Abstract
Objective
The aim of this study was to evaluate the effect of thermocycling on shear bond strength (SBS) of several resin cement materials to different types of zirconia dental ceramics.
Materials and Methods
120 square shaped disc specimens were fabricated using two types of zirconia blocks (Sagemax and Sirona). Each zirconia group was divided into three sub-groups based on the resin cement bonded to the specimens. Three different self-adhesive resin cements were used (Calibra, Breeze and RelyX). The specimens were further grouped into experimental and control groups (n = 10). The experimental specimens were exposed to a thermo-cycling protocol of 1500 cycles in water bath at 5c and 55c. Specimens were then stored at 37c for 24 h then all specimens underwent SBS test with an Instron machine. Mode of failure was inspected visually and microscopically. Data were statistically analyzed using multivariate analysis of variance followed by one-way analysis of variance, Tukey’s multiple comparison test, student’s t-test for independent samples were used to compare the mean values of SBS in relation to the categorical study variables.
Results
The mean SBS values of experimental groups were significantly lower than control groups for all the 6 combinations of Zirconia and cement types (p < 0.0001). The higher mean difference (14.29 MPa) was observed in the combination of Sagemax and Rely-X. Rely-X displayed the highest SBS among all the cements while no significant difference was found in mean SBS values of Calibra and Breez cements in all groups. The mean SBS values of Sagemax zirconia were significantly higher than the Sirona with all three types of cements (p < 0.0001) within control groups. Microscopic and visual analysis demonstrated a majority of adhesive mode of failure.
Conclusion
Thermocycling significantly reduced the SBS between the zirconia materials and self-adhesive resin cements tested. The amount of reduction varies according to cement and zirconia types.
Keywords: Shear bond strength, Resin cements, Zirconia ceramics, Thermocycling
1. Introduction
Dental ceramic materials have become the restorative materials of choice by majority of dentists as well as patients as they possess superior aesthetics together with high mechanical properties (Alrabeah et al., 2023). Of all the ceramic materials, zirconias are the strongest (Zhang and Lawn, 2018). Although zirconia ceramics have increasingly been promoted as high strength tooth-coloured materials for single crowns and fixed partial dentures, their clinical performance does not merely depend on their inherent high strength (Zhang and Lawn, 2018). Bonding properties to their substrate are key factors for the clinical stability of zirconia ceramic materials (de Matos et al, 2020). Conventional luting cements such as zinc phosphate or glass ionomer cements have been widely accepted for cementation of zirconia prosthesis, however, adhesive resin cements are favourable for better retention and marginal adaptation (Lin et al., 2010). The long-term durability of these bonded restorations is highly influenced by the continuously changing oral conditions.
For durability testing of resin bonding to zirconia surfaces, thermocycling has been recognized as an important factor. Based on an ISO standard (ISO 10477, 1996), thermocycling has been known as a test that is often used to study the behaviour of polymer-based dental materials. Some studies have tested its effects on mechanical properties; others used this technique on a routine basis to simulate temperature variations existing in the oral cavity due to the ingestion of hot and cold food and drinks daily. Several studies have reported a decrease in bond strength after going through the process of thermocycling (Blatz et al., 2007, Mattiello et al., 2013, Spitznagel et al., 2014).
Thermocycling is basically an experimental procedure that is performed on the basis of simulation of thermal conditions existing in the oral cavity. The simulation is kept similar to the actual oral conditions that may include thermal stresses which would have been created in the dentins or within the dental material during the procedure. Thermocycling simulations are preferably delivered in vitro and clinical conditions for experimentation (Cheng and Cheng, 2004, Karimzadeh et al., 2014, Mair, 1989). It has been reported in previous studies that thermo-cycling can increase the surface damage in the composites as thermal shock is created within the constituents of composites. These factors can ultimately produce micro-cracks in the dentins (Dhuru and Lloyd, 1986, Mair, 1989, Montes-G and Draughn, 1986). Thus, it has been deemed necessary over the years to assess the mechanical properties of the dental material by exposing it to the process of thermocycling (Karimzadeh et al., 2014).
In an earlier study that has utilized thermocycling test to evaluate the shear bond strength of glass ionomer and resin cements to zirconia ceramics, Luthy et al. (2006) has demonstrated low bond strength values for Ketac-Cem glass ionomer cement. On the other hand, resin cements used in the same study showed favourable bond strength values compared to the glass ionomer. The authors concluded that thermocycling influenced the bond strength of all luting cements studied and that the effect is material dependent. (Luthy et al., 2006). Manufacturers continue to launch new resin cement materials into the market, however, their clinical behaviour after aging by thermocycling requires further investigation. The investigation and comparative analysis of these modalities hold a prominent significance in the field.
