Abstract
Background:
The use of hyaluronic acid (HA) fillers for correcting nasal deformities offers an increasingly popular alternative to surgical rhinoplasty. However, this can sometimes be extremely challenging, for example, in patients with a permanent defect in the nasal septum secondary to chronic drug use.
Methods:
We report a case in which nonsurgical intervention with a high G’ HA filler was used therapeutically to improve the permanent nasal disfigurement of an individual with previous long-term drug use (now in remission)
Results:
This approach led to high levels of patient satisfaction and empowerment in her personal and professional life. Despite the high risk in this case, only immediate minor complications were recorded, including temporary edema and ecchymoses, and these resolved spontaneously
Conclusions:
Nonsurgical treatment using an appropriate HA filler may offer a safe and effective option in selected patients with nasal deformities resulting from pathological conditions.
Surgical intervention remains the gold standard in “cocaine nose” reconstruction. However, this case shows that injection of a high G’ HA filler, based on a systematic approach to treatment, can offer a safe and effective option, with high levels of resulting patient satisfaction. Although not suitable for more severe deformities, the same may also be possible in other individuals with milder forms of permanent nasal damage resulting from previous pathologies. To avoid tragic complications, it is essential for physicians to have a high degree of familiarity with nasal anatomy, but this type of procedure should nonetheless be considered in appropriately selected patients.
Takeaways
Question: Cases of “cocaine nose” after chronic drug use can be difficult to treat surgically owing to the high risks associated with poor circulation and scarring. Could nonsurgical approaches offer an alternative?
Findings: This case demonstrates the utility of a high G’ hyaluronic acid filler for the aesthetic improvement of nasal bridge deformity in a 32-year-old woman with previous chronic drug use (now in remission). The patient experienced no major complications, high levels of satisfaction, and meaningful empowerment in her personal and professional life.
Meaning: Injection of a high G’ hyaluronic acid filler may be a safe and effective alternative to surgery in such patients.
INTRODUCTION
The popularity of nonsurgical rhinoplasty has been increasing in recent years, particularly procedures based on hyaluronic acid (HA) fillers. Compared with surgical approaches, HA fillers can reduce the short-term financial burden on patients, eliminate the need for an extended recovery period, and offer instant results with high rates of patient satisfaction.1–3 In the nose, these products are primarily used for aesthetic purposes (such as beautification, harmonization, or treatment of the signs of aging), but there have also been cases of functional improvement (eg, those relating to internal valve collapse).4
In addition, nonsurgical rhinoplasty has potential to correct nasal deformities secondary to pathological processes, such as cases of “cocaine nose” after chronic drug use. In these individuals, repeated vascular constriction and tissue necrosis leads to loss of supporting cartilage, scarring, and eventual collapse of the nose, with relative sparing of the overlying skin.5,6 This causes permanent disfigurement and may result in a significant social and emotional burden.
A cocaine-injured nose typically has poor circulation and scarring, and hence, surgical manipulation carries a very high risk for infection and delayed healing. As such, in selected patients, nonsurgical approaches may offer a valuable alternative.
CLINICAL CASE
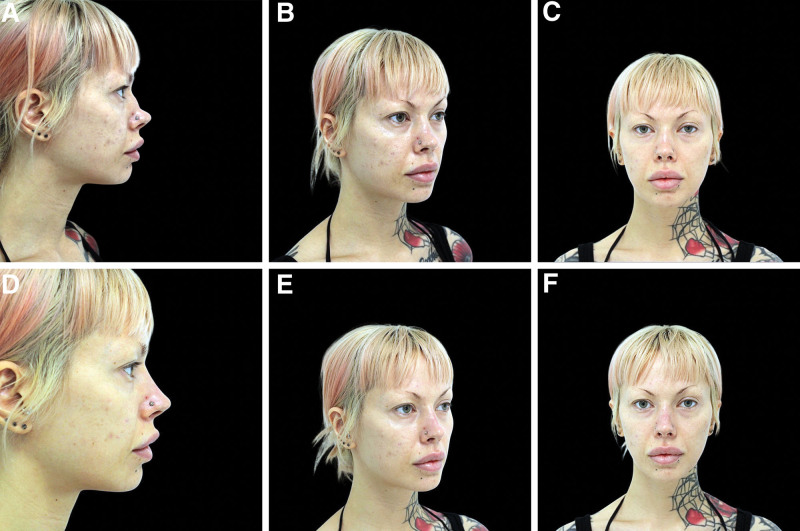
In June 2021, a 32-year-old woman presented with a previous history of long-term drug use during adolescence and early adulthood, including cocaine, heroin, and methamphetamines. She was now in complete remission, but complained of chronic nasal bridge deformity as a result of her past drug use and sought nonsurgical correction (Fig. 1A–C).
Fig. 1.
The patient before (A–C) and after (D–F) initial treatment with 0.6 mL of VYC-25L.
Treatment was performed using 0.6 mL of the high G’ HA filler, VYC-25L (Allergan Aesthetics, AbbVie, Irvine, Calif.). Three key anatomical areas were identified: the radix, rhinion, and supratip. Injections were made deep into the dorsum of the nose, periosteal at the radix; perichondral at the site of deformity past the rhinion, where the upper lateral cartilage was permanently damaged; and at the supratip. A 30G needle was used for all procedures, based on an initial bolus followed by retrograde injection. The aims were to create a straight bridge in full profile and to elevate the dorsum of the nose (Fig. 1D–F).
