Abstract
Background
In Indian context, infertility is often a silent struggle. Despite the high prevalence of infertility in the country, the majority of couples do not share their struggles with family or friends due to social stigma, thus increasing their psychological vulnerability. Heartfulness meditation has shown to decrease stress, anxiety, loneliness and improve sleep along with quality of life.
Objectives
The current retrospective series evaluated the effectiveness of Heartfulness-based integrative therapy on infertility outcomes.
Methods
The program consisted of a 5- day onsite lifestyle modification workshop and online follow up meditation sessions.
Results
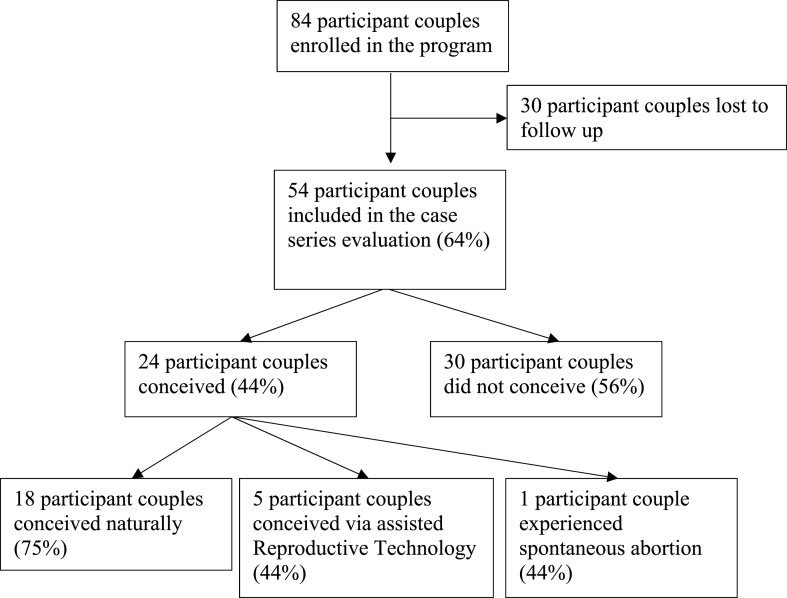
54 couples with infertility participated in the program with a mean age of 30.74 years (SD 5.04) for females and 34.03 years (SD 4.54) for males. 15 couples presented with male infertility, 16 couples presented with female infertility and in 5 couples both partners had infertility problems. Further, 18 couples had unexplained infertility. 24 couples conceived with 18 natural conceptions, five via assisted reproductive technology and one spontaneous abortion.
Conclusion
The program was beneficial in the cohort who utilized it as prescribed resulting in conception of 24 out of 54 couples. Future research investigating the causal relationship of Heartfulness meditation on fertility outcomes in a randomized control study could solidify this treatment method to be used independently or as an adjuvant therapy with assisted reproductive technologies.
Keywords: Anxiety and stress management, Assisted reproductive technology, Heartfulness, Infertility, Integrative practices, Lifestyle modification, Meditation
1. Introduction
Infertility is the inability to conceive within one year of unprotected intercourse and is identified as a public health issue due to dramatically rising infertility rates in the recent decade [1]. Globally, infertility affects up to 15% of couples of reproductive age [2,3]. The National Survey of Family Growth estimated 6% of couples experience infertility issues in the United States [4]. By contrast, among couples of reproductive age in India, prevalence of infertility ranged between 4% to as high as 17% [5,6]. Infertility in male, female or both partners may occur due to a combination of factors attributed to genetic, environmental, infectious diseases and dietary choices [7]. The incidence of infertility among couples is associated with lifestyle factors, stress, postponing parenthood and obesity [[8], [9], [10]]. Moreover, the inability to have children also causes significant emotional and psychological distress with patients reporting feelings of depression, stress, anxiety, isolation, and loss of control. Interestingly, studies have reported the prevalence of anxiety among infertile couples to be similar or higher to patients diagnosed with HIV-positive, cancer, heart diseases, or other serious life-threatening chronic diseases [11].
The rapid evolution of assisted reproduction technology (ART) has overcome numerous seemingly insurmountable barriers to allow couples the chance to have families [12]. Significant development in the past decades has led to greater efficiency and acceptability of these types of treatment methods [12,13]. India currently has one of the highest growth of ART centers and the number of ART cycles performed every year [14]. Despite the successes and advances, the higher costs of the treatment is a significant barrier to access ART and is often considered a luxury service [15,16]. Additionally, the social stigma, costs, safety and uncertainty associated with biomedical treatments often entice those who are having problems conceiving to use.
