Abstract
Background
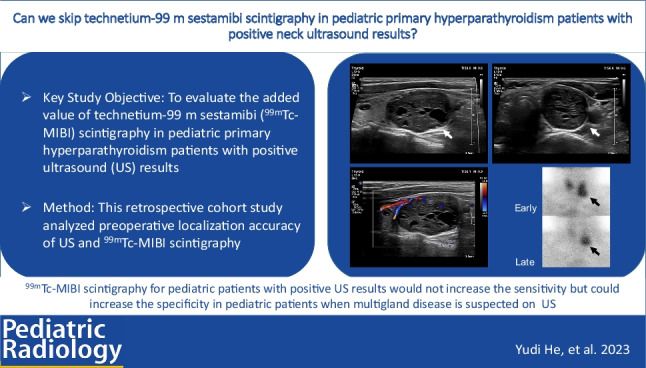
Parathyroidectomy is the only curative treatment for primary hyperparathyroidism (PHPT). Ultrasound (US) and technetium-99 m sestamibi (99mTc-MIBI) scintigraphy are recommended as the first-line localization imaging modalities for PHPT in adults, but the value of preoperative imaging in pediatric patients has not been reported.
Objective
To evaluate the added value of 99mTc-MIBI scintigraphy in pediatric PHPT patients with positive ultrasound results.
Materials and methods
Pediatric patients (≤18 years old) who were diagnosed with PHPT and underwent surgical treatment in Peking Union Medical College Hospital between January 2003 and January 2021 were included in this study. Demographic and clinical characteristics, preoperative localization US, 99mTc-MIBI scintigraphy and pathology results were collected. Preoperative localization results were evaluated by comparison with surgical and pathological findings.
Results
There were 32 pediatric PHPT patients with median age of 14.7 ± 2.5 years who all proved to have single-gland disease without ectopic lesions. The median lesion size was 2.85 cm (range 1.0–5.8 cm). All patients underwent US and 99mTc-MIBI scintigraphy. Neck US demonstrated 100% sensitivity. Of 32 patients with a positive US, 99mTc-MIBI scintigraphy was concordant in 30 (93.8%). In 2 patients (6.3%), US reported suspected multigland disease, which was correctly diagnosed by 99mTc-MIBI scintigraphy as single lesions.
Conclusion
In pediatric PHPT patients, US achieved high sensitivity for preoperative localization. 99mTc-MIBI scintigraphy for pediatric patients with positive US results would not increase the sensitivity. Implementation of 99mTc-MIBI scintigraphy could increase the specificity in pediatric patients with multigland disease suspected by US.
Graphical abstract
Keywords: Children, Primary hyperparathyroidism, Technetium-99 m sestamibi, Ultrasound
Introduction
Primary hyperparathyroidism (PHPT) is characterized by abnormal elevation of serum calcium and parathyroid hormone (PTH) levels due to pathological parathyroid glands and involves multiple organ systems, including the skeletal, urinary and digestive systems [1]. Pediatric PHPT is less common compared to adult PHPT (incidences of 2–5/100000 and 1/1000, respectively). However, the percentage of symptomatic pediatric patients is significantly higher and treatment delays could cause a number of complications, such as nephrolithiasis, osteoporosis and bone fracture and may affect the growth and development of children [2–5].
Parathyroidectomy is the only curative treatment for PHPT [6]. The operative approach includes minimally invasive parathyroidectomy/unilateral neck exploration, which is generally applied to unilateral gland disease with relatively precise localization and bilateral neck exploration, which is usually conducted in patients with bilateral multiple gland disease, obscure localization of lesions or hereditary etiologies [7]. Therefore, preoperative localization of lesions is one of the crucial factors in planning the surgical approach to minimize trauma and achieve operative success.
