity: educational inequality
People with higher levels of education tend to be more informed about pandemic risks, suggesting that health communication messages need to be better tailored to those at lower educational levels in order to reduce inequalities across and within populations (Lin 2014). In general, the most marginalised communities (lower educational and income levels) are the most affected by pandemic outbreaks (ECDC 2020b; Sarria‐Guzman 2021).
The link between knowledge and uptake of preventive behaviours has been highlighted by work on influenza, amongst other diseases, and by surveys on COVID‐19: higher knowledge is associated with a higher likelihood of adherence to preventive measures. Alternative approaches to enhance information uptake, such as visual communication (i.e. infographics or photos), may help overcome literacy barriers, while communicating via written information may help to improve accessibility (particularly in areas of low connectivity) (ECDC 2020b; Sarria‐Guzman 2021).
Educational settings also have a critical role in promoting equity in learning and health (CDC 2022; CDC 2022a; CDC 2022b). School closures, for instance, may negatively impact nutrition (e.g. restricted access to school nutrition programs) and disrupt learning (Seale 2020).
Some groups are also at heightened risk of experiencing severe disease (DES 2020), which means that in‐person learning may pose a greater risk (CDC 2022; CDC 2022a; CDC 2022b). Careful and collaborative planning is required when implementing preventive measures to ensure that equitable access to education is promoted and maintained, and that staff and students at heightened risk of severe disease are supported to engage in learning and/or continue working or studying remotely to reduce exposure to risk (CDC 2022; CDC 2022a; CDC 2022b; DES 2020).
Authorities and school curricula must recognise and act to mitigate learning and health inequalities, including adopting communication strategies to address communication inequalities; providing tailored support to disadvantaged groups (CDC 2022; CDC 2022a; Chu 2020; DES 2020) and working to connect people with resources (e.g. stable housing, healthy food) or services that help to meet their needs (CDC 2022b).
Theme 4: Public communication features: content, timing and duration, delivery
Content of public information and communication
See Figure 16 for a summary of evidence quality for these findings.
16.
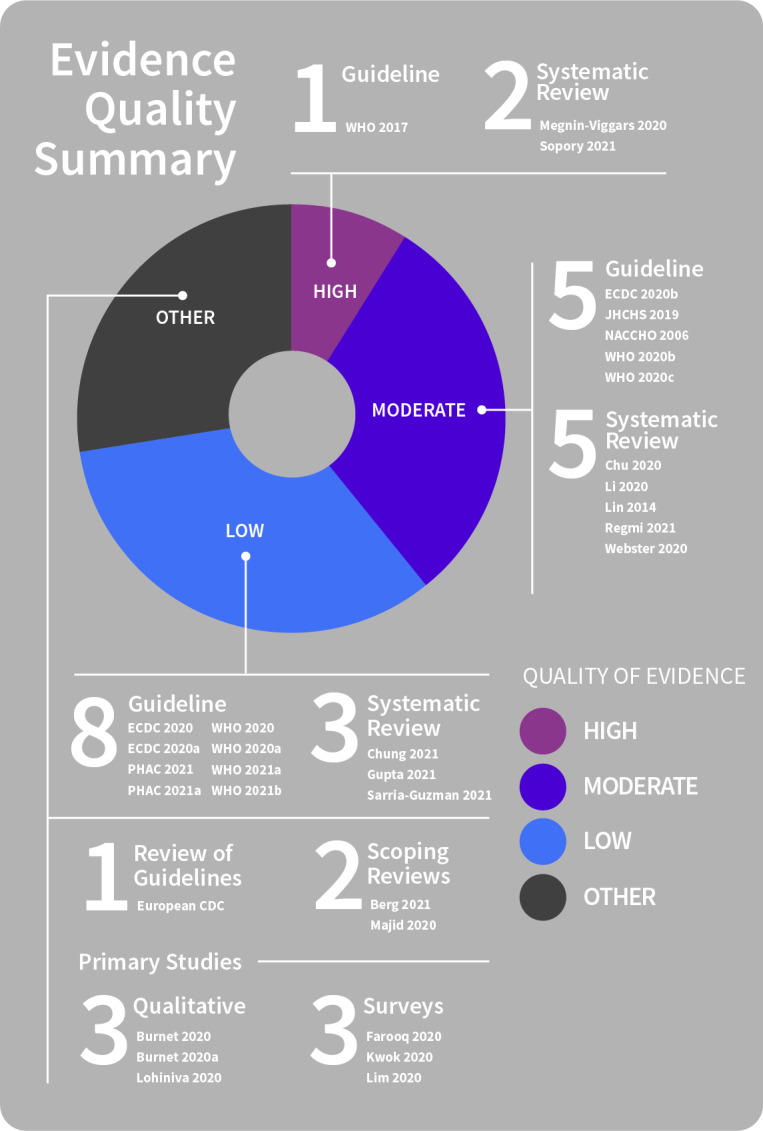
Information and communication content
To improve uptake and adherence to physical distancing measures, public health authorities need to communicate comprehensive, clear and consistent information to the public (Chu 2020; ECDC 2020; ECDC 2020a; ECDC 2020b; Gupta 2021; Li 2020; Lin 2014; Megnin‐Viggars 2020; PHAC 2021; PHAC 2021a; Regmi 2021; Sopory 2021; Webster 2020; WHO 2020; WHO 2020a; WHO 2020b; WHO 2020c; WHO 2021a; WHO 2021b) that includes a clear and accurate rationale for the required measures (i.e. why the measure is needed and what is involved), how to comply, and the services available to support the measures, including how to access available support services (Burnet 2020; Burnet 2020a; Chung 2021; ECDC 2020g; JHCHS 2019; Li 2020; Majid 2020; Megnin‐Viggars 2020; NACCHO 2006; Regmi 2021; Sarria‐Guzman 2021; Sopory 2021; Webster 2020; WHO 2017; WHO 2021b). Such information must be accessible and timely and provided prior to the implementation of the measure in order to improve acceptability and adherence (Chung 2021; Sopory 2021; WHO 2021b). Any changes to measures over time must also be clearly communicated (PHAC 2021; PHAC 2021a; WHO 2020a; WHO 2020c).
Findings also show:
Risk messages written in clear, non‐technical terminology are needed (ECDC 2020; PHAC 2021; WHO 2020; WHO 2021a; WHO 2021b).
Jargon or technical language needs to be kept to a minimum or avoided (Berg 2021; Chu 2020; ECDC 2020a; ECDC 2020b; PHAC 2021; Sopory 2021; WHO 2017; WHO 2020a; WHO 2020c; WHO 2021a).
Agencies need to communicate to encourage knowledge of, adherence to, and correct use of measures (PHAC 2021; Sarria‐Guzman 2021).
Members of the public need clear, practical information about the behaviours they are required to undertake (Burnet 2020a; ECDC 2020b; ECDC 2020g; Lin 2014; Webster 2020) and how the measures will work (Berg 2021; Chu 2020; ECDC 2020b; Megnin‐Viggars 2020; Sarria‐Guzman 2021). This is so that individuals and communities are clear about what they can and cannot do within the measures.
Communicating with empathy to the public and acknowledging difficulties associated with following public health advice is critical.
Clearly and openly acknowledging uncertainty and what is being done to obtain information with the aim of saving lives at a given point in time is also important, particularly for an emerging disease (Chung 2021; ECDC 2020; Majid 2020; WHO 2017; WHO 2020a).
Technical epidemiological information may be explained more easily using visualisations (ECDC 2020); or statistical information might be more accessibly described in words, e.g. using real‐life stories to convey risks and the importance of following public health advice (PHAC 2021; PHAC 2021a). Since communicating visually (e.g. graphics, images, colours) can significantly influence the reach and reception of messages, public communication might occur via several modes and include visual information (Berg 2021).
Public health communications might encourage people to enact the required changes (ECDC 2020g) and promote specific actions individuals can take to protect their health (Farooq 2020; Kwok 2020; Lohiniva 2020; NACCHO 2006; WHO 2017; WHO 2020). Communication strategies aiming to increase self‐efficacy (promote specific actions that individuals or communities can take to protect their health) and ensure that there is sufficient information for people to do so, may foster readiness to change and so promote positive behavioural changes that align with the required public health measures (Berg 2021; Kwok 2020; Li 2020; Lim 2020; Majid 2020; Megnin‐Viggars 2020; Regmi 2021; Sarria‐Guzman 2021; WHO 2020c; WHO 2021a).
Inadequate or insufficient information is related to poor acceptance and other outcomes.
See Figure 17 for a summary of evidence quality for these findings.
17.
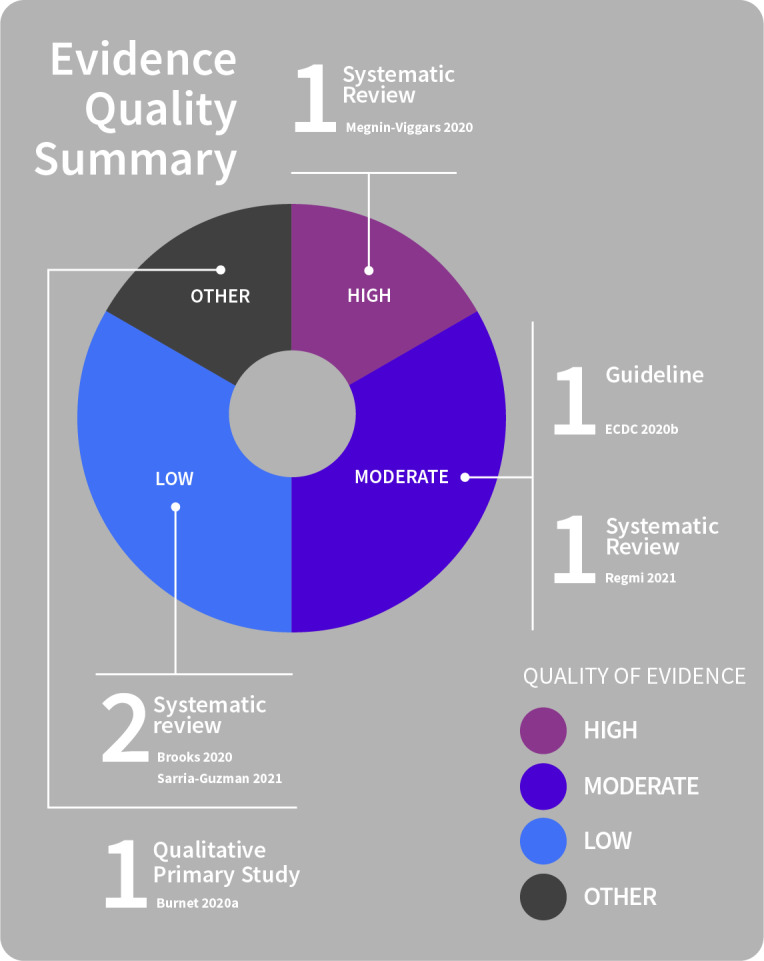
Inadequate or insufficient information effects
The perceptions and experiences of individuals undertaking self‐isolation and quarantine are fundamentally affected by their access to clear information (Burnet 2020a; Regmi 2021). A qualitative study of adults undertaking quarantine for COVID‐19, for instance, indicated that better information and knowledge was needed about required self‐isolation and quarantine measures. This includes information to clearly distinguish between self‐isolation and quarantine measures and other physical distancing measures (Burnet 2020a).
Lack of information (e.g. in people’s own languages), contradictory (inconsistent) or confusing information or information that is difficult‐to‐find about what can and cannot be done while in isolation/quarantine, or required from contact tracing systems, is related to non‐adherence (Brooks 2020; Burnet 2020a; Megnin‐Viggars 2020). Further, a lack of information, communication and support may have negative psychological effects on the acceptability of such measures (Brooks 2020; ECDC 2020b; Megnin‐Viggars 2020), can lead people to be unclear about actions to take and fearful of stigma (ECDC 2020b; Megnin‐Viggars 2020), and may lead to risky behaviours (Sarria‐Guzman 2021).
Emphasis of content on public more than individual health benefit may promote acceptance.
See Figure 18 for a summary of evidence quality for these findings.
18.
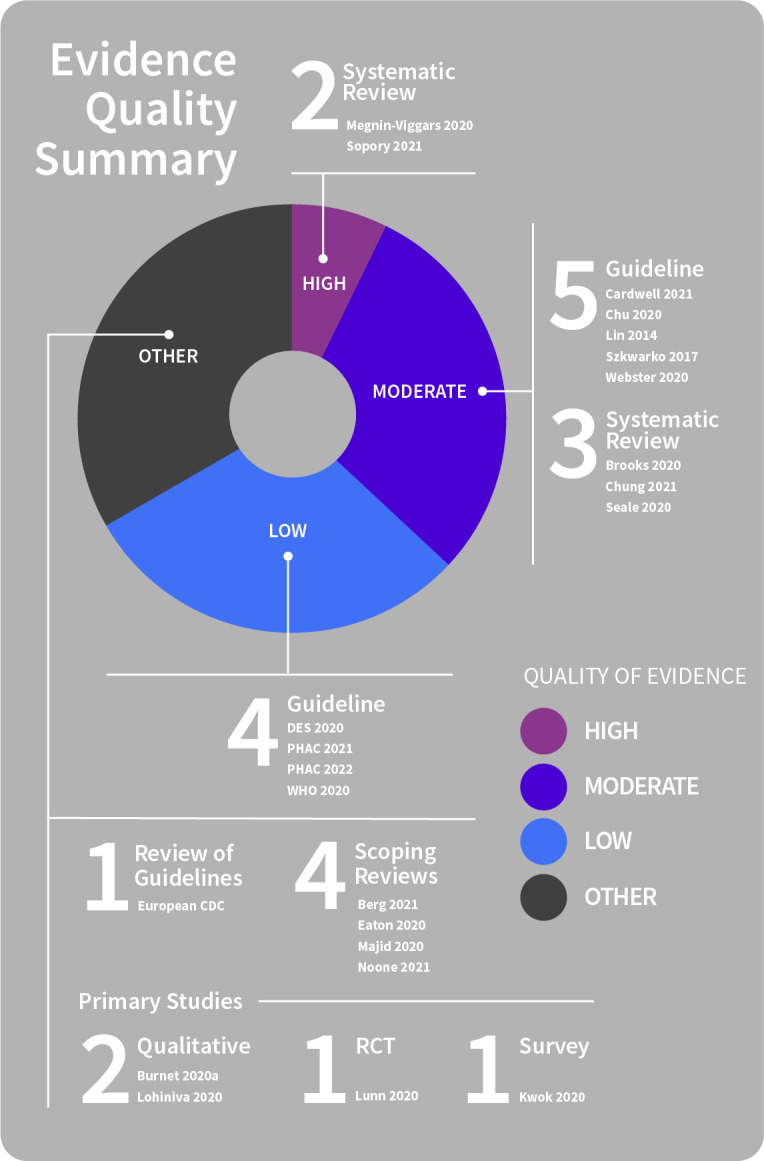
Public versus individual health benefit
Communication emphasising public health benefits and the importance of physical distancing can promote acceptance. In a general sense, the public, including vulnerable groups (e.g. those who are homeless) accept the concept of restrictions (e.g. quarantine) as part of the outbreak response, for several reasons: from a sense of duty, civic‐mindedness, and ethical concerns about the situation (Sopory 2021). When such measures are implemented, public communications might therefore actively promote solidarity, clearly reinforce the need for mutual community support and emphasise both the importance and the benefits of physical distancing measures for protecting public health, such as preventing transmission to others, especially those at higher risk (Cardwell 2021; Chung 2021; Eaton 2020; ECDC 2020g; Kwok 2020; Lin 2014; Lunn 2020; Megnin‐Viggars 2020; Noone 2021; Seale 2020; Sopory 2021; Szkwarko 2017; Webster 2020).
Findings also show:
Where uptake of physical distancing measures is voluntary (i.e. not mandated), messages stressing that the choice of quarantine or self‐isolation is an altruistic one taken on behalf of the community, might be beneficial (Brooks 2020; Chu 2020; Webster 2020).
Encouraging people to consider ways in which they can benefit others and contribute to keeping everyone in the community safe and saving lives may promote acceptability (DES 2020; PHAC 2022; WHO 2020) as, when people feel part of a community response, they may be more likely to adhere to measures; and this is especially so if they see others following the same measures (PHAC 2022).
Authorities may work to promote altruism by developing culturally competent, context‐specific strategies and by focusing on care (i.e. expressing concerns, providing support), rather than on control or enforcement of restrictions (Chu 2020; Sopory 2021).
To effectively motivate the public to comply with public health measures, feelings of collective responsibility in countering disease outbreaks, as well as perceived personal benefit, must outweigh barriers such as privacy concerns and mistrust (Megnin‐Viggars 2020).
Lowering perceived response costs and providing clear information about the severity of risks may also help to motivate members of the public to self‐isolate (Chung 2021).
The narrative tone of authorities’ communications can affect people’s emotional state (anxiety, uncertainty) and influence engagement and behavioural responses to risk mitigation messages. Narrative messages that elicit positive emotions may lead to better community engagement, but they may also undermine perceived seriousness of the threat (risk)(Berg 2021).
Actions of authorities, including by the government, to control the spread of pandemic disease, and to support those undertaking physical distancing measures, might also be communicated to the public (Burnet 2020a; Lohiniva 2020).
Modelling desirable behaviours to make them the social norm may also assist with uptake and adherence to measures (PHAC 2021).
Timing of communications and duration of measures
Knowledge and attitudes change over time.
See Figure 19 for a summary of evidence quality for these findings.
19.
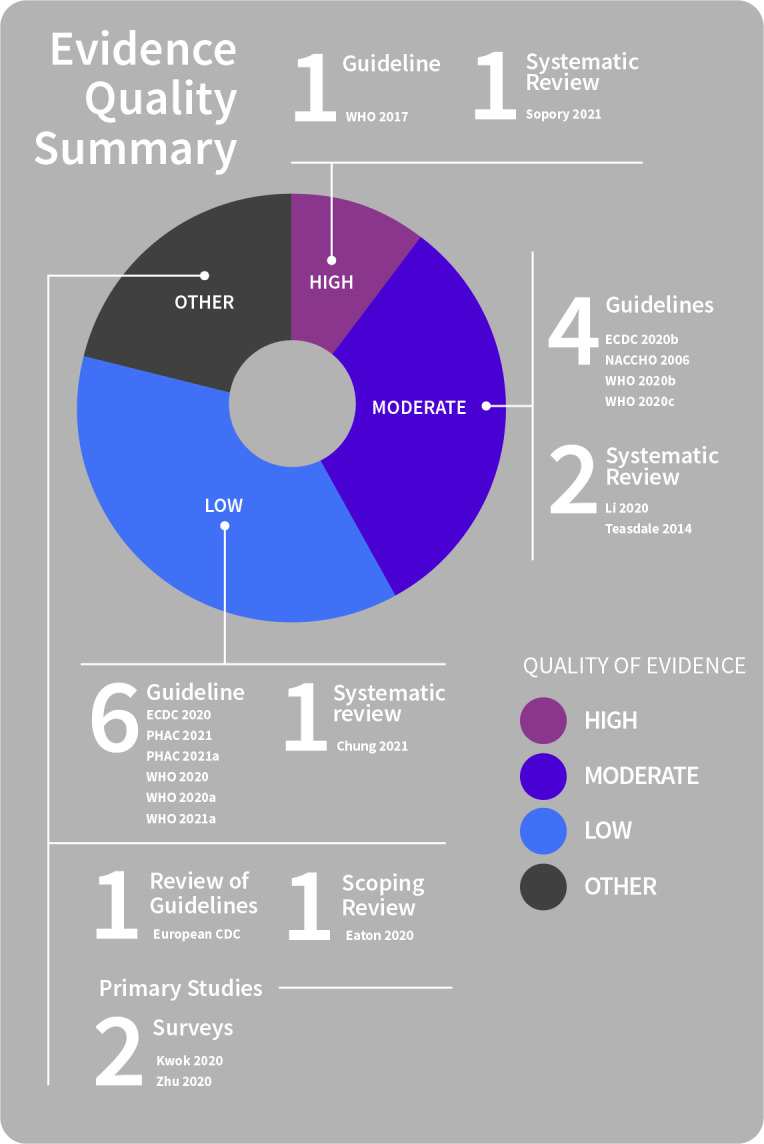
Knowledge and attitudes over time
Public communication about public health measures is needed over the course of a pandemic outbreak. This includes immediate initial communications (as early as possible upon recognition of a pandemic) that are continuously updated over the outbreak, as new information becomes available, or the situation changes (pandemic status, impacts on essential services, actions being taken to address the outbreak, ways that people can protect themselves)(Chung 2021; Li 2020; PHAC 2021; Sopory 2021; WHO 2020a; WHO 2021a). Critically, information about public health measures must be up‐to‐date (Chung 2021; Li 2020; PHAC 2021; WHO 2021b) to promote accurate public knowledge about required preventive measures and about how to adhere (Eaton 2020; ECDC 2020g; NACCHO 2006; WHO 2017; WHO 2020; WHO 2020a; WHO 2021a).
Public health communication about risk is important early in a pandemic. At this stage, perceived risk might be lower, but the disease is being transmitted, and communications at this early point can increase uptake and adherence to preventive measures (Teasdale 2014; Tooher 2013; WHO 2020a). Two surveys undertaken during the COVID‐19 pandemic suggest that proactive government communication to increase public awareness early about disease outbreaks, risk reduction measures and protective behaviours creates earlier opportunities for individuals to take up physical distancing measures. Later communication of such critical information may represent missed opportunities for the public to engage with and take up preventive measures (Kwok 2020; Zhu 2020).
Findings also show:
Authorities must prepare to begin public communication early before the full picture is known and even if information is incomplete, and communicate openly about uncertainty (i.e. manage uncertainty) and the degree of uncertainty (WHO 2020; WHO 2020a).
Public communication needs to include early and frequent announcement of the health threat. There is a need for this to be updated after analysis of public risk perceptions (WHO 2020; WHO 2020a).
Mechanisms to monitor public perceptions of risk and the response are needed throughout the pandemic to allow these to be quickly identified and addressed (ECDC 2020a; ECDC 2020g; WHO 2020a; WHO 2021a).
Engagement with community leaders and other stakeholders is also important for two‐way information exchange over time, particularly because of ongoing uncertainties over the pandemic course (WHO 2020c).
Public health messages additionally need to raise awareness that COVID advice is continually changing, in response to the evolving pandemic and might encourage individuals to assess their own risk (e.g. My COVID Risk tool) so that they are able to make an informed decision before they attend or host gatherings and take measures to stay safe, particularly if at higher risk of severe disease (PHAC 2021a). Such messages might aim to inform people to take preventive measures to protect their own health but also encourage high awareness of knowledge of symptoms and self‐monitoring and provide clear instructions on when and how to isolate, seek medical attention and when to be tested if they suspect they might have COVID‐19 (ECDC 2020b; ECDC 2020; PHAC 2021; PHAC 2021a; WHO 2020; WHO 2020b).
Communicating duration and rationale for measures
See Figure 20 for a summary of evidence quality for these findings.
20.
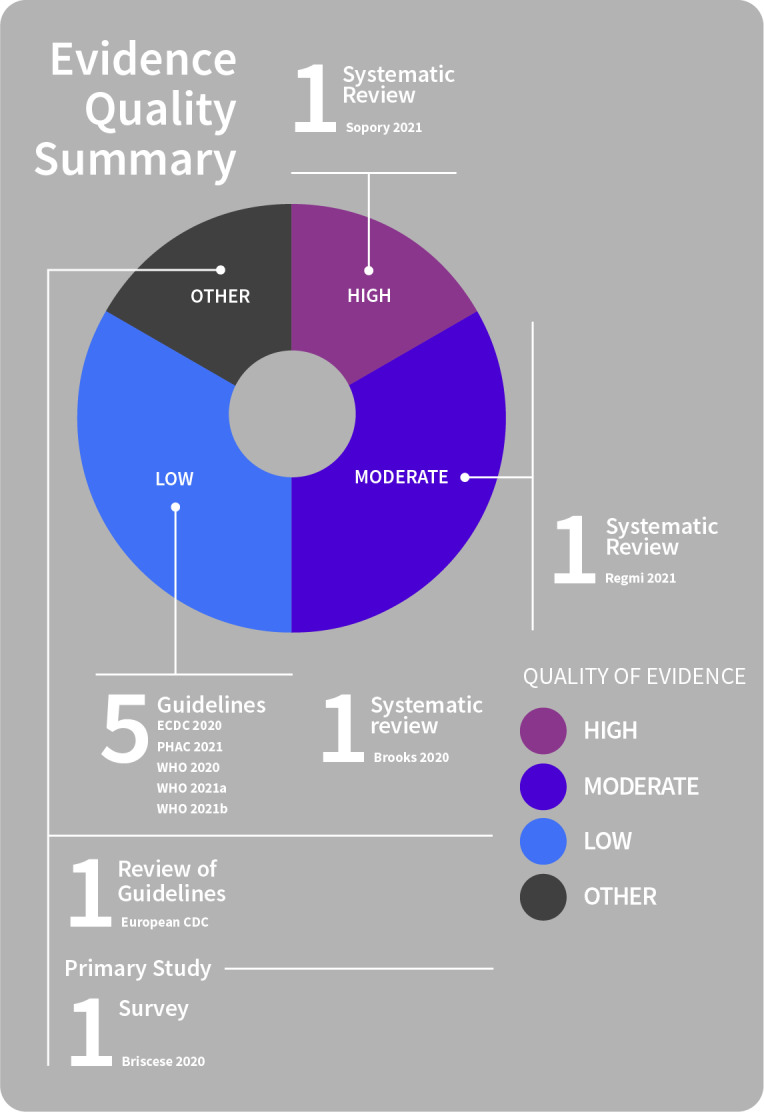
Communicating duration and rationale
Public communications need to signal the duration of new required public health measures, or adjustment of existing measures, and clearly explain and justify the rationale for them before the measures are implemented or adjusted (ECDC 2020; PHAC 2021; Sopory 2021; WHO 2020; WHO 2021a; WHO 2021b).
For more restrictive physical distancing measures, such as quarantine or isolation, such communications may be the most critical. The psychological effects of quarantine (researched in health workers, and adults and children) appear substantial and varied, and may be long‐lived. Duration is one of several stressors, and longer quarantine periods are associated with poorer mental health outcomes (Brooks 2020; Regmi 2021). Such negative psychological impacts might be minimised by isolating people for the shortest possible time. Duration needs to be based on evidence of incubation times (rather than arbitrary or indefinite time frames), and information about the rationale and guidelines (what is happening, and why) provided through clear, consistent communication (Brooks 2020; ECDC 2020; WHO 2020).
Results from a survey undertaken during the COVID‐19 pandemic indicate that most people intend to maintain their self‐isolation behaviours in the context of shifting endpoints for restrictions (irrespective of their own expectations of duration of physical distancing). However, unexpected extension of restrictions may lead to fewer people intending to increase, and more intending to decrease, adherence to self‐isolation measures. Public health messages may therefore need to consider the public’s expectations, as well as the pandemic context in which the measures occur, particularly where there is uncertainty in an emerging disease pandemic that may necessitate extension of restrictions (Briscese 2020; Regmi 2021).
Public acceptance of physical distancing measures might therefore be facilitated by establishing and clearly communicating the anticipated end date (Brooks 2020; ECDC 2020g; WHO 2020).
Communication is also needed to convey that the measures may need to be continued and adjusted, or that some measures may be removed or reduced while others remain in place, and that ending or adjusting measures will require that a range of key criteria are explicitly considered to ensure public safety (ECDC 2020; PHAC 2021; WHO 2020). Such communication aims to transparently prepare public expectation for the possibility of changes, such as during the COVID‐19 outbreak, when initial time frames for self‐isolation measures were uncertain and restrictions may be extended depending on a range of factors such as current epidemiology (e.g. intensity of transmission), capacity of public health and healthcare systems, local context, and the social and economic impacts of measures (Briscese 2020; ECDC 2020; ECDC 2020g; WHO 2020).
Employing multiple delivery mechanisms
See Figure 21 for a summary of evidence quality for these findings.
21.
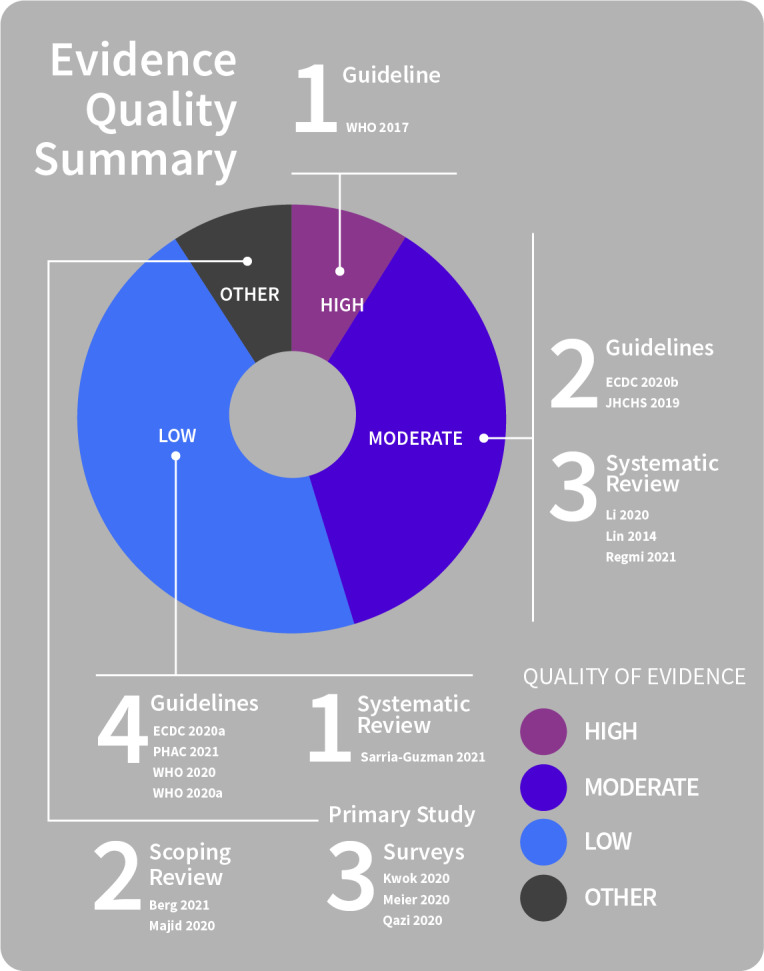
Multiple delivery mechanisms
Several simple, practical measures may be used to reinforce and remind people of physical distancing measures. This includes straightforward approaches such as use of visual cues and directional marking to support recommended distancing (e.g. markings at appropriate distances for spacing as a reminder (e.g. in shops, clinics, school desks)), one‐way flow to reduce number of contacts, signage to support preventive messaging (e.g. maintaining the greatest possible distance, do not enter if symptomatic), or noise reduction strategies to enable people to interact at a distance (avoiding close interaction)(PHAC 2021; WHO 2020). Visual communication and multilingual signage also need to be adopted (i.e. infographics with pictograms or photos) to help overcome literacy barriers and to reinforce communications about preventive measures (ECDC 2020b; PHAC 2021; WHO 2020).
Findings also show:
Public information and education need to be credible, accurate and accessible, and disseminated in multiple ways. This might include adopting different formats (e.g. written information pamphlets, SMS messages and social media posts); and using a range of channels (e.g. traditional media (newspapers, radio, television), digital (e.g. videos, SMS, social media)), written information (e.g. government pamphlets), community groups and leaders (e.g. community faith leaders, community physicians) to aim for maximal community reach (Berg 2021; ECDC 2020a; ECDC 2020b; Li 2020; Majid 2020; PHAC 2021; Regmi 2021; WHO 2017).
Providing consistent information and messages from multiple places (sources; e.g. community leaders plus social media plus traditional media) as part of an integrated communication strategy is more likely to be trusted and acted upon than information coming from a single source (ECDC 2020b; Lin 2014; WHO 2017).
Establishing trusted lines of communication and using these channels to convey information to the public, is also key when planning risk communication efforts as trust is importantly linked to knowledge and protective behaviours (Berg 2021; JHCHS 2019; Majid 2020; Regmi 2021).
Information exchange with family, friends, peers, and healthcare workers is often a primary information source. The role of trust in linking knowledge and behaviour also appears particularly important for healthcare workers, who may themselves provide relevant and timely information on risks and prevention measures (Majid 2020; Sarria‐Guzman 2021).
Building relationships between the media and health authorities may be key, as well as building trust in authorities before a pandemic emerges (Berg 2021; WHO 2017).
Even where individuals are well‐informed, they receive and seek pandemic information through multiple formal and informal channels (e.g. traditional mass media, governmental sources; social media); and are not passive information recipients from a single source. Rather, most people actively seek information about the pandemic, community risks and required preventive actions, from a range of sources, selecting from amongst the total information they encounter (Berg 2021; Li 2020; Majid 2020). Information sources consulted are often diverse in format, language and target audience and include diverse disease, risk, transmission, prevention and aid topics (Majid 2020).
Research indicates that both formal (newspapers, press releases, educational messages) and informal (social media, online reviews and family or peer views) information sources are used by the public and increase people’s perceived understanding (Majid 2020; Meier 2020; PHAC 2021; Sarria‐Guzman 2021). Surveys during the COVID‐19 pandemic also indicate that source use varies considerably across countries, with social media platforms and websites most commonly used in some countries, while in others, more traditional sources (including television, newspaper/news applications) were most often accessed (Kwok 2020; Meier 2020; Qazi 2020). Other research indicates that information sources consulted by members of the public vary considerably across populations and that accessibility (ease of access) and availability of information are major determinants of people’s choice of information sources (Kwok 2020; Majid 2020; Meier 2020; Qazi 2020; Sarria‐Guzman 2021).
Digital technologies may assist in adapting some information and support services for vulnerable people. However, care is needed as lack of easy access to such technologies or familiarity with their use may otherwise further marginalise people from vulnerable groups (ECDC 2020a). Health agencies and governments therefore need to communicate effectively using a range of media or channels, to reach different parts of the community, including disadvantaged groups and those without Internet access (Majid 2020; Sarria‐Guzman 2021).
No single approach (choice of information sources), therefore, appears suitable across all community groups or populations. Providing information via multiple sources appears critical, for instance, via traditional media sources such as newspapers and news broadcasts (radio, television), social media and written information together within an integrated strategy (ECDC 2020b; WHO 2017). However, it is critical to ensure that messages convey consistent information, and that sources are accessible and credible to the community. Overall, the communication strategy must aim to improve credibility, rather than creating confusion, as may be the case if inconsistent messages are communicated rapidly through multiple different channels (Berg 2021; ECDC 2020a; ECDC 2020b; Li 2020; Majid 2020; Regmi 2021).
Theme 5: Supporting behaviour change at individual and population levels
Acceptance, uptake and adherence to physical distancing measures during a pandemic requires behavioural change from individuals and entire communities. Knowledge of what is needed, why, and how to go about it is essential. The evidence also indicates several practical elements are required to directly support behaviour change in these circumstances, including direct support services and financial support, and that these need to be considered in any response that involves implementation of physical distancing measures. Differential types and levels of support may be needed across the community to help redress inequalities. Such considerations help to promote readiness for individuals and whole communities to receive and act on (implement) preventive behaviours.
Communication to influence social attitudes and norms
See Figure 22 for a summary of evidence quality for these findings.
22.
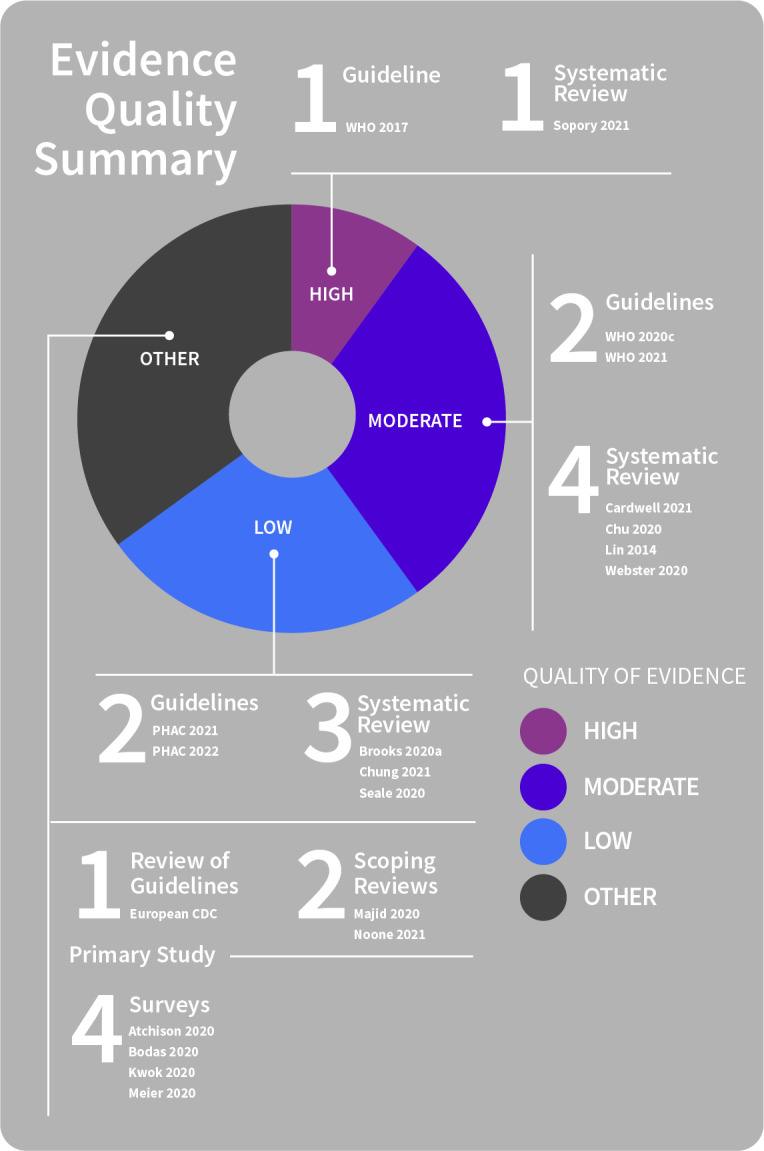
Social attitudes and norms
Public sentiment is key, necessitating communication that targets both individual and population levels to reinforce positive social attitudes and norms towards physical distancing. This relies on the public understanding the benefits and the potential harms of preventive measures (Sopory 2021; WHO 2021).
Sustained changes to behaviour, particularly over long periods, require communication targeted at multiple levels (i.e. not just to the individual), taking broader social and structural systems into account, and ensuring regular reiteration of messages over time (Chung 2021; Kwok 2020; Meier 2020).
Findings also show:
Authorities/agencies need to proactively communicate in an accessible way when changes to individual or community‐based measures are likely to occur and provide a rationale for the changes. Such transparent communication can improve adherence to public health measures as people understand the reasons for the measures, the effectiveness of the measures, and they can prepare for the changes to come into play (PHAC 2022).
Communication which seeks to shift and/or reinforce social norms, such as strong social pressure to adhere to physical distancing measures, may be beneficial. Actively promoting solidarity, mutual community support, and a sense of altruism for adopting and adhering to physical distancing measures, may also have positive effects (Cardwell 2021; Chu 2020; Chung 2021; ECDC 2020g; Kwok 2020; Lin 2014; Majid 2020; Noone 2021; Seale 2020).
Such communications, including those to specifically promote social connectedness amongst community members, may be more successful in improving uptake of and adherence to public health measures than communications targeting individual behaviour change alone (Majid 2020).
School measures
The importance of clear communication and good community understanding of the measures to be enacted is also apparent in relation to school and workplace closures, both of which may be employed in a pandemic, and both requiring support to promote adherence (Seale 2020).
Evidence indicates that school closures are generally accepted and taken up by parents if they perceive the measure to be beneficial, most often related to protecting health (community, child and household). Communicating effectively and consistently with parents to ensure that they understand that both school closure and avoiding social contact are important, and why, crucially determines success (Brooks 2020a).
Where information from schools conflicts with public health advice, there can be negative effects on parental acceptance of closures (Brooks 2020a; Seale 2020). Parents may be unwilling or unmotivated to adhere to school measures if they do not understand the reasons for the measures or practical requirements, do not believe the closure will have any impact or benefit to the community (i.e. decrease infection risk), or do not feel that their children are at risk (i.e. low perceived risk) (Brooks 2020a; Seale 2020). Parental concerns may include uncertainty about the likely closure duration, unequal access to digital education (impacting education continuity), or economic impacts (e.g. lost parental income)(ECDC 2020g). If both schools and workplaces are closed during mass quarantine, parents may be able to provide home‐based schooling. Adolescents may be able to learn remotely and independently if provided with web‐based learning platforms and mobile connections (Chu 2020). However, parent‐supervised schooling may be challenging for many and requires consistent information and support for parents from schools (Seale 2020).
Short school closures up to two weeks may be manageable by parents, but longer closures, such as those that may be required for mitigating the risk of pandemic waves, may be more challenging. Parents may also misunderstand the term “school closure” and associate this with “permitting out‐of‐home activities” i.e. the success of school measures may be undermined by compensatory contact between children out of school. Communication with the community is therefore needed to support school closures (e.g. via sports clubs), otherwise students may not understand that the advice to avoid contact is to prevent themselves from infecting others (Seale 2020). Childcare arrangements (outside home) also hold the potential to increase disease transmission. Families may need assistance with caring for children during closures or leave children to self‐care (with attendant risks). Children in self‐care may be more likely to engage in compensatory behaviours (e.g. visiting school friends or extended family) (Seale 2020). Public health officials might, therefore, consider how best to support parents to prevent this within communities (Brooks 2020a).
Communication to address stigma and lack of acceptance of public health messaging
See Figure 23 for a summary of evidence quality for these findings.
23.
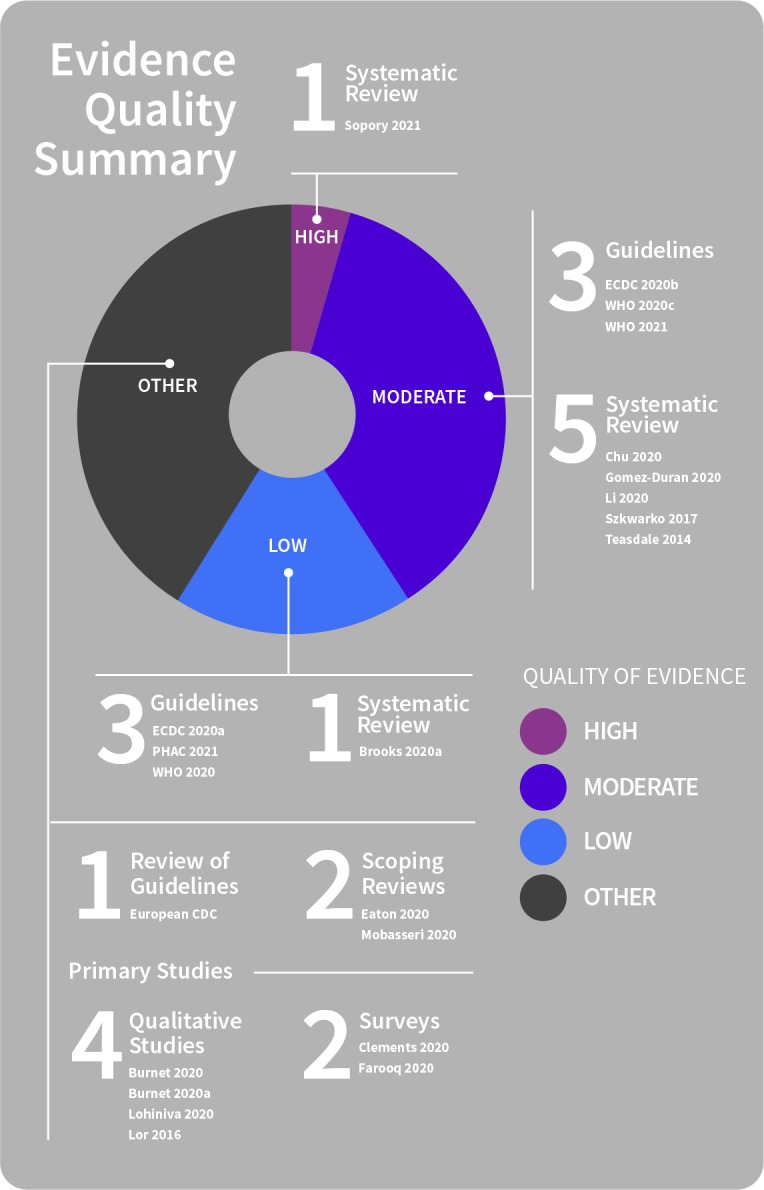
Stigma and lack of acceptance
Stigma or discrimination may undermine the effectiveness of public health messages (Brooks 2020; Eaton 2020; ECDC 2020a; ECDC 2020b; Li 2020; PHAC 2021; Sopory 2021). Negative effects of perceived or actual stigma have been reported for adherence with contact tracing (Szkwarko 2017), quarantine (Brooks 2020) and physical distancing more generally (Eaton 2020; Lor 2016). This has occurred during the COVID‐19 pandemic and previous outbreaks, such as influenza (H1N1), SARS and EVD (Brooks 2020; Burnet 2020; Burnet 2020a; Lohiniva 2020).
People in (or transitioning in or out of) quarantine, or those isolating, for instance, may feel shamed or blamed by public health communications, and so perceive a lack of support for continuing with the measures (Burnet 2020a). Those quarantining may experience social stigma or being publicly labelled as disease carriers, leading to mistrust, fear and avoidance by other people, and negative psychological impacts including distress, anxiety and other symptoms of mental illness (Chu 2020; Sopory 2021). Negative effects like these extend beyond the quarantine period (Chu 2020; Gomez‐Duran 2020; Sopory 2021).
Such impacts negatively affect patients and healthcare workers and their families and, in some cases, whole minority or foreign population groups (Brooks 2020), particularly when people quarantined are from marginalised groups (Sopory 2021). For instance, people may believe the source of an infectious disease in a community to be solely related to a particular group (e.g. foreign nationals or people from abroad, or between racial and religious groups) (Chu 2020; Clements 2020; Farooq 2020). Stigma may also negatively affect those who are medically or socially vulnerable. During COVID‐19, for example, negative views and age‐related stigma led to a loss of public roles for older people and heightened anxiety amongst older adults (Mobasseri 2020). Such effects can slow or prevent enactment of measures to reduce disease spread (Brooks 2020; ECDC 2020a; PHAC 2021; WHO 2020; WHO 2020c).
Findings also show:
To improve acceptance and adherence to measures, stigma related to physical distancing measures needs to be proactively addressed.
Authorities and leaders need to monitor for and speak out against the stigmatisation of particular groups; implement quarantine measures proportionately to risk; and ensure the rights of those in quarantine (or transitioning in/out) are considered (ECDC 2020b).
Authorities need to communicate with the community to improve knowledge and understanding, reinforce that everyone in the population is at risk of an emerging disease, and emphasise respect and each person’s human rights (ECDC 2020b; Gomez‐Duran 2020; Li 2020; PHAC 2021; WHO 2020; WHO 2020c; WHO 2021).
Promoting factual reporting to combat misinformation, stereotypes, and stigmatisation by disseminating contextualised evidence‐based information to the public may also be helpful (e.g. targeting fear/hostility for migrant workers, or quarantining healthcare workers) (Gomez‐Duran 2020; WHO 2021).
Communication to positively influence more accurate perceptions of vulnerability and risk
See Figure 24 for a summary of evidence quality for these findings.
24.
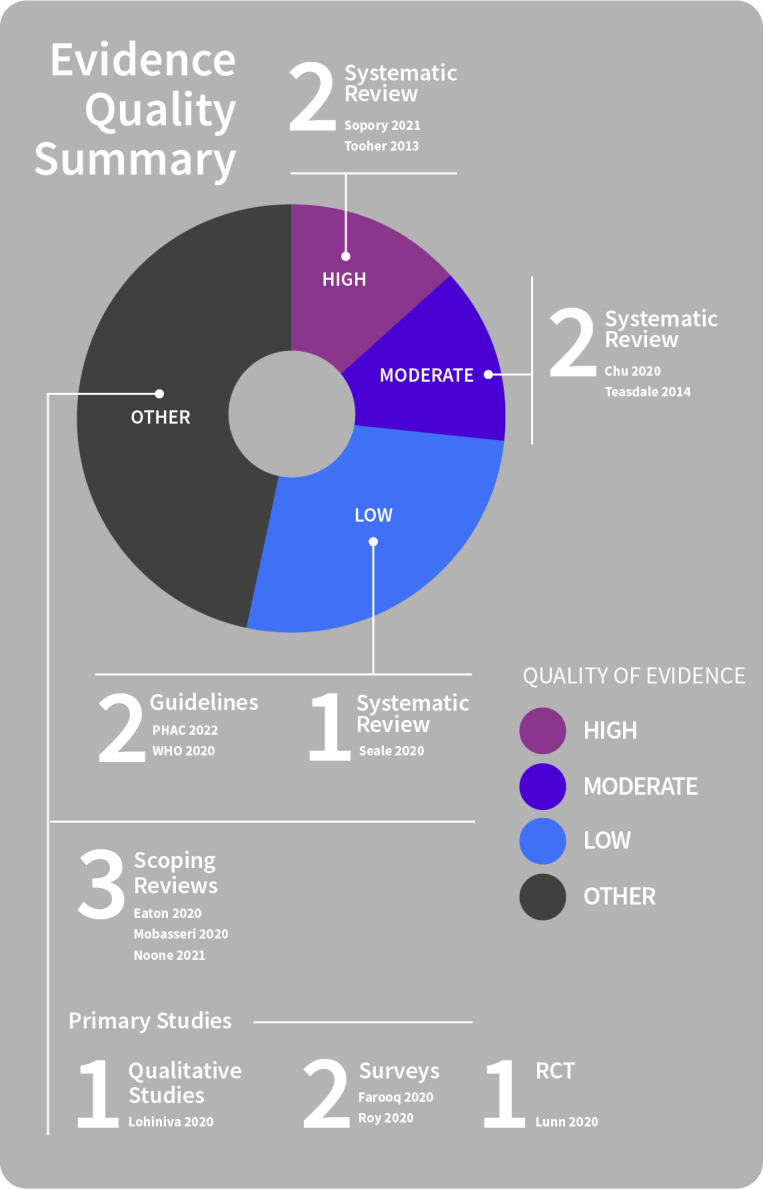
Perceptions of vulnerability and risk
Public knowledge is essential for the implementation of physical distancing, but people’s views and perceptions of the measures and risk of disease (perceived personal vulnerability, transmission and severity of the disease) also influence their acceptance, uptake and adherence (Lohiniva 2020; Majid 2020; Noone 2021; Teasdale 2014; Tooher 2013). In pandemic situations, differences between intended (planned) and actual behaviours may be particularly critical and relate to people’s perceived infection risk (Chu 2020; Farooq 2020; Tooher 2013). For instance, people typically accept that an emerging pandemic risk creates risk to the community at large. However, some identify themselves as less vulnerable (e.g. than people with chronic illnesses, only ‘others’ are at risk), decreasing their own likelihood of adopting preventive measures (Chu 2020; Lohiniva 2020).
Findings also show:
Public communication addressing common beliefs and concerns about the necessity and effectiveness of preventive measures, and attending to key barriers such as perceptions of personal vulnerability, is most likely to improve the adoption of measures (Lohiniva 2020; PHAC 2022; Roy 2020; Sopory 2021; Teasdale 2014).
Communication to pointedly highlight the immediacy and susceptibility of people within the community to a pandemic risk may also be necessary, for example, targeting groups with little or no intention of taking up preventive measures (e.g. younger men), with the aim of improving uptake and adherence (Farooq 2020; Seale 2020).
Communication strategies emphasising the likelihood of infecting vulnerable people or large numbers of people (anticipated regret) can help to motivate physical distancing by increasing people’s intention to be cautious in their own physical distancing behaviours (Lunn 2020; Noone 2021). It can also change people’s attitudes to be less accepting of marginal physical distancing behaviours in others (i.e. to adopt a more cautious attitude to physical distancing). Communications might therefore be most effective when emphasising the impact of non‐compliance with preventive measures on identifiable people and numbers of infections (Lunn 2020).
Another option involves positively framing health messages (expressing advice in terms of maintaining well‐being, rather than with a negative or vulnerable identity, avoiding infection), which may improve the perceived relevance of preventive measures to those who do not acknowledge that they are at risk of infection and so encourage adherence (and decrease stigma) (Lohiniva 2020; Seale 2020). In other cases, availability of guidelines (e.g. shielding guidelines to protect older adults) can be key to informing people’s decisions about preventive measures required (Mobasseri 2020).
During a pandemic, special measures may be enacted to protect vulnerable groups, including people at risk for severe disease (e.g. older people, those with underlying medical conditions); those with social vulnerabilities (e.g. refugees, migrant workers, people experiencing homelessness); those living in closed settings (e.g. detention centres, camps); and those more likely to be exposed occupationally (e.g. health workers, frontline responders) (WHO 2020).
Similarly, people who are at higher risk of severe disease might be encouraged to conduct their own personal risk assessment. This can inform whether additional measures (e.g. crowd avoidance) are needed to protect their health, and people may choose to enact additional measures even during periods of low(er) community transmission. Clear communication by public health authorities is needed about such additional measures in order to promote collective actions for the common safety of the community, including where there is a difference in the level of adoption of preventive measures required based on personal risk – that is, by emphasising that such decisions and behaviours (i.e. for individuals to protect themselves) are acceptable (PHAC 2022).
Essential services to support quarantine or isolation
See Figure 25 for a summary of evidence quality for these findings.
25.
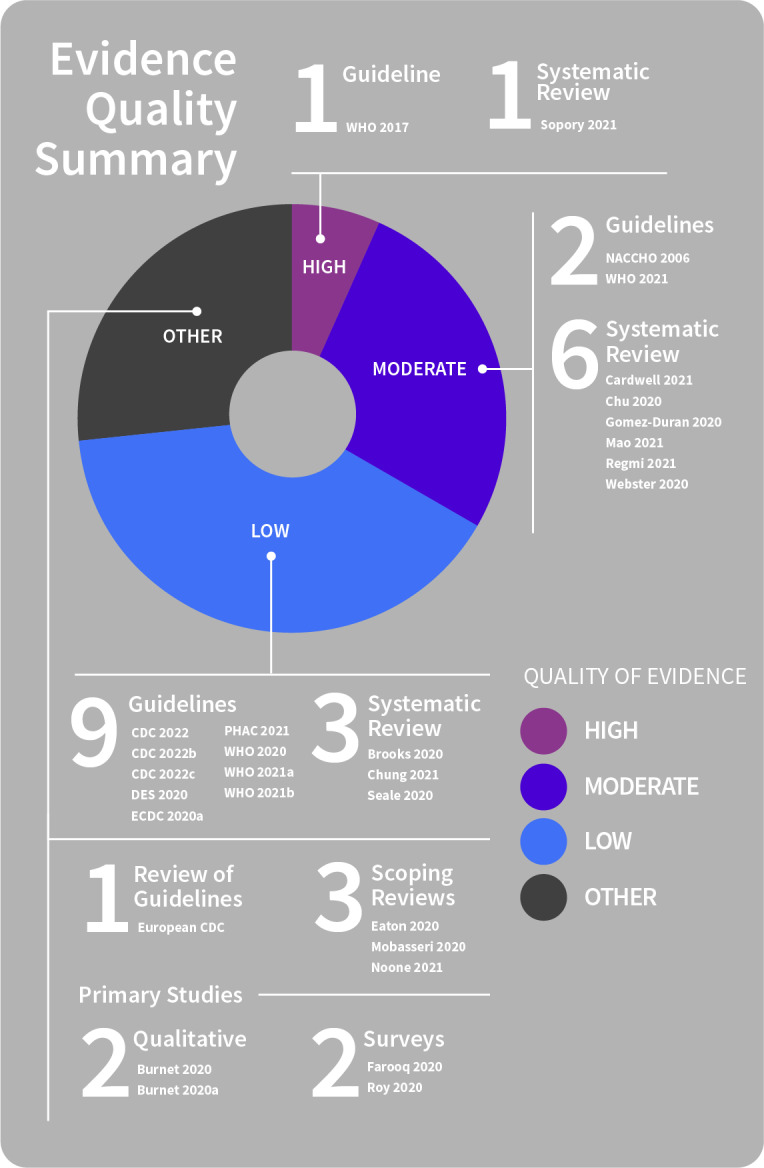
Provision of essential services
Supporting public preparedness
Public communication clearly acknowledging the difficulties of undertaking and adhering to restrictive measures is needed. Such communications might express concern for the public and reassure people that both moral and practical support will be available to help them to adhere to the required physical distancing measures (Burnet 2020; ECDC 2020g; Farooq 2020).