Complementary or alternative medicine (CAM) as a first line of treatment before engaging in ART [17,18], or as an adjuvant therapy can be used to manage stress, anxiety and other emotional distress associated with medically invasive treatments [19].
One of the popular CAM methods is meditation. Meditation is shown to promote hormone balance, helping conception while also decreasing stress, management of anxiety and depressive symptoms and an improved quality of life among couples with infertility [[18], [19], [20], [21]]. The primary objective of this case series was to provide preliminary data for a novel, integrated Heartfulness Meditation program to enhance conception rates and provide emotional stability among couples with infertility.
1.1. Background on Heartfulness meditation
Heartfulness meditation system is based on Raja Yoga, a form of yogic practice, first described by Indian philosopher, Patanjali Maharishi, in the classic text, Yoga Sutras, which is widely acknowledged as the authoritative text on yoga [22]. In Yoga Sutras, Patanjali outlines an eightfold path to awareness and self-realization called ashtanga (eight limbs) [23]. The eight limbs consist of ethical principles for living a meaningful and purposeful life; serving as a prescription for moral, ethical conduct and self-discipline, they direct attention towards one's health while acknowledging the spiritual aspects of one's nature [24]. Based on Patanjali's ashtanga principles, many different yogic systems have been developed, with each discipline having its own method of enhancing physical and mental health. One such technique is the Heartfulness Meditation. It is a simple heart-based meditation system aimed at attaining a balanced state of mind and has previously shown to improve physical health, psychological health, burn out, sleep quality, and loneliness [[25], [26], [27], [28]].
While Heartfulness meditation formed the core practice of the current intervention, several other elements of CAM including yoga, nutrition, exercise among others were incorporated to supplement the current approach based on the abundant literature supporting the techniques. Yogic systems emphasize controlled breathing (pranayama), body postures (asanas), relaxation of mind-body (meditation, polarity) and a sattvic diet (plant-based nutrition) for treatment of diseases through lifestyle modifications [29]. Yoga therapies have found to improve reproductive functions both in men and women by improving the overall integration of physiological systems - primarily known to reduce urinary excretion of catecholamines and aldosterone, decrease serum testosterone and luteinizing hormone (LH) levels in women and increase cortisol excretion, inducing optimal changes in hormonal profiles [[30], [31], [32]]. Further, alterations in brain waves (specifically alpha waves) and decrease in serum cortisol level was observed during yoga therapy [30]. Similarly, there is strong evidence suggesting healthy preconception dietary and lifestyle patterns among men and women to have a beneficial effect on ovulatory disorders and sperm quality [[33], [34], [35]].
2. Materials and methods
2.1. Study design
This is a retrospective case series conducted at the Heartfulness Institute, Kanha Shantivanam, Hyderabad, India, between December 2018–January 2020. Kanha Shantivanam is the international headquarters of the Heartfulness Institute, a 1400-acre meditation retreat center for promoting personal inner experiences, health and wellness.
2.2. Recruitment
Electronic communication channels were the main form of recruitment to the program. Information about the program was disseminated through email correspondence and newsletters. Interested participants were provided with a link to learn more about the program, obtain consent and register voluntarily. Inclusion criteria were couples that were: 1) above 18 years of age, 2) interested in parenthood, 3) Couples who had been actively trying to conceive for more than one year and, 4) Availability of at least one of the partners for the onsite workshop. Further, participants with self reported mental illness, unwilling to participate in meditation sessions or unable to travel on-site to the workshop were excluded from the program.
CONSORT flow chart outlines enrollment of participants (Fig. 1).
Fig. 1.
Participant flow chart.
This case series was an evaluation of a program for infertility offered by the Heartfulness Institute and is thus reported as a program evaluation project. Thus, exempted from ethics approval. Furthermore, all participants provided consent to participate in the program.
2.3. Intervention
The intervention consisted of two main components: A) A 5-day onsite lifestyle modification workshop, followed by B) Weekly online meditation sessions during follow-up period.
