Abstract
Objectives
We work from a stress and life-course perspective to examine the mental health of parents who experienced the death of their child. We examine whether mental health eventually returns to pre-bereavement levels and how social engagement after bereavement may shape the recovery process of depressive symptoms.
Methods
We analyze discontinuous growth curve models to assess the association between a child’s death and trajectories of parents’ depressive symptoms from the 1998–2016 Health and Retirement Study. The sample includes 16,182 parents aged 50 years and older.
Results
Those who transitioned to bereavement experienced an elevation in depressive symptoms and a relatively long recovery time (e.g., 7 years) to their pre-bereavement mental health in our findings. However, when engaging in volunteer work after their loss, depressive symptoms reduce more quickly to their pre-bereavement levels. Volunteering offsets up to 3 years of the negative consequences of child loss.
Discussion
The death of a child is a traumatic event with extensive health consequences, but research should more fully examine the dynamic nature and potential mitigation of these health consequences over time. Our findings expand the temporal lens to encompass healing processes after bereavement, incorporating the importance of social engagement.
Keywords: Family loss, Mental health, Volunteering
Exposure to stressful life events can disrupt and deflect a person’s life-course trajectory. A child’s death, in particular, is one of the most stressful and traumatic events, with lifelong consequences for parents’ psychological well-being (Hendrickson, 2009; Song et al., 2019; Stroebe et al., 2007). From a life-course perspective, child loss is an “off-time” and unexpected event, violating the perceived order of natural living (George, 2013; Leahy, 1993; Song et al., 2019), which could overtax parents’ psychological abilities to cope or adapt. In light of the intensiveness of this grief, it is not surprising that a large body of literature has documented the adverse psychological consequences of the death of a child (Keesee et al., 2008; Leahy, 1993; Rogers et al., 2008; Song et al., 2019; Stroebe et al., 2007; Umberson & Donnelly, 2022a).
Despite a growing interest in the mental health consequences of child loss, prior research on the linkages between a child’s death and psychological well-being pays less attention to the temporal processes of events. Thus, less evidence is available on whether parents’ mental health eventually returns to pre-bereavement levels and, if so, how long the healing process takes. Even less clear is whether there are social factors that may be associated with recovery time. These gaps in knowledge are striking given the recent public attention to grief associated with premature mortality in the United States (Umberson et al., 2017; Verdery et al., 2020).
We analyze the Health and Retirement Study (HRS) 1998–2016, a nationally representative longitudinal data set, to estimate how the death of a child influences the trajectories of parents’ psychological distress from mid-to-later life. We ask how long the recovery takes and whether social engagement, such as socializing with neighbors and volunteering, after child loss is associated with a reduced level of depressive symptoms over time. Conceptually, experiencing a child’s death is not just a distinct event but a process that unfolds and develops over time, leading to parents’ poor psychological well-being. Rather than a snapshot of a traumatic event, we expand the temporal horizon to examine whether post-bereavement psychological distress decreases over time or remains high without signs of improvement. Methodologically, we apply discontinuous growth curve models to show how long recovery takes and how social engagement may help to reduce depression and time to recovery. This method is uniquely suited to incorporate a dynamic point between bereavement and post-bereavement where social intervention may have mental health implications for bereaved parents in mid-to-later life.
Background
During one’s life course, being a parent often engenders a special sense of identity and purpose (Rubin & Malkinson, 2001). Thus, when a child dies, many parents not only experience sadness over losing a valued family member but they also may feel that a part of themselves has died permanently as well (Malkinson & Bar-Tur, 2005). Bereaved parents may experience a chronic sense of regret because parents typically feel a sense of responsibility to protect their children (Rogers et al., 2008). Not surprisingly, adults who have lost a child have significantly higher levels of depression than adults who have lost a spouse or a parent (Leahy, 1993).
We build on previous work by investigating whether the immediate detrimental effects of a child’s death dissipate over time, or whether the impact remains elevated without recovery. We draw upon theoretical insights from the stress and life-course perspectives to better understand the association between traumatic events and psychological distress over time. A core tenet of the life-course perspective is that lives unfold over time in long-term pathways or trajectories and that temporal patterns of health trajectories are crucial. The effect of child loss on mental health is not fixed in time but, rather, may vary across time in mid-to-late life. In addition, the stress model suggests that depression can emerge in response to both proximal and distal stressful life events (George, 2013). Indeed, stressors can impact psychological distress both within a limited time frame and an extended time frame (Torche, 2018).
The current empirical evidence of short-term and long-term trajectories of depression following child loss is inconclusive. It is unclear whether recovery occurs after parents experience child loss across mid-to-later life. Some studies document that people gradually adapt to post-bereavement life and their mental health recovers to their pre-bereavement level within a few years after child loss. For example, administrative data in Denmark documented that while the relative risk of being hospitalized for psychiatric disorders was highest in the first year after the death of a child among parents, this risk dissipated 5 years after loss (Li et al., 2005). Moreover, studies in the United States showed that parents with more recent losses reported higher grief, suggesting a downward trend over time (Keesee et al., 2008). This line of research suggests that the negative consequences of bereavement may be temporary.
On the other hand, other studies have revealed that child loss has enduring negative associations with mental health without signs of full recovery. Prior research on the long-term bereavement effects on parents implies lasting effects (Rogers et al., 2008; Stroebe et al., 2007). For instance, using the Wisconsin Longitudinal Study, Rogers et al. (2008) found that bereaved parents still reported more depressive symptoms even after 18 years following child loss than comparison parents. Bereaved parents reported poorer quality of life than nonbereaved parents even though the experience of child death occurred two decades earlier on average (Song et al., 2010). It may be that it is more difficult for bereaved parents in later life to recover from the loss of care and support from their adult children and to reconstruct their social networks (Umberson et al., 2013).
Questions remain unanswered about how this stressful life event unfolds with time because few studies use longitudinal and nationally representative panel data to study the life-course patterning of child loss on mental health. Using finer age grades in mid-to-later life in this nationally representative data, we estimate whether parents who lost their child eventually return to their pre-bereavement level of well-being. We investigate this by testing the following competing hypotheses:
Hypothesis 1a: Experiencing a child’s death will be associated with higher depression, which will rise immediately after the child’s death but with an eventual recovery over time to pre-bereavement levels.
