Abstract
Background
In the treatment of gender dysphoria, appropriate nipple-areola complex (NAC) positioning is essential for achieving a natural appearing male chest after subcutaneous mastectomy. An accurate predictive model for the ideal personalized position of the NAC is still lacking. The aim of this study is to determine the anthropometry of the male chest to create individualized guidelines for appropriate NAC positioning in the preoperative setting.
Materials and methods
Cisgender male participants were recruited. Multiple chest measurements were manually recorded. Best subset regression using linear models was used to select predictors for the horizontal coordinate (nipple-nipple distance; NN) and vertical coordinate (sternal notch-nipple distance; SNN) of the NAC. Internal validation was assessed using bootstrapping. Furthermore, a cohort of transgender men who had received a mastectomy with replantation of nipples according to current practice was identified. Comparison testing between the algorithm and standard practice was performed to test the limitations of standard practice.
Results
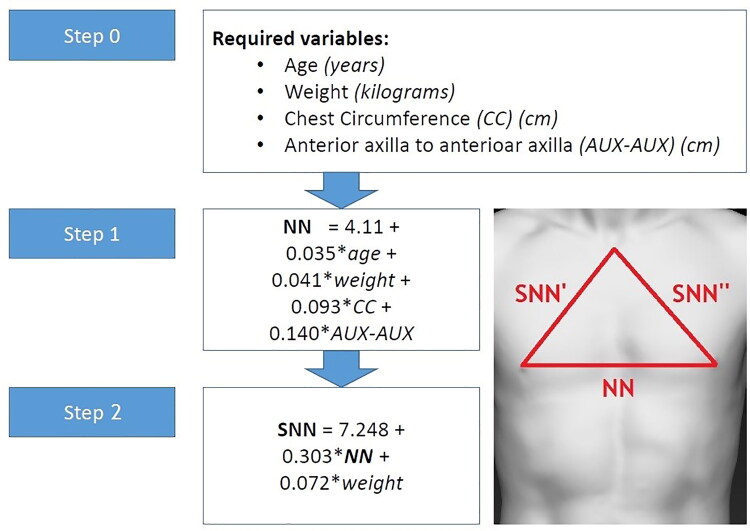
One hundred and fifty cis male participants were included (median age: 26, IQR: 22-34 years). Four predictors were found to predict NN (age, weight, chest circumference (CC), anterior-axillar fold to anterior-axillar fold (AUX-AUX)) and reads as follows: NN = 4.11 + 0.035*age + 0.041*weight + 0.093*CC + 0.140*AUX-AUX Two predictors were found to predict SNN (NN and weight), and reads as follows: SNN = 7.248 + 0.303*NN + 0.072*weight. Both models performed well (Bootstrapped R2: 0.63 (NN), 0.50 (SNN)) and outperformed previous models predicting NAC position. Ninety-six transgender men were eligible for evaluation of current practice and showed an average placement error of −0.9 cm for NN and +2.2 cm for SNN.
Conclusion
The non-standardized approach of NAC repositioning results in a significant error of nipple placement. We suggest that the two predictive models for NN and SNN can be used to optimize NAC positioning on the masculinized chest wall.
Supplemental data for this article is available online at https://doi.org/10.1080/26895269.2021.1884926.
Keywords: Mastectomy, nipples, anthropometry, transgender persons, gender-affirming surgery, chest wall
Introduction
Subcutaneous mastectomy is the foremost surgical treatment option for masculinizing the chest wall and is performed as part of gender-affirming surgeries for transgender men. The outcomes of subcutaneous mastectomies can vary greatly depending on patient habitus, surgical technique and the preferred practice of the surgeon. A mastectomy often calls for the repositioning of the nipple-areola complex (NAC) (Cregten-Escobar et al., 2012; Monstrey et al., 2008; Wolter et al., 2015). It is essential to position the nipples appropriately to achieve a male chest appearance. Up to quite recently, only few studies have asked critical questions about the NAC position in men. This has led to the standard practice of eyeballing the approximate location of the NAC during mastectomies, resulting in the NAC’s often being placed too high or too wide on the chest (Beckenstein et al., 1996; Berry et al., 2012; Hage & van Kesteren, 1995). The negative impact this can have on the experienced outcome emphasizes the necessity to develop strategies and standards that allow for the best possible result (Agarwal et al., 2017; van de Grift et al., 2016; 2018).