Widely accepted first-line localization imaging examinations include neck ultrasound (US) and technetium-99 m sestamibi (99mTc-MIBI) scintigraphy [6, 8–10]. The American College of Radiology Appropriateness Criteria in 2021 and the American Association of Endocrine Surgeons guidelines in 2016 recommend that the choice of imaging examination should be based on expert advice and regional imaging capabilities [6, 11]. Koewar et al. proposed a stepwise manner of imaging studies in which US could be performed routinely while 99mTc-MIBI scintigraphy would be performed when negative US, failed operation or recurrence occurred [12]. Another study used a hypothetical model to build a localization modality in 513 PHPT patients (mean age 58.5 ± 14.1 years) and demonstrated that the value of 99mTc-MIBI scintigraphy after positive US was limited, since added 99mTc-MIBI scintigraphy could only change the operative plan made by referring to US positive results in 2.3% of patients [13]. Children and adolescents are a more sensitive population to radiation exposure, but data are near nonexistent regarding the value of 99mTc-MIBI scintigraphy in pediatric PHPT patients with positive US results.
This study aims to evaluate the added value of 99mTc-MIBI scintigraphy in pediatric PHPT patients who have positive US results.
Materials and methods
This retrospective study was approved by the Institutional Review Board of Peking Union Medical College Hospital. From January 2003 to January 2021, pediatric patients (≤18 years old) who were diagnosed with PHPT according to serum calcium and PTH levels and underwent surgical treatment were enrolled [14]. All patients underwent cervical US and 99mTc-MIBI scintigraphy for the purpose of localization before surgery. The exclusion criterion was patients with incomplete information on preoperative images. Demographics, clinical history and radiology reports were obtained from the electronic medical records. Data collected included age, sex, preoperative PTH, preoperative calcium, US and 99mTc-MIBI scintigraphy imaging findings, pathology results and clinical follow-up.
Preoperative US was performed by Y.J. and H.L., both radiologists with at least 5 years of experience in parathyroid ultrasonography using one of two US machines (IU22 or Epiq; Philips, Amsterdam, The Netherlands) and a broadband linear array probe (L12–5 MHz). For each suspicious lesion identified, longitudinal and transverse views using grayscale and Doppler modes were obtained. The position of the lesions, lesion size, echo pattern and blood flow were recorded. The sonographic appearance of the adjacent thyroid gland was evaluated to provide a differential diagnosis between parathyroid gland lesions and nodular goiters.
Patients received intravenous injection of 99mTc-MIBI (Atom Hitech Co., Ltd, Beijing, China) at a dose of 10~20 mCi according to routine clinical practice. Planar images of the neck and upper chest were obtained 20 min and 120 min after administration with a gamma camera and a pinhole collimator. Images of single photon emission computed tomography/CT (SPECT/CT) were acquired after 120 min on a 64-slice Philips Precedence device (Philips, Amsterdam, The Netherlands). SPECT was performed in a 128 × 128 matrix with a zoom factor of 1.0 and 32 projections over 360°. CT was performed with a current of 30 mAs, voltage of 120 kV and slice thickness of 3 mm. Each examination was independently reviewed by 2 experienced radiologists (Y.P. and Q.P.), subspecialists in endocrine imaging with more than 5 years of experience each.
The accuracy of preoperative localization was evaluated using operative and histological findings as the reference standards. The cervical region was divided into quadrants with a vertical line drawn along the midline of the neck and a horizontal line through the middle thyroid. The preoperative location was classified as left superior, left inferior, right superior, right inferior or ectopic and compared to actual location identifed at surgery.
Parathyroidectomy was conducted within 2 weeks of preoperative localization. Operation procedures were obtained from medical records focusing on operation approach (unilateral or bilateral) and intraoperative findings (size and position of lesions). Operative cure was defined as a postoperative calcium level that remained normal during a follow-up period of at least 6 months [6]. Histological findings (according to the World Health Organization [WHO] classification standard) provided etiological information [15].
Statistical analysis was conducted using SPSS 25.0 software (IBM Inc, Armonk, NY). Categorical variables were described as frequencies and percentages. Continuous variables were described as the mean ± standard deviation (SD) or median value and range. Sensitivity was calculated to reveal the effectiveness of multiple preoperative localization methods. A P-value of <0.05 was considered statistically significant.