Information to support preventive measures needs to consider health literacy levels and other needs for tailoring (e.g. to ethnic minority groups, older people, remote communities), and include information on the impact of measures and how to address or reduce negative impacts (Cardwell 2021; Chu 2020; ECDC 2020a; PHAC 2021; Seale 2020; WHO 2020; WHO 2021).
Findings also show:
Encouraging and supporting people to develop quarantine plans ahead of time (maintaining a supply of essential medicines, food and home supplies) to be prepared in case of restrictions may be beneficial (Burnet 2020; PHAC 2021).
Ensuring people with disabilities have access to essential services and to care pathways that are easy to access, and that caregivers are considered part of the essential workforce and exempted from curfews and other restrictions that may affect their delivery of support or care is also essential (WHO 2021).
Facilitating people with disabilities and their carers to make contingency plans for situations where the carer is sick or quarantined may also help to ensure continuity of care (WHO 2021).
Planning for and informing the public about safe healthcare‐seeking behaviours by disseminating information, including information about new pathways to services if unavailable through the usual routes during a pandemic, opening hours and precautions needed, is also critical (NACCHO 2006; WHO 2020; WHO 2021b).
Access to healthcare may also be affected by reallocation of resources to the outbreak emergency and by widening health inequality in vulnerable populations (Chu 2020), or by a lack of access to reconfigured services (e.g. older people may lack access or knowledge of how to use services delivered by telemedicine or social contacts delivered remotely) (Mobasseri 2020).
Support for restrictive preventive measures (quarantine, isolation)
Comprehensive support systems and services are needed for those undertaking restrictive measures, such as quarantine and isolation (Chung 2021; ECDC 2020g; WHO 2021a). This assists people to be as adherent as possible while reducing long‐term physical and mental health effects (Cardwell 2021; Chu 2020; Chung 2021; Mobasseri 2020; Seale 2020; Sopory 2021; WHO 2020), including people disproportionately affected by the pandemic and public health measures due to one or more vulnerabilities (ECDC 2020a; Sopory 2021; WHO 2021). Since measures such as mass quarantine can lead to several negative social consequences (Sopory 2021), and may worsen existing inequalities, a focus on reducing social inequalities needs to be prioritised for countries to build resilience and preparedness for future outbreaks (Chu 2020).
Support may vary in intensity (comprehensiveness) and target (generally or to specific vulnerable populations) (Cardwell 2021). Support systems and access to social services appear particularly critical for vulnerable groups, who may be disproportionately affected by some measures (e.g. mass quarantine) including people with medical vulnerability (i.e. people at higher risk of death or severe disease e.g. older people, people with underlying medical conditions), social vulnerability (i.e. vulnerable due to the public health measures put in place to control COVID‐19 e.g. people with long‐term physical, mental, intellectual or sensory impairments, people experiencing homelessness, ethnic minorities, irregular migrants), or overlapping or accumulating categories of vulnerability which create particularly challenging circumstances (Chu 2020; ECDC 2020g; Mobasseri 2020; Noone 2021; PHAC 2021; Sopory 2021; WHO 2021; WHO 2021a). There is a need for policy responses that address the particular challenges faced by each type of vulnerable population (ECDC 2020a; WHO 2021), and recognition that intensified or tailored information and supports may be needed for some vulnerable groups (e.g. financial support, food, family violence support, culturally appropriate housing) (Chu 2020; Mobasseri 2020; Regmi 2021). Clear acknowledgement and prioritisation of the needs of people from vulnerable groups is needed (ECDC 2020a; PHAC 2021; WHO 2021; WHO 2021a).
A critical purpose of support systems is to ensure access to essential supplies and services. This includes easily accessed food, water, medications, meaningful activities, and communication with social networks (including support lines) and specialist services (e.g. maternal and child health services, financial support and access to education for quarantined children) (Brooks 2020; Burnet 2020; Burnet 2020a; Chu 2020; ECDC 2020g; Seale 2020; Webster 2020; WHO 2021b).
Findings also show:
Information about the availability of essential services (e.g. financial support, health services) needs to be communicated widely. Research clearly indicates that people must be well‐informed about what services exist, who is eligible, how to access the services, and that the services themselves are easily accessed if needed (Burnet 2020; Burnet 2020a; Cardwell 2021; ECDC 2020g; WHO 2021a). Where people must rely primarily on family or friends for help, with little support from services, they feel vulnerable and this reduces adherence (Burnet 2020; Burnet 2020a; Cardwell 2021; ECDC 2020g; Webster 2020).
Similarly, support services that are difficult to access may cause problems. For instance, difficulties accessing financial support or financial insecurity while in isolation causes distress and non‐adherence, particularly for those of lower socioeconomic status (Burnet 2020a; Chu 2020; Sopory 2021), while negative outcomes (e.g. stigma, fear, loneliness) are worsened by inadequate supplies and inadequate information and communication (Cardwell 2021; Regmi 2021; Seale 2020).
For people in quarantine or isolation, clear lines of communication (e.g. telephone or online services staffed by health professionals) are needed, should they develop symptoms (Brooks 2020; Burnet 2020; Burnet 2020a; WHO 2021b).
Support for mental health and well‐being
During home‐based isolation or quarantine, people are at higher risk of new or recurring mental health problems (Burnet 2020a; Chu 2020; Seale 2020; Sopory 2021), and mental health issues may affect people’s ability to adhere to preventive measures (Brooks 2020; Burnet 2020a; ECDC 2020g). Long‐term psychological impacts (Brooks 2020) may be exacerbated by the population’s uncertainty about the pandemic and the (public health and/or population's) response to the pandemic (Burnet 2020a; Chu 2020; Regmi 2021). The need for community access to health and mental health services has been highlighted by several studies (Brooks 2020; Burnet 2020; Burnet 2020a; Chu 2020; ECDC 2020g; Roy 2020; Sopory 2021; WHO 2021), and might enable people to adhere to restrictive measures while reducing long‐term physical and mental health effects (Brooks 2020; Burnet 2020; Burnet 2020a; Chung 2021; ECDC 2020g; Mobasseri 2020; Seale 2020; Webster 2020).
There is also a role for volunteer organisations in supporting people to adhere to public health measures, and particularly to fill gaps in existing services and supports. Activities might include delivery of essential supplies and working to address unmet needs of community members. Similarly, there is a role for volunteer groups to feed back information on current or future community priorities (e.g. that clear advice is available as restrictions change, that community inequalities are addressed) (Mao 2021).
Facilities (e.g. out‐of‐home quarantine) should be disability‐inclusive and consider the needs of women and children (WHO 2021; WHO 2021a). Limitations of online or digital technologies for vulnerable people and the potential for widening inequalities during the pandemic need to be recognised and contingencies planned (e.g. people without access to or knowledge of telephones or computers) (ECDC 2020a). This is important to ensure access so that COVID‐19 is controlled in vulnerable populations (and, therefore, the rest of the community) (WHO 2021).
Support for workplaces
Employers and public health authorities working together to support employees if services (e.g. childcare or school) are unavailable during a pandemic may be beneficial, particularly if restrictions are longer than a few weeks in duration (Brooks 2020a; Eaton 2020; NACCHO 2006). Workplaces (administrators, managers, supervisors) may also beneficially promote tools and techniques for supporting staff with mental healthcare needs during a crisis. Measures may include training staff to help employees cope with grief, anger, exhaustion and fear (NACCHO 2006).
Support in schools (in educational settings, in workplaces)
Studies have also highlighted the need for support in school settings. Both students and staff require physical and mental health support, as well as clear information and communication (CDC 2022; CDC 2022a; DES 2020). Staff require support to work during the pandemic, education and training in preventive practices and policies, and proactive management of workload and mental health strain (CDC 2022; CDC 2022a). Administrators need to share information about available support services and provide a supportive environment for staff to manage job stress and build resilience (CDC 2022; CDC 2022a). Support and guidance for staff and teachers related to schools reopening is important, in order to support their own well‐being and to equip them to support students (DES 2020). Comprehensive communication campaigns delivering messages of safety and well‐being, access to information, and links to resources (e.g. guidance, support, psychological support services) may be helpful (DES 2020).
Provision is needed (in the form of flexible, non‐punitive, supportive paid sick leave) which is clearly communicated to school staff, to ensure that workers do not attend work if sick and do not fear negative repercussions (loss of pay or employment) for absences (CDC 2022; CDC 2022a; CDC 2022b). Measures are also needed to ensure all staff understand the policy for returning to work after COVID‐19 illness and for reporting related concerns (CDC 2022; CDC 2022b).
Additional supports may be required for children with special educational needs and educational disadvantage. Tailored supports for students and staff at higher risk (e.g. modified work or learning arrangements) may also be needed (CDC 2022; CDC 2022a; CDC 2022b; DES 2020).
Support for healthcare workers
Healthcare workers (HCWs) too are a particular group requiring support to undertake quarantine (the need for which may be acquired occupationally). Much of this literature is outside the scope of this current review, but those relating to the need for additional support for HCWs during a pandemic are highlighted briefly here.
High levels of distress, fear of infection, poor psychological outcomes, isolation and financial losses are common in the public undergoing quarantine. These same outcomes are also prevalent in healthcare workers in quarantine, with additional complexity because of their dual role as HCW and family member. Many HCWs have concerns for their family’s safety based on their occupation, particularly of vulnerable family members and children, as in‐home quarantine may expose their family to further risk. Additional measures such as suitable accommodation (outside the family home) to help to lessen the risks to families and to address workers’ concerns about infection risk may be necessary (Gomez‐Duran 2020). These issues highlight the need for comprehensive support and information for HCWs in quarantine and for accurate information and better communication with the public about the need for and purpose of quarantine, to help mitigate poor outcomes and diminish stigma associated with quarantine (Gomez‐Duran 2020; Sopory 2021). For people undertaking quarantine, clear guidelines need to be provided on minimising infection risk at home and in quarantine, to help to minimise fear of infecting family members and uncertainty about effectively mitigating risk (Gomez‐Duran 2020).
Essential services to address financial insecurity and socioeconomic disadvantage related to preventive measures
See Figure 26 for a summary of evidence quality for these findings.
26.
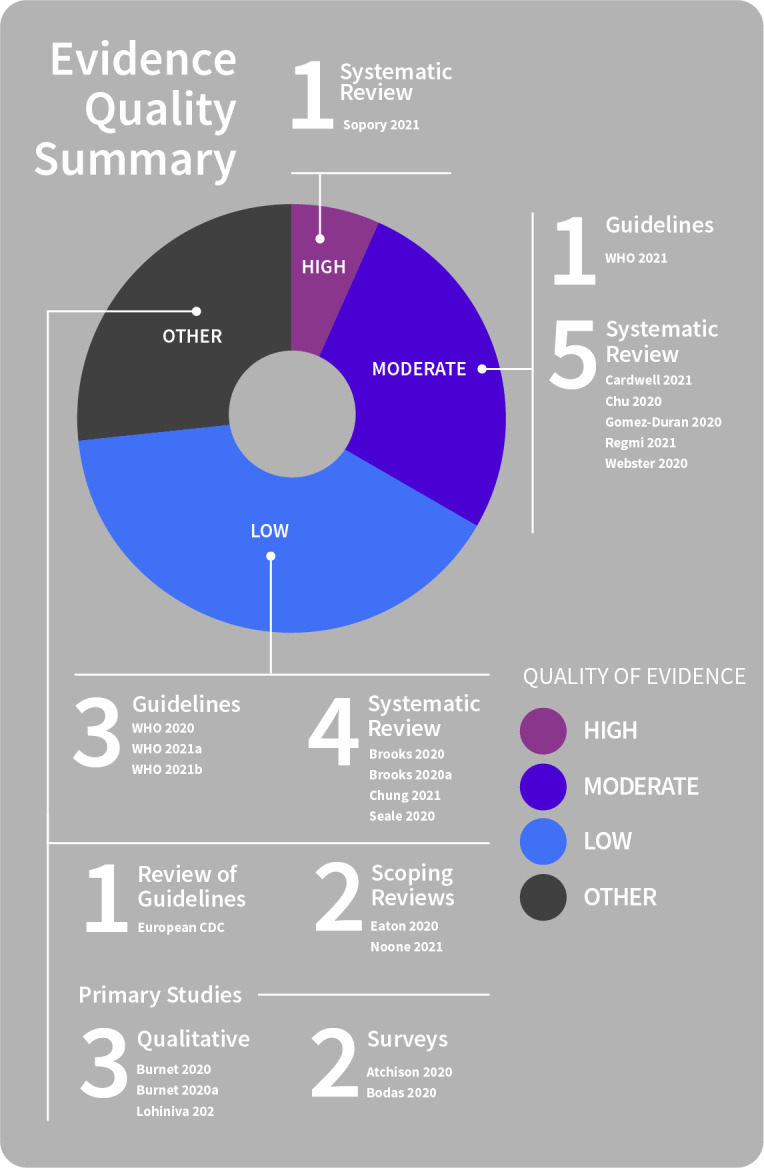
Financial insecurity and socioeconomic disadvantage
Economic effects of mass quarantine and other preventive measures can be profound on individuals and businesses, which can also affect the food supply chain and a range of industries. Financial losses or difficulties accessing financial support during and after quarantine are a common risk factor for psychological distress which may lead to non‐adherence. Of major concern are impacts on employment (job security) and lost or reduced income across all income brackets, but particularly concerning those with lower household incomes or who work part‐time, casually or are self‐employed, not paid for time away from work, or unable to work from home (Chu 2020; Gomez‐Duran 2020; Seale 2020). People may also take additional risks once quarantine/self‐isolation is completed in order to survive financially (e.g. continuing to work in close contact with people despite a lack of physical distancing measures) (Burnet 2020a).
Many studies stress the importance of financial support in promoting adherence to physical distancing measures (Atchison 2020; Bodas 2020; Brooks 2020; Burnet 2020; Burnet 2020a; Chung 2021; ECDC 2020g; Gomez‐Duran 2020; Noone 2021; Regmi 2021; Seale 2020). Measures to compensate people financially for losses (restricted income or employment), due to restrictive physical distancing measures, might be one way to promote adherence, and could take several forms. These include partial/full income replacement (during quarantine), flexible leave and payment arrangements, assurance of job security and economic recovery (at end of quarantine), and payment for housing and utilities (Bodas 2020; Burnet 2020; Burnet 2020a; Cardwell 2021; ECDC 2020g; Sopory 2021; WHO 2020). Healthcare workers are a particular case requiring support, including financial compensation, as financial losses are commonly reported and may increase psychological distress associated with the need to quarantine (Gomez‐Duran 2020).
School and/or work closures also have financial implications which can negatively impact adherence (Eaton 2020). As parents may miss or reduce work when schools are closed, financial compensation might improve adherence to school measures (Brooks 2020a; Eaton 2020) and may also be necessary to improve acceptance, uptake and adherence to workplace measures (e.g. for people unable to work remotely) (Eaton 2020). Financial burden on families due to increased childcare and/or work absence during school closures affects adherence to a variable degree but may have particularly marked effects for people unable to work at home and for single‐parent households (Seale 2020).
If stricter public health measures are implemented, this needs to be balanced against socioeconomic impacts. This is particularly important in settings highly dependent on daily wages and the informal economy, or where social disparities exist (WHO 2021a).
Socioeconomic inequalities may diminish the capacity of some groups within the population to take up and follow physical distancing measures, even where willingness to do so is high (Atchison 2020; Chu 2020; Lohiniva 2020; Regmi 2021; Seale 2020; WHO 2021b). Many studies stress that financial support or compensation for lost income is needed for people undertaking physical distancing measures, as cost is otherwise a barrier (Atchison 2020; Bodas 2020; Brooks 2020; Burnet 2020; Burnet 2020a; Chung 2021; Gomez‐Duran 2020; Noone 2021; Regmi 2021; Seale 2020; Webster 2020).
In disadvantaged communities, fewer people may be able to comply with preventive measures. For example, few of those with the lowest household incomes may be able to work from home or to self‐isolate. Issues, such as residing in high‐density settings (e.g. slums, refugee camps), also commonly have an impact on capacity to adhere to physical distancing in economically disadvantaged communities (Atchison 2020; Eaton 2020; Seale 2020; Webster 2020). People from lower income backgrounds or with other disadvantage therefore need tailored financial assurance and assistance to be able to undertake protective measures (Atchison 2020; Chu 2020; Chung 2021; Gomez‐Duran 2020; Lohiniva 2020; Webster 2020). People from such disadvantaged groups may be particularly vulnerable if the government delays financial support to those under quarantine who cannot work without travel (Chu 2020).
Negative effects of mass quarantine may also more heavily burden countries unprepared for public health emergencies. For instance, food insecurity may lead to panic buying in high‐income countries, but to population‐level famine in low‐income countries; similarly, remote learning may be feasible in urban centres, but not for those living in poverty, or in remote areas with poor digital infrastructure. Interventions are, therefore, needed to address existing disparities, as well as those worsened by mass quarantine (Chu 2020; WHO 2021).
Theme 6: Fostering and sustaining receptiveness and responsiveness to public health communication
Pandemic fatigue as a barrier
See Figure 27 for a summary of evidence quality for these findings.
27.
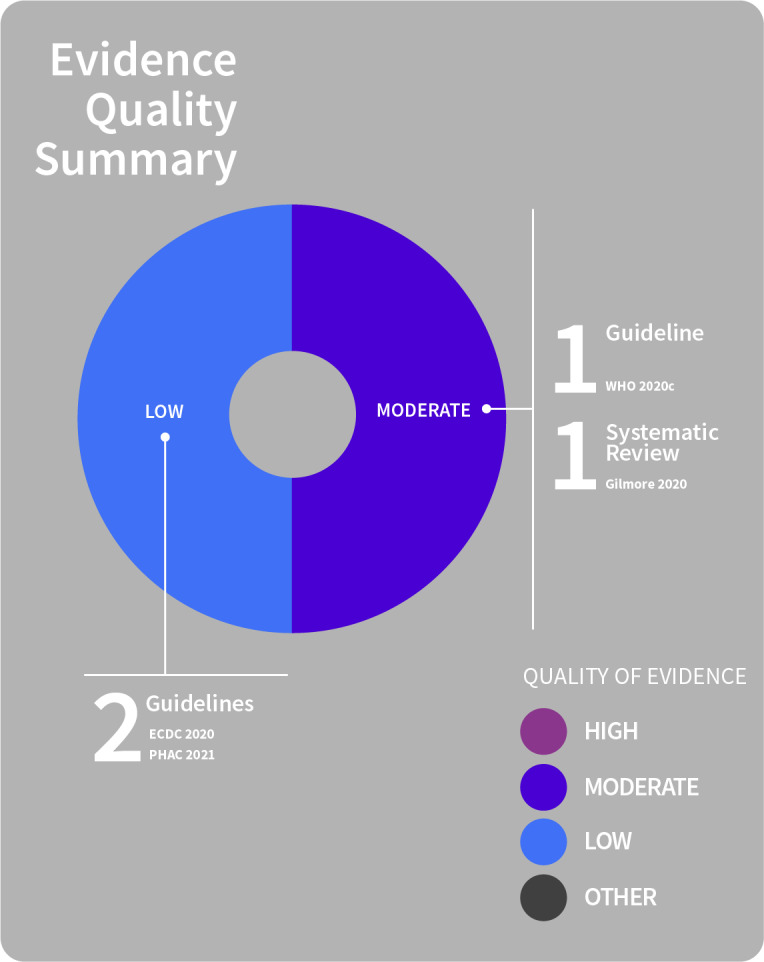
Pandemic fatigue
Around the globe, pandemic fatigue is increasing. As the pandemic continues into a fourth year, people are becoming less motivated to adhere to recommended protective measures and, as a result, people’s efforts to follow preventive measures may fall. Combined with negative news and information overload, efforts to stay informed may also decrease over time, raising further challenges for effective public health communication.
Pandemic fatigue is expected to continue to grow with the continuation of the pandemic, which can increase transmission and undermine the effectiveness of public health measures (ECDC 2020; PHAC 2021; WHO 2020c). This also increases the likelihood that stricter measures may be necessary in future to control transmission (ECDC 2020), but implementing and enforcing such measures in the context of high levels of pandemic fatigue is likely to be increasingly fraught for health agencies and governments.
Pandemic fatigue can be influenced by several factors, including growing complacency coupled with lowered disease risk perceptions, increased socioeconomic and psychological impacts of the pandemic, and public health measures, stress of uncertainty, becoming used to living in a pandemic situation, and decreased trust and confidence in authorities’ ability to control the pandemic (PHAC 2021; WHO 2020c).
Findings also show:
Addressing pandemic fatigue needs to be a key goal of risk communication activities, as engagement of the public is critical to the success of public health measures like physical distancing.
Identifying creative ways to engage and motivate people by partnering with local groups and leaders (community members who have legitimacy and are able to represent and influence the community) improves motivation and engagement and therefore adherence to measures (Gilmore 2020; WHO 2020c).
Since engagement of the public is critical to the success of public health measures, this is more likely to be achieved if the measures are clear, proportionate, transparent, and supported by quantified goals and epidemiological targets (ECDC 2020).
Changes in adherence, trust or acceptance over time
See Figure 28 for a summary of evidence quality for these findings.
28.
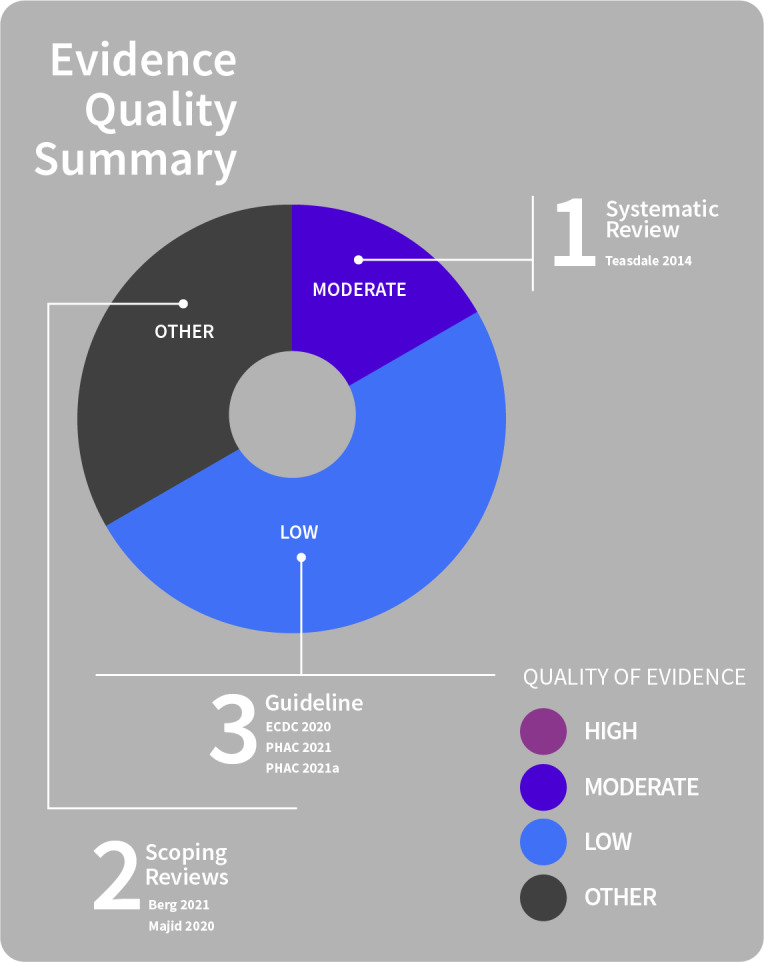
Changes over time
Public health communication is critical as public trust in health authorities and acceptance of/adherence to physical distancing measures change over time. These are related to perceptions of crisis management, which in turn can affect people’s risk perception and behavioural response (Berg 2021; Majid 2020).
Continuing public health communication is also critical, as how people assess risk during a pandemic and the effects on behaviour change over time (e.g. as numbers of articles on the pandemic declined), so too did willingness to adhere to measures such as physical distancing (Majid 2020).
Communications also change over the pandemic course, e.g. analysis of Twitter messages found these concentrated on instructional information in the early pandemic period but shifted to motivational messages to sustain behaviours in the longer term (focusing on the need to protect vulnerable populations) (Berg 2021). Qualitative research indicates that public anxiety is typically high when a new infection emerges but decreases over time. Diminishing anxiety over time can be influenced by people’s views of communications: where people become sceptical about the information provided to them (e.g. mismatches between people’s experience of the pandemic versus information released through official channels), communication may be viewed as unreliable, inconsistent, and alarmist, and lead people to disregard advice about preventive measures (Teasdale 2014). Such findings highlight the fluctuating nature of people’s risk perceptions and understanding as they experience a pandemic over time.
When public health measures change over time or temporarily (e.g. prior to religious or cultural festivals), flexible and up‐to‐date public health communication is key to providing guidance to the community about which measures apply, when, and how to protect themselves and others by mitigating the risk of disease transmission (ECDC 2020; PHAC 2021; PHAC 2021a).
Authorities need to find the balance between epidemiological risk and social and economic risk; and to balance apparently conflicting messages to the public which, on the one hand, convey information about relaxation of measures over key time periods (e.g. end‐of‐year festivities) and, on the other, advocate for restrictions to minimise epidemiological risk (ECDC 2020).
Adaptive and responsive ongoing communication
See Figure 29 for a summary of evidence quality for these findings.
29.
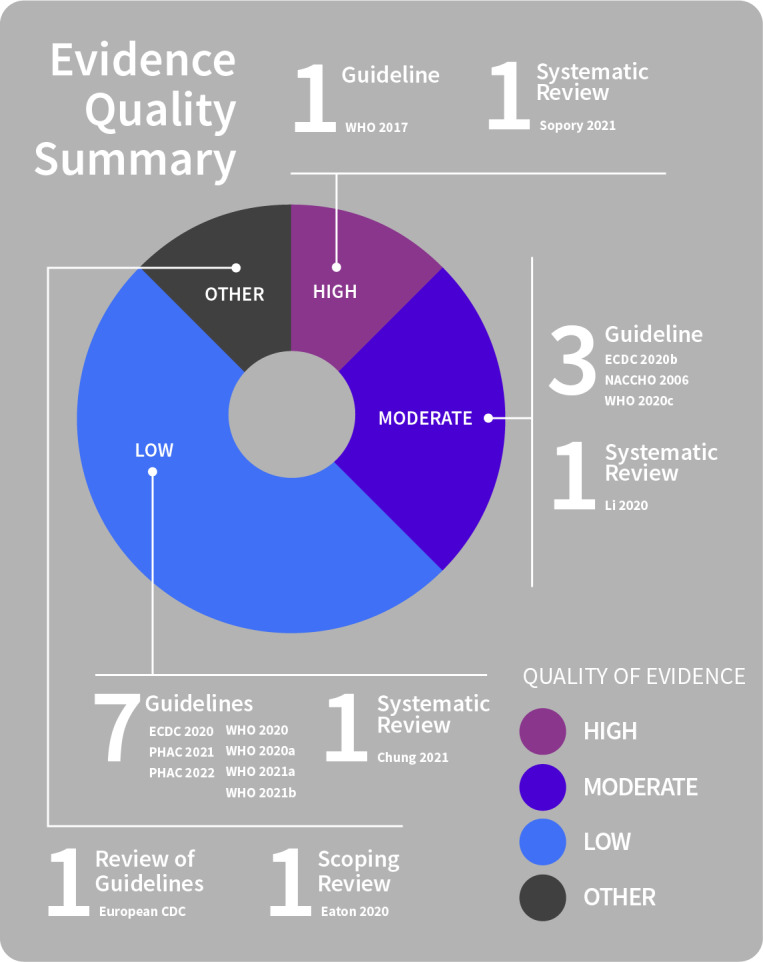
Adaptive and responsive communication
Proactive, accessible public communication about public health measures is needed over the course of a pandemic outbreak. There is a need for continuous updating of messages as new information becomes available, or the situation changes (pandemic status, impacts on essential services, when and how measures are being adjusted, rationale for changes, and when and how people can protect themselves) (Chung 2021; ECDC 2020; Li 2020; PHAC 2022; Sopory 2021; WHO 2020; WHO 2020a). Communication needs to clearly explain what is known and what is uncertain, and be translated into languages appropriate to both the community at large and to people housed within centres for refugees or migrants (ECDC 2020b; WHO 2020a).
Critically, information about public health measures must be up‐to‐date (Chung 2021; Li 2020; PHAC 2021; WHO 2021b), to promote accurate public knowledge about required public health measures and about how to comply with them at any given point in time (Eaton 2020; ECDC 2020g; NACCHO 2006; WHO 2017; WHO 2020; WHO 2020a; WHO 2021a). Mechanisms to monitor public perceptions of the outbreak and public health measures are also needed throughout the pandemic to allow these to be quickly identified and addressed (ECDC 2020g; WHO 2020; WHO 2020a; WHO 2021a).
Community engagement to sustain efforts
See Figure 30 for a summary of evidence quality for these findings.
30.
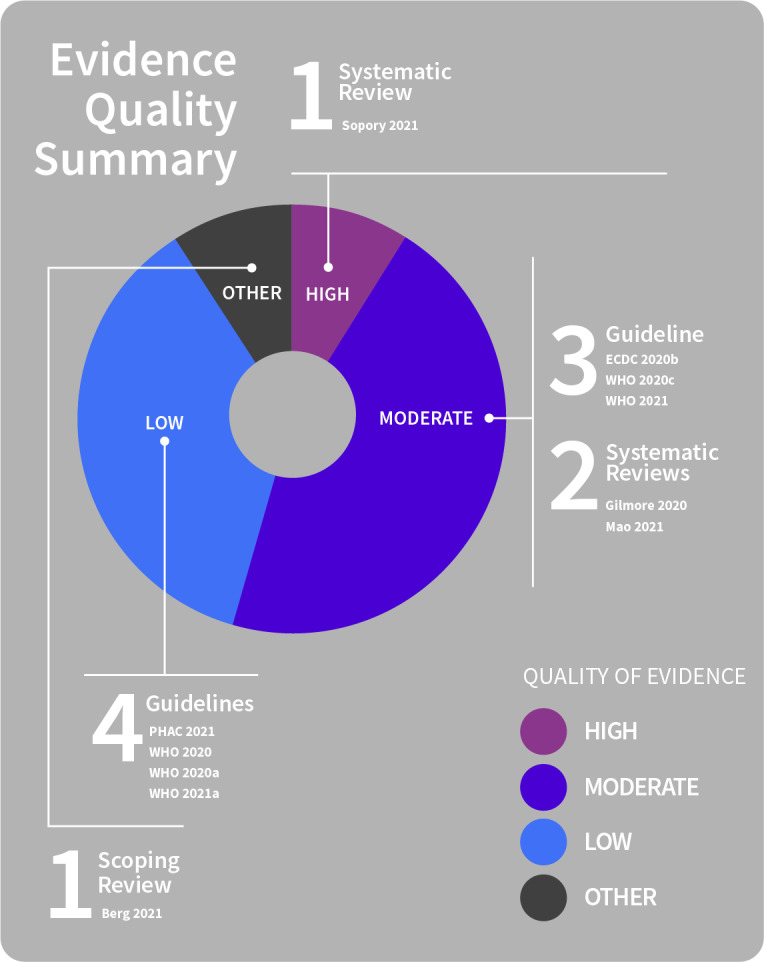
Community engagement for sustaining efforts
Health authorities need to work collaboratively with communities and trusted spokespeople to improve community trust, to ensure that messages are appropriately tailored to communities and reach different groups over time as the pandemic response changes (Berg 2021; ECDC 2020b; PHAC 2021; Sopory 2021; WHO 2020; WHO 2020c; WHO 2021a).
Two‐way public communication and engagement processes need to be ongoing, reassessed and modified over time as needed and as new information emerges (Gilmore 2020; Mao 2021; WHO 2020; WHO 2020a). When the local situation changes (i.e. changes in case numbers, situational assessment) and public health measures are changed in response, communities need to be regularly and fully informed, engaged and enabled prior to the changes occurring (WHO 2021a). Communication and support need to be planned and in place in advance of any introduction of or changes to public health measures, and communication (including messaging) about risk and/or social and behavioural changes occur regularly to keep the public informed about the situation (Gilmore 2020; WHO 2021a).
Such two‐way engagement with communities can help to support and sustain required public health measures over time and so improve acceptability and adherence to measures (WHO 2020a; WHO 2020c; WHO 2021), address misinformation and rumours (WHO 2020a), and enable feedback on societal impacts of public health measures and communications that can be addressed or communications tailored towards (WHO 2021a). Effective communication and engagement processes may help to address both existing and emerging issues (e.g. pandemic fatigue, economic and social pressures, changing levels of trust) which impact uptake and adherence to public health measures (WHO 2020c).
Discussion
Summary of main findings
Good public communication is a critical component of the public health response to a health emergency, such as a pandemic. This updated review draws on a substantial body of evidence (68 included studies) to provide expanded evidence on what good communication in public health emergencies might look like.
The assessed evidence stresses the importance of effective communication and engagement with the public in order to promote uptake and adherence to protective health measures, such as physical distancing. This has been well‐recognised by health agencies around the world for some time. However, at this point in the COVID‐19 pandemic, it is timely to reassess the evidence on pandemic communication and its role in mounting an effective community response. The need is clear for proper recognition, planning and resourcing for public health communication to ensure it is given attention now and in preparation for future pandemics, and considered alongside other implementation issues to protect public health.
Although this review focused on identifying effective communication strategies for physical distancing behaviours as a preventive health measure, the findings may also provide insights about effective public communication practices that can be applied to other protective measures and contexts. Many of the findings are unsurprising. For instance, the evidence indicates that the public need to be informed about how to protect themselves, and what they can and cannot do, in order to enact protective measures effectively. They also need practical supports to engage with, and adhere to, protective measures. Since preventive health measures change over the pandemic, with rising and falling waves of infection across communities, people also need to know how to protect themselves over time, as both risk and public health measures change. Other findings from this review are more nuanced, for instance, highlighting the importance of public trust (in authorities and government) underpinning the public health response and the communications related to it; the need for tailoring of communications and support to local contexts; the importance of considering equity (and inequities that exist within communities) when planning and enacting public health measures; and the key role of two‐way community engagement from the very beginning of the pandemic and over the subsequent weeks, months and years. These findings are comparable to several of the main recommendations arising from the recently‐published World Disasters Report (IFRC 2023).
The assembled evidence was organised into six separate but interrelated themes, and subthemes within each. A summary of each is provided below and may inform approaches to and implementation of public health communication upon recognition of a public health emergency such as a pandemic outbreak, and throughout the emergency response.
Theme 1: Strengthening public trust and countering misinformation: essential foundations for effective public health communication
Public trust in the authorities is essential.
Building and maintaining public trust is an essential element of effective pandemic communication.
Efforts should be made by authorities to maximise public trust prior to an outbreak or introduction/changes to public health measures, to help promote adherence to preventive measures.
Facilitators of public trust
Factors that positively impact trust include:
providing clear, timely and consistent information that is accessible and disseminated widely;
transparently communicating about what is known and what is uncertain;
communicating the commitment to base decisions on the best available scientific knowledge and regularly communicating epidemiological data;
adopting person‐centred community‐led approaches;
assuring protection of privacy and personal information.
Barriers to public trust
Factors eroding public trust include conspiracy beliefs; worries about accuracy of information reported; and worsening inequalities.
Public health messaging is less trusted when it:
includes overstatements or exaggerations;
fosters fear;
appeals to authority;
repeats myths or misinformation;
relies heavily on statistical information;
changes frequently or drastically over time.
Sources of misinformation
Misinformation can negatively affect preventive measure uptake. During pandemics, misinformation can spread quickly if there is:
lack of ready access to accurate information (people then seek information from less reliable sources);
inadequate information to support informed decisions about measures;
conflicting/contradictory public health messages.
Some sources, specifically social media, are more likely to spread misinformation than others.
Addressing misinformation
It is critical that authorities and the media adopt co‐ordinated strategies to identify and counter misinformation. Providing the right (clear, accurate, consistent) information at the right time, to the right people via trusted, credible channels is essential to clarify misconceptions.
Community leaders, healthcare providers and the media are all important for communicating consistent information about preventive measures.
Implementing mechanisms to monitor and address misinformation and respond to public questions/feedback is also key for:
monitoring changes to knowledge, beliefs and behaviours; and
informing future communication and information strategies i.e. tailored based on analysis of public risk perceptions, areas of uncertainty/inaccuracy or misinformation.
Theme 2: Two‐way‐communication: involving communities to improve the dissemination, accessibility and acceptability of information
Community involvement is key in response planning, communication and reach of messages.
Physical distancing uptake and adherence are influenced by many factors. Community engagement is key to understanding local context (people’s concerns, attitudes, beliefs, barriers to protective measures) to ensure an informed, appropriate response. Without community involvement, misinformation, confusion and mistrust can undermine public health efforts.
Communities should be involved in all stages (planning, design, implementation, monitoring and evaluation) of local COVID‐19 responses and aim to balance community needs and benefits of measures against potential harms.
Community engagement might entail sustained two‐way involvement to design and implement communication strategies, alongside mechanisms for community feedback to monitor knowledge, beliefs and practices and adapt the course as required. This helps to build community trust but requires structures and processes to be in place. Similarly, tools and guidance are needed to strengthen community engagement, and build on existing trusted relationships.
Community involvement underpins effective tailoring of measures and communications.
Public health communication should be:
flexible and responsive;
calibrated to local setting and context;
reviewed regularly;
adapted to the local community;
tailored to the intended audience.
Communication about preventive measures should be developed with communities in whom the measures are to be enacted.
Messages in clear, simple language are needed that:
encourage information sharing; and
focus on actionable messages (what people can do).
Absence of contextual tailoring of communication can mean vulnerable groups’ needs are not adequately considered in decision‐making.
Efforts to ensure that vulnerable people are engaged in developing and implementing response measures and communication are also needed.
Theme 3: Development of and preparation for public communication: target audience, equity and tailoring
Target audience and setting for communications
Public communications about physical distancing measures must consider the context, settings, and different audiences in a population, because these factors influence adherence.
Including details specific to communities, such as information about whom, when, where and how measures are to be implemented, are critical elements, so that information is sufficient to support informed decisions about preventive measures.
Tailoring communications
Public health communication tailoring is critical in reaching and informing more of the community, including those for whom information access is unequal.
Recognising population groups who are more likely to be non‐adherent to preventive measures can help public health authorities to identify target populations for pandemic prevention and education efforts.
Information needs to be:
adjusted for delivery e.g. sign language for people with disabilities;
provided via a range of formats;
accessible (follow accessibility standards (clear, non‐technical terminology and language)); and
be disseminated through several channels (mass media, digital, written).
Communicators must also be appropriately skilled and trained.
Tailored messages should be pre‐tested with members of the intended audience, to ensure appropriateness (acceptability) and effectiveness (accurate understanding).
General equity considerations in communication
The need to communicate comprehensively and clearly to a population, as well as to specific community groups, arises because knowledge and adoption of preventive behaviours are not evenly distributed and a consistent pandemic response cannot otherwise be mounted.
Several factors influence community awareness of preventive messages which, in turn, influences behaviours. Public health communications need to account for these factors, and deliberately plan to address inequalities to ensure that communication is as equitable, and achieves as much reach, as possible.
Equity issues for specific population groups
So that information and communication inequalities are not amplified, communications and preventive measures must be designed, adapted and implemented to reach groups who are less likely or less able to take up measures (such as hard to reach/vulnerable populations or those facing cultural or language barriers or educational inequalities).
Theme 4: Public communication features: content, timing and duration, delivery
Content of public information and communication
To improve uptake and adherence to physical distancing measures, authorities need to communicate information to the public that is:
comprehensive;
clear; and
consistent.
This needs to include:
a clear, accurate rationale for the required measures;
how to comply (what to do to protect health); and
services available to support the measures.
Such information must be:
accessible and timely;
provided prior to the implementation of the measure(s); and
clearly explain changes to measures over time.
Effective risk communication might occur via several modes and consider that:
visualisations (e.g. graphics, images) may help to convey the meaning of technical epidemiological data and can significantly influence the reach and reception of messages (e.g. reaching people with lower literacy);
statistical information might be more accessibly presented in words.
Information that is inadequate or insufficient, contradictory (inconsistent), confusing or hard‐to‐find negatively affects acceptance, acceptability and adherence to preventive measures.
Communicating with empathy to the public and acknowledging the difficulties of following public health advice is critical.
Emphasis of content on public health benefit may promote acceptance
Public communications may promote acceptability of and adherence to measures by developing culturally competent, context‐specific strategies emphasising:
public health benefits and importance of measures;
altruistic nature of following prevention measures; or
contribution to keeping everyone in the community safe (collective responsibility, social connectedness, solidarity).
Timing of communications and duration of measures
Knowledge and attitudes change over time.
Communication about public health measures is needed throughout a pandemic, including:
immediate initial communications (as early as possible), so that people can act to protect themselves even if information is incomplete;
openly communicating about uncertainty over time; and
continuously updating communications as new information becomes available.
Critically, information about public health measures must be kept up‐to‐date to promote accurate public knowledge about required measures and about how to adhere to protect health.
Public health messages also need to raise awareness that advice is continually changing, in response to an evolving pandemic.
Communicating duration and rationale for measures
Public communications need to signal the duration of new preventive measures or adjustment of existing measures, and clearly explain and justify the rationale for them before measures change.
Public health messages need to consider public expectations, particularly where there is uncertainty that may require restriction extension. Unexpectedly extending restrictions can negatively affect adherence, whereas public acceptance might be promoted by communicating the anticipated end date, together with the message that measures may need continuation, but decisions will be based on public safety.
Employing multiple delivery mechanisms
Public information that is credible, accurate and accessible, and disseminated using a range of formats or channels (digital, mass media, written), to reach different parts of the community, including disadvantaged groups and those without Internet access, is required. Using trusted lines of communication to convey information to the public is also key.
Information provided from different sources is more likely to be trusted and acted upon than from a single source. Providing information via multiple credible sources appears key, but it is imperative that messages convey consistent information.
Several simple, practical measures can also be used to reinforce and remind people of physical distancing measures, including:
visual cues (e.g. markings at appropriate distances for spacing);
directional marking (e.g. one‐way flow to reduce number of contacts);
signage to support preventive messaging (e.g. maintain the greatest possible distance); or
noise reduction strategies enabling people to interact at a distance.
Theme 5: Supporting behaviour change at individual and population levels
Uptake and adherence to physical distancing measures requires behavioural change from individuals and entire communities. Knowledge of what is needed, why, and how to go about it is essential, as is a range of supports, tailored to redress inequalities.
Communication to influence social attitudes and norms
Public sentiment is key and relies on the public understanding preventive measures’ benefits and potential harms.
Communication targeting multiple (population and individual) levels, taking broader social and structural systems into account, and reinforcing positive social attitudes and norms towards physical distancing (e.g. strong social pressure to adhere) may be necessary to promote sustained behavioural changes.
Communication to address stigma and lack of acceptance of public health messaging
Stigma or discrimination may undermine the effectiveness of public health messages, slowing or preventing enactment of preventive measures.
Stigma needs to be proactively monitored and addressed. Disseminating contextualised information to the community to improve knowledge, counter misinformation, emphasise that an emerging disease places everyone at risk, and reinforce respect, may be helpful.
Communication to influence perceptions of vulnerability and risk
People’s perceptions of preventive measures and risk (perceived personal vulnerability, transmission, severity) influence acceptance, uptake and adherence.
Regular public communication addressing common beliefs or concerns about the necessity and effectiveness of measures, and addressing key barriers (e.g. personal vulnerability perceptions) is most likely to improve adoption of measures. Communicating the immediacy and susceptibility of a risk, may also improve adherence.
Communication strategies may be most effective when emphasising the impact of non‐adherence to preventive measures on identifiable people (e.g. vulnerable people) and numbers of infections.
Essential services to support quarantine or isolation
Public communication acknowledging the difficulties of adhering to restrictive measures is needed, together with reassurance that appropriate supports will be available.
Support systems must ensure easily accessed essential supplies and services, including food, water, medications and specialist services (e.g. financial support, mental health support).
Information about services and support needs to be communicated widely so that people are well‐informed about:
what services exist;
who is eligible; and
how to access services.
Information about supports should be tailored and consider health literacy levels, and needs of specific populations or vulnerable groups.
Supports should be easily accessed, as difficulty accessing support reduces adherence.
Financial insecurity and support
Financial losses due to the need for physical distancing measures are a common risk factor for psychological distress which can lead to non‐adherence.
Implementation of preventive measures needs to be balanced against socioeconomic impacts, particularly in settings highly dependent on daily wages and the informal economy, or where social disparities exist.
Financial support is critical to promoting adherence to preventive measures and can take different forms (e.g. partial/full income replacement, flexible leave/payment). Cost is otherwise a major barrier.
People in disadvantaged groups need tailored financial assistance to undertake protective measures and are particularly vulnerable if financial support is delayed.
Theme 6: Fostering and sustaining receptiveness and responsiveness to public health communication
Pandemic fatigue as a barrier
Over time, pandemic fatigue negatively impacts adherence to preventive measures. Growing complacency, lowered risk perceptions and falling confidence in the authorities’ ability to control the pandemic may contribute to fatigue, alongside socioeconomic and psychological impacts of the pandemic and public health measures.
Addressing pandemic fatigue should be a key goal of communication activities. Creatively engaging and motivating people through local partnerships may be beneficial, and more likely to be achievable if the measures are clear, proportionate, transparent and supported by quantified targets.
Changes in adherence, trust or acceptance over time
How people assess risk, their views of communications, and effects on behaviour fluctuate as they experience a pandemic over time.
When public health measures change, flexible, up‐to‐date public health communication is key to providing guidance about which measures apply, when, and how people can protect themselves and others.
Authorities need to find balance in communicating apparently conflicting public messages when measures change, i.e. on the one hand, conveying information about relaxation of some measures and, on the other, advocating for maintenance of certain restrictions to minimise risk.
Adaptive and responsive ongoing communication
Proactive, accessible public health messages should be continuously updated as new information emerges or the situation changes (e.g. essential service impacts), so that people know how to protect themselves at any given point in time.
Ongoing mechanisms to monitor public perceptions of the pandemic and preventive measures are also needed so that communications can be adjusted to community needs over time.
Community engagement to sustain efforts
Health authorities need to work collaboratively with communities and trusted spokespeople to maintain community trust, appropriately tailor messages and ensure community reach as the pandemic response changes.
Overall completeness and applicability of the evidence
This systematic overview provides evidence on the range of communication approaches to promote and support the use of physical distancing measures throughout a pandemic. Much of this evidence highlights the critical role of high‐quality public information and communication during a public health emergency such as the COVID‐19 pandemic. This requires planning, consistent messaging, continuous updating as information or public health measures change, and the involvement of communities as well as public health experts in planning and delivering communications.
The evidence assembled here can be used to inform decisions about how best to communicate (range of strategies and/or purposes), how to more successfully reach more people (to whom), and how to maximise the chances that public communications can effectively promote and support required preventive measures (what features make communication most effective). It consistently indicates that there are features of better public health communication that can be applied, irrespective of the type of communication itself, and which are key to the communication's effectiveness in promoting and supporting behaviour change by individuals and communities. The findings of this overview can therefore inform decisions about how best to frame the content, currency, timing and context for communications, in order to promote uptake and adherence to preventive measures.
The rapid spread of COVID‐19 across the world has emphasised the necessarily interconnected nature of disease control and public health planning. The findings of this overview echo, and draw on, those of comprehensive pre‐COVID‐19 guidelines for pandemic preparedness (e.g. JHCHS 2019; NACCHO 2006; WHO 2017). They are also consistent with the findings of emerging reviews assessing the pandemic response to COVID‐19 (e.g. IFRC 2023, IPMAC 2022; Shergold 2022). By drawing together evidence from across the globe, across guidelines and diseases, this overview helps to further consolidate these earlier lessons with more contemporary ones, and to provide guidance for future pandemic or public health emergency planning.
The addition of new reviews and guidelines in this update has strengthened and extended many of the findings of the original review, and has also filled many of the evidence gaps originally identified. For instance, this update includes substantial bodies of evidence on how to communicate and support vulnerable populations (defined inclusively) alongside the general public; the requirements of responsive public communication and support occurring over time as the pandemic waxes and wanes within communities; communication to promote and support school and workplace measures; proactively addressing stigma associated with physical distancing measures; and the role and importance of two‐way community engagement. These were all areas identified as gaps in the original review.
Although this update adds a large body of evidence, a number of knowledge gaps are still evident. Persistent gaps include those on the role and implementation of financial incentives to promote adherence to measures (and, conversely, financial disincentives for failure to adhere), approaches which may be used by governments. Communication to promote uptake and adherence to contact tracing was relatively sparsely populated with evidence, but new findings did emphasise the need to ensure privacy and protection of personal information in the context of contact tracing systems. Evidence on communication related to some specific contexts (e.g. public transport) was not identified in the current update. However, many of the findings of this synthesis are applicable across diverse settings and populations and might offer lessons for effective communication in diverse contexts.
It is also important to note that at the time of publication of this update, approximately 24 months had elapsed since running searches for new evidence. The COVID‐19 pandemic period has seen huge growth in the volume of related research and, although communication related to physical distancing is only one area of focus, there will undoubtedly have been further evidence to emerge since August 2021. We did not have the resources to update the searches for this review update, and this is a limitation that could be addressed by future reviews in this area. As it stands, however, this high‐level synthesis draws on a very large volume and range of literature related to COVID‐19 as well as other selected infectious diseases, and can inform both current and future planning for public health communications.
One further noted gap was the lack of research considering the impact of public communication on the pandemic by some public figures (e.g. researchers, decision‐makers) and their subsequent stigmatisation or labelling as providing 'misinformation' through social media. Such potential harms for those involved in communicating with the public about the pandemic is an area where research would be valuable.
An issue emerging from the pandemic, and which remains a major gap in knowledge, relates to people at heightened risk due to COVID‐19 (e.g. due to old age, frailty, chronic health conditions, immunosuppression). In the context of changing public health advice, for instance adjustment of public health measures in response to decreasing or increasing levels of community transmission, people in these groups have been required to maintain protective measures (e.g. isolation, face masks) to protect their health (Ryan 2023). Evidence assembled here addressed the needs of vulnerable groups at a general level, but did not identify evidence to inform more direct policies on how best to communicate with or support people from these groups, or how to tailor information to enable informed decisions about the personal risk of COVID‐19 for those at heightened risk. This is a major gap as people in these groups may remain isolated from the rest of the community for lengthy periods, and this is known to be associated with poor social and psychological outcomes (in addition to existing physical vulnerability to infectious disease).
While this synthesis highlights the importance of developing targeted public health messages that are tailored to specific communities and disseminated through multiple channels and formats, there was relatively less evidence on the use of diverse formats and tools to support pandemic communication. Some evidence suggests adaptations like the adoption of visual communication to overcome literacy barriers, or written information to improve accessibility of community information, may be beneficial. Finally, the original review noted a lack of evidence on the relative effectiveness of different community engagement approaches. This has been a gap in research noted for some time and, while the updated evidence assembled here does not provide a definitive answer, it does indicate a range of features of good practice for engagement approaches. This includes involving the community in two‐way partnership‐style dialogue on pandemic measures and the communications related to them; planning to engage the community in all decisions related to measures and communications (i.e. in planning, designing and implementing, and ensuring responsiveness to community feedback); the need to engage with the community over time; and to ensure diverse representation from community members (including people living with disability and from other vulnerable groups). These findings could guide decisions about how to more effectively engage with communities about public health measures and related communications.
New evidence has also been added in this update to expand what we know about communicating with a range of specific audiences. This includes vulnerable groups within communities, older people, and those from ethnically diverse backgrounds, including migrants and refugees. Included studies are drawn from countries across the world, although not all studies contributed evidence to all main findings. Again, as in the original review, there is a preponderance of studies undertaken in high rather than lower‐income countries and this may limit the applicability of the evidence to the relatively wealthier parts of the world.
Quality of the evidence
This overview aimed to identify communication approaches, and their features, to promote and support the enactment of physical distancing measures. It includes guidelines, primary and secondary research, and qualitative and quantitative research as sources of evidence to address this purpose. Both qualitative and quantitative research was included. This approach can be useful as, for instance, qualitative findings can help to identify key issues for consideration, such as enablers or barriers to the adoption of particular communication strategies, or differences in the experiences of pandemic communication across different groups within communities.
However, the inclusion of both primary and secondary research of different designs does make it difficult to formulate concrete conclusions about the overall quality of the evidence. Although quality was assessed for each of the included pieces of research in this review, assessment was undertaken primarily to provide review readers with an indication of the methodological strength of the research contributing to each of the main findings. These ratings are not intended to imply a hierarchy of evidence quality; nor to form the basis for further formal assessment of evidence certainty (for example, using the GRADE/GRADE‐CERQual approach), as it was neither possible nor meaningful to do so with the evidence assembled here.
Instead, assessments of methodological quality are intended to assist with interpretation of the findings. More specifically, their purpose as reported, is to flag for readers the breadth of evidence contributing to each section of the results and to indicate that there may be limitations from a methodological perspective in the assembled research. For example, this update focused on synthesised (reviews and guidelines) forms of evidence as these often represent analyses of some (often large quantities) of the best available evidence in specific topic areas. However, even the synthesised evidence sources included in this review were of variable quality (mainly being rated as having low or moderate levels of quality).
One of the strengths of this review is that major themes and findings emerged from multiple data sources, and often with similar findings being reported or highlighted by both quantitative and qualitative data. This increases our confidence that the findings are coherent across different research designs, as well as across diverse populations and settings. Additionally, the findings from this update of the review are consistent with, and build on, those of the original rapid review undertaken in 2020. The update adds substantial evidence to the major findings from the original review and fills several major gaps. It has also added more detail and breadth to those findings already reflected in the original six themes. This increasing coverage and depth of the updated findings resulted in the original themes being substantially revised to more appropriately represent areas where there was a large amount of new information. Clear identification of the original themes and issues in the data, and a progressive building on these, additionally adds to our confidence that the findings of this update are coherent across diverse sources of evidence.
Potential biases in the review process
This version updates a rapid review of evidence. Our methods followed those of the original review (Ryan 2021a) and the publicly‐available protocol (Ryan 2021b) closely, with any changes in approach noted.
The choice of methods for the original rapid review was made based on the need for the review to be undertaken quickly and pragmatically while ensuring a high‐quality review from the process. Since the review question required consideration of evidence from multiple different study designs (i.e. qualitative and quantitative), our methods were informed primarily by the McMaster 30‐day rapid response model (Wilson 2018), which is a model for synthesising evidence systematically across diverse types of evidence and disciplines. Methods were also guided by Cochrane rapid review methods (Garritty 2021).
Searching for relevant evidence was challenging due to the breadth of 'communication.' This came about because we deliberately used a comprehensive definition of communication from the outset; and because of the diverse ways in which communication could be operationalised in the literature. The different forms of evidence eligible for inclusion in this review, and the huge volume of available research related to COVID‐19, were also challenging. We searched widely for relevant studies, including electronic databases, grey literature sources, and citing literature from relevant papers. Nevertheless, it is possible that we failed to identify eligible papers and this may have had an effect on the findings.
Screening of studies for inclusion was also challenging. We developed decision rules to operationalise the selection criteria, and refined these iteratively in several rounds of study selection. While preliminary screening was undertaken by a single reviewer, our checks of this method indicated a high level of agreement when selecting studies based on titles and abstracts. All subsequent steps were undertaken by two review authors, with discussions to reach consensus about areas of uncertainty. In general, relevant physical distancing measures were clearly identifiable in papers and decisions about eligibility based on the measures were relatively straightforward. The most challenging aspect of screening was determining whether individual papers were clearly focused on one or more communication element, and where the threshold for inclusion lay. We collaboratively and iteratively refined selection based on communication elements, excluding studies without a major focus on communication, e.g. papers that mentioned communication but only in passing or as one small element of a much larger strategy or approach. This decision was reached in order to maintain the overview's focus on communication related to pandemic measures. While these decisions were undertaken by two authors working collaboratively to reach agreement, such decisions may be made differently by other researchers undertaking this review. While we made every effort to ensure consistent, transparent decisions about inclusion, it is possible that this introduced bias.
All data extraction (including quality assessment) and synthesis steps were undertaken by two authors to minimise errors or oversights. This is a strength of the review and important for quality assurance as the review included a large volume of descriptive information and data, without which there may have been errors or omissions introduced to the review.
Synthesis steps followed the reporting guidance of the SWiM guideline (Campbell 2020) as far as was possible, the aim of which was to transparently report and present data. Data were therefore tabulated to report information for each study in a consistent and structured way. Data were also translated at this stage to identify which question components were relevant, and to identify the communication purpose(s) of the study, and each study was mapped to one or more of the original six thematic categories to enable grouping for preliminary analysis and synthesis of findings. Preliminary analysis of the data according to the original thematic framework was undertaken, and then refined in consultation with the wider review team. All steps were undertaken by one author, and checked for accuracy by a second author. Errors are therefore unlikely to affect the findings in important ways, but, it is possible that another review team analysing the same data might develop different themes and/or highlight different major findings to those we have identified.
