Abstract
Objective
Internet-based cognitive behavior therapy (ICBT) may provide an accessible alternative to face-to-face treatment, but the evidence base in adolescents is limited. This systematic review and meta-analysis aims to comprehensively assess the efficacy of ICBT in addressing depression among adolescents.
Methods
Four electronic databases were searched on June 8, 2023. Randomized controlled trials (RCTs) evaluating the efficacy of ICBT for depression in adolescents were included. The quality of the studies was assessed using the risk of bias tool recommended by the Cochrane Handbook. Furthermore, the GRADE approach was employed to gauge the certainty of the obtained evidence. Meta-analysis was conducted using RevMan 5.4, and Egger's test was implemented through Stata for assessment of potential publication bias.
Results
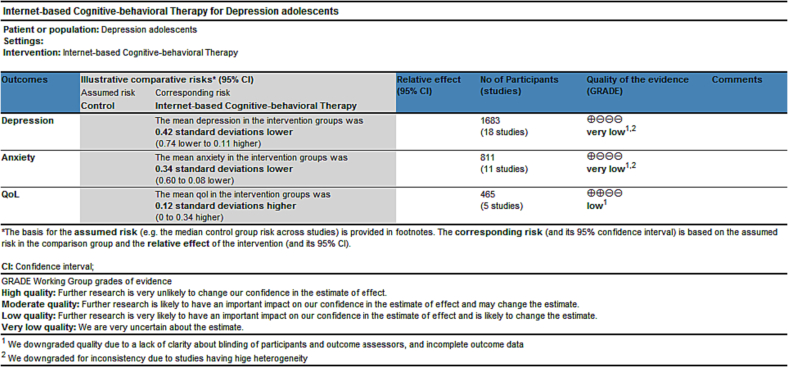
A total of 18 RCTs involving 1683 patients were included. In comparison to control groups like attention control, waiting list, and treatment as usual, our meta-analysis findings elucidate a significant reduction in depression scores (SMD = −0.42, 95 % CI: [−0.74, −0.11], p < .05) as well as anxiety scores (SMD = −0.34, 95 % CI: [−0.60, −0.08], p < .05) in adolescents following ICBT interventions. Furthermore, the analysis indicated no notable distinctions in patient's quality of life (QoL) scores. (SMD = 0.12, 95 % CI: [−0.10, 0.34], p > .05).
Conclusion
Results provide evidence of the efficacy of ICBT to reduce depressive and anxiety symptoms in adolescents. These research findings are of vital significance for the establishment of evidence-based treatment guidelines in the digital era.
Trial registration
PROSPERO registration: CRD42021277562.
Keywords: Cognitive behavioral therapy, Internet, Depression, Adolescents, Meta-analysis
Highlights
-
•
Adolescents are at high risk of depression.
-
•
This study systematically evaluated the efficacy of ICBT in improving depressive symptoms in adolescents.
-
•
ICBT significantly improved depressive symptoms in adolescents compared to the control group.
-
•
A total of 18 RCTs involving 1683 patients were included.
Depression is a profound affective mental disorder primarily characterized by persistent and prolonged feelings of low mood, and anhedonia (Gotlib and Joormann, 2010). Given the inherent instability in psychological development, depressive symptoms often manifest in adolescents (Prieto et al., 2005). By the age of 19, it is estimated that one in five to a quarter of young individuals experience depression (Rohde et al., 2013). The World Health Organization (WHO) reports that depression stands as a leading cause of morbidity and disability among adolescents (Dick and Ferguson, 2015). Moreover, depression during adolescence is linked to adverse outcomes that might extend into adulthood, including suicidal tendencies, susceptibility to mental health disorders, substance misuse, diminished educational attainment, and impaired social functioning (Wickersham et al., 2021a; Wickersham et al., 2021b; Woodward and Fergusson, 2001). Cognitive behavioral therapy (CBT) is widely recognized as the preeminent psychological intervention for addressing adolescent depression (Creswell et al., 2014). Numerous studies have underscored CBT's acceptance and efficacy as an intervention for depressive symptoms in adolescents. A 2019 meta-analysis by Oud et al. demonstrated CBT's effectiveness for youth with depression (Oud et al., 2019). Similarly, a review conducted by Reddy et al. highlighted the robust impact of CBT on depressive symptoms among adolescents (Reddy et al., 2023). Despite these effective interventions, most adolescents with mental health needs do not receive adequate treatment (Essau, 2005; Mojtabai et al., 2016; Merikangas et al., 2011). This discrepancy can be attributed to limited mental health services, the stigma surrounding mental illness, and a preference for self-help strategies (Gulliver et al., 2010; O'Brien et al., 2016). Consequently, there is an urgent imperative to develop interventions that combine efficacy with ease of implementation.
Internet-based cognitive behavioral therapy (ICBT) was developed through a combination of information technology and psychotherapy (Andersson, 2009). ICBT typically offers treatment content similar to conventional face-to-face CBT, except that ICBT relies on a digital platform to deliver treatment. Moreover, ICBT is available in various delivery formats, including blended, guided, and unguided. It often follows a modular format, encompassing interactive audio, video materials, interactive games, and assignments. Participants access these treatment modules consistently within specified timeframes (Poppelaars et al., 2016). ICBT can be self-directed or therapist-directed. Guidance can refer to any form of support from a coach or therapist, such as automated reminders, asynchronous email communications, brief scheduled phone calls, or live chats (Andersson, 2016; Barak et al., 2009). It can overcome the limitations of some traditional therapies. Compared with face-to-face treatment, ICBT offers more flexibility in terms of time and location; greater privacy; effective cost savings; and more independence (MacDonell and Prinz, 2017; Lin et al., 2013; Calear and Christensen, 2010). Young people are very proficient with the internet and show a positive attitude toward computerized mental health interventions (Sweeney et al., 2019). Therefore, ICBT may be an effective alternative to the original face-to-face treatment (Hollis et al., 2017). Internet interventions for depression are currently being developed that can be used to treat and prevent depression. Our study focuses on the efficacy of Internet-based cognitive behavioral therapy for the treatment of depression in adolescents.
Numerous RCTs and meta-analyses have shown that ICBT can be effectively implemented in adults with anxiety and depression (Karyotaki et al., 2017; Andrews et al., 2018). In recent years, there have also been studies dedicated to exploring the effects of ICBT on depressive symptoms in adolescents. However, compared with adults, research evidence based on ICBT among adolescents is very limited. And these reviews are usually insensitive to age effects, making it difficult to determine whether ICBT is equally effective in children, adolescents, and young adults (Calear and Christensen, 2010; Ebert et al., 2015; Richardson et al., 2010; Vigerland et al., 2016). Hollis et al. (2017) carried out an overview of a systematic review in 2016, aiming to explore the effectiveness of digital health interventions for addressing mental health concerns among children and young individuals. Within their study, they incorporated 21 pertinent meta-analyses and 30 randomized controlled trials (RCTs), with only one of these included studies offering evidence concerning Internet-Based Cognitive Behavioral Therapy (ICBT) as a treatment option for depression in adolescents aged 10 to 19 years. Ebert et al. (2015) stratified the meta-analysis by age group and found that studies that tested ICBT in adolescents achieved better results than studies that targeted children or mixed-age groups. And they looked at studies published six years ago and very few studies with adolescents. In 2016, Vigerland et al. conducted a study (Vigerland et al., 2016) that examined the effects of Internet-delivered cognitive behavioral therapy on children and adolescents aged 0 to 18 years, without imposing limitations on the specific type of illness. Lehtimaki et al.'s Overviews of systematic review (Lehtimaki et al., 2021) uncovered evidence supporting the effectiveness of computerized cognitive behavioral therapy for managing anxiety and depression in adolescents and young adults (0–24 years). Notably, the meta-analyses by Christ et al. (2020) and Wickersham et al. (2022) delved into the efficacy of Computer-Based CBT for adolescents with depression; however, the original studies focused on depressed adolescents were relatively scarce. In recent years, digital health has changed considerably. The prominence of mHealth (mobile health) and the integration of artificial intelligence and machine learning have emerged as essential methodologies within the realm of digital health. In particular, mHealth has shown great potential in the field of psychology (Fatehi et al., 2020; Hollis et al., 2017), (Nicol et al., 2022). Therefore, in contrast to previous studies, (Christ et al., 2020; Wickersham et al., 2022) we focused the intervention on ICBT rather than computer-based cognitive behavioral therapy.
