Abstract
Purpose
To evaluate the current literature on the effects of anatomic changes caused by the Latarjet procedure and to identify areas for future research.
Methods
English-language studies that addressed the consequences of anatomic alterations after the open Latarjet procedure were included. Articles written in languages other than English, reviews, and case reports were excluded. Titles and abstracts were screened by 2 authors. Studies that met the inclusion criteria were screened by the same authors. The following data were extracted from the included studies: authors, year of publication, journal, country of origin, aims or purpose, study population and sample size, methods, procedure, intervention type, and key findings that relate to the scoping review questions.
Results
Twenty-two studies were included for analysis, yielding the following findings: First, the Latarjet procedure may change the position of the scapula owing to pectoralis minor tenotomy and/or transfer of the conjoint tendon. Second, dissection of the coracoacromial ligament may result in increased superior translation of the humeral head. The impact of this increased translation on patients’ function remains unclear. Third, the subscapularis split shows, overall, better internal rotation strength compared with subscapularis tenotomy. Fourth, passive external rotation may be limited after capsular repair. Fifth, despite the movement of the conjoint tendon, elbow function seems unchanged. Finally, the musculocutaneous nerve is lengthened with a changed penetration angle into the coracobrachialis muscle, but the clinical impact seems limited.
Conclusions
The Latarjet procedure leads to anatomic and biomechanical changes in the shoulder. Areas of future research may include better documentation of scapular movement (bilateral, as well as preoperative and postoperative) and elbow function, the effect of (degenerative) rotator cuff ruptures after the Latarjet procedure on shoulder function, and the impact of capsular closure and its contribution to the development of glenohumeral osteoarthritis.
Clinical Relevance
This comprehensive overview of anatomic changes after the Latarjet procedure, with its effects on shoulder and elbow function, showed gaps in the current literature. Orthopaedic shoulder surgeons and physical therapists could use our findings when providing patient information and performing future clinical research.
The Latarjet procedure is a surgical treatment option for patients with anteroinferior instability of the shoulder. This procedure involves transferring the coracoid to the anterior rim of the glenoid, resulting in increased glenohumeral stability with relatively low recurrence rates.1, 2, 3 Unlike other bone block procedures, the Latarjet procedure provides stabilization beyond the effect of the bone graft alone, owing to the so-called sling effect of the conjoint tendon.4 The procedure is particularly effective in patients with combined glenoid and humeral bony lesions, as well as those with recurrent glenohumeral instability after a Bankart repair.
The Latarjet procedure is a nonanatomic procedure because the operation involves several steps adapting the shoulder anatomy, possibly leading to functional changes. Orthopaedic surgeons and their patients should be aware of any clinically significant changes in anatomy and function before choosing Latarjet stabilizing surgery. This overview can provide insight into changes that are currently not being evaluated by standard outcome measures.
The purposes of this review were to evaluate the current literature on the effects of anatomic changes caused by the Latarjet procedure and to identify areas for future research. We hypothesized that the literature regarding this subject would be limited, with gaps in the literature, providing outcome measures that require attention.
Methods
A scoping review with a systematic search was performed. Scoping reviews are often considered when the literature on a topic is broad, resulting in an overview of the existing literature on that topic (unlike systematic reviews, which often address focused research questions). This scoping review tried to give an overview of the current literature and focused on gaps in the current literature.5 This study adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-analyses) extension for Scoping Reviews (PRISMA-ScR).6
Inclusion and Exclusion Criteria
English-language studies that addressed anatomic changes after the Latarjet procedure and the consequences of these alterations were included. To facilitate the inclusion of articles that discussed anatomic and functional changes, different steps of the Latarjet procedure were addressed. These steps included (1) tenotomy of the pectoralis minor tendon, (2) release of the coracoacromial ligament (CAL), (3) tenotomy or splitting of the subscapularis tendon, (4) shoulder capsulotomy, (5) transposition of the coracoid with the conjoint tendon, and (6) changes for the musculocutaneous nerve. To minimize heterogeneity in this study, we focused on the open Latarjet procedure. Because the differences between the Latarjet procedure and the open Bristow (or Latarjet-Bristow) procedure are minimal and both techniques are commonly used, both techniques were included. The less commonly performed congruent-arc procedure (in which the coracoid is rotated 90° on its longitudinal axis) and the arthroscopic Latarjet procedure were excluded. In addition, articles written in languages other than English, reviews, and single case reports were excluded.