Recognizing the aforementioned, the need for evidence-based guidelines on NAC positioning is substantial (Cohen et al., 2019; Maas et al., 2020). Guidelines should, ideally, incorporate all relevant anthropometric characteristics that determine the position of the NAC in normative populations. Currently, some studies have identified relationships between positioning, shape and size of the NAC and body and chest measurements (Atiyeh et al., 2009; Beer et al., 2001; Hage & van Kesteren, 1995; Shulman et al., 2001). Several algorithms have been proposed and different sets of anatomic parameters and preset values have been propagated, yet these proposed algorithms were often based on unclear methodology and limited statistical power. More importantly, most of the current approaches did not incorporate and consider inter-patient variability (Ayyala et al., 2020; Lo Russo et al., 2017; Tanini & Lo Russo, 2018). Ideally, NAC positioning should incorporate and be attuned to the large variety in chest dimensions between patients. These differing outcomes and the direct implications they have on quality of life of patients, stress the necessity to develop high quality, uniform standards of care that are easily and broadly applicable to the greater population. Acknowledging this lack in literature, The aim of this study was to estimate how the NAC position depends on the variable anthropometric characteristics of the cis male chest, and to develop a predictive algorithm for the distance from the (1) sternal-notch to the nipple (SNN; vertical coordinate) and the (2) distance between the nipples (NN; horizontal coordinate). These two practical approaches will preoperatively allow to pinpoint the most appropriate location of the NAC for that person specifically.
Material and methods
Study procedure
This was a single-center, observational, cross-sectional study. Cisgender men, aged 18 and above were recruited through open invitation and on a voluntary basis. Eligible men who matched the selection criteria were invited to the outpatient clinic at the Amsterdam University Medical Center, location VUmc in Amsterdam, the Netherlands. Written consent was obtained including (optional) consent to publish images. Collected demographic data included age, weight and height and sport activities. No restrictions were placed on age or body composition. Exclusion criteria included previous thoracic surgery and conditions that affect the anthropometry of the chest wall (e.g., spinal malformations, pectus deformities and gynecomastia).
Measurements
Demographic data and anatomic landmarks utilized for measurements are presented in Table 1. Two examiners (B.J. and M.H.) performed the measurements after having undergone training on the parameters and handling of the measuring tape. Measurements were set to one decimal place in centimeters. Participants were asked to stand in an upright position with arms in 45 degrees and palms faced anteriorly during measurements and photography. The central point on the nipple was considered to parameter for NAC position. All measurements were performed in the same room, with temperature maintained at 21 degrees to prevent cold-induced skin and nipple contraction. The measured variables and parameters are presented in Table 1. The Canfield VECTRA XT three-dimensional camera was used to image the upper body from the laryngeal prominence down to the anterior superior iliac spine.
Table 1.
Overview and instructions for measured variables.
| Variable (abb.) | Instruction | |
|---|---|---|
| Body dimensions | Weight | Body weight when undressed (kg) |
| Height | Body length in supine position (cm) | |
| Nipple position | Sternal notch to nipple (SNN) | Distance from the sternal notch to the nipples (cm) |
| Nipple to nipple (NN) | Distance between the nipples (cm) | |
| Anatomic parameters | Chest circumference (CC) | Circumference at the level the caudal pectoral insertion (cm) |
| Hip circumference (HC) | Circumference at the level of the iliac spines (cm) | |
| Waist circumference (WC) | Circumference at the widest portion of the buttocks (cm) | |
| Shoulder circumference (SC) | Circumference is the maximum circumference of the shoulders at the level of the midpoints of the right and left deltoid muscles with arms along the body (cm) | |
| Axillary fold to axillary fold (AUX-AUX) | Distance between the anterior axillary folds with arms along the body (cm) | |
| Sternal notch to umbilicus (SN-U) | Distance between the sternal notch to the umbilicus (cm) |
Evaluation of current practice
To test the accuracy of current practice, we collected anatomic measurements in a secondary cohort of trans men, who had undergone an inframammary mastectomy with free nipple grafts as part of a prospective clinical study (NTR7412). Informed consent for anatomic data collection was provided with the abovementioned study. The nipple position of these participants were placed according to standard practice of approximation and eyeballing. Baseline demographics and the necessary algorithm-variables were collected at one year follow-up.
Statistical analysis
General statistics
Descriptive measures were calculated over the sample as a whole. Continuous variables were presented as mean ± standard deviation (SD) in case of a normal distribution, in case of a non-normal distribution as median with inter quartile range (IQR) (25th, 75th percentile). Categorical variables were presented as frequencies and percentages. The intra- and inter-observer reliability of both the observers were respectively tested by drawing random samples of 10 participants who were tested twice within the same study visit and in a cohort of 10 similar patients. Intra-class correlation coefficient (ICC) was used to assess the intra-observer and inter-observer reliability. All analyses were performed in R (Version 3.6.3).
Model development
Model building was done according to the steps described by Veen et al. (2020) Candidate predictors were a priori selected based upon previous models and clinical expertise (Atiyeh et al., 2009; Beckenstein et al., 1996; Beer et al., 2001; Hage & van Kesteren, 1995; Shulman et al., 2001). A detailed explanation of all analyses is presented in Supplementary Text 1 and Supplementary Tables 1–4. Two multivariable linear models were developed in order to predict NN and SNN respectively (Figure 1). The means of bilateral measurements (for SNN) was used as the included variables in the model development, assuming a symmetrical NAC position on the vertical coordinate. Predictor selection was done using best subset regression approach to distill the most suitable variables (Miller, 1990).
Figure 1.