Depression and anxiety are frequently observed in children and adolescents, often manifesting concurrently, with a strong correlation between the two (Brady and Kendall, 1992). Furthermore, multiple studies have underscored the adverse influence of depression on the QoL (Fernandes et al., 2023; Gazibara et al., 2018; Christ et al., 2020). The objective of the present study is to conduct an up-to-date comprehensive systematic review and meta-analysis to evaluate the efficacy of ICBT on the depression of adolescents. We are also planning to undertake a meta-analysis to assess the impact of ICBT on anxiety and quality of life among adolescents. Additionally, our objective involves investigating potential associations between treatment outcomes and factors such as passive control versus positive control groups, as well as short-term follow-up versus long-term follow-up. This will be achieved through conducting subgroup analyses.
1. Methods
1.1. Eligibility criteria
We used the P.I.C.O.S. (Population, Interventions, Comparators, Outcomes, and Study Design) framework to identify relevant studies.
1.1.1. Types of participants
Studies that met the following criteria were included: Adolescents (10–19 years old) (Dick and Ferguson, 2015) with depressive symptoms, with or without anxiety symptoms, have no risk of suicide, have no cognitive impairment or any other mental illness. Depressive symptom Judgment Criteria: Diagnosed by physicians or other qualified mental health professionals according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV), the international Classification of diseases(ICD-10), or undiagnosed but assessed as having at least mild depressive symptoms by validated depression scales, such as Children's Depression Rating Scale-Revised (CDRS-R), The Center for Epidemiologic Studies Depression Scale Revised (CESD-R), Beck Depression Inventory (BDI), Beck Depression Inventory-II (BDI-II), Reynolds Adolescent Depression Scale-2(RADS-2), Montgomery-Asberg Depression Rating Scale (MADRS-S), Mood and Feelings Questionnaire (MFQ), Quick Inventory of Depressive Symptomatology for Adolescents (QIDS-A17-SR), and Patient Health Questionnaire-9 (PHQ-9).
1.1.2. Types of studies
In this study, we included only randomized controlled trials (RCTs) that evaluated ICBT as treatment for adolescents with depression symptoms. Studies that did not clearly state study population characteristics, studies for which the full text was not available, and studies with incomplete data reporting were excluded.
1.1.3. Types of interventions
We defined ICBT as intervention via computer or online and using specific CBT-based components. ICBT is delivered over the internet through websites or web applications. Users access therapy materials and tools through web browsers on their computers, tablets, or smartphones. Computerized cognitive behavioral therapy (cCBT) is usually installed and run on the user's computer, which we also included in this study. There were no limitations on the duration and frequency of interventions. Types of comparisons: treatment as usual, waiting list and attention control.
1.1.4. Types of outcome measures
The primary outcomes of interest were depression symptom severity (e.g., symptom scale scores). The secondary outcomes are anxiety symptoms; quality of life.
1.2. Information sources
Four electronic databases for studies published in English (PubMed, Cochrane Library, Web of Science, and EMBASE) were comprehensively searched from inception to June 8, 2023.
1.3. Search strategy
We did keyword and MeSH searches, and the specific search strategy was shown in Appendix 1. We checked reference lists of relevant reviews for additional studies.
1.4. Selection process
Studies were selected independently by 2 reviewers (Yanan Wu and Meng Xu) and disagreements were resolved in consultation with a third reviewer (Fenfen E). After eliminating duplicates, titles and abstracts were read to exclude irrelevant studies, after which the full text was assessed for final study inclusion.
1.5. Data collection process
Two reviewers (Yanan Wu and Yan Wang) extracted data independently using a standardized study form. Any disagreement was resolved through discussion. If the data were not available, we try to contact the study authors.
1.6. Data items
The content of data extraction mainly included study information (i.e., the year of publication and the first author's name, geographic location, and setting); characteristics of participants (i.e., diagnostic information or relevant inclusion criteria, sample size); intervention characteristics (i.e., website/application name, intervention time, comparison group, and length of follow-up), outcomes (i.e., depression, anxiety, quality of life), and guidance.
1.7. Study risk of bias assessment
The Cochrane collaboration tool (RoB 2) (Sterne et al., 2019; Higgins et al., 2011) was used to assess risk of bias in the studies to be included for review and was done independently by the two review authors (Yan Wang and Fenfen E). For each study, the following items were evaluated: (a) bias arising from the randomisation process; (b) bias due to deviations from intended interventions; (c) bias due to missing outcome data; (d) bias in measurement of the outcome; (e) bias in selection of the reported result. Each item was classified as low, high, or some concerns risk of bias, and the results were displayed by summary plots. A third review author (Meng Xu) was consulted and consensus was reached when there was disagreement on the assessment.
1.8. Synthesis methods
The meta-analysis was performed using RevMan version 5.4 software. Depression was the primary outcomes and secondary outcomes were anxiety symptom, quality of life. In this study, treatment response was measured by improvements in depressive symptoms, anxiety symptoms, and quality of life scores. Depression in the included studies was measured by CDRS-R, CESD-R, BDI, BDI-II, RADS-2, MADRS-S, and MFQ-Child. Anxiety was measured using The Spence Children's Anxiety Scale (SCAS), The Screen for Child Anxiety Related Emotional Disorders (SCARED), and Beck Anxiety Inventory (BAI). Quality was measured by the pediatric version of the Short Form of the quality of Life Enjoyment and Satisfaction Questionnaire (PQ-LES-Q), KIDSCREEN-27, The Pediatric Quality of Life Inventory (PedsQL), and EQ-5D-Y. Depression, anxiety, and quality were measured as continuous variables. If the trials evaluated used different scales to measure the same outcome, standardized mean differences (SMD) with 95 % confidence interval (CI) were used to synthesise the data. We used I-squared (I2) statistical tests to assess the heterogeneity of the results. If the results indicate significant heterogeneity (I2 > 50 %), the results were considered to be heterogeneous, and we will proceed with using the random-effects model. If I2 ≤ 50 %, the random-effects model will be used. In order to better understand the factors that contributed to an effective intervention, we performed subgroup analyses for the outcomes when there were sufficient trials.
1.9. Reporting bias assessment
We performed funnel plots and visually examined the signs of asymmetry to investigate publication bias, and used Egger's test as a formal test of publication bias when the number of the included studies for a given outcome exceeded >10 (n ≥ 10).
1.10. Certainty assessment
We used Grades of Recommendation, Assessment, Development, and Evaluation (GRADE) system (Guyatt et al., 2011) to assess the quality of evidence associated with specific outcomes and to construct a summary table of results. The GRADE approach was used to assess the quality of a set of evidence based on the extent to which one's estimate of an effect or association reflects the degree of certainty of the item being assessed. The quality of the evidence was assessed taking into account the methodological quality, directness of the evidence, heterogeneity of data, precision of effect estimates, and risk of publication bias (Norris et al., 2016).
