Abstract
Objectives
To provide a longitudinal analysis of how functional decline over time among older adults affects provision of family and unpaid care, overall and stratified by dementia status.
Methods
Longitudinal cohorts of community-dwelling adults ≥65 years between 2015 and 2017 from the National Health and Aging Trends Study (NHATS; n = 5,103) and their caregivers from the National Study of Caregiving (n = 862 caregivers for 595 NHATS care recipients). A panel data fixed-effects model was used to examine how increases in mobility, self-care, and household activity-related impairment between 2015 and 2017 affected family and unpaid care (care recipient reported: total number of family and unpaid caregivers, total hours of care received; caregiver reported: hours of care provided, caregiving-related emotional, and physical difficulties).
Results
Among community-dwelling older adults overall, impairment in 1 additional self-care activity led to 0.12 more caregivers and 19 additional total monthly hours of care. Among those with dementia, impairment in 1 additional self-care activity led to 0.14 more caregivers and 28 additional total monthly hours of care; among those without dementia, this was 0.11 caregivers and 15 total monthly hours of care. For dementia caregivers, impairment in 1 additional self-care activity among their care recipients led to 8% higher probability of caregiving-related emotional difficulty.
Discussion
There is a mismatch between the large additional hours of care received by older adults who experience functional decline (particularly self-care activities) and the relatively small accompanying increase in family and unpaid caregivers. Targeted functional supports, particularly for self-care activities, may benefit both older adults and their caregivers.
Keywords: Caregiving-related difficulties, Family and unpaid caregivers, Functional impairment, Hours of care, National Health and Aging Trends Study
Functional decline is common among older adults (Freedman & Spillman, 2014; Gill et al., 2010; Johnson & Wiener, 2006) and may lead to increased caregiving needs from family and other unpaid caregivers (Riffin et al., 2017) and increased caregiving-related stress among these caregivers (Spillman et al., 2014). However, how the rate of functional decline is actually linked to the increased care needs—that is, from more total caregivers, existing caregivers providing more hours of care, or both—from family and other unpaid care (hereafter family care) partners is less clear. As the U.S. population ages (Ortman et al., 2014) and the size of American families continues to decline (Redfoot et al., 2013), there is a growing gap between the demand and supply of family care (National Academies of Sciences, Engineering, and Medicine, 2016). Therefore, it is critical to understand how family care and caregiving-related experiences change as older adults’ function declines. This study provides empirical evidence using nationally representative data on changes in family care related to functional decline in older adults and offers implications for policy and interventions regarding improved supports for family care as older adults’ function declines.
Cross-sectional studies indicate that functional impairment is associated with larger caregiver networks (i.e., more family and unpaid caregivers) and more hours of care older adults receive from these networks (Johnson & Wiener, 2006; Pego & Nunes, 2017; Spillman et al., 2014). Also, older adults’ caregiving networks change over time, with increasing reliance on more intensely engaged generalist caregivers that assist in multiple domains of functional tasks as opposed to providing specialized care with only one task type, particularly for those living with dementia (Spillman et al., 2020). Yet it is unclear whether or how this change in caregiving over time is specifically related to older adults’ functional decline. In addition, cross-sectional studies test the association between older adults’ functional decline and caregivers’ caregiving-related difficulties (Parker et al., 2022; Polenick, Leggett, et al., 2020; Polenick, Min, et al., 2020). Yet it is unclear how caregiving-related difficulties change over time as care recipient’s function declines.
Although functional decline is common among older adults for a number of reasons, it is a defining feature of dementia (MacNeil Vroomen et al., 2018; Sheehan, 2012). For example, functional status is a defining feature of the Functional Assessment Staging Test to determine the stage and severity of dementia (Reisberg et al., 2010). Dementia may also contribute directly to the disablement process, from household activities to mobility or self-care activities (Barberger-Gateau et al., 2004). Functional decline among older adults living with dementia undoubtedly contributes to the substantial burden experienced by their caregivers. For example, data from the National Health and Aging Trends Study (NHATS) shows that, for community-dwelling older adults, one-third of all caregivers and 41% of all the hours of care provided are for the 10% of those older adults living with dementia (Kasper, Freedman, Spillman, & Wolff, 2015). Caregivers for older adults with dementia provide more hours of care on average than for those without dementia, even though there are also more caregivers in their networks (Kasper, Freedman, Spillman, & Wolff, 2015). Caregivers for older adults with dementia also more often report caregiving-related emotional and physical difficulties (Chi et al., 2019; Mahoney et al., 2005; Parker et al., 2022; Wolff et al., 2018). Given the outsize demands of dementia-related caregiving, and the illness-defining role of functional impairment in dementia, it is imperative to understand the trajectory of functional impairment and caregiving, and whether this is consistent for all older adults or is fundamentally different for those living with dementia.
About 60% of older adults receive assistance from a broad caregiver network (i.e., with two or more family members and unpaid caregivers; Kasper, Freedman, Spillman, & Wolff, 2015). According to the task-specific model of caregiver selection (Litwak, 1985), the development of a caregiving network depends on a combination of the fit between assistance needed and the potential caregivers available, such as spouses or adult children, friends or neighbors, and paid caregivers to fulfill such needs. When older adults’ function declines, assistance for these additional functional tasks is needed, which requires more caregiving support and potentially a larger caregiver network. However, the size of caregiver network might depend on the potential caregivers available. Therefore, the increasing caregiving needs might fall upon a larger caregiver network, or higher caregiving intensity from existing caregivers if there are no available caregivers in their network, or both. In addition, because the assistance in self-care activities might be more likely to be time-consuming than other tasks (Freedman & Spillman, 2014; Johnson & Wiener, 2006), the decline in self-care activities might lead to the largest increase in family care including total number of family and unpaid caregivers and total hours of care older adults received from them. Using Litwak’s framework, we focus on the interplay of types of functional tasks performed by caregivers and change of family care for community-dwelling older adults and their caregivers, overall and by dementia status of care recipients. We particularly look at how functional decline (i.e., in mobility, self-care, and household activities) over time affects family care (i.e., care from more total caregivers, existing caregivers providing more hours of care, or both).