Literature Search and Study Selection
Relevant studies were identified by searching PubMed, Embase (Ovid), Cochrane Central Register of Controlled Trials (Wiley), SPORTDiscus (EBSCO), and Web of Science (Clarivate Analytics) from inception up to June 16, 2022, by SPV (an information specialist). The following terms, including synonyms, closely related words, and steps of the procedure, were used as index terms or free-text words: Latarjet, Bristow, coracoid transfer, pectoralis minor tenotomy, subscapularis tendon, coracoacromial ligament, conjoint tendon, and shoulder capsule. Full search strategies for all databases are available in Appendix 1. Duplicate articles were excluded by the information specialist (SPV) using EndNote X8 (2018 release; Clarivate Analytics). Titles and abstracts were screened by 2 authors (AvdK and LV). Studies that met the inclusion criteria were screened by the same authors. Discrepancies between the 2 reviewers were assessed by 2 shoulder specialists: a professor of orthopaedic surgery (MvdB) and a professor of musculoskeletal mechanics (HV). References were manually checked, and cross-referencing of the included articles was performed to find additional studies.
Data Extraction
The following data were extracted: authors, year of publication, journal, country of origin, aims or purpose, study population and sample size, methods, procedure, intervention type, and key findings that relate to the scoping review questions.
Results
Literature Screening
A total of 2,358 studies were screened, of which 98 were eligible for inclusion. After reading of the full texts, 22 studies were included for analysis (Appendix Table 1). Cross-referencing revealed no other studies. The findings were addressed in a step-by-step overview, divided according to the steps of the Latarjet procedure.
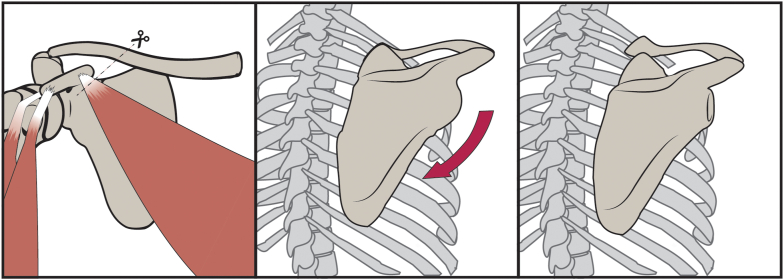
Tenotomy of Pectoralis Minor Tendon
To obtain access to the anterior side of the glenohumeral joint and to pass the coracoid bone block, the pectoralis minor tendon should be released. The pectoralis minor tendon originates from the margins of the third to fifth rib and inserts at the medial border of the coracoid process. In the Latarjet procedure, the pectoralis minor tendon is detached from the coracoid and is not reattached. Pectoralis minor tenotomy may affect the scapular position because its function is protraction of the scapula.7 A computed tomography–based study, performed 6 months after surgery, showed no significant difference in the scapular position between the operative side and nonoperative side, but a small trend toward scapular retraction was observed.8 The α angle (i.e., angle between the tangent to the posterior surface of the scapula and the anterior-posterior axis) of the affected side increased from a mean of 49° to 52° (Fig 1).8 Carbone et al.9 showed the development of scapular dyskinesis 20 months after the Latarjet procedure, with associated lower functional scores (Rowe score, 82 vs 90 for dyskinesis vs no dyskinesis [P = .047]; Subjective Shoulder Value, 81 vs 90 [P = .046]). Direct associations between shoulder function and pectoralis minor tenotomy were not shown in any study.
Fig 1.
Diminished protraction of scapula after pectoralis minor tenotomy. Dashed line on the left shows pectoralis minor tenotomy. The arrow in the middle figure shows increased retraction of the scapula.
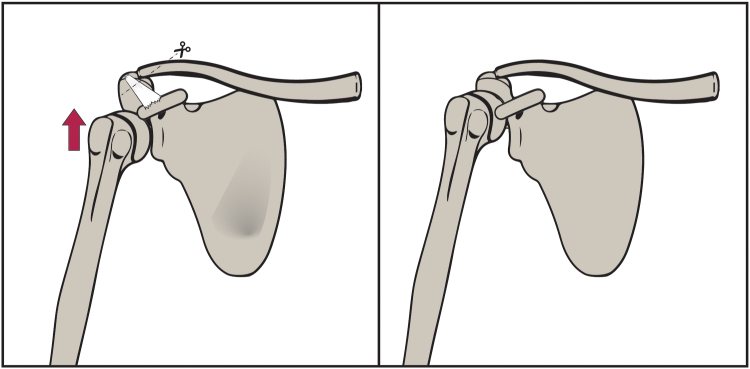
Release of CAL
The CAL is a strong triangular ligament between the acromion and the coracoid process. To move the coracoid from its original place to the anterior rim of the glenoid, the CAL has to be released. Therefore, any function of the CAL may be absent after the Latarjet procedure. The primary function of the CAL is preventing superior translation of the humeral head by acting as a static restraint.10,11 An intact CAL is also interacting with the coracohumeral ligament to provide restraint to anterior and superior translation. Releasing the CAL therefore resulted in increased superior shoulder translation (mean, 2.3 mm) in most joint configurations and loading conditions after the Latarjet procedure in cadavers (Fig 2).12 Di Giacomo et al.13 showed in an in vitro study that active isometric contraction of the internal rotators and adductors in the abduction–external rotation (ABER) position did not result in significant superior translation. Other clinical studies comparing the outcomes of CAL dissection in patients undergoing the Latarjet procedure have not been performed.