2. Results
2.1. Study selection
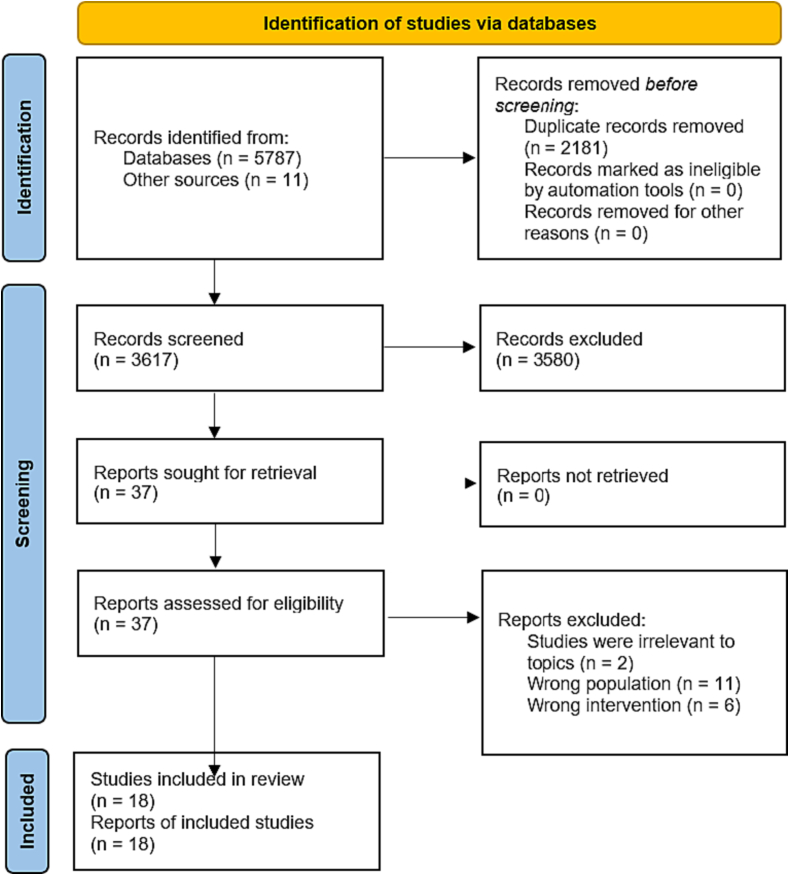
Fig. 1 showed the PRISMA flowchart. A total of 5798 citations were identified in the search strategy, of which 2181 studies were excluded due to duplication, and 3617 studies were screened by browsing titles and abstracts, and after excluding irrelevant literature, a total of 37 full-text studies were assessed for eligibility, with 18 (Fleming et al., 2012; Gladstone et al., 2018; Grudin et al., 2022; Ip et al., 2016; Martínez et al., 2019; Mechler et al., 2022; Merry et al., 2012; Nicol et al., 2022; Poppelaars et al., 2016; Schniering et al., 2022; Smith et al., 2015; Srivastava et al., 2020; Stasiak et al., 2014; Topooco et al., 2018; Topooco et al., 2019; Wright et al., 2017; Wright et al., 2020; Wisman et al., 2023) studies ultimately meeting the inclusion criteria (One of which was unable to obtain usable data, and we contacted its corresponding authors on 22 June 2023, and we received the available information on June 30, 2023. The study (Gladstone et al., 2018) was included). 19 studies were excluded, and the main reasons for excluding studies from this review were shown in Appendix 2.
Fig. 1.
Flow diagram of the literature screening process and result.
2.2. Study characteristics
Table 1 summarized the general characteristics of the included studies. Of the selected trials, 88.90 % were distributed in high-income countries, 5.55 % from upper-middle-income countries, and 5.55 % from lower-middle-income countries (World Bank data), all of which were published between 2012 and 2023. Studies were conducted in schools (33.33 %), communities (27.78 %), and Clinic (38.89 %). The included population ranges in age from 11 to 19 years old. The compliance rate ranges from 54 % to 100 %. Follow-up analyses were conducted in all studies, ranging from 1 month to 24 months. Appendix 3 summarized the additional supplementary features of intervention measures, including specific descriptions of the intervention modality, intervention content, whether parents are involved in the intervention, and whether the intervention is conducted under the guidance of a therapist.
Table 1.
The essential characteristics of the included studies.
| Study | Country | Setting | Age range | N(I/C) | Inclusion | Intervention |
Intervention duration | Follow up | Adherence rate | Outcomes |
|||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | C | Self-report | Clinician-rated | Parent-rated | |||||||||
| Fleming 2012 |
New Zealand | School | 13–16 | 19/11 | CDRS-R > 29 | cCBT SPARX |
Waiting list | 5 weeks | 10 weeks | 94 % | ①RADS-2 ②Spence ③PQ-LES-Q |
①CDRS-R | – |
| Gladstone 2018 |
US. | Clinic | 13–18 | 79/103 | 8 ≤ CES-D10 ≤ 17 or CES-D20 ≥ 16 | ICBT CATCH-IT |
attention control | NR | 24 months | 81 % | ①CESD ②SCARED |
– | – |
| Grudin 2022 |
Sweden | Clinic | 13–17 | 11/11 | mild or moderate MDD according to DSM-5 | ICBT IBA |
TAU | NR | 3 months | 100 % | ①SMFQ-A | ①CDRS-R | ①SMFQ-P |
| IP 2016 |
China | School | 13–17 | 130/127 | 12 ≤ CESD-R ≤ 40 | ICBT CATCH-IT |
attention control | 2 years | 12 months | 97 % | ①CESD-R | – | – |
| Martínez 2019 |
Chile | Clinic | 15–19 | 87/91 | BDI > 10 | cCBT YPSA-M |
EUC | 8 weeks | 6 months | 82 % | ①BDI ③KIDSCREEN-27 |
– | – |
| Mechler 2022 | Sweden | Community | 15–19 | 67/65 | QIDS-A17-SR ≥ 9 | ICBT | IPDT | NR | 10 weeks | 96 % | ①QIDS-A17-SR | – | – |
| Merry 2012 |
New Zealand | Clinic | 12–19 | 94/93 | 10–19 on the PHQ-9 |
cCBT SPARX |
TAU | NR | 3 months | 100 % | ①RADS-2 ②SCAS ③PQ-LES-Q |
①CDRS-R | – |
| Nicol 2022 |
US. | Clinic | 13–17 | 10/7 | Diagnosed with depression | ICBT | Waiting list | 12 weeks | 4 weeks | 94 % | ①PHQ-9 ②GAD-7 |
– | – |
| Poppelaars 2016 |
Netherlands | School | 11–16 | 38/47 | RADS-2 score ≥ 59 | cCBT SPARX |
attention control | 5 months | 12 months | 76 % | ①RADS-2 | – | – |
| Schniering 2022 |
Australia | School | 12–17 | 45/46 | Diagnosed with depression according to DSM-5 | ICBT | Waiting list | 4 h | 3 months | 78 % | ①SMFQ-A ②SCAS-A |
– | ①SMFQ-P ②SCAS-P |
| Smith 2015 |
UK | School | 12–16 | 49/55 | MFQ-C ≥ 20 | cCBT Stressbusters | Waiting list | 8 weeks | 6 months | 93 % | ①MFQ-A ②SCARED-A |
– | ①MFQ-P ②SCARED-P |
| Srivastava 2020 |
India | Clinic | 13–19 | 10/9 | Mild/Moderate Depression | cCBT Smartteen | TAU | 12 weeks | 12 weeks | 90 % | ①BDI-II | – | – |
| Stasiak 2014 |
New Zealand | School | 13–18 | 13/12 | CDRS-R > 29, RADS-2 > 75 | cCBT Journey |
attention control | 4–10 weeks | 1 month | 74 % | ①RADS-2 ③PedsQL |
①CDRS-R | – |
| Topooco 2018 |
Sweden | Community | 15–19 | 22/36 | Mild/Moderate Depression (BDI-II ≥ 14,MINI) | ICBT | attention control | 8 weeks | 6 months | 82 % | ①BDI-II ②BAI |
– | – |
| Topooco 2019 |
Sweden | Community | 15–19 | 31/35 | BDI-II ≥ 14, or fulfilled criteria for MDE | ICBT | attention control | 8 weeks | 12 months | 91 % | ①BDI-II ②BAI |
– | – |
| Wisman 2023 |
Netherlands | Clinic | 13–18 | 17/16 | Diagnosed with depression | ICBT | TAU | NR | 6 months | 85 % | ①CDI-2 ②SCARED |
– | – |
| Wright 2017 |
UK | Community | 12–18 | 25/30 | MFQ ≥ 20 | cCBT Stressbusters | attention control | 4–6 h | 4 months | 60 % | ①MFQ-A ②SCAS-A ③EQ-5D-Y |
– | – |
| Wright 2020 |
UK | Community | 12–18 | 38/37 | MFQ ≥ 20 | cCBT Stressbusters |
attention control | 4–6 h | 12 months | 54 % | ①MFQ-A ②SCAS-A |
– | – |
2.3. Risk of bias in studies
Four studies were assessed as having a high risk of bias; six were assessed as some concerns, and eight as having a low risk of bias. The most common sources of high risk of bias were measurement of the outcome; three of the studies were assessed as high risk of bias in this item. In the Missing outcome data, all studies were assessed as low risk of bias. Only one study was assessed as some concerns on the selection of the reported result, the remaining 17 studies were assessed as low risk of bias. A summary of the risk of bias was provided in Fig. 2.
Fig. 2.
Summary of review authors' judgements about each risk of bias item.