This study was designed to investigate the effect of thermocycling on the shear bond strength of several self-adhesive resin cement materials to different commercially available zirconia ceramics.
2. Materials and methods
2.1. Preparation of specimens
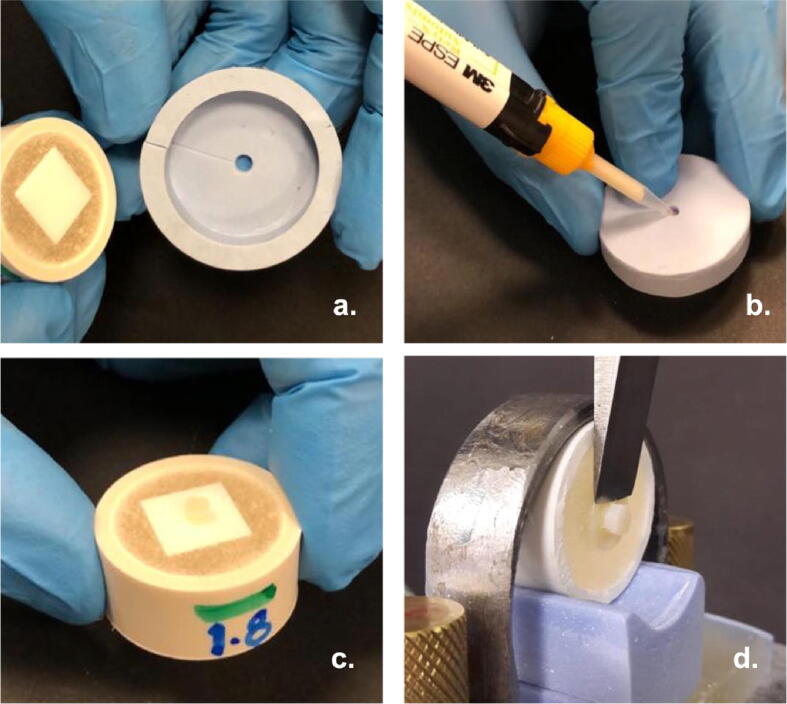
A total of 120 square shaped specimens (12*12*2 mm) were fabricated from machined zirconia blocks. Two types of zirconia ceramics were used in this study; Sagemax (NexxZr S, Sagemax Bioceramics Inc. WA, USA) and Sirona (Cercon ht, Dentsply, Sirona Inc., PA, USA) (Table 1). The specimens were prepared by sectioning a preformed machined zirconia block using high speed Isomet cutting saw machine (Isomet 2000, Bueler Ltd., Lake Bluff, USA). All zirconia specimens (n = 120) were sintered at 1500 °C according to manufacturers’ instructions. The specimens were embedded in an autopolymerizing polyvinyl chloride (PVC) resin within plastic rings leaving one surface exposed for later cement application and forming a custom made cementation jig (Fig. 1a). Each zirconia group (n = 60) was randomly divided into three sub-groups based on the resin cement type bonded to the specimens (n = 20).
Table 1.
Materials used in the study.
| Material | Manufacturer | Chemical Composition |
|---|---|---|
| Breeze | Pentron Clinical, Connecticut, USA | bis-GMA, UDMA, TEGDMA, HEMA, 4-MET, silane treated barium glass, silica, BiOCl, Ca-Al-F-silicate |
| Rely X Unicem | 3 M ESPE, Minnesota USA | dimethacrylate, acetate, methacrylated phosphoric acid ester, glass powder, silica, calcium hydroxide |
| Calibra Universal | Dentsply, Konstanz; Germany | UDMA, dimethacrylate resin, phosphoric acid modified acrylate, barium boron fluoroalumino silicate glass, bis-GMA, Silica, Titanium dioxide and BHT |
| Sirona Circon Ht | Dentsply, Sirona Inc., PA, USA | Zirconium oxide ZrO2 ≥ 89%,, Yttrium oxide Y2O3 5% Hafnium oxide HfO2 < 3%, Aluminium oxide, Silicon oxide < 1% |
| Sagemax NexxZr S | Sagemax Bioceramics Inc. WA, USA | Zirconium oxide ZrO2 ≥ 89%, Yttrium oxide Y2O3 4–6% Hafnium oxide HfO2 ≤ 5%, Aluminium oxide Al2O3 < 1% |
BisGMA, bisphenol a diglycidyl ether dimethacrylate, UDMA, urethane dimethacrylate, TEGDMA, triethyleneglycol dimethacrylate, MDP, methacryloyloxydecyl dihydrogenphosphate, GPDM, glycerol phosphate dimethacrylate, HEMA, 2-hydroxyethyl methacrylate, PEGDMA, polyethylene glycol dimethacrylate, DDDMA, 1,10-decanediol dimethacrylate, EBPADMA, ethoxylated Bisphenol a dimethacrylate, PENTA, dipentaerythritol pentaacrylate monophosphate, 4-META, 4-methacryloxyethyl trimellitate anhydride, and BHT, butylated hydroxytoluene. The composition of the resins and fillers was obtained from the manufacturers.