2.3.1. 5-day lifestyle modification workshop
The workshop was facilitated and delivered by certified trainers with a background in obstetrics and gynecology, physiotherapy, primary care, yoga, nutrition, and other allied health services. Enrolled participants received a ‘starter kit’ email consisting of information on the 5-day workshop schedule at Kanha Shantivanam, Hyderabad. All participants received program collateral including a book on meditation, booklet on fertility, 90 day journal, and other supplies such as affirmation cards, activity sheets and notepads needed for the program period. Participants were responsible to arrange for their own travel to the center. Furthermore, participants were given an option to voluntarily donate to the program to cover costs associated with program care plans. The 5-day workshop included an intensive lifestyle modification program comprising of: 1) 12 h of individual meditation sessions and 10 h of group meditation sessions; 2) 5 h of Yoga; 2) 2.25 h of polarity therapy sessions (Polarity is a CAM technique to influence energy flow and balance); 4) 1 h of nutrition coaching; 5) 1 h of breathing exercise guidance; 6) 5 h of personal coaching, 7) 5 h of self-reflection, positive affirmation, visualization techniques, gratitude practices and journaling activity and, 8) 1 h of nature walk per day.
2.3.2. Heartfulness meditation sessions
Meditation sessions were delivered by certified Heartfulness meditation trainers. Trainers were experienced meditators who received specialized training to conduct the program and were certified through the Heartfulness Institute. All participants received a 40–45 min guided meditation per session from certified Heartfulness meditation trainers with the following instructions.
-
1.
Please sit comfortably and breathe normally. Gently close your eyes
-
2.
Now move your attention to your toes. Wiggle them a little and allow your toes to relax.
-
3.
Feel a very relaxing energy entering your feet from the ground allowing your feet to relax.
-
4.
Let this energy slowly move up, relaxing your ankles, lower legs, calf muscles, your knees, upper legs, and your hips. Feel all these parts completely relaxed.
-
5.
Allow this energy to slowly move up, relaxing your lower back and your upper back. Feel your entire back relaxed.
-
6.
Slowly move your attention to your stomach area and allow all the muscles to relax.
-
7.
Now, let the energy move up into your chest and let your chest deeply relax.
-
8.
Move your attention on to your shoulders and feel as if they are melting away.
-
9.
Let this energy slowly move into your upper arms, elbows, lower arms, hands and your fingers. Feel them completely relaxed.
-
10.
Slowly move your attention to your neck and allow your neck muscles to relax.
-
11.
Gently loosen your jaw and allow your chin and all the muscles of the face to relax. Your lips and your eyes are relaxing. Relax your forehead.
-
12.
Gently move into your mind and allow your mind to deeply and completely relax. Relax the top of your head.
-
13.
Gently scan your whole body from the top of your head to the tips of your toes and feel your entire body relaxed.
-
14.
Now gently move into your heart and settle in there. Rest your attention on the source of light that is already present within. Do this in a very gentle and natural way.
-
15.
Rather than trying to visualize this, participants were asked to simply tune in to their hearts and be open to any experience that they may have. If their mind wandered, participants were advised to gently redirect towards the heart.
Yoga asanas were administered by certified yoga instructors and included pranayama (breathing exercise), surya namaskar (sun salutation), Badhakonasana (butterfly pose), marjari asana (cat pose), parvatasana (mountain pose), shashankasana (hare pose) among others.
2.3.3. Weekly online meditation during follow-up period
Following the on-site workshop, each participating couple were introduced to a meditation trainer to transition to virtual follow up every week for meditation sessions. Meditation techniques were the same for both onsite workshop and virtual follow up period. Trainers coordinated for meditation sessions every week over phone and shared meeting links over Zoom platform to join the virtual meditation session. Individual meditation sessions continued until the participant couple conceived or up to 2 years of the program, whichever was the earliest. For any questions related to the program or intervention, the last 10 min of every meditation session was reserved for clarifications with trainers. Furthermore, collaterals received during the onsite workshop served as a guide to continue practice in the follow up period. Additionally, trainers closely monitored participants to ensure both partners received the intervention and recorded attendance of each session. Participants continued their usual medical care under their respective physicians throughout the program period.
2.4. Primary outcome measures
The outcomes of interest for each participant were clinical outcome (as assessed through conception rate within 24 months) and engagement (measured as proportion of participants completing the program as prescribed).
2.5. Data analysis
Retrospective case-note review and analysis using electronic participant data were performed. The case note review allowed gathering of information on demographic, diagnosis history by program coordinators before enrolling participants. Person identifiers were not used in the analysis. Mean percentages and standard deviations were used to summarize numerical and categorical variables. Univariate analysis to assess for clinical characteristics, program engagement rates and conception rates were performed using STATA v16.1 (College Station, TX: StataCorp LLC).