Results
Demographic and clinical characteristics
Demographic and clinical characteristics are summarized in Table 1. A total of 32 PHPT patients who underwent surgical treatment with a median age of 14.7 ± 2.5 years old (range 9–18 years old) were included. Of 32 patients, 14 (43.8%) were female. Preoperative PTH and calcium levels were 926.60 ± 864.95 pg/ml and 3.03 ± 0.39 mmol/l, respectively. The median lesion size was 2.85 cm (range 1.00–5.80 cm). All 32 patients (100%) had single-gland disease. Of the 32 children in our series, 5 (15.6%) were also diagnosed with multiple endocrine neoplasia type 1 (MEN1). Most lesions (21/32, 65.6%) were parathyroid adenoma, followed by atypical adenoma (5/32, 15.6%) and hyperplasia (6/32, 18.8%). No ectopic lesions were reported. All patients achieved operative success and the curative rate was 100%. Of the five MEN1 patients, three had recurrent lesions during 1–7 years of follow-up after the initial parathyroidectomy.
Table 1.
Demographic and clinical characteristics of pediatric primary hyperparathyroidism patients
| Value (n=32) | |
|---|---|
| Age, years (mean ± SD) | 14.7 ± 2.5 |
| Sex | |
| Female | 14 (43.8%) |
| Male | 18 (56.2%) |
|
Preoperative PTH, pg/ml (mean ± SD) (12.0–68.0) |
926.60 ± 864.95 |
|
Preoperative Ca, mmol/l (mean ± SD) (2.13–2.70) |
3.03 ± 0.39 |
| Subtype | |
| Sporadic | 27 (84.4%) |
| MEN1 | 5 (15.6%) |
| Operative findings | |
| Left sided, superior | 8 (25.0%) |
| Left sided, inferior | 10 (31.3%) |
| Right sided, superior | 4 (12.5%) |
| Right sided, inferior | 10 (31.3%) |
| Ectopic | 0 (0%) |
| Lesion size, cm (median, range) | 2.85 (1.00, 5.80) |
| >2 cm | 24 (75.0%) |
| Histological findings | |
| Adenoma | 21 (65.6%) |
| Atypical adenoma | 5 (15.6%) |
| Hyperplasia | 6 (18.8%) |
Ca calcium, MEN1 multiple endocrine neoplasia type 1, PTH parathyroid hormone
Preoperative localization
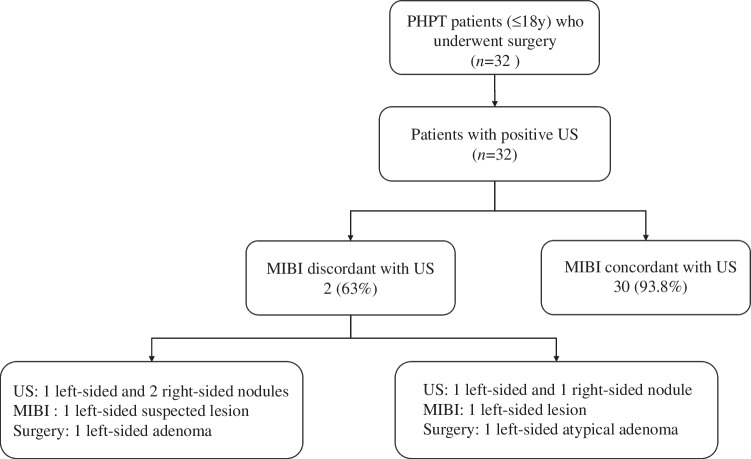
A positive US was defined as patients with US findings suggestive of parathyroid lesions or indeterminate nodules. Of 32 patients who underwent US and 99mTc-MIBI scintigraphy, all had a positive US result, 30 patients (93.8%) had consistent findings on US and 99mTc-MIBI scintigraphy and 2 (6.3%) had discordant preoperative localization (Fig. 1).
Fig. 1.
Preoperative localization in pediatric primary hyperparathyroidism patients. MIBI technetium-99 m sestamibi scintigraphy, PHPT primary hyperparathyroidism, US ultrasound
In 30 patients with concordant imaging results, surgical findings confirmed a single-gland lesion. The most frequent histological type was adenoma, which occurred in 20 patients (66.7%), followed by hyperplasia in 6 (20%) and atypical adenoma in 4 (13.3%). Of the 2 patients with discordant localization results, case 1 was sporadic PHPT with a single left-sided adenoma. Neck US identified one left-sided nodule (maximum diameter 2.8 cm) and two right-sided nodules (maximum diameter 1.3 cm and 2.3 cm respectively). 99mTc-MIBI scintigraphy indicated a suspected gland on the left side. Bilateral neck exploration was conducted and proved that two right-sided nodules found by US were thyroid nodular goiter. Case 2 was diagnosed as multiple endocrine neoplasia (MEN)1 with an atypical left-sided adenoma. Neck US revealed one left-sided nodule (maximum diameter 2.9 cm) and one right-sided nodule (maximum diameter 2.1 cm). 99mTc-MIBI scintigraphy revealed one left-sided abnormal gland. The patient underwent bilateral neck exploration and single-gland resection on the left side. No other parathyroid gland lesions were found. In summary, the sensitivity of US localization was 100% and the accuracy was 93.8%.