Depiction of SNN and NN.
Note: SNN: sternal notch to nipple distance; NN: nipple to nipple distance
Model internal validation
The model was trained on the entire cohort in order to make efficient use of all available data (Steyerberg, 2019). Mean Squared Error (MSE), mean absolute percentage error (MAPE) and R-squared (i.e., the proportion of the outcome predicted by the model) was calculated to asses performance of the model (Harrell, 2006). Bootstrapping was used to assess the performance of the model, as this is the most efficient internal validation procedure (Steyerberg, 2019). In total, 200 bootstrap samples were generated. Additionally, violations of the assumptions of the linear models were assessed (Harrell, 2006).
Model presentation
Individual formulas for NN and SNN were calculated using the regression formula: NN or SNN. In this formula a is the intercept plus the sum of the product of the included predictors (b) and their coefficient (x).
Algorithm comparison and retrospective evaluation of current practice
Performance of the present model was compared with previously published models that allowed for external validation of these models (Atiyeh et al., 2009; Beckenstein et al., 1996; Beer et al., 2001; Shulman et al., 2001). This was done, by comparing the R-squared, MSE and MAPE values calculated over the present sample.
Results
Demographics and anthropometric measures
A total of 150 participants were included in this study. Participant characteristics and the anthropometric measurement outcomes are summarized respectively in Tables 2 and 3. The average NN distance was 23.0 cm (SD 2.0) and the average SNN distance was 19.9 cm (SD 1.7). Intra- and inter-observer reliability scores were excellent (>0.95) for all measurements. In total, 10 predictors were considered for the multivariable linear models (Supplementary Table 5). Missing values were low as 9 out of 10 variables had >95% completeness (Supplementary Figure 1).
Table 2.
Participant characteristics (n = 150).
| Demographics | Mean, median or N= | SD, IQR or (%) |
|---|---|---|
| Age (years) | 26 | 22.0–34.3 |
| Weight (kg) | 79.8 | 10.3 |
| Height (cm) | 182.9 | 6.7 |
| §BMI (kg/m2) | 23.7 | 21.9–26.4 |
| Sport | ||
| No | 30 | 20% |
| Yes | 120 | 80% |
| Frequency of sports | ||
| 1–2 × per week | 50 | 42% |
| 3–4 × per week | 51 | 43% |
| >5 × per week | 19 | 15% |
Table 3.
Manual measurements (n = 150).
| Measurement | Mean (SD) |
|---|---|
| Inter-nipple distance (NN) | 22.9 ± 2.0 |
| Sternal-notch to nipple distance (SNN) | 19.9 ± 1.7 |
| Sternal-notch to umbilicus (SN-U) | 38.7 ± 3.1 |
| Chest circumference (CC) | 93.5 ± 8.0 |
| Shoulder circumference (SC) | 119.3 ± 7.4 |
| Waist circumference (WC) | 84.0 ± 9.3 |
| Hip circumference (HC) | 88.6 ± 8.1 |
NN model development
In total, 4 predictors were selected using best subset regression age, weight, chest circumference (CC), anterior axillary fold to anterior axillary fold (AUX-AUX) (Table 4). The algorithm can best be expressed as the following formula: NN = 4.11 + 0.035*age + 0.041*weight + 0.093*CC + 0.140*AUX-AUX R-squared and MSE were 0.65 and 1.37, respectively. R-squared dropped to 0.63 after bootstrapping. Assumptions of the linear model were not violated and the predicted values of NN were not significantly different from observed values (paired t-test: P > 0.99).
Table 4.
Regression coefficients of multivariable model NN.
| Predictor | B-coefficient | 95% CI | P-value |
|---|---|---|---|
| Intercept | 4.11 | (0.727 to 7.493) | 0.018 |
| Age | 0.035 | (0.018 to 0.052) | <0.001 |
| Weight | 0.041 | (0.011 to 0.071) | 0.008 |
| CC | 0.093 | (0.054 to 0.133) | <0.001 |
| AUX-AUX | 0.14 | (0.061 to 0.219) | 0.001 |
Note: NN; nipple-to-nipple distance. CC; chest circumference. AUX-AUX; anterior-axillary-fold – anterior-axillary-fold.
Table 5.
Regression coefficients of multivariable model SNN.
| Predictor | B-coefficient | 95% CI | P-value |
|---|---|---|---|
| Intercept | 7.248 | (4.985 to 9.511) | <0.001 |
| Weight | 0.072 | (0.046 to 0.098) | <0.001 |
| NN | 0.303 | (0.169 to 0.437) | <0.001 |
Note: SNN; sternal-notch-to-nipple distance, NN; nipple-to-nipple distance.
Table 6.