Fig. 1.
a) Square shaped zirconia specimens embedded in an auto polymerizing PVC resin within plastic rings leaving one surface exposed for cement application. b) Resin cement applied thorough putty mold. c) Finished specimen. d) Mounted specimen on the universal testing machine for SBS test.
2.2. Bonding procedure
Three different types of self- adhesive resin cements were used in this study (Table 1); namely: Calibra (Calibra Universal, Dentsply, Konstanz; Germany), Breeze (Pentron Clinical, Connecticut, USA) and RelyX (Relyx Unicem, 3 M ESPE, Minnesota USA). Each adhesive resin cement was applied by single operator using putty mold (2 mm thickness) (Fig. 1b) and cured according to manufacture instructions using a LED light cure unit (Bluephase G2, Ivoclar Vivadent, Schaan, Liechtenstein). All resin cements were further polymerized with a Triad 2000 machine (Dentsply, York Division USA) for 60 s. All the finished specimens (Fig. 1c) were then stored wet at 37 °C for 24 h.
2.3. Thermocycling procedure
The specimens from the six group combinations (zirconia type & cement type) were further subdivided according to thermocycling exposure into experimental and control groups (n = 10).
The experimental specimens were incorporated into the thermocycling machine (Huber, SD-Mechatronik-Thermocycler, Germany) for 1500 cycles in alternate water bath immersion at 5 °C and 55 °C, with a dwell time of 30 s at each temperature, and a transfer time of 5 s. The thermocycled specimens were left to dry and were stored for 24 h in a non humid environment before testing. The control specimens remained incubated at 37 °C until testing.
2.4. Shear bond strength (SBS) test
After specimens were dried, the SBS for all groups was measured. Cement-to-zirconia bond strength was evaluated using universal testing machine (Instron 5965, Norwood, MA, USA) at a 1.0 mm/min crosshead speed (Fig. 1d). Testing proceeded for either 1 min or until failure. The SBS (in MPa) was calculated by dividing the maximum load (N) by the cross-sectional area (mm2) for each cement resin cylinder over zirconia substrate.
2.5. Analysis of failure
Failure modes were visually and microscopically analysed using optical microscope with fiber-optictrans-illumination under x50 magnification (HIROX digital microscope KH-7700).
The failure type of debonding were classified as follows (Serra-Prat et al., 2014):
Type I: Cohesive, when failure occurred within the cement material, i.e when approximately 2/3 or more of the luting agent has been left on the zirconia surface after SBS testing.
Type II: Adhesive, when failure at cement-zirconia junction, i.e when<1/3 of the cement remained.
Type III: Mixed, when it fell between the limits above.
2.6. Statistical analysis
Data were analysed using SPSS (Statistical Package for Social Sciences) version 26.0 software (IBM Inc., Armonk, NY, USA). Descriptive statistics (mean and standard deviation) were used to describe the quantitative outcome variable sheer bond strength). Multivariate analysis of variance followed by one-way analysis of variance, Tukey’s multiple comparison test, student’s t-test for independent samples were used to compare the mean values of shear bond strength in relation to the categorical study variables two groups (experimental and control), two zirconia types (Sagemax and Sirona) and three cement types (Calibra, Breeze and RelyX). A p-value of ≤ 0.05 was used to report the statistical significance of results.
3. Results
The mean and standard deviation values of shear bond strength of all 12 study groups of zirconia and cement combinations are presented in Table 2.
Table 2.