We planned at the outset of this review to use a staged approach to study selection (i.e. one that would enable systematic screening of primary as well as synthesised evidence sources). The breadth of communication as a topic area and massive growth in research related to COVID‐19 meant that we identified a high volume of primary studies from our searches (reflecting 18 months approximately of updated searches: from May 2020 to August 2021), alongside numerous reviews and guidelines. We therefore decided to focus on evidence drawn from synthesised sources for this update. It is possible that inclusion of the additional body of primary research may have allowed slightly more nuanced messages about communication to have emerged from the findings, or contributed to findings where gaps in the evidence still exist. However, given that many of the primary studies identified as potentially eligible for inclusion were fairly small surveys of very specific community population groups from diverse countries, it is not clear that the bulk of this research would have substantially changed (expanded or added depth to) the main findings of this overview.
Our searches for evidence for this update were undertaken up to August/September 2021 and, in the intervening period, research relevant to this review is likely to have become available or, in the case of guidelines, been updated. This too may have filled some of the gaps that still exist in this review, and may influence the major findings.
Considerations for decision‐makers
This review focused on communication, broadly defined, in the context of a pandemic. The assembled evidence identifies a range of key features of public communication that may inform public health decision‐making during a pandemic. It is important to be clear, however, that public communication happens within a broader, complex social and political environment, and the influence of these factors vary greatly across countries and regions globally (IFRC 2023). Such factors affect how physical distancing measures are enacted within communities, and have a complex relationship with many of the key findings of this review. For instance, factors such as financial and social inequalities can prevent the uptake of preventive public health measures by individuals, particularly under‐served groups or whole communities, and it is therefore imperative that decision‐makers consider the broader local context when implementing public health measures and the communications related to them.
The findings of this review describe a range of consistent features of public health communication to promote and support physical distancing measures that might improve acceptance, uptake and adherence to the measures. These communication features could be applied to public communications, and the preparatory work beforehand, as well as measures to sustain effects after the communication itself, irrespective of the type of communication or medium used, and may also help to inform public communications for other preventive measures. Incorporating these features can help to ensure that public communications have the best chance of success; that is, that they meet identified requirements for communication and avoid mis‐steps that may otherwise occur.
From the review's findings, the main considerations for policy and decision‐makers, in the fields of government, public health, and other healthcare organisations tasked with enabling such preventive measures, and working closely with communication teams, are as follows:
Recognising and working to build and maintain public trust over time is critical, as this underpins the success of public health communications, and therefore, the effectiveness of public health prevention measures.
Two‐way communication (engagement) with the public is needed over the course of a public health emergency: at first recognition of a health threat (despite existing uncertainties), and regularly as public health measures are introduced or adjusted. Engagement needs to be embedded at all stages of the response and inform tailoring of communications and implementation of public health measures over time.
Communication and information must be tailored to reach all groups within populations, with explicit consideration of existing inequities and the needs of disadvantaged population groups, including those who are underserved, vulnerable, from diverse cultural or language groups, or who have lower educational attainment. Awareness that the implementation of public health measures may magnify existing or emerging inequities is also needed in response planning, enactment and adjustments over time.
Public communication needs to be based on clear, consistent, actionable and timely (up‐to‐date) information about preventive measures, including the benefits (whether for individual, social groupings or wider society), harms (likewise) and rationale for use, and including information about supports available to help follow the recommended measures. Communication needs to occur through multiple channels and/or formats in order to build public trust and reach more of the community. Communication also needs to clearly convey uncertainties at any given point in time.
Implementation of public health measures must happen alongside provision of practical supports and services (e.g. essential supplies, financial support). Information about available supports must be widely disseminated and well understood. Supports and communication related to supports and services require flexibility and tailoring to consider community needs and include vulnerable groups' needs. Proactively monitoring and countering stigma related to preventive measures (e.g. quarantine) is also necessary to promote and support adherence.
Efforts to foster and sustain public receptiveness and responsiveness to public health communication are needed throughout a public health emergency. Recognising that trust, acceptance and behaviours change over time and that communication is required to be adaptive and responsive to meet changing needs is critical, alongside community engagement efforts to inform communication and public health response measures.
These measures should be evaluated and adapted according to evidence of effectiveness, evidence of inequalities emerging, changing context and needs of whole or particular under‐served populations.
Authors' conclusions
Implications for practice
From the review's findings, the main considerations for policy and decision‐makers planning and implementing communication about a public health emergency and measures to protect the community are as follows:
Recognising the critical role of public trust is essential. Trust needs to be built and maintained over time in order to successfully communicate with communities about public health preventive measures.
Two‐way public communication (engagement) is needed from the earliest point where a health threat is first recognised and occurs regularly over time, to inform tailoring of communications and implementation of preventive health measures.
Tailoring communication and information to reach all groups (including underserved, vulnerable, diverse cultural/language, lower education levels) and considering existing inequities is needed when planning and implementing the public health response.
Public communication needs to be based on clear, consistent, actionable and timely (up‐to‐date) information about preventive measures, including the benefits (whether for individual, social groupings or wider society), harms (likewise)and rationale for use, and including information about supports available. Communication needs to occur through multiple channels and/or formats to build public trust and reach more of the community.
Implementing public health measures together with practical supports (e.g. essential supplies, financial support) is critical. Ensuring the community knows how to access supports, and that supports and communication are flexible and responsive to different groups' needs is also key. Proactive monitoring and countering of stigma related to preventive measures (e.g. quarantine) is also needed to promote and support adherence.
Efforts to foster and sustain public receptiveness and responsiveness to public health communication are needed throughout a public health emergency. Communication needs to be adaptive and responsive to meet changing needs, alongside community engagement efforts to inform communication and public health response measures.
Implications for research
The COVID‐19 period has seen a massive growth in the volume of research, both primary and secondary, related to the pandemic. Research is needed to fill gaps in particular areas, with resources directed to conducting high‐quality, meaningful research in these areas rather than to those where there is already an abundance of studies of variable scope and quality.
Based on the evidence assembled here, further research might usefully investigate gaps related to communication during public health emergencies:
Exploration of the needs and experiences of people at heightened risk of a public health emergency such as COVID‐19, who may need to continue to observe protective measures over prolonged time periods, alongside the majority of the community returning to life as usual.
Investigation of the barriers particular to lower‐ and middle‐income countries in relation to public communication and implementation of protective public health measures during an emergency (and over time), and how to address these barriers.
Assessment of the role of good communication in promoting uptake and adherence to preventive measures in specific settings, particularly those with implications for known societal inequities, such as access to healthcare, safe use of public transport and safe working environments and conditions.
Research on the duration of effectiveness of the communication measures described, and of interventions to sustain their effectiveness over time as is needed in pandemic and other public health emergency situations.
Acknowledgements
Authors of the original review not contributing to this update: Dianne Lowe, Nami Nelson. The original review was commissioned by the WHO European Office in March 2020.
We are grateful to members of the eCOVID19 Recommendations Map (https://covid19.recmap.org/; eCOVID19 RecMap) team, for assistance with sharing a list of potentially‐relevant guidelines to us for screening in this update; and to the eCOVID19 RecMap critical appraisal team who critically appraised eligible guidelines and shared the results of these appraisals.
We are also grateful to review and study authors who generously responded to requests for information or access to reports.
Finally, we would like to thank Simon Murray of fieldnotes.work for developing and creating the visual quality of evidence snapshots for our review findings.
Editorial and peer‐reviewer contributions
Cochrane Consumers and Communication supported the authors in the development of this review. The following people conducted the editorial process for this review:
Sign‐off Editor (final editorial decision): Sascha Köpke, Institute of Nursing Science, University of Cologne, Medical Faculty and University Hospital Cologne, Germany;
Managing Editor (selected peer reviewers, provided editorial guidance to authors, edited the article): Joey Kwong, Cochrane Central Editorial Service;
Editorial Assistant (conducted editorial policy checks, collated peer‐reviewer comments, supported editorial team): Lisa Wydrzynski, Cochrane Central Editorial Service;
Copy Editor (copy editing and production): Anne Lethaby, Cochrane Central Production Service;
Peer‐reviewers (provided comments and recommended an editorial decision): Annemiek Hammer, VU University Amsterdam, The Netherlands (clinical review), Stella O'Brien (consumer review), Meryem Malik, Harvard University (clinical review), Jo Platt, Cochrane Evidence Production & Methods Directorate (search review), Chantelle Garritty, School of Epidemiology and Public Health, University of Ottawa (methods review), Robert Walton, Cochrane UK (summary version reviewer).
Appendices
Appendix 1. Vulnerable groups within populations
The following comprehensive list of people considered vulnerable in the context of the COVID‐19 pandemic is taken directly from WHO 2020c (COVID-19 Global Risk Communication and Community Engagement Strategy – interim guidance (who.int) Dec 2020).
Older people (> 60 years): who may be unable to access adequate information and health services; need support of caregivers; not understand public health information; have difficulty physically distancing (e.g. assisted living facilities).
People with pre‐existing medical conditions: who may not have access to information about why they are at heightened risk.
Children/young people: may not have access to information or understand required behaviours, and may be amongst the most affected by preventive measures (e.g. school closures).
Ethnic/monitory populations: may not have ready access to information in own language, or face stigma/discrimination in healthcare settings.
Disadvantaged populations (e.g. gender‐based violence survivors, homeless, mental health conditions, sexual and gender minorities, women and girls): who may face disruption of services/support; isolation; lack of understanding of information on preventive measures; exclusion from decision‐making; restricted access to information due to limited education and language learning opportunities.
People deprived of their liberty (e.g. prison, detention centres): may have limited information or opportunities to ask questions, and lack trust of facility staff and information.
People living within humanitarian crises (e.g. refugee camps): access to essentials (e.g. shelter, food, protective supplies) may be disrupted; and timely and accurate information may be lacking due to isolation or language barriers.
People living in overcrowded spaces (e.g. slums, dormitories, urban poor): physical distancing may be difficult with overcrowding/movement of people between dwellings; may be higher levels of distrust of government; lower levels of education and health literacy, all of which may impede access/understanding of public health information and required measures.
People with disabilities: amongst the most marginalised (i.e. live in poverty, higher rates of violence, neglect and abuse); excluded from decision‐making; unequal access to information or available services (particularly those with specific communication needs).
People working in confined conditions (e.g. factories, abattoirs, meat‐packing plants) or informal economy: may be unable to follow physical distancing measures and/or measures may be poorly regulated. Public health information may not be readily available.
Refugees and migrants: may face legal hurdles, discrimination and language barriers which prevent understanding of public health information; may not be included in national response plans; and may be difficult to reach (i.e. mobility which may include cross‐border movements).
Appendix 2. Planned sequence of screening activities
Sequence of review search activities
In the original review, screening was undertaken sequentially in order to identify relevant evidence.
In short, screening was conducted in two phases:
Phase 1: systematic reviews and guidelines (COVID‐19, SARS, MERS, influenza, TB, Ebola)
Phase 2: primary studies to fill gaps in the phase 1 evidence (COVID‐19 only)
The table below outlines the sequence of search activities used for the original review.
We planned to follow the same process for this update. However, screening identified a very large number of synthesised evidence sources (SRs and GLs) in the updated searches. We therefore decided to halt screening at the phase 1 level, selecting only relevant systematic reviews and guidelines with a focus on COVID‐19 for inclusion.
| 1 | 2 | 3 |
| Search for and select (1) guidelines, (2) systematic reviews, and (3) single studies on COVID‐19 Search sources to include sources 1‐4 (above) concurrently Include any guideline or systematic reviews that
|
Map against questions by extracting brief data on:
|
Identify key gaps |
| 4 | 5 | 6 |
| Search for guidelines and systematic reviews (no single studies) related to other infectious diseases (including SARS, MERS, influenza, Ebola, TB and potentially, hypothetical pandemic diseases) Search sources to include sources 1‐4 (above) concurrently Include any guideline or systematic reviews that:
|
Map against questions by extracting data on:
|
Identify key gaps |
| 7 | 8 | 9 |
| Contact experts to check data sources and for advice on gaps | Review search yield of single primary research studies (COVID‐specific) and select those which fill gaps in the guideline or review evidence | Consider any further searches identified from expert consultation to fill outstanding gaps by searching for single studies |
Appendix 3. Cochrane Library search strategy
#1 COVID‐19
#2 MeSH descriptor: [COVID‐19] explode all trees
#3 MeSH descriptor: [SARS‐CoV‐2] explode all trees
#4 MeSH descriptor: [Coronavirus] explode all trees
#5 MeSH descriptor: [Coronavirus Infections] explode all trees
#6 (covid or coronavir* or coronovir*)
#7 ((corona* or corono*) NEAR (virus* or viral* or virinae*))
#8 (ncov or n‐cov or 2019nCoV or nCoV2019 or CO?VID‐19 or CO?VID19 or WN‐CoV or WNCoV or HCoV‐19 or HCoV19 or 2019nov‐el* or SARS‐CoV‐2 or SARSCoV‐2 or SARSCoV2 or SARS‐CoV2 or SARSCov19 or SARS‐Cov19 or SARSCov‐19 or SARS‐Cov‐19 or Ncovor or Ncorona* or Ncorono* or NcovWuhan* or Ncov‐Hubei* or NcovChina* or NcovChinese* or SARS2 or SARS‐2 or SARScoron?virus2 or SARS‐coron?virus‐2 or SARScoron?virus2 or SARScoron?virus2)
#9 {OR #1‐#8}
#10 Leadership OR "Health Knowledge, Attitudes, Practice"
#11 Health Promotion
#12 "Treatment Adherence and Compliance"
#13 MeSH descriptor: [Reminder Systems] this term only
#14 MeSH descriptor: [Health Education] explode all trees
#15 MeSH descriptor: [Consumer Health Information] this term only
#16 MeSH descriptor: [Patient Education as Topic] this term only
#17 MeSH descriptor: [Information Literacy] this term only
#18 MeSH descriptor: [Communication] explode all trees
#19 MeSH descriptor: [Decision Making] this term only
#20 MeSH descriptor: [Competitive Behavior] this term only
#21 MeSH descriptor: [Cooperative Behavior] this term only
#22 MeSH descriptor: [Mass Behavior] this term only
#23 MeSH descriptor: [Social Skills] this term only
#24 MeSH descriptor: [Social Support] this term only
#25 MeSH descriptor: [Pamphlets] this term only
#26 MeSH descriptor: [Communications Media] this term only
#27 ((health OR medical OR clinical OR advice OR patient*) NEAR/3 (educat* OR inform*)):ti,ab,kw.
((patient* OR communit* OR population OR mass) NEAR/3 (literatur* OR material* OR information* OR guide OR guides OR instruction*)):ti,ab,kw.
#28 ((print* OR written OR text* OR social) NEAR/3 (material* OR information* OR guide OR guides OR instruction* OR advice OR advis* OR messag* OR note OR notes OR media)):ti,ab,kw.
#29 ((handout* OR guidebook* OR information) NEAR/3 (card OR cards OR postcard*)):ti,ab,kw.
#30 (information NEAR/2 (pack* OR sheet*)):ti,ab,kw.
#31 (mhealth OR M*health):ti,ab,kw.
#32 (communit* NEAR/3 leader*):ti,ab,kw.
#33 (self‐monitor* OR "self monitor*"):ti,ab,kw.
#34 {OR #13‐#33}
#35 MeSH descriptor: [Coronaviridae] 1 tree(s) exploded
#36 MeSH descriptor: [Coronavirus Infections] this term only
#37 MeSH descriptor: [Hemorrhagic Fever, Ebola] this term only
#38 MeSH descriptor: [Tuberculosis] this term only
#39 MeSH descriptor: [Disease Outbreaks] explode all trees
#40 MeSH descriptor: [Epidemics] explode all trees
#41 MeSH descriptor: [Pandemics] explode all trees
#42 MeSH descriptor: [Influenza, Human] explode all trees
#43 (nCoV OR nCoV OR ((new OR novel OR wuhan) NEAR/3 coronavirus) OR covid19 OR covid‐19 OR SARS‐CoV‐2 OR "Severe Acute Respiratory Syndrome Coronavirus 2"):ti,ab,kw
#44 (coronavirus* OR coronovirus* OR coronoravirus* OR coronaravirus* OR corono‐virus* OR corona‐virus*):ti
#45 (pneumonia OR respiratory‐illness* OR respiratory‐symptom* OR "respiratory disease*"):ti
(ebola OR tuberculosis OR pneumonia OR SARS OR MERS):ti
#46 {OR #35‐#45}
#47 MeSH descriptor: [Contact Tracing] explode all trees
#48 ((trace OR identif*) NEAR/2 contact*):ti,ab,kw.
#49 ((case* OR early OR mobile OR tracing OR contact) NEAR/2 (detect OR detecting OR detection OR find* OR app OR apps)):ti,ab,kw.
#50 {OR #47‐#49}
#51 MeSH descriptor: [Patient Isolation] explode all trees
#52 MeSH descriptor: [Social Isolation] explode all trees
#53 (self‐isolat*):ti,ab,kw.
#54 ((patient* or case* or voluntary or home or social or self) NEAR2 (isolat* OR confine* OR confinement* OR isolation)):ti,ab,kw.
#55 {OR #51‐#54}
#56 MeSH descriptor: [Quarantine] explode all trees
#57 (quarantin*):ti,ab,kw.
#58 {OR #56‐#57}
#59 (school* NEAR/2 (closure* OR closing OR holiday*)):ti,ab,kw.
#60 (college* NEAR/2 (closure* OR closing OR holiday*)):ti,ab,kw.
#61 ((class or classes) NEAR/2 dismiss*):ti,ab,kw.
#62 {OR #59‐#61}
#63 MeSH descriptor: [Work] explode all trees
#64 MeSH descriptor: [Workplace] explode all trees
#65 (work site* OR workplace* OR business* OR organisaton* OR job site* OR organization* OR office*):ti,ab,kw.
#66 {OR #63‐#65}
#67 (shutdown* OR closure* OR close* OR closing OR cease OR cessation* OR leave):ti,ab,kw.
#68 #66 AND #67
#69 MeSH descriptor: [Teleworking] explode all trees
#70 #68 OR #69
#71 Social Behavior
#72 ((social OR community) NEAR/2 (mixing OR distanc* OR mitigat*)):ti,ab,kw.
#73 (gather* OR crowd* OR event* OR meeting* OR sport* OR concert* OR pilgrimage* OR park OR parks OR conference* OR mosque* OR temple* OR party OR parties OR wedding* OR funeral* OR mass OR community OR communities OR church*):ti,ab, kw.
#74 {OR #71‐#73}
#75 (distanc* OR space OR spacing OR avoid* OR remote OR retreat):ti,ab, kw.
#76 #74 AND #75
#77 MeSH descriptor: [Physical Distancing] explode all trees
#78 (lockdown* OR lock down* OR confine*):ti,ab, kw.
#79 ((stay OR remain) NEAR/2 home):ti,ab, kw.
#80 ((physical OR social*) NEAR/2 distanc*):ti,ab, kw.
#81 non pharmaceutical intervention*:ti,ab, kw.
#82 non?pharmaceutical intervention*:ti,ab, kw.
#83 NPI*:ti,ab, kw.
#84 (public health NEAR/2 (measure* OR restriction* OR order*)):ti,ab, kw.
#85 {OR #77‐#84}
#86 #50 OR #55 OR #58 OR #62 OR #70 OR #76 OR #85
#87 #34 AND #46
#88 #87 AND #50
#89 #87 AND #55
#90 #87 AND #58
#91 #87 AND #62
#92 #87 AND #70
#93 #87 AND #76
#94 #87 AND #85
#95 #87 AND #86
Appendix 4. Embase search strategy
1. meta‐analysis:.mp. or search:.tw. or review.pt.
2. exp clinical pathway/
3. exp clinical protocol/
4. exp consensus/
5. exp consensus development conference/
6. exp consensus development conferences as topic/
7. critical pathways/
8. guidelines as topic/
9. exp practice guideline/
10. practice guidelines as topic/
11. health planning guidelines/
12. (position statement* or policy statement* or practice parameter* or best practice*).ti,ab,kw.
13. (standards or guideline or guidelines).ti,kw.
14. ((practice or treatment* or clinical) adj guideline*).ab.
15. (guideline or practice guideline or consensus development conference or consensus development conference, NIH).pt.
16. consensus*.ti,kw.
17. consensus*.ab.
18. ((critical or clinical or practice) adj2 (path or paths or pathway or pathways or protocol*)).ti,ab,kw.
19. recommendat*.ti,kw.
20. (care adj2 (standard or path or paths or pathway or pathways or map or maps or plan or plans)).ti,ab,kw.
21. (algorithm* adj2 (test or tested or testing or assessment* or diagnosis or diagnoses or diagnosed or diagnosing)).ti,ab,kw.
22. (algorithm* adj2 (therap* or treatment* or intervention*)).ti,ab,kw.
23. (CPG or CPGs).ti.
24. or/2‐23
25. 1 or 24
26. attitude to health/
27. health education/
28. consumer health information/
29. reminder system/
30. patient education/
31. information literacy/
32. exp interpersonal communication/
33. exp decision making/
34. competitive behavior/
35. cooperation/
36. mass behavior/
37. social competence/
38. social support/
39. exp mass communication/
40. patient compliance/
41. exp health promotion/
42. leadership/
43. pamphlet*.tw.
44. ((health or medical or clinical or advice or patient*) adj3 (remind* or educat* or inform* or belie*)).tw,kw.
45. ((patient* or communit* or population or mass) adj3 (literatur* or material* or information* or guide or guides or instruction*)).tw,kw.
46. ((print* or written or text* or social) adj3 (material* or information* or guide or guides or instruction* or advice or advis* or messag* or note or notes or media)).tw,kw.
47. ((handout* or guidebook* or information) adj3 (card or cards or postcard*)).tw,kw.
48. (information adj2 (pack* or sheet*)).tw,kw.
49. (mhealth or M#health).tw,kw.
50. (communit* adj3 leader*).tw,kw.
51. (self‐monitor* or "self monitor*" or "self protect*" or self‐protect*).tw,kw.
52. or/26‐51
53. exp severe acute respiratory syndrome coronavirus 2/ or coronavirus disease 2019/ or experimental coronavirus disease 2019/
54. (corona* adj1 (virus* or viral*)).ti,ab,kw.
55. (CoV not (Coefficien* or co‐efficien* or covalent* or covington or covariant* or covarianc* or "cut‐off value*" or "cutoff value*" or "cut‐off volume*" or "cutoff volume*" or "combined optimi?ation value*" or "central vessel trunk" or CoVR or CoVS)).ti,ab,kw.
56. (coronavirus* or 2019nCoV* or 19nCoV* or "2019 novel*" or Ncov* or "n‐cov" or "SARSCoV‐2*" or "SARSCoV‐2*" or SARSCoV2* or "SARS‐CoV2*" or "severe acute respiratory syndrome*" or COVID*2).ti,ab,kw.
57. or/53‐56
58. contact examination/
59. ((trace or identif*) adj2 contact*).tw,kw.
60. ((case* or early) adj2 (detect or detecting or detection or find*)).tw,kw.
61. ((mobile or tracing or contact) adj2 (app or apps)).tw,kw.
62. or/58‐61
63. patient isolation/
64. social isolation/
65. (self‐isolat* or solitary or solitude).tw,kw.
66. ((patient* or case* or voluntar* or home or social or self) adj2 (isolat* or confine or confinement)).tw,kw.
67. or/63‐66
68. exp quarantine/
69. quarantin*.kw,tw.
70. or/68‐69
71. (school* adj2 (closure* or closing or holiday*)).tw,kw.
72. (college* adj2 (closure* or closing or holiday*)).tw,kw.
73. (class* adj2 dismiss*).kw,tw.
74. or/71‐73
75. exp work/
76. (work site* or workplace* or business* or organisaton* or job site* or organization* or office*).tw,kw.
77. or/75‐76
78. (shutdown* or closure* or close* or closing or cease or cessation* or leave).tw,kw.
79. and/77‐78
80. 79 or telework.kw,tw.
81. "social behavior"/
82. "social distance"/
83. (social* adj2 (mixing or distanc*)).kw,tw.
84. (community adj2 mitigat*).tw,kw.
85. (gather* or crowd* or event* or meeting* or sport* or concert* or pilgrimage* or park or parks or conference* or mosque* or temple* or party or parties or wedding* or funeral* or mass or community or communities or church*).tw.
86. or/81‐85
87. (distanc* or space or spacing or avoid* or remote or retreat).tw.
88. and/86‐87
89. social distancing/
90. ("stay at home" or lockdown* or "lock down*" or confine*).tw,kw.
91. ((stay or remain) adj2 home).tw,kw.
92. ((physical or social) adj2 distanc*).tw,kw.
93. non?pharmaceutical.tw,kw.
94. non pharmaceutical intervention*.tw,kw.
95. npi.tw,kw.
96. (public health adj2 (measure* or restriction* or order*)).kw,tw.
97. or/89‐96
98. or/62,67,70,74,80,88,97
99. 52 and 57 and 98
100. 25 and 99
101. 1 and 99
102. 24 and 99
103. 101 or 102
104. Ebola hemorrhagic fever/
105. exp tuberculosis/
106. epidemic/
107. pandemic/
108. influenza/ or experimental influenza/ or influenza a/ or influenza b/ or influenza c/ or pandemic influenza/ or seasonal influenza/ or swine influenza/
109. (ebola or tuberculosis or pneumonia or SARS or MERS).ti,ab,kw.
110. severe acute respiratory syndrome/
111. Middle East respiratory syndrome/
112. or/57,104‐111
113. 25 and 52 and 112
114. 1 and 52 and 112
115. 24 and 52 and 112
116. 114 and 62
117. 114 and 67
118. 114 and 70
119. 114 and 74
120. 114 and 80
121. 114 and 88
122. 114 and 97
123. 115 and 62
124. 115 and 67
125. 115 and 70
126. 115 and 74
127. 115 and 80
128. 115 and 88
129. 115 and 97
Appendix 5. MEDLINE search strategy
1. "Health Knowledge, Attitudes, Practice"/
2. health education/
3. consumer health information/
4. Reminder Systems/
5. patient education as topic/
6. exp information literacy/
7. exp Communication/
8. exp Decision Making/
9. competitive behavior/
10. cooperative behavior/
11. mass behavior/
12. social skills/
13. exp social support/
14. Pamphlets/
15. Communications Media/
16. "Treatment Adherence and Compliance"/
17. Health Promotion/
18. Leadership/
19. ((health or medical or clinical or advice or patient*) adj3 (remind* or educat* or inform* or belie*)).ti,ab,kw.
20. ((patient* or communit* or population or mass) adj3 (literatur* or material* or information* or guide or guides or instruction*)).ti,ab,kw.
21. ((print* or written or text* or social) adj3 (material* or information* or guide or guides or instruction* or advice or advis* or messag* or note or notes or media)).ti,ab,kw.
22. ((handout* or guidebook* or information) adj3 (card or cards or postcard*)).ti,ab,kw.
23. (information adj2 (pack* or sheet*)).ti,ab,kw.
24. (mhealth or M#health).ti,ab,kw.
25. (communit* adj3 leader*).ti,ab,kw.
26. (self‐monitor* or self monitor* or self protect* or self‐protect*).ti,ab,kw.
27. or/1‐26
28. exp Coronaviridae/
29. Coronavirus Infections/
30. Hemorrhagic Fever, Ebola/
31. Tuberculosis/
32. Disease Outbreaks/
33. epidemics/ or pandemics/
34. Influenza, Human/
35. (nCoV or 2019‐nCoV or ((new or novel or wuhan) adj3 coronavirus) or covid19 or covid‐19 or SARS‐CoV‐2 or "Severe Acute Respiratory Syndrome Coronavirus 2").mp.
36. (coronavirus* or coronovirus* or coronoravirus* or coronaravirus* or corono‐virus* or corona‐virus*).ti,ab,kf.
37. (pneumonia or respiratory‐illness* or respiratory‐symptom* or respiratory disease*).ti,ab,kf.
38. (ebola or tuberculosis or pneumonia or SARS or MERS).ti,ab,kf.
39. or/28‐38
40. COVID‐19/
41. SARS‐CoV‐2/
42. exp Coronavirus/
43. exp Coronavirus Infections/
44. (covid or coronavir* or coronovir*).mp.
45. ((corona* or corono*) adj1 (virus* or viral* or virinae*)).ti,ab,kf.
46. (ncov or n‐cov or 2019nCoV or nCoV2019 or CO?VID‐19 or CO?VID19 or WN‐CoV or WNCoV or HCoV‐19 or HCoV19 or 2019nov‐el* or SARS‐CoV‐2 or SARSCoV‐2 or SARSCoV2 or SARS‐CoV2 or SARSCov19 or SARS‐Cov19 or SARSCov‐19 or SARS‐Cov‐19 or Ncovor or Ncorona* or Ncorono* or NcovWuhan* or Ncov‐Hubei* or NcovChina* or NcovChinese* or SARS2 or SARS‐2 or SARScoron?virus2 or SARS‐coron?virus‐2 or SARScoron?virus2 or SARScoron?virus2).ti,ab,kf.
47. or/40‐46
48. 27 and 47
49. Contact Tracing/
50. ((trace or identif*) adj2 contact*).ti,ab,kw.
51. ((case* or early) adj2 (detect or detecting or detection or find*)).ti,ab,kw.
52. ((mobile or tracing or contact) adj2 (app or apps)).ti,ab,kw.
53. or/49‐52
54. Patient Isolation/
55. Social Isolation/
56. (self‐isolat* or solitary or solitude).ti,ab,kw.
57. ((patient* or case* or voluntar* or home or social* or self) adj2 (isolat* or confine* or confinement*)).ti,ab,kw.
58. or/54‐57
59. Quarantine/
60. quarantin*.ti,ab,kw.
61. or/59‐60
62. (school* adj2 (closure* or closing or holiday*)).ti,ab,kw.
63. (college* adj2 (closure* or closing or holiday*)).ti,ab,kw.
64. ((class or classes) adj2 dismiss*).ti,ab,kw.
65. or/62‐64
66. exp Work/
67. Workplace/
68. (work site* or workplace* or business* or organisaton* or job site* or organization* or office*).ti,ab,kw.
69. or/66‐68
70. (shutdown* or closure* or close* or closing or cease or cessation* or leave).ti,ab,kw.
71. and/69‐70
72. 71 or telework.ti,ab,kw.
73. social behavior/
74. (social* adj2 (mixing or distanc*)).ti,ab,kw.
75. (community adj2 mitigat*).ti,ab,kw.
76. (gather* or crowd* or event* or meeting* or sport* or concert* or pilgrimage* or park or parks or conference* or mosque* or temple* or party or parties or wedding* or funeral* or mass or community or communities or church*).ti,ab,kw.
77. or/73‐76
78. (distanc* or space or spacing or avoid* or remote or retreat).ti,ab,kw.
79. and/77‐78
80. Physical Distancing/
81. (lockdown* or lock down* or confine*).ti,ab,kw.
82. ((stay or remain) adj2 home).ti,ab,kw.
83. ((physical or social*) adj2 distanc*).ti,ab,kw.
84. non pharmaceutical intervention*.ti,ab,kw.
85. non?pharmaceutical intervention*.ti,ab,kw.
86. NPI*.ti,ab,kw.
87. (public health adj2 (measure* or restriction* or order*)).ti,ab,kw.
88. or/80‐87
89. or/53,58,61,65,72,79,88
90. and/48,89
91. 48 and 53
92. 48 and 58
93. 48 and 61
94. 48 and 65
95. 48 and 72
96. 48 and 79
97. 48 and 88
Appendix 6. Data tables: characteristics, quality assessment, findings and mapping and translational steps
Data extracted from each of the included studies are presented in the data tables that follow.
Tables are organised by physical distancing measure (focus), presenting evidence first from synthesised sources (guidelines and SRs), followed by primary studies.
Table a contact tracing
Table b isolation
Table c quarantine
Table d school measures
Table e work measures
Table f crowd avoidance
Table g general physical distancing
Within these physical distancing categories, each data table for each study reports:
Characteristics of that study;
Results of quality assessment;
Outcomes and findings;
Translational and mapping steps.
*Please note that the 'mapping to themes...' field of studies added in this update (column 1) refers to initial mapping steps undertaken against the thematic framework derived from the original review. This was an intermediate organisational step undertaken as part of the synthesis of findings; leading to the identification of six final themes that emerged from the inclusion of newly‐added data in this update.
Table a: Contact tracing
| Public Health Measure 1: Contact tracing | Study features | Outcomes and findings | Translational steps |
| Systematic reviews, guidelines | |||
|
Chung 2021# Citation type: SR Public health measure: Contact tracing, and also, maps onto isolation and quarantine Mapping to: Uptake, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 3: support for individual and population behavioural changes Theme 5: public trust and perceptions |
Overview and aim: To examine experiences and approaches of countries implementing find, test, trace, isolate, support (FTTIS) strategies early in the COVID‐19 pandemic Type of study and data: SR; primarily qualitative; N = 118 included (e.g. rapid report/reviews, case study/series, evaluation/simulation studies, narrative reviews) Inclusion and exclusion criteria: Included: English language; published research studies/reviews of contact tracing, testing, isolation or quarantine Participant features and numbers, sampling details: Approaches of interest applied to general population; no specific selection criteria related to participants were stated or reported against. Included disease(s): COVID‐19 Timing: Searches run May 2019 to January 2021. No further consideration of timing, although authors noted that review focused on FTTIS measures early in the pandemic Countries included: Various, not systematically described (included South Korea, Japan, Taiwan, UK, USA, Portugal, Brazil, Bangladesh, India). Studies likely across all income brackets (low to high income) but not specifically identified. Intervention or phenomenon of interest: Communication to support contact tracing, adherence to isolation and subsequent public health actions Quality assessment: AMSTAR 4/11 [1. Not clear whether protocol was established a priori; 2. Unclear re duplicate screening/data extraction; 4. Seems published papers only, in English, included; 5. No excluded studies provided; 8. No integration of quality assessments; 10 no publication bias assessment; 11. No COI for included studies]. Funding source: DP is funded through the EPSRC I sense consortium, and other authors receive no funding for the study. |
Data on testing and contact tracing approaches and infrastructure, test performance or digital contact tracing applications not extracted and reported as unrelated to communication Self‐isolation/quarantine: Features of support for those undertaking self‐isolation (note Webster 2020, Brooks 2020 papers already included in original review cited here, together with additional papers) Factors associated with adherence included knowledge of the disease and process for quarantine, social norms, perceived benefits of quarantine and risk of disease, and access to essential supplies and/or financial support. For informal or low‐income earners, self‐isolation or quarantine may be unaffordable, and people may require financial support to undertake the measures. Isolation or quarantine may have adverse psychological consequences (e.g. anxiety, confusion, anger and PTSD symptoms) and may be related to factors such as fear of infection and inadequate supplies. Increased rates of domestic violence have also been reported. Providing sufficient timely information to people undertaking isolation/quarantine may improve uncertainty, quarantining people for the minimum safe period, and ensuring provision of adequate supplies may mitigate these negative effects. Psychological screening may also help to identify those most in need of support (e.g. counselling, coaching, social prescribing such as exercise or art classes, online communication (e.g. via social media) may help reduce loneliness during & increase coping during isolation. Testing: Communicating information about how to get a test, and under what conditions, has been challenging. This is especially true for some minority ethnic groups. Public awareness and communication: Public perceptions of the reliability of testing services, and effectiveness of communication about actions that can be taken to help contain COVID‐19 both influence uptake. Testing kits and stations also need to be accessible to disadvantaged groups and, if such groups (e.g. ethnic minorities) are at heightened risk, then communication must be tailored to encourage engagement with testing. Communication by authorities to ensure the public are well‐informed and kept up to date about the pandemic as the situation changes is important for increasing awareness of the need for FTTIS and correcting misinformation or rumours that may arise where there is uncertainty or gaps in public knowledge. Regular press conferences by authorities (including progress briefings, policy changes & correcting misinformation) may have a role in such communication to provide clear information about disease risk severity. Social media and the Internet may also influence behaviour when people are in isolation. For instance, social media may increase intention to adhere to public health measures, whereas conspiracy beliefs can be inversely associated with adherence to self‐isolation guidelines. Lowering perceived response costs and clear information about the severity of risks may help motivate the public to self‐isolate. Reliable official sources (e.g. government information, official news and journalism) may be best placed to communicate information about severity of disease risk, while social media may best focus on messaging related to recommended health measures and messages of hope. Public co‐operation: Low public trust of government may prevent public cooperation with FTTI guidelines. Conversely, perceived benefits, self‐efficacy and trust are positively associated with uptake of contact tracing apps. To support uptake of contact tracing apps, personal information must be protected. This can help to promote trust, prioritise care and encourage individuals to cooperate with guidelines to prevent transmission of disease. Recommendations: Implementing an effective FTTIS system includes the need for support measures to promote testing and behaviours such as isolation or quarantine associated with testing. Support can include timely, adequate information to reduce anxiety and uncertainty, or practical supports in the form of provision of adequate supplies or financial assistance. Such measures also serve to build public trust, which is key to controlling COVID‐19 in any population as this relies on people voluntarily providing their information and following public health measures. Public communication by authorities is also critical to provide ongoing information about the pandemic and/or policies over time. An essential part of this is ensuring open and balanced discussions take place about concerns such as data privacy/protection, and limits on personal freedom for the greater societal good. |
Communication purpose: Findings may inform communication strategies for increasing public awareness of the need for FTTIS, such as providing tailored, up‐to‐date information, practical and financial supports, and working to build trust amongst community members and the public more broadly. Related to review questions: Clear, reliable information, including that about disease risk severity and societal benefits of measures, may help to dispel distrust of government/authorities and promote uptake of testing and isolation behaviours required to control disease transmission. Communication of such information needs to be flexible and up‐to‐date as circumstances or required public health measures change over time, and might also aim to address misinformation or areas of uncertainty in order to further build public trust. Provision of tailored support, including practical and financial supports, for those at socioeconomic or other disadvantage may help people to adopt and adhere to measures. |
|
Gilmore 2020#^ Citation type: SR (rapid) Public health measure: Contact tracing, and also maps onto isolation, quarantine, and general PD Mapping to: Uptake, acceptability Mapping to: Theme 2: recipients of public communication: audience, setting and equity Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: To review evidence on community engagement for prevention and control of infectious diseases during epidemics Type of study and data: Rapid SR; 32 included empirical studies (any design) (describing 37 initiatives) plus 11 general guidance documents Inclusion and exclusion criteria: Included: community‐level engagement (range of collaborative processes with community actors). All languages Excluded: Interventions focused on community health workers without wider community engagement. Participant features and numbers, sampling details: Most activities were aimed at entire communities. Authors note a small number of studies targeted marginalised groups (e.g. non‐English‐speaking groups); including all 4 studies of H1N1 outbreaks in which equity was considered in relation to remote/aboriginal populations (but engagement was limited to design and planning activities only in these cases). Composition of community engagement groups often not reported, but some explicitly included marginalised groups (e.g. women representative, EVD survivors, youth). Included disease(s): Previous epidemics: EVD (28 studies), SARS (0), MERS (0), H1N1 (4), Zika (5) Timing: Searches May 2020; literature limited to those published from 2000 onwards Countries included: 28/37 for EVD (25 West African outbreak 2014‐15: Sierra Leone (11), Liberia (9) Guinea (2), Nigeria (1), Ghana (1), mixed country (1); 3 Democratic Republic of Congo 2018‐20 outbreak: Uganda (2)) 5/37 Zika (USA and Puerto Rico (3), Singapore (1), Uruguay (1)); 4/37 H1N1 (Australia (3), Canada (1)). Range of income brackets but most studies undertaken in low‐income countries Intervention or phenomenon of interest: Community engagement strategies Quality assessment: 5/11 AMSTAR [5. No excluded studies reported, unclear 7,8; Quality not assessed or used 9; Synthesis methods not clear and/or appropriate 10; Publication bias not formally assessed 11; COIs of included studies not reported] Funding source: Provenance: Not commissioned |
Identified six broad community engagement approaches aiming to address infection prevention and control through six major channels Major actors or approaches included the following: community leaders (traditional, religious and/or governing); community and faith‐based organisations; community groups; health management committees; individuals; and key stakeholders (students, survivors, women, elderly, youth). Community engagement interventions operated via six main channels:
Community engagement was mostly used for social and behavioural change communication, and risk communication, followed by surveillance and contact tracing; many approaches were multi‐faceted & involved multiple actors. Key enablers and barriers for community engagement were identified from included research. Facilitators:
Barriers:
Recommendations: Best‐practice recommendations were developed based on identified enablers and barriers:
|
Communication purpose: These findings can usefully inform development of community engagement strategies to support prevention and control measures during pandemic outbreaks. Community engagement can occur via different approaches and channels, and several features such as early and ongoing engagement are critical to success. Related to review questions: Community engagement approaches may involve a range of approaches, and channels, operating in various combinations to achieve different purposes, such as planning and design of interventions, trust‐building, and communication (including messaging) about risk and/or social and behavioural changes. To be most effective, community engagement incorporating two‐way dialogue should begin early and be ongoing in order to build trust within the community and to better understand the sociocultural context in which disease prevention and control efforts are needed. Community engagement can inform choice, development and/or appropriateness of measures required within specific groups; co‐design of messaging (information, education, communication) can help to ensure appropriateness and reach of messages to support public health measures. Messaging built on clear, accurate, consistent information, tailored to local context, can help to build trust, clarify misconceptions, and to directly address rumours and misinformation. Meaningful engagement should include mechanisms for regular feedback from the community in order to monitor knowledge, beliefs and practices/behaviours and their changes over time, and to adapt course as required. |
|
Heuvelings 2018* Citation type: SR Maps to: Acceptability |
Overview and aim: Evaluation of effectiveness (including cost‐effectiveness) of service models and organisational structures for TB identification and management Participant features and numbers, sampling details:Included: hard‐to‐reach populations (homeless people, drug users, migrants); countries with low‐to‐moderate TB incidence Intervention or phenomenon of interest: Included interventions: Effects of healthcare worker type or setting type on TB identification and/or management Type of study and data: SR; 11 included studies NICE and Cochrane methods followed; updates NICE review (previously included 6 studies) RCTs, non‐RCTs included Countries included:OECD, EU/EEA countries (UK, Portugal, Spain, Germany) Quality assessment: 7/10 AMSTAR rating% Funding source: Funders who supported this work: European Centre for Disease Prevention and Control; National Institute for Health Research (NIHR) (1): Grant ID: NF‐SI‐0616‐10016 |
Recommendations:
|
Communication purpose: This may inform decisions about who might most effectively conduct contact tracing in hard‐to‐reach populations such as the homeless and migrants. Related to review questions: Findings may provide insight into improving acceptability of contact tracing. |
|
Khorram‐Manesh 2021# Citation type: SR Public health measure: Contact tracing, and also maps onto General PD Mapping to: Uptake, acceptability, adherence Mapping to: Theme 2: recipients of public communication: audience, setting and equity Theme 5: public trust and perceptions |
Overview and aim: To systematically review the literature to identify educational strategies to promote public health measure implementation, particularly contact tracing, prior to public health emergencies Type of study and data: SR; quantitative and qualitative, N = 52 studies Inclusion and exclusion criteria: Included: research, English language Excluded: conference papers, abstracts, reports, and non‐scientific publications Participant features and numbers, sampling details: General public/communities No particular demographic features reported Included disease(s): COVID‐19, H1N1 Timing: Search dates unclear; the majority of papers from 2020, 2021 Countries included: US and Canada (16 studies), Asia‐Pacific (13). European Union (9), UK (7), Middle East (3), Africa (3). Range of income levels, 38/52 high income; remainder of countries middle income (lower‐to‐upper middle) Intervention or phenomenon of interest: Educational strategies to support public health measure implementation Quality assessment: AMSTAR 5/11: [1. No protocol/plan 5. No list of excluded studies 6. Included study characteristics inadequate 8. Quality not integrated explicitly into findings 10. No publication bias assessment 11. No COIs for included studies] Funding source: This research received no external funding. |
Four main themes were identified. Practical aspects
Ethical aspects
Psychological aspects
Community‐level education
Recommendations: Contact tracing efficiency depends inherently on the public’s willingness to engage with authorities and the process. In turn, this depends on the public’s trust of the government in terms of measures imposed to protect health and to protect privacy. Increased availability of technology presents the option of using these as a basis for protection of public health (digital health protection measures) and enable social networking but also have ethical and psychological impacts that need to be factored into decision‐making. In the current pandemic, where treatments and vaccines were lacking, physical distancing measures were the key available public health strategies. These also carry societal and ethical impacts that may influence levels of adherence, and this may vary across countries and populations. Lack of adherence to physical distancing measures may be due to disagreement with the social restrictions, but in other cases the cause is more fundamental and reflect the needs of people under public health surveillance e.g. reflecting issues associated with housing and living arrangements, transport, education, food and essential household supplies. Addressing these needs may help to increase people’s willingness to adhere to physical distancing measures such as quarantine. The current COVID‐19 pandemic and deployment of digital public health technologies have led to efforts to produce guidelines and policies with an emphasis on personal data safety and privacy, and so ensure widespread public trust and uptake. As well as providing information and ensuring quality, to minimise misconceptions, efforts to better understand factors affecting app usability are key, including in relation to contact tracing apps. Public education at all levels but particularly community level, is also needed to support these apps, by increasing perceived usefulness and ease of use. Education needs to be tailored and targeted within the population, including towards people with lower health literacy, who may otherwise be unable to effectively engage with apps and associated public health measures. |
Communication purpose: Findings may inform strategies to support implementation of public health measures such as contact tracing, including public education and various forms of support for physical distancing measures. Related to review questions: Simple, safe technology may increase people’s willingness and ability to participate in contact tracing, but adequate information must be provided about apps used for public health protection, and specific concerns such as those about data protection and privacy, and stigma must be addressed to promote uptake and adherence. Education to increase community knowledge and awareness of the disease and preventive measures is also needed. Tailored information specific to communities may assist with uptake and adherence, and such information needs to include targeting to those in the community of lower general or health‐specific literacy levels. Use of digital technologies for public health measures must consider that people may have differential access to devices that can support apps (e.g. older devices may not run, older people may not have access to technology), and that this may further marginalise vulnerable groups within the community, such as those who are older or poorer. Information and education for the public needs to consider not only information provision related to public health measures but the emotional, psychological and practical impacts of the measures. |
|
Megnin‐Viggars 2020# Citation type: SR, rapid Public health measure: Contact tracing Mapping to: Uptake, acceptability Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: To identify barriers and facilitators to community uptake of, and engagement with, contact tracing during an infectious disease outbreak Type of study and data: Rapid SR; qualitative and quantitative research; 12 included studies (6 qualitative interview and focus group studies, 5 quantitative surveys, 1 mixed methods (qualitative interview plus quantitative survey)) Inclusion and exclusion criteria: Included: Primary qualitative or quantitative research; English language; assessed factors related to contact tracing Excluded: experience of non‐viral and contagious major health incident, sexually transmitted diseases Participant features and numbers, sampling details: People with experience of a major viral and contagious health incident; included general population, contact tracers and their supervisors, public health professionals, CDC staff Included disease(s): COVID‐19 (6 studies), EBV (5), hypothetical (1) Timing: Searches from inception to July 2020 inclusive Timing of population and communication not otherwise considered explicitly Countries included: Single country studies: UK (3), Sierra Leone (3), Netherlands (2), Australia (1), & Liberia (1) Multiple country studies: Sierra Leone, Guinea, Liberia, Mali, Senegal, Nigeria; France, Germany, Italy, UK, US West African countries low income except Senegal (lower middle income); others all high income Intervention or phenomenon of interest: Community engagement with contact tracing, and factors affecting (positive and negative) Quality assessment: 8/11 AMSTAR [8. Quality assessed but not linked to findings explicitly; 10. Publication bias not assessed; 11. COI included studies not reported]. Funding source: PC and OMV were funded by Go‐Science; the review was conducted at the request of the Scientific Pandemic Influenza Group on Behaviours (SPI‐B), a behavioural science advisory group for the Scientific Advisory Group for Emergencies (SAGE): Coronavirus (COVID‐19) response team, who provide scientific and technical advice to support UK government decision‐makers. GJR and DW were funded by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Emergency Preparedness and Response, a partnership between Public Health England, King’s College London and the University of East Anglia. DW is also supported by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Behaviour Change and Evaluation, a partnership between Public Health England and the University of Bristol. |
Reported on: Barriers and enablers of uptake of and engagement with contact tracing (CT) were identified. Enablers: Four themes were identified. Collective responsibility
Personal benefit
Co‐production of CT systems
Perception of system (as efficient, rigorous, reliable)
Barriers: 5 themes identified. Privacy
Mistrust and/or apprehension
Unmet information and support needs
Fear of stigmatisation
Mode‐specific challenges
Recommendations: Engagement with CT systems might be enhanced through:
|
Communication purpose: May inform development and implementation of contact tracing systems, as well as development of messages for communicating with the community to promote engagement with contact tracing systems. Factors may inform messaging and activities used to develop and support CT systems, as well as practical measures to overcome barriers to engagement. Related to review questions: Several factors, both enablers and barriers, influence individual and community engagement with contact tracing systems. This in turn, affects acceptance and uptake of systems. Communication intended to inform people about contact tracing measures need to take account of these factors and ensure that clear, consistent and actionable information is available. Both information and CT systems should be tailored appropriately to the local context. Messages might usefully promote both individual and collective benefits of contact tracing systems, while partnerships with communities may help to counter mistrust and concerns over privacy and stigma. |
|
Saurabh 2017* (SR) Mapping to: Acceptability |
Overview and aim: Assessment of the role of contact tracing in the 2014 Ebola epidemic and to identify factors influencing health workers’ ability to perform contact tracing Inclusion and exclusion criteria: Included: populations or communities exposed to EVD outbreak Type of study and data: SR; 60 included studies/reports. Primary studies (no details), technical reports, reviews, editorial documents Countries included: West Africa (Guinea, Sierra Leone, Liberia, Congo), also USA, Spain Quality assessment: 1/11 AMSTAR rating (critically low quality according to AMSTAR 2) Funding source: Not reported |
Reported on:
Recommendations:
|
Communication purpose: Findings may inform decisions about how and who to provide information to about disease outbreaks and subsequent contact tracing efforts. Related to review questions: Findings may provide insight into improving acceptability of contact tracing and factors influencing uptake (ability to perform) contact tracing in communities. |
|
Szkwarko 2017* (SR) Mapping to: Adherence |
Overview and aim: Tuberculosis Child Contact Management (CCM) implementation, challenges, predictors, and recommendations Inclusion and exclusion criteria: Included: Child population (< 15 years) exposed to TB in household in high‐burden countries. All quantitative, qualitative and mixed‐methods studies Excluded: randomised controlled trials, editorials, or commentaries Type of study and data: 37 studies included (25 quantitative, 3 qualitative, 9 mixed methods) Countries included: 22 studies in African region (most in South Africa (10), Ethiopia (4) and Malawi (3)), 14 in Southeast Asia (most in India (5), Indonesia (4)), and one in the Americas (Peru) Quality assessment: 6/11 AMSTAR rating Funding source: K01 AI104351/AI/NIAID NIH HHS/United States |
Reported on: Focus reported here is on contact identification and tracing (not screening, treatment). Child contact (< 5 years) identification varied widely (24 to 1227 child contacts). Challenges for contact management/tracing included the following:
Recommendations:
|
Communication purpose: This may be used for communication with parents to enhance compliance with contact tracing measures, by filling knowledge gaps, decreasing stigma, and increasing perceived importance of contact tracing. Findings may also help to inform decisions about how to decrease barriers to contact tracing measures, such as difficulties with access, or on stigma associated with TB. Related to review questions: Findings identify factors that may impact on non‐adherence to child contact tracing measures, such as knowledge gaps and competing demands. |
| Primary studies | |||
|
Bodas 2020# (primary) Mapping to: Adherence Also mapping to: Public health measures 3 (quarantine) and 2 (isolation) rather than contact tracing |
Overview and aim: Assessment of public attitudes to self‐quarantine for COVID‐19, including economic factors (compensation for lost wages) as a factor influencing compliance Inclusion and exclusion criteria: Included: adults (18 years and older) Type of study and data: Cross‐sectional survey; 563 participants (representative randomised sample of population of State of Israel) Countries included: Israel Quality assessment: Response rate: + representativeness: ++ COI not declared; results rely on self‐reported intentions (not behaviours), at a single time point; sample may under‐represent those without computer skills/Internet; paper peer reviewed and published |
Reported on: Public attitudes to COVID‐19 outbreak, including personal concern, attitudes towards public health regulations and compliance with public health regulations, including when compensation was provided or not.
Recommendations:
|
Communication purpose: This may inform communication with communities to prevent transmission through adherence to public health measures (short‐term (2 weeks) self‐quarantine), and for communicating with and supporting people undecided about behavioural compliance in the absence of financial compensation. Related to review questions: Findings identify factors influencing behavioural adherence to public health measures, particularly those related to monetary compensation and effects (that financial security is important for guaranteeing adherence to proposed measures). |
#COVID‐19‐specific study; *Non‐COVID‐19 specific study; % AMSTAR rating from McMaster Health Forum (via Health Systems Evidence https://www.healthsystemsevidence.org); European Centre for Disease Prevention and Control. Guidance on tuberculosis control in vulnerable and hard‐to‐reach populations. Stockholm: ECDC; 2016.
Abbreviations: CCM: child contact management CHW: community health worker COI: conflict of interest CT: contact tracing EEA: European Economic Area EU: European Union EVD: Ebola Virus Disease FTTIS: find, test, trace, isolate, support GPS: global positioning system H1N1: H1N1 influenza strain HIV: Human Immunodeficiency Virus MERS: Middle Eastern respiratory syndrome NICE: National Institute for Clinical Excellence NPI: non‐pharmaceutical interventions OECD: Organisation for Economic Co‐operation and Development PD: physical distancing PTSD: post‐traumatic stress disorder QR: quick response SAGE: Scientific Advisory Group for Emergencies SARS: Sudden acute respiratory syndrome SPI‐B: Scientific Pandemic Influenza Group on Behaviours SR: systematic review TB: tuberculosis
Table b: Isolation
| Public health measure 2: Isolation | Study features | Outcomes and findings | Translational steps |
| Systematic reviews, guidelines | |||
|
WHO 2021# Citation type: GL Actions for consideration in the care and protection of vulnerable populations from COVID‐19; interim guidance 13th October 2021; At: WPR-DSE-2020-021-eng.pdf (who.int) Public health measure: Isolation, and also maps onto quarantine, crowd avoidance, and general PD Mapping to: Uptake, acceptability, adherence, feasibility Mapping to: Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: To provide guidance on care and protection of vulnerable populations during COVID‐19 Type of study and data: GL; rapid literature search and guideline development process Method: GL was developed based on a review of relevant literature/guidance on vulnerable populations. Recommendations decided through group consensus Included disease(s): COVID‐19 Timing: Revised October 2021; no further information specific to timing Countries included: Across‐country; developed by WHO Regional Office for the Western Pacific Intervention or phenomenon of interest: To strengthen the care & protection of vulnerable groups from community transmission during COVID‐19 Population addressed in GL: vulnerable populations defined as those experiencing any condition resulting in inequitable access to resources and increased likelihood of adverse health outcomes of COVID‐19. This includes (but not limited to): people living in overcrowded housing, collective sites, informal settlements or slums, or experiencing homelessness; people who have been forcibly displaced, migrant workers; those in rural and remote locations; people living in poverty; people with disability and those living in closed facilities; those adversely affected by the digital divide; and people affected by intersecting, accumulating or other vulnerabilities. Quality assessment: AGREE II: scope and purpose 86.1%; stakeholder involvement 25%; rigour of development 18.8%; clarity of presentation 77.78%; applicability 8.33%; editorial independence 50% Funding source: Not reported |
Reported on: Guidance for the general population may not be feasible for vulnerable groups. Guidance here presents options for ensuring that recommended measures are accessible and appropriate for vulnerable populations; this can not only ensure more equitable access but also that COVID‐19 is controlled in vulnerable populations (which affects the health of the whole population). Findings summarised below focus on communication issues related to physical distancing barriers and mitigation of these for vulnerable groups. Some population groups may have less agency to comply with PD recommendations. Potential barriers impacting PD adherence/uptake include:
Potential strategies for mitigating barriers include:
Longer‐term mitigation strategies might include advocating for provision/expansion of paid sick leave; promoting intersectoral action to deploy and expand safety nets (e.g. cash transfers) to provide temporary relief to affected households; advocating for adequate housing; and advocating to prevent charges or fees for breaking quarantine where people are leaving dangerous households, or for those without adequate housing. Other relevant public communication activities are focused on the following:
For people with disabilities:
Community engagement
Recommendations: Prevention and containment measures for the general population need to be adapted and supported in different ways for people with different vulnerabilities. This can include a range of communication, information, training and practical supports to help to mitigate the risk of COVID‐19 or of severe disease and to help to ensure more equitable health outcomes across the population. |
Communication purpose: May be useful for identifying barriers and mitigation strategies for vulnerable communities in terms of prevention and containment of COVID‐19. Also provides guidance on communication strategies and features that may usefully inform tailoring of public health communications to differentially vulnerable groups within populations. Related to review questions: Identifies several factors which may create vulnerability in different groups and so increase their risk of poor outcomes related to COVID‐19. Provides a range of strategies, both material (practical) and communication‐related, that may be used with the aim of redressing the imbalances or inequalities faced by many vulnerable populations. Implementation of such strategies may help to reduce barriers to uptake of preventive measures and so improve accessibility, feasibility and adherence to physical distancing measures. |
|
Cardwell 2021#^ Citation type: SR (rapid) Public health measure: Isolation, and also maps onto quarantine, and school measures Mapping to: Adherence Mapping to: Theme 3: support for individual and population behavioural changes |
Overview and aim: To identify strategies to support people in isolation or quarantine for COVID‐19 and to assess effectiveness of strategies during respiratory pathogen pandemics to support and improve adherence to these measures Type of study and data: SR; international guidance documents (WHO, ECDC from 19 countries); rapid review of primary studies (n = 1, survey) Inclusion and exclusion criteria: Included: support for people in isolation or quarantine, respiratory viruses e.g. SARS, MERS Excluded: non‐respiratory pathogens or non‐pandemic settings Participant features and numbers, sampling details: General populations across 19 countries; no specific groups noted, although some countries may target support to vulnerable groups or those already receiving state aid. Two primary studies (same dataset): 1) 257 families, 49% under 12 years, 54% male; 2) 133 households Included disease(s): Respiratory diseases e.g. SARS, MERS, influenza Timing: Search up to January 2021, literature limited to 2000 onwards. No further information related to timing of the pandemic or related communications Countries included: International guidance from Austria, Australia, Belgium, Canada, Denmark, England, Finland, France, Iceland, Ireland, Netherlands, New Zealand, Northern Ireland, Norway, Scotland, Singapore, Sweden, Switzerland, Wales Rapid literature review: Australia All high‐income countries Intervention or phenomenon of interest: Support (any public health guidance or measures) for isolation or quarantine measures Quality assessment: 5/11 AMSTAR: [2. Single screening and data extraction only (second reviewer checked extracted data); 5. No excluded studies reported and included not very clear; 6. Characteristics of included studies not clearly reported; 8. Quality not incorporated into findings/conclusions; 10. Publication bias not assessed; 11. No COI included studies reported] Funding source: This research was funded in part by the Health Research Board under grant no. HRB‐CICER‐2016‐1871. |
Reported on: Support measures from 19 countries were analysed and identified 5 categories of support. Psychological, addiction and safety support measures:
Essential needs support measures:
Information:
Financial support:
One study reported different measures put in place to support people during isolation/quarantine for H1N1 in Australia, with positive cases in classrooms the trigger for school closures and quarantine.