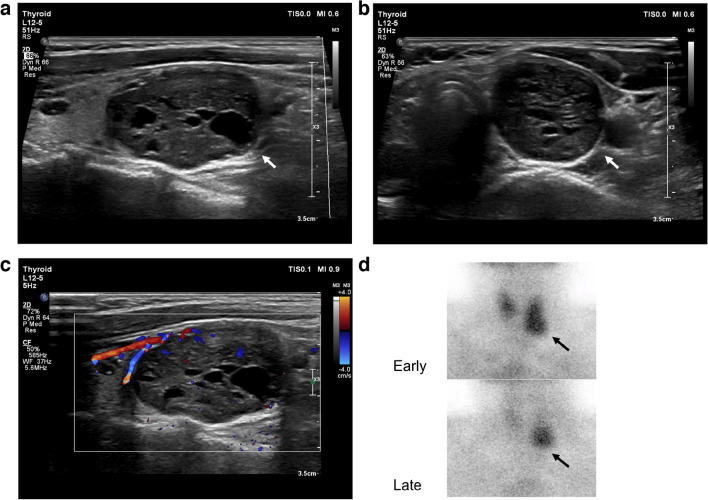
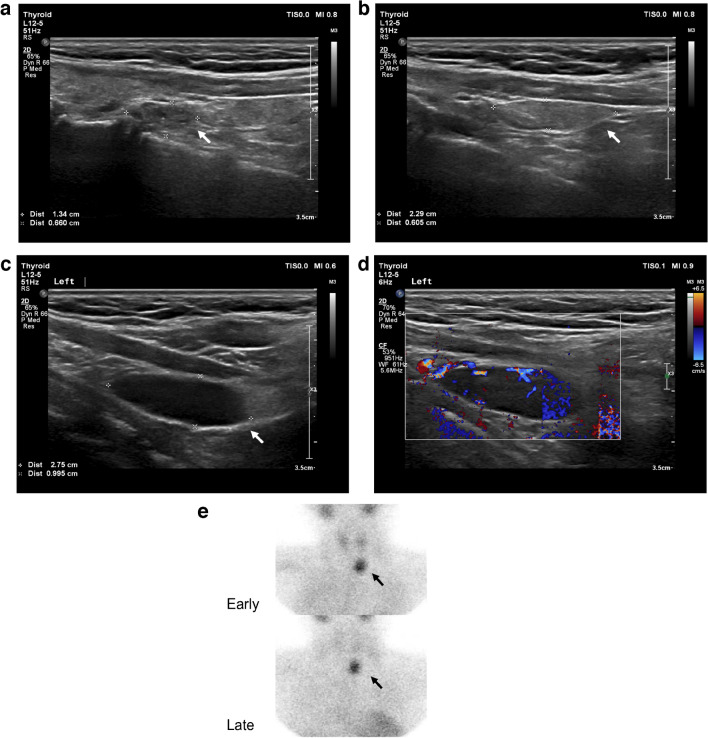
Across the 32 patients, US reported 35 nodules. Among the true positive lesions, 32 (100%) were hypoechoic with oval shapes, circumscribed margins and internal blood flow on color Doppler mode. Cystic changes were found in 4 nodules (12.5%) and a hyperechoic focus was found in 1 nodule (3.1%). Neck US and 99mTc-MIBI scintigraphy images of a parathyroid gland adenoma with concordant localization are shown in Fig. 2. Another case with discordant localization results on US and 99mTc-MIBI scintigraphy is shown in Fig. 3.
Fig. 2.