2.4. Result of syntheses
2.4.1. Depression
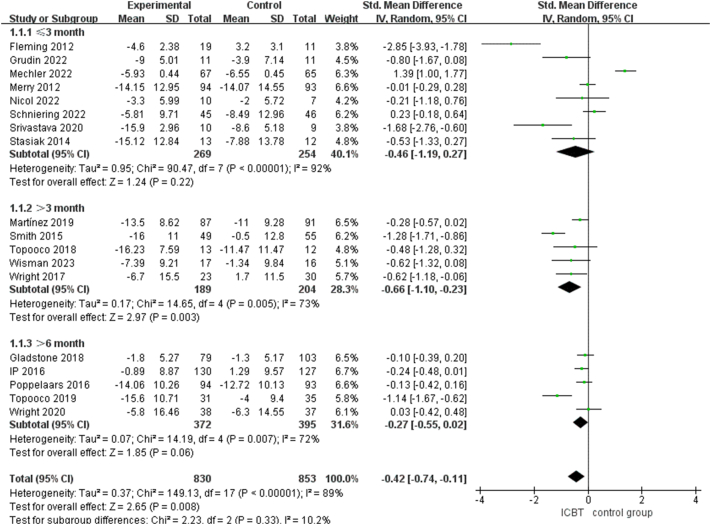
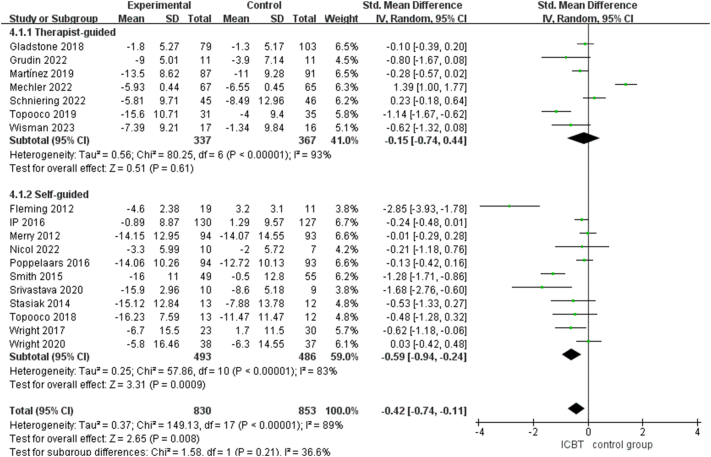
18 trials including 1683 patients evaluated the efficacy of ICBT for depression in adolescents. Compared to the control group, the meta-analysis results from participant self-reported data indicated that ICBT significantly reduces depression scores in adolescents (SMD = −0.42, 95 % CI: [−0.74, −0.11], p < .05; very low certainty). Subgroup analysis of the different control group showed that ICBT significantly reduced depression scores compared to attention control group (SMD = −0.33, 95 % CI: [−0.56, −0.10], p < .05), and the pooled effect size was substantially smaller and not significant when the control groups were limited to waiting list and TAU control group (waiting list: SMD = −0.98, 95 % CI: [−2.14, 0.18], p > .05; TAU: SMD = −0.24, 95 % CI: [−0.94, 0.46], p > .05), as shown in Fig. 3. Subgroup analysis showed that ICBT was effective in improving depression compared to control group at a follow-up time between three and 6 months (SMD = −0.66, 95 % CI: [−1.10, −0.23], p < .05), and there was no significant difference between the intervention group and the control group at <3 months or >6 months (≤3 month: SMD = −0.46, 95 % CI: [−1.1.19, 0.27], p > .05; >6 month: SMD = −0.27, 95 % CI: [−0.55, 0.02], p > .05), as shown in Fig. 4. The subgroup analysis of different guidance elements indicated that the therapist-guided intervention group showed no significant difference in depressive symptoms compared to the control group (SMD = −0.15, 95 % CI: [−0.74, 0.44], p > .05), while the self-guided intervention group significantly improved depressive symptoms in adolescents compared to the control group (SMD = −0.59, 95 % CI: [−0.94, −0.24], p < .05), as shown in Fig. 5. The sensitivity analysis showed that results were stable, and no single study significantly affected overall heterogeneity. Meanwhile, our results were robust. Compared to the control group, the meta-analysis results from clinician-rated data indicated that ICBT significantly reduces depression scores in adolescents (SMD = −8.09, 95 % CI: [−15.40, −0.77], p < .05), as shown in Fig. 6. Compared to the control group, the meta-analysis results from parent-rated data indicated that ICBT significantly reduces depression scores in adolescents (SMD = −0.48, 95 % CI: [−0.81, −0.15], p < .05), as shown in Fig. 7.
Fig. 3.
Effect of the ICBT on the depression scores in adolescents (with different control groups as subgroups).
Fig. 4.
Effect of the ICBT on the depression scores in adolescents (with different follow-up times as subgroups).
Fig. 5.
Effect of the ICBT on the depression scores in adolescents (with different guidance as subgroups).
Fig. 6.
Effect of the ICBT on the depression scores in adolescents (clinician-rated).
Fig. 7.
Effect of the ICBT on the depression scores in adolescents (parent-rated).
2.4.2. Anxiety
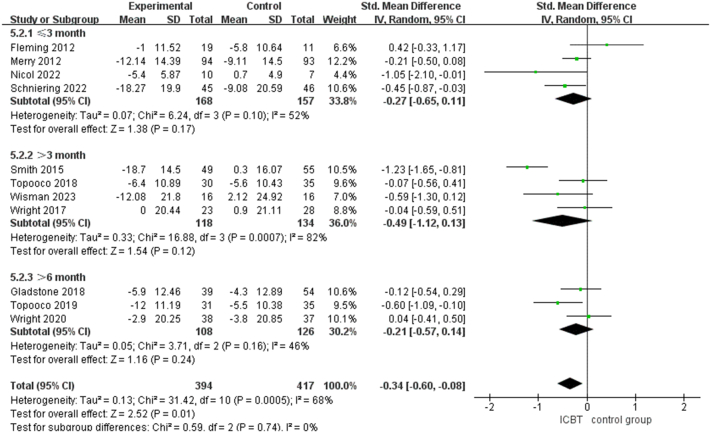
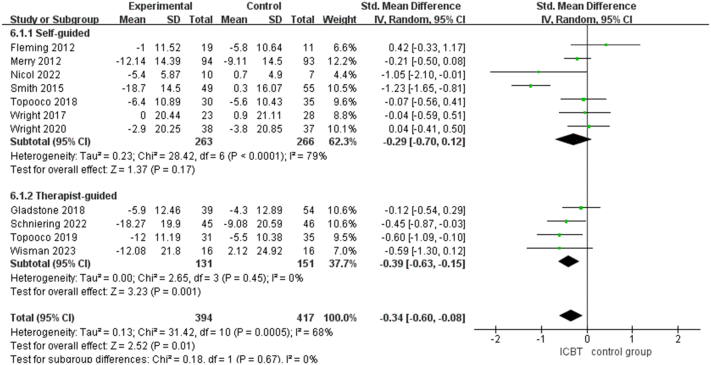
11 trials including 811 patients evaluated the efficacy of ICBT for anxiety in adolescents. Compared to the control group, the meta-analysis results from participant self-reported data indicated that ICBT significantly reduces anxiety scores in adolescents (SMD = −0.34, 95 % CI: [−0.60, −0.08], p < .05; very low certainty). Subgroup analysis by control group showed no significant difference in the results obtained compared to the different control groups (waiting list: SMD = −0.58, 95 % CI: [−1.27, 0.10], p > .05; attention control: SMD = −0.15, 95 % CI: [−0.37, 0.06], p > .05; TAU: SMD = −0.26, 95 % CI: [−0.53, 0.00], p = .05), as shown in Fig. 8. Subgroup analyses with different follow-up times showed that ICBT did not significantly improve anxiety compared with the control group (≤3 month: SMD = −0.27, 95 % CI: [−0.65, 0.11], p > .05; >3 month: SMD = −0.49, 95 % CI: [−1.12, 0.13], p > .05; >6 month: SMD = −0.21, 95 % CI: [−0.57, 0.14], p > .05), as shown in Fig. 9. The sensitivity analysis showed that one trial significantly affected overall heterogeneity. Meanwhile, after excluding one trial (Smith et al., 2015) our results are robust, indicating the stability of the results. The subgroup analysis of different guidance elements indicated that the self-guided intervention group showed no significant difference in anxiety symptoms compared to the control group (SMD = −0.29, 95 % CI: [−0.70, 0.12], p > .05), while the therapist-guided intervention group significantly improved anxiety symptoms in adolescents compared to the control group (SMD = −0.39, 95 % CI: [−0.63, −0.15], p < .05), as shown in Fig. 10. Compared to the control group, the meta-analysis results from parent-rated data indicated that ICBT significantly reduces anxiety scores in adolescents (SMD = −0.49, 95 % CI: [−0.85, −0.14], p < .05), as shown in Fig. 11.