Recommendations: Across countries there is variation in the type and intensity of support offered to people undertaking isolation or quarantine measures to protect public health during the COVID‐19 pandemic. Some countries target support to vulnerable groups; and many countries leverage support during the pandemic from existing services rather than creating new structures and services to provide such support. Most services are reactive, requiring individuals to initiate the support, although some proactively target vulnerable (medically or financially) populations. As well as support for isolation and quarantine, many countries have in place punitive measures for lack of adherence. Adherence to measures may be influenced by the culture in which the measures are implemented. Adherence to isolation and quarantine measures may be improved by better knowledge of the measures and their rationale, and provision of financial support and essential supplies. Providing consistent and factual information may promote adherence to measures; warning people about misinformation and addressing inaccuracies or conspiracies in available information is similarly important. Information and messages emphasising the supports that will be provided should isolation or quarantine be needed are beneficial, so that people know what is available as well as how to access supports, should they be needed. Framing messages positively in terms of the benefits for society and for themselves and communicating to promote solidarity and the altruistic nature of adherence, may also improve adherence. |
Communication purpose: May inform the purpose(s) and range of supports available for people undertaking isolation or quarantine. May also inform communication strategies to inform individuals and communities about the supports available to them, including what these are, who is eligible, and how to access them, should they be needed. Related to review questions: Different supports are needed for people undertaking isolation/quarantine. These range from information and mental health services to access to essential supplies, PPE and financial support. Supports may vary in intensity (comprehensiveness) and target (generally or to specific vulnerable populations). Clear, consistent information about isolation and quarantine measures, and their rationale and features (e.g. duration, what is required), is needed to help people know what to do and how to adhere to the measures. Information is also needed about what supports for isolation and quarantine are available, and how, where and who can access these supports, so that people are clear about the options in place and what to do if the situation requires it. Information may be consumed via multiple sources and communicated via different media, such as websites and helplines, information pamphlets and portals, and mobile phone apps. Financial insecurity is a major contributor to lack of adherence, particularly for those of lower socioeconomic status. Lack of suitable accommodation and essential supplies are further barriers, as are inconsistent information, stress and stigma associated with quarantine. |
|
Chu 2020#^ Citation type: SR Public health measure: Isolation, and also maps onto quarantine Mapping to: Acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication Theme 5: public trust and perceptions Theme 6: distancing measures in schools and workplaces |
Overview and aim: To identify social consequences of mass quarantine (measures that restrict physical contacts and mobility of 10,000 or more people or all residents in a specific jurisdiction) during infectious disease outbreaks; and to identify strategies to mitigate negative social impacts of movement restrictions for COVID‐19 Type of study and data: SR; qualitative, quantitative and mixed methods studies; N = 15 (6 qualitative, 6 quantitative, 1 mixed‐methods, 2 ethical) Surveys (telephone, web‐based, mail; cross‐sectional), interviews and focus group methods and evidence synthesis (for ethical studies). Inclusion and exclusion criteria: Included: Social impacts of mass quarantine during infectious disease outbreaks; empirical research Excluded: Studies without peer‐reviewed original empirical evidence (e.g. thesis, book chapters and reviews) or focusing only on epidemiological consequences of mass quarantine (e.g. estimates of infection, disease rates/risks) Participant features and numbers, sampling details: Sample sizes ranged from small numbers of key informants (e.g. n = 9 to 42) to larger samples up to approximately 1000 people responding to surveys. Participants included residents of affected villages, regions, or cities, community leaders and key informants for organisations and communities, healthcare workers, printing company workers and university faculty. Included disease(s): SARS (8 studies), EVD (4), COVID‐19 (2), H1N1/influenza (1) Timing: Searches inception to April 9, 2020 Eight studies focused on 2003 SARS outbreak; 4 on 2014‐16 EVD outbreak; 1 on 2009‐2010 H1N1 outbreak; 2 on 2020 COVID‐19 outbreak. Quarantine range: 7 days to 1 month; not specified in 3 studies, not applicable in a further 2 studies Countries included: SARS outbreak Canada, China, across‐countries (8 studies): EVD Sierra Leone and Liberia (4), COVID‐19 China and multiple countries (2), H1N1/influenza Canada (1) Country income tended towards high and upper‐middle income (SARS, H1N1, COVID‐19); and low income for EVD. Intervention or phenomenon of interest: Social consequences of mass quarantine, and strategies to mitigate negative effects Quality assessment: AMSTAR 7/11: [5. No excluded studies list provided; 8. Quality assessment not integrated into most findings; 10. Publication bias not assessed; 11. No COI for included studies] Funding source: WT/Wellcome Trust/United Kingdom |
Reported on: 6/15 studies were rated as low quality, 9/15 as high quality; with seven consequences of mass quarantine identified. Psychological distress (11 studies):
Heightened communication inequalities (9 studies):
Food insecurity (8 studies):
Economic challenges (7 studies):
Diminished access to healthcare (6 studies):
Disrupted education (4 studies):
Gender inequality and violence (3 studies):
Recommendations: Several negative effects of mass quarantine were identified; the only positive effect identified was altruism. Since mass quarantine can lead to several negative social consequences and may worsen existing inequalities, a focus on reducing social inequalities should be a priority for countries to build resilience and preparedness for future outbreaks. Authorities should implement specific interventions and equity‐based strategies to mitigate socioeconomic implications and mental health impacts of mass quarantine, and clearly tackle social inequalities during mass quarantine and in preparation for lifting such restrictions. Negative social consequences of mass quarantine, such as poor psychological outcomes, can exacerbate existing inequalities or determinants of health. Negative effects may disproportionately affect people experiencing financial hardship, those who are unemployed, or who cannot work from home. Limited access to overloaded healthcare services may also worsen psychological effects, inhibit consultations for those with existing conditions, and substance abuse may be left untreated. A sense of altruism was a positive consequence of mass quarantine; authorities may promote altruism by developing culturally competent, context‐specific strategies; promote use of digital technologies to increase healthcare capacity and harness technology to better enable social connectedness amongst populations. Negative impacts of mass quarantine included reinforcing stigma against minority populations, increased misinformation, and lowered trust in authorities. Such effects have exaggerated existing communication inequalities, which may be negatively associated with outbreak preparedness; these have been compounded by poor information governance across authorities (e.g. no rationale for decision‐making, inconsistent information and instructions and lack of coordination of mass quarantine). Authorities can improve communication by designing equity‐based communication messages (such as information tailored to individual needs based on age, educational level, language), based on accurate data and measures adjusted for risk of disease, consulting community representatives (e.g. those from social minority groups) in developing supplementary measures to lockdowns, and learn from examples of successful misinformation curbing. Community engagement, transparency and tailored strategies to address misinformation are key elements of communication inequality mitigation. Responses should also aim to mitigate existing social disparities (e.g. those for women or ethnic minorities) and respond to needs of vulnerable populations identified directly. Negative effects of mass quarantine may more heavily burden countries unprepared for public health emergencies. For instance, food insecurity may lead to panic buying in high‐income countries but to population‐level famine in low‐income countries; similarly, remote learning may be feasible in urban centres but not for those living in poverty, or in remote areas with poor digital infrastructure. Interventions are therefore needed to address existing disparities as well as those worsened by mass quarantine. |
Communication purpose: Findings may inform authorities’ planning and implementation of mass quarantine, including communication to inform populations of measures and to support them in practical terms. Related to review questions: Mass quarantine has several negative effects on society and may worsen existing inequalities. Communication strategies to engage with and inform populations about the measures therefore needs to explicitly address such communication inequalities. Communication between authorities and the population should provide clear, accurate and consistent information; actionable messages; and these must be tailored to different groups within the population (e.g. those of lower health literacy or minority racial groups). Introducing mass quarantine needs to recognise the unintended negative effects of such measures upon the population, and that vulnerable groups may be disproportionately affected. This may require tailored or intensified support (e.g. financial support, food, family violence support and other necessities) to be provided to some or all of the population under quarantine. Strengthening of health systems, and associated support (e.g. access to psychological support) is also indicated. |
|
ECDC 2020b# Citation type: GL Guidance on infection prevention and control of COVID-19 in migrant and refugee reception and detention centres in the EU/EEA and the UK (europa.eu) June 2020 Public health measure: Isolation, and also maps onto quarantine, and crowd avoidance Mapping to Uptake, acceptability, adherence, feasibility Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: To describe measures for prevention and control of COVID‐19 for refugees and migrants (including asylum seekers and others) living in reception and detention centres Type of study and data: GL (technical report) Included disease(s): COVID‐19 Timing: None specific Countries included: EU/EAA and UK Higher‐income countries Intervention or phenomenon of interest: Communication to support preventive health measures in refugee/migrant detention centres Quality assessment: AGREE II: scope and purpose 86.1%; rigour of development 12.50%; editorial independence 25% Funding source: Not reported |
Reported on:
Risk communication and community engagement:
Actionable messaging:
Addressing rumours and fears:
Addressing stigma and discrimination:
Recommendations: Preventive measures like physical distancing may be difficult to implement in refugee/migrant reception or detention centres, due to problems such as overcrowding and lack of facilities. Despite this, physical distancing and other measures should be promoted by providing clear, accurate, understandable information to residents, focusing on actionable messages about prevention and healthcare. Information must be tailored appropriately to language, health literacy and culture, and should aim to address misconceptions or rumours. |
Communication purpose: Findings can inform strategies for developing appropriately tailored (to health literacy, cultural background) information to communicate with refugee and migrant populations to reduce risk of COVID‐19 transmission. Related to review questions: Despite the difficulties inherent in implementing preventing measures in migrant/refugee detention centres, the aim should be to enact physical distancing and others measures as well as possible given practical limitations (e.g. overcrowding). Communication is key in such situations, to convey risk of disease and actionable messages about prevention. Information needs to be trusted and tailored appropriately to the audience, which may be assisted by community engagement. Information should address misinformation that might otherwise create a barrier to behavioural changes to protect health. |
|
ECDC 2020a# [Guidance on the provision of support for medically and socially vulnerable populations in EU/EEA countries and the United Kingdom during the COVID‐19 pandemic, 3 July 2020. Stockholm: ECDC; 2020] Citation type: GL Public health measure: Isolation, and also maps onto quarantine, general PD Mapping to: Acceptability, adherence, feasibility Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: To provide guidance (for civil society, NGOs and national, regional authorities) on major challenges, successes and lessons learned from organisations providing support to medically and socially vulnerable people during the COVID‐19 pandemic Type of study and data: GL: guidance presented as technical report based on triangulation of findings from rapid review and across‐country survey (EU/EEA/UK). Authors noted this is exploratory, rather than exhaustive. Included disease(s): COVID‐19 Timing: Survey completed June 2020; in response to stay‐at‐home measures from March‐May 2020 but in anticipation of further restrictive measures as pandemic progresses Countries included: EU/EEA/UK high income Intervention or phenomenon of interest: Challenges for people living in vulnerable situations during pandemic (medically vulnerable or socially vulnerable) and ways to address these Quality assessment: AGREE II: scope and purpose 75.0%; stakeholder involvement 55.56%; rigour of development 13.5%; clarity of presentation 66.67%; applicability 6.25%; editorial independence 0% Funding source: Not reported |
Reported on: [data extraction focuses on findings of the joint review + survey data, not on the separate results of each] The COVID‐19 pandemic has created huge challenges in terms of morbidity and mortality, but also in terms of social and economic impacts. Within populations, some people are much more vulnerable to the effects of COVID‐19 than others. This may be a medical vulnerability (i.e. people at higher risk of death or severe disease e.g. older people, people with underlying medical conditions), a social vulnerability (i.e. vulnerable due to the public health measures put in place to control COVID‐19 e.g. people with long‐term physical, mental, intellectual or sensory impairments, homeless people, ethnic minorities, irregular migrants), or overlapping or accumulating categories of vulnerability which create particularly challenging circumstances. There is need for policy responses that recognise the particular challenges faced by each type of vulnerable population, and that allow a more comprehensive approach to address shared challenges and needs across groups. Some of the challenges identified for people who are medically/socially vulnerable have included:
Information jointly analysed from a rapid review and across‐country survey indicated a range of strategic good practices to better support vulnerable groups during the pandemic, particularly if there are surges of cases requiring reintroduction of restrictive measures (i.e. movement restrictions and stay‐at‐home orders) and their accompanying challenges. Those practices most closely related to communication and physical distancing measures are summarised below. Clear communication between service providers and users: Standard risk communication principles should be used when communicating with service users, including:
Community engagement:
Use of online/digital technologies: Online technologies (e.g. video or telephone services, virtual peer support groups, group sites for sharing information and lessons), have been an essential way to provide support during the pandemic, and to assist with continuity of existing services. However, such services may not be appropriate in all cases, for instance:
In such cases, other means of reaching people are needed and must be accessible (e.g. by providing financial reimbursement for costs, mobile devices, training). Maintaining social connections: Efforts are needed to ensure that vulnerable people are not socially, as well as physically, isolated. These might include assistance with planning how to keep in touch with family/friends, counselling or psychosocial support, and online group activities. Other key good practices identified include the following:
Recommendations: Recognition of and attention to addressing the particular challenges of vulnerable groups during the pandemic is key. Principles of risk communication can inform communication strategies for such groups, and community engagement may critically inform responses developed to support vulnerable people within the population, as well as helping to build trust, sustainability and acceptability of responses. Digital technologies may assist in adapting some support services for vulnerable people; but care must be exercised as lack of easy access to such technologies may otherwise further marginalise people from vulnerable groups. Provision of material, including financial, support is crucial to ensure that routine services are maintained and extended for those experiencing disproportionate effects of the pandemic due to one or more vulnerabilities. |
Communication purpose: Findings can inform development of public health communication and information strategies to more effectively and appropriately reach vulnerable groups within the community. Related to review questions: Improving communication and support of vulnerable populations may improve uptake, acceptability and adherence to measures; and may mitigate some of the unintended consequences of PH measures in vulnerable groups within the community. |
|
Mao 2021# Citation type: SR (rapid) Public health measure: Isolation, and also maps onto quarantine, and general PD Mapping to: Adherence, feasibility Mapping to: Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication |
Overview and aim: To identify models and features of volunteering in the UK during the COVID‐19 pandemic (volunteering defined as giving unpaid help as an individual or through a group, club or organisation, to people who are not a relative) Type of study and data: Rapid SR; qualitative and quantitative; N = 27 (13 reports, 3 briefings, 5 blog posts, 2 newspaper articles, 2 websites entries, 2 peer reviewed journal articles) Inclusion and exclusion criteria: Included: studies of community/volunteering groups, volunteers, community champions; UK only. Diverse research included: peer reviewed articles, reports, briefings, blog posts, newspaper articles, online media. English language only. Excluded: Non‐English language; commentary/review; not empirical or analytical Participant features and numbers, sampling details: Sample sizes varied enormously, depending in part on method e.g. 7 interviews plus 57 survey responses up to approximately 32,000 survey responses. Included disease(s): COVID‐19 Timing: Search for evidence January to October 2020. Results are discussed in terms of timing of lockdowns (early/later) and stage of pandemic. Authors note that the timing of the review (2020) represents a limitation in that findings are only relevant to the relatively early stages of the pandemic. Countries included: UK only; high‐income country Intervention or phenomenon of interest: Community volunteer activities and outcomes during the pandemic Quality assessment: AMSTAR 5/11: [1. No protocol/plan; 2. No mention of screening/data extraction details; 5. No excluded studies list; 8. Quality not integrated with findings; 10. No publication bias assessment; 11. no study COI reported]. Funding source: This work was supported by the UK Research and Innovation/Economic and Social Research Council (grant reference number ES/V005383/1). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. |
Reported on: Several major topics identified through thematic analysis Volunteering activities: addressing needs:
Volunteering activities: adapting through digital tool use:
Volunteering models:
Volunteer profiles:
Successes, challenges, and determinants of effectiveness:
Relationships with authorities:
Recommendations: Diverse volunteering activities and organisations have been apparent during COVID‐19, reflecting existing community support groups adjusting their activities and scope of their activities and the emergence of new groups to meet needs within communities. Importantly, groups appear to have modified their activities following the first lockdown (earlier section of the research sampling window), with an overall shift from immediate demands towards more structural needs. Social connections, local knowledge and social trust were key factors associated with volunteering. Volunteers also tended to be of working age, women, highly educated and middle class. To date community engagement with volunteer groups has been limited but public engagement and community support have been critical during the COVID‐19 pandemic and are likely to have a key role in future public emergencies. |
Communication purpose: Findings may be useful for informing strategies to communicate with communities about isolation and lockdown measures, as well as identifying a range of needs of communities during enactment of such measures. Related to review questions: Volunteer groups and activities are diverse and have a critical role in supporting people during the pandemic, e.g. in relation to adherence to isolation (lockdown). Early activities focused on delivery of essential supplies; later, on overcoming social isolation apparent in many in the community; and after the first lockdown, activities shifted to address wider pandemic impacts and unmet needs of community members. Provision of such supports may assist people to adhere to isolation measures. Volunteer activities and organisations have needed to remain flexible in order to respond the changing circumstances with the prolonged pandemic emergency, for instance moving services to digital delivery or adapting delivery and activities undertaken, while attempting to address issues such as digital exclusion through other communication methods (e.g. mass leaflet drops). New partnerships and knowledge formed through mutual aid groups responding in early stages of the pandemic may be valuable as the pandemic continues but also in future emergencies. Volunteering structures which incorporate leadership together with information sharing and shared decision‐making may be best placed to respond to the wide range of needs that are encountered. Co‐ordination and communication with authorities by a community‐led infrastructure may help to ensure that the needs of those people within the community not met by standard government services are identified and met. People who volunteer tend to show social support and engagement, strong trust in people to follow guidelines and trust in government, as well as social connection. A promising model includes community champion schemes, where volunteers are provided with the most recent information (including infographics in community languages) on COVID‐19 to share with their community, as well as providing feedback from the community to authorities about which communications are effective and which are not. Authorities consulting with community groups may provide helpful information on current or future priorities and needs within the community, for example, that clear advice is available to communities as they move out of restrictions (lockdown), that inequalities within communities are addressed, and that support for children to return to school or for businesses to reopen is provided. |
|
Mobasseri 2020# Citation type: SR (scoping) Public health measure: Isolation, and also maps onto general PD Mapping to: Adherence Mapping to: Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes |
Overview and aim: To review the evidence on issues faced by older people during the COVID‐19 pandemic Type of study and data: Scoping review; 210 included papers; quantitative and qualitative (included guidelines, reviews, epidemiological research, editorials, brief reports etc.) Inclusion and exclusion criteria: Included: all publications on COVID‐19 and older adults (research, reports, guidelines, news articles, and scientific material); English language Excluded: non‐English language papers Participant features and numbers, sampling details: ‘Older adults’; no further details Included disease(s): COVID‐19 Timing: Searches for literature January to end July 2020 Countries included: China, France, US, UK, Italy, Germany, Spain, Australia, Ireland, other. All upper middle‐ or high‐income countries Intervention or phenomenon of interest: Issues for older people living through a pandemic Quality assessment: AMSTAR 4/11: [1. No protocol/plan; 5. No real features of included studies; 6. Excluded studies listed; 7,8 quality not assessed or integrated into findings; 10. Publication bias not assessed; 11. No COI for included studies] Funding source: This study is the part of research project funded by Tabriz University of Medical Sciences (Grant No: 65164) and approved by regional research ethics committee of Tabriz University of Medical Sciences; Approval ID: IR.TBZMED.REC.1398.1278. |
Reported on: Six themes identified; those relevant to communication are summarised below. Support and information sources:
E‐Health services:
Essential supply access:
Physical and mental consequences of self‐isolation:
Neglect and age discrimination:
Recommendations: Older people have a range of needs, issues and challenges associated with living through the pandemic. These may require tailored services, information and support to improve and maintain people’s well‐being. The media has a key role in educating the public and preventing age discrimination. Telemedicine may be an effective way to deliver healthcare, but older people need support and information to be able to access health or social care online. Younger people can support older people in isolation through grocery delivery, helping with everyday tasks and supporting their use of technology, so they can remain socially connected. |
Communication purpose: Findings indicate some specific issues for older adults, particularly related to remotely accessing health or other services, and so may inform strategies to improve support to these people. Related to review questions: A range of services, including access to food and essential supplies, is needed to support older adults during isolation required to protect their health during the pandemic. Although remotely delivered health and social care may assist older people to participate in these activities more readily, many do not have ready access to technology or know how to use it. Information and guidance are therefore needed to enable older people to make use of such services. |
|
Regmi 2021# Citation type: SR Public health measure: Isolation, and also maps onto quarantine, crowd avoidance and general PD Mapping to: [major outcome categories] Acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 3: support for individual and population behavioural changes Theme 5: public trust and perceptions |
Overview and aim: Identification of factors associated with implementation of non‐pharmaceutical (NPI) measures (physical distancing, isolation, quarantine) for reducing COVID‐19 transmission Type of study and data: SR; qualitative and quantitative primary research. N = 33 studies included (cross‐sectional (26), 4 qualitative, 2 cohort, 1 case‐controlled study) Inclusion and exclusion criteria: Included: Participants of any age, gender or ethnicity, and healthcare workers; NPIs (physical distancing, isolation, quarantine); all effectiveness studies (RCTs, non‐RCTs, observational) including pre‐prints Excluded: publications lacking primary data Participant features and numbers, sampling details: 116,897 participants in total Explicitly considered older people (over 70 years) and/or those with comorbidity; as well as those ethnic populations in lower SES groups Included disease(s): COVID‐19 only Timing: Searches December 2019 to March 2021. No further consideration of pandemic timing Countries included: 17 countries including the UK (5), China (8 including Hong Kong), USA (4), Germany (3), Italy (3), the Netherlands (2), Paraguay, India, Saudi Arabia, Ireland, Tanzania, Singapore, UAE, Nepal, Sudan, Georgia, Bangladesh Studies across all income brackets (low to high income) but approximately 80% high‐income countries Intervention or phenomenon of interest: Implementation of specific NPIs, and factors (enablers and barriers) associated with these Quality assessment: AMSTAR 7/11: [5. No excluded studies listed/provided; 8. Quality assessed and reported but not linked to results specifically; 10. Publication bias not assessed; 11. No COI for included studies reported] Funding source: This research received no external funding. |
Reported on: Identified seven themes on enablers (3 themes) and barriers (4) to NPI measures No enabling themes related to communication specifically; rather focused on effective NPI elements (e.g. behavioural change following NPI measures) Of barriers identified, two relate to communication:
Further factors affecting adherence (equity implications) (13 studies):
Recommendations: Research is needed to better understand and promote adoption of specific NPIs within different countries and contexts, and to further consider the many factors that might influence this including sociopolitical, socioeconomic and cultural factors. Improving factual communication about pandemic risks, and understanding the needs and behaviours of individuals and specific populations are important.
|
Communication purpose: Factors (enablers and barriers) may be useful for developing targeted messages and information to target disadvantaged groups, and to consider tailored support for those less likely, or less able, to follow NPI measures. Related to review questions: Clear, reliable information may help to dispel distrust of public health authorities and the media, and to support adoption of behaviours needed to enact NPI measures. Provision of tailored support for those at socioeconomic or other disadvantage may also help people to adopt and adhere to measures. |
|
Seale 2020# Citation type: SR (rapid; not truly systematic) Public health measure: Isolation, and also maps onto quarantine, school measures, and work measures Mapping to: Uptake, acceptability, adherence Mapping to: Theme 3: support for individual and population behavioural changes Theme 6: school measures |
Overview and aim: To identify key determinants of community engagement with individual protective behaviours and non‐pharmaceutical measures for COVID‐19, and their impacts on individuals, and to identify behaviour change interventions to promote and support community participation in required measures Type of study and data: Rapid SR; qualitative and quantitative studies; 53 included Inclusion and exclusion criteria: Included: Community settings (general population, non‐healthcare); English language; published, peer‐reviewed research; COVID‐19, SARS, MERS, H1N1, influenza A, hypothetical pandemics; personal protective and environmental measures (data not extracted) and NPI measures (isolation and quarantine, school and workplace measures, crowd avoidance) Participant features and numbers, sampling details: Not reported across included studies; specific examples cited related to described results Included disease(s): COVID‐19, SARS, MERS, H1N1, influenza A, hypothetical pandemics Timing: Searches January to March 2020 (early in pandemic). No specific time‐related factors highlighted. COVID‐19 studies published as of July 2020 were included. Countries included: Not clear for study set as a whole; NPI measure studies mentioned Australia (Aboriginal communities), Canada, New Zealand, Japan, The Netherlands, USA, Taiwan, Liberia. All high income except Taiwan (upper middle‐income) and Liberia (low‐income) Intervention or phenomenon of interest: Community engagement with NPI measures, and effects upon behaviours such as adherence to measures Quality assessment: 3/11 [1. No protocol; 4. Only published literature considered; 5.6 no list or complete characteristics of included studies; 7. No quality assessment or 8. Use in formulating results; 10. Publication bias not assessed; 11. COI for included studies missing] Funding source: There was no funding associated with this study. |
Reported on: [N.B. results related to personal protective measures not extracted – outside review scope] Isolation and quarantine:
Recommendations: NPI measures need to be introduced with practical supports (e.g. financial support, communication systems for contact while in isolation/quarantine). Information to support the measures needs to consider health literacy levels; be written in clear lay language including acknowledgement of the difficulties of adhering as well as information on the impact of measures and how to address or reduce negative impacts. School measures:
Communication themes:
Recommendations: A key focus needs to be community participation and co‐design of communication messages, materials and delivery of these (outreach) to support community behaviour change (adherence). Clear, consistent information about measures, including rationale for their use and practical ‘how to’ information (what can and cannot be done; who, what, when and where), as well as emphasising benefits of adherence, is critical as NPIs are introduced and implemented. Reciprocal support (social, healthcare, financial supports) is needed alongside communications to promote adherence. Communications need to be tailored to the community, including to lower health literacy levels, and/or to those less likely to adhere to measures. Involving community leaders in communicating key messages may help to build trust and move the community towards action. |
Communication purpose: Findings may inform development of communication messages for communities and individuals who are being asked to adhere to NPI measures such as isolation, quarantine and school closures. They may also inform development of tailored communication messages to particular groups within communities, such as those less likely to adhere to measures, or those with lower health literacy levels. Related to review questions: Clear, consistent communication and information about NPIs are needed to support people’s adherence to the required measures. NPI strategies should be proportional to the risk, and communications accompanied by reciprocal support (e.g. social and financial supports) for those adhering to the measures. A clear rationale for the measures needs to be widely communicated so that people accurately understand the risks, and should be accompanied by clear, actionable and consistent information about what people need to do to protect their health. Involving communities in developing and delivering messages to support the required behaviour changes may build trust and improve adherence. Communication and information provision should be tailored to local communities and groups within communities, such as those who are less likely to adhere, and use a range of media (e.g. social media, posters) to optimise reach. |
|
WHO 2020c# At: COVID-19 Global Risk Communication and Community Engagement Strategy – interim guidance (who.int) Interim guidance December 2020 Citation type: GL Public health measure: Isolation, and also maps onto crowd avoidance, and general PD Mapping to: Uptake, acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: To describe components of revised risk communication and community engagement framework and guidance in the context of the ongoing COVID‐19 pandemic Type of study and data: GL: based on series of stakeholder consultations and underpinned by meta‐analysis of 9 databases Included disease(s): COVID‐19 Timing: Nonspecific Countries included: WHO; international Intervention or phenomenon of interest: Risk communication and community engagement elements as key to pandemic PH responses Quality assessment: AGREE II: scope and purpose 52.8%; stakeholder involvement 44.44%; rigour of development 24.0%; clarity of presentation 58.33%; applicability 29.17%; editorial independence 33.3% Funding source: The RCCE Collective Service is a collaborative partnership between RCCE practitioners, convened by IFRC, WHO and UNICEF, with support from the Global Outbreak Alert and Response Network (GOARN), and key stakeholders from the public health and humanitarian sectors |
Reported on: Extracted data focuses on RCCE strategy components and purposes related most closely to PD measures for COVID‐19 prevention and control. Revised RCCE strategy reflects shift from directive, one‐way communication to community engagement and participatory approaches that have been successful in control and elimination of past disease outbreaks. The overall goal is to promote person‐centred, community‐led approaches in order to increase trust and social cohesion, and to decrease negative impacts of COVID‐19. Generally, data show that people know about COVID‐19 and the preventive measures needed to protect themselves, but risk perceptions are falling and complacency growing alongside increasing pandemic fatigue and uncertainty and falling confidence in ability to control the pandemic. Uptake of protective behaviours and adherence to measures will continue to be critical to controlling COVID‐19 even with effective vaccines and treatment; therefore strengthened RCCE will be critical to improve knowledge, acceptance and uptake of measures. Community engagement is key to understanding local contexts and ensuring an informed, appropriate (person‐centred) response, without which misinformation, confusion and mistrust can undermine public health efforts. Pandemic fatigue is growing and is likely to lead to fewer people being motivated to follow recommended preventive behaviours, and can be influenced by several factors including: lowered disease risk perceptions, increased socioeconomic and psychological impacts of the pandemic and restrictions, stress of uncertainty, becoming used to living in a pandemic situation and decreased trust in authorities. Importance of engaging stakeholders to design and implement communication strategies is emphasised, alongside mechanisms for feedback from stakeholders (which underpins effective two‐way communication and engagement). Meta‐analysis of multiple datasets identified the following related to communication and physical distancing measures:
Objectives of RCCE include:
RCCE efforts need to prioritise the most medically or socially vulnerable, with many different groups identified, including:
Major themes anticipated in immediate‐to‐medium term future (with relevance to communication for physical distancing measures:
Recommendations: Global trends in knowledge, perceptions, fatigue and related factors (e.g. economic impacts) indicate that effects of the pandemic are many and complex and make effective communication to increase PHSMs uptake challenging. RCCE and community engagement are key to promoting PHSMs and to addressing problems evident across communities and populations worldwide. At its heart, this should engage communities in two‐way dialogue to support locally appropriate processes, interventions and mechanisms to support and sustain implementation of required PHSMs. This should include deliberate consideration and engagement with those who are vulnerable (of which there are many) and work to ensure that engagement is representative of local communities. Co‐ordinated efforts to tackle misinformation will be critical, as this can lead to poor adherence to public health advice (as well as increase stigma and adversely affect health), which limits the effectiveness of the measures in countries’ pandemic responses. Pandemic fatigue will increase with the continuation of the pandemic, and better understanding is needed of the effects of this, e.g. people’s efforts to follow preventive measures may fall, their efforts to stay informed may also fall. Identifying and creating ways to engage and motivate people by partnering with local groups and leaders may help to improve motivation and therefore adherence to measures. |
Communication purpose: Findings may inform effective communication and engagement strategies and processes to address both existing and emerging issues (e.g. pandemic fatigue, economic and social pressures) experienced by people across the world that can impact on uptake and adherence to PHSMs to prevent and control COVID‐19. Related to review questions: Many factors affect adherence to physical distancing measures. Some are structural or practical; others reflect sociocultural factors within local communities and populations. Community engagement and clear communication and information may assist with addressing some of the identified barriers to adherence to measures. |
| Primary studies | |||
|
Burnet 2020a# (primary) Mapping to: Adherence, also to acceptability Also relevant to public health measures 3 (quarantine) and 6 (crowd avoidance) |
Overview and aim: Exploration of Australians’ experiences of self‐isolation/quarantine and barriers and enablers to successful self‐isolation/quarantine Inclusion and exclusion criteria: Included: Adults (20 to 73 years), self‐isolating (or have done so) in Australia after being instructed to by a health or government authority Types of study and data: Primary qualitative study Countries included:Australia Quality assessment: 6/10 CASP score (recruitment strategy not reported; no referral to researcher/participant relationship; ethics approval not reported; no primary quotations used, analysis method not stated, coding framework not included) |
Reported on:
Communication:
Service provision/support:
Recommendations: Enhance immediate and ongoing communications to promote better knowledge about required self‐isolation/quarantine measures, including information to make the distinction between these measures and physical distancing measures clear. Create and disseminate consistent central information using lay language and incorporating practical information about initiation of measures, compliance, and services available to support the measures (including mental health services). Develop better ongoing support to enable people to be as compliant in home‐based and community‐based quarantine as possible, while reducing long‐term physical and mental health effects. This includes easily accessed food, medication, mental health services and financial support. This will be particularly important for those who are in home‐based quarantine without all the immediate government supports. Communicate the availability of these support services widely. Communicate about home and community‐based quarantine in a supportive, ‘no blame’ manner. |
Communication purpose: This may inform communication with individuals who have been asked to self‐isolate or are in quarantine to adhere to health or government authority requirements. These findings may also inform communication with communities about preparing for, or complying with, isolation or quarantine. Related to review questions: Findings show that individuals’ perceptions and experiences of self‐isolation and quarantine are affected by their access to clear information. Lack of information, contradictory/confusing information or difficult‐to‐find information about what people can and cannot do while in isolation/quarantine was related to non‐adherence. Access to basic services for those in isolation/quarantine must be assured, and information about these services communicated widely, including about mental health services and financial support, and how to access these services. |
|
Burnet 2020# (primary) Mapping to: Adherence (primary) but may also map to acceptability Also relevant to public health measures 3 (quarantine) and 6 (crowd avoidance) |
Outcomes and aim: Exploration of Australians’ experiences of self‐isolation/quarantine and barriers and enablers to successful self‐isolation/quarantine Intervention or phenomenon of interest: Adults (18 to 73 years), self‐isolating (or have done so) in Australia after being instructed to by a health or government authority Types of study and data: Primary qualitative study Countries included: Australia Quality assessment: 6/10 CASP score (recruitment strategy not reported; no referral to researcher/participant relationship; ethics approval not reported; some primary quotations used but analysis method not stated, coding framework not included) |
Reported on:
Findings reported here focus on social distancing measures and communication. Communication and information access: Fear and a lack of clear advice is driving symptomatic (COVID‐19) people to travel back to Australia without reporting symptoms, as they do not trust they will be supported to return home, and they do not understand Australian government policy.
Service provision:
Recommendations: Key recommendations to improve compliance with quarantine and reduce negative population‐wide health effects include:
|
Communication purpose: This may inform communication with individuals who have been asked to self‐isolate or are in quarantine to adhere to health or government authority requirements and also clarify transmission risks once quarantine is complete. These findings may also inform communication with communities about preparing for, or complying with, isolation or quarantine and also transmission risks once recovered from COVID to reduce stigma. Related to review questions: Better communication and information about home‐based quarantine, including practical information, are needed to support people’s adherence to required measures. Access to support services for those in self‐isolation/quarantine must be assured, and information about these services communicated clearly, including mental health services, maternal and child checks and financial support, and how to access these services. Community‐level plain language information must be communicated about transmission risks in those transitioning from quarantine to physical distancing and aiming to reduce stigma so that people can safely transition out of quarantine. People with COVID experience stigma due to fear of community transmission and which may potentially negatively impact testing and contact tracing, so threatening the effectiveness of public health measures. |
|
Farooq 2020# (primary) Mapping to: Uptake Also relevant to general PD measures, particularly crowd avoidance |
Outcomes and aims: Investigates the impact of cyberchondria (continuous impulses to go online and read about concerning health topic) and information overload on voluntary self‐isolation intention Intervention or phenomenon of interest: Study develops and tests a model based on protection‐motivation theory to identify whether intermediate constructs (related to threat appraisal and coping appraisal) are impacted by cyberchondria or information overload and then influence self‐isolation intention. Inclusion and exclusion criteria: Included: Students, faculty, and employees of a university Type of study and data: Questionnaire‐based survey; 225 respondents; (March 19, 2020) using online survey tool Webropol. Descriptive statistics for all survey measures Countries included: Finland Quality assessment: Response rate: + representativeness: + COI: authors declared no COI exists; participants were geographically (Finland) and socially limited (students/staff of a university); pre‐print paper (not peer‐reviewed) |
Reported on:
Recommendations: Generally, cyberchondria and information overload are regarded as negative consequences of online information, however, during the COVID‐19 pandemic, they may indirectly contribute to self‐isolation intention. Sourcing information primarily from social media increases both cyberchondria and information overload. Recommended personalising communication by providing: 1) reassuring/hopeful messages targeting individuals experiencing cyberchondria; 2) communication aiming to increase perceived severity of the situation targeting those with no intention to self‐isolate; 3) clearly structured communication using reliable health information targeting those experiencing information overload. |
Communication purpose: Findings may be useful for enabling communication; facilitating decision‐making and supporting individuals’ behaviour change in relation to uptake of physical distancing behaviours (intention to adopt self‐isolation). Related to review questions: Findings link information provision (cyberchondria and information overload) to perceived threat and appraisal of coping and through them, influences intention to self‐isolate. Findings suggest that clear, tailored communication targeting particular groups may help to counteract some of these effects, particularly associated with social media as the primary information source, and so positively influence intention to self‐isolate. |
|
Qazi 2020# (primary) Mapping to: Uptake Focused on general PD measures particularly crowd avoidance |
Outcomes and aim: Effects of formal and informal information sources on situational awareness (perceived public understanding) to predict adoption of PD measures during COVID‐19 Inclusion and exclusion criteria: Included: Adults 18 years and older Type of study and data: Questionnaire‐based survey; 210 responses. Formal information sources (e.g. newspapers, press releases, educational messages) and informal sources (social media, peer and family views) Countries included: Unclear, likely Pakistan Included disease(s): Specific to COVID‐19 but based on same theory used for SARS outbreak analysis Quality assessment: Response rate: + representativeness: + authors declare no COI; people with lower computer skills/access underrepresented; paper published (peer reviewed) |
Reported on:
Recommendations: Formal and informal information sources influence public situational awareness. This in turn increases adoption of preventive behaviours (physical distancing). Formal sources are associated with greater compliance with physical distancing measures; informal sources may not be influential until preventive behaviours have been adopted by the community. |
Communication purpose: This may guide communication with communities to prevent transmission through adoption of public health measures (physical distancing). Related to review questions: Findings link information provision through informal and formal routes to changes in perceived understanding, and with adoption of physical distancing measures. |
# COVID‐19‐specific study
Abbreviations: AGREE II: Appraisal of Guidelines for Research & Evaluation II tool AMSTAR: A Measurement Tool to Assess Systematic Reviews BAME: Black, Asian and minority ethnic COI: conflict of interest ECDC: European Centre for Disease Prevention and Control EEA:European Economic Area EU: European Union EVD: Ebola virus disease FAQ: frequently asked questions GL: guideline GOARN: Global Outbreak Alert and Response Network H1N1: H1N1 influenza strain IFRC: Internation Federation of Red Cross and Red Crescent Societies LMIC: low and middle income country MERS: Middle Eastern respiratory syndrome NGO: non‐goverment organisation NPI: non‐pharmaceutical intervention PD: physical distancing PH: public health PHSM: public health and social measures PPE: personal protective equipment RCCE: risk communication and community engagement RCT: radomised controlled trial SARS: Severe Acute Respiratory Syndrome SES: socioeconomic status SIM: subscriber identity module SMS: short message/ messaging service SR: systematic review UAE: United Arab Emirates UNICEF: United Nations International Children's Emergency Fund WHO: World Health Organization
Table c: Quarantine
| Public health measure 3: Quarantine | Study features | Outcomes and findings | Translational steps |
| Systematic reviews, guidelines | |||
|
Brooks 2020*^ (rapid review) Mapping to: Acceptability, feasibility and related factors |
Outcomes and aim: Psychological impact of quarantine and mitigation Inclusion and exclusion criteria: Included: participants entering quarantine of at least 24 hours, outside hospital setting Types of study and data: Rapid SR; 24 included studies. Surveys (cross‐sectional, longitudinal, other), observations; focus groups and interviews Included disease(s): SARS (14 studies), EVD (5), H1N1 (2), MERS (2), equine influenza (1) Countries included: Taiwan (2), Canada (8), Australia (2), Liberia (2), South Korea (2), China (4), Canada and USA (1), Sierra Leone, Senegal, Hong Kong Quality assessment: 4/9 AMSTAR rating% Funding source: The research was funded by the National Institute for Health Research (NIHR) Health Protection Research Unit in Emergency Preparedness and Response at King’s College London, in partnership with Public Health England, and in collaboration with the University of East Anglia and Newcastle University. |
Reported on:
Recommendations: Quarantine people for the shortest possible time (based on scientific evidence of incubation times, rather than indefinitely). Provide information (rationale and guidelines for quarantine – what is happening, and why) through clear, consistent communication. Provide adequate supplies, both general and medical. Reduce boredom by providing meaningful activities and ensuring communication with social networks (including support lines). Provide clear lines of communication for those in quarantine, should they develop symptoms (e.g. phone line/online service staffed by health professionals). Consider health professionals as special cases, needing support from both immediate colleagues and organisationally. Public health messages should reinforce the protective, altruistic choice of quarantine/self‐isolation. |
Communication purpose: Factors identified here may inform strategies for communicating with and supporting people in quarantine/self‐isolation, in particular to identify information required and channels of communication that may best support people in order to minimise psychological impacts of quarantine. Related to review questions: Findings suggest that lack of information, communication and support may have negative psychological effects that influence acceptability and related factors. |
|
Gomez‐Duran 2020#^ Citation type: SR (rapid) Public health measure: Quarantine Mapping to: Acceptability Mapping to: Theme 3: support for individual and population behavioural changes Theme 6: distancing measures in schools and workplaces |
Overview and aim: To investigate the psychological effects of quarantine on healthcare workers (HCWs) in order to better understand the needs and concerns of this group Type of study and data: SR; N = 12 studies; qualitative (3 studies) and quantitative (7 cross‐sectional, 1 observational, 1 prospective). 10/12 related to SARS outbreak, 2/12 EVD Inclusion and exclusion criteria: Included: primary research on HCWs in quarantine; report mental health/psychological outcomes related to quarantine; published in peer‐reviewed journal. No timing or language restrictions Excluded: not primary research, HCWs in quarantine or psychological outcomes Participant features and numbers, sampling details: Sample sizes ranged from 10 to approximately 270 HCWs, often as part of larger sample. Few details of professional role or demographics. Quarantine duration 10 days to 3 weeks Included disease(s): Outbreaks prior to COVID‐19 (included: SARS and EVD) Timing: Search for evidence April 2020 Countries included: Canada (5 studies), China (3), Taiwan (2), Senegal (1), Sweden (1) Most (8/12) studies in high‐income brackets; also middle income (upper‐middle China lower‐middle Senegal) Intervention or phenomenon of interest: Psychological impact of quarantine in HCWs, potential needs and concerns Quality assessment: AMSTAR 5/11 [1. No protocol; 4. Published papers only; 5. No excluded studies list provided; 8. Quality assessed but not closely integrated to findings; 10. no publication bias assessment; 11. no COI for included studies] Funding source: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not‐for‐profit sectors. |
Reported on: Mental health issues:
Emotional responses:
Inadequate information:
Financial losses:
Stigma:
Recommendations: Quarantine of HCWs leads to considerable psychological distress, mental health problems, isolation and financial losses, as well as stigma from various sources. Additionally, HCWs experience conflict between professional and family (personal) roles, with many expressing concerns about the impact of quarantine on their family’s safety and well‐being, especially their children. Psychological support for HCWs in and following quarantine is needed; without this, poor psychological effects can persist for years after the outbreak and quarantine period. Quarantine may present the opportunity to deliver psychological support to HCWs who would otherwise be too busy working to engage with these services. Clear, unambiguous information from health authorities and the media are needed to convey accurate information to the public about quarantined HCWs; while accurate, timely information to HCWs undergoing quarantine would assist them to manage uncertainty and consequent effects on their own health and well‐being. Concerns about their family was a common issue for HCWs; providing suitable accommodation to HCWs (outside the family home) may help to lessen the risk to families and alleviate HCWs’ concerns about infection risk. |
Communication purpose: Findings may be useful in developing public communication strategies to convey accurate information about quarantine and associated risks. Findings may also inform communication strategies for HCWs in quarantine and help to identify better mechanisms of support. Related to review questions: High levels of distress, fear of infection and poor psychological outcomes are common in the public undergoing quarantine. These same outcomes are also prevalent in HCWs in quarantine, with additional complexity because of their dual role as HCW and family member. Such issues highlight the need for better support and information for HCWs in quarantine. Providing clear, accurate and timely information about disease and quarantine risks to both those undergoing quarantine and the general public may help to mitigate some of the poor outcomes people commonly experience. It may also serve to diminish stigma associated with quarantine by members of the general public and others. Psychological support is needed to help to address some of the poor outcomes experienced by HCWs in quarantine, some of which may be long‐lasting. Quarantine may provide a window of opportunity to intervene and provide support, as otherwise HCWs may be too busy during a disease outbreak. Support for HCWs might also include financial compensation, as financial losses are commonly reported and may increase psychological distress. |
|
Lin 2014* (SR) Mapping to: Adherence Relevant to general PD measures (particularly crowd avoidance/individual PD) |
Outcomes and aim: Identification of factors associated with communication inequalities during H1N1 pandemic Inclusion and exclusion criteria: Included: communication with public during H1N1 pandemic, empirical data Excluded: not published in English, French, Italian, Spanish, Chinese or Portuguese; focused on communication between agencies or health professionals, on development of telecommunication strategies, or on public health surveillance or epidemiology; or not related specifically to the H1N1 pandemic in 2009 Type of study and data: SR; 118 included studies Population‐based studies (92/118), studies on information environment; primarily survey‐based (cross‐sectional or other), some interview or focus group‐based Countries included: USA, China, UK main countries Quality assessment: 5/11 AMSTAR rating Funding source: We acknowledge funding support from the U.S. Centers for Disease Control and Prevention (CDC) grant number 5PO1TP000307‐05 Supplement. |
Reported on:
Recommendations:
|
Communication purpose: Results may be useful for those planning communication campaigns and seeking to reduce communication inequalities across communities. Factors identified may be useful for developing targeted messages to vulnerable groups, and may inform the medium of communication, as well as the sources of information drawn upon. Related to review questions: Findings suggest that several factors influence community awareness of public health messages related to a pandemic, and this in turn influences compliance with recommended protective measures, including physical distancing measures. Communications intended to inform populations about pandemic disease and preventive measures need to take account of such factors to ensure that communication is as equitable and has as much reach within communities as is possible, in order to mount a consistent preventive response to a pandemic. |
|
Sopory 2021#^ Citation type: SR (QES) Public health measure: Quarantine Mapping to: Acceptability adherence, Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes |
Overview and aim: To examine adherence to quarantine by exploring strategies to influence adherence, identifying barriers and enablers of acceptance and identifying benefits and harms of quarantine Type of study and data: QES; any primary qualitative research. N = 17 included studies (16 qualitative, 1 mixed‐methods with separate qualitative component) Inclusion and exclusion criteria: Included: Published 2001 onwards, English language; qualitative method. Excluded: Documents (e.g. commentary) Participant features and numbers, sampling details: Quarantined population general public (14 studies), healthcare workers (7). Vulnerable populations addressed 5/16 studies Included disease(s): General infectious disease (1 study), EBV (4), influenza (4), SARS (7) Timing: Published evidence sought 2001 onwards. Event year varied across time period 2003 to 2016. Data collection period was pre‐event (4 studies), post‐real event (10), and during a real event (6). Countries included: Canada (6 studies), United States (4), Australia (1), international (1), Taiwan (1), remote First Nations Canada (2), Africa (Liberia) (1), Senegal (1)) 12/17 conducted in high‐income countries. Authors noted that the synthesis was conducted for the US context, and this may have introduced bias weighted towards understanding the phenomenon for high‐, rather than low‐middle‐ income countries. Intervention or phenomenon of interest: Adherence to quarantine Quality assessment: AMSTAR 8/11 [5. No excluded studies listed; 10. Publication bias not assessed; 11. COI of included studies not reported] Re item 1. No protocol or a priori mentioned in published paper but formed part of a larger evidence synthesis report for National Academy so determined scope is implied 2. Duplicate processes confirmed by author response. 4. Extensive searching including grey literature outlined in accompanying report Funding source: Funding for the review was received by Pradeep Sopory and Julie Novak. The review was commissioned by the National Academies of Sciences, Engineering, and Medicine (National Academies) Committee on Evidence‐Based Practices for Public Health Emergency Preparedness and Response (Contract# 20000010696), which was sponsored by the United States Centers for Disease Control and Prevention (CDC). |
Reported on: 18 synthesised findings were reported. Quarantine adherence (3 major findings, low‐high confidence):
Quarantine adherence facilitators/acceptance (2 main findings, moderate ‐high confidence):
Quarantine acceptance (4 main findings, high confidence). Restrictions may be more acceptable to people undertaking quarantine when there is:
Harms of quarantine restrictions (4 main findings, high confidence):
Quarantine and vulnerable groups (1 finding, high confidence):
Recommendations: Findings were used to develop a conceptual framework, outlining topics for considerations in situations where quarantine may be implemented to curb disease outbreak. These may help to improve acceptance and adherence to quarantine in particular. Findings indicate two major sets of communication activities to be undertaken related to the topics identified: communication within and across agencies and organisations related to the coordination of quarantine activities, and communication of information about quarantine to the general public. Quarantine is controversial and relies on the public understanding the benefits as well as risks and potential harms. These need to be effectively communicated to the public by the agencies involved in planning and implementing the restrictions. When planning and implementing quarantine, vulnerable groups within the population such as the poor or marginalised, may need additional protections. Such groups may be more at risk of harms, or the harms may be more severe – such as financial hardships that are worsened by being required to quarantine, and/or the need to safeguard civil rights of vulnerable groups. |
Communication purpose: Findings may inform development of communication strategies to provide information to the public about quarantine restrictions. Related to review questions: Information about quarantine is important to both the general public and to healthcare workers, and effective communication from agencies, tailored to local context and undertaken co‐operatively with local structures and leadership, is needed to promote acceptance and adherence to quarantine measures. Effective information and communication might best involve two‐way dialogue with the community, happen over the course of the disease outbreak, and involve multiple channels and sources. Information should be clear and accessible, non‐stigmatising or inflammatory, and include a rationale for the quarantine measures as well as information on the process and supports available for people. Recognition of the supports needed for the public undertaking quarantine is needed, alongside particular awareness of heightened risks of harms of quarantine in vulnerable groups is needed. Acceptance of quarantine may be greater, and harms minimised, where people’s needs are met, including financial compensation, food and essential supplies, and social support, and that there is some flexibility in the system to accommodate particular needs. |
|
Webster 2020#^ (rapid review) Mapping to: Adherence |
Outcome and aim: To identify factors affecting adherence to quarantine during disease outbreaks Inclusion and exclusion criteria: Included: participants entering quarantine of at least 24 hours, outside hospital setting. Studies reporting primary research, published in English or French, reporting factors associated with or reasons for (non)‐adherence outcomes Type of study and data: Rapid SR; 14 included studies. Surveys (cross‐sectional), retrospective cohort, interviews, focus groups Included disease(s): H1N1 (5 studies), EVD (3), SARS (5), mumps (1) Quarantine varied: Home quarantine (up to 14 days), EVD studies included restriction of movements (1 month), check‐ups and social distancing (21 days), state‐enforced home and neighbourhood quarantine (21 days). Countries included: Australia (5), Canada (3), Senegal, Liberia, Sierra Leone, Germany, Taiwan, USA Quality assessment: 5/11 AMSTAR rating Funding source: The research was funded by the National Institute for Health Research Health Protection Research Unit (NIHR HPRU) in Emergency Preparedness and Response at King's College London in partnership with Public Health England (PHE), in collaboration with the University of East Anglia and Newcastle University. |
Reported on:
Recommendations: To increase adherence to quarantine protocols, public health officials should provide:
|
Communication purpose: Results may inform decisions about main information messages to communicate to populations and individuals being asked to quarantine. Related to review questions: Findings indicate that several factors influence adherence to quarantine measures. Consideration of these factors should inform public health communications related to quarantine. |
|
WHO 2021b# Citation type: GL (interim advice) Considerations for quarantine of contacts of COVID-19 cases: WHO interim guidance June 2021 Public health measure: Quarantine Mapping to: Acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication |
Overview and aim: Updated advice on implementation of quarantine for contacts of COVID‐19 cases, including provision of support for people under quarantine Type of study and data: GL (interim advice); based on review of evidence and informed by experiences from Member States Included disease(s): COVID‐19 Timing: Guidance refers to importance of early communication with the public about quarantine (i.e. prior to implementation), including engagement with communities at early stages to help improve acceptability of quarantine. The importance of communicating with those undertaking quarantine at the beginning of their confinement is also emphasised. Countries included: N/A, developed by WHO, across‐country application Intervention or phenomenon of interest: Quarantine implementation and communication with those involved Quality assessment: AGREE II scope and purpose 63.9%; stakeholder involvement 38.89%; rigour of development 8.3%; clarity of presentation 77.78%; applicability 22.92%; editorial independence 0% Funding source: Not reported |
Reported on:
Recommendations: People undertaking quarantine need clear, accessible information about why the measure is needed and what is involved, as well as a range of support to enable them to undertake quarantine safely and to adhere to the restrictions during the quarantine period. |
Communication purpose: Guidance may be useful when considering communication with the public and with individuals in relation to quarantine. Related to review questions: Clear communication and information, together with community engagement, are needed prior to implementation of quarantine. This may improve acceptability and adherence to the measures. Provision of the range of supports identified may enable people to adhere to quarantine measures safely and to mitigate the economic and social risks of doing so. |
| Primary studies | |||
|
Zhu 2020# (primary) Mapping to: Uptake. Relevant to general awareness of measures required (crowd avoidance) |
Overview and aim: Public attention to a disease outbreak can be captured by social media posts, where awareness and attentiveness have implications for acceptance and adoption of prevention and control measures. Inclusion and exclusion criteria: Included: randomly sampled accounts of Weiboscope database, a nationally representative sample of the Weibo user population Timing: Between December 31, 2019, and February 12, 2020 Type of study and data: Longitudinal analysis of posts from cohort (52,268 randomly sampled accounts) of Weiboscope database Countries included: China Disease(s) included: Cohort’s posts were searched for COVID‐19‐related keywords and a daily percentage calculated (no. COVID‐related posts/no. total daily posts) Quality assessment: Response rate: + Representativeness: +++ Authors declared no COI; possibility of Internet censorship in China, sample included only one of several social media platforms; paper published (peer reviewed) |
Reported on:
Recommendations:
|
Communication purpose: Might inform decisions about timing of communication of outbreak information to communities and populations, where earlier awareness might promote better engagement with required physical distancing measures. Related to review questions: Findings suggest that lack of outbreak awareness creates missed opportunities for the public to take up preventive and control measures. |
# COVID‐19‐specific, #^ included research not COVID‐19‐specific but review conducted in context of current pandemic outbreak, *non COVID‐19 specific, % AMSTAR rating from McMaster Health Forum (via Health Systems Evidence https://www.healthsystemsevidence.org)
Abbreviations: AGREE II: Appraisal of Guidelines for Research & Evaluation II tool AMSTAR: A Measurement Tool to Assess Systematic Reviews COI: conflict of interest EVD: Ebola Virus Disease GL: guideline H1N1: H1N1 influenza strain HCW: health care worker MERS: Middle East Respiratory Syndrome N/A: not applicable NIHR: National Institute for Health Research NPI: non‐pharmaceutical interventions PD: physical distancing PTSD: Post‐Traumatic Stress Disorder QES: qualitative evidence synthesis SARS: Severe Acute Respiratory Syndrome, SR: systematic review WHO: World Health Organization Table d: School measures
| Public health measure 4: School measures | Study features | Outcomes and findings | Map to |
| Systematic reviews, guidelines | |||
|
Brooks 2020a*^ (SR) Mapping to: Adherence, acceptability, feasibility |
Outcomes and aim: Assessment of effects of unplanned school closures on children’s activities and contacts outside home Inclusion and exclusion criteria: Included: primary, peer‐reviewed research, written in English or Italian; reporting children’s social activities during temporary unplanned school closure Excluded: research on hypothetical/simulation scenarios, or intentions Type of study and data: SR; 19 included studies. 18 cross‐sectional design with questionnaire, 1 qualitative study Disease(s) included: Most (12) reported school closures related to H1N1 pandemic or other influenza/influenza‐like outbreaks (6). Duration of closures was 1‐14 days. Countries included: US (10), Australia (4), 1 each in Argentina, Japan, Russia, Taiwan, UK Quality assessment: 3/11 AMSTAR rating% Funding source: Not reported |
Reported on:
Recommendations: Ensuring parents understand why school closure is important will be a key factor determining the success of the measure in future disease outbreaks. Although most children may not need childcare arrangements (outside home) that might increase disease transmission risk, public health officials should consider how to support parents and to prevent this. Advice from schools should be consistent with public health advice; hosting extracurricular activities/sporting events during a closure sends mixed messages that can be confusing or detrimental. Short closures (up to two weeks) may be manageable by parents but longer closures (e.g. for mitigating pandemic waves) may be more challenging. |