Mean, standard deviation (Sd.) and mean difference values of shear bond strength of experimental and control groups in relation to the two zirconiz types and three types of cement.
| Type of Zirconia | Type of cement | Mean (Sd.,) of Groups |
Mean Difference | |
|---|---|---|---|---|
| Experimental | Control | |||
| Sagemax | Calibra Breeze Rely X |
6.08(1.18) 6.99(1.33) 8.55(1.22) |
15.66(1.74) 14.66(1.94) 22.79(2.10) |
9.58 7.66 14.29 |
| Sirona | Calibra Breeze Rely X |
5.37(0.45) 5.02(0.36) 6.46(1.12) |
8.32(1.60) 6.59(0.77) 17.52(2.42) |
2.94 1.57 11.06 |
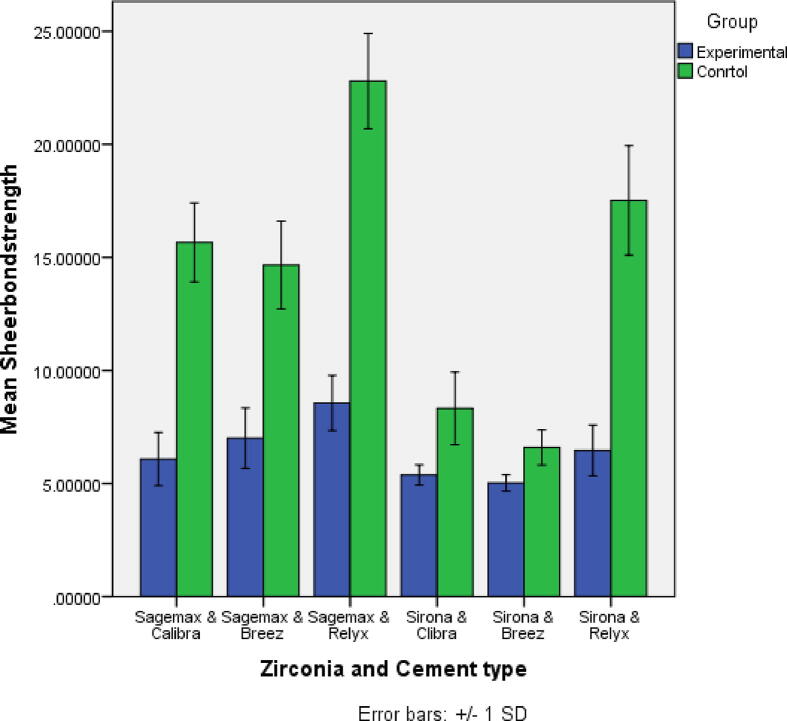
Overall, there was a significant reduction on shear bond strength after thermocycling in all experimental samples compared to the control groups (p < 0.0001) (Fig. 2). The higher mean difference (14.29) was recorded for the combination of Sagemax and RelyX (Table 2) followed by Sirona and RelyX (11.06), Sagemx and Calibra (9.58), Sagemax and Breeze (7.66), Sirona and Calibra (2.94) and Sirona and Breeze (1.57).
Fig. 2.
Comparison of mean values of shear bond strength (MPa) between experimental and control groups for each of the two Zirconia types (Sagemax and Sirona) and three cement types (Calibra, Breeze and RelyX).
The comparison of mean values of shear bond strength across the three types of cements showed that the type of cement significantly influenced the shear bond strength (p < 0.0001) with RelyX demonstrating the highest bond strength to Sagemax and Sirona zirconia substrates (22.79 and 17.52 respectively) and no significant difference was found in mean shear bond strength values between Calibra and Breeze cements (Tables 3).
Table 3.
Comparison of mean values of shear bond strength among the three cements for each zirconia type and between the two zirconia types within each cement type in control and experimental groups.
| Control Groups | |||
|---|---|---|---|
| Sagemax | Sirona | p-value | |
| Calibra Breeze RelyX |
15.66(1.75) 14.66(1.94) 22.80(2.10) |
8.32(1.60) 6.59(0.77) 17.52(2.42) |
< 0.0001 < 0.0001 < 0.0001 |
| p-value | < 0.0001 | < 0.0001 | |
| Experimental Groups | |||
| Sagemax | Sirona | p-value | |
| Calibra Breeze RelyX |
6.08(1.17) 6.99(1.33) 8.56(1.22) |
5.38(0.45) 5.02(0.36) 6.46(1.12) |
0.095 < 0.0001 < 0.001 |
| p-value | 0.001 | < 0.0001 | |
The type of zirconia significantly influenced the shear bond strength within each cement in the control groups where Sagemax zirconia type showed significantly higher mean shear bond strength values than the Sirona zirconia type with all three types of cements (p < 0.0001) (Table 3). The comparison of mean values of shear bond strength between Sagemax and Sirona type within each of the three cements in experimental groups showed statistically significant difference for the two cements (Breeze and RelyX), where the mean sheer bond strength values of Sagemax zirconia type were significantly higher than the Sirona zirconia type (p < 0.0001). However, there was no statistically significant difference between two zirconia types for Calibra cement (p = 0.095) (Table 3).