Hypothesis 1b: Experiencing a child’s death will be associated with higher depression, which will rise immediately after the child’s death and remain at a higher level without an eventual recovery to pre-bereavement levels.
Bereavement, Social Engagement, and Mental Health Trajectories
A large body of literature documents the mental health consequences of grief; however, less work examines social factors that may reduce the impact of child loss for parents’ depressive symptom trajectories. Scholars have recognized that social engagement is critical for mental health in later life (Li & Ferraro, 2006; Musick & Wilson, 2003). Social integration theory suggests that one of the primary ways that social engagement may attenuate the mental health consequences of child loss is through promoting greater social attachment through social ties. Greater social attachment can provide a sense of purpose and meaning as well as increase motivation to take better care of one’s health (Berkman et al., 2000). Social engagement may sustain a sense of social involvement, mattering, belonging, and self-esteem, which, in turn, may reduce emotional distress (Thoits, 2011). Social engagement can also influence the body through physiological mechanisms such as diminishing neuroendocrine reactivity (Seeman & McEwen, 1996). Moreover, there is evidence that social engagement can buffer the impact of depressive symptoms; Schwerdtfeger and Friedrich-Mai (2009) found that participants who were depressed had higher negative affect only when they were alone, but not when they were socially engaged. Social engagement may alleviate the pressures or burdens of a problematic situation, diminishing the degree of perceived stress and, thus, its emotional influences (Carr, 2018; Thoits, 2011). Thus, it is possible that social engagement may offset the depressive consequences of child loss.
We focus on ties to the broader community (e.g., involvement in social activities such as volunteering and socializing with others) after the bereavement to examine buffering effects of social engagement. Although close ties may provide emotional support when people experience the death of family members, prior research shows that relying solely on close ties can have negative consequences (Lyngstad, 2013; Stroebe et al., 2005). The death of a child not only affects parents but also other close family members, which can strain relationships and limit social interaction (Lyngstad, 2013; Stroebe et al., 2005). Moreover, a closely knit network could become a disadvantage as close ties may entrap the individual within a limited set of normative expectations (e.g., the grief as a bereaved parent), rather than fulfill their need to make a transition to new social roles (Stroebe & Schut, 2010). Prior research documented that seeking social support outside of friends and family networks can be more effective in dealing with loss (Aoun et al., 2015; Logan et al., 2018). A less dense network that includes weak or bridging ties helps parents reintegrate their lives and satisfy the needs of the bereaved after loss (Walker et al., 1977).
Moreover, although we investigate social engagement both before and after the death of a child, our primary focus is on the effects of social engagement after the loss as a feasible behavioral intervention that can enhance the well-being of parents who are grieving. We extend prior research on bereavement and mental health, as well as the role of social engagement, by testing the following hypothesis among parents in mid-to-later life:
Hypothesis 2: Social engagement (e.g., socializing with neighbors and volunteering) after the death of a child will be associated with reduced levels of depressive symptoms.
Data and Methods
We analyzed data from the HRS from 1998 to 2016 to assess the association between a child’s death and trajectories of parents’ depressive symptoms. The HRS is a nationally representative longitudinal study of persons in the United States age 50 and older, surveyed every 2o years. The initial sample included 16,530 respondents who reported having at least one child. We excluded 147 respondents who did not answer questions regarding depressive symptoms at any wave and 201 who were missing data on covariates. This yields an analytic sample of 16,182 adults with 113,284 person-waves. We used complete case analysis because our covariates had less than 1% missing values.
Measures
Depression
We measured depressive symptoms using an abbreviated version of the Center for Epidemiologic Studies—Depression Scale (CES-D; Radloff 1977). Consistent with prior research (Lin et al., 2019), we summed the eight binary indicators (whether the respondent experienced the following sentiments all or most of the time over the week prior to the interview): feeling depressed, feeling that everything was an effort, having restless sleep, being unhappy, feeling lonely, feeling sad, being unable to get going, and not enjoying life. Higher values indicate higher levels of depression. The internal reliability for all eight items in the study ranged from 0.77 to 0.82 across the 1998–2016 waves.
Death of a child
The HRS asked retrospective questions about child bereavement from 2006 to 2014 (they were not asked in 2016): whether respondents had ever experienced a child’s death and in what year their child died or the most recent year of a child’s death if parents experienced multiple deaths. We first included a binary indicator of experiencing a child’s death before/at baseline to adjust for baseline differences. Then, we constructed a time-invariant indicator of whether the parent eventually experienced child loss (1 = yes) and a time-varying indicator (1 = yes) measured at each wave regarding whether parents experienced a child’s death during the study period.
Social engagement
We utilized two time-varying indicators of social engagement: socializing with neighbors and doing volunteer work. They were derived from the Social Network Index, a widely accepted measure of social integration (Umberson et al., 2022b; Yang et al., 2013). Socializing with neighbors was measured with the question: “How often do you get together with any of your neighbors just to chat or for a social visit?” We coded 1 if respondents socialized with neighbors more than weekly and 0 otherwise. The HRS did not collect the measure of socializing with neighbors from 2014. To retain waves when adults were missing information, we replaced missing values on this measure with the most recent response from the same person. Results are substantively similar when analyzing the models from 1998 to 2012 waves. Volunteering was measured with the question, “Have you spent any time in the past 12 months doing volunteer work for religious, educational, health-related or other charitable organizations?” (1 = yes, 0 = otherwise).
We developed two indicators of social engagement for our analysis. First, we used baseline measures of social engagement at age 50 for both bereaved and nonbereaved parents to adjust for any pre-existing differences in neighbor interactions and volunteering. Second, we constructed time-varying measures of post-bereavement social engagement to explore how it could potentially alleviate depressive symptoms among bereaved parents. Following Mirowsky’s (1999) approach, this variable was conditionally relevant as it only applied to parents who had experienced child loss (i.e., a valid value on this variable depended on having a specific value on another variable). To account for parents who had not experienced child loss, we assigned a placeholder value for social engagement after loss in the overall model estimation, which dropped out when multiplied by zero (i.e., in the absence of child loss; see Mirowsky, 1999, for more details about this approach).