Fig. 8.
Effect of the ICBT on the anxiety scores in adolescents (with different control groups as subgroups).
Fig. 9.
Effect of the ICBT on the anxiety scores in adolescents (with different follow-up as subgroups).
Fig. 10.
Effect of the ICBT on the anxiety scores in adolescents (with different guidance as subgroups).
Fig. 11.
Effect of the ICBT on the anxiety scores in adolescents (parent-rated).
2.4.3. QoL
5 trials including 465 patients evaluated the efficacy of ICBT for QoL in adolescents. Compared with the control group, our meta-analysis results demonstrated that there was no significant difference in the QoL scores of adolescents between the ICBT and control group (SMD = 0.12, 95 % CI: [−0.10, 0.34], p > .05; low certainty), as shown in Fig. 12.
Fig. 12.
Effect of the ICBT on the QoL scores in adolescents.
2.5. Reporting bias
The funnel plot of depression is presented in Fig. 13. Visual inspection of the plot and Egger's test suggested that no publication bias was observed, with the funnel plot showing a relatively symmetrical distribution (Egger's test, p > .05). The funnel plot of anxiety is presented in Fig. 14. Visual inspection of the plot and Egger's test suggested that no publication bias was observed, with the funnel plot showing a relatively symmetrical distribution (Egger's test, p > .05).
Fig. 13.

Funnel plot of depression.
Fig. 14.

Funnel plot of anxiety.
2.6. Certainty of evidence
Overall, the certainty of the evidence was low, mainly due to high heterogeneity between studies (inconsistency), and the risk of bias. As shown in Fig. 15.
Fig. 15.
Summary of findings.
3. Discussion
3.1. Principal findings
This review examined the efficacy of ICBT for depression in adolescents. We included 18 published RCTs including a total of 1683 participants from Sweden (n = 4), New Zealand (n = 3), UK (n = 3), Netherlands (n = 2), US (n = 2), India (n = 1), Australia (n = 1), China (n = 1), and Chile (n = 1). Overall, compared with the control group, the meta-analysis showed that ICBT may be useful in improving depressive symptoms in adolescents. The findings are also similar to those of the adult population, for example, a recent meta-analysis found that ICBT was effective in treating depression in adults (Andrews et al., 2018; Etzelmueller et al., 2020). It's worth noting that the research from Etzelmueller et al. indicates that compared to adolescents; Internet-Based Cognitive Behavioral Therapy (ICBT) has a greater effect size in improving depression and anxiety within the adult population. The results of the subgroup analysis revealed that the ICBT group demonstrated a greater improvement in depressive symptoms compared to the attention control group. However, there were no significant differences in the improvement of adolescent depression between the ICBT group and the treatment as usual group, as well as the waiting list group. Nonetheless, the potential of ICBT cannot be overlooked, given its advantages, such as more flexibility in terms of time and location, more privacy, effective cost savings, and should therefore be recommended. The results of subgroup analysis, considering the duration of follow-up as a moderating factor, demonstrated that the intervention was effective when the follow-up period ranged from 3 to 6 months. However, beyond 6 months, there was no significant improvement compared to the control group. This highlights the importance of not only focusing on post-intervention outcomes but also placing emphasis on the long-term effects on participants. Furthermore, whether it was patient self-reported outcomes, parent-rated assessments, or clinician-rated, the results obtained were consistent. They all indicated that ICBT was effective in improving patient's depressive symptoms compared to the control group. This distinction also sets our study apart from previous research: we have reported outcomes from multiple perspectives, providing a comprehensive depiction of the effects of ICBT on participants.
Compared with the control group, the meta-analysis showed that ICBT may be useful in improving anxiety symptom in adolescents. This result is similar to the findings of Wickersham et al. (2022). Notably, analysis of subgroups with different guidance elements showed that the self-guided intervention did not significantly improve participants' anxiety symptoms compared to the control group. The therapist-guided intervention significantly improved the participants' anxiety symptoms compared to the control group. It can be seen that whether the therapist intervenes or not, as well as the supervision and guidance of the participants have a significant impact on the intervention effect. Moreover, the findings of the study by Ebert et al. also revealed a significant moderating effect of age on treatment outcomes. They observed that, in comparison to adolescents, Internet-Based Cognitive Behavioral Therapy (ICBT) had a more pronounced therapeutic effect on childhood anxiety. Therefore, future research could delve deeper into the association between age and the effectiveness of ICBT interventions for depression and anxiety symptoms.
Moreover, the evidence showed that there was no significant difference in the QoL scores of adolescents between the ICBT and control group. In fact, only 5 of the 18 studies included reported quality of life outcomes. The results may therefore have been limited by the number of studies included. A study by Elfghi also suggested that the underpowered studies may be due to insufficient sample size (Elfghi et al., 2020). Therefore, further high-quality evidence is needed to elucidate the impact of ICBT on QoL in adolescents.
Some statistical heterogeneity was found in our meta-analysis on depression and anxiety. Statistical heterogeneity is the variation in individual study effect sizes. This may be due to differences in study population, study design, interventions or outcome assessment (clinical heterogeneity) or risk of bias (statistical heterogeneity) (Lau et al., 1998). To explore sources of heterogeneity in depression outcome, we did subgroup analyses with separate subgroups for control measures, follow-up time, and guidance elements, and none of the heterogeneity was significantly reduced. It can be seen that none of the above factors was a major source of heterogeneity. Research indicates that a small sample size could be a potential source of heterogeneity. In this study, all three included studies have sample sizes below 30. Consequently, we postulate that the significant heterogeneity observed in the statistical results may be attributed to the relatively small sample sizes (Ishaque et al., 2018). In addition, risk of bias is also a possible source of heterogeneity.
Due to the risk of bias of the included studies, the results of this review should be interpreted with caution. There was a high risk of bias for measurement of the outcome in our meta-analysis. The high risks of bias may significantly reduce the reliability of the results (Zeng et al., 2008). In addition, it has been noted that the quality and reporting of RCTs needs to be improved, particularly with regard to reporting methods and outcomes (Li et al., 2022; Li et al., 2021). Therefore, according to the Cochrane quality assessment tool, researchers need rigorous training to clearly understand the importance of study quality and to improve the reliability of RCTs (Yao et al., 2016; Tian et al., 2017).
3.2. Strengths and limitations
This is a meta-analysis of this type specifically for the adolescent age group to determine the efficacy of ICBT in this different developmental period. There are few studies that have specifically explored the effects of ICBT on adolescent depression. Existing studies such as Ebert; (Ebert et al., 2015) Vigerland; (Vigerland et al., 2016) Christ; (Christ et al., 2020) et al. identified the study population as adolescents and young adults and did not examine the specific group of adolescents. Given the unique biological and social transitions associated with adolescence, and the associated prevalence of mental health disorders in this age group, this is an important addition to the literature (Costello et al., 2003; Merikangas et al., 2010). While Wickersham et al. (2022) systematically evaluated the efficacy of ICBT for adolescent depression. However, we added to their study by including five articles that explored the efficacy of ICBT in treating depression in adolescents. In addition, we used a comprehensive and systematic search strategy to ensure the validity of the results obtained. Moreover, we included studies from a wide range of countries, suggesting that ICBT may be an effective intervention in a variety of cultural settings. Some limitations of this study should also be mentioned. We focused on participants aged 10 to 19 years but acknowledge that the age of adolescents is widely disputed and therefore some of the studies excluded from this review due to the age of the participants may have produced findings relevant to the adolescent population. Second, some studies were not included due to data availability limitations, although we did our best to search for access database resources and references. Third, this study focused on the effects of ICBT on depression, with limited inclusion of evidence on anxiety and quality of life as outcomes. Therefore, more high-quality trials are still needed to further elucidate the effects of ICBT on adolescents.
3.3. Clinical implications
This article systematically reviews the existing randomized controlled trials of ICBT in the treatment of adolescent depression to provide clarity for clinical decision-making. Nevertheless, the influence of the trials' overall low quality impedes the formation of definitive conclusions. Our findings do suggest that ICBT could potentially yield a favorable impact on adolescent depression, a notion that merits consideration among clinicians. Particularly, ICBT displays promise, especially in alleviating depressive and anxiety symptoms in adolescents. Notably, the positive influence of clinician guidance on intervention effects is significant. Hence, it is advisable to employ cognitive behavioral therapy as an intervention for adolescents with depression and anxiety symptoms, guided by therapists. Moreover, owing to the constrained number of included studies, the existing evidence is inadequate to conclusively demonstrate the clinical value of ICBT in enhancing the quality of life. Consequently, further rigorous trials of high quality are imperative to comprehensively unveil the effects of ICBT.