Fig 2.
Increased superior shoulder translation after resection of coracoacromial ligament. The dashed line on the left figure shows resection of the coracoacromial ligament. The arrow on the left figure shows the direction of humerus translation after resection.
Subscapularis Tendon
The primary function of the subscapularis tendon is internal rotation of the humeral head, and it functions as an active anterior stabilizer of the glenohumeral joint. To obtain access to the glenohumeral joint from a deltopectoral approach, the subscapularis tendon should be “opened.” Originally, the entrance to the glenoid was obtained by tenotomy and detachment of the tendon at the insertion. Later, a modification of the procedure was introduced, in which a longitudinal divulsion (split) of the subscapularis muscle was used.14 Over the years, multiple studies have investigated the outcomes of tenotomy and splitting of the subscapularis muscle during Latarjet surgery. This subject is important because an intact subscapularis tendon is a necessary prerequisite for an optimal outcome of stabilization.15 Several studies showed no differences between preoperative and postoperative subscapularis strength16 or between the affected and unaffected sides17 after splitting the tendon. Studies that compared splitting versus tenotomy showed significantly less peak torque in the tenotomy group compared with the splitting group.18,19 An imaging study showed no fatty infiltration—or only minimal fatty infiltration—in the subscapularis muscle after splitting,20 whereas muscle atrophy and fatty infiltration were found after tenotomy.21 On the contrary, Ersen et al.22 reported no difference in internal rotation strength between the 2 methods. Moreover, 1 study showed reduced function compared with the contralateral side after splitting.23
Shoulder Capsulotomy
The shoulder capsule is opened during the Latarjet procedure. According to Walch and Boileau,24 the success of the Latarjet procedure results from a combination of the (1) the conjoint tendon sling effect, (2) the bone block effect, and (3) the capsular repair. Repairing the capsule is therefore considered an important step in the Latarjet procedure because it may contribute to the stabilizing mechanism.15,25 However, a previous study of the Latarjet procedure showed a decrease in external rotation with capsular repair in comparison to the same procedure without capsular repair.26 The same results were found in a study that included patients undergoing the Bristow procedure.27 The rationale behind this restriction is that capsular repair leads to tightening of the anterior structures.26,28 Another study of the Latarjet procedure showed clinically insignificant changes in external rotation.29 Closing the capsule to the coracoid process resulted in greater range of motion compared with closing to the native glenoid.28 However, closing the capsule to the glenoid caused the bone block to remain extra-articular, which may prevent osteoarthritis in the long term.28
Transposition of Coracoid With Conjoint Tendon
The conjoint tendon, consisting of the short head of the biceps tendon and the coracobrachialis tendon, inserts at the coracoid bone block. During the Latarjet procedure, the origin of the conjoint tendon changes from the coracoid to the anterior rim of the glenoid, resulting in a different, shorter trajectory, which theoretically may impact its function. The primary function of the short head of the biceps is flexion and supination of the forearm, and the function of the coracobrachialis muscle is adduction and flexion of the glenohumeral joint. Two studies investigated the impact of the Latarjet procedure on the function of the short head of the biceps and showed preserved supination and flexion function in the elbow joint.30,31 Imaging studies showed no difference in the echogenicity of the biceps tendon before versus after the Latarjet procedure, with no differences for the dominant versus nondominant side,32 and showed that the conjoint tendon remained intact.17 The function of the coracobrachialis muscle was not studied.
Changes for Musculocutaneous Nerve
The musculocutaneous nerve arises from the lateral cord of the brachial plexus and enters the coracobrachialis muscle at the level of the latissimus dorsi tendon. It runs between the short head of the biceps tendon and the brachialis muscle. The musculocutaneous nerve innervates the lateral side of the forearm, as well as the coracobrachialis, brachialis, and biceps tendon. Injury to the musculocutaneous nerve is a described complication of the Latarjet procedure, occurring in 1.8% of cases.33 The literature shows that the musculocutaneous nerve is lengthened (mean distance between lateral cord of brachial plexus to entry point of nerve into coracobrachialis muscle of 47.2 mm; after Latarjet procedure, 48.4 mm) and that the penetration angle of the nerve into the coracobrachialis muscle differs after the Latarjet procedure (121° before and 136° after).34 The nerve is also described as notably lax and as overlapping the axillary nerves postoperatively.35 A clinical study showed no changes in nerve conduction of the musculocutaneous nerve in the neutral position, but changes did occur in the externally rotated position.36
Discussion
The most important finding of this review is that the Latarjet procedure results in anatomic and functional changes in the shoulder. First, the Latarjet procedure may change the position of the scapula owing to pectoralis minor tenotomy and/or transfer of the conjoint tendon. Second, dissection of the CAL may result in increased superior translation of the humeral head. The impact of this increased translation on patients’ function remains unclear. Third, the subscapularis split shows, overall, better internal rotation strength compared with subscapularis tenotomy. The split approach is therefore more preferable for the management of the subscapularis muscle during the Latarjet procedure. Fourth, passive external rotation may be limited after capsular repair. Fifth, despite the movement of the conjoint tendon, elbow flexion function seems unchanged. Finally, the musculocutaneous nerve is lengthened with a changed penetration angle into the coracobrachialis muscle, but the clinical impact seems limited. Possible consequences of the Latarjet procedure are discussed in the following sections.