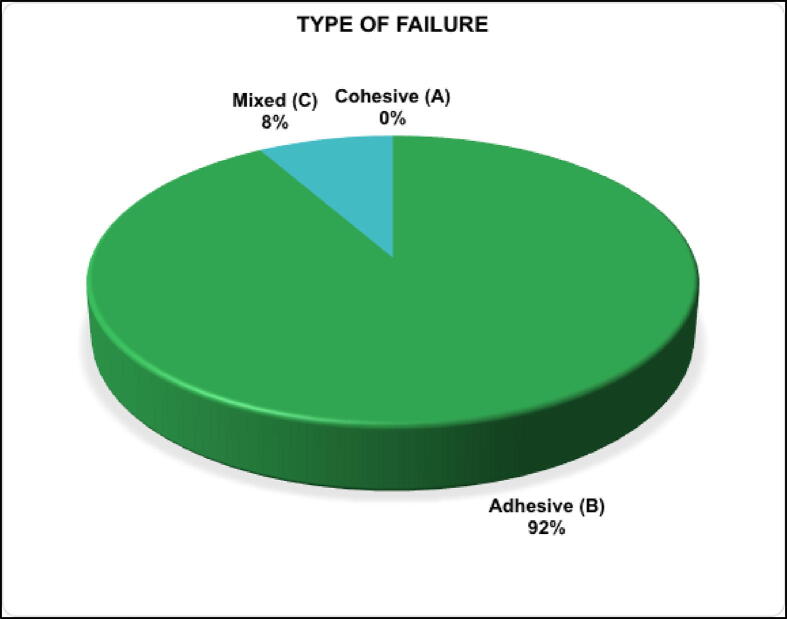
Microscopic and visual analysis of failed samples revealed that most of the failure was adhesive mode of failure 91.7% (Fig. 3a.) The remaining samples showed a combination of adhesive and cohesive failures (Fig. 3b) but none of the specimens demonstrated a pure cohesive failure (Fig. 4).
Fig. 3.
a) A microscopic image (x50) of one specimen from the experimental Sagemax & Calibra combination after SBS test showing adhesive mode of failure, the arrow denotes uniform borders of separation where the luting resin completely detached with no cements left on the zirconia surface. b) A microscopic image (x50) of one specimen from the experimental Sirona & RelyX combination after SBS test showing mixed mode of failure, the arrows denote few luting cement areas left on the zirconia surface.
Fig. 4.
Analysis of failure mode observed microscopically for all test groups.
4. Discussion
The present study has evaluated the effect of thermocycling on shear bond strength of three self-adhesive resin cements luted to two types of commonly used zirconia dental ceramics. Thermocycling is an artificial aging process that simulates clinical settings in in-vitro studies (Amaral et al.,2007). In this method, the samples are embedded in alternating cold and hot water baths for the purpose of simulating the temperature cycles existing in the oral cavity. It is performed aiming to create thermal strains at the bonding interface by thermal changes in water baths between 5 and 55 °C (Kiomarsi et al., 2017). During the procedure, the temperature gradient and the absorbed water by the dental materials induce changes in material properties. Repetition of thermal alterations in such a process is assumed to weaken the bond between resin matrix and filling material in composite restorations (Rinastiti et al., 2011). The effect of thermocycling on shear bond strength however is influenced by several factors such as the temperature setting, dwell time and number of cycles (Amaral et al., 2007, Kiomarsi et al., 2017). The frequency of thermal cycles has been linked to negative effects of thermocycling (Kiomarsi et al., 2017). It has been suggested that 10,000 thermal cycles correspond to about one year of clinical service of dental restorative material (Gale and Darvell, 1999). However, earlier studies have illustrated that thermocycling for periods shorter than a year of service was sufficient to reduce the repair bond strength of composite-to-composite restorations (Ozcan et al., 2007, Rinastiti et al., 2011). Therefore, the effect of 1500 thermal cycles were selected in the current study to resemble a period of approximately two months of service. In fact, the results have demonstrated that the artificial aging protocol implemented in the present study reduced the shear bond strength of all the materials tested. Therefore, the null hypothesis that states that thermocycling has no effect on shear bond strength between the self-adhesive resin cements used and the zirconia substrates was rejected. This finding was in line with previous studies (Abhishek et al., 2022, Lee et al., 2015, Lüthy et al., 2006, Malysa et al., 2022, Ruales-Carrera et al., 2019, Serra-Prat et al., 2014). According to Ozcan et al., this could be explained by the fact that the high heat in alternating cycles weakens the physicochemical properties of resin material and reduces the number of unreacted double bonds on the surface and within the resin structure (Ozcan et al., 2007).