3.4. Future directions
Among the eighteen studies included, sixteen were conducted in high-income countries, one in upper-middle-income countries, and one in lower-middle-income countries. It is evident that there remains a substantial need for future research that investigates the feasibility and effectiveness of ICBT in low- and middle-income countries. Secondly, the prevailing studies in this domain predominantly comprise pilot projects characterized by modest sample sizes and diminished quality. This underscores the necessity for researchers to persist in conducting large-scale, high-quality trials in the forthcoming endeavors. Thirdly, the variances observed in intervention effects across different follow-up periods underscore the importance of focusing not solely on post-intervention effects but also on the enduring impact of interventions on participants. Fourthly, forthcoming research could delve deeper into the potential negative effects encompassing participants' mood deterioration and inclinations toward self-harm during the intervention. Fifthly, this study centers on the efficacy of ICBT for adolescent depression. Future strides in machine learning and intelligent algorithms hold the potential to pave the way for more nuanced and pertinent intervention strategies. Thus, upcoming research can continue to explore the efficacy of more advanced interventions that result from the synergy between the Internet and machine learning, as well as intelligent algorithms.
4. Conclusion
The meta-analysis suggests that ICBT may be an effective intervention to help improve depression and anxiety symptoms in adolescents, showing a statistically significant effect. Furthermore, our results suggest that ICBT is similar to control groups in terms of improving quality of life in adolescents. Researchers must have a clear understanding of the importance of study quality and be committed to self-checking study design against the Cochrane Quality Assessment Tool through. Importantly, this study also demonstrates the need for higher quality methodological research in this population.
Registration and protocol
Our findings were reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guideline (Ziegler et al., 2011) and detailed analysis protocol was registered on the International Prospective Register of Systematic Reviews (PROSPERO registration number: CRD42021277562). The PRISMA guideline can be found in Appendix 4.
Funding
This research is supported by the Fundamental Research Funds for the Central Universities (Project No. lzujbky-2021-ct06, lzujbky-2021-kb22) and the Open Project of the National Institute of Health Security of the Capital Medical University: A study on the quality evaluation system of health insurance services based on DIP (Project No. YB2021B07).
Declaration of competing interest
The authors have no conflicts of interest to declare, have all read and approved the manuscript, and agree with its submission.
Acknowledgments
The authors would like to thank all members of the Evidence-Based Medicine Center, Lanzhou University, China, for their help with this study.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2023.100673.
Contributor Information
Kehu Yang, Email: kehuyangebm2006@126.com.
Xiuxia Li, Email: lixiuxia@lzu.edu.cn.
Appendix A. Supplementary data
Search Strategy.
Literature for Exclusion and Exclusion Reasons.
Additional features of intervention measures.
PRISMA 2020 Checklist.
References
- Andersson G. Using the internet to provide cognitive behaviour therapy. Behav. Res. Ther. 2009;47:175–180. doi: 10.1016/j.brat.2009.01.010. [DOI] [PubMed] [Google Scholar]
- Andersson G. In: Annual Review of Clinical Psychology. Cannon T.D., Widiger T., editors. Vol. 12. 2016. Internet-delivered psychological treatments. [DOI] [PubMed] [Google Scholar]
- Andrews G., Basu A., Cuijpers P., Craske M.G., Mcevoy P., English C.L., Newby J.M. Computer therapy for the anxiety and depression disorders is effective, acceptable and practical health care: an updated meta-analysis. J. Anxiety Disord. 2018;55:70–78. doi: 10.1016/j.janxdis.2018.01.001. [DOI] [PubMed] [Google Scholar]
- Barak A., Klein B., Proudfoot J.G. Defining internet-supported therapeutic interventions. Ann. Behav. Med. 2009;38:4–17. doi: 10.1007/s12160-009-9130-7. [DOI] [PubMed] [Google Scholar]
- Brady E.U., Kendall P.C. Comorbidity of anxiety and depression in children and adolescents. Psychol. Bull. 1992;111:244–255. doi: 10.1037/0033-2909.111.2.244. [DOI] [PubMed] [Google Scholar]
- Calear A.L., Christensen H. Review of internet-based prevention and treatment programs for anxiety and depression in children and adolescents. Med. J. Aust. 2010;192:S12–S14. doi: 10.5694/j.1326-5377.2010.tb03686.x. [DOI] [PubMed] [Google Scholar]
- Christ C., Schouten M.J., Blankers M., van Schaik D.J., Beekman A.T., Wisman M.A., Stikkelbroek Y.A., Dekker J.J. Internet and computer-based cognitive behavioral therapy for anxiety and depression in adolescents and young adults: systematic review and meta-analysis. J. Med. Internet Res. 2020;22 doi: 10.2196/17831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Costello E.J., Mustillo S., Erkanli A., Keeler G., Angold A. Prevalence and development of psychiatric disorders in childhood and adolescence. Arch. Gen. Psychiatry. 2003;60:837–844. doi: 10.1001/archpsyc.60.8.837. [DOI] [PubMed] [Google Scholar]
- Creswell C., Waite P., Cooper P.J. Assessment and management of anxiety disorders in children and adolescents. Arch. Dis. Child. 2014;99:674–678. doi: 10.1136/archdischild-2013-303768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dick B., Ferguson B.J. Health for the world’s adolescents: a second chance in the second decade. J. Adolesc. Health. 2015;56:3–6. doi: 10.1016/j.jadohealth.2014.10.260. [DOI] [PubMed] [Google Scholar]
- Ebert D.D., Zarski A.C., Christensen H., Stikkelbroek Y., Cuijpers P., Berking M., Riper H. Internet and computer-based cognitive behavioral therapy for anxiety and depression in youth: a meta-analysis of randomized controlled outcome trials. PLoS One. 2015;10 doi: 10.1371/journal.pone.0119895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elfghi M., Jordan F., Sultan S., Tawfick W. Study within a trial protocol: same-day consent vs. delayed consent in a randomized trial. J. Evid. Based Med. 2020;13:246–248. doi: 10.1111/jebm.12392. [DOI] [PubMed] [Google Scholar]
- Essau C.A. Frequency and patterns of mental health services utilization among adolescents with anxiety and depressive disorders. Depress. Anxiety. 2005;22:130–137. doi: 10.1002/da.20115. [DOI] [PubMed] [Google Scholar]
- Etzelmueller A., Vis C., Karyotaki E., Baumeister H., Titov N., Berking M., Cuijpers P., Riper H., Ebert D.D. Effects of internet-based cognitive behavioral therapy in routine care for adults in treatment for depression and anxiety: systematic review and meta-analysis. J. Med. Internet Res. 2020:22. doi: 10.2196/18100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatehi F., Samadbeik M., Kazemi A. What is digital health? Review of definitions. Stud. Health Technol. Inform. 2020;275:67–71. doi: 10.3233/SHTI200696. [DOI] [PubMed] [Google Scholar]
- Fernandes M., Mendonça C.R., da Silva T.M.V., Noll P., de Abreu L.C., Noll M. Relationship between depression and quality of life among students: a systematic review and meta-analysis. Sci. Rep. 2023;13:6715. doi: 10.1038/s41598-023-33584-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fleming T., Dixon R., Frampton C., Merry S. A pragmatic randomized controlled trial of computerized CBT (SPARX) for symptoms of depression among adolescents excluded from mainstream education. Behav. Cogn. Psychother. 2012;40:529–541. doi: 10.1017/S1352465811000695. [DOI] [PubMed] [Google Scholar]
- Gazibara T., Pekmezovic T., Popovic A., Paunic M., Kisic-Tepavcevic D. Chronic diseases among university students: prevalence, patterns and impact on health-related quality of life. Vojnosanit. Pregl. 2018;75:1178–1184. [Google Scholar]