In addition, according to the stress process model of caregiving, objective care stressors (e.g., care recipients’ cognitive and functional impairment) can heighten subjective caregiving-related stress that negatively impacts caregivers’ well-being (Pearlin et al., 1990). Hence, it is plausible that functional decline, particularly among older adults with dementia, may lead to increased caregiving-related emotional and physical difficulties. We particularly look at how functional decline over time among care recipients affects the change of caregiving-related emotional and physical difficulties among caregivers.
We use longitudinal data from the NHATS linked with the National Study of Caregiving (NSOC) in 2015 and 2017 to examine (1) older adult functional decline over time and the associated change in family care (i.e., number of family and unpaid caregivers, total hours of care older adults received from these caregivers, hours of care provided by each caregiver, and caregiving-related emotional and physical difficulties for each caregiver), and (2) whether the impact of functional decline on change of family care differs by dementia status of care recipients. To our best knowledge, this study provides the first longitudinal analysis of functional decline over time and the associated changes in the provision of family care, leveraging the unique advantages of two nationally representative surveys of older adults and their caregivers (i.e., NHATS and NSOC, respectively). We hypothesized that functional decline over time would lead to: more family and unpaid caregivers; additional total hours of care older adults received from them; more hours of care provided by individual caregivers; and higher rates of caregiving-related emotional and physical difficulties. We further hypothesized that the impact of functional decline on change of family care outcomes would be larger among older adults living with dementia and their caregivers giving the outsize demands of dementia-related caregiving.
Method
Data and Study Population
We used data from the NHATS linked with the NSOC in 2015 and 2017. Both are ongoing longitudinal, nationally representative studies of older adults (i.e., NHATS respondents) and their caregivers (i.e., NSOC respondents; Freedman et al., 2020; Freedman, Schrack, et al. 2022). Leveraging the longitudinal data from both NHATS and NSOC allows us to jointly capture the change of functional status and family care from the perspectives of both older adults and their caregivers.
NHATS samples participants from among Medicare enrollees aged ≥65 years who live in the contiguous U.S.; enrolled respondents are interviewed annually (Freedman, Schrack, et al., 2022). Of 7,859 respondents in 2015, 5,695 were followed in 2017. We excluded respondents who lived in a residential care or nursing home setting in 2015 and/or 2017 (n = 592), because their pattern of family care is quite different from that of community-dwelling respondents (Coe & Werner, 2022). We finally included a longitudinal analytic cohort of 5,103 community-dwelling older adults who participated in both the 2015 and 2017 interviews. Proxy respondents (mostly family members) were interviewed when the sample person could not respond and participated on behalf of 2% of all the community-dwelling NHATS respondents, specifically 32% for those with dementia and 0.4% for those without dementia.
The presence of dementia was determined using the NHATS-developed probable dementia classification (vs possible or no dementia), determined by any of: (1) self- or proxy-report of dementia diagnosis; (2) a score of ≥2 on the AD8 Dementia Screening Interview administrated to proxy respondents; or (3) scoring ≥1.5 standard deviations below the mean in ≥2 domains on cognitive tests of memory, orientation, and executive function (Kasper et al., 2013; Kasper, Freedman, Spillman, Skehan, et al. 2015). The probable dementia criteria in NHATS have strong sensitivity and specificity and are validated against a 3–4 hr structured in-person assessment and clinical consensus diagnosis from another nationally representative survey, Aging, Demographics, and Memory Study (Kasper et al., 2013). Among the longitudinal analytic cohort of 5,103 community-dwelling older adults, 627 (12%) had probable dementia in 2015 and/or 2017.
The NSOC is a supplement of NHATS that surveys family and unpaid caregivers of NHATS participants who received assistance with mobility, self-care, and/or household activities due to health or functioning reasons (Freedman et al., 2020). Up to five caregivers per care recipient (i.e., NHATS respondent) are included in NSOC. Of 2,204 NSOC caregiver respondents in 2015, 1,453 were reinterviewed in 2017. We excluded caregivers who did not provide assistance in the last month due to missing information on variables of interest such as caregiving-related emotional and physical difficulties (n = 61) and who provided assistance to older adults living in the residential care or nursing home settings in 2015 and/or 2017 (n = 530). A longitudinal cohort of 862 caregivers for 595 community-dwelling care recipients (i.e., NHATS respondents) was included from 2015 to 2017, among which 308 (29%) provided assistance for 206 care recipients living with dementia in 2015 and/or 2017. Here, we limited the analysis to the 595 NHATS care recipients who had NSOC caregivers to examine the impact of functional decline among care recipients on hours of care provided and caregiving-related emotional and physical difficulties for each individual caregiver.
Functional Impairment
We measured functional impairment by count of self- or proxy-reported difficulties in performing or needing help with the following task domains: mobility, self-care, and household activities due to health or functioning reasons (Freedman & Spillman, 2014). Mobility activities included getting out of bed, getting around inside and outside. Self-care activities included bathing, dressing, eating, and using the toilet. Household activities included doing laundry, going shopping, preparing meals, handling banking, and managing medications. Separate summed scores were determined for functional impairment in mobility (range = 0–3), self-care (range = 0–4), and household activities (range = 0–5). Functional decline over time means that, between 2015 and 2017, a NHATS respondent reported additional functional impairment, that is, additional tasks with which they had difficulty or required assistance in the mobility, self-care, or household task domains.