Communication purpose: May be used to inform communication with parents about why school closures and adherence to avoiding social contacts are important. Related to review questions: Despite public health advice, many children have social contact outside the household during school closures. Parents may accept and adhere to school closures if they perceive benefits from the measure. Parents may not accept or adhere to school closures if they do not perceive the measure will decrease infection risk, or they have concerns about practicalities and impact of the closure e.g. on the child’s education, difficulty making childcare arrangements and economic impacts (such as lost income). |
|
CDC 2022# Citation type: GL At: COVID-19 Guidance for Operating Early Care and Education/Child Care Programs (cdc.gov) Public health measure: School measures, and also maps onto work measures Mapping to: Adherence, feasibility Mapping to: Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication Theme 6: distancing measures in schools and workplaces |
Overview and aim: To provide guidance on protecting young children and adults in early childhood education (ECE) settings Type of study and data: Official CDC guidance; periodically updated in line with updated quarantine/isolation advice, community vaccination and other relevant variables. Based on CDC Science Brief Included disease(s): COVID‐19 Timing: None Countries included: USA advice (CDC) High‐income country Intervention or phenomenon of interest: Providing guidance on physical distancing and other layered measures to protect children and adults in ECE settings Quality assessment: AGREE II: scope and purpose 72.2%; stakeholder involvement 30.56%; rigour of development 2.1%; clarity of presentation 69.44%; applicability 27.08%; editorial independence 0% Funding source: Not reported |
Reported on:
Equity in ECE settings:
Physical distancing and cohorting:
Staying home/returning from isolation:
Children with disabilities or other healthcare needs:
ECE staff:
Recommendations: Access to and attendance at ECE programmes is important for children’s learning and social and emotional well‐being. Prevention measures to safely enable children to attend ECE programmes need to be layered, and staff supported and protected, to reduce the risk of transmission and help to maintain open and accessible in‐person ECE services during the pandemic. |
Communication purpose: Guidance indicates the several communication strategies to support implementation of preventive measures in ECE services. Implementation of layered preventive approaches needs to be developed and supported with an understanding of the community’s needs, and with communication to the community about the measures put in place to protect the health of children and staff. Related to review questions: Physical distancing measures may not be possible in all situations in ECE services, therefore a layered approach to protecting health is needed. Families, services and the community need to work together to plan such measures, ensuring that the diverse needs of the community are taken into account, including those for children with disabilities, healthcare concerns, or homelessness, and with a focus on including those disproportionately affected by the pandemic. ECE services should communicate clearly with families and children, and staff, about preventive measures in place, as well as the process for returning to ECE services post‐COVID‐19 illness. ECE staff need to be supported to work during the pandemic, educated and trained in preventive practices and policies, and workload and mental health strain managed proactively. Provision needs to be made, and clearly communicated, for staff who become ill to help ensure that they do not attend work if sick or fear negative repercussions of being absent or homelessness, and with a focus on including those disproportionately affected by the pandemic. ECE services should communicate clearly with families and children, and staff, about preventive measures in place; about monitoring for symptoms and undertaking testing, as well as the process for returning to ECE services post‐COVID‐19 illness. ECE staff need to be supported to work during the pandemic, educated and trained in preventive practices and policies, and workload and mental health strain managed proactively. Provision needs to be made, and clearly communicated, for staff who become ill to help ensure that they do not attend work if sick or fear negative repercussions of being absent. |
|
CDC 2022a# Citation type: GL At: Guidance for COVID-19 Prevention in K-12 child care | CDC Public health measure: School measures, and also maps onto work measures Mapping to: Adherence, feasibility Mapping to: Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication Theme 6: distancing measures in schools and workplaces |
Overview and aim: To provide guidance on protecting students and staff in school settings Type of study and data: Official CDC guidance; periodically updated in line with updated quarantine/isolation advice, community vaccination and other relevant variables. Based on CDC Science Brief Included disease(s): COVID‐19 Timing: None Countries included: USA advice (CDC) High‐income country Intervention or phenomenon of interest: Promoting physical distancing and other layered measures to protect students and adults in school settings Quality assessment: AGREE II: scope and purpose 69.4%; stakeholder involvement 25%; rigour of development 0%; clarity of presentation 69.44%; applicability 45.83%; editorial independence 0% Funding source: Not reported |
Reported on:
Equity in schools:
Physical distancing and cohorting:
Staying home/returning from isolation:
School staff:
Recommendations: Access to in‐person school learning is important for children’s learning and social and emotional well‐being. Prevention measures to safely enable children to attend school need to be layered, and staff supported and protected, to reduce the risk of transmission and help to maintain open and accessible in‐person school learning during the pandemic. |
Communication purpose: Guidance indicates several communication strategies to support implementation of preventive measures in schools. Implementation of layered preventive approaches needs to be developed and supported with an understanding of the community’s needs, and with communication to the school community about the measures put in place to protect the health of students and staff. Related to review questions: Physical distancing measures may not be possible in all situations in schools, therefore a layered approach to protecting health is needed. Families, schools and the community need to work together to plan such measures, ensuring that the diverse needs of the community are taken into account. School teachers and staff need to be supported to work during the pandemic, educated and trained in preventive practices and policies, and workload and mental health strain managed proactively. Provision needs to be made, and clearly communicated, for staff who become ill to help ensure that they do not attend work if sick or fear negative repercussions if absent due to illness. |
|
CDC 2022b# Citation type: GL Guidance for Institutions of Higher Education (IHEs) | CDC Public health measure: School measures, and also maps onto work measures Mapping to: Adherence, feasibility Mapping to: Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication Theme 6: distancing measures in schools and workplaces |
Overview and aim: To provide guidance on protecting students and staff in higher education settings Type of study and data:Official CDC guidance; periodically updated in line with updated quarantine/isolation advice, community vaccination and other relevant variables. Based on CDC Science Brief Included disease(s): COVID‐19 Timing: None Countries included: USA advice (CDC) High‐income country Intervention or phenomenon of interest: Promoting physical distancing and other layered preventive measures to protect students and staff in higher education settings Quality assessment: AGREE II: scope and purpose 77.8%; stakeholder involvement 33.33%; rigour of development 17.7%; clarity of presentation 69.44%; applicability 27.08%; editorial independence 0% Funding source: Not reported |
Reported on:
Communicating prevention strategies:
Health equity:
People with disabilities:
Recommendations: Equal access to in‐person higher education is important for learning and social and emotional well‐being. Prevention measures to safely enable higher educational attendance, need to be layered, and the measures communicated clearly to the entire IHE community, to reduce the risk of transmission and help to maintain open and accessible in‐person education during the pandemic. |
Communication purpose: Guidance indicates several communication strategies to support implementation of preventive measures in within higher educational settings. Implementation of layered preventive approaches needs to be developed and supported with an understanding of the community’s needs, and with communication to the school community about the measures put in place to protect the health of students and staff, and to ensure equitable access to in‐person learning. Related to review questions: Physical distancing is one of a suite of measures to be implemented in a layered way in IHEs. IHEs should engage with the local community to plan preventive measures, ensuring that the diverse needs of the community are taken into account and the equitable access is promoted. Students and staff need to be trained and supported to attend IHEs during the pandemic, including providing clear communication and education on preventive practices and policies. Provision needs to be made, and clearly communicated, for staff who become ill to help ensure that they do not attend work if sick or fear negative repercussions if absent due to illness. |
|
DES 2020# Citation type: GL The Department of Education and Skills (Ireland) (2020). Reopening Our Schools ‐ The Roadmap for the Full Return to School Public health measure: School measures Mapping to: Adherence feasibility Mapping to: Theme 3: support for individual and population behavioural changes Theme 6: distancing measures in schools and workplaces |
Overview and aim: Outlines the public health advice and implications of school reopening, including specific measures to be implemented at different levels. Plans include those for effective communications to ensure that all stakeholders have access to clear, relevant and timely information to support reopening and sustained school opening. Type of study and data: GL: contributing evidence is not reported. Included disease(s): COVID‐19 Timing: Predominantly targeted at preparing for schools to reopen (August 2020), but also with explicit recognition that remote learning may be required at later stages of the pandemic and of the need for schools to be prepared for this possibility Countries included: Ireland; high income Intervention or phenomenon of interest: Communication to support school reopening and the maintenance of open schools over time (focus of data extraction) Quality assessment: AGREE II: scope and purpose 58.3%; stakeholder involvement 16.67%; rigour of development 4.2%; clarity of presentation 83.33%; applicability 62.5%; editorial independence 0% Funding source: Not reported |
Reported on:
Ongoing communication arrangements: Communications aim to ensure that schools, communities and all stakeholders have access to clear, timely and relevant information to support reopening and continued operation of schools. Continuing stakeholder engagement:
Providing support for schools: The Education Department is providing materials to support school planning for reopening and communication with school communities in advance of reopening, including:
Supporting students, parents and school communities: Providing materials to schools for distribution (augmented by Department communications via digital channels) to returning students and families ahead of reopening, including:
Direct communication channels for schools: Several direct communication channels will be available to directly support schools as they reopen, including:
In recognition of the range of responses possible from the school community upon reopening, well‐being is to be a major focus; specific supports to be made available to students including vulnerable groups, those experiencing bereavement. A significant shift is required behaviourally, with all members of the community playing their part to keep everyone safe e.g. those with symptoms to stay home, respecting physical distancing practices and minimising social contacts. Extensive communication by schools with their communities is required to support this shift ‐ which requires not only achieving physical distancing minimum standards but supporting re‐engagement of students in learning and social activities; students will need support from families, teachers and school staff to make this transition successfully. Key public health advice messages will need to be communicated and reinforced throughout the community, including being aware of what to do to protect themselves and others, continuing to observe physical distancing and other measures. Recommendations: School reopening and remaining open requires students, families, teachers and staff to have high awareness of and adherence to preventive measures such as physical distancing. Extensive communication and support are needed to support this transition and to ensure that schools are able to remain open once students return to face‐to‐face learning. |
Communication purpose: Clear, proactive communication from schools to their communities is needed as part of the preparation to re‐open. Support for students, and for teachers and staff is also indicated, particularly for those at particular disadvantage or at higher risk of severe disease. Engagement of stakeholders, providing clear information to different groups within school communities, and ensuring ongoing two‐way communication and support mechanisms are in place, flexible, and adapted as circumstances change will be essential for ongoing management of school settings during the pandemic. Related to review questions: Promoting clear and comprehensive communication between schools and their communities will be essential as schools reopen, to help to ensure high levels of awareness and adherence to required measures to prevent COVID‐19 transmission, and to help support children, teachers, staff and families as they undertake this transition. |
*Non‐COVID‐19‐specific study; % AMSTAR rating from McMaster Health Forum (via Health Systems Evidence https://www.healthsystemsevidence.org) Abbreviations: AGREE II: Appraisal of Guidelines for Research & Evaluation II tool CDC: Centres for Disease Control and Prevention ECE: early care and education GL: guideline H1N1: Influenza A virus subtype IHE: institute of higher education PH: public health SR: systematic review
Table e: Workplace measures
| Public health measure 5: Workplace measures | Study features | Outcomes and findings | Translational steps |
| No studies were identified that focused on workplace measures only (several studies mapped also to other physical distancing measures included workplace measures). | |||
Table f: Crowd avoidance, including individual physical distancing measures
| Public health measure 6: Crowd avoidance | Study features | Outcomes and findings | Translational steps |
| Systematic reviews, guidelines | |||
|
ECDC 2020# At: Risk of COVID-19 transmission related to the end-of-year festive season (europa.eu) Citation type: GL Public health measure: Crowd avoidance, and also maps onto general PD Mapping to: Uptake, acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity Theme 5: public trust and perceptions |
Overview and aim: To assess the risk of COVID‐19 transmission to the general population and medically vulnerable people, in the period leading up to Christmas; and to provide guidance on mitigation measures and on risk communication activities to support these measures. Type of study and data: GL, rapid risk assessment based on ECDC methodology Included disease(s): COVID‐19 Timing: Pre‐Christmas festive season 2020 (4 December 2020); guidance developed in preparation for the festive season, with background risk of COVID‐19 in the community at high levels and prior to the availability of vaccination against COVID‐19 Countries included: Advice for countries in the EU/EEA and UK. Predominantly high‐income Intervention or phenomenon of interest: Communication of risk and mitigation measures leading up to festive season Quality assessment: AGREE II: scope and purpose 61.1%; stakeholder involvement 22.22%; rigour of development 11.5%; clarity of presentation 55.56%; applicability 2.08%; editorial independence 0% Funding source: Not reported; this report was written with the co‐ordination and assistance of an Internal Response Team at the European Centre for Disease Prevention and Control. |
Reported on:
Risk communication: addressing pandemic fatigue:
Risk communication principles to be considered include the following:
Measures for public health protection should be applied and layered irrespective of underlying level of community transmission, and in all settings i.e. ensuring physical distance, hand and respiratory hygiene, use of masks, and ensuring sufficient ventilation; cancelling or limiting the size and length of social events, offering online alternatives, and within‐household only gatherings, creating and maintain small social bubbles, self‐quarantine, and shielding medically and socially‐vulnerable people may all help to reduce risk. Authorities should implement strategies to protect people who are medically or socially vulnerable; particularly those in long‐term care facilities and others living in confined spaces (e.g. prisons, migrant camps). Strategies might include helping people to avoid crowds and providing support for infection prevention and control, practical and mental support, while accounting for people’s need for social interactions. Social bubbles and/or self‐quarantine before gatherings with vulnerable people is also advisable. Authorities should communicate the above measures and precautions to the public, so that people are encouraged to reduce travel and social activities; take extra precautions before gatherings (e.g. self‐quarantine); and consider alternatives to those traditionally practised (e.g. creating social bubbles, moving gatherings online). Authorities should also communicate to the public that they might consider the potential consequences of infecting others or sparking a chain of transmission that could lead to severe illness or death. Recommendations: Authorities need to work to balance the epidemiological risk of disease transmission against the relaxation of public health measures; and to communicate effectively with the public to convey information about measures to mitigate risk in situations where measures are temporarily relaxed. |
Communication purpose: Guidance may inform public health communication strategies in situations where public health measures are changing or there is anticipated change in future. Provision of clear, accessible and transparent information about measures, supported by concrete goals and epidemiological targets to directly address pandemic fatigue, which has the potential to undermine the effectiveness of public health measures Related to review questions: Clear communication and community engagement are key to providing guidance to the community about which measures apply, when, and how to protect themselves and others by mitigating the risk of disease transmission. This may be particularly important as public health restrictions change and people still need to minimise transmission risks to themselves and to vulnerable members of the community. Addressing pandemic fatigue through effective risk communication is essential, as lack of adherence to measures may increase transmission and undermine effectiveness of public health measures. |
|
NACCHO 2006*+ Mapping to: Adherence, acceptability |
Overview and aim: Assistance for local health departments writing new, or improving existing, local pandemic influenza plans by identifying common elements Intervention or phenomenon of interest: We focus here on guidance related to communication targeting community dwelling general public about physical distancing to limit viral transmission. Inclusion and exclusion criteria: Included: numerous local level Health Department pandemic flu plans reviewed by NACCHO to develop the guide Countries included: USA Quality assessment: (AGREE II) ⁱ: Scope and purpose: 100% Stakeholder involvement: 67% Rigour of development: 44% Clarity of presentation: 94% Applicability: 33% Editorial independence: 25% Funding source: This product was funded through the “Linking Centers for Excellence and Public Health Departments” Cooperative Agreement between the Centers for Disease Control and Prevention and the National Association of County and City Health Officials (# U50 /CCU 302718). |
Reported on:
Phases 4 and 5 (pandemic alert period with increasing clusters of cases):
Phase 6 (pandemic period, increased and sustained transmission):
Recommendations: Consider the following issues when planning for and responding to pandemic: How the necessity of isolation/quarantine should be communicated, and what advice will be given. How to urgently convey the importance of staying at home (unless requiring medical care); where to direct people to get usual medical care (if unavailable through usual routes). How to ensure consistent information and messages, and to address misinformation that may arise. How to reach groups not reached through traditional communication channels (e.g. other channels, involvement of other groups such as community groups). How to ensure translated information is available (e.g. could information prepared in advance be translated in advance). |
Communication purpose: These guidelines may be useful for enabling communication; and supporting behaviour change in pandemic influenza planning that focuses on public education and risk communication related to limiting the spread of the disease. Related to review questions: Findings indicate the critical role of public information and risk communication in a pandemic outbreak. Consideration of these information requirements should inform communication planning prior to an outbreak and be updated throughout. |
|
PHAC 2021 Public Health Agency of Canada (PHAC) 2021 Individual and community‐based measures to mitigate the spread of COVID‐19 in Canada At: Individual and community-based measures to mitigate the spread of COVID-19 in Canada - Canada.ca Citation type: GL Public health measure: Crowd avoidance, and also maps onto general PD Mapping to: Uptake, acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: Identification of non‐pharmaceutical PH measures to mitigate COVID‐19 transmission risks for individuals and communities, considering a range of settings and issues specific to different groups within communities Type of study and data: Guideline; the best available evidence and expert opinion; included rapid evidence reviews, policy advice from PH agencies (WHO, CDC), economic advice and research Included disease(s): COVID‐19 Timing: Guideline to be interpreted in the context of changes in timing and intensity of COVID‐19 activity across jurisdictions, and local adaptations to legislation, regulations and policies Countries included: Canadian context; some included evidence from Canadian agencies, others from international or national sources (e.g. WHO, UNICEF, ECDC, CDC, SAGE UK) High‐income countries well represented; but within these, disadvantaged and/or remote groups considered Intervention or phenomenon of interest: PH measures to mitigate transmission risk in a range of settings and population groups Quality assessment: AGREE II: scope and purpose 83.3%; stakeholder involvement 30.56%; rigour of development 19.8%; clarity of presentation 63.89%; applicability 25.0%; editorial independence 0% Funding source: Not reported |
Reported on: Several factors influence adherence to PH measures, including contextual (e.g. living, working, community conditions), social and financial circumstances, and cultural and spiritual factors. These may also influence whether individuals can adopt measures and sustain adherence over time. Duration of the pandemic and pandemic fatigue due to sustained efforts also impact adherence. To promote adherence, public education and communication strategies should be tailored to a range of factors including age, sex and gender, ability status, caregiving responsibilities and other SES/identity factors. Communication and public education:
Specific communication considerations for physical distancing measures for mitigating risk:
Communication for remote/isolated communities:
Communication for community congregate living facilities (e.g. shelters for homeless people, industrial camps, group homes for people with disabilities):
Communication for public transport:
Recommendations: Public health communication and information provision are a critical part of the emergency response and help to support awareness and enactment of preventive measures over time. |
Communication purpose: May inform development of more effective and appropriate communications around PH measures, including physical distancing measures Related to review questions: Describes measures to tailor and improve communication to support preventive measures. Identifies several factors and contextual features that might influence PH messaging; and which might be deliberately considered when communicating with communities and regions. Improving such communication may promote better acceptability, uptake and adherence to required physical distancing measures. Provides recommendations for improved communication about mitigation strategies (including PD) for vulnerable/isolated communities and in certain settings (e.g. on public transport). |
|
PHAC 2021a# At: COVID-19: Advice for gatherings, events and celebrations - Canada.ca December 2021 version Citation type: GL Public health measure: Crowd avoidance, and also maps onto general PD Mapping to: Acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery |
Overview and aim: To provide guidance for individuals planning private indoor gatherings in the context of community transmission of COVID‐19 Type of study and data: Guidance from national agency Included disease(s): COVID‐19 Timing: Nonspecific Countries included: Advice for Canada High‐income Intervention or phenomenon of interest: Communication and informed decision‐making in the context of social gatherings Quality assessment: AGREE II: scope and purpose 44.4%; stakeholder involvement 11.11%; rigour of development 2.1%; clarity of presentation 61.11%; applicability 0%; editorial independence 0% Funding source: Not reported |
Reported on:
Recommendations: People considering hosting or attending gatherings need to be aware of the risks of contracting COVID. People hosting gatherings have a responsibility to communicate with guests ahead of time what measures will be in place to help to minimise risks, so that they can make informed decisions about whether to attend. |
Communication purpose: Inform individuals who are hosting gatherings about the role of communication/information provision in relation to COVD risk and protective measures, as well as the responsibility of those attending gatherings to assess risk and to be informed of the required public health measures in place. Related to review questions: Indicates the need for a joint effort from all to maintain safety during gatherings i.e. to be up‐to‐date with the latest public health advice regarding risk and protective measures, and to consistently follow the recommendations. Those hosting gatherings have a role to play in communicating in advance about the measures that will be in place to improve safety, but responsibility for maintaining public health measures during gatherings falls to all involved. |
|
Teasdale 2014* (SR) Mapping to: Acceptability, uptake, adherence, feasibility Also relevant to public health measures 3 (quarantine), 4 (school) and 5 (workplace measures) |
Overview and aim: Exploration of public perceptions of non‐pharmaceutical interventions aiming to reduce the transmission of acute respiratory infections Inclusion and exclusion criteria: Included: qualitative or mixed‐methods studies (if having a substantial qualitative component) assessing adult (17 years or older) public (general public or patients) beliefs and perceptions of NPIs for acute respiratory infections and/or interventions that aimed to promote non‐pharmaceutical respiratory infection control Excluded: studies of health professionals or children Type of study and data: Qualitative systematic review. 16 included studies, total participants 1022; most (12) assessed general public, (2 focused on ethnic groups, 2 on people with chronic conditions). Most (10) studies focused on actual respiratory infection outbreak/pandemic (SARS and H1N1 2009 pandemic). 9/16 studies included physical distancing as an element of NPI. Included studies generally examined multiple NPIs or NPIs in combination with pharmaceutical measures. Countries included: UK (6), USA (4), one study each in Canada, Australia, Hong Kong, Bangladesh, New Zealand, Spain Quality assessment: 6/11 AMSTAR rating Funding source: This research was undertaken as part of doctoral research funded by the National Institute for Health Research (NIHR) School for Primary Care Research (SPCR). |
Reported on: Focus here is on findings related to physical distancing measures
Perceived vulnerability to respiratory infection
Anxiety about emerging respiratory infections
Communications about emerging respiratory infections
Recommendations: NPI measure adoption is likely to be improved by addressing common public beliefs and concerns about the necessity, effectiveness, acceptability and feasibility of the measures, and by addressing key barriers such as personal vulnerability to emerging infections, rejection of personal risk and concerns about possible costs and stigma associated with some NPIs. Enabling people to associate NPIs with a positive identity rather than a negative or vulnerable identity e.g. positive framing of advice messages around maintaining well‐being rather than avoiding infection might improve the perceived relevance of non‐pharmaceutical respiratory infection control to those who do not acknowledge that they could be at risk of infection. |
Communication purpose: Findings may inform communication with communities to improve the acceptability, feasibility, and uptake of physical distancing, and to support behaviour change required for these measures. Related to review questions: People’s views and perceptions of physical distancing may impact their acceptance, uptake and adherence. Messages should be framed positively where possible to reduce stigma and encourage adherence. Communication should also target people’s perceptions that only ‘others’ are at risk, and therefore they do not need to comply and aim to also address other barriers such as costs. |
|
Tooher 2013* (SR) Mapping to: Uptake, adherence Also relevant to public health measures 3 (quarantine), 2 (isolation) and 5 (workplace measures) |
Overview and aim: Assessment of behavioural responses to H1N1 pandemic (including adoption of non‐pharmaceutical mitigation measures) and association with community knowledge levels, perceived severity, and level of concern Inclusion and exclusion criteria: Included: Community response to pandemic assessed by surveys during or after 2009 H1N1 pandemic Excluded: Studies of population subgroups, other respiratory diseases, mathematical modelling, qualitative studies Type of study and data: SR; 19 included studies. Cross‐sectional or repeated population surveys Countries included: Australia (n = 5), the US (n = 4), the UK (n = 1), Hong Kong (n = 2), Saudi Arabia (n = 1), China (n = 1) and Mexico (n = 1), and several European countries (n = 5) Quality assessment: 8/11 AMSTAR rating Funding source: This work was supported by the National Health and Medical Research Council [Grant Number 626867]. Author HM is supported by an NHMRC Career Development Fellowship No. 1016272 |
Reported on: Pandemic knowledge
Levels of concern and risk perception
Pandemic behaviours
Recommendations:
|
Communication purpose: May inform communication with communities about pandemic health threats and the importance of behavioural mitigation measures, including to populations less likely to take up those measures, such as younger people and those with lower education. It may also inform policymakers about communication strategies to enhance knowledge about prevention methods and perceived risk, to maximise behavioural uptake of required measures. Related to review questions: Findings link knowledge and perceived risk levels to behavioural change and may provide insight into improving acceptability and uptake of physical distancing measures such as staying away from work with symptoms. |
|
WHO 2020b# At: Public health considerations for elections and related activities in the context of the COVID-19 pandemic (who.int) December 2020 Citation type: GL Public health measure: Crowd avoidance, and also maps onto general PD Mapping to: Acceptability, feasibility Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 4: community engagement to support communication |
Overview and aim: To provide guidance on measures to minimise COVID‐19 transmission in relation to in‐person electoral and related activities Type of study and data: Guidance (across‐country) Included disease(s): COVID‐19 Timing: Nonspecific Countries included: WHO; international Intervention or phenomenon of interest: Communication to support PHSMs to mitigate risk associated with elections and related activities Quality assessment: AGREE II: scope and purpose 72.2%; stakeholder involvement 36.11%; rigour of development 10.40%; clarity of presentation 83.33%; applicability 39.58%; editorial independence 0% Funding source: Not reported; this document was developed by the WHO Health Emergencies Programme in consultation with WHO Regional Offices, the WHO Office at the United Nations, other WHO Offices and external experts. |
Reported on:
Risk communication: Public communication is needed to promote acceptance of changes required to promote safety and to address rumours, misinformation and concerns about the transmission of COVID‐19. Such communication should be in place before, during and after voting, and should aim to convey the following key messages:
Factors enabling precautionary measures to be implemented include facilitated dialogue between stakeholders involved in the safety of activities; co‐ordination between electoral authorities and those responsible for health and safety planning in the context of COVID‐19; alignment between electoral precautionary measures and local/national COVID‐19 policies; information on precautionary measures, and training in their application, for electoral and related staff; supervision and feedback on precautionary measures during activities. Precautionary measures to be planned and put in place for elections should consider not only the voting process but also the full range of related activities (e.g. meetings, workshops, electoral campaigns, rallies, voter registration, vote counting, gatherings for announcement of results). Recommendations: Elections and related activities require planning and implementation of a range of precautionary measures to minimise risk of COVID‐19, as well as communication with the public about these risks and measures taken to mitigate risk. |
Communication purpose: Findings may inform public communications in preparation for, pre, during and post‐election activities; and assist with informing individuals and communities of the risks, measures in place to mitigate risks, and to address misinformation directly. Related to review questions: Communication to the public about COVID‐19 risk mitigation measures for electoral activities should include clear information about risk and measures implemented; help to support implementation of the measures, as well as adaptation of these to vulnerable groups within the population; and address misinformation about the mechanisms in place. Measures to mitigate risks, and to communicate with the public about both the risks and the measures need to be planned ahead of time and communication should occur regularly throughout and after the election process and associated activities. |
| Scoping review, qualitative analysis | |||
|
Eaton 2020*^ (scoping review) Mapping to: uptake, acceptability, adherence; also people’s views and experiences |
Overview and aim: To outline broad, scoping lessons learned from the HIV epidemic tailored to the nature of what is currently known about COVID‐19 using the Social Ecological Model of Health as a unifying framework Inclusion and exclusion criteria: Included: Study types not stated. No method to indicate inclusion/exclusion of study types Type of study and data: Review: scoping (no review method included) Countries included: Not explicit (no method), but there are studies in the paper from South Africa, USA, Bulgaria, Thailand, “Africa”. Likely other countries represented, but these were the countries/regions that could be identified in the body or reference list of the paper Quality assessment: AMSTAR 0/11% (no method provided, non‐systematic) |
Reported on:
Recommendations: Sustained changes to behaviour, particularly over long periods of time, require multi‐level approaches (not just interventions targeted at the individual) and regular communication/reiteration of messages over time. Approaches to addressing stigma and disadvantage in the context of promoting well‐being and preventing disease already exist and are likely relevant to COVID‐19. |
Communication purpose: Findings may inform the development of communication around public health measures (including physical distancing) beyond behaviour change messages targeted at the individual and/or may help communicators consider wider societal factors which influence individual behaviour change. Related to review questions: Factors outside individual control (often socioeconomic) influence ability to take up or adhere to public health recommendations around physical distancing. Acceptance of communication may be negatively influenced by anti‐science communication or conspiracy thinking. Communication which seeks to shift social norms is more likely to result in uptake of and adherence to public health measures than communications aiming for individual behaviour change. |
|
Lor 2016* (qualitative analysis of meeting reports) Mapping to: Adherence, also feasibility/barriers Also maps to public health measures, 3 (quarantine) and 2 (isolation) |
Overview and aim: Identification of cultural perspectives that may shape thinking about ethical considerations relevant to pandemic influenza preparedness and response Inclusion and exclusion criteria: Included: 168 health professionals, scientists, academics, ethicists, religious leaders, and other community members representing 40 countries (attended the meeting) Type of study and data: Analysis of four regional meetings funded by the Centre for Disease Control and Prevention (CDC). Qualitative thematic analysis of meeting reports, notes, and stories Countries included: 40 countries from Africa, Asia, Latin America, and the Eastern Mediterranean region Quality assessment: 6/10 CASP score (potential bias not discussed; no mention of ethics approval/consent; data analysis methods unclear) |
Reported on: Outcomes mapped to key ethical challenges for pandemic influenza response described in WHO guidance ‘Ethical Considerations in Developing a Public Health Response to Pandemic Influenza’:
Recommendations: Decision‐makers must consider the importance of procedural ethics, especially transparency and inclusiveness when planning pandemic response. Decision‐makers should consider that procedural ethics can play an important role in bringing people and countries together to respond to the shared health threat posed by a pandemic influenza despite existing cultural differences. |
Communication purpose: Findings may guide communication and promote inclusiveness and public engagement in order to develop culturally appropriate messages, for instance, in relation to physical distancing measures. This may also inform communication with and support of health staff facing competing obligations during a pandemic. Related to review questions: Findings identify cultural factors influencing behavioural adherence to public health measures and indicate that communication regarding such measures requires tailoring to cultural and contextual factors. |
| Primary studies | |||
|
Atchison 2020# (primary) Mapping to: Uptake, adherence; also feasibility Also relevant to public health measure, 2 (isolation) |
Overview and aim: Perceptions and behavioural responses to COVID‐19 Inclusion and exclusion criteria: Included: adults aged 18 years and over, within 48 hours of government advice to stop non‐essential contacts and to cease unnecessary travel Type of study and data: Cross‐sectional survey; 2108 participants (representative of UK population) Descriptive statistics for all survey measures Included disease(s): COVID‐19 outbreak Quality assessment: Response rate: ++ Representativeness: ++ COI declared and reported no conflicts; results rely on self‐reported data; those without Internet under‐represented; pre‐print (not peer reviewed). |
Reported on:
Recommendations: Ability to take up and comply with certain NPI measures is lowest in lowest socioeconomic groups (self‐isolation, working from home). Social and economic policies should mitigate this. Factors affecting uptake/compliance with preventive measures are critical. Those from lower‐income backgrounds in particular may need financial assurance and assistance to be able to implement some protective measures. |
Communication purpose: Findings may inform strategies to communicate with and support behaviour change within the community, focusing on groups who may be less likely to practice measures such as crowd avoidance, and those with fewer socioeconomic resources to enact behaviour change required to prevent transmission. Related to review questions: Findings suggest that even where willingness to comply with physical distancing measures is high, those with lower household incomes may lack the practical and financial resources to do so and this may affect uptake and adherence to physical distancing measures. |
|
Briscese 2020# (primary) Mapping to: adherence, acceptability Also relevant for isolation/quarantine |
Overview and aim: Intentions to comply with self‐isolation measures, and assessment of effects of duration of restrictions on people’s intended compliance Inclusion and exclusion criteria: Included: adults, representative sample of national population (drawn from market research company database of 60,000 individuals) Type of study and data: Survey; 894 participants (representative of Italian population) Descriptive statistics for all survey measures Time: Survey period March 18‐20, 2020 [in the context of national lockdown period, declared March 9th until April 3rd 2020] Countries included: Italy Quality assessment: Response rate: + Representativeness: +++ COI not declared; results rely on self‐reported compliance data; paper unpublished (working paper) |
Reported on:
Recommendations: People’s intended compliance with self‐isolation measures is influenced by the communicated duration of measures and the match or mismatch with people’s own expectations of such measures. Public health authorities need to consider these findings and find approaches to manage population expectations in cases such as the current COVID‐19 pandemic where self‐isolation measures may be prolonged and/or extended beyond initially proposed time frames. |
Communication purpose: This may be useful for planning communications with populations and communities about restrictions and required self‐isolation measures. Related to review questions: Results indicate that most people intend to maintain current self‐isolation behaviours in the context of shifting endpoints for restrictions (irrespective of their own expectations). However, restrictions being extended beyond what people expected led to fewer intending to increase compliance and more intending to decrease compliance with self‐isolation measures. This suggests that public health messages related to self‐isolation measures need to consider expectations, particularly in cases such as the current pandemic where timelines are uncertain, and restrictions may be extended. |
|
Clements 2020# (primary) Mapping to: Adherence |
Overview and aim: Assessment of COVID‐19 knowledge and influence on behaviours, including crowd avoidance Inclusion and exclusion criteria: Included: adults 18 years and older, recruited through Amazon Mechanical Turk Type of study and data: Cross‐sectional survey; 1034 participants (of 1070 respondents). Descriptive statistics for all survey measures Time: Survey conducted March 17, 2020; based on survey by Zhong 2020. Assessed approximately 8 weeks after 1st case diagnosed in the USA Countries included: USA Quality assessment: Response rate: + Representativeness: + Authors report no COI; > 60% had bachelor degree or higher education, other groups may be under‐represented; pre‐print (not peer‐reviewed) |
Reported on:
Recommendations: Knowledge of COVID‐19 is influenced by several factors, and in turn affects compliance with recommendations such as crowd avoidance. Addressing knowledge differences will be necessary to promote behavioural compliance with preventive recommendations and may require a nationally coordinated pandemic response. |
Communication purpose: May be useful for planning communication to improve knowledge of populations and associated risk behaviours. Related to review questions: Findings suggest that knowledge is associated with several factors and may influence compliance to recommended measures such as crowd avoidance. |
|
Kwok 2020# (primary) Mapping to: Uptake |
Overview and aim: Assessment of psychological and behavioural responses in early phase of COVID‐19 outbreak, include perceived effectiveness and adoption of preventive measures (including social distancing measures) Inclusion and exclusion criteria: Included: adults (18 years and older), understood Chinese and lived 5 days/week in Hong Kong within last month; recruited via District Councilors for all 452 areas Type of study and data: Cross‐sectional survey; 1715 participants Descriptive statistics for all survey measures Time: Within 36 hours first confirmed COVID‐19 cases (January 24 to February 13, 2020) Quality assessment: Response rate + Representativeness ++ No COI statement: respondents were working age and majority female, older people and those without Internet access may be under‐represented; pre‐print (not peer reviewed) |
Reported on:
Recommendations: Since those with good knowledge of COVID‐19 may be more likely to adopt preventive measures, promoting community knowledge may assist with uptake. Decisions about how to communicate information on COVID‐19 and preventive measures might be guided by information sources trusted and most commonly used. Public health officials should collaborate with the associations of medical doctors (doctors being the most trusted source of information) to share official information in more social communication channels. |
Communication purpose: Findings may be useful for planning communication with communities, particularly in deciding how to provide information more readily from trusted sources. Related to review questions: Findings suggest that knowledge and anxiety may affect adoption of physical distancing and other preventive measures and indicate that risk communication strategies to convey information about COVID‐19 and preventive measures might be informed by consideration of how trustworthy different sources are, as well as their usage. |
|
Lohiniva 2020# (primary) Mapping to: acceptability, uptake, adherence |
Overview and aim: Analysis of risk perceptions and trust in public authorities to inform risk communication efforts related to COVID‐19 Inclusion and exclusion criteria: Included: members of the public requesting information from the Finnish Institute for Health and Welfare (THL) or commenting on COVID‐19 via THL’s email or social media Type of study and data: Qualitative study Thematic analysis of emails and social media posts (n = 116) from the public Time: 3 to 25 February 2020 Countries included: Finland Quality assessment: 7/10 CASP score (Sample may not reflect full range of risk perceptions; no referral to researcher/participant relationship; ethics approval not reported) |
Reported on: Public’s risk perceptions related to the domains:
Catastrophic potential:
Probability of death:
Reasons for exposure for COVID‐19:
Controllability beliefs:
Trust in authorities:
Recommendations: Risk communication should:
|
Communication purpose: May inform risk communication efforts and identify effective features to consider in order to effectively convey information about COVID‐19 to the community. Related to review questions: The content and delivery of information to the community about COVID‐19 should account for people’s perceptions of risks related to COVID. Lack of trust in government messages, and lack of belief in the individual’s ability to control spread in particular may negatively impact acceptance, uptake and adherence to physical distancing measures and may represent targets for risk communication efforts. |
|
Lunn 2020# (primary) Mapping to: Uptake |
Overview and aim: Examines the effect of two communication interventions focusing on different COVID‐19 messaging Inclusion and exclusion criteria: Included: broadly nationally representative participants recruited by a market research agency Type of study and data: Randomised controlled trial; 3 arms Control: standard information poster Intervention 1: ‘identifiable person’ poster (highlighting risk to vulnerable people e.g. older people) Intervention 2: ‘transmission rate’ poster (highlighting exponential infection rate and risk of transmission to large numbers of people) Outcomes measured were cautious intentions to engage in ‘marginal’ physical distancing behaviours (behaviours that some individuals deem acceptable, and others do not) and attitudes towards acceptability of ‘marginal’ physical distancing behaviours of others. ‘Marginal’ behaviours were identified through focus groups (e.g. own intention to visit others in their home, meet others outside; and attitude towards others e.g. allowing children to play outdoors with others). Countries included: Ireland 500 participants, 15‐minute online study (received €5 incentive for completing) Quality assessment: 6/10 CASP tool (no detail about randomisation, allocation concealment; no details on participants completing study; confounding of interventions effects possible; not all relevant outcomes considered (but note, rapid trial). Not peer‐reviewed) |
Reported on:
Recommendations: The mismatch between participants’ judgements about the memorability and persuasive effect of the intervention posters and their actual effect on attitude or intention suggest that even though participants do not like intervention posters, they were nonetheless effective, potentially because they evoke an emotional response. Combined, intervention posters had a significant effect on intention and attitude (increasing participants’ caution about marginal behaviours) compared to the control. Both the ‘identifiable persons’ poster alone and the ‘transmission rate’ poster alone led to participants judging the marginal physical distancing behaviours of others to be less acceptable than control participants. Communications aiming not only to inform people about recommended behaviours but to also emphasise the impact of non‐compliance with recommended measures on identifiable people and numbers of infections may motivate physical distancing. |
Communication purpose: Findings may be useful for enabling more effective communication and supporting behaviour change in relation to changing people’s attitudes and intentions towards reducing the risk of infection to themselves or others in the community. Related to review questions: Communication strategies that emphasise the likelihood of infecting vulnerable people or large numbers of people can help to motivate physical distancing by increasing people’s intention to be cautious in own physical distancing behaviours and change their attitudes to be less accepting of marginal physical distancing behaviours in others. |
|
Meier 2020# (primary) Mapping to: Acceptability, uptake |
Overview and aim: Assessment of public belief in protective measures’ effectiveness, uptake of measures in daily life and sources (communication channels) used to obtain relevant information on COVID‐19 Inclusion and exclusion criteria: Included: adults, countries with > 500 respondents Type of study and data: Cross‐sectional survey (adapted from validated Flu TEST survey template); 9796 respondents Descriptive statistics for all survey measures Countries included: The Netherlands (88%), Germany, Italy, other countries. The Netherlands and Germany classified as Stage III restrictions (community‐wide measures to increase social distance) and Italy Stage IV (widespread community quarantine including cordon sanitaire) at the time of the survey Quality assessment: Response rate: + Representativeness: ++ All authors but one (not lead) declared no COI; digital online survey and recruitment may introduce selection bias; pre‐print (not peer‐reviewed) |
Reported on:
Recommendations: Public belief in effectiveness, and their response to (implementation of) prescribed protective measures (physical distancing), during the survey period (March 2020) were high. Respondents were adequately informed, through different communication channels but most often relied on traditional information sources. |
Communication purpose: Findings may guide information dissemination strategies underpinning physical distancing measures for communities and may inform choice of information dissemination routes to support individuals’ decision‐making in relation to protective behaviours. Related to review questions: Findings indicate that high levels of perceived effectiveness and feeling adequately informed about required measures co‐occurred with strong uptake of physical distancing and other measures to protect against COVID‐19 infection. |
|
Roy 2020# (primary) Mapping to: Acceptability, feasibility and other factors |
Overview and aim: Assessment of knowledge, attitudes, anxiety, and perceived mental healthcare needs during the COVID‐19 pandemic Inclusion and exclusion criteria: Included: adults (18 years and older), able to understand English and to give informed consent, and with Internet access Type of study and data: Cross‐sectional survey; 662 respondents. Descriptive statistics for all survey measures Countries included: India Quality assessment: Response rate: + Representativeness: + Authors reported no COI; respondents limited to English speakers with Internet access, educated (half health professionals), snowball recruitment; paper published |
Reported on:
Recommendations: Knowledge and attitudes influence degree of adherence to protective measures. Accuracy of knowledge about COVID‐19 was variable but willingness to follow physical distancing and quarantine measures were high amongst respondents, as were measures of anxiety. Mental healthcare needs appear high and need to be addressed as part of the current pandemic and public awareness enhanced. Sensible media reporting during the current pandemic may be beneficial in mitigating and tackling mental health challenges. |
Communication purpose: Findings may be used to prioritise strategies for improving knowledge in communities, and for supporting people experiencing particularly high levels of anxiety. Related to review questions: Willingness to comply with required physical distancing measures was high, despite variable knowledge levels about COVID‐19, and anxiety associated with the pandemic may represent an unmet need. |
|
Zhong 2020# (primary) Mapping to: Adherence |
Overview and aim: Investigation of knowledge, attitudes and practices towards COVID‐19 during the rapid rise period of the outbreak Inclusion and exclusion criteria: Included: Chinese nationality, aged 16 years or over, able to understand the content of the recruitment poster, agreed to participate in the study Excluded: history of infection with COVID‐19 Type of study and data: Online self‐report survey conducted from Jan 27–Feb 1, 2020. Convenience sampling, recruitment through social media channels of the authors, and websites/social media accounts of media outlets in the Hubei province. 6910 participants in final sample (6919 recruited, 9 excluded for having been infected with COVID‐19) Countries included: China Quality assessment: Response rate: + Representativeness: + Authors declared no COI; women, well‐educated people and those involved in ‘mental labour’ occupations (associated with higher knowledge, attitudes and practices) over‐represented in sample; paper published (peer‐reviewed) |
Reported on:
Recommendations: The findings around demographic groups who are more likely to be non‐adherent to prevention measures can help public health policymakers and health workers to recognise target populations for COVID‐19 prevention and health education. Public health education measures may be more effective if they target demographic groups more at risk of low knowledge and risky behaviour. That higher knowledge is associated with lower likelihood of dangerous practices and negative attitudes, highlights the importance of educating people about COVID‐19 to improve their knowledge which may result in improvements in attitudes and adherence to public health measures. |
Communication purpose: This study may be useful for understanding groups more at risk of low knowledge, poor attitudes and poor preventive health practices, which can help people designing communication interventions target their interventions to higher risk groups. Related to review questions: Knowledge about COVID‐19, and some demographic factors (gender, education level, age, occupation), affects adherence to physical distancing measures (avoiding crowds). |
# COVID‐19 specific, *^ non COVID‐19 specific but interpreted specifically in light of COVID‐19 outbreak, * non‐COVID‐19 specific, + NACCHO National Association of County & City Health Officials, % AMSTAR rating from McMaster Health Forum (via Health Systems Evidence https://www.healthsystemsevidence.org); ⁱAGREE instrument Appraisal of Guidelines for Research & Evaluation (via AGREE Enterprise https://www.agreetrust.org/agree-ii/)
Abbreviations: AGREE II: Appraisal of Guidelines for Research & Evaluation II tool AMSTAR: A Measurement Tool to Assess Systematic Reviews CASP: Critical Appraisal Skills Programme CDC: Centres for Disease Control and Prevention COI: conflict of interest ECDC: European Centres for Disease Control and Prevention EEA: European Economic Area EU: European Union GL: guideline H1N1: H1N1 influenza strain HIV: human immunodeficiency virus NACCHO: National Association of County and City Health Officials NIHR: National Institute for Health Research NPI: non‐pharmaceutical interventions PH: public health PHAC: Public Health Agency Canada PHM: public health measures PHSM: public health and social measures SAGE: Scientific Advisory Group for Emergencies SARS: Severe Acute Respiratory Syndrome SR: systematic review THL: Finnish Institute for Health and Welfare UNICEF: United Nations International Children's Emergency Fund WHO: World Health Organization
Table g: included studies with general physical distancing focus
| General | Study features | Outcomes and findings | Translational steps |
| Systematic reviews, guidelines | |||
|
Bekele 2020# Citation type: SR Public health measure: General PD Mapping to: Adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery |
Overview and aim: To identify patterns and determinants of knowledge, attitudes, and practices towards COVID‐19: within the general population and in healthcare workers across the globe. Type of study and data: SR, cross‐sectional studies; N = 21 Inclusion and exclusion criteria: Included: studies on COVID‐19 of adults, published in English Excluded: unclear outcomes of interest, pre‐prints and letters Participant features and numbers, sampling details: General population and healthcare workers. Healthcareworkers comprised psychiatrists and other specialists, doctors, nurses and pharmacists. Range of educational levels and occupations across studies. Sample sizes ranged from approximately 300 to 8500. Included disease(s): COVID‐19 Timing: Search period: March 16 to July 30, 2020 Countries included: China (3), India (3), Saudi Arabia (3), Malaysia (2), USA +/‐ UK (2); remainder single studies: Turkey, Iran, Vietnam, Jordan, Pakistan, Nigeria, Philippines, Qatar Income levels predominantly high‐ or middle‐income levels across included countries Intervention or phenomenon of interest: Patterns and factors determining levels of knowledge, attitudes and practice of preventive behaviours. Quality assessment: AMSTAR 5/11: [1. No protocol; 4. Seems published only, English only papers included; 5. No excluded studies provided; 8. No integration of quality assessment into the findings/interpretation; 10. No publication bias assessed; 11 no COI of included studies reported]. Funding source: The author(s) received no financial support for the research, authorship, and/or publication of this article. |
Reported on: COVID‐19 knowledge
Attitudes
Practices
Associated factors
Recommendations: Although many participants show good knowledge levels, attitudes and practices towards prevention of COVID‐19, these are variable across studies, populations and across outcomes. Many factors may influence these outcomes, and so indirectly influence adoption of preventive behaviours. |
Communication purpose: Findings may be useful in suggesting factors that might importantly influence knowledge, attitudes and practices when requiring populations to understand and take up preventive measures for COVID‐10. Related to review questions: Knowledge, attitudes and preventive practices for COVID‐19 may be at high levels in some populations and samples but far lower in others. Many factors may influence each of these outcomes and so importantly determine the success or otherwise of public health measures to protect people from COVID‐19. |
|
Berg 2021# Citation type: SR (rapid, scoping) Public health measure: General PD Mapping to: Uptake, acceptability Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity Theme 5: public trust and perceptions |
Overview and aim: Synthesis of evidence on different modes of communication used by health authorities for pandemic risk communication. Type of study and data: Scoping review (rapid). 48 studies. Included surveys (primarily cross‐sectional, n = 15), mixed‐methods (n = 1), qualitative research (n = 10), policy studies (n = 1), experimental (n = 4, 1 RCT), quantitative statistical analysis (n = 18) Inclusion and exclusion criteria: English language, published, published January 2009 to October 2020. Studies on communication related to H1N1, COVID‐19 or flu more generally Participant features and numbers, sampling details: Varied; several surveys randomly or representatively sampled general adult populations within and across countries. Small number qualitative studies with selected population groups (e.g. Aboriginal people from Canada, Spanish‐speaking Hispanic people from US). Other analyses based on media analyses (e.g. websites, press releases, video sites). Included disease(s): H1N1 or pandemic ‘flu' more generally or COVID‐19 Timing: Search dates were based on coverage of the whole H1N1 outbreak (2009 onwards) and coverage of the response phase of the COVID‐19 pandemic. No further information reported Countries included: North America (n = 15; 11 of which were USA), Asia (n = 13; 8 of which were Chinese), Europe (n = 9), Africa (n = 1), Australia (n = 1), global/cross‐continent (n = 9). Income levels range from low to high‐income countries, no further details Intervention or phenomenon of interest: Communication modes used by health authorities during disease outbreaks with pandemic potential Quality assessment: AMSTAR 3/11: [2. Single selection and data extraction; 3. Search was not comprehensive as two databases only; 4. published data only; 5. Excluded studies not reported; 7,8. No quality assessment or use in formulating findings; 10. No publication bias assessment; 11. No declarations of interest for included studies] Funding source: The COVID communication: Fighting a pandemic through translating science (COVCOM) project has received funding from the Trond Mohn Foundation under grant agreement number TMS2020TMT10 and the University of Stavanger. JKO is supported by the National Institute for Health Research Yorkshire and Humber Patient Safety Translational Research Centre (NIHR Yorkshire and Humber PSTRC). |
Reported on: Three main communication mode categories identified in authorities’ risk communication: (1) Communication channels (media types) (2) Source credibility, and (3) How the message is communicated. Communication channels
Source credibility (i.e. perceived trust in formal (health authorities, governments, public health professionals) and informal pandemic health risk information sources and impact on protective behaviour):
How the message is communicated :
Recommendations: Ensure health authorities’ risk communication considers the range of factors (e.g. tailoring, trust, multiple channels, layout, accessibility, readability, timeliness of information, format) that might influence community engagement, knowledge and self‐efficacy, and subsequent behavioural changes to mitigate risk. Health authorities should disseminate information through multiple channels, including through social media, although care is needed to ensure that messages remain consistent and improve credibility (rather than creating confusion as may be the case if messages are communicated rapidly through multiple channels). Misinformation related to pandemic risks may be a substantial problem on social media sites. Countering this (misinformation, rumours and contradictory messages) remains problematic for health authorities. A remaining challenge for health authorities is to engage effectively with social media and to provide readily available, accessible information that is kept up to date, tailored to different reading levels and with consideration of layout to improve access, with the aim of avoiding amplification of risks communicated through mass media messages. Public trust in health authorities changes over time and is related to perceptions of crisis management. This in turn can affect people’s risk perception and behavioural response to risk. Health authorities need to work collaboratively with communities and trusted spokespeople to improve community trust, to ensure that messages are appropriately tailored to communities and to reach different groups, including migrants and ethnic groups, over time as the pandemic response changes. Risk communication messages should be balanced and evidence‐based, motivate self‐efficacy, and include actionable information that people can use to protect their health. Jargon may not have a negative impact in all cases, but may need to be considered as part of the tailoring of information to audiences’ educational and health literacy levels. |
Communication purpose: May inform health authorities’ risk communication messages and choice of channels, for communicating about pandemic risk to populations and groups within populations. Identified factors may usefully inform decisions about channels to be used, and tailoring of messages. Related to review questions: Communication of pandemic risk messages from authorities to the community is influenced by many factors, and these may affect behavioural mitigation measures. Such communication need to take account of these factors to ensure that risk communication messages are accessible and available to all groups within the population, to ensure consistency of messages to promote trust and understanding of required behavioural change to protect health. |
|
ECDC 2020g# (Review of guidelines; non‐SR) Mapping to: Acceptability, adherence; also feasibility/barriers |
Overview and aim: Supports public health preparedness planning and response activities based upon physical distancing measures aimed at minimising the spread of COVID‐19. Inclusion and exclusion criteria: Included: Several ECDC documents: Guidelines, rapid risk assessment, technical report, guidance document Countries included: EU/EEA Member states and UK Quality assessment: 1/11 AMSTAR rating:% (non‐systematic review) Funding source: Not reported |
Reported on: Focus here is on communication related to physical distancing measures. Public health
Educational institutions (school measures)
Workplaces (workplace measures)
Mass gathering cancellation, including faith‐based events:
Recommendations: Decisions about implementing physical distancing measures need to be tailored to context and setting (social and political factors). Identified importance of promoting solidarity and mutual community support when social distancing measures are implemented. Clear, co‐ordinated, and comprehensive communication of information about physical distancing measures is needed. To improve adherence to physical distancing measures, inequalities in terms of information provision (e.g. vulnerable populations), financial losses (e.g. those unable to work from home), educational disadvantage (e.g. unequal access to digital learning), stigma (for those self‐isolating/quarantined) need to be recognised and addressed, and support systems to ensure essential services and supplies put in place. |
Communication purpose: This may inform decisions about how to address potential barriers to physical distancing measures and actions to take, and guide communication with communities about measures that may promote improved acceptance of and adherence to physical distancing measures. Related to review questions: Findings identify a range of factors that may impede uptake of and adherence to physical distancing measures, such as financial losses, stigma, and unequal access to information and support. These vary across populations but need to be addressed to ensure that physical distancing measures are enacted. |
|
Gupta 2021# Citation type: SR Public health measure: General PD Mapping to: Adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery |
Overview and aim: To review research studies on knowledge, attitudes and practices towards the COVID‐19 pandemic Type of study and data: SR; N = 21 studies, all cross‐sectional Inclusion and exclusion criteria: None described Participant features and numbers, sampling details: General population (11 studies), healthcare workers (7 studies) and students (n = 3). Sample sizes ranged from approximately 60 to almost 7000 Included disease(s): COVID‐19 Timing: No timing of searches or literature reported. Paper submitted September 2020; included studies will reflect literature available prior to this date. Early pandemic Countries included: China (3 studies), Iran (3), global (2), Nepal (2); single studies in Egypt, USA and UK, Tanzania, Paraguay, Jordan/Arabia/Kuwait, Kenya, Peru, Malaysia, Uganda, Pakistan, India Income levels all middle‐income (low and upper) levels except UK/USA (high‐income) and Uganda (low‐income) Intervention or phenomenon of interest: Knowledge attitudes and practices related to COVID‐19 in general public, healthcare workers and students Quality assessment: AMSTAR 2/11: [rated down all items except 6. Included studies characteristics provided; and 9. Method of synthesis appropriate] Funding source: Not reported |
Reported on: General public
Healthcare workers
Students
Recommendations: Findings suggest the general population has a basic level of knowledge about the COVID‐19 pandemic. Commonly accessed information sources may contribute to spread of information and misinformation about required preventive measures within the general public. Government information is required to raise awareness about the causes and effects of COVID‐19. Healthcare workers have a generally good level of knowledge and a positive outlook towards the pandemic, as do medical students in general. Despite the generally high levels of knowledge amongst healthcare workers and students, there is still need for consistent reminders and messaging from authorities to improve public knowledge levels. |
Communication purpose: Findings may indicate some factors that might importantly influence knowledge, in particular about the use of preventive measures for COVID‐10. Awareness of preventive measures in vulnerable slum communities could be increased by media campaigns. Related to review questions: Knowledge, attitudes and preventive practices for COVID‐19 may be at high levels in some groups but lower in others. Many factors may influence each of these outcomes and so importantly determine the success or otherwise of public health measures to protect people from COVID‐19. |
|
JHCHS 2019* (Guideline) Mapping to: Acceptability, uptake, adherence Public health measure: 6 (crowd avoidance), one specific example relating to quarantine |
Overview and aim: Identification of priority actions ‘for countries, international organisations, and other stakeholders to pursue that would mitigate the public health, economic, social, and political consequences of the emergence of a high‐impact respiratory pathogen.’ (p. 7) Inclusion and exclusion criteria: Included: several high‐level reviews on global preparedness, interviews with international experts in pandemic preparedness and response Type of study and data: Review of reviews and interviews with specialists in the field Countries included: Not explicitly described Quality assessment: (AGREE II)ⁱ: Scope and purpose: 90%; Stakeholder involvement: 62%; Rigour of development: 34%; Clarity of presentation: 67%; Applicability: 50%; Editorial independence: 14%. Funding source: This report was commissioned by and prepared for the Global Preparedness Monitoring Board. |
Reported on: Only data most relevant to communication interventions in the context of the current rapid review have been extracted.