Covariates
We included respondent’s age (in years), a binary indicator of gender (1 = women), a set of dummy variables for race/ethnicity (White [reference], Black, Hispanic, other racial/ethnic groups), education (in years), and total number of living children (top coded at 5) as a proxy of informal ties. Cohort consisted of four dichotomous variables based on respondents’ year of birth: the Asset and Health Dynamics Among the Oldest Old Study (AHEAD) cohort (born before 1930) [reference], HRS cohort (1931–1941), Warbabies (1942–1947), and the Boomer cohort (1948–1960).
Additionally, we adjusted for several time-varying covariates: logged family income (imputed from RAND), a binary indicator of marital status (1 = married), whether respondents experienced other family losses (spouse, sibling, and parents) during the course of the study, and the number of chronic conditions (ranging from 0 to 7).
Analytic Plan
First, we estimated discontinuous growth curve models to capture pre-bereavement depressive symptoms and the trajectory of depressive symptoms during and after bereavement. This procedure allows us to assess how individual depressive symptoms change in response to a child’s death in mid-to-later life. Then, we further considered whether the effect is temporary or chronic and whether social engagement after bereavement offsets the negative influences of a child’s death on depressive symptoms. Consistent with prior research (Brown et al., 2016), we assessed individual change with age, where repeated observations (Level 1) were nested within adults (Level 2). The models showed intraindividual change in mental health as a function of age. We compared the nested likelihood-ratio tests of several types of depression trajectories (e.g., linear, quadratic, cubic) and the test results revealed that a linear growth curve with random intercepts and random linear age slopes provided the best model fit. We centered age at 50 to facilitate model interpretation. We specified Model 1 as follows:
Level 1
Level 2
The Level 1 equation examines how each respondent i’s depression Y changes over time t. The Level 1 equation normally has only one intercept (, depression recorded at time 0 for person i) and one slope (, rate of change in respondent i’s depression trajectory after time 0). Informed by previous method-building studies (Lin et al., 2019; Singer & Willett, 2003), we included three additional intercepts and slopes to examine person-specific discontinuities in the trajectory after the loss of a child to allow individuals’ trajectories in Y to change at the point at which they transitioned to some state (i.e., child’s death).
First, is a dichotomous indicator that varies over time and captures whether person i experienced the death of a child (coded as 1) or not (coded as 0) at a specific age t. In this study, age serves as the time metric (e.g., age 50, 51, 52, etc.) to track changes in. Coefficient gauges the shift in depressive symptom elevation in response to child loss. Second, measures the time since child loss (measured in years). We coded 0 if adults did not experience child loss and started counting time since child loss for those who experienced the death of a child. Coefficient captures the shift in the slope after child death occurred. Third, we included squared terms to allow nonlinear changes in depression after child loss. By testing, we can estimate whether the negative consequences of child loss remain elevated without or with signs of recovery. Moreover, is a vector of time-varying covariates to adjust for confounding between child loss and depression, and is the error term for observation t for adult i.
The Level 2 equations show how the change in depressive symptoms varies between respondents. Population averages of the Level 1 intercept and slope are coefficients and, respectively, for the nonbereaved group. The population average difference in the Level 1 intercept for a one-unit difference in the Level 2 predictor vector is the coefficient vector. The population average difference in the Level 2 predictor is the coefficient vector. Both and are time-constant covariates (e.g., gender, race/ethnicity, etc.) that may adjust for the between-individual differences. Level 2 residual variances are and.
Next, we examined whether social engagement after bereavement offsets the negative association between child loss and depressive symptoms. We specified Model 2 as follows:
Level 1
Level 2
We added four additional variables: NeighborAfterCDit, VolunteerAfterCDit, TimeNeighborAfterCDit, and TimeVolunteerAfterCDit to the Level 1 equation. We coded NeighborAfterCDit as 1, if adults had contact with neighbors more than weekly after a child’s death and VolunteerAfterCDit as 1, if adults did volunteer work after a child’s death, and 0 otherwise for each. A negative value of (or) implies that bereaved parents who visited their neighbors more than weekly (or who volunteered) experienced a reduction in depressive symptoms compared to bereaved parents who were not socially engaged in these ways. Both TimeNeighborAfterCDit and TimeVolunteerAfterCDit count the time since social engagement after child death. We coded these two variables as 0 before bereaved parents visited their neighbors/volunteered and started counting the time once they participated in these social activities after the death of a child. A negative value of (or) suggests that bereaved parents who visited their neighbors frequently (or who volunteered) would have a steeper decrease in depression. We did not add squared terms of these variables because nonlinear changes showed poor model fit. Additionally, we tested, and to assess whether the gain from social engagement offsets the increase of depression from child loss.
Given that parents with depression are more likely to drop out of the study than those who are nondepressed, we controlled wave-specific binary indicators (1 = attrition at a given follow-up and 0 = remaining in the study; Lin et al., 2019; Muthén et al., 2011) to correct for bias due to differential dropout. We accounted for the complex survey design of the HRS, applying the respondent-level weight in the descriptive statistics in Table 1. We did not apply the weight in the regression analysis given that the models included covariates related to sample selection. Regression models yielded unbiased coefficients without weights (Winship & Radbill, 1994). However, as a sensitivity check, we used normalized wave-specific sample weights to Level 1 and baseline sample weights to Level 2 of the model (Heeringa et al., 2017). Applying weights did not alter the main conclusions. We also estimated robust standard errors to consider the intraclustering correlations. Discontinuity growth curve models were estimated using Mixed in Stata version 16.1, and all plots were generated using the R plot function.
Table 1.