Pectoralis Minor Tenotomy
From the current literature, it was concluded that the scapular position may be changed by the Latarjet procedure, resulting in changed scapular movement and reduced functional scapula scores. Included studies hypothesized that this may be because of the pectoralis minor tenotomy procedure, which results in decreased protraction.8,9 The patients in whom scapular dyskinesis developed (with lower Subjective Shoulder Values for function, n = 5) were classified as having type I dyskinesis, which is characterized by the prominence of the inferior-medial scapular angle and is associated with excessive anterior tilting of the scapula. However, one would have expected type III dyskinesis (diminished anterior tilting) after pectoralis minor tenotomy. A possible explanation for this is the shifted vector of the conjoint tendon toward lateral and inferior. This is in line with the study of Cerciello et al.,8 who observed a loss of balance between groups of antagonist muscles, with increased scapular motion in the axial plane in the early postoperative period (45 days). After a follow-up period of 6 months (after rehabilitation was finished), no differences in the scapular position were observed.8 A pectoralis minor–sparing Latarjet method has been studied, in which no scapular dyskinesis was found.37 However, this study was performed in only 9 patients and is therefore not very sensitive to possible changes in scapular position.
Unfortunately, preoperative scapular motion was not observed in most of the studies discussed in this article (except the study of Cerciello et al.8). This makes the interpretation questionable because it cannot be assumed that the preoperative scapular function was normal. Moreover, scapular position and function depend on multiple other factors that have not been studied so far, for example, transposition of the conjoint tendon and the loss of balance between groups of antagonists due to detachment of the tendons.
Some studies noted that scapular function of the operative shoulder differed from that of the nonoperative shoulder. From the current literature, it remains unclear whether this concerns a functional adaptation or a negative “side effect” of the procedure. However, because some studies showed reduced patient-reported outcomes, it is important to observe scapular position and motion in patients undergoing the Latarjet procedure before and after surgery, comparing the affected side with the unaffected side. Clinical methods as described by McClure et al.38 or Kibler et al.,39 in addition to more sophisticated methods such as a 3-dimensional wing computed tomography,40 can be used. This is especially important for patients with ongoing pain after the rehabilitation program is finished.
Release of CAL
Performing the Latarjet procedure can lead to increased superior translation of the humeral head in most joint configurations, as shown in cadaveric studies. Values of superior translation after the Latarjet procedure were found to be significantly increased; however, it is unknown whether they are clinically relevant (difference of around a few millimeters).12 In a situation in which an allograft was used for the Latarjet procedure, the CAL remained intact, and testing of this allograft showed that there was no significant difference in superior translation.12 From an evolutionary perspective, this ligament exists only in hominoids and is probably a response to the loads imposed by the humeral head; it has been described as a “neo-articulation.”41 The application of muscle loads (rotator cuff, conjoint tendon, and deltoid) decreased the abnormal superior displacement.12,13 It is therefore suggested that the impact of CAL dissection is minimal in patients with an intact rotator cuff, which is a requirement for all patients undergoing the Latarjet procedure. Currently, no studies have published the results of patients with (degenerative) cuff tears after the Latarjet procedure, which may impact superior translation.
In acromioplasty (which is often performed for subacromial impingement symptoms), CAL resection has also been discussed, and preservation or repair has been indicated.10,42,43 One of the approaches is reconstruction through suture fixation of the detached portion. However, it has also been shown that the CAL can re-form spontaneously after a few years.44 To prevent dissection of the CAL, a study investigated whether preservation of the posterior bundle would be feasible (to keep some of its function intact) and showed that the posterior bundle may be spared during harvesting of the coracoid process.45
Next to the CAL’s function as a neo-articulation, 2 other functions of the CAL have not been addressed in the current literature. Because the CAL comprises many Pacinian corpuscles (measuring acceleration of shoulder during movement), Ruffini receptors, and Golgi tendon organ–like receptors (providing information about static position and angle of joint rotation),46 it is possible that the CAL serves as a sensory organ that provides afferent static and dynamic proprioceptive signals.10 In addition, the CAL transmits load across the scapula10,47: Forces that are exerted on the coracoid process by all the muscles connected are partially transmitted to the acromion, and vice versa. However, the clinical significance of missing this force transmitter is currently unknown.