Recommendations: Risk communication during outbreaks is an essential component of the response, requiring planning prior to outbreaks and involving communities as well as public health experts. Risk communication messages must be consistent, timely and accurate. Public trust is essential for effective risk communication, and community engagement can facilitate effective public health responses. Authorities must provide strong, evidence‐based rationale for public health measures, such as NPIs, so that they can be implemented effectively and their role in disease prevention be communicated effectively to the affected public. |
Communication purpose: Aspects of this report may inform the development of more effective public health communications and engagement, including those around physical distancing. Related to review questions: Describes actions countries can take to prepare, and optimal conditions for, effective communication to the public during a pandemic. Implementing the communication actions may lead to greater acceptability and uptake/adherence to physical distancing measures. |
|
Li 2020# Citation type: SR (rapid) Public health measure: General PD Mapping to: [major outcome categories] Uptake, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity |
Overview and aim: To identify how health provider should advise parents or families to obtain health education information (in relation to an infectious disease outbreak) Type of study and data: Rapid SR; observational studies (cross‐sectional survey studies); 24 studies included, n = 35,967 participants Inclusion and exclusion criteria: Included: People from the general population Observational studies available in English or Chinese before March 31, 2020 Excluded: participants from specific groups within the population (e.g. specific occupational groups) Participant features and numbers, sampling details: 35,967 participants sampled from across SARS, MERS and COVID‐19 outbreaks. Most (19/24) sampled adults aged 16 years and older; no further details reported Included disease(s): COVID‐19 (6 studies), SARS and MERS (18 studies) Timing: Authors note that accurate, reliable information about a disease outbreak is needed, and that this needs to be timely and kept up‐to‐date over the course of the pandemic/outbreak. Countries included: China (12 studies), Saudi Arabia or the Middle East (6), France (2), single studies in Hong Kong, Australia, Turkey, Canada Approximately half of studies (13/24) in upper‐middle income countries, remainder high‐income Intervention or phenomenon of interest: Health education and health promotion issues during COVID‐19, SARS and MERS outbreaks Quality assessment: AMSTAR 6/11: [1. No protocol, stated explicitly not registered; 5. No excluded studies provided 8. General limitations of studies described but not linked to findings specifically 10. Publication bias not assessed 11. COI for included studies not reported]. Funding source: This work was supported by grants from National Clinical Research Center for Child Health and Disorders (Children’s Hospital of Chongqing Medical University, Chongqing, China) (grant number NCRCCHD‐2020‐EP‐01) to EL; Special Fund for Key Research and Development Projects in Gansu Province in 2020, to YC; the Fourth Batch of “Special Project of Science and Technology for Emergency Response to COVID‐19” of Chongqing Science and Technology Bureau, to EL; special funding for prevention and control of emergency of COVID‐19 from Key Laboratory of Evidence Based Medicine and Knowledge Translation of Gansu Province (grant number No. GSEBMKT‐2020YJ01), to YC; The Fundamental Research Funds for the Central Universities (lzujbky‐2020‐sp14), to YC. |
Reported on: 9 studies mentioned information channels where people obtained health education information; 3 studies focused on health education campaigns. Lack of public awareness of infectious disease
Mode and health education reliability
The effect of health education
Recommendations: Improving public awareness of infectious diseases can positively influence preventive behaviours to slow disease transmission. However, stigma, discrimination and fear may also be present and may delay care or early quarantine or treatment, which in turn may increase spread of disease. It is therefore important to promote better knowledge while working to prevent stigma. Health education needs to be tailored to particular groups within the general public, such as children, the elderly and other vulnerable groups or those with particular needs (e.g. travellers likely to come into contact with the infectious disease). People often use multiple sources of information, and while new media may be more easily accessible there may also be a growing risk of misinformation with some of these sources. Public health agencies, governments and health authorities might be relied upon to deliver accurate, timely information and health education about an infectious disease and its prevention, changing over the stages of a pandemic or outbreak as required. |
Communication purpose: Findings may be useful for planning public health education and information, particularly when considering purpose(s), media and channels for such communication. Related to review questions: Public information or education about an infectious disease may improve knowledge and awareness of the disease and required preventive measures. However, there needs to be an awareness of the potential for stigma and discrimination and communications need to address these potential adverse consequences directly. A range of channels (media) are accessed by the public for public health information. Information and education should be credible and accurate, and public communication strategies might be planned with this in mind. Special groups may lack adequate knowledge about emerging diseases and communication strategies that specifically target special groups may be needed. |
|
Majid 2020#^ Citation type: SR (scoping) Public health measure: General PD Mapping to: Acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 5: public trust and perceptions |
Overview and aim: To examine how knowledge, awareness and misconceptions influence risk perceptions and behaviours. Type of study and data: Scoping review (cross‐sectional, cohort, qualitative, mixed methods); n=149 studies. Inclusion and exclusion criteria: Included: primary quantitative, qualitative, and mixed‐methods studies (including social media analyses) on response to global outbreak/pandemic (with focus on SARS 2003, influenza A/H1N1 2009, MERS 2012, EBV 2013, COVID‐19 (2020)). Excluded: mass media communication strategies (e.g. newspapers, television); abstracts, theses, dissertations and published papers without empirical primary data. Participant features and numbers, sampling details: No details systematically synthesised. Included disease(s): H1N1 (66 studies), EBV (42), SARS (32), MERS (10), and COVID‐19 (1). Timing: Searches for evidence were conducted March 2020. Authors note that information provided and effects on behaviour can change over the course of a pandemic outbreak (e.g. as reports on the pandemic decrease, so too may willingness to adhere to public health measures). Countries included: Studies took place across all continents except South America. Ranged from high income countries (US (26 studies), Hong Kong (13), Canada (11), Netherlands (10)), to middle income (China (9), Malaysia (5)) to low‐income countries (Sierra Leone (1), Liberia (4), Guinea (2)). Far more studies (120+) conducted in high rather than low (21 studies) income countries. Intervention or phenomenon of interest: Knowledge, awareness and misconceptions about infectious disease outbreaks and effects on preventive behaviours (e.g. physical distancing). Quality assessment: 3/11 [no items met except 6. Included study characteristics reported; 7. Quality of included studies assessed; 9. Synthesis methods (appropriate for scoping review)]. Funding source: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Umair Majid receives financial support from the Canadian Institutes of Health Research and the Government of Ontario, Canada. Neither party was involved in the design and conduct of this research. |
Reported on: Knowledge levels of disease, pandemic outbreak episodes, and modes of transmission or infection, were generally high across studies (8 studies). Information sources:
Social distancing:
Social pressures:
Knowledge, risk perceptions and behaviour:
Misconceptions: Misconceptions fell into several categories.
Recommendations: Knowledge, awareness, and misconceptions influence risk perception and behaviours, but changes depend on a range of factors such as country, population, and societal characteristics. During pandemics, knowledge generally spreads rapidly, and both accurate and inaccurate information spread quickly, but it is unclear how individuals and communities navigate accurate knowledge that promotes protective behaviours and inaccurate information that does not. Misconceptions may play a role in determining whether people with accurate knowledge develop high‐risk perceptions that then lead to behaviour change; where misinformation can effectively dilute the perception of risk and also lead to ineffective protective behaviours. Misconceptions may also increase risk perceptions (where there is uncertainty), leading to people adopting behaviours they believe are effective even if they are not. Social pressures may exert a strong positive influence on protective behaviours. However, they may also be the source of misconceptions. Introducing information that contradicts misconceptions may help, but this depends on the source and format of the information and on the level of trust people have in the source. Information that contradicts existing misconceptions may require people to process information at a higher level to inform their decisions and behaviours; this may delay the adoption of protective behaviours, lead to information overload and negative emotional states. Information that challenges or contradicts misconceptions, communicated from a trusted source, may reduce misconceptions if the communication is coherent. Frequent, drastic changes in reporting may be perceived as inaccurate by the public and lead to a loss of trust. Authorities should communicate clearly about what is known and what is not to build and sustain trust. |
Communication purpose: Findings may inform development of information materials for communicating with communities and individuals; and may help to identify areas where misconceptions are common and may require particular information to be communicated. Related to review questions: People may rely on several diverse information sources during a pandemic outbreak, including social networks and social media; but some may be prone to inaccuracies and misinformation. Trust is importantly linked to knowledge and protective behaviours during a pandemic, therefore trusted sources such as community leaders and government play a key role in communicating information about the pandemic and protective measures required by individuals and the community. Social pressures and influences may promote adherence to physical distancing measures; as did higher perceived risk, but behaviour change was not consistently at a high level and is influenced by a range of factors. A range of misconceptions, arising from a range of sources including social media and social networks, may exist about the disease and symptoms, transmission, treatments and origins. These can co‐exist alongside accurate information. Both tend to grow rapidly as the pandemic progresses, and misinformation can grow in the absence of available or accessible information, or in the presence of conflicting public health messages. People may also not tend to check information they receive from social networks. Misconceptions may negatively affect adoption of protective behavioural measures during a pandemic, and so are important to address. It may be important to work to counter misinformation or misconceptions by providing contradictory information, but this requires more cognitive work from people. Misconceptions may be more common amongst those with less trust of the government or of healthcare; therefore, community leaders, healthcare providers, the media and government all play an important role in communicating accurate information about disease and required health protection measures during a pandemic. |
|
Noone 2021# Citation type: ScR, rapid Public health measure: General PD Mapping to: Adherence Mapping to: Theme 3 support for individual and population behavioural changes |
Overview and aim: Assessment of the focus, quality and generalisability of the evidence on determinants of adherence to physical distancing measures. Specific questions included: Focus (what measures were assessed? How was adherence conceptualised and measured?); Quality (how great is the risk of bias?); and generalisability (where was the research set? Were representative groups studied?). Type of study and data: Scoping review; 84 studies, quantitative (59 cross‐sectional, 20 longitudinal, 5 randomised or non‐randomised). Inclusion and exclusion criteria: Included: evaluation of adherence to physical distancing measures, including potential determinants of adherence as independent variables. Quantitative study design; published in any language Excluded: studies focusing only on intention to adhere. Participant features and numbers, sampling details: 26% of studies used nationally representative samples for study; remaining were based on convenience sampling of some type. Included disease(s): COVID‐19. Timing: Searches July 2020 (first wave of the COVID‐19 pandemic). Searches were restricted to 2020. Countries included: 42 (50%) USA; majority of the remainder occurred in Western Europe, few taking place in Africa, Latin America and Asia (India, Japan, Thailand, China, Korea, Saudi Arabia, Qatar, Brazil). Indicates that most studies were undertaken in high income countries. Intervention or Phenomenon of interest: Potential determinants of adherence to physical distancing measures. Quality assessment: AMSTAR 8/11 [5. no list of excluded studies; 10. Publication bias not mentioned/assessed; 11. Sources of support included studies not reported]. Funding source: NW was funded by a summer scholarship award from Evidence Synthesis Ireland, Cochrane Ireland and the HRB‐Trials Methodology Research Network. HD was funded by the Health Research Board and the Irish Research Council under the COVID‐19 Pandemic Rapid Response Funding Call [COV19‐2020‐097]. |
Reported on: Adherence conceptualised (e.g. reduced mobility, stay at home, physical distance from others) and measured in a range of ways, mostly relying on smartphone GPS location data (n = 30) or on self‐reported adherence (e.g. to PH measures, reduced contacts) (n = 53). Coding using Theoretical Domains Framework for potential determinants of adherence to physical distancing measures identified the following:
Other domains related to communication and PD were typically less frequently coded but included Knowledge (understanding of COVID‐19) and Skills (e.g. health literacy). Recommendations: Several potential determinants of physical distancing adherence were identified, with adherence conceptualised and measured in a range of ways. These may serve as potential targets for strategies (interventions) seeking to improve adherence to physical distancing measures during a pandemic. |
Communication purpose: Findings may be useful when planning communication and support for communities undertaking physical distancing measures. Related to review questions: Potential determinants of physical distancing adherence appear wide‐ranging. Aspects related on a practical level to individuals’ context and resources, such as economic circumstances and the local pandemic situation, may be important. People’s beliefs in support of physical distancing, perceptions of risk and anticipated regret may also influence their behaviours related to adherence. Other aspects related to emotional state, social influences, knowledge of COVID‐19 and skills may also play a role in determining people’s adherence to physical distancing measures. |
|
PHAC 2022# Public Health Agency of Canada. Adjusting public health measures in the context of COVID‐19 vaccination At: Adjusting public health measures in the context of COVID-19 vaccination - Canada.ca Citation type: GL Public health measure: General PD Mapping to: Acceptability, uptake, adherence Mapping to: Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes |
Overview and aim: Provides considerations for adjusting PHMs as vaccination coverage increases and as numbers of new and active cases changes within the population and public health and health system pressures ease. Type of study and data: Guideline; best available evidence and expert opinion; and informed by PHAC 2021 (individual and community PHM measures; itself developed from rapid evidence reviews, policy advice from PH agencies (WHO, CDC), economic advice and research). Included disease(s): COVID‐19. Countries included: Canadian context; some included evidence from Canadian agencies, others from international or national sources (e.g. WHO, UNICEF, ECDC, CDC, SAGE UK). High income countries well‐represented; but within these disadvantaged and/or remote groups considered. Timing: Guideline developed to assist with planning and adjusting PHMs in response to changes in COVID‐19 activity occurring over time. Last modified Feb 22. Intervention or Phenomenon of interest: Considerations for adjusting PHMs including key communications required. Quality assessment: AGREE II scope and purpose 61.1%; stakeholder involvement 19.44%; rigor of development 7.3%; clarity of presentation 66.67%; applicability 2.08%; editorial independence 0%. Funding source: Not reported; this technical guidance was developed in consultation with the Canadian Pandemic Influenza Preparedness (CPIP) Task Group and with federal, provincial and territorial partners via the Technical Advisory Committee (TAC) and/or the Special Advisory Committee (SAC). This guidance was also developed in consultation with other government departments, various multilateral partners, Indigenous stakeholders, and other external stakeholders with an interest in this subject matter. |
Reported on:
Recommendations: The risk of COVID‐19 is associated with many factors, that change over time. Local responses based on assessment of such factors is required, leading to adjustment in PHMs. Agencies should proactively plan and communicate with communities about expected adjustments to measures, including reasons for the decisions. There should also be planning in place to support those at higher risk of COVID‐19 (e.g. at risk of more severe disease; not fully vaccinated) to adjust measures based on their own circumstances, including communication to normalise such actions where required. |
Communication purpose: May inform development of communications around PH measures, and adjustments required to these over time and with changing COVID‐19 risk level within communities. Related to review questions: Describes features of effectively communicating to support preventive measures, including physical distancing, against a backdrop of changing COVID‐19 risk. Acknowledges that personal information and decision‐making required for some individuals to follow additional measures; and the role that PH agencies have in communicating with communities to prevent stigma and promote collective actions for the common safety. Improving such communication may help to promote and improve acceptability of PHMs and changes to these over time, and to support adherence to required measures for communities and for individuals, including where there is a difference in the level of adoption of PHMs required based on personal risk. |
|
Sarria‐Guzman 2021# Citation type: SR Public health measure: General PD Mapping to: Uptake, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity |
Overview and aim: To identify and synthesise research on knowledge, attitudes and practices (KAP) related to COVID‐19 in America. Type of study and data: SR; cross‐sectional survey; N=13 studies, >18,000 participants. Inclusion and exclusion criteria: Included: research on KAP; peer‐reviewed, published English‐language studies; conducted in American continent. Excluded: abstracts; non‐peer‐reviewed source; non‐English; review or meta‐analysis; non‐American setting; high risk of bias (Hoy tool). Participant features and numbers, sampling details: All studies adults aged 18 years or older. General public (7/13 studies), elderly with chronic conditions (3/13), healthcare workers and endodontists (2 /13) and farming/non‐farming Latin migrant workers (1). Household income varied across studies, several included participants from lower socioeconomic groups. Included disease(s): COVID‐19. Timing: Searches conducted for research published 1 December 2019 to 24 September 2020. No further details. Countries included: 8/13 USA, 2/13 Brazil, 1 each Paraguay, Ecuador, Colombia All high or upper middle countries. Intervention or Phenomenon of interest: Knowledge, attitudes and practices towards COVID‐19 in the general population and within specific groups. Quality assessment: AMSTAR 4/11: [1. No protocol/plan referred to 3. Databases only, no supplemental searches 4. Published, English language studies only 5. No characteristics of excluded studies provided 8. Quality assessment not integrated/used for interpretation 10. Publication bias not reported 11. No COI of included studies reported]. Funding source: Not reported |
Reported on: All included studies assessed knowledge; two thirds also assessed attitudes and practices. General public:
People with chronic diseases:
Recommendations: Many factors influence KAP levels related to COVID‐19, and can be categorised as:
While people access information from various sources (television, websites, newspapers and social networks), social media is popular but may be the source of many inaccuracies and misinformation. Most people do not check the source of COVID‐19 information presented on social media, and this can lead to poor behaviours and decision‐making. Governments should ensure that high‐quality research and expert opinion are delivered clearly, accurately and impartially through a range of media (e.g. awareness campaigns, television). Materials to educate the public about COVID‐19 are critical to ensuring people understand what is required to prevent disease transmission. Healthcare workers also need specific, up‐to‐date information from reliable sources (e.g. WHO, CDC) in order to be able to adopt the required mitigation and prevention measures in different settings. Generally, the most marginalised communities (lower education and income levels) are often the most affected by pandemic outbreaks, with lower KAP amongst the elderly, less educated and rural residents. Health agencies and governments need to communicate effectively using a range of media or channels, to reach different parts of the community, including disadvantaged groups and those without Internet access. Educational activities may need to be accompanied by economic support to facilitate adherence to behavioural risk mitigation strategies. Preventative behaviours may vary across different family dynamics, as families with small children are more careful in following preventative behaviours than single people. |
Communication purpose: Findings may inform communication with populations for effectively informing them of disease risks and prevention measures, including those at disadvantage and/or those at higher risk of complications due to COVID‐19. Related to review questions: Public KAP related to COVID‐19 critically influence the spread of disease, but levels are variable within and across population groups. People obtain information from a variety of sources e.g. traditional and social media sources, but some (social media in particular) may be more prone to spreading misinformation than others. In some cases, the information may itself be inadequate to support informed decisions regarding adoption of preventive measures. To support better knowledge and behaviour change related to prevention of disease, official sources need to target different groups within the population, including those who are particularly vulnerable to COVID‐19 complications or who are greater disadvantage, such as those who are educated to a lower level, in remote areas, or of lower income or employment levels. Information provided must be accurate, timely, comprehensive and delivered through different channels. Lack of information (gaps) or misinformation may lead to risky behaviours. Improving the accuracy, reliability and dissemination of information related to preventive behaviours is therefore critical to controlling disease transmission. For some groups, even where knowledge of disease and prevention measures is good, there may be structural issues, such as the need to work outside the home or larger family groups, that necessitate additional supports such as financial support. |
|
WHO 2017* (guideline) Mapping to: Uptake, adherence, acceptability; also feasibility and barriers |
Overview and aim: Provides up‐to date evidence‐based systems‐focused guidance on emergency preparedness and response, based on systematic analyses of the literature, and developed particularly for the public health aspects of emergencies. Inclusion and exclusion criteria: Included: Evidence assembled under 3 overarching themes (A‐C), 12 questions framed and used to guide the development of evidence reviews; included the following research types: 1. Quantitative research with comparison groups (randomized, non‐randomized) 2. Quantitative research with descriptive survey methods 3. Qualitative research 4. Mixed‑method research and case studies. Intervention or phenomenon of interest: Emergency responses ranged from infectious disease to floods, earthquakes, volcanic eruption, bioterrorism, food‐borne illness, and radiological radiation emergencies. Countries included: Studies of all UN countries were reviewed; however, most analysed emergency events in high‐ and middle‐income countries in Asia, Europe, North America, and Oceania. Quality assessment:(AGREE II) Scope and purpose: 81% Stakeholder involvement: 86% Rigour of development: 83% Clarity of presentation: 88% Applicability: 67% Editorial independence: 100%. Funding source: Core WHO funds were used to finance 70% of the total cost of the project. This was supplemented by Pandemic Influenza Preparedness (PIP) risk communication capacity building project funds, and unearmarked funds provided to the WHO Health Emergencies Programme by the Government of Japan and the Government of the United Kingdom of Great Britain and Northern Ireland. |
Reported on:
Recommendations (directly relevant to review questions):
Strong recommendation; moderate‐quality evidence.
Conditional recommendation, moderate‐quality evidence.
|
Communication purpose: This may be useful for improving communication with communities by emphasising the provision of clear, transparent and consistent risk information (messages) that is disseminated widely and through different media, informs people about specific actions for protection of their health, and builds trust through transparency and acknowledgement of uncertainty. Findings may also inform efforts to engage local stakeholders in risk communication planning and dissemination. Related to review questions: Recommendations link effective risk communication strategies with enhanced trust and understanding of public health messaging, which may increase uptake of and adherence to risk mitigation measures (such as physical distancing measures). |
|
WHO 2020# Overview of public health and social measures Available: Overview of Public Health and Social Measures in the context of COVID-19 (who.int) Citation type: GL Public health measure: General PD Mapping to: Uptake, acceptability, adherence Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication |
Overview and aim: To provide an overview of PH and social measures for preventing or slowing COVID‐19 transmission and identify strategies to limit potential harms (social and economic impact). Type of study and data: Overview of several guidelines and policy briefings. Included disease(s): COVID‐19 but also drawing on pandemic preparedness literature more generally. Timing: May 2020 Authors note need for authorities and governments to regularly review and calibrate the PH/social response as pandemic changes over time. Changes need to be communicated to the public over time; and strategies to minimise unintended effects of PH/social measures applied and adapted over time. Countries included: No specific country identified. Intervention or phenomenon of interest: Public health/social measures (including personal measures, PD, movement measures & special protection measures) to suppress disease, as well as social and economic impacts and possible strategies to mitigate negative impacts. Quality assessment: AGREE II: scope and purpose 66.7%; stakeholder involvement 30.56%; rigour of development 19.8%; clarity of presentation 50.0%; applicability 6.25%; editorial independence 12.5%. Funding source: Not reported. |
Reported on:
Engagement of the public is needed to ensure success of PH and social measures. To achieve this, regular dialogue through trusted channels is needed, so that people have access to the right information at the right time and so can make informed decisions to protect themselves or their families. Decision‐makers should engage with communities and communicate openly and regularly about how to implement measures, at all stages of the pandemic and recovery.
Communicating effectively and engaging communities: For individuals/community:
At government level:
Promoting adherence: For individuals/community:
At government level:
Mitigating unintended effects of PH/social measures includes the following: Support families and the community:
Protect income and economy:
Protect access to food and water:
Maintain essential health services:
Recommendations: Public health and social measures to prevent and suppress COVID‐19 must be applied appropriately to the local context, and with unintended (adverse) effects of such measures acknowledged and targeted with strategies to minimise negative outcomes. |
Communication purpose: This report may inform development of public communication strategies over time to inform people of preventive measures and alterations to measures, as well as strategies to counteract negative effects of PH/social measures to control disease. Measures should be communicated clearly, and regularly, to the public; should be informed by the local context & should provide information on the length of implementation. Community engagement is needed to help ensure the success of PH/social measures and adherence and acceptability of these within communities. Related to review questions: Describes communication and actions to be undertaken by authorities to promote adherence to PH and social measures, and to offset unintended effects of such measures. Strategies to provide support such as economic support, essential services and supplies, and to promote informed decisions, may be particularly key to promoting and supporting adherence to measures to protect health. |
|
WHO 2020a# At WHO-2019-nCoV-RCCE-v2020.1-eng.pdf January 2020 interim guidance Citation type: GL; interim guidance Public health measure: General PD Mapping to: Uptake, acceptability Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: To provide actionable guidance for countries to implement effective risk communication and community engagement (RCCE) strategies, with the aim of protecting the public’s health in the early COVID‐19 response Type of study and data: Interim guidance Included disease(s): COVID‐19 Timing: January 2020 (early pandemic) Countries included: WHO, international Intervention or Phenomenon of interest: Guidance on RCCE strategies Quality assessment: AGREE II: scope and purpose 63.90%; stakeholder involvement 8.33%; rigour of development 4.20%; clarity of presentation 52.78%; applicability 2.08%; editorial independence 0%. Funding source: Not reported |
Reported on: RCCE is a core component of health emergency preparedness and response. Data extracted focuses on findings most focused on communication in relation to promotion of preventive physical distancing measures. Clearly and proactively communicating about what is known, what is not, and what is being done to obtain information with the aim of saving lives, is a critical intervention in public health responses to any event. This helps to prevent spread of misinformation which can otherwise undermine the response, builds trust, and increases the chances that people will follow public health advice. Proactive and consistent public communication and engagement can reduce confusion; help people to understand their risk; identify how this might differ from authorities’ risk perceptions; and enables understandable, accessible and trusted information to be delivered to the public. Assessment of readiness (for countries without known cases):
RCCE initial response (for countries with cases)
Recommendations: Effective RCCE strategies form a critical part of the public health response to an emergency. They are multifaceted and require assessment, co‐ordination and ongoing monitoring and adjustment. |
Communication purpose: Findings may inform communication strategies particularly information provision to the public and may assist with planning and implementing communication and community engagement. Related to review questions: Clear, accurate and consistent communication of information, from and through trusted sources, may build trust and increase the likelihood of people following public health advice. Monitoring and addressing misinformation and rumours, and questions from members of the public, may also help to promote uptake of public health advice. Community engagement is also critical to understanding public perceptions and concerns and to identifying feedback to improve subsequent communications and information provision. |
|
WHO 2021a# Considerations for implementing and adjusting public health and social measures in the context of COVID‐19. Interim guidance 14 June 2021 Citation type: GL Public health measure: General PD Mapping to: Acceptability, adherence, feasibility Mapping to: Theme 1: features of public communication: content, timing and duration, and delivery Theme 2: recipients of public communication: audience, setting and equity Theme 3: support for individual and population behavioural changes Theme 4: community engagement to support communication Theme 5: public trust and perceptions |
Overview and aim: To provide guidance to Member States on introducing, lifting or adjusting public health and social measures (PHSMs) Type of study and data: GL (interim update, June 2021) Included disease(s): COVID‐19 Timing: Guidelines not specific to a particular stage of pandemic but focusses on need for adjustment of PHSMs over time according to COVID‐19 prevalence and communication and support measures needed to enable adjustment to measures over time Countries included: WHO, international Intervention or Phenomenon of interest: Guideline for countries to assess situation at national and subnational levels and need for introducing, adapting, or lifting PHSMs Quality assessment: AGREE II: scope and purpose 63.9%; stakeholder involvement 33.33%; rigour of development 6.3%; clarity of presentation 72.22%; applicability 0%; editorial independence 22.92%. Funding source: Not reported |
Reported on: Globally, COVID‐19 control will continue to rely on PHSMs for the foreseeable future, which is influenced by different vaccination levels and unequal access to vaccines around the world, but also by changing community transmission levels, and emergence of variants of concern. Adjusting public health and social measures: Decisions about implementing, lifting, or strengthening PHSMs should include consideration of several factors, including:
Community engagement and risk communication:
Individualised public health measures:
Recommendations: Establishing, adjusting, or reinstating PHSMs are needed to control COVID transmission and outbreaks. Decisions to adjust measures should be made rapidly in response to local transmission levels. All such decision‐making needs to balance the benefits and potential harms of enacting measures on both individuals and communities. Engagement with communities and stakeholders is needed throughout planning and decision‐making stages. Communication and support should be planned and in place in advance of any changes to PHSMs, and communication should occur regularly to keep the public informed about the situation. Special attention is needed to ensure that vulnerable/disadvantaged communities are engaged and communicated with effectively. |
Communication purpose: Guidance can inform strategies for planning and implementing public communication and support as PHSMs are adjusted to respond to changing COVID‐19 transmission levels within communities. Related to review questions: Proactive communication in advance of PHSM changes Identifies the need for clear, purposeful communication with communities about PHSMs and changes to these occurring over time. Highlights the need for community engagement and involvement of stakeholders in decisions about adjustments to PHSMs and to the public communication around these measures. Clear, transparent, timely communication tailored to local communities may help to build trust, to improve feasibility of implementation of the measures, and to improve acceptability and adherence to PHSMs. |
| Primary studies | |||
|
Lim 2020# (primary) Maps to: Uptake |
Overview and aim: Assessment of initial perceptions and responses towards COVID‐19 in Singapore, China and Italy in order to identify factors associated with anxiety and behavioural change (included avoidance of workplaces, public spaces, social engagements or public transportation, and changes to work‐related or personal travel plans) Inclusion and exclusion criteria: Included: invited (via email and SMS) online panel members (received incentive for completing), as well as Facebook users who clicked the survey link advertised (but did not receive incentive) Type of study and data: Online questionnaire‐based survey; 4,505 respondents (February to March 2020) Countries included: Singapore, China, Italy Quality assessment: Response rate: +++ (Singapore); ++ (China); + (Italy); Overall: ++ Sample methodology: ++ Authors declared no COI exists; sample underrepresented older people(China), younger people (Singapore), men and those without tertiary education (all 3 countries); majority of Italian respondents were from Lombardia and Veneto; preprint paper (not peer reviewed) |
Reported on:
Recommendations:
|
Communication purpose: Findings may be useful for enabling communication; facilitating decision‐making and supporting behaviour change in relation to modifying or engaging in specific behaviours to reduce people’s risk of infection for themselves or others. Related to review questions: Lower anxiety was associated with higher self‐efficacy and information sufficiency. Higher acceptance of restrictive control measures and information sufficiency were associated with participants modifying or engaging in specific behaviours to reduce the risk of infection to themselves or others (included avoidance of workplaces, public spaces, social engagements or public transportation, and changes to work‐related or personal travel plans). |
Abbreviations:
AMSTAR: A Measurement Tool to Assess Systematic Reviews CDC: Centres for Disease Control and Prevention EEA: European Economic Area ECDC: European Centres for Disease Control and Prevention ERC: emergency risk communication EU: European Union GL: guideline GPS: global positioning system H1N1: H1N1 influenza strain KAP: knowledge, attitudes, practices MERS: Middle East Respiratory Syndrome NIHR: National Institute for Health Research PD: physical distancing PH: public health PHM: public health measure PHSM: public health and social measures RCCE: risk communication and community engagement RCT: randomised controlled trial SARS: Severe Acute Respiratory Syndrome SR: systematic review WHO: World Health Organization
Appendix 7. Themes used as framework for thematic synthesis
The six themes arising from the original synthesis of studies and used as framework for synthesis in this update (taken from Ryan 2021a):
Public communication: features of communication (content, timing and duration, and delivery);
Public communication: recipients of communication (audience and setting, and equity issues);
Supporting changes to behaviour at population and individual levels (including changing attitudes or intentions related to behaviour change);
Engaging the community and its members in developing and delivering communication;
Public trust and perceptions;
Communication and support considerations specific to distancing measures in schools and workplaces.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Atchison 2020.
| Study characteristics | ||
| Notes | ||
Bekele 2020.
| Study characteristics | ||
| Notes | ||
Berg 2021.
| Study characteristics | ||
| Notes | ||
Bodas 2020.
| Study characteristics | ||
| Notes | ||
Briscese 2020.
| Study characteristics | ||
| Notes | ||
Brooks 2020.
| Study characteristics | ||
| Notes | ||
Brooks 2020a.
| Study characteristics | ||
| Notes | ||
Burnet 2020.
| Study characteristics | ||
| Notes | ||
Burnet 2020a.
| Study characteristics | ||
| Notes | ||
Cardwell 2021.
| Study characteristics | ||
| Notes | ||
CDC 2022.
| Study characteristics | ||
| Notes | ||
CDC 2022a.
| Study characteristics | ||
| Notes | ||
CDC 2022b.
| Study characteristics | ||
| Notes | ||
Chu 2020.
| Study characteristics | ||
| Notes | ||
Chung 2021.
| Study characteristics | ||
| Notes | ||
Clements 2020.
| Study characteristics | ||
| Notes | ||
DES 2020.
| Study characteristics | ||
| Notes | ||
Eaton 2020.
| Study characteristics | ||
| Notes | ||
ECDC 2020.
| Study characteristics | ||
| Notes | ||
ECDC 2020a.
| Study characteristics | ||
| Notes | ||
ECDC 2020b.
| Study characteristics | ||
| Notes | ||
ECDC 2020g.
| Study characteristics | ||
| Notes | ||
Farooq 2020.
| Study characteristics | ||
| Notes | ||
Gilmore 2020.
| Study characteristics | ||
| Notes | ||
Gomez‐Duran 2020.
| Study characteristics | ||
| Notes | ||
Gupta 2021.
| Study characteristics | ||
| Notes | ||
Heuvelings 2018.
| Study characteristics | ||
| Notes | ||
JHCHS 2019.
| Study characteristics | ||
| Notes | ||
Khorram‐Manesh 2021.
| Study characteristics | ||
| Notes | ||
Kwok 2020.
| Study characteristics | ||
| Notes | ||
Li 2020.
| Study characteristics | ||
| Notes | ||
Lim 2020.
| Study characteristics | ||
| Notes | ||
Lin 2014.
| Study characteristics | ||
| Notes | ||
Lohiniva 2020.
| Study characteristics | ||
| Notes | ||
Lor 2016.
| Study characteristics | ||
| Notes | ||
Lunn 2020.
| Study characteristics | ||
| Notes | ||
Majid 2020.
| Study characteristics | ||
| Notes | ||
Mao 2021.
| Study characteristics | ||
| Notes | ||
Megnin‐Viggars 2020.
| Study characteristics | ||
| Notes | ||
Meier 2020.
| Study characteristics | ||
| Notes | ||
Mobasseri 2020.
| Study characteristics | ||
| Notes | ||
Moya‐Salazar 2021.
| Study characteristics | ||
| Notes | ||
NACCHO 2006.
| Study characteristics | ||
| Notes | ||
Noone 2021.
| Study characteristics | ||
| Notes | ||
PHAC 2021.
| Study characteristics | ||
| Notes | ||
PHAC 2021a.
| Study characteristics | ||
| Notes | ||
PHAC 2022.
| Study characteristics | ||
| Notes | ||
Qazi 2020.
| Study characteristics | ||
| Notes | ||
Regmi 2021.
| Study characteristics | ||
| Notes | ||
Roy 2020.
| Study characteristics | ||
| Notes | ||
Sarria‐Guzman 2021.
| Study characteristics | ||
| Notes | ||
Saurabh 2017.
| Study characteristics | ||
| Notes | ||
Seale 2020.
| Study characteristics | ||
| Notes | ||
Sopory 2021.
| Study characteristics | ||
| Notes | ||
Szkwarko 2017.
| Study characteristics | ||
| Notes | ||
Teasdale 2014.
| Study characteristics | ||
| Notes | ||
Tooher 2013.
| Study characteristics | ||
| Notes | ||
Webster 2020.
| Study characteristics | ||
| Notes | ||
WHO 2017.
| Study characteristics | ||
| Notes | ||
WHO 2020.
| Study characteristics | ||
| Notes | ||
WHO 2020a.
| Study characteristics | ||
| Notes | ||
WHO 2020b.
| Study characteristics | ||
| Notes | ||
WHO 2020c.
| Study characteristics | ||
| Notes | ||
WHO 2021.
| Study characteristics | ||
| Notes | ||
WHO 2021a.
| Study characteristics | ||
| Notes | ||
WHO 2021b.
| Study characteristics | ||
| Notes | ||
Zhong 2020.
| Study characteristics | ||
| Notes | ||
Zhu 2020.
| Study characteristics | ||
| Notes | ||
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| AASLD 2020 | Primary clinical management/ pathway |
| Abbas 2021 | No physical distancing focus |
| Adlhoch 2020 | No communication focus |
| Allen 2020 | No communication and physical distancing focus |
| Alom 2021 | Primarily clinical management/ pathway; health system (not community) |
| Alvarez‐Galvez 2021 | No physical distancing focus |
| Amerio 2020 | Non‐systematic review/overview (commentary) |
| Andrikopoulos 2020 | Non‐systematic review/overview |
| Anglemyer 2020 | No communication focus |
| Aniceto 2021 | Non‐systematic review/overview (commentary) |
| ANZICS 2020 | Primarily clinical management/ pathway |
| ANZICS 2020b | No physical distancing focus |
| ASRM 2020 | No communication and physical distancing focus |
| Barry 2013 | No physical distancing focus |
| Bhaumik 2020 | No communication focus |
| Bin 2021 | Non‐systematic review/overview; not intersection between communication and physical distancing |
| Bittencourt 2020 | Primarily clinical management/pathway; health system (not community); no communication focus |
| Blasioli 2022 | Non‐systematic review/overview; not intersection between communication and physical distancing |
| Bokolo 2020 | No communication and physical distancing focus |
| Bolcato 2020 | No communication focus |
| Bonell 2020 | Non‐systematic review/overview |
| Boschiero 2021 | Non‐systematic review/overview; no communication focus |
| Bouznad 2020 | Non‐systematic review/overview |
| Braithwaite 2020 | No communication focus |
| Brooks 2021 | Health system (not community) |
| Busa 2021 | Non‐systematic review/overview; no physical distancing focus |
| Cachon‐Zagalaz 2020 | No communication focus |
| Carter 2021 | No communication focus; no intersection between communication and physical distancing |
| CDC 2020 | No communication focus |
| CDC 2020a | No communication focus |
| CDC 2020b | No intersection between communication and physical distancing; health system (not community); primarily clinical management/pathway |
| CDC 2020c | No communication focus |
| CDC 2020d | No communication and physical distancing focus |
| CDC 2020e | No communication and physical distancing focus |
| CDC 2020f | No communication focus |
| CDC 2020g | No communication focus |
| CDC 2020h | No communication focus |
| CDC 2020i | No intersection between communication and physical distancing |
| CDC 2020j | No communication focus |
| CDC 2020k | No communication focus |
| CDC 2020l | No communication focus |
| CDC 2020n | No communication focus |
| CDC 2020o | No communication focus |
| CDC 2020p | No communication and physical distancing focus |
| CDC 2020q | No communication and physical distancing focus |
| CDC 2020r | No communication and physical distancing focus |
| CDC 2020s | Primarily clinical management/pathway; no communication focus |
| CDC 2020t | No communication and physical distancing focus |
| CDC 2020u | No intersection between communication and physical distancing |
| CDC 2020v | No communication focus |
| CDC 2020w | No communication focus |
| CDC 2020x | Not research, communication toolkit sample |
| CDC 2021 | No communication focus |
| CDC 2021a | No communication and physical distancing focus |
| CDC 2021aa | No communication and physical distancing focus |
| CDC 2021ab | No communication focus |
| CDC 2021ac | No communication and physical distancing focus |
| CDC 2021ad | No communication focus |
| CDC 2021ae | No communication focus |
| CDC 2021af | No communication and physical distancing focus |
| CDC 2021ag | No intersection between communication and physical distancing |
| CDC 2021ah | No communication focus |
| CDC 2021ai | No communication focus |
| CDC 2021aj | No communication and physical distancing focus |
| CDC 2021ak | No communication and physical distancing focus |
| CDC 2021al | Primarily clinical management/pathway |
| CDC 2021am | No communication and physical distancing focus |
| CDC 2021an | No communication and physical distancing focus |
| CDC 2021ao | No communication and physical distancing focus |
| CDC 2021ap | No communications focus; health care (not community) |
| CDC 2021aq | No communication focus |
| CDC 2021ar | No communication focus |
| CDC 2021b | No communication focus |
| CDC 2021c | No communication and physical distancing focus |
| CDC 2021d | No communication focus |
| CDC 2021e | No communication focus |
| CDC 2021m | No communication focus |
| CDC 2021n | No communication focus |
| CDC 2021o | No communication and physical distancing focus |
| CDC 2021p | Health system (not community) |
| CDC 2021q | No communication focus |
| CDC 2021s | Health system (not community) |
| CDC 2021t | No communication or physical distancing focus (cleaning) |
| CDC 2021u | No communication focus |
| CDC 2021v | Health system (not community) |
| CDC 2021w | No communication focus |
| CDC 2021x | No communication focus |
| CDC 2021y | No communication focus |
| CDC 2021z | No communication focus |
| Chackalackal 2021 | No communication focus |
| Chan 2020 | No communication focus |
| Chawla 2020 | Primarily clinical management/pathway |
| Choukou 2021 | No communication and physical distancing focus |
| Cobb 2021 | No communication and physical distancing focus |
| Collins 2020 | Non‐systematic review/overview |
| Couto 2020a | Non‐systematic review/overview |
| Daszak 2021 | Non‐systematic review/overview; no physical distancing focus |
| DEHS 2020 | No communication and physical distancing focus |
| Deolmi 2020 | Non‐systematic review/overview |
| DES 2020a | No communication focus |
| DES 2020b | No communication and physical distancing focus |
| Desveaux 2021 | Non‐systematic review/overview |
| DFE 2021 | No communication and physical distancing focus |
| Dhamija 2021 | Primarily clinical management/pathway; no communication focus |
| DHCS 2021 | No communication focus |
| DiLorenzo 2021 | Primarily clinical management/pathway; no intersection between communication and physical distancing |
| Dos Santos 2020 | No communication focus |
| Downes 2020 | No intersection between communication and physical distancing |
| Dubey 2020 | Non‐systematic review/overview; no communication focus |
| EC 2020 | No communication and physical distancing focus |
| ECDC 2020c | No communication focus |
| ECDC 2020d | No communication focus |
| ECDC 2020e | No communication focus |
| ECDC 2020f | No communication focus |
| Ekberg 2020 | Non‐systematic review/overview; no communication or physical distancing focus |
| EMSA 2021 | No communication focus |
| Feiz 2020 | Not systematic review/overview |
| Ferreira 2020 | Non‐systematic review/overview; health system (not community); primarily clinical management/pathway |
| Finset 2020 | Non‐systematic review/overview |
| Flores 2020 | Non‐systematic review/overview; no communication focus |
| Flumignan 2020 | No communication and physical distancing focus; health system (not community) |
| Geerts 2021 | No physical distancing focus; health system (not community) |
| Gelfand 2021 | Primarily clinical management/pathway; no communication focus |
| Ghate 2020 | No communication and physical distancing focus |
| Government Ireland 2021 | No communication and physical distancing focus |
| Graber 2021 | No communication focus |
| Greysen 2021 | No communication and physical distancing focus; health system (not community) |
| Griffin 2021 | Non‐systematic review/overview |
| Hagan 2020 | Non‐systematic review/overview |
| Hamouche 2021 | No communication focus; non‐systematic review/overview |
| Hirt 2022 | No communication focus |
| Honein 2020 | No communication and physical distancing focus |
| Horcher 2021 | Non‐systematic review/overview; no communication focus |
| Hossain 2020 | No communication focus |
| IASC 2020 | No intersection between communication and physical distancing |
| Iezadi 2021 | No communication focus |
| Imtiaz 2020 | No communication focus |
| Jammu 2021 | No communication focus |
| Jesus 2021 | No communication focus |
| Johansen 2020 | No communication focus |
| Kamposioras 2020 | No communication focus; primarily clinical management/pathway |
| Kondylakis 2020 | Not physical distancing focus |
| Kumar 2020 | No communication focus |
| Kunzler 2021 | No physical distancing and communication focus |
| Kurniawan 2021 | No communication or physical distancing focus; primarily clinical management/pathway |
| Lal 2020 | No physical distancing focus; non‐systematic review/overview |
| Landewe 2020 | No communication and physical distancing focus |
| Lebrasseur 2021 | No intersection between communication and physical distancing |
| Leon Singh 2020 | No communication focus |
| Lo 2020 | No communication focus |
| Lotfi 2021 | Non‐systematic review/overview |
| Maldonado 2020 | Non‐systematic review/overview |
| Mastura 2020 | Non‐systematic review/overview |
| Matos 2020 | No communication and physical distancing focus |
| Matras 2020 | Primarily clinical management/pathway; no communication and physical distancing focus |
| Matterne 2021 | No intersection between communication and physical distancing; non‐systematic review/overview |
| Mendez‐Brito 2021 | No communication and physical distancing focus |
| Michie 2020 | Non‐systematic review/overview |
| Mikuls 2020 | Health system (not community); no communication focus; primary clinical management/pathway |
| Ministry of Health | No communication focus |
| Miralles 2021 | Non‐systematic review/overview |
| Mistraletti 2020 | No physical distancing focus; no intersection between communication and physical distancing |
| Morina 2021 | No communication focus |
| Muhammad 2020 | Non‐systematic review/overview; no communication focus |
| Murphy 2021 | Primarily clinical management/pathway; no physical distancing and communication focus |
| Nachega 2020 | Non‐systematic review/overview |
| Nagata 2021 | Health impact assessment; not review of research |
| Najafizada 2021 | No communication and physical distancing focus |
| Narla 2021 | Primarily clinical management/pathway; no communication focus; health system (not community) |
| NICE 2020 | Primarily clinical management/pathway; no physical distancing focus |
| Novak 2020 | Health system, not community; no intersection between communication and physical distancing |
| NSW DoH 2020 | No communication and physical distancing focus; no intersection between communication and physical distancing; health system (not community) |
| Nursalam 2020 | No communication and physical distancing focus |
| O'Connell 2021 | No communication focus |
| Ogunleye 2020 | Non‐systematic review/overview |
| Orchard 2021 | No communication focus; primarily clinical management/pathway |
| Pahl 2021 | No communication and physical distancing focus |
| Parajuli 2020 | No intersection between communication and physical distancing |
| Parker 2020 | No communication focus |
| Patel 2020 | No communication focus |
| Patel 2021 | Non‐systematic review/overview |
| Perski 2021 | No physical distancing focus; no intersection between communication and physical distancing |
| PHAC 2020 | No communication and physical distancing focus |
| PHAC 2020a | No communication focus |
| PHAC 2020b | No communication focus |
| PHAC 2020c | No intersection between communication and physical distancing |
| PHAC 2021b | Not physical distancing, communication |
| PHAC 2021c | No communication and physical distancing focus |
| PHAC 2021d | No intersection between communication and physical distancing |
| PHAC 2021e | No communication focus |
| PHAC 2021f | No communication focus |
| PHAC 2021g | No intersection between communication and physical distancing |
| Pimenta 2020 | No physical distancing focus |
| Polonsky 2021 | No intersection between communication and physical distancing (protocol; focus on mental health outcomes not physical distancing) |
| Pourroy 2020 | No communication and physical distancing focus; health system (not community) |
| Price 2020 | No communication focus |
| Puspitasari 2020 | No intersection between physical distancing and communication |
| Qazi 2021 | No communication and physical distancing focus |
| Qi 2021 | No communication and physical distancing focus |
| Rao 2020 | No communication and physical distancing focus |
| RCP 2020 | Primarily clinical management/pathway |
| Ribal 2020 | No communication and physical distancing focus; primarily clinical management/pathway |
| Riggioni 2020 | Primarily clinical management/pathway; no communication focus |
| Robertson 2020 | No physical distancing and communication focus; health system (not community) |
| Robinson 2020 | Primary clinical management/pathway; health system (not community); non‐systematic review/overview |
| Rocha 2021 | No communication focus |
| Ryan 2020 | No communication focus |
| Saadatjoo 2021 | No communication focus |
| Santos 2020 | Non‐systematic review/overview |
| Santos 2020a | Non‐systematic review/overview; primarily clinical management/pathway; no communication and physical distancing focus |
| SCDPC 2020 | No physical distancing focus and no communication focus |
| Schellack 2020 | Non‐systematic review/overview; no physical distancing and communication focus; primarily clinical management/pathway |
| Schoonees 2021 | No physical distancing focus |
| Selman 2020 | Non‐systematic review/guidelines; no physical distancing focus |
| Sendzikaite 2021 | Primarily clinical management/pathway; no communication focus |
| Serafini 2020 | Non‐systematic review/overview; no physical distancing focus |
| Sharma 2020 | Non‐systematic review/overview; no intersection between communication and physical distancing |
| Sheen 2020 | No intersection between communication and physical distancing (poster, excluded based on abstract only) |
| Sheen 2020a | No communication focus; non‐systematic review/overview (poster, excluded based on abstract only) |
| Silva 2021 | No communication focus |
| Srikanth 2020 | No intersection between communication and physical distancing |
| Stavridou 2020 | No communication focus |
| Stawicki 2020 | No intersection between communication and physical distancing |
| Stephen 2020 | No communication and physical distancing focus |
| Stoilov 2020 | No communication focus; primary clinical management/overview |
| Stojanovski 2021 | No communication and physical distancing focus |
| Stratil 2020 | No communication focus |
| Sullivan 2020 | Primarily clinical management/pathway; no communication focus |
| Tabari 2020 | Non‐systematic review/overview; no communication focus; no intersection between communication and physical distancing |
| Tam 2020 | Primarily clinical management/pathway; no communication focus |
| Tam 2021 | Primarily clinical management/pathway; no communication focus |
| Taylor 2020 | Non‐systematic review/overview; lack of communication focus |
| TC 2020 | No communication focus |
| Tegegne 2021 | Health system (not community) |
| Ting 2020 | No communication and physical distancing focus |
| Tonin 2020 | No communication and physical distancing focus; non‐systematic review/overview |
| Tsao 2021 | Lack of communication and physical distancing focus |
| Turner 2021 | No communication focus; health system (not community) |
| UK HSA | No communication focus |
| Ul Haq 2021 | No physical distancing focus |
| Vaezi 2020 | Not systematic review/overview |
| Viero 2021 | No communication focus |
| Wake 2020 | Non‐systematic review/overview; no interaction between communication and physical distancing |
| Wallace 2020 | Non‐systematic review/overview; no communication and physical distancing focus |
| Wang 2020 | Non‐systematic review/overview |
| WHO 2020d | No communication and physical distancing focus |
| WHO 2020e | No communication focus |
| WHO 2020f | No communication focus |
| WHO 2020g | No communication and physical distancing focus |
| WHO 2020h | No communication and physical distancing focus |
| WHO 2020i | No communication and physical distancing focus |
| WHO 2020j | No communication and physical distancing focus |
| WHO 2020k | No physical distancing focus |
| WHO 2020l | No intersection between communication and physical distancing |
| WHO 2020m | No communication and physical distancing focus |
| WHO 2020n | No intersection between communication and physical distancing |
| WHO 2020o | No communication and physical distancing focus |
| WHO 2020p | No communication focus |
| WHO 2020q | Communication not a focus |
| WHO 2021c | No communication focus |
| WHO 2021d | No communication and physical distancing focus; health system (not community) |
| Wilkinson 2020 | No communication and physical distancing focus |
| Yazew 2021 | No interaction between communication and physical distancing |
| Yu 2020 | Primarily clinical management/pathway |
| Yuan 2021 | No communication and physical distancing focus |
| Yue 2020 | No intersection between communication and physical distancing |
| Zhang 2021 | No communication and physical distancing focus |
Characteristics of studies awaiting classification [ordered by study ID]
Adab‐Corpa 2021.
| Notes | Requires translation from Spanish. English abstract suggests the review may be relevant. |
Dreyer 2020.
| Notes | Unable to locate full text for assessment |
Ghungrud 2021.
| Notes | Unable to locate full text for assessment |
Jun 2020.
| Notes | Requires translation from Chinese: English abstract indicates potential relevance although unclear if guideline or systematic review. |
Kang 2020.
| Notes | Cannot locate full text for assessment |
Odendaal 2020.
| Notes | Cannot identify full text for assessment |
Thomson 2021.
| Notes | Cannot locate full text for assessment |
Characteristics of ongoing studies [ordered by study ID]
Grimani 2021.
| Study name | Systematic review of effective communication strategies for infectious diseases population behaviour change |
| Starting date | Unclear |
| Contact information | Correspondence to Dr Aikaterini Grimani; aikaterini.grimani@wbs.ac.uk |
| Notes | Research questions: Are messages focusing on protecting others effective in changing a defined list of behavioural outcomes compared with other messages/controls? What behaviours (eg, social distancing, hand washing, face touching, using hygiene products, and so on) do messages about protecting others appear to affect positively? What populations do messages about protecting others appear to affect positively? |
Monteiro 2021.
| Study name | Systematic review on barriers and facilitators |
| Starting date | Unclear |
| Contact information | Correspondence to Dr Karla Morganna Pereira Pinto de Mendonça; karla‐morganna@hotmail.com |
| Notes | This study aims to summarise and evaluate the evidence on barriers and facilitators to populational adherence to prevention and control measures in COVID‐19 and other respiratory infectious diseases. |
Differences between protocol and review
The protocol described a two‐stage approach to selecting relevant evidence (following the methods of the original review published in 2021): stage one identifying synthesised evidence sources (systematic reviews and guidelines); stage two identifying primary research studies that filled gaps in the evidence arising from synthesised evidence sources. Screening for stage 1 identified a large volume and range of synthesised evidence for inclusion and the decision was therefore made to halt screening at this level (rather than proceed to selecting primary studies).
Contributions of authors
Rebecca Ryan: led the protocol and all review stages including study screening, data extraction, quality assessments and data synthesis.
Charlotte Silke: contributed substantially to the protocol and all review stages including study screening, data extraction, quality assessments and data synthesis.
Anne Parkhill: developed and ran all searches; located studies for assessment and contributed to the drafting of the protocol and review.
Ariane Virgona: assisted with data extraction and checking, and with drafting the protocol and review.
Bronwen Merner: assisted with data extraction and checking, data synthesis and thematic analysis, and with drafting the protocol and review.
Shauna Hurley: contributed substantially to drafts of the protocol, review and thematic analysis, wrote the review background and advised on results and quality assessments.
Louisa Walsh: contributed substantially to drafts of the protocol and review and wrote the plain language summary.
Caroline de Moel: assisted with study screening, data extraction and checking, and provided input to thematic analysis and to the protocol and review drafts.
Lina Schonfeld: assisted with data extraction and checking, and provided input to the protocol draft.
Adrian GK Edwards: provided input on thematic analysis and contributed substantially to protocol and review drafts.
Jessica Kaufman: provided input on thematic analysis and contributed substantially to protocol and review drafts.
Alison Cooper: provided input on thematic analysis and contributed substantially to protocol and review drafts.
Rachel Kar Yee Chung: provided substantial input to all review drafts and to thematic analysis results.
Karla Solo: provided support for use of guidelines and provided input to review drafts.
Margaret Hellard: provided input on thematic analysis and to the protocol draft.
Gian Luca Di Tanna: provided input to protocol and review drafts.
Alisa Pedrana: provided input to the protocol draft.
Freya Saich: provided input to the protocol draft.
Sophie Hill: provided input and oversight at all stages of the protocol and review drafts.