A parathyroid gland adenoma in an 18-year-old girl. a, b Longitudinal (a) and transverse (b) ultrasound images show a nodule (arrows) with cystic components below the inferior pole of the left lobe of the thyroid gland. c Longitudinal Doppler image shows a peripheral feeding vessel with an arc of vascularity and internal blood flow. d Technetium-99 m sestamibi scintigraphy shows a focus of intense accumulation at the level of the inferior pole of the left lobe of the thyroid (arrows)
Fig. 3.
A case of discordant localization between ultrasound (US) and technetium-99 m sestamibi (99mTc-MIBI) scintigraphy in a 13-year-old boy. a, b Longitudinal US images show two indeterminate nodules (arrows) on the right side of the neck without feeding vessels on Doppler mode (images not shown). Histology confirmed a nodular goiter. c, d Longitudinal US images suggestive of a parathyroid lesion on the left side of the neck. The grayscale image (c) shows a hypoechoic oval-shaped nodule with a well-circumscribed margin (arrow). The color Doppler flow image (d) illustrates a feeding vessel and internal blood flow. Histology confirmed a parathyroid adenoma. e 99mTc-MIBI scintigraphy shows a focus of intense accumulation at the level of the inferior pole of the left lobe of the thyroid (arrows)
Discussion
PHPT is less prevalent but more severe in pediatric patients than in adults and parathyroidectomy is the only curative therapy. Preoperative localization plays a crucial role in achieving operative success. First-line imaging localization modalities include US and 99mTc-MIBI scintigraphy which have a comparable diagnosed efficacy in adults [8]. A recent study revealed that adding 99mTc-MIBI scintigraphy after positive US results might have limited value since 99mTc-MIBI scintigraphy can only correct the operative plan in 2.3% of patients and the proportion is 0.35% when the lesion size is over 1.2 cm [13]. Ebner et al. revealed a similar operative success in three groups with only US, only 99mTc-MIBI scintigraphy, or US-99mTc-MIBI scintigraphy matched positive results, indicating that one type of imaging examination with positive results might be adequate for preoperative localization [16]. Children and adolescents are a special population and should be exposed to as little radiation exposure as possible. There are limited studies in PHPT imaging analysis focusing on the pediatric population, lacking the evidence to elaborate on the value of a second imaging examination after obtaining a positive US result for children and adolescents. Our study shows that preoperative US localization had a high sensitivity (100%) and accuracy (93.8%) in this pediatric cohort while 99mTc-MIBI scintigraphy only corrected localization in 6.3% patients after positive US results, which is similar to what is already known.
In our study, parathyroid lesions were solitary, large in size and had eutopic localization.
Lesion size can be a contributing factor to imaging localization efficacy. With increases in lesion size, the sensitivity of imaging examinations also increases [17]. Yalon et al. confirmed that the proportion of patients with positive US who received correction by 99mTc-MIBI scintigraphy decreased to 0.35% (1/287) when the lesion size was over 1.2 cm, compared to 2.3% (12/513) in the whole cohort [13]. For the pediatric population, lesion size or weight was quite different among multiple cohorts. The reported mean lesion weight varys from less than 0.4 g to more than 5 g [18–20]. In our group, the median lesion maximum diameter of parathyroid gland lesions was 2.85 cm (range 1.0–5.8 cm) and 75% were over 2 cm. This could help explain the outstanding performance of US.
Multigland disease is one of the most difficult situations for preoperative localization imaging. It is widely accepted that there is an association between multigland disease and MEN1 in the pediatric population. MEN1 patients may have have a higher incidence of multigland disease [3, 21]. In our study, 5 (15.6%) patients were diagnosed with MEN1 and no multigland disease was found, nevertheless 3 in 5 MEN1 patients had recurrent lesions after a follow-up of 1–7 years. To our knowledge, sufficient evidence that the combination of US and 99mTc-MIBI scintigraphy could increase the sensitivity and specificity compared to single US in an underage population with multigland disease is lacking and further study might be needed.
Ectopic glands are another challenge for localization [10]. The proportion of ectopic adenomas in adult patients is 6–16% [22]. In two studies with 52 (<19 years old) and 86 (<22 years old) patients, ectopic lesions accounted for 9.6% and 25%, respectively [22, 23]. In our group, no ectopic location was reported according to surgical findings. Thus, a larger cohort might be needed for further study.