- Gladstone T., Terrizzi D., Stinson A., Nidetz J., Canel J., Ching E., Berry A., Cantorna J., Fogel J., Eder M., Bolotin M., Thomann L.O., Griffith K., Ip P., Aaby D.A., Brown C.H., Beardslee W., Bell C., Crawford T.J., Fitzgibbon M., Schiffer L., Liu N., Marko-Holguin M., Van Voorhees B.W. Effect of internet-based cognitive behavioral humanistic and interpersonal training vs. internet-based general health education on adolescent depression in primary care: a randomized clinical trial. JAMA Netw. Open. 2018:1. doi: 10.1001/jamanetworkopen.2018.4278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotlib I.H., Joormann J. Cognition and depression: current status and future directions. Annu. Rev. Clin. Psychol. 2010;6:285–312. doi: 10.1146/annurev.clinpsy.121208.131305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grudin R., Ahlen J., Mataix-Cols D., Lenhard F., Henje E., Månsson C., Sahlin H., Beckman M., Serlachius E., Vigerland S. Therapist-guided and self-guided internet-delivered behavioural activation for adolescents with depression: a randomised feasibility trial. BMJ Open. 2022;12 doi: 10.1136/bmjopen-2022-066357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulliver A., Griffiths K.M., Christensen H. Perceived barriers and facilitators to mental health help-seeking in young people: a systematic review. BMC Psychiatry. 2010;10:113. doi: 10.1186/1471-244X-10-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guyatt G., Oxman A.D., Akl E.A., Kunz R., Vist G., Brozek J., Norris S., Falck-Ytter Y., Glasziou P., Debeer H., Jaeschke R., Rind D., Meerpohl J., Dahm P., Schünemann H.J. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- Higgins J.P., Altman D.G., Gøtzsche P.C., Jüni P., Moher D., Oxman A.D., Savovic J., Schulz K.F., Weeks L., Sterne J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollis C., Falconer C.J., Martin J.L., Whittington C., Stockton S., Glazebrook C., Davies E.B. Annual research review: digital health interventions for children and young people with mental health problems - a systematic and meta-review. J. Child Psychol. Psychiatry. 2017;58:474–503. doi: 10.1111/jcpp.12663. [DOI] [PubMed] [Google Scholar]
- Ip P., Chim D., Chan K.L., Li T.M., Ho F.K., van Voorhees B.W., Tiwari A., Tsang A., Chan C.W., Ho M., et al. Effectiveness of a culturally attuned internet-based depression prevention program for Chinese adolescents: a randomized controlled trial. Depress. Anxiety. 2016;33:1123–1131. doi: 10.1002/da.22554. [DOI] [PubMed] [Google Scholar]
- Ishaque S.M., Khosruzzaman S.M., Ahmed D.S., Sah M.P. A randomized placebo-controlled clinical trial of a multi-strain probiotic formulation (Bio-Kult®) in the management of diarrhea-predominant irritable bowel syndrome. BMC Gastroenterol. 2018;18:71. doi: 10.1186/s12876-018-0788-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karyotaki E., Riper H., Twisk J., Hoogendoorn A., Kleiboer A., Mira A., Mackinnon A., Meyer B., Botella C., Littlewood E., Andersson G., Christensen H., Klein J.P., Schröder J., Bretón-López J., Scheider J., Griffiths K., Farrer L., Huibers M.J., Phillips R., Gilbody S., Moritz S., Berger T., Pop V., Spek V., Cuijpers P. Efficacy of self-guided internet-based cognitive behavioral therapy in the treatment of depressive symptoms: a meta-analysis of individual participant data. JAMA Psychiatry. 2017;74:351–359. doi: 10.1001/jamapsychiatry.2017.0044. [DOI] [PubMed] [Google Scholar]
- Lau J., Ioannidis J.P., Schmid C.H. Summing up evidence: one answer is not always enough. Lancet. 1998;351:123–127. doi: 10.1016/S0140-6736(97)08468-7. [DOI] [PubMed] [Google Scholar]
- Lehtimaki S., Martic J., Wahl B., Foster K.T., Schwalbe N. Evidence on digital mental health interventions for adolescents and young people: systematic overview. JMIR Mental Health. 2021;8 doi: 10.2196/25847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X., Li Y., Guo K., Chen N., Cui X., Bai Z., Chen Y., Yang K. Evidence based social science in China paper 3: the quality of social science RCTs published from 2000–2020. J. Clin. Epidemiol. 2022;141:64–73. doi: 10.1016/j.jclinepi.2021.09.014. [DOI] [PubMed] [Google Scholar]
- Li Y., Cao L., Zhang Z., Hou L., Qin Y., Hui X., Li J., Zhao H., Cui G., Cui X., Li R., Lin Q., Li X., Yang K. Reporting and methodological quality of COVID-19 systematic reviews needs to be improved: an evidence mapping. J. Clin. Epidemiol. 2021;135:17–28. doi: 10.1016/j.jclinepi.2021.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin J., Ebert D.D., Lehr D., Berking M., Baumeister H. Internet based cognitive behavioral interventions: state of the art and implementation possibilities in rehabilitation. Rehabilitation (Stuttg) 2013;52:155–163. doi: 10.1055/s-0033-1343491. [DOI] [PubMed] [Google Scholar]
- MacDonell K.W., Prinz R.J. A review of technology-based youth and family-focused interventions. Clin. Child. Fam. Psychol. Rev. 2017;20:185–200. doi: 10.1007/s10567-016-0218-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martínez V., Rojas G., Martínez P., Gaete J., Zitko P., Vöhringer P.A., Araya R. Computer-assisted cognitive-behavioral therapy to treat adolescents with depression in primary health care centers in Santiago, Chile: a randomized controlled trial. Front. Psychol. 2019;10:552. doi: 10.3389/fpsyt.2019.00552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechler J., Lindqvist K., Carlbring P., Topooco N., Falkenström F., Lilliengren P., Andersson G., Johansson R., Midgley N., Edbrooke-Childs J., Dahl H.J., Sandell R., Thorén A., Ulberg R., Bergsten K.L., Philips B. Therapist-guided internet-based psychodynamic therapy versus cognitive behavioural therapy for adolescent depression in Sweden: a randomised, clinical, non-inferiority trial. Lancet Digit. Health. 2022;4:e594–e603. doi: 10.1016/S2589-7500(22)00095-4. [DOI] [PubMed] [Google Scholar]
- Merikangas K.R., He J.P., Burstein M., Swanson S.A., Avenevoli S., Cui L., Benjet C., Georgiades K., Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) J. Am. Acad. Child Adolesc. Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas K.R., He J.P., Burstein M., Swendsen J., Avenevoli S., Case B., Georgiades K., Heaton L., Swanson S., Olfson M. Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A) J. Am. Acad. Child Adolesc. Psychiatry. 2011;50:32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merry S.N., Stasiak K., Shepherd M., Frampton C., Fleming T., Lucassen M.F. The effectiveness of SPARX, a computerised self help intervention for adolescents seeking help for depression: randomised controlled non-inferiority trial. BMJ. 2012;344 doi: 10.1136/bmj.e2598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mojtabai R., Olfson M., Han B. National trends in the prevalence and treatment of depression in adolescents and young adults. Pediatrics. 2016;138 doi: 10.1542/peds.2016-1878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicol G., Wang R., Graham S., Dodd S., Garbutt J. Chatbot-delivered cognitive behavioral therapy in adolescents with depression and anxiety during the COVID-19 pandemic: feasibility and acceptability study. JMIR Form. Res. 2022;6 doi: 10.2196/40242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris S.L., Meerpohl J.J., Akl E.A., Schünemann H.J., Gartlehner G., Chen Y., Whittington C. The skills and experience of GRADE methodologists can be assessed with a simple tool. J. Clin. Epidemiol. 2016;79:150–158.e1. doi: 10.1016/j.jclinepi.2016.07.001. [DOI] [PubMed] [Google Scholar]
- O’Brien D., Harvey K., Howse J., Reardon T., Creswell C. Barriers to managing child and adolescent mental health problems: a systematic review of primary care practitioners’ perceptions. Br. J. Gen. Pract. 2016;66:e693–e707. doi: 10.3399/bjgp16X687061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oud M., de Winter L., Vermeulen-Smit E., Bodden D., Nauta M., Stone L., van den Heuvel M., Taher R.A., de Graaf I., Kendall T., Engels R., Stikkelbroek Y. Effectiveness of CBT for children and adolescents with depression: a systematic review and meta-regression analysis. Eur. Psychiatry. 2019;57:33–45. doi: 10.1016/j.eurpsy.2018.12.008. [DOI] [PubMed] [Google Scholar]