Sources of support
Internal sources
No sources of support provided
External sources
-
National Health and Medical Research Council, Australia
Rebecca Ryan receives support for her position as Coordinating Editor of the Cochrane Consumers and Communication Group under the NHMRC funding to Australian Cochrane Groups (2020‐2023).
-
Health Research Board (Ireland) and the HSC Public Health Agency through Evidence Synthesis Ireland, Ireland
Charlotte Silke was partly supported by the Health Research Board (Ireland) and the HSC Public Health Agency (Grant number CBES‐2018‐001) through Evidence Synthesis Ireland/Cochrane Ireland.
Declarations of interest
Rebecca Ryan: no relevant interests; Coordinating Editor, Cochrane Consumers and Communication.
Charlotte Silke: none known.
Anne Parkhill: none known.
Ariane Virgona: none known.
Bronwen Merner: no relevant interests; joint Managing Editor for Cochrane Consumers and Communication from 2016 to June 2021.
Shauna Hurley: no relevant interests; adviser to Cochrane's Editor in Chief and as Communications Manager for Cochrane Australia.
Louisa Walsh: Gilead Sciences Inc (Consultant); shared my own opinions and comments on my own social media regarding consumer engagement in health service design and health service research; registered physiotherapist who works in health service research and teaches subjects in physiotherapy and public health degrees; consulting work for Consumers Health Forum of Australia (an ongoing relationship); Managing Editor of Cochrane Consumers and Communication; consumer representative, and have ongoing consumer roles with Consumers Health Forum of Australia and the Victorian Clinical Informatics Council (Department of Health).
Caroline de Moel: none known.
Lina Schonfeld: no relevant interests; Clinical Psychologist BSS Psychology.
Adrian GK Edwards: Wales COVID‐19 Evidence Centre (Grant/Contract); Cochrane Consumers and Communication Editor.
Jessica Kaufman: no relevant interests; Editor, Cochrane Consumers and Communication.
Alison Cooper: no relevant interests; General Practitioner, Rumney Primary Care Centre, Cardiff, UK Clinical Research Fellow, Cardiff University, UK.
Rachel Kar Yee Chung: none known.
Karla Solo: none known.
Margaret Hellard: no relevant interests; published opinion pieces and commentary related to COVID; Infectious Disease Physician, Alfred Hospital; .
Gian Luca Di Tanna: Gilead Sciences Inc (Consultant); works as a health professional at The George Institute for Global Health, University of New South Wales; Statistical Editor of Cochrane Consumer and Communication and Cochrane Breast Cancer.
Alisa Pedrana: Gilead Sciences Inc (Consultant); affiliated to the Burnet Institute ‐ provided advice to the Victorian Government about policy decisions for COVID‐19; Burnet Institute led a longitudinal cohort study on COVID‐19 (The Optimise Study) ‐ and we have published data from this study that may be relevant to this work; involved in the Optimise study received funding support from the Victorian Government Department of Jobs, Precincts and Regions, the Victorian Department of Health, the Macquarie Group Foundation, and Burnet Institute donors.
Freya Saich: Burnet Institute (Employment); Burnet Institute conducts social research into COVID‐19 through various studies; involved in the Optimise Study ‐ Victorian Government COVID‐19 Victorian Consortium, the Macquarie Group Foundation and Burnet Institute donors; the Optimise Study Longitudinal cohort study and social network study. It is a partnership between the Burnet Institute and the Doherty Institute in collaboration with University of Melbourne, Swinburne University of Technology, Monash University, La Trobe University, Murdoch Children's Research Institute, the Centre for Culture Ethnicity and Health, the Health Issues Centre and external collaborators including Alison Coelho.
Sophie Hill: no relevant interests; Cochrane Consumers and Communication Group, Joint Coordinating Editor, 2000‐June 2022.
Rebecca Ryan, Anne Parkill, Bronwen Merner, Louisa Walsh, Adrian Edwards, Gian luca Di Tanna and Sophie Hill have past or current editorial roles with the Cochrane Consumers and Communication Group. None were involved in the editorial processes for this review.
New
References
References to studies included in this review
Atchison 2020 {published data only}
- Atchison C, Bowman LR, Vrinten C, Redd R, Pristerà P, Eaton J, et al. Early perceptions and behavioural responses during the COVID-19 pandemic: a cross- sectional survey of UK adults. BMJ Open 2021;11:e043577. [DOI: 10.1136/bmjopen-2020-043577] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atchison CJ, Bowman L, Vrinten C, Redd R, Pristera P, Eaton JW, et al. Perceptions and behavioural responses of the general public during the COVID-19 pandemic: a cross-sectional survey of UK adults. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.04.01.20050039] [DOI] [PMC free article] [PubMed]
Bekele 2020 {published data only}
- Bekele F, Sheleme T, Fekadu G, Bekele K. Patterns and associated factors of COVID-19 knowledge, attitude, and practice among general population and health care workers: a systematic review. SAGE Open Medicine 2020;8:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Berg 2021 {published data only}
- Berg SH, O'Hara JK, Shortt MT, Thune H, Bronnick KK, Lungu DA, et al. Health authorities' health risk communication with the public during pandemics: a rapid scoping review. BMC Public Health 2021;21(1):1401. [DOI: 10.1186/s12889-021-11468-3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bodas 2020 {published data only}
- Bodas M, Peleg K. Self-isolation compliance in the COVID-19 era influenced by compensation: findings from a recent survey in Israel. Health Affairs 2020;39(6):936-41. [DOI: 10.1377/hlthaff.2020.00382] [DOI] [PubMed] [Google Scholar]
Briscese 2020 {published data only}
- Briscese G, Lacetera N, Macis M, Tonin M. IZA DP No. 13092: Compliance with COVID-19 Social-Distancing Measures in Italy: The Role of Expectations and Duration. Available at https://www.iza.org/publications/dp/13092/compliance-with-covid-19-social-distancing-measures-in-italy-the-role-of-expectations-and-duration 2020. [DOI] [PMC free article] [PubMed]
Brooks 2020 {published data only}
- Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 2020;395(10227):912-20. [DOI: 10.1016/S0140-6736(20)30460-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brooks 2020a {unpublished data only}
- Brooks S, Smith L, Webster R, Weston D, Woodland L, Hall I, et al. The impact of unplanned school closure on children's social contact: rapid evidence review. medRxiv [Preprint] 2020. [DOI: ] [DOI] [PMC free article] [PubMed]
- Brooks SK, Smith LE, Webster RK, Weston D, Woodland L, Hall I, et al. The impact of unplanned school closure on children's social contact: rapid evidence review. Eurosurveillance 2020;25(13):2000188. [DOI: 10.2807/1560-7917.ES.2020.25.13.2000188.] [DOI] [PMC free article] [PubMed] [Google Scholar]
Burnet 2020 {unpublished data only}
- Burnet Institute. COVID-19 Self-Isolation – Quarantine Study. Report 2. 2 April 2020. Data on file.
Burnet 2020a {unpublished data only}
- Burnet Institute. COVID-19 Self-Isolation – Quarantine Study. Report 1. 26 March 2020. Data on file.
Cardwell 2021 {published data only}
- Cardwell K, O'Neill SM, Tyner B, Broderick N, O'Brien K, Smith SM, et al. A rapid review of measures to support people in isolation or quarantine during the Covid-19 pandemic and the effectiveness of such measures. Reviews in Medical Virology 2021;32(1):e2244. [DOI: 10.1002/rmv.2244] [DOI] [PMC free article] [PubMed] [Google Scholar]
CDC 2022 {published data only}
- Centers for Disease Control and Prevention. COVID-19 Guidance for Operating Early Care and Education/Child Care Programs. https://stacks.cdc.gov/view/cdc/113923 (accessed 16 March 2022).
CDC 2022a {published data only}
- Centers for Disease Control and Prevention. Guidance for COVID-19 prevention in K-12 schools. https://pesquisa.bvsalud.org/global-literature-on-novel-coronavirus-2019-ncov/resource/pt/grc-747554 (accessed 16 March 2022).
CDC 2022b {published data only}
- Centers for Disease Control and Prevention. Guidance for Institutions of Higher Education (IHEs). https://stacks.cdc.gov/view/cdc/114196 (accessed 17 March 2022).
Chu 2020 {published data only}
- Chu IY-H, Prima A, Larson HJ, Lin L. Social consequences of mass quarantine during epidemics: a systematic review with implications for the COVID-19 response. Journal of Travel Medicine 2020;27(7):taaa192. [DOI: 10.1093/jtm/taaa192] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chung 2021 {published data only}
- Chung SC, Marlow S, Tobias N, Alogna A, Alogna I, You SL, et al. Lessons from countries implementing find, test, trace, isolation and support policies in the rapid response of the COVID-19 pandemic: a systematic review. BMJ Open 2021;11(7):e047832. [DOI: doi: 10.1136/bmjopen-2020-047832] [DOI] [PMC free article] [PubMed] [Google Scholar]
Clements 2020 {published data only}
- Clements JM. Knowledge and behaviors toward COVID-19 among US residents during the early days of the pandemic: cross-sectional onling questionnaire. JMIR Public Health and Surveillance 2020;6(2):e19161. [DOI: 10.2196/19161PMID: 32369759PMCID: 7212816] [DOI] [PMC free article] [PubMed] [Google Scholar]
DES 2020 {published data only}
- Department of Education and Skills, Ireland. Reopening Our Schools The Roadmap for the Full Return to School. https://www.gov.ie/en/publications/ (accessed 9 November 2021).
Eaton 2020 {published data only}
- Eaton LA, Kalichman SC. Social and behavioral health responses to COVID-19: lessons learned from four decades of an HIV pandemic. Journal of Behavioral Medicine 2020;3(3):341-5. [DOI: 10.1007/s10865-020-00157-y] [DOI] [PMC free article] [PubMed] [Google Scholar]
ECDC 2020 {published data only}
- European Centre for Disease Prevention and Control. Rapid Risk Assessment: Risk of COVID-19 transmission related to the end-of-year festive season. https://www.ecdc.europa.eu/en/publications-data/risk-assessment-covid-19-festive-season (accessed 16 March 2022).
ECDC 2020a {published data only}
- European Centre for Disease Prevention and Control. Guidance on the provision of support for medically and socially vulnerable populations in EU/EEA countries and the United Kingdom during the COVID-19 pandemic. https://www.ecdc.europa.eu/en/publications-data/guidance-medically-and-socially-vulnerable-populations-covid-19 (accessed 16 March 2022).
ECDC 2020b {published data only}
- European Centre for Disease Prevention and Control. Guidance on infection prevention and control of coronavirus disease (COVID-19) in migrant and refugee reception and detention centres in the EU/EEA and the United Kingdom. https://www.ecdc.europa.eu/en/publications-data/covid-19-guidance-prevention-control-migrant-refugee-centres (accessed 16 March 2022).
ECDC 2020g {unpublished data only}
- European Centre for Disease Prevention and Control. Considerations relating to social distancing measures in response to COVID-19 – second update. Publication Technical report. https://www.ecdc.europa.eu/en/publications-data/considerations-relating-social-distancing-measures-response-covid-19-second (accessed 1 May 2022).
Farooq 2020 {published data only}
- Farooq A, Laato S, Islam A. The impact of online information on self-isolation intention during the COVID-19 pandemic: a cross-sectional study. Journal of Medical Internet Research 2020;22(5):e19128. [DOI: 10.2196/19128] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gilmore 2020 {published data only}
- Gilmore B, Ndejjo R, Tchetchia A, Claro V, Mago E, Diallo AA, al et. Community engagement for COVID-19 prevention and control: a rapid evidence synthesis. BMJ Global Health 2020;5(10):e003188. [DOI: 10.1136/bmjgh-2020-003188] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gomez‐Duran 2020 {published data only}
- Gomez-Duran EL, Martin-Fumado C, Forero CG. Psychological impact of quarantine on healthcare workers. Occupational and Environmental Medicine 2020;77(10):666-74. [DOI: 10.1136/oemed-2020-106587] [DOI] [PubMed] [Google Scholar]
Gupta 2021 {published data only}
- Gupta PK, Kumar A, Joshi S. A review of knowledge, attitude, and practice towards COVID‐19 with future directions and open challenges. Journal of Public Affairs 2021;21(4):e2555. [DOI: 10.1002/pa.2555] [DOI] [Google Scholar]
Heuvelings 2018 {published data only}
- Heuvelings CC, Greve PF, Vries SG, Visser BJ, Bélard S, Janssen S, et al. Effectiveness of service models and organisational structures supporting tuberculosis identification and management in hard-to-reach populations in countries of low and medium tuberculosis incidence: a systematic review. BMJ Open 2018;8(9):e019642. [DOI: 10.1136/bmjopen-2017-019642] [DOI] [PMC free article] [PubMed] [Google Scholar]
JHCHS 2019 {published data only}
- Nuzzo JB, Mullen L, Snyder M, Cicero A, Inglesby TV. Preparedness for a High-Impact Respiratory Pathogen Pandemic. Johns Hopkins Center for Health Security https://www.centerforhealthsecurity.org/our-work/pubs_archive/pubs-pdfs/2019/190918-GMPBreport-respiratorypathogen.pdf (accessed April 2020).
Khorram‐Manesh 2021 {published data only}
- Khorram-Manesh A, Dulebenets MA, Goniewicz K. Implementing public health strategies-the need for educational initiatives: a systematic review. International Journal of Environmental Research and Public Health 2021;18(11):5888. [DOI: 10.3390/ijerph18115888] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kwok 2020 {published data only}
- Kwok KO, Li KK, Chan HH, Yi YY, Tang A, Wei Wi, et al. Community responses during the early phase of the COVID-19 epidemic in Hong Kong: risk perception, information exposure and preventive measures. Emerging Infectious Diseases 2020;26(7):1575-9. [DOI: 10.3201/eid2607.200500] [DOI] [PMC free article] [PubMed] [Google Scholar]
Li 2020 {published data only}
- Li W, Liao J, Li Q, Baskota M, Wang X, Tang Y, et al. Public health education for parents during the outbreak of COVID-19: a rapid review. Annals of Translational Medicine 2020;8(10):628. [DOI: 10.21037/atm-20-3312] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lim 2020 {published data only}
- Lim JM, Tun ZM, Kumar V, Quaye SED, Offeddu V, Cook AR, et al. Population anxiety and positive behaviour change during the COVID-19 epidemic: cross-sectional surveys in Singapore, China and Italy. Influenza and Other Respiratory Viruses 2021;15(1):45-55. [DOI: 10.1111/irv.12785] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim JM, Tun ZM, Kumar V, Quaye Sharon ED, Offeddu V, Cook AR, et al. Population anxiety and positive behaviour change during the COVID-19 epidemic: cross-sectional surveys in Singapore, China and Italy. medRxiv [Preprint] 2020. [DOI: ] [DOI] [PMC free article] [PubMed]
Lin 2014 {published data only}
- Lin L, Savoia E, Agboola F, Viswanath K. What have we learned about communication inequalities during the H1N1 pandemic: a systematic review of the literature. BMC Public Health 2014;14(1):484. [DOI: 10.1186/1471-2458-14-484] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lohiniva 2020 {published data only}
- Lohiniva AL, Sane J, Sibenberg K, Puumalainen T, Salminen M. Understanding coronavirus disease (COVID-19) risk perceptions among the public to enhance risk communication efforts: a practical approach for outbreaks, Finland, February 2020. Eurosurveillance 2020;25(13):2000317. [DOI: 10.2807/1560-7917.ES.2020.25.13.2000317] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lor 2016 {published data only}
- Lor A, Thomas JC, Barrett DH, Ortmann LW, Guibert D, Herrera J. Key ethical issues discussed at CDC-sponsored international, regional meetings to explore cultural perspectives and contexts on pandemic influenza preparedness and response. International Journal of Health Policy and Management 2016;5(11):653. [DOI: 10.15171/ijhpm.2016.55] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lunn 2020 {published data only}
- Lunn PD, Timmons S, Belton CA, Barjaková M, Julienne H, Lavin C. Motivating social distancing during the Covid-19 pandemic: An online experiment. Social Science & Medicine 2020;265:113478. [DOI: 10.1016/j.socscimed.2020.113478] [DOI] [PubMed] [Google Scholar]
Majid 2020 {published data only}
- Majid U, Wasim A, Bakshi S, Truong J. Knowledge, (mis-)conceptions, risk perception, and behavior change during pandemics: a scoping review of 149 studies. Public Understanding of Science 2020;29(8):777-99. [DOI: 10.1177/0963662520963365] [DOI] [PubMed] [Google Scholar]
Mao 2021 {published data only}
- Mao G, Fernandes-Jesus M, Ntontis E, Drury J. What have we learned about COVID-19 volunteering in the UK? a rapid review of the literature. BMC Public Health 2021;21(1):1470. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Megnin‐Viggars 2020 {published data only}
- Megnin-Viggars O, Carter P, Melendez-Torres GJ, Weston D, Rubin GJ. Facilitators and barriers to engagement with contact tracing during infectious disease outbreaks: a rapid review of the evidence. PLoS One 2020;15(10):e0241473. [DOI: 10.1371/journal.pone.0241473] [DOI] [PMC free article] [PubMed] [Google Scholar]
Meier 2020 {published data only}
- Meier K, Glatz T, Guijt MC, Piccininni M, Meulen M, Atmar K, et al. Public perspectives on social distancing and other protective measures in Europe: a cross-sectional survey study during the COVID-19 pandemic. medRxiv [Preprint] 2020. [DOI: 10.1101/2020.04.02.20049676] [DOI] [PMC free article] [PubMed]
- Meier K, Toivo G, Mathijs CG, Piccininni M, Meulen M, Atmar K, et al. Public perspectives on protective measures during the COVID-19 pandemic in the Netherlands, Germany and Italy: a survey study. PLoS One 2020;15(8):e0236917. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mobasseri 2020 {published data only}
- Mobasseri K, Azami-Aghdash S, Khanijahani A, Khodayari-Zarnaq R. The main Issues and challenges older adults face in the SARS-CoV-2 pandemic: a scoping review of literature. Iranian Journal of Public Health 2020;49(12):2295-2307. [DOI: 10.18502/ijph.v49i12.4810] [DOI] [PMC free article] [PubMed] [Google Scholar]
Moya‐Salazar 2021 {published data only}
- Moya-Salazar J, Cañari B, Gomez-Saenz L, Contreras-Pulache H. Other ways of communicating the pandemic - memes and stickers against COVID-19: a systematic review. F1000Research 2021;10(287):287. [DOI: 10.12688/f1000research.51541.1] [DOI] [PMC free article] [PubMed] [Google Scholar]
NACCHO 2006 {published data only}
- National Association of County, City Health Officials. Local health department guide to pandemic influenza planning. https://stacks.cdc.gov/view/cdc/11439/cdc_11439_DS1.pdf (accessed April 2020).
Noone 2021 {published data only}
- Noone C, Warner NZ, Byrne M, Durand H, Lavoie KL, McGuire BE, et al. A scoping review of research on the determinants of adherence to social distancing measures during the COVID-19 pandemic. Health Psychology Review 2021;15(3):350-70. [DOI: 10.1080/17437199.2021.1934062] [DOI] [PubMed] [Google Scholar]
PHAC 2021 {published data only}
- Public Health Agency of Canada. Individual and community-based measures to mitigate the spread of COVID-19 in Canada. https://open.canada.ca/data/en (accessed 1 March 2022).
PHAC 2021a {published data only}
- Public Health Agency of Canada. COVID-19: advice for gatherings, events and celebrations. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/prevention-risks/private-indoor-gatherings.html (accessed 1st March 2022).
PHAC 2022 {published data only}
- Public Health Agency of Canada. Adjusting public health measures in the context of COVID-19 vaccination. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/adjusting-public-health-measures-vaccination.html (accessed 8th August 2022).
Qazi 2020 {published data only}
- Qazi A, Qazi J, Naseer K, Zeeshan M, Hardaker G, Maitama JZ, et al. Analyzing situational awareness through public opinion to predict adoption of social distancing amid pandemic COVID‐19. Journal of Medical Virology 2020;92(7):849-55. [DOI: 10.1002/jmv.25840] [DOI] [PMC free article] [PubMed] [Google Scholar]
Regmi 2021 {published data only}
- Regmi K, Lwin CM. Factors associated with the implementation of non-pharmaceutical interventions for reducing coronavirus disease 2019 (COVID-19): a systematic review. International Journal of Environmental Research and Public Health 2021;18(8):4274. [DOI: 10.3390/ijerph18084274] [DOI] [PMC free article] [PubMed] [Google Scholar]
Roy 2020 {published data only}
- Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian Journal of Psychiatry 2020;51:102083. [DOI: 10.1016/j.ajp.2020.102083] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sarria‐Guzman 2021 {published data only}
- Sarria-Guzman Y, Fusaro C, Bernal JE, Mosso-Gonzalez C, Erik Gonzalez-Jimenez F, Serrano-Silva N. Knowledge, attitude and practices (KAP) towards COVID-19 pandemic in America: a preliminary systematic review. Journal of Infection in Developing Countries 2021;15(1):9-21. [DOI: 10.3855/jidc.14388] [DOI] [PubMed] [Google Scholar]
Saurabh 2017 {published data only}
- Saurabh S, Prateek S. Role of contact tracing in containing the 2014 ebola outbreak: a review. African Health Sciences 2017;17(1):225-36. [DOI: 10.4314/ahs.v17i1.28] [DOI] [PMC free article] [PubMed] [Google Scholar]
Seale 2020 {published data only}
- Seale H, Dyer CEF, Abdi I, Rahman KM, Sun Y, Qureshi MO, et al. Improving the impact of non-pharmaceutical interventions during COVID-19: examining the factors that influence engagement and the impact on individuals. BMC Infectious Diseases 2020;20(1):607. [DOI: 10.1186/s12879-020-05340-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sopory 2021 {published data only}
- Sopory P, Novak JM, Noyes JP. Quarantine acceptance and adherence: qualitative evidence synthesis and conceptual framework. Journal of Public Health 2021;30(9):2091-101. [DOI: 10.1007/s10389-021-01544-8] [DOI] [PMC free article] [PubMed] [Google Scholar]
Szkwarko 2017 {published data only}
- Szkwarko D, Hirsch-Moverman Y, Du Plessis L, Du Preez K, Carr C, Mandalakas AM. Child contact management in high tuberculosis burden countries: a mixed-methods systematic review. PLoS ONE 2017;12(8):e0182185. [DOI: 10.1371/journal.pone.0182185] [DOI] [PMC free article] [PubMed] [Google Scholar]
Teasdale 2014 {published data only}
- Teasdale E, Santer M, Geraghty AW, Little P, Yardley L. Public perceptions of non-pharmaceutical interventions for reducing transmission of respiratory infection: systematic review and synthesis of qualitative studies. BMC Public Health 2014;14(1):589. [DOI: 10.1186/1471-2458-14-589] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tooher 2013 {published data only}
- Tooher R, Collins JE, Street JM, Braunack‐Mayer A, Marshall H. Community knowledge, behaviours and attitudes about the 2009 H1N1 Influenza pandemic: a systematic review. Influenza and Other Respiratory Viruses 2013;7(6):1316-27. [DOI: 10.1111/irv.12103] [DOI] [PMC free article] [PubMed] [Google Scholar]
Webster 2020 {published data only}
- Webster K, Brooks SK, Smith LE, Woodland L, Wessely S, Rubin GJ. How to improve adherence with quarantine: rapid review of the evidence. Public Health 2020;182:163-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2017 {published data only}
- World Health Organisation. Communicating risk in public health emergencies. A WHO guideline for emergency risk communication (ERC) policy and practice. https://www.who.int/emergencies/risk-communications#:~:text=For%20public%20health%20emergencies%2C%20risk%20communication%20includes%20the,positive%20behaviour%20change%20and%20the%20maintenance%20of%20trust. (accessed April 2020). [PubMed]
WHO 2020 {published data only}
- World Health Organization. Overview of public health and social measures in the context of COVID-19. Interim guidance 18 May 2020. https://www.who.int/publications/i/item/overview-of-public-health-and-social-measures-in-the-context-of-covid-19 (accessed November 1st 2021).
WHO 2020a {published data only}
- World Health Organization. Risk communication and community engagement readiness and initial response for novel coronaviruses (nCoV): interim guidance, 10 January 2020. https://apps.who.int/iris/handle/10665/332301 (accessed November 1st 2021).
WHO 2020b {published data only}
- World Health Organization. Public health considerations for elections and related activities in the context of the COVID-19 pandemic. https://www.who.int/publications/i/item/WHO-2019-nCoV-elections-2020-1 (accessed November 1 2021).
WHO 2020c {published data only}
- World Health Organization. COVID-19 global risk communication and community engagement strategy December 2020 - May 2021: interim guidance, 23 December 2020. https://www.who.int/publications/i/item/covid-19-global-risk-communication-and-community-engagement-strategy (accessed November 2nd 2021).
WHO 2021 {published data only}
- World Health Organization. Actions for consideration in the care and protection of vulnerable population groups for COVID-19. https://apps.who.int/iris/handle/10665/333043 (accessed March 10th 2022).
WHO 2021a {published data only}
- World Health Organization. Considerations for implementing and adjusting public health and social measures in the context of COVID-19: interim guidance, 14 June 2021. https://www.who.int/publications/i/item/considerations-in-adjusting-public-health-and-social-measures-in-the-context-of-covid-19-interim-guidance (accessed November 1st 2021).
WHO 2021b {published data only}
- World Health Organization. Considerations for quarantine of contacts of COVID-19 cases: interim guidance. https://apps.who.int/iris/handle/10665/342004 (accessed November 1st 2021).
Zhong 2020 {published data only}
- Zhong BL, Luo W, Li HM, Zhang QQ, Liu XG, Li WT, et al. Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. International Journal of Biological Sciences 2020;16(10):1745-52. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhu 2020 {published data only}
- Zhu Y, Fu KW, Grepin KA, Liang H, Fung IC. Limited early warnings and public attention to COVID-19 in China, January-February, 2020: a longitudinal cohort of randomly sampled Weibo users. Disaster Medicine & Public Health Preparedness 2020;14(5):e24-e27. [DOI: 10.1017/dmp.2020.68] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies excluded from this review
AASLD 2020 {published data only}
- American Association for the Study of Liver Diseases. Clinical insights for hepatology and liver transplant providers during the COVID-19 pandemic. https://www.aasld.org/news/aasld-releases-clinical-insight-guide-treating-patients-liver-disease-and-covid-19 (accessed 2 November 2021).
Abbas 2021 {published data only}
- Abbas J, Wang D, Su Z, Ziapour A. The role of social media in the advent of COVID-19 pandemic: crisis management, mental health challenges and implications. Risk Management & Healthcare Policy 2021;14:1917-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Adlhoch 2020 {published data only}
- Adlhoch C, Baka A, Cenciarelli O, Penttinen P, Palm D, Plachouras D. Contact tracing: public health management of persons, including healthcare workers, having had contact with COVID-19 cases in the European Union - third update. https://www.ecdc.europa.eu/sites/default/files/documents/covid-19-contact-tracing-public-health-management-third-update.pdf (accessed 2 November 2021).
Allen 2020 {published data only}
- Allen D, Allen JG, Jenkins H, Levinson M. Schools and the path to zero: strategies for pandemic resilience in the face of high community spread. 2020; published online Dec. https://ethics.harvard.edu/schools-and-path-zero (accessed 2 November 2021).
Alom 2021 {published data only}
- Alom S, Chiu CM, Jha A, Lai SHD, Yau THL, Harky A. The effects of COVID-19 on cancer care provision: a systematic review. Cancer Control 2021;28:1073274821997425. [DOI] [PMC free article] [PubMed] [Google Scholar]
Alvarez‐Galvez 2021 {published data only}
- Alvarez-Galvez J, Suarez-Lledo V, Rojas-Garcia A. Determinants of infodemics during disease outbreaks: a systematic review. Frontiers in Public Health 2021;9:603603. [DOI] [PMC free article] [PubMed] [Google Scholar]
Amerio 2020 {published data only}
- Amerio A, Odone A, Marzano L, Costanza A, Aguglia A, Serafini G, et al. Covid-19: the last call for telepsychiatry. Acta Bio-medica: Atenei Parmensis 2020;91(3):e2020050. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andrikopoulos 2020 {published data only}
- Andrikopoulos S, Johnson G. The Australian response to the COVID-19 pandemic and diabetes - lessons learned. Diabetes Research and Clinical Practice 2020;165:108246. [DOI] [PMC free article] [PubMed] [Google Scholar]
Anglemyer 2020 {published data only}
- Anglemyer A, Moore TH, Parker L, Chambers T, Grady A, Chiu K, et al. Digital contact tracing technologies in epidemics: a rapid review. Cochrane Database of Systematic Reviews 2020, Issue 8. Art. No: CD013699. [DOI: 10.1002/14651858.CD013699] [DOI] [PMC free article] [PubMed] [Google Scholar]
Aniceto 2021 {published data only}
- Aniceto NB. Pandemic privilege: a student's perspective. American Journal of Public Health 2021;111(4):582-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
ANZICS 2020 {published data only}
- Australian and New Zealand Intensive Care Society. COVID-19 guidelines version 2 - April 15 2020. https://www.anzics.com.au/anzics-covid-19-guidelines (accessed November 16th 2021).
ANZICS 2020b {published data only}
- Australian and New Zealand Intensive Care Society. COVID-19 guidelines version 3 20 October 2020. https://www.anzics.com.au/anzics-covid-19-guidelines (accessed 16 November 2021).
ASRM 2020 {published data only}
- American Society for Reproductive Medicine. Patient management and clinical recommendations during the coronavirus (COVID-19) pandemic. March 17 2020. https://www.asrm.org/globalassets/asrm/asrm-content/news-and-publications/covid-19/covidtaskforce.pdf (accessed 16 November 2021).
Barry 2013 {published data only}
- Barry MM, Sixsmith J, Infanti JJ. A literature review on effective risk communication for the prevention and control of communicable diseases in Europe. https://www.ecdc.europa.eu/en/publications-data/literature-review-effective-risk-communication-prevention-and-control (accessed 1 November 2021).
Bhaumik 2020 {published data only}
- Bhaumik S, Moola S, Tyagi J, Nambiar D, Kakoti M. Community health workers for pandemic response: a rapid evidence synthesis. BMJ Global Health 2020;5(6):e002769. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bin 2021 {published data only}
- Bin Naeem S, Kamel Boulos MN. COVID-19 misinformation online and health literacy: a brief overview. International Journal of Environmental Research and Public Health 2021;18(15):8091. [DOI: 10.3390/ijerph18158091] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bittencourt 2020 {published data only}
- Bittencourt MS, Generoso G, Melo PHMC, Peixoto D, Miranda EJFP, Mesquita ET, et al. Statement - protocol for the reconnection of cardiology services with patients during the COVID-19 pandemic - 2020. Arquivos Brasileiros de Cardiologia 2020;115(4):776-99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Blasioli 2022 {published data only}
- Blasioli E, Hassini E. E-Health technological ecosystems: advanced solutions to support informal caregivers and vulnerable populations during the COVID-19 outbreak. Telemedicine and e-Health 2022;28(2):138-49. [DOI] [PubMed] [Google Scholar]
Bokolo 2020 {published data only}
- Bokolo A. Use of telemedicine and virtual care for remote treatment in response to COVID-19 pandemic. Journal of Medical Systems 2020;44(7):1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bolcato 2020 {published data only}
- Bolcato M, Aurilio MT, Aprile A, Di Mizio G, Della Pietra B, Feola A. Take-home messages from the COVID-19 pandemic: strengths and pitfalls of the Italian national health service from a medico-legal point of view. Healthcare 2020;9:17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bonell 2020 {published data only}
- Bonell C, Michie S, Reicher S, West R, Bear L, Yardley L, et al. Harnessing behavioural science in public health campaigns to maintain ‘social distancing’in response to the COVID-19 pandemic: key principles. Journal of Epidemiology and Community Health 2020;74(8):617-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Boschiero 2021 {published data only}
- Boschiero MN, Capasso Palamim CV, Ortega MM, Mauch RM, Lima Marson FA. One year of coronavirus disease 2019 (Covid-19) in Brazil: a political and social overview. Annals of Global Health 2021;87(1):44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bouznad 2020 {published data only}
- Bouznad S, Ibourk A. School closures, equality of opportunity: some recommendations. Revista Romaneasca Pentru Educatie Multidimensionala 2020;12(2):103-10. [Google Scholar]
Braithwaite 2020 {published data only}
- Braithwaite I, Callender T, Bullock M, Aldridge RW. Automated and partially-automated contact tracing: a rapid systematic review to inform the control of COVID-19. Lancet Digital Health 2020;2(11):e607-e621. [DOI: 10.1016/S2589-7500(20)30184-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Brooks 2021 {published data only}
- Brooks SK, Greenberg N, Wessely S, Rubin GJ. Factors affecting healthcare workers’ compliance with social and behavioural infection control measures during emerging infectious disease outbreaks: rapid evidence review. BMJ Open 2021;11(8):e049857. [DOI] [PMC free article] [PubMed] [Google Scholar]
Busa 2021 {published data only}
- Busa F, Bardanzellu F, Pintus MC, Fanos V, Marcialis MA. COVID-19 and school: to open or not to open, that is the question. The first review on current knowledge. Pediatric Reports 2021;13(2):257-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cachon‐Zagalaz 2020 {published data only}
- Cachon-Zagalaz J, Sanchez-Zafra M, Sanabrias-Moreno D, Gonzalez-Valero G, Lara-Sanchez AJ, Zagalaz-Sanchez ML. Systematic review of the literature about the effects of the COVID-19 pandemic on the lives of school children. Frontiers in Psychology 2020;11:569348. [DOI: 10.3389/fpsyg.2020.569348] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carter 2021 {published data only}
- Carter P, Megnin-Viggars O, Rubin GJ. What factors influence symptom reporting and access to healthcare during an emerging infectious disease outbreak? A rapid review of the evidence. Health Security 2021;19(4):353-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
CDC 2020 {published data only}
- Centers for Disease Control and Prevention. Operating schools during COVID-19: CDC considerations. https://stacks.cdc.gov/view/cdc/92308 (accessed November 16th 2021).
CDC 2020a {published data only}
- Centers for Disease Control and Prevention. Interim guidance: get your mass gatherings or large community events ready for Coronavirus disease 2019 (COVID-19). https://stacks.cdc.gov/view/cdc/85893 (accessed November 2nd 2021);March 15 2020.
CDC 2020b {published data only}
- Centers for Disease Control and Prevention. Standard Operating Procedure (SOP) for triage of suspected COVID-19 patients in non-US healthcare settings: early identification and prevention of transmission during triage. Updated 2021. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/sop-triage-prevent-transmission.html (accessed November 2nd 2021);July 14th 2021.
CDC 2020c {published data only}
- Centers for Disease Control and Prevention. Additional considerations for the use of masks among K12 students: coronavirus disease 2019 (COVID-19) factsheet. https://www.cdc.gov/coronavirus/2019-ncov/downloads/community/CFC_Guide_for_School_Administrators.pdf (accessed November 17th 2021).
CDC 2020d {published data only}
- Centers for Disease Control and Prevention. Considerations for school closure. https://www.cdc.gov/coronavirus/2019-ncov/community/index.html (accessed November 16th 2021).
CDC 2020e {published data only}
- Centers for Disease Control and Prevention. COVID-19 and cooling centers. https://www.cdc.gov/coronavirus/2019-ncov/php/cooling-center.html (accessed November 17th 2021).
CDC 2020f {published data only}
- Centers for Disease Control and Prevention. Preventing the spread of COVID-19 in a variety of settings throughout your community: guidance about preventing COVID-19 infections in diverse settings. https://www.cdc.gov/coronavirus/2019-ncov/php/infection-control.html (accessed November 2nd 2021).
CDC 2020g {published data only}
- Centers for Disease Control and Prevention. Guidance for administrators in parks and recreational facilities. https://stacks.cdc.gov/view/cdc/96157 (accessed November 17th 2021).
CDC 2020h {published data only}
- Centers for Disease Control and Prevention. What law enforcement personnel need to know about coronavirus disease 2019 (COVID-19). https://stacks.cdc.gov/view/cdc/85653 (accessed 2 November 2021).
CDC 2020i {published data only}
- Centers for Disease Control and Prevention. Preventing the spread of COVID-19 in retirement communities and independent living facilities (interim guidance). https://www.cdc.gov/coronavirus/2019-ncov/downloads/guidance-retirement-communities.pdf (accessed November 2nd 2021).
CDC 2020j {published data only}
- Centers for Disease Control and Prevention. COVID-19 considerations for traveling amusement parks and carnivals. https://stacks.cdc.gov/view/cdc/96189 (accessed November 2nd 2021).
CDC 2020k {published data only}
- Centers for Disease Control and Prevention. COVID-19 critical infrastructure sector response planning. https://stacks.cdc.gov › cdc › cdc_97252_DS1 (accessed November 17th 2021).
CDC 2020l {published data only}
- Centers for Disease Control and Prevention. Guidance for large or extended families living in the same household. https://stacks.cdc.gov/view/cdc/98341 (accessed November 2nd 2021).
CDC 2020n {published data only}
- Centers for Disease Control and Prevention. Considerations for memory care units in long-term care facilities. Updated May 12, 2020. https://public4.pagefreezer.com/browse/CDC%20Covid%20Pages/11-05-2022T12:30/https://www.cdc.gov/coronavirus/2019-ncov/hcp/memory-care.html (accessed November 17th 2021).
CDC 2020o {published data only}
- Centers for Disease Control and Prevention. Considerations for preventing spread of COVID-19 in assisted living facilities. https://www. cdc. gov/coronavirus/2019-ncov/hcp/assisted-living. html (accessed November 23 2021).
CDC 2020p {published data only}
- Centers for Disease Control and Prevention. COVID-19 guidance for shared or congregate housing. https://stacks.cdc.gov/view/cdc/87266 (accessed 23rd November 2021).
CDC 2020q {published data only}
- Centers for Disease Control and Prevention. Guidance for K-12 school administrators on the use of masks in schools. https://stacks.cdc.gov/view/cdc/98906 (accessed November 23rd 2021).
CDC 2020r {published data only}
- Centers for Disease Control and Prevention. Interim guidance for syringe services programs. https://public4.pagefreezer.com/browse/CDC%20Covid%20Pages/19-04-2022T12:28/https://www.cdc.gov/coronavirus/2019-ncov/php/syringe-service-programs.html (accessed 2nd November 2021).
CDC 2020s {published data only}
- Centers for Disease Control and Prevention. Interim recommendations for emergency medical services (EMS) systems and 911 public safety answering points/emergency communication centers (PSAP/ECCs) in the United States during the coronavirus disease (COVID-19) pandemic. https://stacks.cdc.gov/view/cdc/90581 (accessed November 2nd 2021).
CDC 2020t {published data only}
- Centers for Disease Control and Prevention. Markets: operational considerations for COVID-19 mitigation measures in low resource settings. https://stacks.cdc.gov/view/cdc/91489 (accessed November 23rd 2021).
CDC 2020u {published data only}
- Centers for Disease Control and Prevention. Using telehealth to expand access to essential health services during the COVID-19 pandemic. https://public4.pagefreezer.com/browse/CDC%20Covid%20Pages/11-05-2022T12:30/https://www.cdc.gov/coronavirus/2019-ncov/hcp/telehealth.html (accessed November 23rd 2021).
CDC 2020v {published data only}
- Centers for Disease Control and Prevention. Protecting seafood processing workers from COVID-19. https://stacks.cdc.gov/view/cdc/96190 (accessed November 16th 2021).
CDC 2020w {published data only}
- Centers for Disease Control and Prevention. How to mitigate COVID-19 transmission in densely populated areas globally. https://stacks.cdc.gov/view/cdc/95858 (accessed November 2nd 2021).
CDC 2020x {published data only}
- Centers for Disease Control and Prevention. Interim infection control guidance for public health personnel evaluating persons under investigation (PUIs) and asymptomatic close contacts of confirmed cases at their home or non-home residential settings. https://stacks.cdc.gov/view/cdc/85936 (accessed November 17th 2021).
CDC 2021 {published data only}
- Public Health Agency of Canada. COVID-19 guidance for schools Kindergarten to Grade 12. URL 2021 version not available. 2022 update avaiable at: https://www.cdc.gov/coronavirus/2019-ncov/community/schools-childcare/k-12-guidance.html#physical-distancing (accessed November 16th 2021).
CDC 2021a {published data only}
- Centers for Disease Control and Prevention. Operational strategy for K-12 schools through phased prevention. https://stacks.cdc.gov/view/cdc/106255 (accessed November 16th 2021).
CDC 2021aa {published data only}
- Control Centers for Disease. Considerations for aquatic venues. URL not available Archived.
CDC 2021ab {published data only}
- Control Centers for Disease, Prevention. Considerations for institutions of higher education. stacks.cdc.gov/view/cdc/96143 (accessed November 1 2021).
CDC 2021ac {published data only}
- Control Centers for Disease, Prevention. CDC’s interim guidance for general population disaster shelters during the COVID-19 pandemic. https://www.cdc.gov/coronavirus/2019-ncov/php/eh-practitioners/general-population-disaster-shelters.html (accessed November 23rd 2021).
CDC 2021ad {published data only}
- Centers for Disease Control and Prevention. Considerations for community-based organizations. https://stacks.cdc.gov/view/cdc/96195 (accessed November 2nd 2021).
CDC 2021ae {published data only}
- Centers for Disease Control and Prevention. Considerations for non-emergency vehicle transportation for tribal communities during COVID-19. https://www.cdc.gov/coronavirus/2019-ncov/community/tribal/non-ems-transportation.html (accessed November 2nd 2021).
CDC 2021af {published data only}
- Centers for Disease Control and Prevention. Considerations for restaurant and bar operators. URL 2021 guidance unavailable (accessed November 16th 2021).
CDC 2021ag {published data only}
- Centers for Disease Control and Prevention. Interim guidance for homeless service providers to plan and respond to coronavirus disease 2019 (COVID-19). https://stacks.cdc.gov/view/cdc/106928 (accessed November 23rd 2021).
CDC 2021ah {published data only}
- Centers for Disease Control and Prevention. Interim guidance on unsheltered homelessness and coronavirus disease 2019 (COVID-19) for homeless service providers and local officials. URL 2021 version unavailable (accessed November 24th 2021).
CDC 2021ai {published data only}
- Centers for Disease Control and Prevention. Interim guidance on people experiencing unsheltered homelessness. https://stacks.cdc.gov/view/cdc/107838 (accessed November 24th 2021).
CDC 2021aj {published data only}
- Centers for Disease Control and Prevention. Investigating and responding to COVID-19 cases at homeless service provider sites. URL for 2021 version not available (accessed November 22nd 2021).
CDC 2021ak {published data only}
- Centers for Disease Control and Prevention. Manufacturing workers and employers. URL 2021 version not available (accessed November 2nd 2021).
CDC 2021al {published data only}
- Centers for Disease Control and Prevention. Providing care and treatment for people living with HIV in low-resource non-US settings during COVID-19 pandemic. https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/maintaining-essential-HIV-services.html (accessed November 17th 2021).
CDC 2021am {published data only}
- Centers for Disease Control and Prevention. Safe watering points during COVID-19. https://stacks.cdc.gov/view/cdc/89691 (accessed November 16th 2021).
CDC 2021an {published data only}
- Centers for Disease Control and Prevention. Interim guidance for SARS-CoV-2 testing and screening at institutions of higher education (IHEs). URL not available (accessed November 16th 2021).
CDC 2021ao {published data only}
- Centers for Disease Control and Prevention. What bus transit operators need to know about COVID-19. URL June 2021 not available (accessed November 17th 2021).
CDC 2021ap {published data only}
- Centers for Disease Control and Prevention. COVID-19 overview and infection prevention and control priorities in non-US healthcare settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/non-us-settings/overview/index.html (accessed November 2nd 2021).
CDC 2021aq {published data only}
- Centers for Disease Control and Prevention. Guidance and tips for tribal community living during COVID-19. URL 2021 advice not available (accessed November 23rd 2021).
CDC 2021ar {published data only}
- Centers for Disease Control and Prevention. Operational considerations for schools. https://stacks.cdc.gov/view/cdc/107218 (accessed November 2nd 2021).
CDC 2021b {published data only}
- Centers for Disease Control and Prevention. Operational considerations for adapting a contact tracing program to respond to the COVID-19 pandemic in non-US settings. https://www.cdc.gov/coronavirus/2019-ncov/downloads/global-covid-19/operational-considerations-contact-tracing.pdf (accessed November 16th 2021).
CDC 2021c {published data only}
- Centers for Disease Control and Prevention. Performing broad-based testing for SARS-CoV-2 in congregate correctional, detention, and homeless service settings. https://www.cdc.gov/coronavirus/2019-ncov/hcp/broad-based-testing.html (accessed November 2nd 2021).
CDC 2021d {published data only}
- Centers for Disease Control and Prevention. Contact tracing for COVID-19. URL no longer available (accessed November 2nd 2021).
CDC 2021e {published data only}
- Centers for Disease Control and Prevention. Guidance for organizing large events and gatherings. https://stacks.cdc.gov/view/cdc/104842 (accessed November 9th 2021).
CDC 2021m {published data only}
- Centers for Disease Control and Prevention. Agriculture workers and employers. https://stacks.cdc.gov/view/cdc/107141 (accessed November 16th 2021).
CDC 2021n {published data only}
- Centers for Disease Control and Prevention. Considerations for communities of faith. https://stacks.cdc.gov/view/cdc/98788 (accessed November 2nd 2021).
CDC 2021o {published data only}
- Centers for Disease Control and Prevention. Guidance for general population disaster shelters during a pandemic. https://www.cdc.gov/disasters/general-population-shelters-guidance.html (accessed November 16th 2021).
CDC 2021p {published data only}
- Centers for Disease Control and Prevention. Interim infection prevention and control recommendations for healthcare personnel during the coronavirus disease 2019 (COVID-19) pandemic. https://stacks.cdc.gov/view/cdc/109674 (accessed November 30th 2021).
CDC 2021q {published data only}
- Centers for Disease Control and Prevention. Operational considerations for community isolation centers for COVID-19 in low-resource settings. URL not available for 2021 advice (accessed November 2nd 2021).
CDC 2021s {published data only}
- Centers for Disease Control and Prevention. Operational considerations for the identification of healthcare workers and inpatients with suspected COVID-19 in non-US healthcare settings. https://stacks.cdc.gov/view/cdc/104355 (accessed November 16th 2021).
CDC 2021t {published data only}
- Centers for Disease Control and Prevention. Cleaning and disinfecting your facility: every day and when someone is sick. https://www.cdc.gov/coronavirus/2019-ncov/community/disinfecting-building-facility.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fcoronavirus%2F2019-ncov%2Fcommunity%2Freopen-guidance.html (accessed November 2nd 2021).
CDC 2021u {published data only}
- Centers for Disease Control and Prevention. Strategies for protecting K-12 school staff from COVID-19. https://stacks.cdc.gov/view/cdc/95771 (accessed November 2nd 2021).
CDC 2021v {published data only}
- Centers for Disease Control and Prevention. Strategies to mitigate healthcare personnel staffing shortages. URL to March 2021 version no longer active (accessed November 16th 2021).
CDC 2021w {published data only}
- Centers for Disease Control and Prevention. Interim Guidance for Businesses and Employers Responding to Coronavirus Disease 2019 (COVID-19), May 2020. URL no longer available (accessed 24 November 2021).
CDC 2021x {published data only}
- Centers for Disease Control and Prevention. Interim public health recommendations for fully vaccinated people. https://stacks.cdc.gov/view/cdc/110779 (accessed November 16th 2021).
CDC 2021y {published data only}
- Centers for Disease Control and Prevention. Mitigation measures for COVID-19 in households and markets in non-US low-resource settings. https://www.cdc.gov/coronavirus/2019-ncov/global-covid-19/global-urban-areas.html (accessed November 2nd 2021).
CDC 2021z {published data only}
- Centers for Disease Control and Prevention. Interim guidance on management of coronavirus disease 2019 (COVID-19) in correctional and detention facilities. https://stacks.cdc.gov/view/cdc/107037 (accessed November 17th 2021).
Chackalackal 2021 {published data only}
- Chackalackal DJ, Al-Aghbari AA, Jang SY, Ramirez TR, Vincent J, Joshi A, et al. The Covid-19 pandemic in low-and middle-income countries, who carries the burden? Review of mass media and publications from six countries. Pathogens and Global Health 2021;115(3):178-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chan 2020 {published data only}
- Chan EY, Shahzada TS, Sham TST, Dubois C, Huang Z, Liu S, et al. Narrative review of non-pharmaceutical behavioural measures for the prevention of COVID-19 (SARS-CoV-2) based on the Health-EDRM framework. British Medical Bulletin 2020;136(1):46-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
Chawla 2020 {published data only}
- Chawla D, Chirla D, Dalwai S, Deorari AK, Ganatra A, Gandhi Al, et al. Perinatal-neonatal management of COVID-19 infection—guidelines of the Federation of Obstetric and Gynaecological Societies of India (FOGSI), National Neonatology Forum of India (NNF), and Indian Academy of Pediatrics (IAP). Indian Pediatrics 2020;57(6):536-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
Choukou 2021 {published data only}
- Choukou MA, Taha A, Qadeer A, Monnin C. Digital health technology for remote care in response to the COVID-19 pandemic: a scoping review. European Review for Medical and Pharmacological Sciences 2021;25(8):3386-94. [DOI] [PubMed] [Google Scholar]
Cobb 2021 {published data only}
- Cobb NA, Pisani L, Schultz MJ, Ferreira JC. Pragmatic recommendations for infection prevention and control practices for healthcare facilities in low-and middle-income countries during the COVID-19 pandemic. The American Journal of Tropical Medicine and Hygiene 2021;104(3 Suppl):25. [DOI] [PMC free article] [PubMed] [Google Scholar]
Collins 2020 {published data only}
- Collins Montgomery E, Tam PI, Trehan I, Cartledge P, Bose A, Lanaspa M, et al. Strengthening health systems and improving the capacity of pediatric care centers to respond to epidemics, such as COVID-19 in resource-limited settings. Journal of Tropical Pediatrics 2020;66(4):357-65. [DOI] [PMC free article] [PubMed]
Couto 2020a {published data only}
- Couto KC, Lorenzo FM, Tagliabue M, Henriques MB, Lemos RF. Underlying principles of a Covid-19 behavioral vaccine for a sustainable cultural change. International Journal of Environmental Research and Public Health 2020;17(23):9066. [DOI] [PMC free article] [PubMed] [Google Scholar]
Daszak 2021 {published data only}
- Daszak P, Keusch GT, Phelan AL, Johnson CK, Osterholm MT. Infectious disease threats: a rebound to resilience. Health Affairs 2021;40(2):204-11. [DOI] [PubMed] [Google Scholar]
DEHS 2020 {published data only}
- The Department of Environmental Health Services (DEHS), Government of The Bahamas. Reopening guidance for cleaning and disinfecting public spaces, workplaces, businesses, schools, and homes. https://76e8ca5c-b0d6-41c1-a80e-fa1785909945.filesusr.com/ugd/e822df_eacfc515e534400390a38c2f012352b8.pdf (accessed November 2nd 2021).
Deolmi 2020 {published data only}
- Deolmi M, Pisani F. Psychological and psychiatric impact of COVID-19 pandemic among children and adolescents. Acta Biomedica 2020;91(4):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
DES 2020a {published data only}
- Department of Education and Skills Ireland. Framework to maintain physical distancing in the classroom in post primary schools with a full return of all students for the 2020/21 school year. https://assets.gov.ie/83472/ca0e3029-2d43-4e77-8181-bc3dc89455d2.pdf (accessed November 17th 2021).
DES 2020b {published data only}
- Department of Education and Skills Ireland. Returning to school Guidance on learning and school programmes for post-primary school leaders and teachers. https://www.gov.ie/en/publication/63fc3-returning-to-school-guidance-on-learning-and-school-programmes-for-post-primary-school-leaders-and-teachers/ July 2020;(accessed November 22nd 2021).
Desveaux 2021 {published data only}
- Desveaux L, Mosher R, Buchan JL. Behavioural science principles for enhancing adherence to public health measures. Science Briefs of the Ontario COVID-19 Science Advisory Table 2021;2:24. [Google Scholar]
DFE 2021 {published data only}
- Department for Education, UK. Restricting attendance during the national lockdown: schools: guidance for all schools in England. https://dera.ioe.ac.uk/37041/ (accessed November 2nd 2021).
Dhamija 2021 {published data only}
- Dhamija RK, Srivastava A, Chauhan S, Shah U, Nagda T, Palande D, et al. Consensus statement on neurorehabilitation during COVID-19 times: Expert group on behalf of the Indian Federation of Neurorehabilitation (IFNR). Annals of Indian Academy of Neurology 2021;24(2):138-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
DHCS 2021 {published data only}
- Government of Newfoundland and Labrador, Department of Health and Community Services, Public Health Division. COVID-19 Variant of Concern: Case, Contact and Outbreak Management Interim Guidance. https://www.gov.nl.ca/covid-19/files/Measures-for-COVID-19-Variants-of-Concern-Case-Contact-and-Outbreak-Management-Interim-Guidance-for-Newfoundland-and-Labrador-1.pdf (accessed November 17th 2021).
DiLorenzo 2021 {published data only}
- DiLorenzo MA, O’Connor SK, Ezekwesili C, Sampath S, Zhao M, Yarrington C, et al. COVID‐19 guidelines for pregnant women and new mothers: A systematic evidence review. International Journal of Gynaecology and Obstetrics 2021;153(3):373-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dos Santos 2020 {published data only}
- Dos Santos JLG, Stein Messetti PA, Adami F, Bezerra IMP, Maia PCGGS, Tristan-Cheever E, et al. Collision of fundamental human rights and the right to health access during the novel Coronavirus pandemic. Frontiers in Public Health 2020;8:570243. [DOI] [PMC free article] [PubMed] [Google Scholar]
Downes 2020 {published data only}
- Downes KJ, Danziger-Isakov LA, Cousino MK, Green M, Michaels MG, Muller WJ, et al. Return to school for pediatric solid organ transplant recipients in the United States during the coronavirus disease 2019 pandemic: expert opinion on key considerations and best practices. Journal of the Pediatric Infectious Diseases Society 2020;9(5):551-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dubey 2020 {published data only}
- Dubey S, Biswas P, Ghosh R, Dubey MJ, Chatterjee S, Lahiri D, et al. Psychosocial impact of COVID-19. Diabetes and Metabolic Syndrome: Clinical Research and Reviews 2020;14(5):779-88. [DOI] [PMC free article] [PubMed] [Google Scholar]
EC 2020 {published data only}
- European Commission. Staying safe from COVID-19 during winter. https://ec.europa.eu/commission/presscorner/detail/en/ip_20_2254 (accessed November 17th 2021).
ECDC 2020c {published data only}
- European Center for Disease Prevention and Control. Guidelines for the use of non-pharmaceutical measures to delay and mitigate the impact of 2019-nCoV. https://www.ecdc.europa.eu/sites/default/files/documents/novel-coronavirus-guidelines-non-pharmaceutical-measures_0.pdf (accessed November 16th 2021).
ECDC 2020d {published data only}
- European Centre for Disease Prevention and Control. COVID-19 Rail Protocol: Recommendations for safe resumption of railway services in Europe. https://www.ecdc.europa.eu/sites/default/files/documents/Covid-19-Rail-Protocol_v1.4.pdf (accessed November 17th 2021).
ECDC 2020e {published data only}
- European Centre for Disease Prevention and Control. Infection prevention and control in the household management of people with suspected or confirmed coronavirus disease (COVID-19). https://www.ecdc.europa.eu/sites/default/files/documents/Home-care-of-COVID-19-patients-2020-03-31.pdf (accessed November 16th 2021).
ECDC 2020f {published data only}
- European Centre for Disease Prevention and Control. Guidelines for the implementation of nonpharmaceutical interventions against COVID-19. https://www.ecdc.europa.eu/en/publications-data/covid-19-guidelines-non-pharmaceutical-interventions (accessed November 2nd 2021).
Ekberg 2020 {published data only}
- Ekberg S, Parry R, Land V, Ekberg K, Pino M, Antaki C. Communicating with patients and families about difficult matters: a rapid review in the context of the COVID-19 pandemic. medRxiv [Preprint] 2020. [DOI: ]
EMSA 2021 {published data only}
- European Maritime Safety Agency. COVID 19: EU guidance for cruise ship operations. Guidance on the gradual and safe resumption of operations of cruise ships in the European Union in relation to the COVID-19 pandemic. https://www.emsa.europa.eu/publications/inventories/item/4273-covid-19-eu-guidance-for-cruise-ship-operations.html (accessed 2 November 2021).