Baseline Weighted Descriptive Statistics of the Sample by Later-Life Child Bereavement
| Nonbereaved | Transition to bereavement | Significance | |||
|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | |
| Depressive symptoms | 1.40 | 0.02 | 1.82 | 0.07 | * |
| Age | 59.50 | 0.07 | 65.21 | 0.27 | * |
| Women | 0.52 | 0.63 | * | ||
| Race and ethnicity | |||||
| White | 0.80 | 0.73 | * | ||
| Black | 0.09 | 0.15 | * | ||
| Hispanic | 0.08 | 0.08 | * | ||
| Other racial/ethnic groups | 0.03 | 0.03 | |||
| Years of education | 13.05 | 0.03 | 11.99 | 0.09 | * |
| Cohort | |||||
| AHEAD | 0.15 | 0.36 | * | ||
| HRS | 0.31 | 0.46 | * | ||
| Warbabies | 0.14 | 0.09 | * | ||
| Boomer | 0.40 | 0.09 | * | ||
| Number of children | 2.69 | 0.02 | 3.33 | 0.04 | * |
| Socializing with neighbors | 0.52 | 0.52 | |||
| Volunteering | 0.38 | 0.34 | * | ||
| Logged family income | 10.29 | 0.01 | 9.90 | 0.03 | * |
| Married | 0.72 | 0.67 | * | ||
| Other family losses | 0.40 | 0.01 | 0.54 | 0.02 | * |
| Chronic conditions | 0.20 | 0.00 | 0.36 | 0.02 | * |
| Unweighted n | 14,782 | 1,400 | |||
Notes: Column totals may not equal 100% due to rounding. Asterisks indicate the two groups are statistically different at p < .05 (two-tailed tests). The sample includes 16,182 adults. AHEAD = the Asset and Health Dynamics Among the Oldest Old Study; HRS = Health and Retirement Study; SD = standard deviation.
Results
Table 1 presents the descriptive statistics of the variables in the study by child bereavement status. On average, at baseline, adults who experienced child loss during the survey period reported higher levels of depression (mean =1.82) compared to those who did not experience child loss (mean = 1.40). Although there is no difference regarding socializing with neighbors between the two groups, those who experienced child loss during the study reported lower levels of volunteering (34%) than nonbereaved parents (38%) at baseline. In general, those who experienced child loss during the course of the study are more likely to be racial/ethnic minorities and have lower socioeconomic status measured by education and logged family income. Parents who experienced child loss were less likely to be married than nonbereaved parents.
Next, we examine whether the association between child loss and elevated depressive symptoms dissipates over time or remains elevated without recovery. In particular, we test the relationship between elapsed time since bereavement and depressive symptoms and compared how the trajectories differed from those who did not experience the death of a child. Estimates from Model 1 in Table 2 reveal that individuals who become bereaved at age 50 or older exhibit higher levels of depressive symptoms at baseline, 0.268 points higher than those who did not experience a child’s death in mid-to-late life. Despite adjusting for pre-bereavement differences, following a child’s death, depression still rises immediately (β = 0.249, p < .05). The heightened depression due to child loss lasts for several years, although the level of depressive symptoms slowly dissipates (β = −0.031, p < .05) and then levels off (β = 0.001, p < .05). A post hoc test shows that the time since child loss (i.e., the shift in the slope after loss; β = −0.031 + 0.001, p < .001) is statistically significant from zero. This suggests the signs of recovery over time, consistent with Hypothesis 1a.
Table 2.
Regression Coefficients From Discontinuous Multilevel Models Predicting Depressive Symptoms, Health and Retirement Study, 1998 to 2016 (N = 113,284 person-waves)
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| Variable | Initial status | Rate of change | Initial status | Rate of change |
| Intercept | 4.773* (0.403) |
−0.091* (0.017) |
4.759* (0.403) |
−0.091* (0.017) |
| Time-invariant covariates | ||||
| Bereaved group | 0.268* (0.081) |
−0.004 (0.004) |
0.305* (0.084) |
−0.006 (0.005) |
| Age at baseline | −0.016** (0.005) |
0.001* (0.000) |
−0.016** (0.005) |
0.001* (0.000) |
| Women | 0.293* (0.036) |
−0.004* (0.002) |
0.293* (0.036) |
−0.004* (0.002) |
| Black | 0.309* (0.053) |
−0.011* (0.003) |
0.310* (0.053) |
−0.011* (0.003) |
| Hispanic | 0.356* (0.073) |
−0.008* (0.004) |
0.354* (0.073) |
−0.008* (0.004) |
| Other racial/ethnic groups | 0.439* (0.116) |
−0.011 (0.006) |
0.439* (0.116) |
-0.011 (0.006) |
| Years of education | −0.110* (0.007) |
0.001** (0.000) |
−0.110* (0.007) |
0.001** (0.000) |
| HRS cohort | 0.129 (0.093) |
−0.010** (0.004) |
0.123 (0.093) |
−0.010** (0.004) |
| Warbabies cohort | 0.185 (0.121) |
−0.003 (0.006) |
0.181 (0.121) |
−0.003 (0.006) |
| Boomer cohort | 0.330** (0.118) |
−0.008 (0.006) |
0.327** (0.118) |
−0.007 (0.006) |
| Number of children | 0.033** (0.012) |
−0.002** (0.001) |
0.032** (0.012) |
−0.002** (0.001) |
| Experienced child death before age 50 | 0.286* (0.066) |
−0.008** (0.003) |
0.287* (0.066) |
−0.008** (0.003) |
| Social visit with neighbors at baseline | −0.112** (0.035) |
−0.001 (0.002) |
−0.110** (0.035) |
−0.001 (0.002) |
| Doing volunteer work at baseline | −0.362* (0.035) |
0.003 (0.002) |
−0.359* (0.035) |
0.003 (0.002) |
| Time-varying covariates | ||||
| Logged household income | −0.074* (0.012) |
0.000 (0.001) |
−0.075* (0.012) |
0.000 (0.001) |
| Married | −0.732* (0.042) |
0.012* (0.002) |
−0.732* (0.042) |
0.012* (0.002) |
| Other losses | −0.036 (0.022) |
0.002 (0.001) |
−0.036 (0.022) |
0.002 (0.001) |
| Chronic conditions | 0.086* (0.022) |
0.002** (0.001) |
0.087* (0.022) |
0.002** (0.001) |
| Transition to child bereavement | 0.249* (0.056) |
0.343* (0.064) |
||
| Years since bereavement | −0.031* (0.009) |
−0.035* (0.011) |
||
| Years since bereavement, squared | 0.001** (0.000) |
0.001** (0.000) |
||
| Social visit with neighbors after bereavement | −0.088 (0.046) |
|||
| Doing volunteer work after bereavement | −0.144** (0.051) |
|||
| Years since social visit after bereavement | 0.017 (0.017) |
|||
| Years since volunteer work after bereavement | −0.003 (0.015) |
|||
| Variance components | ||||
| Within-person | 1.628* (0.017) |
1.628* (0.017) |
||
| Initial status (1) | 18.240* (0.810) |
18.214* (0.810) |
||
| Rate of change (2) | 0.003* (0.000) |
0.003* (0.000) |
||
| Covariance between (1) and (2) | −1.959* (0.027) |
−1.959* (0.027) |
||
| Log likelihood | −206,824.881 | −206,816.366 | ||
Notes: All models include dichotomous indicators adjusting for attrition. Robust standard errors are shown in parentheses. HRS = Health and Retirement Study.
***p < .001. **p < .01. *p < .05.
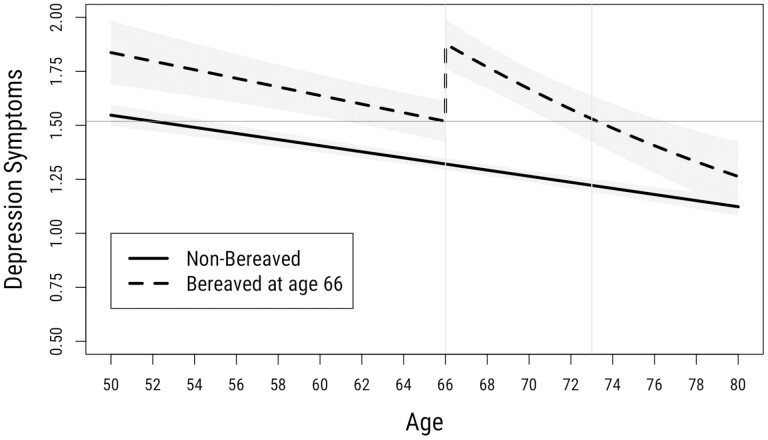
Figure 1 visualizes the predicted depression trajectories for nonbereaved parents and those who become bereaved at age 66 (the mean age of experiencing a child’s death in mid-to-later life, for illustration purposes) while holding other covariates at their mean levels. As shown in Figure 1, it takes about 7 years (at age 73) for those who experience a child’s death at age 66 to return to pre-bereavement levels of depression. This is at odds with Hypothesis 1b stipulating persistent negative effects that remain elevated over time.
Figure 1.
Depression trajectories by bereavement of a child. Note: For visualization purposes, we chose age 66 because this is the mean age of experiencing a child’s death in mid-to-later life. The horizontal line indicates average depressive symptoms before child loss and illustrates when the bereaved depression trajectory returns to the pre-bereavement level.
Finally, we consider the role of social engagement, in terms of socializing with neighbors and volunteering. Model 2 of Table 2 shows that socializing with neighbors and volunteering at baseline are associated with lower initial levels of depressive symptoms. We also assess whether social engagement after bereavement offsets the negative consequences of a child’s death for depressive symptoms. Socializing with neighbors after bereavement is not statistically significantly related to lower levels of depressive symptoms. We find a statistically significant association between volunteering after child loss and depression. Depressive symptoms decreased by 0.144 (p < .05) immediately following volunteering for those who are bereaved.
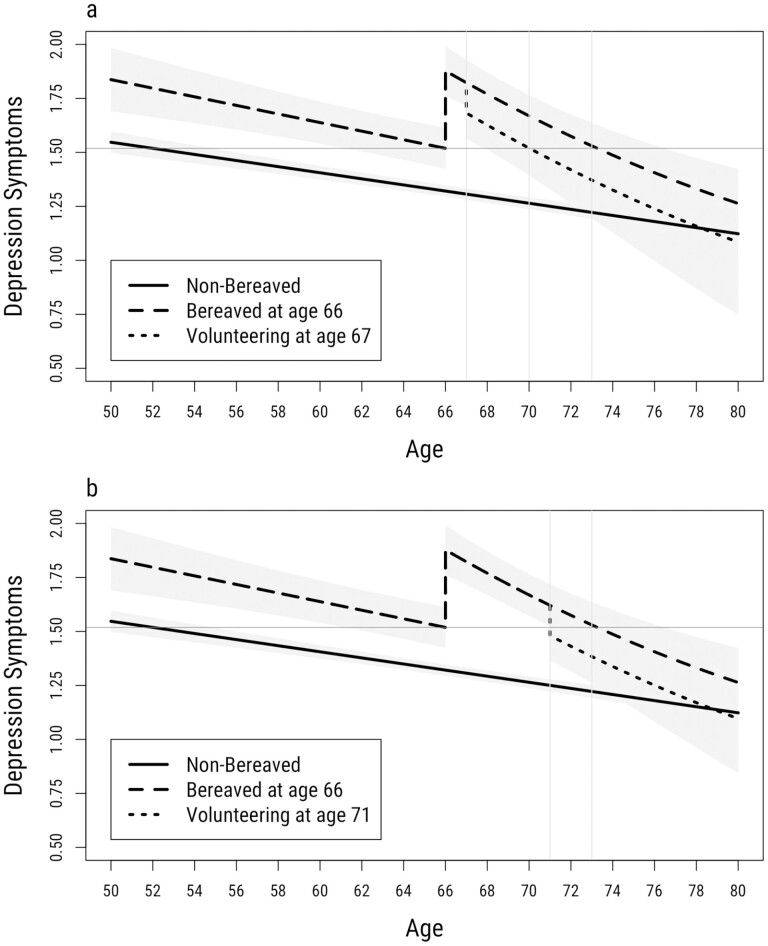
To facilitate interpretation, we plot the predicted depression trajectories by fixing their transition to volunteering at age 67 (Panel A) and 71 (Panel B) in Figure 2. We first choose age 67 (a year after loss) to assess whether there are implications for volunteering relatively soon after child loss. We also illustrate the association between volunteering at age 71 and depression trajectories because the average age of volunteering among bereaved parents is around age 71 in our sample. Alternative specifications of volunteering at different ages do not alter the main findings. As illustrated in Figure 2, Panel A, volunteering a year after loss immediately reduces parents’ depression with recovery to pre-bereavement level by age 70. In Panel B of Figure 2, volunteering 5 years after bereavement (at age 71) significantly reduces parents’ psychological distress with recovery to pre-bereavement levels almost immediately. Given that parents’ recovery typically lasted about 7 years, volunteering can offset up to 3 years (i.e., age 73 vs age 70) of the negative mental health consequences of child loss, depending on age of volunteering. Moreover, regardless of age of volunteering after child loss, depression converges to the level of the nonbereaved at age 80 among those who volunteer, although the confidence intervals begin to overlap at age 72 (Panel A) and age 74 (Panel B).