- Poppelaars M., Tak Y.R., Lichtwarck-Aschoff A., Engels R., Lobel A., Merry S.N., Lucassen M.F.G., Granic I. A randomized controlled trial comparing two cognitive-behavioral programs for adolescent girls with subclinical depression: a school based program (Op Volle Kracht) and a computerized program (SPARX) Behav. Res. Ther. 2016;80:33–42. doi: 10.1016/j.brat.2016.03.005. [DOI] [PubMed] [Google Scholar]
- Prieto J.M., Atala J., Blanch J., Carreras E., Rovira M., Cirera E., Espinal A., Gasto C. Role of depression as a predictor of mortality among cancer patients after stem-cell transplantation. J. Clin. Oncol. 2005;23:6063–6071. doi: 10.1200/JCO.2005.05.751. [DOI] [PubMed] [Google Scholar]
- Reddy A., Mansuri Z., Vadukapuram R., Shah K., Thootkur M., Trivedi C. Efficacy of cognitive behavioral therapy for insomnia for the treatment of child and adolescent anxiety and depression: a systematic review from randomized controlled trials. J. Nerv. Ment. Dis. 2023;211:238–243. doi: 10.1097/NMD.0000000000001613. [DOI] [PubMed] [Google Scholar]
- Richardson T., Stallard P., Velleman S. Computerised cognitive behavioural therapy for the prevention and treatment of depression and anxiety in children and adolescents: a systematic review. Clin. Child. Fam. Psychol. Rev. 2010;13:275–290. doi: 10.1007/s10567-010-0069-9. [DOI] [PubMed] [Google Scholar]
- Rohde P., Lewinsohn P.M., Klein D.N., Seeley J.R., Gau J.M. Key characteristics of major depressive disorder occurring in childhood, adolescence, emerging adulthood, adulthood. Clin. Psychol. Sci. 2013;1 doi: 10.1177/2167702612457599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schniering C.A., Einstein D., Kirkman J.J.L., Rapee R.M. Online treatment of adolescents with comorbid anxiety and depression: a randomized controlled trial. J. Affect. Disord. 2022;311:88–94. doi: 10.1016/j.jad.2022.05.072. [DOI] [PubMed] [Google Scholar]
- Smith P., Scott R., Eshkevari E., Jatta F., Leigh E., Harris V., Robinson A., Abeles P., Proudfoot J., Verduyn C., et al. Computerised CBT for depressed adolescents: randomised controlled trial. Behav. Res. Ther. 2015;73:104–110. doi: 10.1016/j.brat.2015.07.009. [DOI] [PubMed] [Google Scholar]
- Srivastava P., Mehta M., Sagar R., Ambekar A. Smartteen - a computer assisted cognitive behavior therapy for Indian adolescents with depression - a pilot study. Asian J. Psychiatr. 2020;50:101970. doi: 10.1016/j.ajp.2020.101970. [DOI] [PubMed] [Google Scholar]
- Stasiak K., Hatcher S., Frampton C., Merry S.N. A pilot double blind randomized placebo controlled trial of a prototype computer-based cognitive behavioural therapy program for adolescents with symptoms of depression. Behav. Cogn. Psychother. 2014;42:385–401. doi: 10.1017/S1352465812001087. [DOI] [PubMed] [Google Scholar]
- Sterne J.A.C., Savović J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., Cates C.J., Cheng H.Y., Corbett M.S., Eldridge S.M., Emberson J.R., Hernán M.A., Hopewell S., Hróbjartsson A., Junqueira D.R., Jüni P., Kirkham J.J., Lasserson T., LI T., McAleenan A., Reeves B.C., Shepperd S., Shrier I., Stewart L.A., Tilling K., White I.R., Whiting P.F., Higgins J.P.T. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- Sweeney G.M., Donovan C.L., March S., Forbes Y. Logging into therapy: adolescent perceptions of online therapies for mental health problems. Internet Interv. 2019;15:93–99. doi: 10.1016/j.invent.2016.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian J., Zhang J., Ge L., Yang K., Song F. The methodological and reporting quality of systematic reviews from China and the USA are similar. J. Clin. Epidemiol. 2017;85:50–58. doi: 10.1016/j.jclinepi.2016.12.004. [DOI] [PubMed] [Google Scholar]
- Topooco N., Berg M., Johansson S., Liljethörn L., Radvogin E., Vlaescu G., Nordgren L.B., Zetterqvist M., Andersson G. Chat- and internet-based cognitive-behavioural therapy in treatment of adolescent depression: randomised controlled trial. BJPsych Open. 2018;4:199–207. doi: 10.1192/bjo.2018.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topooco N., Bylehn S., Nysater E.D., Holmlund J., Lindegaard J., Johansson S., Aberg L., Nordgren L.B., Zetterqvist M., Andersson G. Evaluating the efficacy of internet-delivered cognitive behavioral therapy blended with synchronous chat sessions to treat adolescent depression: randomized controlled trial. J. Med. Internet Res. 2019:21. doi: 10.2196/13393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vigerland S., Lenhard F., Bonnert M., Lalouni M., Hedman E., Ahlen J., Olén O., Serlachius E., Ljótsson B. Internet-delivered cognitive behavior therapy for children and adolescents: a systematic review and meta-analysis. Clin. Psychol. Rev. 2016;50:1–10. doi: 10.1016/j.cpr.2016.09.005. [DOI] [PubMed] [Google Scholar]
- Wickersham A., Dickson H., Jones R., Pritchard M., Stewart R., Ford T., Downs J. Educational attainment trajectories among children and adolescents with depression, and the role of sociodemographic characteristics: longitudinal data-linkage study. Br. J. Psychiatry. 2021;218:151–157. doi: 10.1192/bjp.2020.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickersham A., Sugg H.V.R., Epstein S., Stewart R., Ford T., Downs J. Systematic review and meta-analysis: the association between child and adolescent depression and later educational attainment. J. Am. Acad. Child Adolesc. Psychiatry. 2021;60:105–118. doi: 10.1016/j.jaac.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wickersham A., Barack T., Cross L., Downs J. Computerized cognitive behavioral therapy for treatment of depression and anxiety in adolescents: systematic review and meta-analysis. J. Med. Internet Res. 2022;24 doi: 10.2196/29842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisman M.A., Emmelkamp J., Dekker J.J.M., Christ C. Internet-based emotion-regulation training added to CBT in adolescents with depressive and anxiety disorders: a pilot randomized controlled trial to examine feasibility, acceptability, and preliminary effectiveness. Internet Interv. 2023;31:100596. doi: 10.1016/j.invent.2022.100596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodward L.J., Fergusson D.M. Life course outcomes of young people with anxiety disorders in adolescence. J. Am. Acad. Child Adolesc. Psychiatry. 2001;40:1086–1093. doi: 10.1097/00004583-200109000-00018. [DOI] [PubMed] [Google Scholar]
- Wright B., Tindall L., Littlewood E., Allgar V., Abeles P., Trépel D., Ali S. Computerised cognitive-behavioural therapy for depression in adolescents: feasibility results and 4-month outcomes of a UK randomised controlled trial. BMJ Open. 2017;7 doi: 10.1136/bmjopen-2016-012834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright B., Tindall L., Hargate R., Allgar V., Trépel D., Ali S. Computerised cognitive-behavioural therapy for depression in adolescents: 12-month outcomes of a UK randomised controlled trial pilot study. BJPsych Open. 2020;6 doi: 10.1192/bjo.2019.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao L., Sun R., Chen Y.L., Wang Q., Wei D., Wang X., Yang K. The quality of evidence in Chinese meta-analyses needs to be improved. J. Clin. Epidemiol. 2016;74:73–79. doi: 10.1016/j.jclinepi.2016.01.003. [DOI] [PubMed] [Google Scholar]
- Zeng J., Li Y.Q., Zuo X.L., Zhen Y.B., Yang J., Liu C.H. Clinical trial: effect of active lactic acid bacteria on mucosal barrier function in patients with diarrhoea-predominant irritable bowel syndrome. Aliment. Pharmacol. Ther. 2008;28:994–1002. doi: 10.1111/j.1365-2036.2008.03818.x. [DOI] [PubMed] [Google Scholar]
- Ziegler A., Antes G., Koenig I.R. Preferred report items for systematic reviews and meta-analysis: the PRISMA statement. Dtsch. Med. Wochenschr. 2011;136:E9–E15. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search Strategy.
Literature for Exclusion and Exclusion Reasons.
Additional features of intervention measures.
PRISMA 2020 Checklist.