Feiz 2020 {published data only}
- Feiz Arefi M, Babaei-Pouya A, Poursadeqiyan M. The health effects of quarantine during the COVID-19 pandemic. Work 2020;67(3):523-7. [DOI] [PubMed] [Google Scholar]
Ferreira 2020 {published data only}
- Ferreira LL, Sampaio DL, Chagas ACP, Guimaraes HP, Hajjar LA, Lobo SMA, et al. AMB Guidelines: COVID -19. Revista Da Associacao Medica Brasileira 2020;66(Suppl 2):17-21. [DOI] [PubMed] [Google Scholar]
Finset 2020 {published data only}
- Finset A, Bosworth H, Butow P, Gulbrandsen P, Hulsman RL, Pieterse AH, et al. Effective health communication–a key factor in fighting the COVID-19 pandemic. Patient Education and Counseling 2020;103(5):873. [DOI] [PMC free article] [PubMed] [Google Scholar]
Flores 2020 {published data only}
- Flores J, Clancy D. Class dismissed: Massachusetts' lack of preparedness for K-12 digital learning during COVID-19. White Paper No. 208. Pioneer Institute for Public Policy Research, https://files.eric.ed.gov/fulltext/ED605641.pdf (accessed April 2020).
Flumignan 2020 {published data only}
- Flumignan RLG, Nakano LCU, Pascoal PIF, Santos BCD, Correia RM, Silveira BP, et al. Evidence from Cochrane systematic reviews for controlling the dissemination of COVID-19 infection. A narrative review. Sao Paulo Medical Journal 2020;138(4):336-44. [DOI: 10.1590/1516-3180.2020.029105062020] [DOI] [PMC free article] [PubMed] [Google Scholar]
Geerts 2021 {published data only}
- Geerts JM, Kinnair D, Taheri P, Abraham A, Ahn J, Atun R, et al. Guidance for health care leaders during the recovery stage of the COVID-19 pandemic: a consensus statement. JAMA Network Open 2021;4(7):e2120295-e2120295. [DOI] [PubMed] [Google Scholar]
Gelfand 2021 {published data only}
- Gelfand JM, Armstrong AW, Bell S, Anesi GL, Blauvelt A, Calabrese C, et al. National Psoriasis Foundation COVID-19 Task Force guidance for management of psoriatic disease during the pandemic: Version 2—Advances in psoriatic disease management, COVID-19 vaccines, and COVID-19 treatments. Journal of the American Academy of Dermatology 2021;84(5):1254-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ghate 2020 {published data only}
- Ghate S, Parekh BJ, Thapar RK, Nadkarni PR, Sen S, Bansal U, et al. Indian Academy of Pediatrics guidelines on school reopening, remote learning and curriculum in and after the COVID-19 pandemic. Indian Pediatrics 2020;57(12):1153-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
Government Ireland 2021 {published data only}
- Government of Ireland. Work safely protocol COVID-19 specific national protocol for employers and workers. https://www.lenus.ie/handle/10147/627678?show=full (accessed November 17th 2021).
Graber 2021 {published data only}
- Graber KM, Byrne EM, Goodacre EJ, Kirby N, Kulkarni K, O'Farrelly C, et al. A rapid review of the impact of quarantine and restricted environments on children's play and the role of play in children's health. Child: Care, Health and Development 2021;47(2):143-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Greysen 2021 {published data only}
- Greysen SR, Auerbach AD, Mitchell MD, Goldstein JN, Weiss R, Esmaili A, et al. Discharge practices for COVID-19 patients: rapid review of published guidance and synthesis of documents and practices at 22 US academic medical centers. Journal of General Internal Medicine 2021;36(6):1715-21. [DOI: 10.1007/s11606-021-06711-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Griffin 2021 {published data only}
- Griffin M, Sohrabi C, Alsafi Z, Nicola M, Kerwan A, Mathew G, et al. Preparing for COVID-19 exit strategies. Annals of Medicine and Surgery 2021;61:88-92. [DOI: 10.1016/j.amsu.2020.12.012] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hagan 2020 {published data only}
- Hagan JE, Ahinkorah BO, Seidu AA, Ameyaw EK, Schack T. Africa's COVID-19 situation in focus and recent happenings: a mini review. Frontiers in Public Health 2020;8:573636. [DOI: 10.3389/fpubh.2020.573636] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hamouche 2021 {published data only}
- Hamouche S. Covid-19, physical distancing in the workplace and employees mental health: implications and insights for organizational interventions-narrative review. Psychiatria Danubina 2021;33(2):202-8. [DOI: 10.24869/psyd.2021.202] [DOI] [PubMed] [Google Scholar]
Hirt 2022 {published data only}
- Hirt J, Janiaud P, Hemkens LG. Randomized trials on non-pharmaceutical interventions for COVID-19: a scoping review. BMJ Evidence-Based Medicine 2022;27:334-44. [DOI: 10.1136/bmjebm-2021-111825] [DOI] [PMC free article] [PubMed] [Google Scholar]
Honein 2020 {published data only}
- Honein MA, Christie A, Rose DA, Brooks JT, Meaney-Delman D, Cohn A, et al. Summary of guidance for public health strategies to address high levels of community transmission of SARS-CoV-2 and related deaths, December 2020. MMWR - Morbidity & Mortality Weekly Report 2020;69(49):1860-67. [DOI: 10.15585/mmwr.mm6949e2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Horcher 2021 {published data only}
- Horcher D, Singh R, Graham DJ. Social distancing in public transport: mobilising new technologies for demand management under the Covid-19 crisis. Transportation 2021;49:735-64. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hossain 2020 {published data only}
- Hossain MM, Sultana A, Purohit N. Mental health outcomes of quarantine and isolation for infection prevention: a systematic umbrella review of the global evidence. Epidemiology and Health 2020;42:e2020038. [DOI: 10.4178/epih.e2020038] [DOI] [PMC free article] [PubMed] [Google Scholar]
IASC 2020 {published data only}
- Inter-Agency Standing Committee (UNICEF, WHO, IFRC). Interim guidance for COVID-19 prevention and control in schools. https://www.wfp.org/publications/interim-guidance-covid-19-prevention-and-control-schools (accessed November 2nd 2021).
Iezadi 2021 {published data only}
- Iezadi S, Gholipour K, Azami-Aghdash S, Ghiasi A, Rezapour A, Pourasghari H, et al. Effectiveness of non-pharmaceutical public health interventions against COVID-19: a systematic review and meta-analysis. PLoS ONE [Electronic Resource] 2021;16(11):e0260371. [DOI: 10.1371/journal.pone.0260371] [DOI] [PMC free article] [PubMed] [Google Scholar]
Imtiaz 2020 {published data only}
- Imtiaz Memon R, Imran N, Aamer I, Imran Sharif M, Hassan Bodla Z, Naveed S. 1.16 The effect of quarantine on the emotional well-being of kids: a systematic review. Journal of the American Academy of Child and Adolescent Psychiatry 2020;59 (10 Supplement):S144. [Google Scholar]
Jammu 2021 {published data only}
- Jammu AS, Chasen MR, Lofters AK, Bhargava R. Systematic rapid living review of the impact of the COVID-19 pandemic on cancer survivors: update to August 27, 2020. Supportive Care in Cancer 2021;29(6):2841-50. [DOI: 10.1007/s00520-020-05908-w] [DOI] [PMC free article] [PubMed] [Google Scholar]
Jesus 2021 {published data only}
- Jesus TS, Bhattacharjya S, Papadimitriou C, Bogdanova Y, Bentley J, Arango-Lasprilla JC, et al. Lockdown-related disparities experienced by people with disabilities during the first wave of the COVID-19 pandemic: scoping review with thematic analysis. International Journal of Environmental Research and Public Health 2021;18(12):6178. [DOI: 10.3390/ijerph18126178] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johansen 2020 {published data only}
- Johansen TB, Astrup E, Jore S, Nilssen H, Dahlberg BB, Klingenberg C, et al. Infection prevention guidelines and considerations for paediatric risk groups when reopening primary schools during COVID-19 pandemic, Norway, April 2020. Eurosurveillance 2020;25(22):2000921. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kamposioras 2020 {published data only}
- Kamposioras K, Mauri D, Papadimitriou K, Anthoney A, Hindi N, Petricevic B, et al. Synthesis of recommendations from 25 countries and 31 oncology societies: how to navigate through Covid-19 labyrinth. Frontiers in Oncology 2020;10:575148. [DOI: 10.3389/fonc.2020.575148] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kondylakis 2020 {published data only}
- Kondylakis H, Katehakis DG, Kouroubali A, Logothetidis F, Triantafyllidis A, Kalamaras I, et al. COVID-19 mobile apps: a systematic review of the literature. Journal of Medical Internet Research 2020;22(12):e23170. [DOI: 10.2196/23170] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kumar 2020 {published data only}
- Kumar R, Nedungalaparambil NM, Mohanan N. Emergency and primary care collaboration during COVID-19 pandemic: a quick systematic review of reviews. Journal of Family Medicine and Primary Care 2020;9(8):3856-62. [DOI: 10.4103/jfmpc.jfmpc_755_20] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kunzler 2021 {published data only}
- Kunzler AM, Roethke N, Guenthner L, Stoffers-Winterling J, Tuescher O, Coenen M, et al. Mental burden and its risk and protective factors during the early phase of the SARS-CoV-2 pandemic: systematic review and meta-analyses. Globalization and Health 2021;17(1):1-29. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kurniawan 2021 {published data only}
- Kurniawan A, Halim DA, Sutandyo N. Multiple myeloma management in COVID-19 era. Asian Journal of Oncology 2021;7(1):1-7. [DOI: 10.1055/s-0040-1716813] [DOI] [Google Scholar]
Lal 2020 {published data only}
- Lal A, Ashworth HC, Dada S, Hoemeke L, Tambo E. Optimizing pandemic preparedness and response through health information systems: lessons learned from Ebola to COVID-19. Disaster Medicine & Public Health Preparedness 2020;16(1):333-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
Landewe 2020 {published data only}
- Landewe RBM, MacHado PM, Kroon F, Bijlsma HWJ, Burmester GR, Carmona L, et al. EULAR provisional recommendations for the management of rheumatic and musculoskeletal diseases in the context of SARS-CoV-2. Annals of the Rheumatic Diseases 2020;79(7):851-58. [DOI] [PubMed] [Google Scholar]
Lebrasseur 2021 {published data only}
- Lebrasseur A, Fortin-Bedard N, Lettre J, Bussieres EL, Best K, Boucher N, et al. Impact of COVID-19 on people with physical disabilities: a rapid review. Disability and Health Journal 2021;14(1):101014. [DOI: 10.1016/j.dhjo.2020.101014] [DOI] [PMC free article] [PubMed] [Google Scholar]
Leon Singh 2020 {published data only}
- Leon Singh HJ, Couch D, Yap K. Mobile health apps that help with COVID-19 management: scoping review. JMIR Nursing 2020;3(1):e20596. [DOI: 10.2196/20596] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lo 2020 {published data only}
- Lo Moro G, Sinigaglia T, Bert F, Savatteri A, Gualano MR, Siliquini R. Reopening schools during the COVID-19 pandemic: overview and rapid systematic review of guidelines and recommendations on preventive measures and the management of cases. International Journal of Environmental Research and Public Health 2020;17(23):1-21. [DOI: 10.3390/ijerph17238839] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lotfi 2021 {published data only}
- Lotfi T, Stevens A, Akl EA, Falavigna M, Kredo T, Mathew JL, et al. Getting trustworthy guidelines into the hands of decision-makers and supporting their consideration of contextual factors for implementation globally: recommendation mapping of COVID-19 guidelines. Journal of Clinical Epidemiology 2021;135:182-86. [DOI: 10.1016/j.jclinepi.2021.03.034] [DOI] [PMC free article] [PubMed] [Google Scholar]
Maldonado 2020 {published data only}
- Maldonado BMN, Collins J, Blundell HJ, Singh L. Engaging the vulnerable: a rapid review of public health communication aimed at migrants during the COVID-19 pandemic in Europe. Journal of Migration and Health 2020;1:100004. [DOI: 10.1016/j.jmh.2020.100004] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mastura 2020 {published data only}
- Mastura MS, Sharifah Azdiana TD, Teoh SH. Malaysia experience in tackling Covid19: a narrative review. Pakistan Journal of Medical and Health Sciences 2020;14(3):1354-56. [Google Scholar]
Matos 2020 {published data only}
- Matos RI, Chung KK. DoD COVID-19 practice management guide: clinical management of COVID-19. https://deployedmedicine.com/market/31/content/1440 (accessed November 16th 2021).
Matras 2020 {published data only}
- Matras P, Klek S, Folwarski M, Zmarzly A, Bartoszewska L, Cebulski W, et al. Home medical nutrition during SARS-CoV-2 pandemic–a position paper. Clinical Nutrition ESPEN 2020;38:196-200. [DOI: 10.1016/j.clnesp.2020.05.002] [DOI] [PMC free article] [PubMed] [Google Scholar]
Matterne 2021 {published data only}
- Matterne U, Egger N, Tempes J, Tischer C, Lander J, Dierks M-L, et al. Health literacy in the general population in the context of epidemic or pandemic coronavirus outbreak situations: rapid scoping review. Patient Education and Counseling 2021;104(2):223-34. [DOI: 10.1016/j.pec.2020.10.012] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mendez‐Brito 2021 {published data only}
- Mendez-Brito A, El Bcheraoui C, Pozo-Martin F. Systematic review of empirical studies comparing the effectiveness of non-pharmaceutical interventions against COVID-19. Journal of Infection. 2021;83(3):281-93. [DOI: 10.1016/j.jinf.2021.06.018] [DOI] [PMC free article] [PubMed] [Google Scholar]
Michie 2020 {published data only}
- Michie S, West R, Rogers MB, Bonell C, Rubin GJ, Amlot R. Reducing SARS-CoV-2 transmission in the UK: a behavioural science approach to identifying options for increasing adherence to social distancing and shielding vulnerable people. British Journal of Health Psychology 2020;25(4):945-56. [DOI: 10.1111/bjhp.12428] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mikuls 2020 {published data only}
- Mikuls TR, Johnson SR, Fraenkel L, Arasaratnam RJ, Baden LR, Bermas BL, C et al. American College of Rheumatology Guidance for the management of rheumatic disease in adult patients during the COVID-19 pandemic: Version 1. Arthritis and Rheumatology 2020;72(8):1241-51. [DOI: 10.1002/art.41596] [DOI] [PubMed] [Google Scholar]
Ministry of Health {published data only}
- Office of the Superintendent of Public Health. Advice and guidelines to the educational sector for the re-opening of primary and secondary schools in Malta. https://deputyprimeminister.gov.mt/en/health-promotion/covid-19/Documents/mitigation-conditions-and-guidances/Advice-and-guidelines-for-educational-sector_02Sep20.pdf (accessed November 17th 2021).
Miralles 2021 {published data only}
- Miralles O, Sanchez-Rodriguez D, Marco E, Annweiler C, Baztan A, Betancor E, et al. Unmet needs, health policies, and actions during the COVID-19 pandemic: a report from six European countries. European Geriatric Medicine 2021;12(1):193-204. [DOI: 10.1007/s41999-020-00415-x] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mistraletti 2020 {published data only}
Morina 2021 {published data only}
- Morina N, Kip A, Hoppen TH, Priebe S, Meyer T. Potential impact of physical distancing on physical and mental health: a rapid narrative umbrella review of meta-analyses on the link between social connection and health. BMJ Open 2021;11(3):e042335. [DOI: 10.1136/bmjopen-2020-042335] [DOI] [PMC free article] [PubMed] [Google Scholar]
Muhammad 2020 {published data only}
- Muhammad T, Zafar N. Policy brief on child protection during covid-19 crisis in Pakistan. Pakistan Paediatric Journal 2020;44(2):186-92. [Google Scholar]
Murphy 2021 {published data only}
- Murphy MT, Latif U. Pain during COVID-19: a comprehensive review and guide for the interventionalist. Pain Practice 2021;21(1):132-43. [DOI: 10.1111/papr.12976] [DOI] [PubMed] [Google Scholar]
Nachega 2020 {published data only}
- Nachega JB, Mbala-Kingebeni P, Otshudiema J, Mobula LM, Preiser W, Kallay O, et al. Responding to the challenge of the dual COVID-19 and Ebola epidemics in the Democratic Republic of Congo - priorities for achieving control. American Journal of Tropical Medicine & Hygiene 2020;103(2):597-602. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nagata 2021 {published data only}
- Nagata T, Ito D, Nagata M, Fujimoto A, Ito R, Odagami K, et al. Anticipated health effects and proposed countermeasures following the immediate introduction of telework in response to the spread of COVID-19: the findings of a rapid health impact assessment in Japan. Journal of Occupational Health 2021;63(1):e12198. [DOI] [PMC free article] [PubMed] [Google Scholar]
Najafizada 2021 {published data only}
- Najafizada M, Rahman A, Taufique Q, Sarkar A. Social determinants of multidrug-resistant tuberculosis: a scoping review and research gaps. Indian Journal of Tuberculosis 2021;68(1):99-105. [DOI: 10.1016/j.ijtb.2020.09.016] [DOI] [PubMed] [Google Scholar]
Narla 2021 {published data only}
- Narla S, Watchmaker J, Ozog DM, Rohrer TE. Cosmetic practices in the COVID-19 era. Advances in Cosmetic Surgery 2021;4(1):109-21. [DOI: 10.1016/j.yacs.2021.01.004] [DOI] [Google Scholar]
NICE 2020 {published data only}
- National Institute for Health and Care Excellence. COVID 19 rapid guideline: renal transplantation. https://www.nice.org.uk/guidance/ng178 (accessed November 2nd 2021). [PubMed]
Novak 2020 {published data only}
- Novak JM, Sopory P. Communicating public health alerts and guidance with technical audiences: qualitative research evidence synthesis. In: Evidence-Based Practice for Public Health Emergency Preparedness and Response. Washington, USA: National Academies Press, 2020:160-79. [Google Scholar]
NSW DoH 2020 {published data only}
- New South Wales Government Department of Health. Preserving consumer and patient partnership during COVID-19. https://www.ciap.health.nsw.gov.au/assets/docs/covid-19/evidence-checks/2020/20200528_Evidence%20check_%20Preserving%20consumer%20and%20patient%20partnership.pdf (accessed October 4th 2021).
Nursalam 2020 {published data only}
- Nursalam N, Sukartini T, Priyantini D, Mafula D, Efendi F. Risk factors for psychological impact and social stigma among people facing COVID 19: a systematic review. Systematic Reviews in Pharmacy 2020;11(6):1022-8. [Google Scholar]
O'Connell 2021 {published data only}
- O'Connell J, Abbas M, Beecham S, Buckley J, Chochlov M, Fitzgerald B, et al. Best practice guidance for digital contact tracing apps: a cross-disciplinary review of the literature. JMIR mHealth and uHealth 2021;9(6):e27753. [DOI: 10.2196/27753] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ogunleye 2020 {published data only}
- Ogunleye OO, Basu D, Mueller D, Sneddon J, Seaton RA, Yinka-Ogunleye AF, et al. Response to the novel Corona Virus (COVID-19) pandemic across Africa: successes, challenges, and implications for the future. Frontiers in Pharmacology 2020;11:1205. [DOI: 10.3389/fphar.2020.01205] [DOI] [PMC free article] [PubMed] [Google Scholar]
Orchard 2021 {published data only}
- Orchard K, Dignan FL, Lee J, Pearce R, Desai M, McFarlane E, et al. The NICE COVID-19 rapid guideline on haematopoietic stem cell transplantation: development, implementation and impact. British Journal of Haematology 2021;192(3):467-73. [DOI: 10.1111/bjh.17280] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pahl 2021 {published data only}
- Pahl DA, Wieder MS, Steinberg DM. Social isolation and connection in adolescents with cancer and survivors of childhood cancer: asystematic review. Journal of Adolescence 2021;87:15-27. [DOI: 10.1016/j.adolescence.2020.12.010] [DOI] [PubMed] [Google Scholar]
Parajuli 2020 {published data only}
- Parajuli RR, Mishra B, Banstola A, Ghimire BR, Poudel S, Sharma K, et al. Multidisciplinary approach to COVID-19 risk communication: a framework and tool for individual and regional risk assessment. Scientific Reports 2020;10(1):21650. [DOI: 10.1038/s41598-020-78779-0] [DOI] [PMC free article] [PubMed] [Google Scholar]
Parker 2020 {published data only}
- Parker J, Boles C, Leleck O, Buerger A, Egnot N, Sundermann A, et al. Advancing toward normal operations for arenas and stadiums. Toxicology & Industrial Health 2020;36(9):718-27. [DOI: 10.1177/0748233720964651] [DOI] [PubMed] [Google Scholar]
Patel 2020 {published data only}
- Patel A, Jernigan DB, Abdirizak F, Abedi G, Aggarwal S, Albina D. Initial public health response and interim clinical guidance for the 2019 novel coronavirus outbreak—United States, December 31, 2019–February 4, 2020. Morbidity and Mortality Weekly Report 2020;69(5):140-6. [DOI: 10.15585/mmwr.mm6905e1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Patel 2021 {published data only}
- Patel J, Fernandes G, Sridhar D. How can we improve self-isolation and quarantine for Covid-19? BMJ 2021;372:n625. [DOI: 10.1136/bmj.n625] [DOI] [PubMed] [Google Scholar]
Perski 2021 {published data only}
- Perski O, Szinay D, Corker E, Shahab L, West R, Michie S. Interventions to increase personal protective behaviours to limit the spread of respiratory viruses: a rapid evidence review and meta-analysis. British Journal of Health Psychology. 2021;27(1):215-64. [DOI: 10.1111/bjhp.12542] [DOI] [PMC free article] [PubMed] [Google Scholar]
PHAC 2020 {published data only}
- Public Health Agency of Canada. COVID-19: Guidance on indoor ventilation during the pandemic. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/guide-indoor-ventilation-covid-19-pandemic.html (accessed November 23rd 2021).
PHAC 2020a {published data only}
- Public Health Agency of Canada. Guidance for post-secondary institutions during the COVID-19 pandemic. https://open.canada.ca/data/en/dataset/762f0cf4-f888-4ff2-b624-fb093b6eba1a/resource/f97f22d7-81e9-4522-8e92-545115b02fb2 (accessed November 16th 2021).
PHAC 2020b {published data only}
- Public Health Agency of Canada. Guidance for providers of services for people experiencing homelessness (in the context of COVID-19). https://open.canada.ca/data/en/dataset/c8c8a7e7-8fbc-4723-8510-4e7375a844cf (accessed November 23rd 2021);June 29 2020.
PHAC 2020c {published data only}
- Public Health Agency of Canada. Protecting the health and safety of Indigenous communities in close proximity to natural resource operations. https://www.sac-isc.gc.ca/eng/1592487905243/1592487940872 (accessed November 23rd 2021).
PHAC 2021b {published data only}
- Public Health Agency of Canada. Guidance on the use of influenza vaccine in the presence of COVID-19. URL no longer available (2022 version only) (accessed November 17th 2021).
PHAC 2021c {published data only}
- Public Health Agency of Canada. Planning guidance for immunization clinics for COVID-19 vaccines. https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/planning-immunization-clinics-covid-19-vaccines.html (accessed November 16th 2021).
PHAC 2021d {published data only}
- Public Health Agency of Canada. Guidance for a strategic approach to lifting restrictive public health measures. URL no longer available, 2022 update available at https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/lifting-public-health-measures.html (accessed November 2nd 2021).
PHAC 2021e {published data only}
- Public Health Agency of Canada. Updated: Public health management of cases and contacts associated with COVID-19. URL July 2021 not available: Updated December 2021 version available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/health-professionals/interim-guidance-cases-contacts.html (accessed November 16th 2021).
PHAC 2021f {published data only}
- Public Health Agency of Canada. Community-based measures to mitigate the spread of COVID-19 in Canada. URL no longer available (accessed November 2nd 2021) .
PHAC 2021g {published data only}
- Public Health Agency of Canada. COVID-19 and people with disabilities in Canada. URL 2021 advice not available. Updated 2022 advice available at: https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/guidance-documents/people-with-disabilities.html (accessed November 16th 2021).
Pimenta 2020 {published data only}
- Pimenta IDSF, Sousa Mata AN, Braga LP, Medeiros GCBS, Azevedo KPM, Bezerra INM, et al. Media and scientific communication about the COVID-19 pandemic and the repercussions on the population's mental health: a protocol for a systematic review and meta-analysis. Medicine 2020;99(50):e23298. [DOI: 10.1097/MD.0000000000023298] [DOI] [PMC free article] [PubMed] [Google Scholar]
Polonsky 2021 {published data only}
- Polonsky JA, Bhatia S, Fraser K, Hamlet A, Skarp J, Stopard IJ, et al. Feasibility, acceptability, and effectiveness of non-pharmaceutical interventions for infectious disease prevention and control in crisis-affected settings and informal settlements: a scoping review. medRxiv [Preprint] 2021. [DOI: ]
Pourroy 2020 {published data only}
- Pourroy B, Tournamille JF, Bardin C, Slimano F, Chevrier R, Rioufol C, et al. Providing oncology pharmacy services during the coronavirus pandemic: French society for oncology pharmacy (Societe Francaise de Pharmacie Oncologique [SFPO]) guidelines. JCO Oncology Practice 2020;16(11):E1282-E1290. [DOI: 10.1200/OP.20.00295] [DOI] [PubMed] [Google Scholar]
Price 2020 {published data only}
- Price E, MacPhie E, Kay L, Lanyon P, Griffiths B, Holroyd C, et al. Identifying rheumatic disease patients at high risk and requiring shielding during the COVID-19 pandemic. Clinical Medicine 2020;20(3):256. [DOI: 10.7861/clinmed.2020-0149] [DOI] [PMC free article] [PubMed] [Google Scholar]
Puspitasari 2020 {published data only}
- Puspitasari IM, Yusuf L, Sinuraya RK, Abdulah R, Koyama H. Knowledge, attitude, and practice during the COVID-19 pandemic: a review. Journal of Multidisciplinary Healthcare 2020;13:727-33. [DOI: 10.2147/JMDH.S265527] [DOI] [PMC free article] [PubMed] [Google Scholar]
Qazi 2021 {published data only}
- Qazi A, Hardaker G, Ahmad IS, Darwich M, Maitama JZ, Dayani A. The role of information & communication technology in elearning environments: a systematic review. IEEE Access 2021;9:45539-51. [DOI: 10.1109/ACCESS.2021.3067042.] [DOI] [Google Scholar]
Qi 2021 {published data only}
- Qi S, Hua F, Xu S, Zhou Z, Liu F. Trends of global health literacy research (1995-2020): analysis of mapping knowledge domains based on citation data mining. PLoS One 2021;16(8):e0254988. [DOI: 10.1371/journal.pone.0254988] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rao 2020 {published data only}
- Rao SR, Spruijt O, Sunder P, Daniel S, Chittazhathu RK, Nair S, et al. Psychosocial aspects of COVID-19 in the context of pliative care - a quick review. Indian Journal of Palliative Care 2020;26(5):S116-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
RCP 2020 {published data only}
- Royal College of Physicians. Management and care of tracheostomised patients with prolonged disorders of consciousness duringthe COVID-19 crisis. Supplementary guidance to the Royal College of Physicians’ national clinical guidelines for prolonged disorders of consciousness March 2020. https://www.rcplondon.ac.uk/news/managing-tracheostomised-patients-prolonged-disorders-consciousness-during-covid-19 (accessed 17th November 2021).
Ribal 2020 {published data only}
- Ribal MJ, Cornford P, Briganti A, Knoll T, Gravas S, Babjuk M, et al. European Association of Urology Guidelines Office Rapid Reaction Group: an organisation-wide collaborative effort to adapt the European Association of Urology guidelines recommendations to the coronavirus disease 2019 era. European Urology 2020;78(1):21-8. [DOI: 10.1016/j.eururo.2020.04.056] [DOI] [PMC free article] [PubMed] [Google Scholar]
Riggioni 2020 {published data only}
- Riggioni C, Comberiati P, Giovannini M, Agache I, Akdis M, Alves-Correia M, et al. A compendium answering 150 questions on COVID-19 and SARS-CoV-2. Allergy: European Journal of Allergy and Clinical Immunology 2020;75(10):2503-41. [DOI: 10.1111/all.14449] [DOI] [PMC free article] [PubMed] [Google Scholar]
Robertson 2020 {published data only}
- Robertson LJ, Maposa I, Somaroo H, Johnson O. Mental health of healthcare workers during the COVID-19 outbreak: a rapid scoping review to inform provincial guidelines in South Africa. South African Medical Journal 2020;110(10):1010-9. [DOI: 10.7196/SAMJ.2020.v110i10.15022] [DOI] [PubMed] [Google Scholar]
Robinson 2020 {published data only}
- Robinson C, Ruhl M, Kirpalani A, Alabbas A, Noone D, Teoh CW, et al. Management of Canadian Pediatric Patients With Glomerular Diseases During the COVID-19 Pandemic: Recommendations From the Canadian Association of Pediatric Nephrologists COVID-19 Rapid Response Team. Canadian Journal of Kidney Health and Disease 2020;7:2054358120970713. [DOI: 10.1177/2054358120970713] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rocha 2021 {published data only}
- Rocha DM, Silva JS, Abreu IM, Mendes PM, Leite HDCS, Ferreira MCS. Psychosocial effects of social distancing during coronavirus infections: integrative review. Acta Paulista De Enfermagem 2021;34:eAPE01141. [Google Scholar]
Ryan 2020 {published data only}
- Ryan J, Okeibunor J, Talisuna A, Wiysonge CS. Setting up and relaxation of public health social and physical distancing measures for covid-19: a rapid review. Pan African Medical Journal 2020;35(Supplement 2):1-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Saadatjoo 2021 {published data only}
- Saadatjoo S, Miri M, Hassanipour S, Ameri H, Arab-Zozani M. Knowledge, attitudes, and practices of the general population about Coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis with policy recommendations. Public Health 2021;194:185-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Santos 2020 {published data only}
- Santos C, Tavares A, Tzanno-Martins C, Barros Neto J, Silva A, Lotaif L, et al. Palliative renal care and the Covid-19 pandemic. Jornal Brasileiro de Nefrologia 2020;42(2 suppl 1):44-6. [DOI: 10.1590/2175-8239-JBN-2020-S111] [DOI] [PMC free article] [PubMed] [Google Scholar]
Santos 2020a {published data only}
- Souza Santos FP, Sampaio Tavares R, Borgia Borbosa Pagnano K. Guidelines for therapy of patients with chronic myeloproliferative neoplasms during the novel coronavirus SARS-CoV2 pandemic. Hematology, Transfusion and Cell Therapy 2020;42(3):195-9. [DOI: 10.1016/j.htct.2020.06.005] [DOI] [PMC free article] [PubMed] [Google Scholar]
SCDPC 2020 {published data only}
- Saudi Centre for Disease Prevention and Control. Coronavirus Disease. COVID-19 guidelines. https://moh.gov.sa/Ministry/MediaCenter/Publications/Documents/Coronavirus-Disease-2019-Guidelines-v1.2.pdf (accessed November 15th 2021);v1.3 May 2020.
Schellack 2020 {published data only}
- Schellack N, Coetzee M, Schellack G, Gijzelaar M, Hassim Z, Milne M, et al. COVID-19: Guidelines for pharmacists in South Africa. Southern African Journal of Infectious Diseases 2020;35(1):1-10. [DOI: 10.4102/sajid.v35i1.206] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schoonees 2021 {published data only}
- Schoonees A, Naude CE, Claassen GN, Young T. Mapping existing global strategies to improve health intervention research reporting in mass media: a scoping review protocol. https://osf.io/za93n (accessed 4 November 2021). [DOI: ]
Selman 2020 {published data only}
- Selman LE, Chao D, Sowden R, Marshall S, Chamberlain C, Koffman J. Bereavement support on the frontline of COVID-19: recommendations for hospital clinicians. Journal of Pain and Symptom Management 2020;60(2):e81-6. [DOI: 10.1016/j.jpainsymman.2020.04.024] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sendzikaite 2021 {published data only}
- Sendzikaite S, Heying R, Milanesi O, Hanseus K, Michel-Behnke I. COVID-19 FAQs in paediatric and congenital cardiology: AEPC position paper. Cardiology in the Young 2021;31(3):344-51. [DOI: 10.1017/S1047951120005028] [DOI] [PMC free article] [PubMed] [Google Scholar]
Serafini 2020 {published data only}
- Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM 2020;113(8):229-35. [DOI: 10.1093/qjmed/hcaa201] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sharma 2020 {published data only}
- Sharma I, Vashnav M, Sharma R. COVID-19 pandemic hype: losers and gainers. Indian Journal of Psychiatry 2020;62(9 Supplement 3):S420-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sheen 2020 {published data only}
- Sheen A, Ro G, Holani K, Pinheiro Dos Santos ACZ, Kagadkar F, Zeshan M. 51.7 Impact of Covid-19-Related School Closures on Children and Adolescents Worldwide: A Literature Review. Journal of the American Academy of Child and Adolescent Psychiatry 2020;59 (10 Supplement):S253. [Google Scholar]
Sheen 2020a {published data only}
- Sheen A, Ro G, Pinheiro Dos Santos ACZ, Kagadkar F, Zeshan M. 51.15 Screen Time in the Context of Covid-19: The Good, the Bad, and the Ugly. Journal of the American Academy of Child and Adolescent Psychiatry 2020;59 (10 Supplement):S255. [Google Scholar]
Silva 2021 {published data only}
- Silva AB, Sindico SRF, Carneiro AC, Henrique SM, Fernandes AG, Gomes JP, et al. COVID-19 remote consultation services and population in health inequity-concentrating territories: a scoping review. Telemedicine Journal and eHealth: the official journal of the American Telemedicine Association. 2021;27(8):881-97. [DOI: 10.1089/tmj.2021.0145] [DOI] [PMC free article] [PubMed] [Google Scholar]
Srikanth 2020 {published data only}
- Srikanth A, Bhagavathula Wafa A, Aldhaleei J, Rahmani J, Khubchandani J. Knowledge, attitude, perceptions and practice towards COVID-19: a systematic review and meta-analysis. MedRxiv [Preprint] 2020. [DOI: 10.1101/2020.06.24.20138891] [DOI]
Stavridou 2020 {published data only}
- Stavridou A, Stergiopoulou AA, Panagouli E, Mesiris G, Thirios A, Mougiakos T, et al. Psychosocial consequences of COVID-19 in children, adolescents and young adults: a systematic review. Psychiatry and Clinical Neurosciences 2020;74(11):615-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stawicki 2020 {published data only}
- Stawicki S, Jeanmonod R, Miller A, Paladino L, Gaieski D, Yaffee A, et al. The 2019-2020 novel coronavirus (severe acute respiratory syndrome coronavirus 2) pandemic: a joint American College of Academic International Medicine-World Academic Council of Emergency Medicine multidisciplinary COVID-19 working group consensus paper. Journal of Global Infectious Diseases 2020;12(2):47-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stephen 2020 {published data only}
- Stephen S, Issac A, Jacob J, Vijay VR, Radhakrishnan RV, Krishnan N. COVID-19: weighing the endeavors of nations, with time to event analysis. Osong Public Health and Research Perspectives 2020;11(4):149-157. [DOI: 10.24171/j.phrp.2020.11.4.02] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stoilov 2020 {published data only}
- Stoilov R, Boyadzhieva V, Stoilov N, Ivanova M, Batalov A, Kolarov Z, et al. Bulgarian Rheumatology Society recommendations for behavior during an epidemic with COVID-19. Revmatologiia (Bulgaria) 2020;28(3):3-6. [Google Scholar]
Stojanovski 2021 {published data only}
- Stojanovski K, Naja-Riese G, King EJ, Fuchs JD. A systematic review of the social network strategy to optimize HIV testing in key populations to end the epidemic in the United States. AIDS Behavaviour 2021;25(9):2680-98. [DOI: 10.1007/s10461-021-03259-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stratil 2020 {published data only}
- Stratil JM, Voss M, Arnold L. WICID framework version 1.0: criteria and considerations to guide evidence-informed decision-making on non-pharmacological interventions targeting COVID-19. BMJ Global Health 2020;5(11):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sullivan 2020 {published data only}
- Sullivan M, Bouffet E, Rodriguez-Galindo C, Luna-Fineman S, Khan MS, Kearns P, et al. The COVID-19 pandemic: a rapid global response for children with cancer from SIOP, COG, SIOP-E, SIOP-PODC, IPSO, PROS, CCI, and St Jude Global. Pediatric Blood and Cancer 2020;67(7):e28409. [DOI: 10.1002/pbc.28409] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tabari 2020 {published data only}
- Tabari P, Amini M, Moghadami M, Moosavi M. International public health responses to COVID-19 outbreak: a rapid review. Iranian Journal of Medical Sciences 2020;45(3):157-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tam 2020 {published data only}
- Tam LS, Tanaka Y, Handa R, Chang CC, Cheng YK, Isalm N, et al. Care for patients with rheumatic diseases during COVID‐19 pandemic: a position statement from APLAR. International Journal of Rheumatic Diseases 2021;23(6):717-22. [DOI: 10.1111/1756-185X.13863] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tam 2021 {published data only}
- Tam LS, Tanaka Y, Handa R, Li Z, Lorenzo JP, Louthrenoo W, et al. Updated APLAR consensus statements on care for patients with rheumatic diseases during the COVID-19 pandemic. International Journal of Rheumatic Diseases 2021;24(6):733-45. [DOI: 10.1111/1756-185X.14124] [DOI] [PMC free article] [PubMed] [Google Scholar]
Taylor 2020 {published data only}
- Taylor T, Das R, Mueller K, Pransky G, Christian J, Orford R, et al. Safely returning America to work part i: general guidance for employers. Journal of Occupational and Environmental Medicine 2020;62(9):771-9. [DOI] [PubMed] [Google Scholar]
TC 2020 {published data only}
- Transport Canada. Federal safety guidance to protect drivers and limit the spread of COVID-19 in commercial vehicle operations. https://tc.canada.ca/en/initiatives/covid-19-measures-updates-guidance-issued-transport-canada/covid-19-measures-updates-guidance-road-issued-transport-canada/federal-safety-guidance-protect-drivers-limit-spread-covid-19-commercial-vehicle-operations (accessed November 23rd 2021).
Tegegne 2021 {published data only}
- TTegegne GT, Kefale B, Engidaw MT, Degu A, Tesfa D, Ewunetei A, et al. Knowledge, attitude, and practice of healthcare providers toward Novel Coronavirus 19 during the first months of the pandemic: a systematic review. Frontiers in Public Health 2021;9:606666. [DOI: 10.3389/fpubh.2021.606666] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ting 2020 {published data only}
- Ting FI, Mendoza MJ, Sacdalan DB, Abarquez HS. Updated general recommendations in cancer management during the COVID-19 pandemic in the Philippines. ecancermedicalscience 2020;14:1128. [DOI: 10.3332/ecancer.2020.1128] [DOI] [PMC free article] [PubMed] [Google Scholar]
Tonin 2020 {published data only}
- Tonin L, Lacerda MR, Caceres NTG, Hermann AP. Recommendations in Covid-19 times: a view for home care. Revista Brasileira de Enfermagem 2020;73(Supple 2):e20200310. [DOI: ] [DOI] [PubMed] [Google Scholar]
Tsao 2021 {published data only}
- TTsao SF, Chen H, Tisseverasinghe T, Yang Y, Li L, Butt ZA. What social media told us in the time of COVID-19: a scoping review. The Lancet Digital Health 2021;3(3):e175-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Turner 2021 {published data only}
- Turner S, Botero-Tovar N, Herrera MA, Borda Kuhlmann JP, Ortiz F, Ramirez JC, et al. Systematic review of experiences and perceptions of key actors and organisations at multiple levels within health systems internationally in responding to COVID-19. Implementation Science 2021;16(1):50. [DOI: 10.1186/s13012-021-01114-2] [DOI] [PMC free article] [PubMed] [Google Scholar]
UK HSA {published data only}
- UK Health Security Agency. Guidance for contacts of people with confirmed coronavirus (COVID-19) infection who do not live with the person. https://www.gov.uk/government/publications/guidance-for-contacts-of-people-with-possible-or-confirmed-coronavirus-covid-19-infection-who-do-not-live-with-the-person (accessed November 2nd 2021).
Ul Haq 2021 {published data only}
- Ul Haq Z, Mirza Z, Oyewale TO, Sultan F. Leaving no one behind: Pakistan’s risk communication and community engagement during COVID-19. Journal of Global Health 2021;11:03091. [DOI: 10.7189/jogh.11.03091] [DOI] [PMC free article] [PubMed] [Google Scholar]
Vaezi 2020 {published data only}
- Vaezi A, Javanmard SH. Infodemic and risk communication in the era of CoV-19. Advanced Biomedical Research 2020;9:10. [DOI: 10.4103/abr.abr_47_20] [DOI] [PMC free article] [PubMed] [Google Scholar]
Viero 2021 {published data only}
- Viero A, Barbara G, Montisci M, Kustermann K, Cattaneo C. Violence against women in the Covid-19 pandemic: a review of the literature and a call for shared strategies to tackle health and social emergencies. Forensic Science International 2021;319:110650. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wake 2020 {published data only}
- Wake AD. Knowledge, attitude, practice, and associated factors regarding the novel coronavirus disease 2019 (COVID-19) pandemic. Infection and Drug Resistance 2020;13:3817-32. [DOI: 10.2147/IDR.S275689] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallace 2020 {published data only}
- Wallace CL, Wladkowski SP, Gibson A, White P. Grief during the COVID-19 pandemic: considerations for palliative care providers. Journal of Pain & Symptom Management 2020;60(1):e70-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2020 {published data only}
- Wang LY, Low TT, Yeo TJ. Telehealth in COVID-19 and cardiovascular disease-ensuring equitable care. Annals of the Academy of Medicine, Singapore 2020;49(11):902-4. [PubMed] [Google Scholar]
WHO 2020d {published data only}
- World Health Organization. Addressing noncommunicable diseases in the COVID-19 response. https://apps.who.int/iris/handle/10665/331923 (accessed 23rd November 2021).
WHO 2020e {published data only}
- World Health Organization. Considerations in adjusting public health and social measures in the context of COVID-19: interim guidance, 16 April 2020. https://apps.who.int/iris/handle/10665/331773 (accessed November 2nd 2021).
WHO 2020f {published data only}
- World Health Organization. Safe Eid al Adha practices in the context of COVID-19: interim guidance, 25 July 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-Eid_al_Adha-2021.1 (accessed November 2nd 2021).
WHO 2020g {published data only}
- World Health Organization. Coronavirus disease ( COVID-19) outbreak: rights, roles and responsibilities of health workers, including key considerations for occupational safety and health: interim guidance, 19 March 2020. https://apps.who.int/iris/handle/10665/331510 (accessed November 23rd 2021).
WHO 2020h {published data only}
- World Health Organization. Rational use of personal protective equipment for coronavirus disease (COVID-19) and considerations during severe shortages: interim guidance, 6 April 2020. https://apps.who.int/iris/handle/10665/331695 (accessed November 2nd 2021).
WHO 2020i {published data only}
- World Health Organization. Guidance on COVID-19 for the care of older people and people living in long-term care facilities, other non-acute care facilities and home care. https://www.who.int/publications/i/item/WPR-DSE-2020-015 (accessed November 23rd 2021).
WHO 2020j {published data only}
- World Health Organization. Information note on HIV and COVID-19. https://apps.who.int/iris/handle/10665/331919 (accessed November 23rd 2021).
WHO 2020k {published data only}
- World Health Organization. Role of primary care in the COVID-19 response. https://apps.who.int/iris/handle/10665/331921 (accessed November 23rd 2021).
WHO 2020l {published data only}
- World Health Organization. Supporting healthy urban transport and mobility in the context of COVID-19. https://www.who.int/europe/publications/i/item/9789240012554 (accessed November 2nd 2021).
WHO 2020m {published data only}
- World Health Organization. Preparedness, prevention and control of COVID-19 in prisons and other places of detention: interim guidance 15 March 2020. https://apps.who.int/iris/handle/10665/336525 (accessed November 2nd 2021).
WHO 2020n {published data only}
- World Health Organization. Disaster evacuation shelters in the context of COVID-19. https://www.who.int/publications/i/item/WPR-DSE-2020-033 (accessed November 2nd 2021).
WHO 2020o {published data only}
- World Health Organization. Calibrating long-term non-pharmaceutical interventions for COVID-19: principles and facilitation tools. https://apps.who.int/iris/handle/10665/332099 (accessed November 2nd 2021).
WHO 2020p {published data only}
- World Health Organization. Promoting public health measures in response to COVID-19 on cargo ships and fishing vessels: interim guidance, 25 August 2020. https://reliefweb.int/report/world/promoting-public-health-measures-response-covid-19-cargo-ships-and-fishing-vessels (accessed November 17th 2021).
WHO 2020q {published data only}
- Organization World Health. Promoting public health measures in response to COVID-19 on cargo ships and fishing vessels: interim guidance, 25 August 2020. https://iris.who.int/handle/10665/333978 (accessed November 16th 2021).
WHO 2021c {published data only}
- World Health Organization. Safe Ramadan practices in the context of COVID-19: interim guidance, 7 April 2021. https://apps.who.int/iris/handle/10665/340661 (accessed November 17th 2021).
WHO 2021d {published data only}
- World Health Organization. COVID-19: Occupational health and safety for health workers: interim guidance, 2 February 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-HCW_advice-2021-1 (accessed November 2nd 2021).
Wilkinson 2020 {published data only}
- Wilkinson R, Hines L, Holland A, Mandal S, Phipps E. Rapid evidence review of harm reduction interventions and messaging for people who inject drugs during pandemic events: implications for the ongoing COVID-19 response. Harm Reduction Journal 2020;17(1):1-10. [DOI: 10.1186/s12954-020-00445-5] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yazew 2021 {published data only}
- Yazew BG, Abate HK, Mekonnen CK. Knowledge, Attitude and Practice Towards COVID-19 in Ethiopia: A Systematic Review; 2020. Patient Preference and Adherence 2021;15:337-48. [DOI: 10.2147/PPA.S288186] [DOI] [PMC free article] [PubMed] [Google Scholar]
Yu 2020 {published data only}
- Yu MS, Kutishenko NP, Lukina Yu V, Tolpygina SN, Ivanova LP, Dmitrieva NA, et al. Self-monitoring and treatment of chronic non-communicable diseases in the context of the COVID-19 pandemic. Consensus of experts of the National Society of Evidence-Based Pharmacotherapy and the Russian Society of the Prevention of Non-Communicable Diseases. [Russian]. Cardiovascular Therapy and Prevention (Russian Federation) 2020;19(3):295-301. [Google Scholar]
Yuan 2021 {published data only}
- Yuan K, Gong Y-M, Liu L, Sun Y-K, Tian S-S, Wang Y-J, et al. Prevalence of posttraumatic stress disorder after infectious disease pandemics in the twenty-first century, including COVID-19: a meta-analysis and systematic review. Molecular Psychiatry 2021;26(9):4982-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yue 2020 {published data only}
- Yue JL, Yan W, Sun YK, Yuan K, Su SZ, Han Y, et al. Mental health services for infectious disease outbreaks including COVID-19: a rapid systematic review. Psychological Medicine 2020;50(15):2498-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhang 2021 {published data only}
- Zhang JY, Shang T, Ahn D, Chen K, Coté G, Espinoza J, et al. How to best protect people with diabetes from the impact of SARS-CoV-2: report of the International COVID-19 and Diabetes Summit. Journal of Diabetes Science and Technology 2021;15(2):478-514. [DOI: 10.1177/1932296820978399] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Adab‐Corpa 2021 {published data only}
- Abad-Corpa E, Sanchez-Lopez D, Moreno-Casbas MT. Scoping review about the recommendations for home isolation in the COVID-19 pandemic [ Scoping review sobre las recomendaciones para el aislamiento domiciliario en la pandemia de COVID-19]. Enfermería Clínica 2021;31:S94-S99. [DOI] [PMC free article] [PubMed] [Google Scholar]
Dreyer 2020 {published data only}
- Dreyer G, Snyman L. South Africa’s response to COVID-19: on the positive side. In: Obstetrics and Gynaecology Forum. Vol. 30(2). 2020:1-1.
Ghungrud 2021 {published data only}
- Ghungrud D, Singh S, Sharma R, Pohekar S. Engaging school going children during Covid-19 lockdown. Indian Journal of Forensic Medicine & Toxicology 2021;15(1):375-81. [Google Scholar]
Jun 2020 {published data only}
- Jun MA. Key messages and actions for coronavirus peneumonia prevention and control in education institutions. Chinese Journal of School Health 2020;41(4):481-83. [Google Scholar]
Kang 2020 {published data only}
- Kang C. How should messages be communicated in Covid 19 pandemic? Let’s use the expressions “self-caring during quarantine” and “distancing for preventing the spread of infection”! [코로나19 팬데믹 상황에서 메시지는 어떻게 소통되어야 하는가? ‒'격리 중 자기돌봄'과 '감염확산방지를 위한 거리두기'라는 표현을 사용하자!]. Cheolhak-Korean Journal of Philosophy 2020;143:87-109. [Google Scholar]
Odendaal 2020 {published data only}
- Odendaal N. ITU, WHO leverage text messaging to reach billions of unconnected. www.miningweekly.com/article/itu-who-leverage-texts-to-reach-billions-of-unconnected-2020-05-08.
Thomson 2021 {published data only}
- Thomson A, Jordan H, Wilson E. Improving communication and family connection with a new asynchronous video messaging service within adult critical care, during the COVID-19 pandemic. Anaesthesia 2021;76(70):70-70. [Google Scholar]
References to ongoing studies
Grimani 2021 {published data only}
- Grimani A, Bonell C, Michie S, Antonopoulou V, Kelly MP, Vlaev I. Effect of prosocial public health messages for population behaviour change in relation to respiratory infections: a systematic review protocol. BMJ Open 2021;11:e044763. [DOI: 10.1136/ bmjopen-2020-044763] [DOI] [PMC free article] [PubMed] [Google Scholar]
Monteiro 2021 {published data only}
- Monteiro KS, Santino TA, Jácome AC, Silva B, Patino CM, Chaves G, et al. Barriers and facilitators to populational adherence to prevention and control measures of COVID-19 and other respiratory infectious diseases: a rapid qualitative evidence synthesis protocol. BMJ Open 2021;11(1):e045529-e. [DOI: 10.1136/bmjopen-2020-045529] [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Berger 2022
- Berger E. Biden’s claim that Covid pandemic is over sparks debate over future. 24 Sep 2022. https://www.theguardian.com/world/2022/sep/24/covid-not-over-biden-remarks-cbs-60-minutes.
Brouwers 2010
- Brouwers M, Kho M, Browman G, Burgers J, Cluzeau F, Feder G, et al. AGREE II: Advancing guideline development, reporting and evaluation in healthcare. CMAJ 2010;182(18):E839-42. [DOI: doi: 10.1503/cmaj.090449] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2020
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: a reporting guideline. BMJ 2020;368:l6890. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cochrane 2020
- Cochrane. Cochrane Convenes: Preparing for and responding to global health emergencies. What have we learnt from COVID-19? Reflections and recommendations from the evidence synthesis community. https://convenes.cochrane.org/report.
Garritty 2021
- Garritty C, Gartlehner G, Nussbaumer-Streit B, Klin VJ, Hamel C, Kamel C, et al. Cochrane rapid reviews methods group offers evidence-informed guidance to conduct rapid reviews. Journal of Clinical Epidemiology 2021;130:13-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hill 2011
- Hill S, Lowe D, Ryan R. Interventions for communication and participation: their purpose and practice. In: Hill S, editors(s). The Knowledgeable Patient: Communication And Participation in Health. Chichester, UK: Wiley Blackwell, 2015:27-39. [Google Scholar]
IFRC 2023
- International Federation of Red Cross and Red Crescent Societies. World disasters report 2022. Equity, trust and local action: lessons from the COVID-19 pandemic to avert the next global crisis. https://www.ifrc.org/document/world-disasters-report-2022 (accessed February 6th 2023).
IPMAC 2022
- Independent Pandemic Management Advisory Committee. Review of COVID-19 communications in Victoria. Available at: https://www.health.vic.gov.au/research-and-reports/review-of-covid-19-communications-in-victoria (accessed December 20th 2022).
Kaufman 2017
- Kaufman J, Ames H, Bosch-Capblanch X, Cartier Y, Cliff J, Glenton C, et al. The comprehensive ‘Communicate to Vaccinate’ taxonomy of communication interventions for childhood vaccination in routine and campaign contexts. BMC Public Health 2017;17(1):423. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ritchie 1994
- Ritchie J, Spencer L. Analyzing Qualitative Data. In: Bryman A, Burgess B, editors(s). Analyzing Qualitative Data. London: Routledge, 1994. [DOI: ] [Google Scholar]
Ryan 2014
- Ryan R, Santesso N, Lowe D, Hill S, Grimshaw JM, Prictor M, et al. Interventions to improve safe and effective medicines use by consumers: an overview of systematic reviews. Cochrane Database of Systematic Reviews 2014, Issue 4. Art. No: CD007768. [DOI: 10.1002/14651858.CD007768.pub3] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ryan 2023
- Ryan R, Jessup R, Hill S, Walsh L, Oldenburg B. People at heightened risk of deterioration from COVID-19: living ‘with’ or living ‘despite’ public health communications? Australian and New Zealand Journal of Public Health 2023;47(2):100049. [DOI: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sachs 2022
- Sachs JD, Karim SSA, Aknin L, Allen J, Brosbøl K, Colombo MAF et al. The Lancet Commission on lessons for the future from the COVID-19 pandemic. The Lancet 2022;400(10359):1224-80. [DOI: DOI: https://doi.org/10.1016/S0140-6736(22)01585-9] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shea 2007
- Shea BJ, Grimshaw JM, Wells GA, Boers M, Andersson N, Hamel C, et al. Development of AMSTAR: a measurement tool to assess the methodological quality of systematic reviews. BMC Medical Research Methodology 2007;7:10. [DOI: DOI: 10.1186/1471-2288-7-10] [DOI] [PMC free article] [PubMed] [Google Scholar]
Shergold 2022
- Shergold P, Broadbent J, Marshall I, Varghese P. Fault lines: an independent reviewinto Australia’s response to COVID-19. 20 October 2022. Available at https://independentcovidreview.com/. [AVAILABLE AT: HTTPS://APO.ORG.AU/SITES/DEFAULT/FILES/RESOURCE-FILES/2022-10/APO-NID320067_0.PDF: Accessed December 20th 2022]
Tricco 2017
- Tricco AC, Langlois EV, Strauss SE, Alliance for Health Policy and Systems Research, World Health Organization. Rapid reviews to strengthen health policy and systems: a practical guide. World Health Organization 2017.
Tricco 2020
- Tricco AC, Garritty CM, Boulos L, Lockwood C, Wilson M, McGowan J, et al. Rapid review methods more challenging during COVID-19: commentary with a focus on 8 knowledge synthesis steps. Journal of Clinical Epidemiology 2020;126:177-83. [DOI: 10.1016/j.jclinepi.2020.06.029] [DOI] [PMC free article] [PubMed] [Google Scholar]
United Nations 2022
- The end of the COVID-19 pandemic is in sight: WHO. https://news.un.org/en/story/2022/09/1126621 (accessed February 15th 2023).
Vitello 2022
- Vitiello L, Ilari S, Sansone L, Belli M, Cristina M, Marcolongo F, et al. Preventive measures against pandemics from the beginning of civilization to nowadays - how everything has remained the same over the millennia. Journal of Clinical Medicine 2022;11(7):1960. [DOI: doi: 10.3390/jcm11071960] [DOI] [PMC free article] [PubMed] [Google Scholar]
WHO 2019
- World Health Organization. Non-pharmaceutical public health measures for mitigating the risk and impact of epidemic and pandemic influenza. Annex: report of systematic literature reviews. https://apps.who.int/iris/bitstream/handle/10665/329439/WHO-WHE-IHM-GIP-2019.1-eng.pdf?ua=1 (accessed 1 December 2020).
WHO 2023
- World Health Organization. COVID-19 policy briefs. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-policy-briefs (accessed February 15th 2023).
Wilson 2018
- Wilson M. Rapid response program: summary of service timelines. McMaster Health Forum; 2018; Hamilton Canada. https://www.mcmasterforum.org/docs/default-source/resources/14_rr_timelines.pdf?sfvrsn=e58552d5_8 (accessed March 25 2021).
References to other published versions of this review
Ryan 2021a
- Ryan RE, Parkhill A, Schonfeld L, Walsh L, Lowe D, Merner B, et al. What are relevant, feasible and effective approaches to promote acceptance, uptake and adherence to physical distancing measures for COVID-19 prevention and control?. World Health Organization. Regional Office for Europe. https://apps.who.int/iris/handle/10665/339887. [PubMed]
Ryan 2021b
- Ryan R, Parkhill A, Schonfeld L, Merner B, Kaufman J, et al. Promoting and supporting physical distancing for COVID: protocol for rapid review update August 2021. Available at https://opal.latrobe.edu.au/articles/journal_contribution/Promoting_and_supporting_physical_distancing_for_COVID_Protocol_for_rapid_review_update_August_2021/16592540. [DOI: ]