Subscapularis Tendon
Splitting or dissecting the subscapularis tendon may impact functional outcomes after the Latarjet procedure, especially internal rotation strength. A subscapularis split generally shows superior outcomes to tenotomy, according to a recent systematic review and meta-analysis.48 One study showed that the subscapularis had less strength compared with the healthy contralateral side after the splitting method.23 However, whether this is the impact of the subscapularis tenotomy or split or is due to the problem itself (recurrent dislocations) remains unclear if preoperative measurements are not performed.
Clinical studies that focused on the function of the subscapularis itself were not found in the current literature. This is because internal rotation is the result of multiple muscles, which include the subscapularis tendon, teres major, pectoralis major, and latissimus dorsi, as well as the anterior part of the deltoid muscle. Studying the single effect of the subscapularis in a clinical setting is therefore difficult. However, from magnetic resonance imaging studies, it is known that after splitting, the tendon recovers without atrophy or fatty infiltration.20
Capsulotomy
The range of external rotation may be decreased after a bone block transfer procedure with capsular repair, possibly owing to anterior tightening. Repairing the capsule to the coracoid appears to be beneficial to avoid limited range of motion.28 However, direct contact of the humeral head with the transferred coracoid might increase the risk of osteoarthritis. The effect on the development of osteoarthritis in the long term has been studied, showing an incidence of osteoarthritis of 8.5% after 10 years of follow-up.49 The extracapsular situation of the bone block appeared to be an important factor in the prevention of osteoarthritis in the study.49
Transposition of Coracoid With Conjoint Tendon
The functions of the short head of the biceps muscle remain largely intact after the Latarjet procedure. Flexion in the elbow joint was shown to be retained or even increased after the Latarjet procedure in all studies. This movement is provided not only by the short head of the biceps but also by the brachialis and brachioradialis muscle. The reason for this retained or even increased flexion might be the effect of postoperative rehabilitation and training, but it also may be due to increased mental trust because of the treated instability.30 From studies based on distal biceps ruptures, it is known that the biceps contributes to around 30% of flexion power in the elbow.50 The amount of flexion power loss due to changes in the conjoint tendon is currently unknown, but this will generally not exceed 30% (because the percentage of 30% is based on a rupture of the insertion) and is therefore considered acceptable. Supination in the elbow joint is slightly decreased in most studies, although the significance remains questionable.30,31 This movement is also provided not only by the short head of the biceps muscle but also by the supinator muscle. From distal biceps rupture studies, it is known that the biceps muscle contributes to 40% of the supination strength.50 Again, the impact of shortening on final strength is unknown.
Changes for Musculocutaneous Nerve
When the Latarjet procedure is performed, the musculocutaneous nerve may be lengthened and may penetrate, with a changed angle, into the coracobrachialis muscle, as has been shown in cadaveric studies. To determine the clinical impact of the transposition, Lópiz et al.36 studied the neurophysiological effects on the musculocutaneous nerve. They found no changes in conduction in the neutral position, but 36% of cases (n = 4) showed neurophysiological changes in the externally rotated position.36 However, in the medium-term follow-up, this did not have a clinical impact. Because the impact on functional outcomes seems limited, the adapted anatomy is relevant for revision surgery. Freehill et al.35 described that the musculocutaneous nerve covers the axillary nerve after the Latarjet procedure, meaning that both nerves are at potential risk during revision surgery.
Limitations
This study has several limitations. First, the Latarjet procedure is a well-known procedure, which has resulted in many variations in the surgical technique. It might therefore be difficult to compare studies because the procedures have minor differences that may have implications on the function of the shoulder. To minimize this problem, we excluded congruent-arc and arthroscopic Latarjet procedures. Second, we have shown that for most subjects, the existing evidence is limited. Our conclusions are therefore based on only a few studies.
Conclusions
The Latarjet procedure leads to anatomic and biomechanical changes in the shoulder. Areas of future research may include better documentation of scapular movement (bilateral, as well as preoperative and postoperative) and elbow function, the effect of (degenerative) rotator cuff ruptures after the Latarjet procedure on shoulder function, and the impact of capsular closure and its contribution to the development of glenohumeral osteoarthritis.