Figure 2.
Depression trajectories by bereavement of a child and volunteering. Note: For visualization purposes, we chose age 66 because this is the mean age of experiencing a child’s death in mid-to-later life.
Sensitivity Checks
We conducted several auxiliary analyses to test the robustness of our findings. First, we investigated potential gender differences in the consequences of child loss on mental health. Prior research has suggested that mothers may experience more severe consequences than fathers (Lee et al., 2014). However, our analysis did not show any significant gender differences in the mental health outcomes of bereaved parents. Second, we examined whether coping responses, such as health behaviors (e.g., smoking, drinking, regular exercise), might influence our findings. Our results remained similar to the main findings, suggesting that these coping responses did not significantly alter the association between child loss and mental health. Third, we used wave as the time metric rather than age to test whether this choice influenced our results (see Supplementary Table 2). Again, the pattern of results remained consistent with the main findings, indicating that our findings were not dependent on the choice of time metric. Fourth, we explored the possibility of selection issues with volunteering after child loss among bereaved parents. For example, parents who volunteer after a child’s death may have certain characteristics that make them less likely to experience depression. We used fixed-effects models to eliminate time-constant confounding and found that the association between volunteering after bereavement and depression remained statistically significant (see Supplementary Table 3). Finally, we conducted an additional sensitivity check to account for reverse causation. We added a lagged dependent variable to our model and found that the association between volunteering and depression decreased but remained statistically significant (available upon request). This suggests that reverse causality may partially explain the association between volunteering and depression, but it does not fully account for it. Overall, our auxiliary analyses provide further evidence for the robustness of our findings and strengthen our confidence in the association between volunteering after bereavement and improved mental health outcomes among bereaved parents.
Discussion
A stressful life event is not just a discrete event but a process that unfolds with time. We aim to understand the impact of a particular traumatic event—the death of a child—on trajectories of mental health in mid-to-late life. A great deal of research documents adverse mental health consequences for parents who lose children (Song et al., 2019; Stroebe et al., 2007; Umberson & Donnelly, 2022a). However, prior work does not fully examine the temporal processes of depressive symptom trajectories for bereaved parents or the social dimensions of healing processes. As such, the present study considers how losing a child in mid-to-later life is associated with trajectories of depression and how social engagement may alter the temporal processes of this depression.
We find that those experiencing the death of a child in mid- to late-life experience elevated depressive symptoms and it takes a long time (e.g., 7 years) for their depressive symptoms to recover to pre-bereavement levels. In our data, although psychological distress lasts for around 7 years, ultimately bereaved parents exhibit full recoveries on average. These findings echo the general findings of others for the short- and long-term effects of widowhood on mental health, documenting that adults ultimately recovered from widowhood, but it takes about 8 years to recover from the negative impact of their loss (Lin et al., 2019).
Second, social engagement after child loss––volunteering, in particular––was beneficial for recovery. We find that when bereaved parents do volunteer work after child loss, their levels of depressive symptoms recover more quickly, up to 3 years earlier. These findings are consistent with prior research that has documented the positive health impact of prosocial behaviors as an active form of social engagement (Huo et al., 2022; Poulin et al., 2013). With the death of a child, which can involve losing a loved one coupled with a loss of purpose and identity, it may be that volunteering helps bereaved parents find more meaning and purpose in their lives to help their mental health recovery. In contrast, our findings suggest that socializing with neighbors post-bereavement did not show a significant reduction in levels of depression. This could potentially be explained by the presence of alternative social networks. For instance, individuals may turn to their relatives for support and may allocate less time to interacting with neighbors.
This study attends to the important question of temporal trajectories in the link between the death of a child in mid-to-later life with depression; however, limitations of the present study should be noted. First, these data do not have detailed information about cause of death, gender of the child, and age of the child when they died. This is an unfortunate limitation of most nationally representative datasets in the United States, which typically collect information on family deaths based on retrospective questions and do not probe for this level of detail (Donnelly et al., 2020). Future research may navigate the heterogeneous effects on mental health by types of deaths, gender, and age of the focal child. Second, future research may benefit from examining potential heterogeneous trajectories by race/ethnicity. For example, Black adults are more likely to be exposed to child loss (Umberson et al., 2017) and poor mental health (Jackson et al., 2010). In addition, social support systems in later life may be different between racial and ethnic groups (Ferraro & Koch, 1994). Third, although our social engagement measures captured community ties from a standard social network index (Umberson et al., 2022b; Yang et al., 2013), future research could examine other dimensions of both formal and informal types of social support. Finally, future research could focus on disentangling the nuances of temporal processes by cohort.
Conclusion
Burdens of stress are key mechanisms of poor mental health in mid-to-late life (Pearlin, 2010; Thoits, 2010). The death of a child is a devastating and stressful life event that occurs more frequently than many may realize. About 13% of adults in the United States experience child loss across their life course (Umberson et al., 2017). Guided by a stress and life-course perspective and social integration theory, we examine whether the mental health consequences of child loss eventually recover to pre-bereavement levels and, if so, how long the healing process takes. Moreover, we assess how social engagement after bereavement may offset the negative association between child loss and mental health. We find that depressive symptoms rise precipitously immediately following the death of a child, with a long-term consequence followed by a recovery. However, if adults participate in volunteering after their child loss, it helps their depressive symptoms significantly decline to pre-bereavement levels within a shorter period. In sum, by focusing on the temporal healing process, an emerging yet understudied phenomenon in mental health research, these findings highlight an important research frontier that explores temporal dynamics in the association between child loss and depressive symptoms and how bereaved families may overcome their psychological distress more quickly.
Supplementary Material
Contributor Information
Hyungmin Cha, Department of Sociology, Center on Aging and Population Sciences and Population Research Center, University of Texas at Austin, Austin, Texas, USA.