The above features of our cohort might explain the excellent performance of US. It would be interesting to include PHPT patients with negative US and further discuss the performance of 99mTc-MIBI scintigraphy in such patients in future studies.
There are several limitations of this study. First, the PHPT patients were enrolled from a national tertiary care referral center; thus, they represented more severe conditions which might lead to selection bias. Second, since this is a retrospective study, it was difficult for radiologists to be completely blinded to other imaging examinations before reaching a diagnosis. A future prospective study is warranted. Third, although our cohort is one of the largest pediatric PHPT cohorts focusing on imaging analysis, we only enrolled 32 patients. Sampling error might be the possible reason why this study has a higher percentage in which MIBI would dictate the surgical approach compared to an adult PHPT cohort [13].
Conclusion
In our cohort, parathyroid lesions of pediatric PHPT patients were solitary, large in size and had eutopic localization. Neck US has high sensitivity for identifying abnormal glands and is useful for preoperative localization, while adding 99mTc-MIBI scintigraphy for those with positive US results would not improve the sensitivity. Implementation of 99mTc-MIBI scintigraphy might increase the specificity in pediatric patients with suspected multigland disease as shown on US.
Acknowledgements
The authors thank the Department of Nuclear Medicine of Peking Union Medical College Hospital for their suggestions in interpretations of 99mTc-MIBI scintigraphy results and providing the 99mTc-MIBI scintigraphy figures.
Author contribution
Q.Z. and H.L. designed and supervised the study. Y.H. and Y.L. collected the data. Y.H. and S.J. completed data analysis. O.W. and Q.L. took part in data interpretation. Y.H. wrote the manuscript. Q.Z. and H.L. revised the manuscript and provided final approval. All authors contributed to the article and approved the submission of the final manuscript.
Funding
This work was supported by National High Level Hospital Clinical Research Funding (2022-PUMCH-B-066).
Data availability
The data generated during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Written informed consent was signed by legally authorized representatives of the patients. The Institutional Review Board of Peking Union Medical College Hospital (PUMCH) has reviewed the protocol of this manuscript and has determined that this study is exempt from full IRB review since it is a retrospective study.
Conflicts of interest
None
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Qingli Zhu and He Liu contributed equally to this work.
Contributor Information
Qingli Zhu, Email: zqlpumch@126.com.
He Liu, Email: liuhebj@126.com.
References
- 1.Walker MD, Silverberg SJ. Primary hyperparathyroidism. Nat Rev Endocrinol. 2018;14:115–125. doi: 10.1038/nrendo.2017.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McKenna K, Dunbar NS, Parham K (2021) Why is primary hyperparathyroidism more severe in children? Med Hypotheses 147:110482 [DOI] [PubMed]
- 3.Lo HB, Tebben PJ. Primary hyperparathyroidism in children and adolescents. Hyperparathyroidism A Clin Caseb. 2016;75:117–128. doi: 10.1007/978-3-319-25880-5_14. [DOI] [Google Scholar]
- 4.Jovanovic M, Paunovic I, Zdravkovic V et al (2020) Case-control study of primary hyperparathyroidism in juvenile vs. adult patients. Int J Pediatr Otorhinolaryngol 131:109895 [DOI] [PubMed]
- 5.Zivaljevic V, Jovanovic M, Diklic A, et al. Differences in primary hyperparathyroidism characteristics between children and adolescents. J Pediatr Surg. 2020;55:1660–1662. doi: 10.1016/j.jpedsurg.2019.09.023. [DOI] [PubMed] [Google Scholar]
- 6.Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. 2016;151:959–968. doi: 10.1001/jamasurg.2016.2310. [DOI] [PubMed] [Google Scholar]
- 7.Alagaratnam S, Brain C, Spoudeas H, et al. Surgical treatment of children with hyperparathyroidism: single centre experience. J Pediatr Surg. 2014;49:1539–1543. doi: 10.1016/j.jpedsurg.2014.05.032. [DOI] [PubMed] [Google Scholar]