Acknowledgment
Footnotes
The authors report the following potential conflicts of interest or sources of funding: The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Allain J., Goutallier D., Glorion C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J Bone Joint Surg Am. 1998;80:841–852. doi: 10.2106/00004623-199806000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Ernstbrunner L., Wartmann L., Zimmermann S.M., Schenk P., Gerber C., Wieser K. Long-term results of the open Latarjet procedure for recurrent anterior shoulder instability in patients older than 40 years. Am J Sports Med. 2019;47:3057–3064. doi: 10.1177/0363546519872501. [DOI] [PubMed] [Google Scholar]
- 3.Hardy A., Sabatier V., Laboudie P., et al. Outcomes after Latarjet procedure: Patients with first-time versus recurrent dislocations. Am J Sports Med. 2020;48:21–26. doi: 10.1177/0363546519879929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Giles J.W., Boons H.W., Elkinson I., et al. Does the dynamic sling effect of the Latarjet procedure improve shoulder stability? A biomechanical evaluation. J Shoulder Elbow Surg. 2013;22:821–827. doi: 10.1016/j.jse.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 5.Munn Z., Peters M.D.J., Stern C., Tufanaru C., McArthur A., Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:1–8. doi: 10.1186/s12874-018-0611-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tricco A.C., Lillie E., Zarin W., et al. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169:467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 7.Kibler W Ben, Sciascia A. The role of the scapula in preventing and treating shoulder instability. Knee Surg Sports Traumatol Arthrosc. 2016;24:390–397. doi: 10.1007/s00167-015-3736-z. [DOI] [PubMed] [Google Scholar]
- 8.Cerciello S., Edwards T.B., Cerciello G., Walch G. Scapular position after the open Latarjet procedure: Results of a computed tomography scan study. J Shoulder Elbow Surg. 2015;24:199–202. doi: 10.1016/j.jse.2014.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Carbone S., Moroder P., Runer A., Resch H., Hertel R., Gumina S. Scapular dyskinesis after Latarjet or a modified Eden-Hybinette procedure. J Orthop Traumatol. 2014;15:S53. [Google Scholar]
- 10.Rothenberg A., Gasbarro G., Chlebeck J., Lin A. The coracoacromial ligament: Anatomy, function, and clinical significance. Orthop J Sport Med. 2017;5 doi: 10.1177/2325967117703398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pieper H.G., Radas C.B., Krahl H., Blank M. Anatomic variation of the coracoacromial ligament: A macroscopic and microscopic cadaveric study. J Shoulder Elbow Surg. 1997;6:291–296. doi: 10.1016/s1058-2746(97)90019-7. [DOI] [PubMed] [Google Scholar]
- 12.Degen R.M., Giles J.W., Boons H.W., Litchfield R.B., Johnson J.A., Athwal G.S. A biomechanical assessment of superior shoulder translation after reconstruction of anterior glenoid bone defects: The Latarjet procedure versus allograft reconstruction. Int J Shoulder Surg. 2013;7:7–13. doi: 10.4103/0973-6042.109879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Di Giacomo G., Scarso P., De Vita A., Rojas Beccaglia M.A., Pouliart N., de Gasperis N. Glenohumeral translation in ABER position during muscle activity in patients treated with Latarjet procedure: An in vivo MRI study. Knee Surg Sport Traumatol Arthrosc. 2016;24:521–525. doi: 10.1007/s00167-015-3896-x. [DOI] [PubMed] [Google Scholar]
- 14.Dos Santos R.B.M., Kauffman F.N., de Lima G.P., Ferreira A.M.C., Dos Santos S.M., de Andrade Aguiar J.L. Evaluation of isometric strength and fatty infiltration of the subscapularis in Latarjet surgery. Acta Ortop Bras. 2015;23:129–133. doi: 10.1590/1413-785220152303144944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wellmann M., de Ferrari H., Smith T., et al. Biomechanical investigation of the stabilization principle of the Latarjet procedure. Arch Orthop Trauma Surg. 2012;132:377–386. doi: 10.1007/s00402-011-1425-z. [DOI] [PubMed] [Google Scholar]
- 16.Elkousy H., Gartsman G.M., Labriola J., O’Connor D.P., Edwards T.B. Subscapularis function following the Latarjet coracoid transfer for recurrent anterior shoulder instability. Orthopedics. 2010;33:1–4. doi: 10.3928/01477447-20100924-08. [DOI] [PubMed] [Google Scholar]