Patricia A Thomas, Department of Sociology, Center on Aging and the Life Course, Purdue University, West Lafayette, Indiana, USA.
Funding
This research was supported by the National Institute on Aging (Grants P30AG066614 and R01AG054624) and by the U.S. Eunice Kennedy Shriver National Institute of Child Health and Human Development (Grant P2CHD042849).
Conflict of Interest
None.
Author Contributions
H. Cha developed the conceptual framework, conducted the analysis, and drafted the paper. P. A. Thomas contributed to the conceptual framework, supervision of data analysis, and writing.
References
- Aoun, S. M., Breen, L. J., Howting, D. A., Rumbold, B., McNamara, B., & Hegney, D. (2015). Who needs bereavement support? A population based survey of bereavement risk and support need. PLoS One, 10(3), e0121101. doi: 10.1371/journal.pone.0121101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman, L. F., Glass, T., Brissette, I., & Seeman, T. E. (2000). From social integration to health: Durkheim in the new millennium. Social Science & Medicine, 51(6), 843–857. doi: 10.1016/s0277-9536(00)00065-4 [DOI] [PubMed] [Google Scholar]
- Brown, T. H., Richardson, L. J., Hargrove, T. W., & Thomas, C. S. (2016). Using multiple-hierarchy stratification and life course approaches to understand health inequalities: The intersecting consequences of race, gender, SES, and age. Journal of Health and Social Behavior, 57(2), 200–222. doi: 10.1177/0022146516645165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr, D. (2018). Volunteering among older adults: Life course correlates and consequences. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(3), 479–481. doi: 10.1093/geronb/gbx179 [DOI] [PubMed] [Google Scholar]
- Donnelly, R., Umberson, D., Hummer, R. A., & Garcia, M. A. (2020). Race, death of a child, and mortality risk among aging parents in the United States. Social Science & Medicine, 249, 112853. doi: 10.1016/j.socscimed.2020.112853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferraro, K. F., & Koch, J. R. (1994). Religion and health among black and white adults: Examining social support and consolation. Journal for the Scientific Study of Religion, 33(4), 362–375. doi: 10.2307/1386495 [DOI] [Google Scholar]
- George, L. K. (2013). Life-course perspectives on mental health. In Phelan J. C. & Bierman A. (Eds.), Handbook of the sociology of mental health (pp. 585–602). Springer Netherlands. doi: 10.1007/978-94-007-4276-5_28 [DOI] [Google Scholar]
- Heeringa, S., West, B. T., & Berglund, P. A. (2017). Applied survey data analysis. Chapman & Hall/CRC. [Google Scholar]
- Hendrickson, K. C. (2009). Morbidity, mortality, and parental grief: A review of the literature on the relationship between the death of a child and the subsequent health of parents. Palliative & Supportive Care, 7(1), 109–119. doi: 10.1017/S1478951509000133 [DOI] [PubMed] [Google Scholar]
- Huo, M., Kim, K., & Wang, D. (2022). Long-term psychological consequences of parental bereavement prior to midlife: Volunteering helps. Aging & Mental Health, 0(0), 1–9. doi: 10.1080/13607863.2022.2087209 [DOI] [PubMed] [Google Scholar]
- Jackson, J. S., Knight, K. M., & Rafferty, J. A. (2010). Race and unhealthy behaviors: Chronic stress, the HPA axis, and physical and mental health disparities over the life course. American Journal of Public Health, 100(5), 933–939. doi: 10.2105/AJPH.2008.143446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keesee, N. J., Currier, J. M., & Neimeyer, R. A. (2008). Predictors of grief following the death of one’s child: The contribution of finding meaning. Journal of Clinical Psychology, 64(10), 1145–1163. doi: 10.1002/jclp.20502 [DOI] [PubMed] [Google Scholar]
- Leahy, J. M. (1993). A comparison of depression in women bereaved of a spouse, child, or a parent. OMEGA—Journal of Death and Dying, 26(3), 207–217. doi: 10.2190/ylg9-p4r7-w2vw-kafr [DOI] [Google Scholar]
- Lee, C., Glei, D. A., Weinstein, M., & Goldman, N. (2014). Death of a child and parental wellbeing in old age: Evidence from Taiwan. Social Science & Medicine, 101, 166–173. doi: 10.1016/j.socscimed.2013.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li, J., Laursen, T. M., Precht, D. H., Olsen, J., & Mortensen, P. B. (2005). Hospitalization for mental illness among parents after the death of a child. New England Journal of Medicine, 352(12), 1190–1196. doi: 10.1056/nejmoa033160 [DOI] [PubMed] [Google Scholar]
- Li, Y., & Ferraro, K. F. (2006). Volunteering in middle and later life: Is health a benefit, barrier or both? Social Forces, 85(1), 497–519. doi: 10.1353/sof.2006.0132 [DOI] [Google Scholar]
- Lin, I.-F., Brown, S. L., Wright, M. R., & Hammersmith, A. M. (2019). Depressive symptoms following later-life marital dissolution and subsequent repartnering. Journal of Health and Social Behavior, 60(2), 153–168. doi: 10.1177/0022146519839683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Logan, E. L., Thornton, J. A., Kane, R. T., & Breen, L. J. (2018). Social support following bereavement: The role of beliefs, expectations, and support intentions. Death Studies, 42(8), 471–482. doi: 10.1080/07481187.2017.1382610 [DOI] [PubMed] [Google Scholar]
- Lyngstad, T. H. (2013). Bereavement and divorce: Does the death of a child affect parents’ marital stability? Family Science, 4(1), 79–86. doi: 10.1080/19424620.2013.821762 [DOI] [Google Scholar]
- Malkinson, R., & Bar-Tur, L. (2005). Long term bereavement processes of older parents: The three phases of grief. OMEGA—Journal of Death and Dying, 50(2), 103–129. doi: 10.2190/w346-up8t-rer6-bbd1 [DOI] [Google Scholar]
- Mirowsky, J. (1999). Analyzing associations between mental health and social circumstances. In Aneshensel C. S. & Phelan J. C. (Eds.), Handbook of the sociology of mental health (pp. 105–123). Springer Nature/Books. [Google Scholar]
- Musick, M. A., & Wilson, J. (2003). Volunteering and depression: The role of psychological and social resources in different age groups. Social Science & Medicine, 56(2), 259–269. doi: 10.1016/S0277-9536(02)00025-4 [DOI] [PubMed] [Google Scholar]