Several safety measures were instituted to mitigate the associated risk: thorough cleansing of the nose and surrounding area with chlorhexidine pre- and posttreatment, injection into the midline where possible, use of aspiration as a safety checkpoint, slow product administration, thorough patient briefing on appropriate aftercare, and follow-up telephone calls on the 2 days after treatment.7,8
Following the procedure, the patient experienced transient edema (lasting ~10 days) and minor ecchymoses. There were no other complications, such as asymmetry, infection, vascular occlusion, or necrosis. Patient satisfaction was assessed using the validated, standardized FACE-Q Nose and FACE-Q Outcome questionnaires, with perfect scores recorded, thus demonstrating high levels of satisfaction.
The patient returned 18 months later. No lumps, granulomas, or nodules had developed during the intervening period. Furthermore, the dorsum of the nasal bridge continued to be significantly elevated, and only mild decline was noted. Maintenance treatment was performed using 0.3 mL of VYC-25L (Fig. 2). She again experienced transient edema lasting ~10 days, but no ecchymoses, infection, asymmetry, vascular occlusion, or necrosis was observed. The patient had a subsequent follow-up visit 6 weeks later, and no further issues were identified.
Fig. 2.
The patient before (A–C) and after (D–F) retreatment with 0.3 mL of VYC-25L performed 18 months after the initial treatment.
DISCUSSION
With its high rates of patient satisfaction,1–3,9 nonsurgical rhinoplasty has potential to offer a valuable alternative to surgery in selected individuals, including those with permanent deformity as a result of pathological conditions. It is well known that nonsurgical rhinoplasty carries an increased risk of catastrophic adverse events compared with many other nonsurgical facial aesthetic procedures.10 Furthermore, cases like this one are at even greater risk due to vascular and soft-tissue changes resulting from previous trauma. A high level of expertise and a deep knowledge of nasal anatomy are therefore essential. Other risk reduction strategies must also be considered. In particular, injections should be delivered deep and into the midline of the nose (where possible) to reduce the risk of intravascular placement. The present author favors preinjection aspiration; although controversial in some quarters, this practice can be a valuable checkpoint when used alongside other safety measures.7 Clinicians must always be vigilant for any unexpected pain or blanching that could be an indicator of intravascular injection.7 In addition, practitioners should have preset protocols in place for managing major complications in the rare instances when they do occur.
A small amount of HA filler is generally sufficient when treating the nose. Overcorrection must be avoided to prevent unfavorable aesthetic outcomes and minimize the risk of compression of the surrounding vasculature, and in turn, catastrophic adverse effects.11
The modifications to this patient’s appearance were life changing. She described having increased self-esteem and self-confidence, and was able to further her career, obtaining a position in her desired field of work (where she had previously experienced difficulties owing to her disfigurement). Moreover, she reported significant improvements in social aspects of her life, as well as her emotional state. This case highlights the therapeutic potential of nonsurgical aesthetic procedures, particularly to the nose, demonstrating compelling patient empowerment with regard to both her personal and professional life.
DISCLOSURE
The author has no financial interest to declare in relation to the content of this article.
PATIENT CONSENT
The patient provided written consent for the use of her image.
ACKNOWLEDGMENT
This article discusses an off label use of VYC-25L, which is currently approved by the U.S. Food and Drug Administration for nonsurgical lower face augmentation.
Footnotes
Disclosure statements are at the end of this article, following the correspondence information.
REFERENCES
- 1.Rauso R, Colella G, Zerbinati N, et al. Safety and early satisfaction assessment of patients seeking nonsurgical rhinoplasty with filler. J Cutan Aesthet Surg. 2017;10:207–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bertossi D, Malchiodi L, Albanese M, et al. Nonsurgical rhinoplasty with the novel hyaluronic acid filler VYC-25L: results using a nasal grid approach. Aesthet Surg J. 2021;41:NP512–NP520. [DOI] [PubMed] [Google Scholar]
- 3.Kumar V, Jain A, Atre S, et al. Non-surgical rhinoplasty using hyaluronic acid dermal fillers: A systematic review. J Cosmet Dermatol. 2021;20:2414–2424. [DOI] [PubMed] [Google Scholar]
- 4.Nyte CP. Spreader graft injection with calcium hydroxylapatite: a nonsurgical technique for internal nasal valve collapse. Laryngoscope. 2006;116:1291–1292. [DOI] [PubMed] [Google Scholar]
- 5.Millard DR, Mejia FA. Reconstruction of the nose damaged by cocaine. Plast Reconstr Surg. 2001;107:419–424. [DOI] [PubMed] [Google Scholar]
- 6.Guyuron B, Afrooz PN. Correction of cocaine-related nasal defects. Plast Reconstr Surg. 2008;121:1015–1023. [DOI] [PubMed] [Google Scholar]
- 7.Heydenrych I, De Boulle K, Kapoor KM, et al. The 10-point plan 2021: updated concepts for improved procedural safety during facial filler treatments. Clin Cosmet Investig Dermatol. 2021;14:779–814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Swift A, Remington K, Frank K, et al. Superficial nasal filler injections—how I do it. Facial Plast Surg Clin North Am. 2022;30:183–191. [DOI] [PubMed] [Google Scholar]
- 9.Radulesco T, De Bonnecaze G, Penicaud M, et al. Patient satisfaction after non-surgical rhinoplasty using hyaluronic acid: a literature review. Aesthetic Plast Surg. 2021;45:2896–2901. [DOI] [PubMed] [Google Scholar]
- 10.Kapoor KM, Kapoor P, Heydenrych I, et al. Vision loss associated with hyaluronic acid fillers: a systematic review of literature. Aesthetic Plast Surg. 2020;44:929–944. [DOI] [PubMed] [Google Scholar]
- 11.Chen Q, Liu Y, Fan D. Serious vascular complications after nonsurgical rhinoplasty: a case report. Plast Reconstr Surg Glob Open. 2016;4:e683. [DOI] [PMC free article] [PubMed] [Google Scholar]