Clinical translation of mean. minimum and maximum algorithm variables represented by corresponding case subjects.
| Age | Weight | ||||||
|
Subject 1
(min) |
Subject 2
(mean) |
Subject 3
(max) |
Subject 4
(min) |
Subject 5
(mean) |
Subject 6
*
(max) |
||
| Age | 18 | 31 | 74 | 23 | 21 | 26 | |
| Weight | 70 | 75 | 82.0 | 61 | 79 | 113.5 | |
| CC | 89.1 | 91 | 98.0 | 81.6 | 84.4 | 117.0 | |
| AUX-AUX | 41.4 | 40.4 | 40.3 | 37.5 | 39.6 | 40.2 | |
| NN | Calculated | 21.7 | 22.4 | 22.4 | 20.3 | 21.5 | 26.2 |
| Measured | 21.8 | 21.3 | 21.3 | 19.5 | 21.5 | 27.5 | |
| Difference | 0.1 | −1.0 | 1.1 | −0.8 | 0 | 1.3 | |
| SNN | Calculated | 18.9 | 19.4 | 19.4 | 17.8 | 19.4 | 23.4 |
| Measured | 18.2 | 20.1 | 20.1 | 17.9 | 19.2 | 23.3 | |
| Difference | −0.7 | 0.7 | 0.7 | 0.1 | −0.2 | −0.1 | |
| CC | AUX-AUX | ||||||
|
Subject 7
(min) |
Subject 8
(mean) |
Subject 9
*
(max) |
Subject 10
(min) |
Subject 11
(mean) |
Subject 12
(max) |
||
| Age | 18 | 26 | 26 | 26 | 19 | 35 | |
| Weight | 65 | 70.0 | 113.5 | 85 | 74 | 91 | |
| CC | 78.3 | 93.5 | 117.0 | 97.3 | 80.3 | 96.2 | |
| AUX-AUX | 36.3 | 41.2 | 40.2 | 34.4 | 41.1 | 47 | |
| NN | Calculated | 19.8 | 22.4 | 26.2 | 22.4 | 21.0 | 24.6 |
| Measured | 19.9 | 22.2 | 27.5 | 21.2 | 19.3 | 25 | |
| Difference | 0.1 | −0.2 | 1.3 | −1.2 | −1.7 | 0.4 | |
| SNN | Calculated | 17.9 | 19.1 | 23.4 | 20.2 | 19.0 | 21.3 |
| Measured | 17.2 | 18.8 | 23.3 | 20 | 18.3 | 21.2 | |
| Difference | −0.7 | −0.3 | −0.1 | −0.2 | −0.6 | −0.1 | |
Note: CC: chest circumference; AUX-AUX: anterior-axillary-fold to anterior-axillary-fold; NN: nipple-to-nipple distance; SNN: sternal-notch-to-nipple distance.
Subject 6 and 9 are the same patient.
SNN model development
In total, 2 predictors were selected using best subset regression (NN, weight) (Table 2). The algorithm can best be expressed as the following formula: SNN = 7.248 + 0.303*NN + 0.072*weight. R-squared and MSE were 0.51 and 1.43, respectively. R-squared dropped to 0.50 after bootstrapping. Assumptions of the linear model were not violated and the predicted values of SNN were not significantly different from observed values (paired t-test: P > 0.99).
Sensitivity analyses
Sensitivity test confirmed the robustness of the model. Running the model on the four other imputed datasets resulted in similar coefficients and significance, as did the pooled model (Supplementary Tables 6 and 7). Incorporating the predicted value of NN instead of the observed value of NN in the model for SNN resulted in a R-squared of 0.49 (compared with 0.50 when including the observed NN) with good agreement between the predicted SNN and observed SNN (paired t-test: P > 0.99).
Clinical translation
A depiction of how to apply the algorithm in practice is shown in Figure 2. After calculating the NN and SNN, the first step is to draw out a centralized NN-line as a horizontal line. Subsequently, the SNN should be drawn or measured to intersect with the corners of the NN-line, or the perpendicular axis of the NN-borders. This approach allows for the best translation of the calculated NN and SNN onto the blank chest. Furthermore, to illustrate the applicability of the algorithm on both the mean values as well as on the outliers, a clinical translation was performed for outliers on each included variable (age, weight, CC and AUX-AUX). A subject was extracted from the database based on the mean, minimum and maximum value of each variable included in the final model. We therefore applied the models in the following outliers for age (18 and 74 years old), weight (61.0 and 117.0 kg), CC (78.3 and 117.0 cm) and AUX-AUX (34.4 and 47.0 cm). This resulted in 11 subjects; as one patient was the outlier of both weight and CC. The different habitus of subjects 4, 5 and 6 are illustrated in Figure 3. Within these patients with the mean and outlier variables, the range of error for NN was −1.7 to 1.1 and −0.7 to 0.7 for SNN.
Figure 2.
A depiction of how to apply the algorithm in the clinical setting.
Figure 3.
Illustration of the habitus of subject 4 (ectomorph), 5 (mesomorph) and 6 (endomorph) as presented in Table 6.
Comparison to other proposed NAC-algorithms
Five known algorithms of which three for NN and two for SNN were tested for external validation using the data of the present cohort. The outcomes are presented in Table 7. Most algorithms performed worse in predicting the nipple position compared to using the mean of NN and SSN values. As an example for NN calculations, on average, Schulman was 12.7% off, whereas our model was on average 4.1% off.