- Muthén, B., Asparouhov, T., Hunter, A. M., & Leuchter, A. F. (2011). Growth modeling with nonignorable dropout: Alternative analyses of the STARD antidepressant trial. Psychological Methods, 16(1), 17–33. doi: 10.1037/a0022634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pearlin, L. I. (2010). The life course and the stress process: Some conceptual comparisons. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65B(2), 207–215. doi: 10.1093/geronb/gbp106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poulin, M. J., Brown, S. L., Dillard, A. J., & Smith, D. M. (2013). Giving to others and the association between stress and mortality. American Journal of Public Health, 103(9), 1649–1655. doi: 10.2105/AJPH.2012.300876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff, L. S. (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. doi: 10.1177/014662167700100306 [DOI] [Google Scholar]
- Rogers, C. H., Floyd, F. J., Seltzer, M. M., Greenberg, J., & Hong, J. (2008). Long-term effects of the death of a child on parents’ adjustment in midlife. Journal of Family Psychology, 22(2), 203–211. doi: 10.1037/0893-3200.22.2.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin, S. S., & Malkinson, R. (2001). Parental response to child loss across the life cycle: Clinical and research perspectives. In Handbook of bereavement research: Consequences, coping, and care (pp. 219–240). American Psychological Association. doi: 10.1037/10436-009 [DOI] [Google Scholar]
- Schwerdtfeger, A., & Friedrich-Mai, P. (2009). Social interaction moderates the relationship between depressive mood and heart rate variability: Evidence from an ambulatory monitoring study. Health Psychology, 28(4), 501–509. doi: 10.1037/a0014664 [DOI] [PubMed] [Google Scholar]
- Seeman, T. E., & McEwen, B. S. (1996). Impact of social environment characteristics on neuroendocrine regulation. Psychosomatic Medicine, 58(5), 459–471. doi: 10.1097/00006842-199609000-00008 [DOI] [PubMed] [Google Scholar]
- Singer, J. D., & Willett, J. B. (2003). Applied longitudinal data analysis: Modeling change and event occurrence. Oxford University Press. [Google Scholar]
- Song, J., Floyd, F. J., Seltzer, M. M., Greenberg, J. S., & Hong, J. (2010). Long-term effects of child death on parents’ health-related quality of life: A dyadic analysis. Family Relations, 59(3), 269–282. doi: 10.1111/j.1741-3729.2010.00601.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song, J., Mailick, M. R., Greenberg, J. S., & Floyd, F. J. (2019). Mortality in parents after the death of a child. Social Science & Medicine, 239, 112522. doi: 10.1016/j.socscimed.2019.112522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroebe, M., & Schut, H. (2010). The dual process model of coping with bereavement: A decade on. OMEGA—Journal of Death and Dying, 61(4), 273–289. doi: 10.2190/om.61.4.b [DOI] [PubMed] [Google Scholar]
- Stroebe, M., Schut, H., & Stroebe, W. (2007). Health outcomes of bereavement. The Lancet, 370(9603), 1960–1973. doi: 10.1016/s0140-6736(07)61816-9 [DOI] [PubMed] [Google Scholar]
- Stroebe, W., Zech, E., Stroebe, M. S., & Abakoumkin, G. (2005). Does social support help in bereavement? Journal of Social and Clinical Psychology, 24(7), 1030–1050. doi: 10.1521/jscp.2005.24.7.1030 [DOI] [Google Scholar]
- Thoits, P. A. (2010). Stress and health: Major findings and policy implications. Journal of Health and Social Behavior, 51(1_Suppl), S41–S53. doi: 10.1177/0022146510383499 [DOI] [PubMed] [Google Scholar]
- Thoits, P. A. (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145–161. doi: 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- Torche, F. (2018). Prenatal exposure to an acute stressor and children’s cognitive outcomes. Demography, 55(5), 1611–1639. doi: 10.1007/s13524-018-0700-9 [DOI] [PubMed] [Google Scholar]
- Umberson, D., & Donnelly, R. (2022a). The death of a child and parents’ psychological distress in mid to later life: Racial/ethnic differences in exposure and vulnerability. The Journals of Gerontology: Series B, 77(8), 1561–1570. doi: 10.1093/geronb/gbab206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D., Lin, Z., & Cha, H. (2022b). Gender and social isolation across the life course. Journal of Health and Social Behavior, 63(3), 319–335. doi: 10.1177/00221465221109634 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D., Olson, J. S., Crosnoe, R., Liu, H., Pudrovska, T., & Donnelly, R. (2017). Death of family members as an overlooked source of racial disadvantage in the United States. Proceedings of the National Academy of Sciences, 114(5), 915–920. doi: 10.1073/pnas.1605599114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson, D., Thomeer, M. B., & Williams, K. (2013). Family status and mental health: Recent advances and future directions. In Handbook of the sociology of mental health (pp. 405–431). Springer Netherlands. doi: 10.1007/978-94-007-4276-5_20 [DOI] [Google Scholar]
- Verdery, A. M., Smith-Greenaway, E., Margolis, R., & Daw, J. (2020). Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proceedings of the National Academy of Sciences, 117(30), 17695–17701. doi: 10.1073/pnas.2007476117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker, K. N., MacBride, A., & Vachon, M. L. S. (1977). Social support networks and the crisis of bereavement. Social Science & Medicine, 11(1), 35–41. doi: 10.1016/0037-7856(77)90143-3 [DOI] [PubMed] [Google Scholar]
- Winship, C., & Radbill, L. (1994). Sampling weights and regression analysis. Sociological Methods & Research, 23(2), 230–257. doi: 10.1177/0049124194023002004 [DOI] [Google Scholar]
- Yang, Y. C., McClintock, M. K., Kozloski, M., & Li, T. (2013). Social isolation and adult mortality: The role of chronic inflammation and sex differences. Journal of Health and Social Behavior, 54(2), 183–203. doi: 10.1177/0022146513485244 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.