Zirconia ceramic restorations can either be luted to abutment teeth by conventional cementation or adhesive fixation (Lin et al., 2010). Besides improved bonding to teeth and ceramics substrates, self-adhesive resin cements were chosen because they have the advantages of favourable mechanical properties, superior aesthetics and ease of handling (Samran et al.,2019). Resin cement selection seems to be a more relevant factor in bonding to zirconia (Lin et al., 2010). In the two zirconia groups tested, the application of phosphate monomer-containing self- adhesive cement (Rely X) attained the best bonding results. Manufacturers recommend self-adhesive resin cements that contain phosphate monomer components, because increased bond strength is possible to achieve when using them. Resin cements containing phosphate monomer agents show excellent bonding strength and remain stable even after thermocycling treatment and long-term storage in water (Lee et al., 2015, Mirmohammadi et al., 2010). Furthermore, phosphate monomers, such as phosphoric acid and methacrylated phosphoric ester, bond to zirconia and to teeth directly, which results in better bonding strength (Mirmohammadi et al., 2010). Among the three cement materials tested in the current study, only Rely X had methacrylated phosphoric acid ester group in its ingredient. This explains the high shear bond strength values observed in comparison to the other two cements, Calibra and Breeze, which contained Bis-GMA as their adhesive monomer and both have showed comparable SBS values. In fact, the current results illustrated that the highest shear bond strength was noted when Sagemax zirconia was combined with Rely X both in the control and experimental groups, and when looking into the Sagemax manufacturer’s instructions it was recommended to use SpeedCem Plus® as the adhesive cement for Sagmax NexxZr S; this cement has a methaacrylated phosphoric acid ester group which is similar to the one found in the Rely-X cement used in the present study. This finding highlights the importance of following the manufacturer’s instructions clinically when choosing the right cement for zirconia ceramic restorations. However, a significant drop in SBS was noticed in Rely X cement after thermocycling which could be related to the hydrophilicity of resin cements (da Silva et al., 2014). Samran et al. stated that self-adhesive resin cements are hydrophilic due to the high content of acidic phosphate functional monomers, which in turn induce higher water sorption and, consequently, may be susceptible to hydrolytic degradation particularly at the resin cement-zirconia interface (Samran et al.,2019). Water molecule diffusion into the bonding interface may weaken the bond strength by means of hydrolytic degradation. Nevertheless, thermal stress created by the difference in coefficients of thermal expansion between zirconia and adhesive resin cement during thermocycling could enhance further hydrolytic degradation of the bonding interface (Samran et al.,2019).
To achieve long term durable chemical bond to zirconia surfaces, it has been recommended to pre-treat the intaglio surface by airborne particle abrasion using Al2O3 particles. Such treatment increases the surface roughness, surface area, and surface energy which in turn enhances the wettability of zirconia surfaces21,28. Many studies have also reported that when using resin cements including phosphate monomer in combination with alumina air blasting, bonding strength increased (Lin et al., 2010, Samran et al., 2019). In these studies, groups with airborne-particle abrasion demonstrated mostly cohesive failure modes; suggesting even stronger chemical bonding to the zirconia surface. The zirconia surfaces in the present study, however, didn’t not receive any form of surface pre-treatment and therefore were lacking the micromechanical interlocking forces between the cement and zirconia surfaces which explains the abundance of adhesive mode of failure detected compared to the results of previous studies (Lin et al., 2010, Samran et al., 2019). Unabraded or untreated zirconium oxide ceramic is a relatively inert substrate with low surface energy and wettability (Lin et al., 2010, Yang et al., 2010). Moreover, airborne-particle abrasion may generate hydroxyl groups on the zirconia surfaces, facilitating the chemical reaction with self-adhesive resin cement containing phosphate monomers (Samran et al., 2019, Yang et al., 2010).
It is critical for the bonding strength of resin cements to be maintained after a long-term aging process. Regardless of the types of cements, the shear bonding strength in the current study tended to decrease in all groups after thermocycling. A weak mechanochemical bond between zirconia restorations and resin cement have a significant effect on the prognosis and clinical survival of these ceramic restorations. Further studies on bond strengths using various surface treatments on zirconia and various kinds of cements are mandatory to recommend the best cement-restoration combination that could withstand such hostile oral environment.
5. Conclusion
Within the limitations of this study, the following conclusions were obtained,
-
1.
Thermocycling significantly reduced the shear bond strength between the zirconia materials and self-adhesive resin cements tested.
-
2.
The shear bond strength of resin cements to zirconia ceramics was influenced by the cement type. RelyX cement demonstrated the highest shear bond strength among the three cement materials tested.
-
3.
The failure mode between the cements and zirconia substrates was mainly adhesive mode of failure.
CRediT authorship contribution statement
Ghada Alrabeah: Conceptualization, Methodology, Visualization, Formal analysis, Writing – review & editing, Project administration, Resources, Supervision, Validation. Sadeem Alomar: Methodology, Data curation, Investigation, Software, Resources, Writing – original draft. Azizah Almutairi: Methodology, Data curation, Investigation, Software, Resources, Writing – original draft. Hafsah Alali: Methodology, Data curation, Investigation, Software, Resources, Writing – original draft. Aws ArRejaie: Conceptualization, Methodology, Visualization, Writing – review & editing, Project administration, Supervision, Validation, Resources, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank the College of Dentistry Research Center at King Saud University for facilitating the project and providing physical laboratory to run the experiment. This research received no external funding
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Ghada Alrabeah, Email: galrabeah@ksu.edu.sa.
Sadeem Alomar, Email: dsash98@gmail.com.
Azizah Almutairi, Email: azizah200000@gmail.com.
Hafsah Alali, Email: alali.hafsah@gmail.com.
Aws ArRejaie, Email: aarrejaie@ksu.edu.sa.
References
- Abhishek G., Vishwanath S.K., Nair A., Prakash N., Chakrabarty A., Malalur A.K. Comparative evaluation of bond strength of resin cements with and without 10-methacryloyloxydecyl dihydrogen phosphate (mdp) to zirconia and effect of thermocycling on bond strength–An in vitro study. J. Clin. Exper. Dent. 2022;14(4):e316. doi: 10.4317/jced.59324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alrabeah G., Shabib S., Almomen R., Alhedeithi N., Alotaibi S., Habib S.R. Effect of home bleaching on the optical properties and surface roughness of novel aesthetic dental ceramics. Coatings. 2023;13(2):330. [Google Scholar]
- Amaral F.L., Colucci V., Palma-Dibb R.G., Corona S.A. Assessment of in vitro methods used to promote adhesive interface degradation: a critical review. J. Esthet. Restor. Dent. 2007;19:340–345. doi: 10.1111/j.1708-8240.2007.00134.x. [DOI] [PubMed] [Google Scholar]
- Blatz MB, Chiche G, Holst S, Sadan A. 2007. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 1;38(9). [PubMed]
- Cheng YT, Cheng CM. 2004. Scaling, dimensional analysis, and indentation measurements. Mater Sci Engin: Reports. 1;44(4):91-149.
- da Silva E.M., Miragaya L., Sabrosa C.E., Maia L.C. Stability of the bond between two resin cements and an yttria-stabilized zirconia ceramic after six months of aging in water. J. Prosthet. Denti. 2014;112(3):568–575. doi: 10.1016/j.prosdent.2013.12.003. [DOI] [PubMed] [Google Scholar]
- de Matos J.D., Nakano L.J., Bottino M.A., de Jesus R.H., Maciel L.C. Current considerations for dental ceramics and their respective union systems. Rev. Bras Odontol. 2020;77:e1768. [Google Scholar]
- Dhuru VB, Lloyd CH. 1986. The fracture toughness of repaired composite. J Oral Rehab. 1;13(5):413-21. [DOI] [PubMed]
- Gale M.S., Darvell B.W. Thermal cycling procedures for laboratory testing of dental restorations. J. Dent. 1999;27:89–99. doi: 10.1016/s0300-5712(98)00037-2. [DOI] [PubMed] [Google Scholar]
- ISO. International Standards Organization. Amendment ISO 10477. Dentistry—Polymer-Based Crown and Bridge Materials. Geneva: ISO, 1996.
- Karimzadeh A., Ayatollahi M.R., Shirazi H.A. Mechanical properties of a dental nano-composite in moist media determined by nano-scale measurement. Int. J. Mater. Mech. Manufactur. 2014;2(1):67–72. [Google Scholar]
- Kiomarsi N, Saburian P, Chiniforush N, Karazifard MJ, Hashemikamangar SS. 2017. Effect of thermocycling and surface treatment on repair bond strength of composite. J Clin Exp Dent. 1;9(8):e945-e951. [DOI] [PMC free article] [PubMed]
- Lee J.J., Kang C.K., Oh J.W., Seo J.M., Park J.M. Evaluation of shear bond strength between dual cure resin cement and zirconia ceramic after thermocycling treatment. J. Adv. Prosthod. 2015;7(1):1–7. doi: 10.4047/jap.2015.7.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., Shinya A., Gomi H., Shinya A. Effect of self-adhesive resin cement and tribochemical treatment on bond strength to zirconia. Int. J. Oral Sci. 2010;2(1):28–34. doi: 10.4248/IJOS10002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lüthy H, Loeffel O, Hammerle CH. 2006. Effect of thermocycling on bond strength of luting cements to zirconia ceramic. Dent Mater. 28;22(2):195-200. [DOI] [PubMed]
- Mair LH. 1989. Surface permeability and degradation of dental composites resulting from oral temperature changes. Dent Mater. 1;5(4):247-5 [DOI] [PubMed]
- Malysa A., Wezgowiec J., Grzebieluch W., Danel D.P., Wieckiewicz M. Effect of thermocycling on the bond strength of self-adhesive resin cements used for luting CAD/CAM ceramics to human dentin. Inter. J. Molec. Sci. 2022;23(2):745. doi: 10.3390/ijms23020745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mattiello R.D., Coelho T.M., Insaurralde E., Coelho A.A., Terra G.P., Kasuya A.V., Favarão I.N., Gonçalves L.D., Fonseca R.B. A review of surface treatment methods to improve the adhesive cementation of zirconia-based ceramics. ISRN Biomaterials. 2013:1–10. [Google Scholar]
- Mirmohammadi H., Aboushelib M.N., Salameh Z., Feilzer A.J., Kleverlaan C.J. Innovations in bonding to zirconia based ceramics: Part III. Phosphate monomer resin cements. Dent Mater. 2010;26(8):786–792. doi: 10.1016/j.dental.2010.04.003. [DOI] [PubMed] [Google Scholar]
- Montes-G GM, Draughn RA. 1986. In vitro surface degradation of composites by water and thermal cycling. Dent Mater. 1;2(5):193-7. [DOI] [PubMed]
- Ozcan M., Barbosa S.H., Melo R.M., Galhano G.A., Bottino M.A. Effect of surface conditioning methods on the microtensile bond strength of resin composite to composite after aging conditions. Dent. Mater. 2007;23:1276–1282. doi: 10.1016/j.dental.2006.11.007. [DOI] [PubMed] [Google Scholar]
- Rinastiti M., Zcan M., Siswomihardjo W., Busscher H.J. Effects of surface conditioning on repair bond strength of nonaged and aged microhybrid, nanohybrid, and nanofilled composite resins. Clin. Oral Investig. 2011;15:625–633. doi: 10.1007/s00784-010-0426-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruales-Carrera E., Cesar P.F., Henriques B., Fredel M.C., Özcan M., Volpato C.A. Adhesion behavior of conventional and high-translucent zirconia: Effect of surface conditioning methods and aging using an experimental methodology. J. Esthet. Rest. Dent. 2019;31(4):388–397. doi: 10.1111/jerd.12490. [DOI] [PubMed] [Google Scholar]
- Samran A., Al-Ammari A., El Bahra S., Halboub E., Wille S., Kern M. Bond strength durability of self-adhesive resin cements to zirconia ceramic: An in vitro study. J. Prosthet. Dent. 2019;121(3):477–484. doi: 10.1016/j.prosdent.2018.03.026. [DOI] [PubMed] [Google Scholar]
- Serra-Prat J, Cano-Batalla J, Cabratosa-Termes J, Figueras-Àlvarez O. 2014. Adhesion of dental porcelain to cast, milled, and laser-sintered cobalt-chromium alloys: shear bond strength and sensitivity to thermocycling. J Prosth Dent. 1;112(3):600-5. [DOI] [PubMed]
- Spitznagel FA, Horvath SD, Guess PC, Blatz MB. 2014. Resin bond to indirect composite and new ceramic/polymer materials: a review of the literature. J of Esthet Rest Dent. 1;26(6):382-93. [DOI] [PubMed]
- Yang B., Barloi A., Kern M. Influence of air-abrasion on zirconia ceramic bonding using an adhesive composite resin. Dent. Mater. 2010;26(1):44–50. doi: 10.1016/j.dental.2009.08.008. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Lawn B.R. Novel zirconia materials in dentistry. J. Dent. Res. 2018;97(2):140. doi: 10.1177/0022034517737483. [DOI] [PMC free article] [PubMed] [Google Scholar]