- 17.Azizi S., Urbanschitz L., Bensler S., Lenz C.G., Borbas P., Eid K. Structural and functional results of subscapularis and conjoint tendon after Latarjet procedure at 8-year average follow-up. Am J Sports Med. 2022;50:321–326. doi: 10.1177/03635465211061599. [DOI] [PubMed] [Google Scholar]
- 18.Paladini P., Merolla G., De Santis E., Campi F., Porcellini G. Long-term subscapularis strength assessment after Bristow-Latarjet procedure: Isometric study. J Shoulder Elbow Surg. 2012;21:42–47. doi: 10.1016/j.jse.2011.03.027. [DOI] [PubMed] [Google Scholar]
- 19.Maynou C., Cassagnaud X., Mestdagh H. Function of subscapularis after surgical treatment for recurrent instability of the shoulder using a bone-block procedure. J Bone Joint Surg Br. 2005;87-B:1096–1101. doi: 10.1302/0301-620X.87B8.14605. [DOI] [PubMed] [Google Scholar]
- 20.Caubère A., Lami D., Boileau P., Parratte S., Ollivier M., Argenson J.N. Is the subscapularis normal after the open Latarjet procedure? An isokinetic and magnetic resonance imaging evaluation. J Shoulder Elbow Surg. 2017;26:1775–1781. doi: 10.1016/j.jse.2017.03.034. [DOI] [PubMed] [Google Scholar]
- 21.Scheibel M., Nikulka C., Dick A., Schroeder R.J., Popp A.G., Haas N.P. Structural integrity and clinical function of the subscapularis musculotendinous unit after arthroscopic and open shoulder stabilization. Am J Sport Med. 2007;35:1153–1161. doi: 10.1177/0363546507299446. [DOI] [PubMed] [Google Scholar]
- 22.Ersen A., Birisik F., Ozben H., et al. Latarjet procedure using subscapularis split approach offers better rotational endurance than partial tenotomy for anterior shoulder instability. Knee Surg Sport Traumatol Arthrosc. 2018;26:88–93. doi: 10.1007/s00167-017-4480-3. [DOI] [PubMed] [Google Scholar]
- 23.Ernstbrunner L., Waltenspül M., Suter C., El-Nashar R., Scherr J., Wieser K. Primary open Latarjet procedure results in functional differences but no structural changes in subscapularis muscle quality vs the healthy contralateral shoulder at long-term follow-up. Am J Sports Med. 2022;50:1495–1502. doi: 10.1177/03635465221079858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walch G., Boileau P. Latarjet-Bristow procedure for recurrent anterior instability. Tech Shoulder Elb Surg. 2000;1:256–261. [Google Scholar]
- 25.Yamamoto N., Muraki T., An K.N., et al. The stabilizing mechanism of the Latarjet procedure: A cadaveric study. J Bone Joint Surg Am. 2013;95:1390–1397. doi: 10.2106/JBJS.L.00777. [DOI] [PubMed] [Google Scholar]
- 26.Kleiner M.T., Payne W.B., McGarry M.H., Tibone J.E., Lee T.Q. Biomechanical comparison of the Latarjet procedure with and without capsular repair. Clin Orthop Surg. 2016;8:84–91. doi: 10.4055/cios.2016.8.1.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Abdulian M.H., Kephart C.J., McGarry M.H., Tibone J.E., Lee T.Q. Biomechanical comparison of the modified Bristow procedure with and without capsular repair. Knee Surg Sport Traumatol Arthrosc. 2016;24:489–495. doi: 10.1007/s00167-015-3915-y. [DOI] [PubMed] [Google Scholar]
- 28.Itoigawa Y., Hooke A.W., Sperling J.W., et al. Repairing the capsule to the transferred coracoid preserves external rotation in the modified Latarjet procedure. J Bone Joint Surg Am. 2016;98:1484–1489. doi: 10.2106/JBJS.15.01069. [DOI] [PubMed] [Google Scholar]
- 29.Sahu D. Capsular repair is not an important part of the Latarjet-Walch procedure. J Shoulder Elbow Surg. 2022;31:948–956. doi: 10.1016/j.jse.2021.10.030. [DOI] [PubMed] [Google Scholar]
- 30.Lacheta L., Rupp M.C., Achtnich A., et al. Biceps brachii alterations following the Latarjet procedure: A prospective multicenter study. J Clin Med. 2021;10:5487. doi: 10.3390/jcm10235487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malavolta E.A., Cruz D.G., Gracitelli M.E.C., et al. Isokinetic evaluation of the shoulder and elbow after Latarjet procedure. Orthop Traumatol Surg Res. 2020;106:1079–1082. doi: 10.1016/j.otsr.2020.04.012. [DOI] [PubMed] [Google Scholar]
- 32.Castoldi F., Rossi R., Lollino N., Renzulli F., Berrino E., Rossi P. Coracoid transfer in Bristow-Latarjet procedure: Does it modify the biceps muscle? Knee Surg Sport Traumatol Arthrosc. 2008;16:81–85. doi: 10.1007/s00167-007-0436-3. [DOI] [PubMed] [Google Scholar]
- 33.Griesser M.J., Harris J.D., McCoy B.W., et al. Complications and re-operations after Bristow-Latarjet shoulder stabilization: A systematic review. J Shoulder Elbow Surg. 2013;22:286–292. doi: 10.1016/j.jse.2012.09.009. [DOI] [PubMed] [Google Scholar]