3. Results
3.1. Cohort description
Eighty-four couples registered to the program and 54 met inclusion criteria for the case series evaluation providing baseline and follow up measures. Table 1 presents the demographic and clinical characteristics of these 54 couples. The mean age for females was 30.74 years (SD 5.04), while that of the male was 34.03 years (SD 4.54). The average marital duration was 5.29 years (SD 3.15) with couples reporting an average time of 2.6 years (SD 1.6) seeking fertility treatments to aid in conception. Fifteen couples (n = 15) presented with male infertility, sixteen couples (n = 16) presented with female infertility and in five couples (n = 5) both partners had infertility problems. Further, eighteen couples (n = 18) had unexplained infertility. Majority of male infertility stemmed from a diagnosis of oligospermia (n = 16), followed by azoospermia (n = 3). The most common causes for female infertility were polycystic ovarian syndrome (n = 10) and tubal defects (n = 4).
Table 1.
Participant demographics and clinical characteristics.
| Characteristic | Mean (SD) |
|---|---|
| Women age (years) | 30.74 (5.04) |
| Men age (years) | 34.03 (4.54) |
| Marital duration (years) | 5.29 (3.15) |
| Time in Infertility care | 2.6 (1.6) |
| History of Infertility | |
| Male factor | 15 |
| Female factor | 16 |
| Both partners with infertility problem | 5 |
| Do not know/unexplained infertility | 18 |
| Male Factors (n = 20) | |
| Oligospermia | 16 |
| Azoospermia | 3 |
| Oligoasthenospermia | 1 |
| Female Factors (n = 21) | |
| PCOS | 10 |
| Tubal defect | 4 |
| Irregular menstrual cycle | 2 |
| Fibroids | 1 |
| Endometrial polyps | 1 |
| Depression | 1 |
| Gene Defect | 1 |
| History of failed IVF | 1 |
3.2. Engagement outcomes
Of the 84 couples registered, 54 couples completed the program with 30 couples lost to follow-up As participants enrolled to the program on a rolling basis, four onsite workshops were conducted during the program period (Table 2).
Table 2.
Engagement outcomes.
| Results | n |
|---|---|
| Number of participants registered for the program | 84 |
| Number of participants completing the program | 54 |
| Lost to follow up | 30 |
| Number of onsite workshops | 4 |
| Participants in workshop 1 | 36 |
| Participants in workshop 2 | 7 |
| Participants in workshop 3 | 6 |
| Participants in workshop 4 | 5 |
3.3. Conception
In the present population, 24 out of 54 participant couples conceived. Majority of couples (n = 18 conceived naturally and five couples through ART (n = 5). Further, 6 couples conceived within 6 months of participation in the program and 11 couples conceived within 12 months of participation while 7 couples had conception from 13th month through 24 months (Table 3). Couples with unexplained infertility had the highest rate for conception (n = 10), followed by oligospermia (n = 4) and PCOS (n = 2). No adverse effects (such as ectopic pregnancy or psychological changes) were recorded during the program period.
Table 3.
Conception results.
| Results | n |
|---|---|
| Number of couples conceived | 24 |
| Number of couples that did not conceive | 30 |
| Modality of conception | |
| Natural | 18 |
| In Vitro Fertilization | 4 |
| Intrauterine Insemination | 1 |
| Spontaneous abortion | 1 |
| Conception Results by Diagnosis | |
| Unexplained infertility | 10 |
| Oligospermia | 4 |
| Oligospermia & PCOS | 2 |
| PCOS | 2 |
| Tubal defect | 2 |
| Depression | 1 |
| Endometrial polyps | 1 |
| Oligoasthenospermia | 1 |
| History of failed IVF | 1 |
4. Discussion
The case series is one of the first reports on Heartfulness meditation based integrative therapy for infertility treatment. Program engagement rates and whether pregnancy was achieved were examined and provided a baseline for future research on this CAM technique. The cohort achieved a 44% conception rate comparing favorably to other CAM techniques typically ranging between 28% and 45% [36,37]. Findings from the current program evaluation concur with prior literature on similar lifestyle modification based integrative studies inferring a positive effect of incorporating CAM to enhance fertility with an average effect size between 0.35 and 0.82 for psychological variables [38,39]. Notably, in the present findings, majority of conception occurred naturally which is a distinct feature of this case series report as compared to prior studies that mostly evaluated CAM techniques as an adjuvant treatment for assisted reproductive technologies [40,41]. Given that participating couples reported an average time of 2.6 years (SD 1.6) spent in seeking fertility treatments prior to participation in the program, majority of conceptions occurring naturally through this intervention is an important finding of this case series evaluation. Furthermore, the engagement rate with the program was acceptable with 64% participation over the period of two years. Given the high variability in ART discontinuation rates reported in prior research, ranging from 15% to 65% [42,43], the acceptable engagement rate in this case series suggests that participants are motivated to use CAM methods to enhance chances of conception. Our findings concur with work of others that demonstrated the key reasons to use CAM were to enhance conception rates, develop emotional resilience while seeking fertility care, minimize invasive medical treatments among others [40,44].