Table 7.
Statistical comparison to other proposed NAC-algorithms.
| Measure | Author(s) | Algorithm | MSE (95% CI) | MAPE (95% CI) | R 2 |
|---|---|---|---|---|---|
| NN | Timmermans et al. (this study) | NN = 4.11 + (0.035 * age + 0.041 * weight + 0.093 * CC + 0.14 * AUX-AUX) | 1.37 (1.08–1.68) | 4.1% (3.6–4.6) | 0.650 |
| Beer et al. Beer et al., 2001) | NN = 2 * (2.4 + 0.09 * CC) | 3.48 (2.74–4.23) | 6.4% (5.7–7.1) | 0.112 | |
| Atiyeh et al. (2009) | NN = 0.618 * AUX-U | 5.06 (3.91–6.22) | 8.0% (7.0–9.0) | −0.291 | |
| Schulman et al. (2001) | NN = 2.192 + (0.19 * CC) | 10.61 (9.23–12.0) | 12.7% (11.9–13.6) | −1.704 | |
| SNN | Timmermans et al. (this study) | SNN = 7.248 + (0.303 * NN + 0.072 * weight) | 1.43 (1.13–1.74) | 4.7% (4.1–5.3) | 0.510 |
| Schulman et al. (2001) | SNN = (0.12 * height) − 2.782 | 3.58 (2.79–4.38) | 7.2% (6.4–8.1) | −0.210 | |
| Beckerstein et al. (1996) | SNN = 11.1 + (0.13 * height in inches) | 3.11 (2.54–3.70) | 7.6% (6.7–8.5) | −0.057 |
Note: AUX-AUX: anterior-axillary-fold to anterior-axillary-fold; NN: nipple-to-nipple distance; SNN: sternal-notch-to-nipple distance; AUX-U: anterior-axillary-fold-to-umbilicus, MSE: mean squared error, MAPE: mean absolute percentage error.
Predicted NAC position versus NAC position after masculinization surgery
We analyzed a total of 96 trans men following gender-affirming mastectomy. All had undergone a double incision mastectomy at the inframammary level with free nipple grafting. After imputing the five variables needed for the algorithm (age, weight, CC, AUX-AUX and the calculated NN), the horizontal and vertical coordinates of the NAC significantly differed from what would be predicted from the NN and SNN models: the measured NN was 19.8 (SD 2.2) versus the calculated NN of 20.7 cm (SD 1.9, p ≤ 0.001), and the measured SNN was 16.2 cm (SD 1.8) versus the calculated SNN of 18.4 cm (SD 1.5, p ≤ 0.001). This implies that on average the NAC was positioned too close together and too high on the chest, compared to cisgender males with similar chest dimensions.
Discussion
Nipple areolar complex (NAC) positioning in men has been studied to a far less extent than in women (Lewin et al., 2016). Therefore, no widely accepted standard of care exists to assist in positioning the NAC during subcutaneous mastectomy. A common practice remains eyeballing, often in combination with using a set of fixed values or anatomic markers. But these methods sometimes fall short, and if body proportions are not well-considered, might lead to unsatisfactory results (Ayyala et al., 2020; Lo Russo et al., 2017; McEvenue et al., 2018; Monstrey et al., 2008; Tanini & Lo Russo, 2018). In order to enable accurate prediction of NAC position, two accompanying models were developed to predict nipple-to-nipple distance (NN) and sternal-notch-to-nipple distance (SNN). The outcomes of the sensitivity analyses justifies this stepwise approach and the use of the calculated NN when calculating SNN. Furthermore, these models are based on patient demographics and anthropometric body dimension, and therefore allow for a highly individualized and proportionate positioning of the NAC in the pre-operative setting. The wide range of the dependent variables and resulting NN and SNN with small margins of error attest to the applicability of our algorithm on our Dutch population. This means that the NAC position is predicted accurately for widely varying chest dimensions.
Importantly, specific consideration was given to only include pre-surgically measurable variables such as chest circumference, and not breast circumference or sternal-notch-to-umbilicus, and not axillary-fold-to-umbilicus. Another consideration was that the variables should be easily measurable without the assistance of highly specialized devices such as 3-D cameras. Furthermore, all measurements were performed with the arms at a 45 degree angle from the body. In performing this study, we saw no change of nipple position between the 45 degree angle and when arms were placed alongside the body. Therefore, this algorithms also applies to the perioperative setting where the arms are commonly placed alongside the body. Altogether, the personalized approach to NAC-positioning lends itself perfectly as a translational tool from the consulting room to the surgical theater.
When specifically looking at the algorithm composition, the appearance of age in predicting NN tells us that with the increase of age, the NN and SNN increases. This reflects the change of body proportions due to aging. The association between age and NAC position in men has not been described before, but is already known in women (Kono et al., 2018). In both models weight was found to be a positive predictor. Prior studies have shown an association between BMI and position of the NAC; suggesting that nipples tend to lateralize with increased BMI (Kasai et al., 2015; Vaucher et al., 2016). Also, the Yue et al. model found that de SNN increases with increased BMI (Yue et al., 2018). At first, chest circumference (CC) and a broader chest (AUX-AUX) was found as a predictor for NN distance, corresponding to findings of earlier published models, including Beer et al. (2001) and Shulman et al. (2001). However, Atiyeh et al mentioned the U-AX distance as predictor of the inter nipple distance (Atiyeh et al., 2009), a finding that we were not able to confirm due to our variable selection criteria. As the horizontal coordinates of the NAC lays in the same horizontal plane as the CC and AUX-AUX, these values are more likely to predict for the NN than U-AX. Interestingly, no variable on the vertical axis was found to be predictive for SNN which is also a vertical vector.
Equations similar to ours have been proposed, which also consider anatomic variability to be dependent on body composition and patient factors such as age. We tested these algorithms using our data and they all scored substandardly in predicting the nipple positions in our cohort. Unfortunately, none of the studies reported performance measures, such as R-squared, of their models and we were forced to externally validate the proposed algorithms using our data. This precludes direct comparison of the performance of our model with the previous models. Furthermore, we evaluated current practice according to our models. The outcomes underlined and objectified an anecdotally known problem in the current practice, which is the placement of nipples too high or too wide on the chest (Beckenstein et al., 1996; Berry et al., 2012; Hage & van Kesteren, 1995). The algorithm was able to significantly objectify this shortcoming in standard practice and underlines the importance of a more personalized and standardized approach. Conclusively, the previously reported algorithms performed disappointingly at predicting NAC positioning of our trans male cohort and objectified the shortcomings of current practice.
In addition to the use of algorithms, other attempts have been made to standardize nipple repositioning such as the use of mean values. A review study found that the average SNN was 19.3 cm and the average NN was 22.3 cm, which were both slightly smaller than our SNN of 19.9 cm and NN of 23.0 cm (Maas et al., 2020). Regardless of the similarity of outcomes, applying a universal mean distances does not take the interpatient variability into account (Yue et al., 2018). Similarly, the use of anatomic landmarks for NAC repositioning has been propagated. Different examples exist such as; positioning between the fourth and fifth or fifth and sixth intercostal space, a set 5 mm above the horizontal incision or using the lateral border of the pectoral muscle (Ayyala et al., 2020; Hage & van Kesteren, 1995; Lo Russo et al., 2017; McEvenue et al., 2018; Monstrey et al., 2008; Tanini & Lo Russo, 2018). Even though the use of means and landmarks is highly reproducible and practical, no account is taken of the notion that shape and proportions of the body can differ greatly between cisgender men and transgender men. Especially the notion of using fixed distances in transgender men seems to fail to consider that the generally shorter and narrower chest seen in transgender men, does usually not allow for the fixed measurements founds in cisgender men. The use of consolidated cis male means might therefore result an overly lateralized and lowered position of nipples in transgender men.
This study has several limitations worth addressing. Firstly, most of the volunteers participating in this study were employees or students of the hospital. This might be a biased representation of the general population. Secondly, since participants contribute to this study on a voluntary basis, people who felt more insecure about their body appearance might more easily decline participation, resulting in selection bias. Importantly, no restrictions were placed on age with the intention to resemble the normative cisgender male population. However, the average age of patients undergoing a subcutaneous mastectomy as part of gender-affirming surgeries was found to lie around 26 years in two high-volume clinics, which is highly similar to the included population (McEvenue et al., 2018; van de Grift et al., 2017). Lastly, mainly Caucasian men participated in this study. As addressed by Maas et al., this could be a limitation to the general applicability to populations with more divergent ethnic groups (Kaoutzanis et al., 2020; Kasai et al., 2015). Further research should be undertaken with more focus on ethnicity. Nevertheless, this ethnic composition is a comparable representation of the Dutch population and therefore remains applicable to our specific population. Furthermore, in our model we could only perform internal validation of model performance, as a proper external validation requires a cohort from another center. Conversely, the prospectively collected cohort of trans men allowed for the retrospective analysis of current practice. Therefore, in line with the methodology for proposing predictive models, a second phase of this study is warranted for the collection of an unrelated cohort of cis men for testing the external validity of the algorithm. In future endeavors, we will also aim to elaborately explore the relationship between nipple anthropometry and mastectomy technique with patient reported outcome measures. Regardless of some of the aforementioned limitations, we believe this study has allowed for a statistically reliable and validated approach to personalize the position of the NAC during masculinizing subcutaneous mastectomy.
Acknowledgements
We would like to thank all the participants of this study for their contribution.
Ethical issue
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The Ethics Board for Research (Medisch Ethische Toetsingscommissie) of the VU Medical Center in Amsterdam approved the execution of this study and is registered as 2017.431.
Funding
The authors have the following to disclose: None.
Disclosure statement
The authors declare that they have no conflict of interest.
References
- Agarwal, C. A., Wall, V. T., Mehta, S. T., Donato, D. P., & Walzer, N. K. (2017). Creation of an aesthetic male nipple areolar complex in female-to-male transgender chest reconstruction. Aesthetic Plastic Surgery, 41(6), 1305–1310. 10.1007/s00266-017-0935-7 [DOI] [PubMed] [Google Scholar]
- Atiyeh, B. S., Dibo, S. A., & El Chafic, A. H. (2009). Vertical and horizontal coordinates of the nipple-areola complex position in males. Annals of Plastic Surgery, 63(5), 499–502. 10.1097/SAP.0b013e3181953854 [DOI] [PubMed] [Google Scholar]
- Ayyala, H. S., Mukherjee, T. J., Le, T. M., Cohen, W. A., Luthringer, M., & Keith, J. D. (2020). A three-step technique for optimal nipple position in transgender chest masculinization. Aesthetic Surgery Journal, 40(11), 619–625. 10.1093/asj/sjaa150 [DOI] [PubMed] [Google Scholar]
- Beckenstein, M. S., Windle, B. H., & Stroup, R. T. Jr. (1996). Anatomical parameters for nipple position and areolar diameter in males. Annals of Plastic Surgery, 36(1), 33–36. 10.1097/00000637-199601000-00007 [DOI] [PubMed] [Google Scholar]
- Beer, G. M., Budi, S., Seifert, B., Morgenthaler, W., Infanger, M., & Meyer, V. E. (2001). Configuration and localization of the nipple-areola complex in men. Plastic and Reconstructive Surgery, 108(7), 1947–1952. 10.1097/00006534-200112000-00015 [DOI] [PubMed] [Google Scholar]
- Berry, M. G., Curtis, R., & Davies, D. (2012). Female-to-male transgender chest reconstruction: A large consecutive, single-surgeon experience. Journal of Plastic, Reconstructive & Aesthetic Surgery: JPRAS, 65(6), 711–719. 10.1016/j.bjps.2011.11.053 [DOI] [PubMed] [Google Scholar]
- Cohen, W. A., Shah, N. R., Iwanicki, M., Therattil, P. J., & Keith, J. D. (2019). Female-to-male transgender chest contouring: A systematic review of outcomes and knowledge gaps. Annals of Plastic Surgery, 83(5), 589–593. 10.1097/SAP.0000000000001896 [DOI] [PubMed] [Google Scholar]
- Cregten-Escobar, P., Bouman, M. B., Buncamper, M. E., & Mullender, M. G. (2012). Subcutaneous mastectomy in female-to-male transsexuals: A retrospective cohort-analysis of 202 patients. The Journal of Sexual Medicine, 9(12), 3148–3153. 10.1111/j.1743-6109.2012.02939.x [DOI] [PubMed] [Google Scholar]
- Hage, J. J., & van Kesteren, P. J. (1995). Chest-wall contouring in female-to-male transsexuals: Basic considerations and review of the literature. Plastic and Reconstructive Surgery, 96(2), 386–391. 10.1097/00006534-199508000-00019 [DOI] [PubMed] [Google Scholar]
- Harrell, F. E. (2006). Regression modeling strategies. Springer-Verlag. [Google Scholar]
- Kaoutzanis, C., Schneeberger, S. J., Wormer, B., Song, H., Ye, F., Al Kassis, S., Winocour, J., Higdon, K., & Perdikis, G. (2020). Current perceptions of the aesthetically ideal position and size of the male nipple-areola complex. Aesthetic Surgery Journal, 40(5), NP228–NP237. 10.1093/asj/sjz276 [DOI] [PubMed] [Google Scholar]
- Kasai, S., Shimizu, Y., Nagasao, T., Ohnishi, F., Minabe, T., Momosawa, A., & Kishi, K. (2015). An anatomic study of nipple position and areola size in Asian men. Aesthetic Surgery Journal, 35(2), NP20–27. 10.1093/asj/sju023 [DOI] [PubMed] [Google Scholar]
- Kono, T., Kusano, T., Sato, N., Yoshimoto, S., & Nakamura, S. (2018). Natural mastopexy repositioning based on age-related mean breast shape. Asian Journal of Surgery, 41(4), 295–300. 10.1016/j.asjsur.2016.12.005 [DOI] [PubMed] [Google Scholar]
- Lewin, R., Amoroso, M., Plate, N., Trogen, C., & Selvaggi, G. (2016). The aesthetically ideal position of the nipple-areola complex on the breast. Aesthetic Plastic Surgery, 40(5), 724–732. 10.1007/s00266-016-0684-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo Russo, G., Tanini, S., & Innocenti, M. (2017). Masculine chest-wall contouring in FtM transgender: A personal approach. Aesthetic Plastic Surgery, 41(2), 369–374. 10.1007/s00266-017-0796-0 [DOI] [PubMed] [Google Scholar]
- Maas, M., Howell, A. C., Gould, D. J., & Ray, E. C. (2020). The ideal male nipple-areola complex: A critical review of the literature and discussion of surgical techniques for female-to-male gender-confirming surgery. Annals of Plastic Surgery, 84(3), 334–340. 10.1097/SAP.0000000000002018 [DOI] [PubMed] [Google Scholar]
- McEvenue, G., Xu, F. Z., Cai, R., & McLean, H. (2018). Female-to-male gender affirming top surgery: A single surgeon’s 15-year retrospective review and treatment algorithm. Aesthetic Surgery Journal, 38(1), 49–57. 10.1093/asj/sjx116 [DOI] [PubMed] [Google Scholar]
- Miller, A. J. (1990). Subset selection in regression. Chapman and Hall. Publisher description http://www.loc.gov/catdir/enhancements/fy0744/89077350-d.html
- Monstrey, S., Selvaggi, G., Ceulemans, P., Van Landuyt, K., Bowman, C., Blondeel, P., Hamdi, M., & De Cuypere, G. (2008). Chest-wall contouring surgery in female-to-male transsexuals: A new algorithm. Plastic and Reconstructive Surgery, 121(3), 849–859. 10.1097/01.prs.0000299921.15447.b2 [DOI] [PubMed] [Google Scholar]
- Shulman, O., Badani, E., Wolf, Y., & Hauben, D. J. (2001). Appropriate location of the nipple-areola complex in males. Plastic and Reconstructive Surgery, 108(2), 348–351. 10.1097/00006534-200108000-00010 [DOI] [PubMed] [Google Scholar]
- Steyerberg, E. W. (2019). Overfitting and optimism in prediction models. In Clinical prediction models: A practical approach to development, validation, and updating (pp. 95–112). Springer International Publishing. 10.1007/978-3-030-16399-0_5 [DOI] [Google Scholar]
- Tanini, S., & Lo Russo, G. (2018). Shape, position and dimension of the nipple areola complex in the ideal male chest: A quick and simple operating room technique. Aesthetic Plastic Surgery, 42(4), 951–957. 10.1007/s00266-018-1131-0 [DOI] [PubMed] [Google Scholar]
- van de Grift, T. C., Elfering, L., Bouman, M. B., Buncamper, M. E., & Mullender, M. G. (2017). Surgical indications and outcomes of mastectomy in transmen: A prospective study of technical and self-reported measures. Plastic and Reconstructive Surgery, 140(3), 415e–424e. 10.1097/PRS.0000000000003607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Grift, T. C., Elfering, L., Greijdanus, M., Smit, J. M., Bouman, M. B., Klassen, A. F., & Mullender, M. G. (2018). Subcutaneous mastectomy improves satisfaction with body and psychosocial function in Trans men: Findings of a cross-sectional study using the BODY-Q Chest Module. Plastic and Reconstructive Surgery, 142(5), 1125–1132. 10.1097/PRS.0000000000004827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van de Grift, T. C., Kreukels, B. P., Elfering, L., Ozer, M., Bouman, M. B., Buncamper, M. E., Smit, J. M., & Mullender, M. G. (2016). Body image in transmen: Multidimensional measurement and the effects of mastectomy. The Journal of Sexual Medicine, 13(11), 1778–1786. 10.1016/j.jsxm.2016.09.003 [DOI] [PubMed] [Google Scholar]
- Vaucher, R., Dast, S., Assaf, N., & Sinna, R. (2016). Anatomical study of men’s nipple areola complex. Annales de Chirurgie Plastique Esthétique, 61(3), 206–211. (Etude anatomique du complexe aerolo-mamelonnaire (CAM) chez l’homme.) 10.1016/j.anplas.2016.01.002 [DOI] [PubMed] [Google Scholar]
- Veen, K. M., de Angst, I. B., Mokhles, M. M., Westgeest, H. M., Kuppen, M., Groot, C. A. U., Gerritsen, W. R., Kil, P. J. M., & Takkenberg, J. J. M. (2020). A clinician’s guide for developing a prediction model: a case study using real-world data of patients with castration-resistant prostate cancer. Journal of Cancer Research and Clinical Oncology, 146(8), 2067–2075. 10.1007/s00432-020-03286-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolter, A., Diedrichson, J., Scholz, T., Arens-Landwehr, A., & Liebau, J. (2015). Sexual reassignment surgery in female-to-male transsexuals: An algorithm for subcutaneous mastectomy. Journal of Plastic, Reconstructive & Aesthetic Surgery: JPRAS, 68(2), 184–191. 10.1016/j.bjps.2014.10.016 [DOI] [PubMed] [Google Scholar]
- Yue, D., Cooper, L. R. L., Kerstein, R., Charman, S. C., & Kang, N. V. (2018). Defining normal parameters for the male nipple-areola complex: A prospective observational study and recommendations for placement on the chest wall. Aesthetic Surgery Journal, 38(7), 742–748. 10.1093/asj/sjx245 [DOI] [PubMed] [Google Scholar]