- 34.Clavert P., Lutz J.C., Wolfram-Gabel R., Kempf J.F., Kahn J.L. Relationships of the musculocutaneous nerve and the coracobrachialis during coracoid abutment procedure (Latarjet procedure) Surg Radiol Anat. 2009;31:49–53. doi: 10.1007/s00276-008-0426-2. [DOI] [PubMed] [Google Scholar]
- 35.Freehill M.T., Srikumaran U., Archer K.R., McFarland E.G., Petersen S.A. The Latarjet coracoid process transfer procedure: Alterations in the neurovascular structures. J Shoulder Elbow Surg. 2013;22:695–700. doi: 10.1016/j.jse.2012.06.003. [DOI] [PubMed] [Google Scholar]
- 36.Lópiz Y., Checa P., García-Fernández C., Martín Albarrán S., López de Ramón R., Marco F. Complications after open Latarjet procedure: Influence of arm positioning on musculocutaneous and axillary nerve function. Eur J Orthop Surg Traumatol. 2022;32:243–248. doi: 10.1007/s00590-021-02960-y. [DOI] [PubMed] [Google Scholar]
- 37.Beckers J., Van Isacker T., Berghs B. Coracoid process transfer for anterior shoulder instability : A pectoralis minor sparing method. Acta Orthop Belg. 2020;86:497–501. [PubMed] [Google Scholar]
- 38.McClure P., Tate A.R., Kareha S., Irwin D., Zlupko E. A clinical method for identifying scapular dyskinesis, part 1: Reliability. J Athl Train. 2009;44:160–164. doi: 10.4085/1062-6050-44.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kibler W Ben, Uhl T.L., Maddux J.W.Q., Brooks P.V., Zeller B., McMullen J. Qualitative clinical evaluation of scapular dysfunction: A reliability study. J Shoulder Elbow Surg. 2002;11:550–556. doi: 10.1067/mse.2002.126766. [DOI] [PubMed] [Google Scholar]
- 40.Park J.Y., Hwang J.T., Kim K.M., Makkar D., Moon S.G., Han K.J. How to assess scapular dyskinesis precisely: 3-Dimensional wing computer tomography—A new diagnostic modality. J Shoulder Elbow Surg. 2013;22:1084–1091. doi: 10.1016/j.jse.2012.10.046. [DOI] [PubMed] [Google Scholar]
- 41.Voisin J.L., Ropars M., Thomazeau H. The human acromion viewed from an evolutionary perspective. Orthop Traumatol Surg Res. 2014;100(suppl):S355–S360. doi: 10.1016/j.otsr.2014.09.011. [DOI] [PubMed] [Google Scholar]
- 42.Lee T.Q., Black A.D., Tibone J.E., McMahon P.J. Release of the coracoacromial ligament can lead to glenohumeral laxity: A biomechanical study. J Shoulder Elbow Surg. 2001;10:68–72. doi: 10.1067/mse.2001.111138. [DOI] [PubMed] [Google Scholar]
- 43.Su W.R., Budoff J.E., Luo Z.P. The effect of coracoacromial ligament excision and acromioplasty on superior and anterosuperior glenohumeral stability. Arthroscopy. 2009;25:13–18. doi: 10.1016/j.arthro.2008.10.004. [DOI] [PubMed] [Google Scholar]
- 44.Hansen U., Levy O., Even T., Copeland S.A. Mechanical properties of regenerated coracoacromial ligament after subacromial decompression. J Shoulder Elbow Surg. 2004;13:51–56. doi: 10.1016/j.jse.2003.09.016. [DOI] [PubMed] [Google Scholar]
- 45.Chahla J., Marchetti D.C., Moatshe G., et al. Quantitative assessment of the coracoacromial and the coracoclavicular ligaments with 3-dimensional mapping of the coracoid process anatomy: A cadaveric study of surgically relevant structures. Arthroscopy. 2018;34:1403–1411. doi: 10.1016/j.arthro.2017.11.033. [DOI] [PubMed] [Google Scholar]
- 46.McGinley J.C., Agrawal S., Biswal S. Rotator cuff tears: Association with acromion angulation on MRI. Clin Imaging. 2012;36:791–796. doi: 10.1016/j.clinimag.2012.04.007. [DOI] [PubMed] [Google Scholar]
- 47.Gallino M., Battiston B., Annaratone G., Terragnoli F. Coracoacromial ligament: A comparative arthroscopic and anatomic study. Arthroscopy. 1995;11:564–567. doi: 10.1016/0749-8063(95)90133-7. [DOI] [PubMed] [Google Scholar]
- 48.Davey M.S., Davey M.G., Hurley E.T., Mullett H. Subscapularis management during open Latarjet procedure: Does subscapularis split versus tenotomy matter? A systematic review and meta-analysis. J Shoulder Elbow Surg. 2022;31:2169–2175. doi: 10.1016/j.jse.2022.03.008. [DOI] [PubMed] [Google Scholar]
- 49.Bouju Y., Gadéa F., Stanovici J., Moubarak H., Favard L. Shoulder stabilization by modified Latarjet-Patte procedure: Results at a minimum 10 years’ follow-up, and role in the prevention of osteoarthritis. Orthop Traumatol Surg Res. 2014;100:S213–S218. doi: 10.1016/j.otsr.2014.03.010. (suppl) [DOI] [PubMed] [Google Scholar]
- 50.Morrey B.F., Askew L.J., An K.N., Dobyns J.H. Rupture of the distal tendon of the biceps brachii. A biomechanical study. J Bone Joint Surg Am. 1985;67:418–421. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.