An important limitation of this retrospective case series research design is its inherent selection bias lacking generalizability of the results to a larger population of patients. The participants self-selected themselves to the program. Additionally, the protocol was based on integrative therapy involving principles of nutrition, exercise, polarity and meditation. As the case series was an evaluation of a program for infertility offered by the Heartfulness Institute, and hence, reported as a program evaluation project. Moreover, the program did not restrict participants from continuing their medical care or using medication therapy for their infertility while participating in the program, as such the exclusive effect of meditation is difficult to ascertain. The program was offered as an integrative approach to have the availability of the current standard of care available to the participants without any restriction.
5. Conclusion
The findings provide preliminary evidence that Heartfulness Meditation based integrative therapy to be a safe and viable treatment option for couples with infertility and should be investigated further. The program was beneficial in the cohort who utilized it as prescribed. Therefore, future research investigating the causal relationship of Heartfulness Meditation on fertility outcomes in a randomized controlled study could solidify this treatment method to be used independently or as an adjuvant therapy for assisted reproductive technologies.
Funding details
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
The authors gratefully acknowledge the support of Dr. Veronique Nicolai, Ms. Sarojini, Mrs Abirami J, of Heartfulness Institute in development and management of the infertility program.
Footnotes
Peer review under responsibility of Transdisciplinary University, Bangalore.
References
- 1.Warner L., Jamieson D.J., Barfield W.D. CDC releases a national public health action plan for the detection, prevention, and management of infertility. J Womens Health (Larchmt). 2015;24(7):548–549. doi: 10.1089/jwh.2015.5355. [DOI] [PubMed] [Google Scholar]
- 2.Cui W. Mother or nothing: the agony of infertility. Bull World Health Organ. 2010;88(12):881–882. doi: 10.2471/BLT.10.011210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poongothai J., Gopenath T.S., Manonayaki S. Genetics of human male infertility. Singap Med J. 2009;50(4):336–347. PMID: 19421675. [PubMed] [Google Scholar]
- 4.Sun H., Gong T.T., Jiang Y.T., Zhang S., Zhao Y.H., Wu Q.J. Global, regional, and national prevalence and disability-adjusted life-years for infertility in 195 countries and territories, 1990-2017: results from a global burden of disease study. Aging (Albany NY) 2017;11(23):10952–10991. doi: 10.18632/aging.102497. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katole A., Saoji A.V. Prevalence of primary infertility and its associated risk factors in urban population of Central India: a community-based cross-sectional study. Indian J Community Med. 2019;44(4):337–341. doi: 10.4103/ijcm.IJCM_7_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganguly S., Unisa S. Trends of infertility and childlessness in India: findings from NFHS data. Facts Views Vis Obgyn. 2010;2(2):131–138. [PMC free article] [PubMed] [Google Scholar]
- 7.Sarkar S., Gupta P. Socio-demographic correlates of women's infertility and treatment seeking behavior in India. J Reproduction Infertil. 2016;17(2):123–132. PMID: 27141468; PMCID: PMC4842234. [PMC free article] [PubMed] [Google Scholar]
- 8.Bala R., Singh V., Rajender S., Singh K. Environment, lifestyle, and female infertility. Reprod Sci. 2021;28(3):617–638. doi: 10.1007/s43032-020-00279-3. [DOI] [PubMed] [Google Scholar]
- 9.Yilmaz N., Kilic S., Kanat-Pektas M., Gulerman C., Mollamahmutoglu L. The relationship between obesity and fecundity. J Womens Health (Larchmt). 2009;18(5):633–636. doi: 10.1089/jwh.2008.1057. [DOI] [PubMed] [Google Scholar]
- 10.Schmidt L., Sobotka T., Bentzen J.G., Nyboe Andersen A. