Abstract
Previously excluded internal iliac artery (IIA) aneurysms can continue to expand and pose a risk of rupture. In this case series, we present three patients with previously excluded, expanding IIA aneurysms after endovascular stent coverage or open surgical ligation of the proximal IIA. We describe a hybrid approach to treat these patients safely and effectively.
Keywords: Endovascular treatment, Excluded aneurysm, Internal iliac artery aneurysm
Internal iliac artery (IIA) aneurysms (IIAAs) are conventionally treated with endovascular techniques, including embolization, exclusion with a covered stent graft, or open surgical repair.1,2 According to most recent guidelines, treatment is recommended for an aneurysm diameter of >3.5 cm.1,3,4 Previously excluded IIAAs present a particular challenge. Open endoaneurysmorrhaphy is the classic approach; however, deep pelvic exposure of large aneurysms can be difficult and risky. Other techniques, including direct percutaneous sac puncture and a transgluteal approach through the IIA branches, have also been described.5, 6, 7, 8, 9, 10, 11 In this case series, we describe a hybrid approach with open retroperitoneal cutdown and direct access. All included patients provided written informed consent for the report of their clinical information and related imaging studies.
Case report
Patient 1
An 81-year-old man was referred to our clinic for an asymptomatic, enlarging left IIAA (Fig 1). More than 18 years ago, he underwent open repair of an infrarenal abdominal aortic aneurysm (AAA) with ligation of the proximal left IIA and right aortoiliac and left aortofemoral reconstruction. The patient subsequently underwent fenestrated endovascular repair of an extent II thoracoabdominal aortic aneurysm. On surveillance computed tomography angiography, a left IIAA was noted that was 6.5 cm in diameter with intact retrograde perfusion.
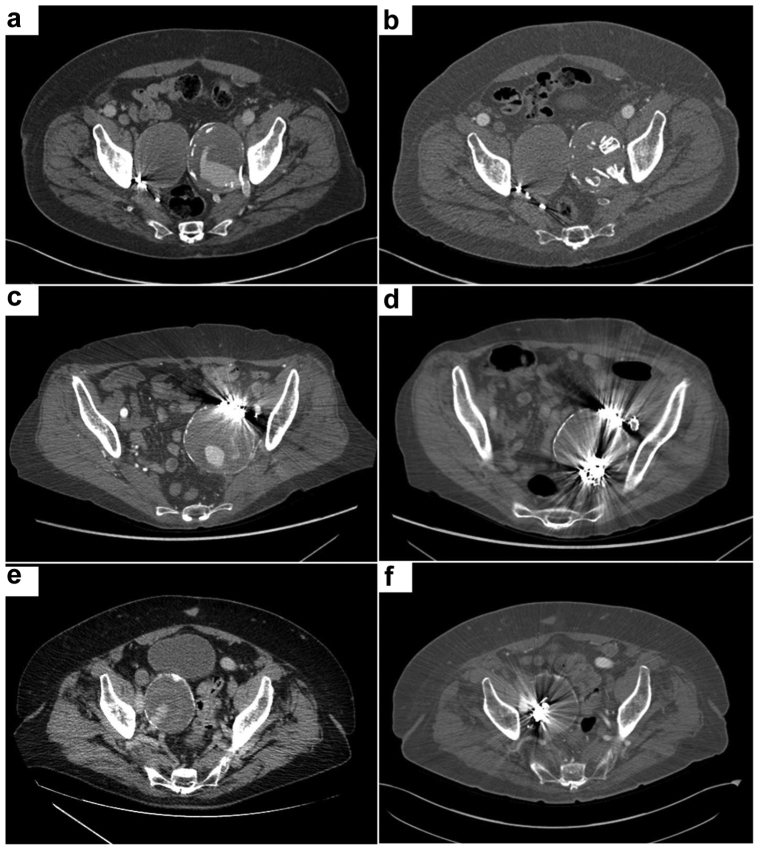
Fig 1.
Preoperative computed tomography angiograms demonstrating large internal iliac artery aneurysms (IIAAs) with retrograde flow in patients 1 (a), 2 (c), and 3 (e). Follow-up computed tomography angiograms demonstrating a stable or reduced size of IIAAs in patients 1 (b), 2 (d), and 3 (f).