Outcomes
Family care received
We obtained information about the nature and intensity of care received from the NHATS Other Person file, which includes all unique persons that the NHATS respondent identified as providing any functional assistance, along with the hours of care each helper provided. For each care recipient (i.e., NHATS respondent), we calculated the total number of family and unpaid caregivers and total hours of care received from them in the last month. Family and unpaid caregivers included individuals related to the care recipient such as spouse, adult children, grandchildren, or siblings, as well as unrelated, unpaid helpers such as friends or neighbors (Freedman et al., 2020). Hours of care were imputed for caregivers with missing values (24.9%) using multivariate regression adjusting for caregiver’s relationship to care recipient, whether help was provided on a regular schedule (vs varied), for only one activity, only for activities that were asked during the last year not last month (i.e., money matters or medical activities), binary indicators for each of the mobility, self-care, household, or other activities with which the caregiver provided help, and an indicator of whether the care recipient was in high need (i.e., receiving help with mobility, self-care, or household activity due to health or functioning reasons; Freedman et al., 2014). We used NHATS to capture family care received because the NHATS Other Person file contains caregiver data from the full network of caregivers, whereas NSOC only samples a subset of the caregivers reported in NHATS (Freedman et al., 2020).
Family care provided
To examine change in family care provided from the caregiver perspective, we used NSOC to examine the hours of care individual caregiver respondents reported providing in the last month. Hours of care were imputed for caregivers with missing values (4.5%) using a similar strategy as in the NHATS Other Person file (Freedman et al., 2014), based on multivariate regression including caregiver’s relationship to care recipient, whether help was provided on a regular schedule (vs varied), binary indicators for any mobility, self-care, household, balance, transportation, handling bills or banking, ordering medication, and medical activities with which the caregiver provided help. In addition, we examined binary indicators of whether caregivers reported that providing care was emotionally or physically difficult. We used NSOC to examine care provided by individual caregivers for two reasons: first, the caregiving-related difficulty outcomes are only available in NSOC, and second, when weighted appropriately to account for sampling and nonresponse, NSOC is nationally representative of all family and unpaid caregivers whereas the NHATS Other Person file is not.
Covariates
Covariates were selected based on potential confounding with functional decline and family care outcomes. We controlled for older adults’ sociodemographic characteristics (sex [female vs male], age in years, race/ethnicity [non-Hispanic White, non-Hispanic Black, Hispanic, and other]), socioeconomic characteristics (marital status [married or living with a partner vs other], education [some college or above vs high school or less], family income, Medicare and Medicaid dual eligibility [yes vs no], living alone [yes vs no]), and comorbidities (binary indicators [yes vs no] for dementia, heart disease, diabetes, lung disease, stroke, cancer, arthritis, hypertension, depression, and anxiety). We also controlled for caregivers’ sociodemographic characteristics (sex, age, race/ethnicity), socioeconomic characteristics (marital status, education, family income, and Medicaid enrollment), general health status (excellent or very good, good, and fair or poor), and caregiving characteristics (coresidence with care recipient [yes vs no] and relationship to care recipient [spouse/partner, daughter/step-daughter/daughter-in-law, son/step-son/son-in-law, and other]).
Statistical Analysis
Unobserved health or family traits that simultaneously affect functional decline and family care, such as genes and family lifestyle, may not be captured in the survey data, and these traits might lead to biased estimates of the impact of functional decline on family care outcomes (i.e., endogeneity). Therefore, we applied a panel data fixed-effects model using within-person variation to generate causal estimates for the impact of functional decline over time on change in the family care outcomes of interest, whereby the longitudinal nature of NHATS and NSOC accounts for time-invariant unobserved confounders.
To examine the impact of functional decline on family care received by older adults (total number of family and unpaid caregivers and total hours of care each older adult received from them), we used NHATS and adjusted for potentially time-varying care recipient demographic (age), socioeconomic (marital status, family income, Medicare and Medicaid dual eligibility, and living alone), and health characteristics (dementia, heart disease, diabetes, lung disease, stroke, cancer, arthritis, hypertension, depression, and anxiety), and an indicator for survey year 2017. Time-invariant care recipient characteristics (sex, race/ethnicity, and education) were omitted from the panel data fixed-effects model. We ran models for older adults overall and stratified by their dementia status to test variation in the impact of functional decline on family care outcomes among older adults living with and without dementia. In addition, to comprehensively capture the impact of functional decline on the care older adults received, we performed a sensitivity analysis to examine the impact of functional decline on paid care received by older adults (total number of paid caregivers and total hours of care each older adult received from them). Paid caregivers included all caregivers identified in the NHATS Other Person file who were reported to be paid regardless of source of payment or relationship to care recipients (Reckrey et al., 2022). NHATS longitudinal analytic weights were applied to generate national estimates; standard errors were clustered at the older adult level (Freedman, Hu, et al., 2022).
To examine the impact of functional decline on family care provided from the perspective of the caregivers (hours of care each individual caregiver provided and caregiving-related emotional and physical difficulties by the caregiver), we limited the analysis to those caregivers who participated in NSOC and adjusted for potentially time-varying caregiver demographic (age), socioeconomic (marital status, education, family income, and Medicaid enrollment), general health status, and caregiving characteristics (coresidence with care recipient) and care recipient health characteristics (number of chronic conditions), and an indicator for survey year 2017. Time-invariant caregiver and caregiving characteristics (sex, race/ethnicity, and relationship to care recipient) were omitted from the panel data fixed-effects model. We ran models for caregivers overall and stratified by dementia status of care recipients to test the variation in the impact of functional decline on family care outcomes among caregivers for older adults with and without dementia. NSOC longitudinal analytic weights were applied to generate national estimates; standard errors were clustered at the caregiver respondent level (Freedman, Hu, et al., 2022). Statistical significance was set at two-tailed p < .05. All analyses were performed using STATA, version 17.0.
Results
Family Care Received
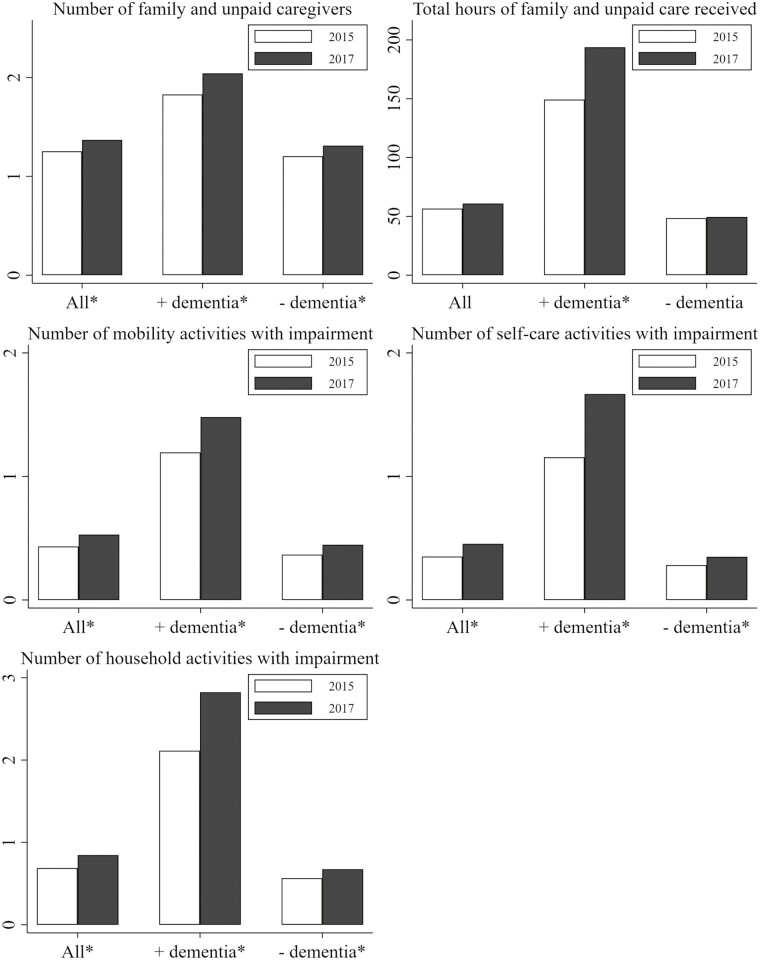
Among community-dwelling older adults, the mean age was 74 years at baseline and 55% were female (Supplementary Table 1). From 2015 to 2017, older adults’ average functional impairment increased slightly for all task domains, including mobility (0.4 vs 0.5), self-care (0.4 vs 0.5), and household activities (0.7 vs 0.8), as well as the number of family and unpaid caregivers from whom they received care (1.3 vs 1.4; p < .05 for all; Figure 1). Among older adults with dementia, average functional impairment increased substantially for all task domains including mobility (1.2 vs 1.5), self-care (1.2 vs 1.7), and household activities (2.1 vs 2.8) as well as the number of family and unpaid caregivers (1.8 vs 2.0) and total hours of care from whom they received care (149.3 vs 193.7 hr; p < .05 for all).
Figure 1.
Family care and functional impairment among community-dwelling older adults overall and by dementia status in 2015 and 2017.
Among community-dwelling older adults overall from 2015 to 2017, reporting impairment in one additional mobility activity led to having 0.07 (95% confidence interval [CI]: 0.02 to 0.12) more family and unpaid caregivers but not receiving additional total hours of family care (Table 1). Impairment in one additional self-care activity led to 0.12 (95% CI: 0.07 to 0.17) more family and unpaid caregivers and 19.3 (95% CI: 10.0 to 28.6) additional total monthly hours of care received. Impairment in one additional household activity led to 0.04 (95% CI: 0.004 to 0.08) more family and unpaid caregivers and 7.9 (95% CI: 1.8 to 13.9) additional total monthly hours of care. Among older adults living with dementia, impairment in one additional self-care activity led to 0.14 (95% CI: 0.03 to 0.25) more family and unpaid caregivers and 28.2 (95% CI: 1.7 to 54.7) additional total monthly hours of care, but additional mobility and household activity impairment did not affect family care they received. Among older adults living without dementia, the impact of functional decline over time on change of family care was in line with the full sample (i.e., older adults overall). Impairment in one additional mobility activity led to 0.06 (95% CI: 0.002 to 0.11) more family and unpaid caregivers but not additional total hours of care. Impairment in one additional self-care activity led to 0.11 (95% CI: 0.06 to 0.17) more caregivers and 15.0 (95% CI: 5.8 to 24.1) additional total monthly hours of care; impairment in one additional household activity led to 0.05 (95% CI: 0.01 to 0.10) more caregivers and 8.0 (95% CI: 2.8 to 13.2) additional total monthly hours of care.
Table 1.
Impact of Functional Decline on Family Care Received by Community-Dwelling Older Adults Overall and by Dementia Status, Coefficients (95% Confidence Intervals [CI])
| All older adults (N = 5,103) |
Older adults with dementia (N = 627) |
Older adults without dementia (N = 4,476) |
||||
|---|---|---|---|---|---|---|
| Number of family and unpaid caregivers, n | Total hours of family and unpaid care received, na | Number of family and unpaid caregivers, n | Total hours of family and unpaid care received, na | Number of family and unpaid caregivers, n | Total hours of family and unpaid care received, na | |
| Mobility activities | 0.07* (0.02–0.12) |
6.0 (−0.8–12.9) |
0.12 (−0.01–0.24) |
17.7 (−8.1–43.4) |
0.06* (0.002–0.11) |
4.0 (−2.9–11.0) |
| Self-care activities | 0.12*** (0.07–0.17) |
19.3*** (10.0–28.6) |
0.14* (0.03–0.25) |
28.2* (1.7–54.7) |
0.11*** (0.06–0.17) |
15.0** (5.8–24.1) |
| Household activities | 0.04* (0.004–0.08) |
7.9* (1.8–13.9) |
−0.01 (−0.09–0.07) |
3.7 (−19.3–26.7) |
0.05** (0.01–0.10) |
8.0** (2.8–13.2) |
Notes: Authors’ analysis of data from the 2015 and 2017 National Health and Aging Trends Study (NHATS) for a longitudinal cohort of community-dwelling older adults between 2015 and 2017. A panel data fixed-effects model was used to examine the impact of functional decline on change of family care received by older adults (total number of family and unpaid caregivers and total hours of care each older adult received from them). We accounted for potentially time-varying care recipient (i.e., NHATS respondent) demographic (age), socioeconomic (marital status, family income, Medicare and Medicaid dual eligibility, and living alone), and health characteristics (dementia, heart disease, diabetes, lung disease, stroke, cancer, arthritis, hypertension, depression, and anxiety), and an indicator for survey year 2017. Time-invariant care recipient characteristics (sex, race/ethnicity, and education) were omitted from the panel data fixed-effects model. Ninety-five percent CI were reported in brackets. Data were weighted using the NHATS longitudinal analytic weights and standard errors were clustered at the older adult respondent level.
aWe examined the total hours of care each older adult received in the last month from all family and unpaid caregivers identified in the NHATS Other Person file.
*p < .05. **p < .01. ***p < .001.
Sensitivity analysis examining the impact of functional decline on paid care older adults received (total number of paid caregivers and total hours of care each older adult received from them) showed similar results as family and unpaid care outcomes (Supplementary Table 2). Functional decline in all task domains (particularly self-care activities) was associated with increased paid care received among older adults: with impairment in one additional self-care activity leading to 0.04 (95% CI: 0.01 to 0.07) more paid caregivers and 4.8 (95% CI: 1.9 to 7.7) additional total monthly hours of care older adults received from them. But among older adults with dementia, the increase in paid care associated with self-care activity function decline was not statistically significant.
Family Care Provided
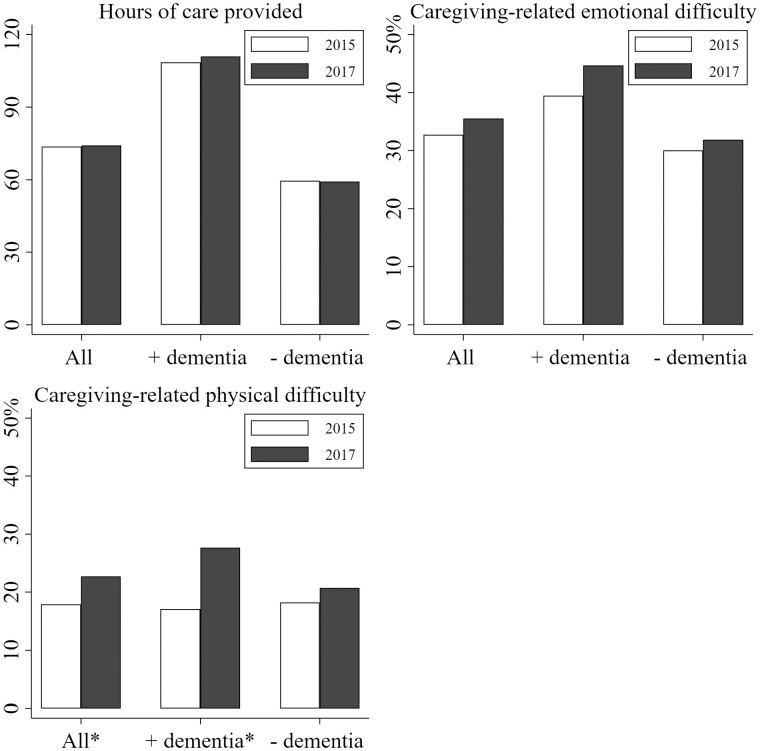
Among the subset of family and unpaid caregivers who participated in NSOC, 64% were females, 28% were spouses, and 32% were daughters (Supplementary Table 3). From 2015 to 2017, hours of care reported by each individual caregiver did not increase, rates of reported emotional difficulty did not increase significantly, but rates of reported physical difficulty did increase (caregivers overall: 17.9% vs 22.7%; caregivers for older adults living with dementia: 17.1% vs 27.7%; p < .05 for both; Figure 2).
Figure 2.
Hours of care and caregiving-related difficulties among caregivers for community-dwelling older adults overall and by dementia status in 2015 and 2017.
Among caregivers overall, care recipients’ additional impairment in mobility or self-care activities were not associated with additional hours of care reported by individual caregivers, but impairment in one additional household activity among care recipients led to 13.0 (95% CI: 6.1 to 20.0) additional monthly hours of care for each individual caregiver (Table 2). Additional impairment in all task domains was not associated with a significant increase in emotional or physical difficulty for caregivers overall. Among caregivers for older adults living with dementia, additional impairment in all task domains was not associated with a significant increase in hours of care and reported physical difficulty for each individual caregiver but impairment in one additional self-care activity led to an 8.4 (95% CI: 1.4 to 15.5) percentage points increase in the probability of reported caregiving-related emotional difficulty. Among caregivers for older adults without dementia, the impact of functional decline on family care was consistent with the effects on caregivers overall, with impairment in one additional household activity leading to 13.0 (95% CI: 5.9 to 20.1) additional monthly hours of care by individual caregivers but no impact on reported caregiving-related emotional or physical difficulty.
Table 2.