- 8.Moghadam RN, Amlelshahbaz AP, Namiranian N et al (2017) Comparative diagnostic performance of ultrasonography and 99mTc-Sestamibi scintigraphy for parathyroid adenoma in primary hyperparathyroidism; systematic review and meta-analysis. Asian Pacific J Cancer Prev 18:3195–3200 [DOI] [PMC free article] [PubMed]
- 9.Khalatbari H, Cheeney SHE, Manning SC, Parisi MT. Pediatric hyperparathyroidism: review and imaging update. Pediatr Radiol. 2021;51:1106–1120. doi: 10.1007/s00247-021-05050-7. [DOI] [PubMed] [Google Scholar]
- 10.Kuzminski SJ, Sosa JA, Hoang JK. Update in parathyroid imaging. Magn Reson Imaging Clin N Am. 2018;26:151–166. doi: 10.1016/j.mric.2017.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Zander D, Bunch PM, Policeni B, et al. ACR Appropriateness Criteria® parathyroid adenoma. J Am Coll Radiol. 2021;18:S406–S422. doi: 10.1016/j.jacr.2021.08.013. [DOI] [PubMed] [Google Scholar]
- 12.Korwar V, Yuen Chang F, Teasdale E, et al. Stepwise approach for parathyroid localisation in primary hyperparathyroidism. World J Surg. 2020;44:803–809. doi: 10.1007/s00268-019-05269-4. [DOI] [PubMed] [Google Scholar]
- 13.Yalon T, Neymark M, Rottenberg A, et al. The added value of technetium-99 m sestamibi scan in patients with primary hyperparathyroidism and positive ultrasound. World J Surg. 2021;45:2148. doi: 10.1007/s00268-021-06066-8. [DOI] [PubMed] [Google Scholar]
- 14.Bandeira F, Griz L, Chaves N, et al. Diagnosis and management of primary hyperparathyroidism: a scientific statement from the Department of Bone Metabolism, the Brazilian Society for Endocrinology and Metabolism. Arq Bras Endocrinol Metabol. 2013;57:406–424. doi: 10.1590/S0004-27302013000600002. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd RV, Osamura RY, Klöppel G et al (2017) WHO classification of tumours of endocrine organs 4th, edn. International Agency for Research of Cancer, Lyon
- 16.Ebner Y, Garti-Gross Y, Margulis A, et al. Parathyroid surgery: correlation between pre-operative localization studies and surgical outcomes. Clin Endocrinol (Oxf) 2015;83:733–738. doi: 10.1111/cen.12835. [DOI] [PubMed] [Google Scholar]
- 17.Abd Elhameed Elsayed W, Ali RA (2019) Efficacy of scintigraphy, ultrasound and both scintigraphy and ultrasonography in preoperative detection and localization of primary hyperparathyroidism. Cureus 11(6):e4960 [DOI] [PMC free article] [PubMed]
- 18.Mancilla EE, Levine MA, Adzick NS. Outcomes of minimally invasive parathyroidectomy in pediatric patients with primary hyperparathyroidism owing to parathyroid adenoma: a single institution experience. J Pediatr Surg. 2017;52:188–191. doi: 10.1016/j.jpedsurg.2016.01.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bhadada SK, Bhansali A, Dutta P, et al. Characteristics of primary hyperparathyroidism in adolescents. J Pediatr Endocrinol Metab. 2008;21:1147–1153. doi: 10.1515/JPEM.2008.21.12.1147. [DOI] [PubMed] [Google Scholar]
- 20.Paunovic I, Zivaljevic V, Stojanic R, et al. Primary hyperparathyroidism in children and young adults:–a single institution experience. Acta Chir Belg. 2013;113:35–39. doi: 10.1080/00015458.2013.11680882. [DOI] [PubMed] [Google Scholar]
- 21.Saponaro F, Marcocci C, Cacciatore F, et al. Clinical profile of juvenile primary hyperparathyroidism: a prospective study. Endocrine. 2018;59:344–352. doi: 10.1007/s12020-017-1318-1. [DOI] [PubMed] [Google Scholar]
- 22.Rampp RD, Mancilla EE, Adzick NS, et al. Single gland, ectopic location: adenomas are common causes of primary hyperparathyroidism in children and adolescents. World J Surg. 2020;44:1518–1525. doi: 10.1007/s00268-019-05362-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kollars J, Zarroug AE, van Heerden J, et al. Primary hyperparathyroidism in pediatric patients. Pediatrics. 2005;115:974–980. doi: 10.1542/peds.2004-0804. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data generated during the current study are available from the corresponding author on reasonable request.