Patient 2
A 76-year-old woman was referred to our clinic for pelvic pain in the setting of a 7.0-cm proximally excluded left IIAA and a 5.0-cm separate infrarenal AAA (Fig 1). More than 10 years before, she underwent an attempted endovascular repair of a 4.0-cm left IIAA, with a common iliac artery to external iliac artery stent graft and embolization of the proximal IIA stump. We proceeded with endovascular aortic repair for an infrarenal AAA with simultaneous hybrid repair of the left IIAA.
Patient 3
A 76-year-old man was referred to our clinic with an asymptomatic 6.0-cm right IIAA (Fig 1). He had previously undergone endovascular aortic repair for an infrarenal aortoiliac aneurysm, with coil embolization and coverage of proximal right IIA. On surveillance imaging, the aneurysm sac had expanded to 6.0 cm with intact retrograde perfusion. We proceeded with hybrid repair of the IIAA.
Surgical technique
With the patient under general anesthesia and in a supine position, a limited retroperitoneal incision is made above the inguinal ligament. The dissection is carried down to the abdominal wall, with hemostasis ensured. The external oblique aponeurosis is incised along the direction of its fibers, and the external, internal oblique, and transversus abdominis muscle fibers are spread apart in the direction of their fibers, achieving access directly into the retroperitoneum. With careful dissection, the viscera are mobilized medially, exposing the cephalad portion of the IIAA. The ureter and lumbar plexus are preserved. The proximal part of the IIAA is accessed directly using an 18-gauge access needle with blood aspiration, and an angiogram is performed to confirm placement within the endoleak nidus (Fig 2). A separate stab incision is made over the abdomen just above the access site, and a Rosen guidewire, followed by a 6F, 55-cm sheath, is advanced through the incision into the IIAA (Fig 3). This sheath is then secured to the skin and looped downward, providing the surgeon access to the catheters away from the radiation field. An angiogram is then performed, and all outflow branches are identified. Using a combination of standard 0.035-in. endovascular angled catheters, 0.025- and 0.018-in. microcatheters, and appropriate guidewires, these branches are accessed sequentially and embolized using a combination of detachable and push-able coils. The catheter is then retracted into the aneurysm sac, and coils and plugs of various sizes are used to obliterate the cavity completely. In our patients, a mean of 12 coils (range, 10-14 coils) and 4 plugs (range, 1-9 plugs) were used. Next, completion angiography is performed to confirm full exclusion (Fig 2). The sheath is removed, and the access site is closed using 5-0 Prolene suture. The surgical incision is then closed in a multilayered fashion.
Fig 2.
Angiograms before embolization demonstrating large internal iliac artery aneurysms (IIAAs) with multiple outflow branches in patients 1 (a), 2 (c), and 3 (e). Completion angiograms demonstrating complete exclusion of the aneurysm sac and outflow branches in patients 1 (b), 2 (d), and 3 (f).
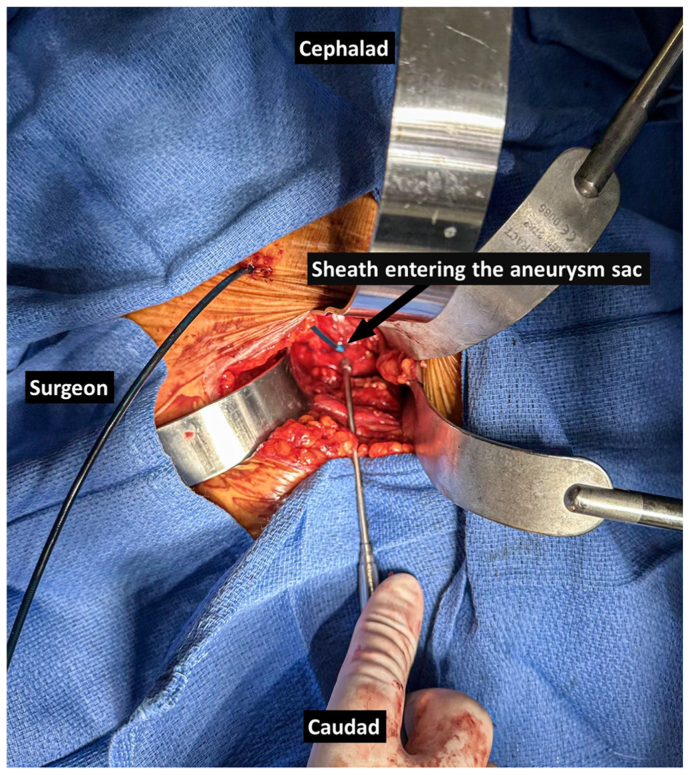
Fig 3.
Intraoperative photograph demonstrating the setup showing a small retroperitoneal incision with the cephalad portion of the aneurysm exposed, a separate stab incision through which the sheath is introduced, and the sheath looped downward to be accessible by the surgeon.
Outcomes
All three patients were followed up in the clinic at 14, 10, and 12 months after treatment, with a minimum of two serial axial imaging studies. Computed tomography angiography showed a stable or shrinking sac size in all three patients and no endoleaks (Fig 1). None of the three patients experienced pelvic ischemic symptoms or buttock claudication.
Discussion
IIAAs are commonly found in association with aortoiliac anerusyms.1,12 The mortality rate of IIAA rupture is reported to be as high as 53%.13 Open endoaneurysmorrhaphy is the conventional approach; however, endovascular treatment is preferred, because it is associated with lower periprocedural morbidity and mortality. With better diagnosis and improved survival after aortoiliac aneurysm repairs, it is not uncommon for isolated IIAs to be encountered in patients previously treated for aortoiliac aneurysms with endovascular or open surgical exclusion of the IIA inflow. In all three of our patients, the IIAA was previously excluded by either stent coverage with embolization of the proximal IIA or ligation during a prior open surgical repair, making it impractical to use an antegrade approach for access.
Historically, exclusion of the IIAA sac has been used as a strategy for smaller localized aneurysms in the proximal portion of the artery. However, multiple case series and retrospective reviews have shown continued expansion of IIAAs after previous exclusion.14,15 This is especially true for IIAAs that extend deep into the pelvis or are larger.12 Our experience also shows that these excluded aneurysms can stay intact to quite a large size, because all three IIAAs in this series were >6 cm. This mechanism can be postulated to be secondary to lower retrograde perfusion pressure. In this rare situation, different techniques have been described previously to achieve access into the aneurysm sac or its feeding vessels. The superior or inferior gluteal artery can be accessed with fluoroscopic guidance or from a buttock incision and can be embolized.5, 6, 7, 8 Alternatively, the IIAA sac can be accessed directly using a percutaneous approach.9, 10, 11 In addition to coils, liquid embolic agents can be used for adequate control of a type II endoleak, especially in cases in which all outflow branches cannot be accessed. These approaches, however, have their own potential limitations, including the risk of damaging critical structures, such as the ureter, lumbar plexus, and viscera, and the inability to embolize all feeding vessels.
A hybrid technique was chosen as the preferred approach for all three of our patients because the surgeons were more comfortable with a minimally morbid retroperitoneal cutdown, direct access of the aneurysm, and endovascular embolization of all feeding vessels and the aneurysm sac. A similar approach has been described for previously excluded hypogastric artery aneurysms.16 We believe that this approach has some potential advantages in specific conditions: (1) all critical structures can be avoided if no clear window is available for direct percutaneous access or a transgluteal approach; and (2) minimal dissection is needed compared with conventional open endoaneurysmorrhaphy. The importance of adequate aneurysmal outflow vessel management at the index operation must be emphasized to avoid continued expansion and possible rupture.
Conclusions
We present a hybrid repair technique for the treatment of previously excluded, expanding IIAAs. This technique provides a safe and effective alternative for patients in whom antegrade endovascular access is impractical. This hybrid approach allows for direct visualization of critical structures, minimizes dissection and blood loss, and ensures successful embolization of all feeding vessels.
Disclosures
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Rana M.A., Kalra M., Oderich G.S., et al. Outcomes of open and endovascular repair for ruptured and nonruptured internal iliac artery aneurysms. J Vasc Surg. 2014;59:634–644. doi: 10.1016/j.jvs.2013.09.060. [DOI] [PubMed] [Google Scholar]
- 2.Ryer E.J., Garvin R.P., Webb T.P., Franklin D.P., Elmore J.R. Comparison of outcomes with coils versus vascular plug embolization of the internal iliac artery for endovascular aortoiliac aneurysm repair. J Vasc Surg. 2012;56:1239–1245. doi: 10.1016/j.jvs.2012.05.001. [DOI] [PubMed] [Google Scholar]
- 3.Perini P., Mariani E., Fanelli M., et al. Surgical and endovascular management of isolated internal iliac artery aneurysms: a systematic review and meta-analysis. Vasc Endovascular Surg. 2021;55:254–264. doi: 10.1177/1538574420981812. [DOI] [PubMed] [Google Scholar]
- 4.Wanhainen A., Verzini F., Van Herzeele I., et al. Editor’s choice – European Society for Vascular Surgery (ESVS) 2019 clinical practice guidelines on the management of abdominal aorto-iliac artery aneurysms. Eur J Vasc Endovasc Surg. 2019;57:8–93. doi: 10.1016/j.ejvs.2018.09.020. [DOI] [PubMed] [Google Scholar]
- 5.Magishi K., Izumi Y., Tanaka K., Shimizu N., Uchida D. Surgical access of the gluteal artery to embolize a previously excluded, expanding internal iliac artery aneurysm. J Vasc Surg. 2007;45:387–390. doi: 10.1016/j.jvs.2006.10.040. [DOI] [PubMed] [Google Scholar]
- 6.Tigkiropoulos K., Lazaridis I., Stavridis K., Tympanidou M., Karamanos D., Saratzis N. Inferior gluteal artery surgical access for embolization of large internal iliac artery aneurysm in a hostile abdomen. J Surg Case Rep. 2019;2019 doi: 10.1093/jscr/rjz098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Werner-Gibbings K., Rogan C., Robinson D. Novel treatment of an enlarging internal iliac artery aneurysm in association with a type 2 endoleak via percutaneous embolisation of the superior gluteal artery through a posterior approach. Case Rep Vasc Med. 2013;2013:1–4. doi: 10.1155/2013/861624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shafique S., Cooke J., Dell K., Flanders V. Transgluteal coil embolization of internal iliac artery aneurysm. J Vasc Surg. 2020;72:e306. [Google Scholar]
- 9.Rogoff P., Stock Percutaneous transabdominal embolization of an iliac artery aneurysm. Am J Roentgenol. 1985;145:1258–1260. doi: 10.2214/ajr.145.6.1258. [DOI] [PubMed] [Google Scholar]
- 10.Kamada K., Koya A., Tochikubo-Suzuki A., Kikuchi S., Uchida D., Azuma N. Successful endovascular therapy involving direct puncture for spontaneous internal iliac artery aneurysm rupture. J Vasc Surg Cases Innov Tech. 2022;8:125–128. doi: 10.1016/j.jvscit.2021.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Worgul C.A., Wu G., Kansal N. Percutaneous access of an expanding internal iliac artery aneurysm via a direct posterior transgluteal approach. Ann Vasc Surg. 2019;55:311.e1–311.e4. doi: 10.1016/j.avsg.2018.07.051. [DOI] [PubMed] [Google Scholar]
- 12.Huang Y., Gloviczki P., Duncan A.A., et al. Common iliac artery aneurysm: expansion rate and results of open surgical and endovascular repair. J Vasc Surg. 2008;47:1203–1211.e2. doi: 10.1016/j.jvs.2008.01.050. [DOI] [PubMed] [Google Scholar]
- 13.Wilhelm B.J., Sakharpe A., Ibrahim G., Baccaro L.M., Fisher J. The 100-year evolution of the isolated internal iliac artery aneurysm. Ann Vasc Surg. 2014;28:1070–1077. doi: 10.1016/j.avsg.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 14.Nakajima T., Kawazoe K., Komoda K., et al. Failure of exclusion of internal iliac artery aneurysms. J Vasc Surg. 2001;33:476–480. doi: 10.1067/mva.2001.111975. [DOI] [PubMed] [Google Scholar]
- 15.Ruurda J.P., Rijbroek A., Vermeulen E.G., Wisselink W., Rauwerda J.A. Continuing expansion of internal iliac artery aneurysms after surgical exclusion of the inflow. A report of two cases. J Cardiovasc Surg. 2001;42:389–392. [PubMed] [Google Scholar]
- 16.Kang N., Bornak A. Hybrid treatment of an enlarging hypogastric aneurysm previously excluded during abdominal aortic aneurysm repair. Ann Vasc Surg. 2020;68:573.e1–573.e3. doi: 10.1016/j.avsg.2020.04.069. [DOI] [PubMed] [Google Scholar]