Impact of Functional Decline on Family Care Provided by Caregivers for Community-Dwelling Older Adults Overall and by Dementia Status, Coefficients (95% Confidence Intervals [CI])
| Caregivers for all older adults (N = 862) |
Caregivers for older adults with dementia (N = 308) |
Caregivers for older adults without dementia (N = 554) | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Hours of care provided, na | Emotional difficulty, % | Physical difficulty, % | Hours of care provided, na | Emotional difficulty, % | Physical difficulty, % | Hours of care provided, na | Emotional difficulty, % | Physical difficulty, % | |
| Mobility activities | −6.0 (−14.5–2.5) |
−1.9 (−6.0–2.2) |
−2.1 (−5.8–1.6) |
2.7 (−19.6–25.0) |
−2.5 (−10.0–5.1) |
−4.4 (−12.8–4.1) |
−7.9* (−14.2–1.6) |
−3.2 (−7.7–1.3) |
−0.7 (−4.3–2.8) |
| Self-care activities | −2.3 (−11.8–7.3) |
2.3 (−2.2–6.8) |
3.2 (−0.7–7.1) |
−13.7 (−35.3–7.9) |
8.4* (1.4–15.5) |
5.3 (−1.6–12.3) |
3.1 (−6.0–12.2) |
0.1 (−5.4–5.7) |
2.2 (−2.5–7.0) |
| Household activities | 13.0*** (6.1–20.0) |
2.3 (−1.0–5.6) |
0.7 (−2.3–3.6) |
11.5 (−7.4–30.4) |
0.5 (−4.3–5.2) |
3.1 (−2.0–8.1) |
13.0*** (5.9–20.1) |
3.9 (−0.4–8.3) |
−0.1 (−3.5–3.4) |
Notes: Authors’ analysis of data from the 2015 and 2017 National Study of Caregiving (NSOC) linked with the National Health and Aging Trends Study (NHATS) for a longitudinal cohort of caregivers for community-dwelling care recipients (limited to NHATS respondents who had NSOC caregivers) between 2015 and 2017. A panel data fixed-effects model was used to examine the impact of functional decline on family care provided by individual caregivers (hours of care each individual caregiver provided and caregiving-related emotional and physical difficulties by the caregiver). We accounted for potentially time-varying caregivers’ demographic (age), socioeconomic (marital status, education, family income, and Medicaid enrollment), general health status, and caregiving characteristics (coresidence with care recipient), care recipient (i.e., NHATS respondent) health characteristics (number of chronic conditions), and an indicator for survey year 2017. Time-invariant caregiver and caregiving characteristics (sex, race/ethnicity, and relationship to care recipient) were omitted from the panel data fixed-effects model. Ninety-five percent CI were reported in brackets. Data were weighted using the NSOC longitudinal analytic weights and standard errors were clustered at the caregiver respondent level.
aWe examined the hours of care each NSOC respondent provided to the care recipient (i.e., NHATS respondent) in the last month.
*p < .05. **p < .01. ***p < .001.
Discussion
This study provides the first longitudinal analysis of how older adults’ functional decline leads to change in the family care provided to them in a nationally representative sample of older adults and their caregivers. Over a 2-year span from 2015 to 2017, community-dwelling older adults’ functional impairment and the amount of family and unpaid care received increased significantly, particularly for those living with dementia, for whom the average total hours of care received increased by 30%. For care recipients, loss of self-care activity function was associated with the largest increase in both the number of family and unpaid caregivers and total hours of care received from them. For those with dementia, impairment in one additional self-care activity required nearly 30 additional total monthly hours of care. The increase in total hours of care associated with functional decline was larger than the increase in total number of family and unpaid caregivers. Our finding of this significantly increased caregiving demand associated with a decline in self-care function echoes prior work that found functional impairment in self-care activities, but not household activities, increased the risk of institutionalization among older adults with dementia (Scott et al., 1997).
Somewhat paradoxically, from the perspective of individual caregivers (i.e., NSOC respondents), decline in mobility or self-care activity function was not associated with providing additional caregiving hours, whereas decline in household activity function was. This suggests that the additional total hours of care older adults received related to a decline in self-care activities may be provided by additional caregivers as opposed to their existing caregivers providing more care. At the same time, decline in self-care activities among care recipients with dementia led to higher emotional difficulty for their caregivers. It may be that the decline in self-care activities among older adults with dementia does not lead to increased caregiving provided by individual caregivers because they have no additional hours available to provide, and this increased functional need that the individual caregiver cannot meet then contributes to further emotional difficulty. But we should interpret these findings with caution because the CIs were relatively large, possibly due to the small sample size (particularly among older adults with dementia and their caregivers; Du Prel et al., 2009) and the complex research design in this study (i.e., panel data fixed-effects model).
There are several potential reasons to help reconcile the discrepancies between findings at the older adult and caregiver levels. First, as care recipients’ function in mobility or self-care activities declined, their additional need might be provided from across a larger (family and unpaid) caregiving network rather than by individual current caregivers. In addition, care recipients might supplement family and unpaid care with paid care (Reckrey et al., 2020). This is confirmed by our findings of similar increase in paid care as family and unpaid care received among older adults associated with their functional decline. Further, older adults’ caregiver networks may change frequently and some caregivers, particularly nonspouse caregivers, might stop providing caregiving over time (Lin & Wu, 2019). These reasons may all help explain why individual current caregivers might not report increased hours of care provided even though the care recipients reported receiving more total hours of care. Lastly, the functional tasks caregivers support might change over time. For example, even if a caregiver was helping an adult with a self-care activity in 2015, by 2017 that caregiver may shift their help to mobility or household activities, and therefore do not report additional self-care-related help despite the additional functional need from the older adults.
This analysis has important policy implications. Interventions to help older adults maintain function as long as possible are crucial to manage limited caregiving capacity, whereas specific types of functional decline may merit differential types of supports. Families may benefit from additional education regarding functional decline as a key aspect of the dementia syndrome. Beyond education, they may benefit from initiatives that promote more routine referral to occupational therapy for strategies to address and manage these functional changes. Caregivers of older adults living with dementia may need particular support related to declines in care recipient’s self-care activity function. Presence of this specific type of functional decline or limitation could be used to both help determine eligibility for formal care assistance programs as well as guide specific targeted supports that are offered. Finally, absent formal care assistance programs, this specific domain of functional support could be the focus of education and resources (e.g., home modifications such as shower chairs) provided to help family and unpaid caregivers.
However, several limitations should be noted. First, the panel data fixed-effects model could not account for any time-varying, unobserved characteristics, such as dementia severity, which was not captured in the survey data (e.g., behavioral and psychological symptoms). Second, self-reported functional status and family care outcomes might be subject to recall bias and subjective bias and might vary by self and proxy older adult respondents. Third, findings about family and unpaid care received at the older adult (i.e., NHATS respondent) level and provided at the caregiver (i.e., NSOC respondent) level might not be comparable because NSOC only interviewed a subset of family and unpaid caregivers listed in the NHATS Other Person file. Finally, those caregivers who agree to participate in NSOC and are followed longitudinally may not generalize to the full population of family and unpaid caregivers of older adults.
In conclusion, our longitudinal analysis of community-dwelling older adults and their caregivers found that functional decline—particularly of self-care activities—among older adults led to increases in the number of family and unpaid caregivers and total hours of care received from them, particularly for those living with dementia. However, as care recipients’ self-care function declines, hours of care among individual current caregivers did not increase significantly, suggesting that the additional care is distributed across the caregiving network. Decline in self-care activity function among care recipients led to higher emotional difficulty for caregivers of older adults with dementia. Enhanced support for care recipients and their caregivers is needed particularly as older adults’ self-care function decline.
Supplementary Material
Acknowledgments
National Health and Aging Trends Study is sponsored by the National Institute on Aging (NIA U01AG032947) through a cooperative agreement with the Johns Hopkins Bloomberg School of Public Health. The National Study of Caregiving (NSOC) is funded by the NIA (R01AG054004). An earlier version of this paper was presented as a poster at the NHATS/NSOC Dementia Care Conference, May 2–3, 2022.
Contributor Information
Lianlian Lei, Department of Psychiatry, University of Michigan, Ann Arbor, Michigan, USA.
Donovan T Maust, Department of Psychiatry, Institute for Healthcare Policy and Innovation, University of Michigan, Ann Arbor, Michigan, USA; Center for Clinical Management Research, VA Ann Arbor Healthcare System, Ann Arbor, Michigan, USA.
Amanda N Leggett, Department of Psychology, Institute of Gerontology, Wayne State University, Detroit, Michigan, USA.
Funding
This work was supported by the National Institute on Aging (R01AG056407 to D. T. Maust and L. Lei; K99AG075145 to L. Lei; R01AG079097 and P30AG053760 to A. N. Leggett).
Conflict of Interest
None.
Author Contributions
L. Lei and D. T. Maust planned the study. L. Lei analyzed the data and drafted the paper. L. Lei, D. T. Maust, and A. N. Leggett revised the paper and approved the final version.
References
- Barberger-Gateau, P., Alioum, A., Pérès, K., Regnault, A., Fabrigoule, C., Nikulin, M., & Dartigues, J.-F. (2004). The contribution of dementia to the disablement process and modifying factors. Dementia and Geriatric Cognitive Disorders, 18(3–4), 330–337. 10.1159/000080127 [DOI] [PubMed] [Google Scholar]
- Chi, W., Graf, E., Hughes, L., Hastie, J., Khatutsky, G., Shuman, S., & Lamont, H. (2019). Community-dwelling older adults with dementia and their caregivers: Key indicators from the National Health and Aging Trends Study. US Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation. https://aspe.hhs.gov/reports/community-dwelling-older-adults-dementia-their-caregivers-key-indicators-national-health-aging-0 [Google Scholar]
- Coe, N. B., & Werner, R. M. (2022). Informal caregivers provide considerable front-line support in residential care facilities and nursing homes: Study examines the informal caregivers’ considerable frontline support in residential care facilities and nursing homes. Health Affairs, 41(1), 105–111. 10.1377/hlthaff.2021.01239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du Prel, J. -B., Hommel, G., Röhrig, B., & Blettner, M. (2009). Confidence interval or p-value?: Part 4 of a series on evaluation of scientific publications. Deutsches Ärzteblatt International, 106(19), 335–339. 10.3238/arztebl.2009.0335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V. A., Hu, M., DeMatteis, J., & Kasper, J. D. (2022). Accounting for sample design in NHATS and NSOC analyses: Frequently asked questions. NHATS Technical Paper #23 v2. Johns Hopkins Bloomberg School of Public Health. www.nhats.org [Google Scholar]
- Freedman, V. A., Schrack, J. A., Skehan, M. E., & Kasper, J. D. (2022). National Health and Aging Trends Study User Guide: Rounds 1–11 final release. Johns Hopkins University School of Public Health. www.nhats.org [Google Scholar]
- Freedman, V. A., Skehan, M. E., Hu, M., Wolff, J., & Kasper, J. D. (2020). National Study of Caregiving I–III User Guide. Johns Hopkins University School of Public Health. www.nhats.org [Google Scholar]
- Freedman, V. A., & Spillman, B. C. (2014). Disability and care needs among older Americans. The Milbank Quarterly, 92(3), 509–541. 10.1111/1468-0009.12076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V. A., Spillman, B. C., & Kasper, J. (2014). Hours of care in rounds 1 and 2 of the National Health and Aging Trends Study. NHATS Technical Paper #7. Johns Hopkins University School of Public Health. www.nhats.org [Google Scholar]
- Gill, T. M., Allore, H. G., Gahbauer, E. A., & Murphy, T. E. (2010). Change in disability after hospitalization or restricted activity in older persons. Journal of the American Medical Association, 304(17), 1919–1928. 10.1001/jama.2010.1568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, R. W., & Wiener, J. M. (2006). A profile of frail older Americans and their caregivers. Urban Institute. https://core.ac.uk/download/pdf/71348389.pdf [Google Scholar]
- Kasper, J. D., Freedman, V. A., & Spillman, B. C. (2013). Classification of persons by dementia status in the National Health and Aging Trends Study. NHATS Technical Paper #5. Johns Hopkins Bloomberg School of Public Health. www.NHATS.org [Google Scholar]
- Kasper, J. D., Freedman, V. A., Spillman, B. C., Skehan, M. E., & Hu, M. (2015). Addendum to classification of persons by dementia status in the National Health and Aging Trends Study for follow-up rounds. Johns Hopkins Bloomberg School of Public Health. www.NHATS.org [Google Scholar]
- Kasper, J. D., Freedman, V. A., Spillman, B. C., & Wolff, J. L. (2015). The disproportionate impact of dementia on family and unpaid caregiving to older adults. Health Affairs, 34(10), 1642–1649. 10.1377/hlthaff.2015.0536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, I.-F., & Wu, H.-S. (2019). Changes in older adults’ informal care networks. Innovation in Aging, 3(Suppl 1), S825–S825. 10.1093/geroni/igz038.3042 [DOI] [Google Scholar]
- Litwak, E. (1985). Helping the elderly: The complementary roles of informal networks and formal systems. Guilford Press. [Google Scholar]
- MacNeil Vroomen, J. L., Han, L., Monin, J. K., Lipska, K. J., & Allore, H. G. (2018). Diabetes, heart disease, and dementia: National estimates of functional disability trajectories. Journal of the American Geriatrics Society, 66(4), 766–772. 10.1111/jgs.15284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahoney, R., Regan, C., Katona, C., & Livingston, G. (2005). Anxiety and depression in family caregivers of people with Alzheimer disease: The LASER-AD study. The American Journal of Geriatric Psychiatry, 13(9), 795–801. 10.1176/appi.ajgp.13.9.795 [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, & Medicine. (2016). Families caring for an aging America. National Academies Press. 10.17226/23606 [DOI] [PubMed] [Google Scholar]
- Ortman, J. M., Velkoff, V. A., & Hogan, H. (2014). An aging nation: The older population in the United States. United States Census Bureau, Economics and Statistics Administration. https://www.census.gov/content/dam/Census/library/publications/2014/demo/p25-1140.pdf [Google Scholar]
- Parker, L. J., Fabius, C., Rivers, E., & Taylor, J. L. (2022). Is dementia-specific caregiving compared with non-dementia caregiving associated with physical difficulty among caregivers for community-dwelling adults? Journal of Applied Gerontology, 41(4), 1074–1080. 10.1177/07334648211014352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin, L. I., Mullan, J. T., Semple, S. J., & Skaff, M. M. (1990). Caregiving and the stress process: An overview of concepts and their measures. The Gerontologist, 30(5), 583–594. 10.1093/geront/30.5.583 [DOI] [PubMed] [Google Scholar]
- Pego, M. A., & Nunes, C. (2017). Aging, disability, and informal caregivers: A cross-sectional study in Portugal. Frontiers in Medicine, 4, 255. 10.3389/fmed.2017.00255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polenick, C. A., Leggett, A. N., Webster, N. J., Han, B. H., Zarit, S. H., & Piette, J. D. (2020). Multiple chronic conditions in spousal caregivers of older adults with functional disability: Associations with caregiving difficulties and gains. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(1), 160–172. 10.1093/geronb/gbx118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polenick, C. A., Min, L., & Kales, H. C. (2020). Medical comorbidities of dementia: Links to caregivers’ emotional difficulties and gains. Journal of the American Geriatrics Society, 68(3), 609–613. 10.1111/jgs.16244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reckrey, J. M., Li, L., Zhan, S., Wolff, J., Yee, C., & Ornstein, K. A. (2022). Caring together: Trajectories of paid and family caregiving support to those living in the community with dementia. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 77(S1), S11–S20. 10.1093/geronb/gbac006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reckrey, J. M., Morrison, R. S., Boerner, K., Szanton, S. L., Bollens-Lund, E., Leff, B., & Ornstein, K. A. (2020). Living in the community with dementia: Who receives paid care? Journal of the American Geriatrics Society, 68(1), 186–191. 10.1111/jgs.16215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redfoot, D., Feinberg, L., & Houser, A. N. (2013). The aging of the baby boom and the growing care gap: A look at future declines in the availability of family caregivers. AARP Public Policy Institute. https://www.aarp.org/content/dam/aarp/research/public_policy_institute/ltc/2013/baby-boom-and-the-growing-care-gap-insight-AARP-ppi-ltc.pdf [Google Scholar]
- Reisberg, B., Jamil, I. A., Khan, S., Monteiro, I., Torossian, C., Ferris, S., Sabbagh, M., Gauthier, S., Auer, S., & Shulman, M. B. (2010). Staging dementia. In Abou-Saleh M. T., Katona C., & Kumar A. (Eds.), Principles and practice of geriatric psychiatry, (pp. 162–169). Wiley-Blackwell. 10.1002/9780470669600.ch31 [DOI] [Google Scholar]
- Riffin, C., Van Ness, P. H., Wolff, J. L., & Fried, T. (2017). Family and other unpaid caregivers and older adults with and without dementia and disability. Journal of the American Geriatrics Society, 65(8), 1821–1828. 10.1111/jgs.14910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scott, W. K., Edwards, K. B., Davis, D. R., Cornman, C. B., & Macera, C. A. (1997). Risk of institutionalization among community long-term care clients with dementia. The Gerontologist, 37(1), 46–51. 10.1093/geront/37.1.46 [DOI] [PubMed] [Google Scholar]
- Sheehan, B. (2012). Assessment scales in dementia. Therapeutic Advances in Neurological Disorders, 5(6), 349–358. 10.1177/1756285612455733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillman, B. C., Freedman, V. A., Kasper, J. D., & Wolff, J. L. (2020). Change over time in caregiving networks for older adults with and without dementia. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(7), 1563–1572. 10.1093/geronb/gbz065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spillman, B. C., Wolff, J., Freedman, V. A., & Kasper, J. D. (2014). Informal caregiving for older Americans: An analysis of the 2011 National Study of Caregiving. https://aspe.hhs.gov/sites/default/files/migrated_legacy_files//44496/NHATS-IC.pdf
- Wolff, J. L., Mulcahy, J., Huang, J., Roth, D. L., Covinsky, K., & Kasper, J. D. (2018). Family caregivers of older adults, 1999–2015: Trends in characteristics, circumstances, and role-related appraisal. The Gerontologist, 58(6), 1021–1032. 10.1093/geront/gnx093 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.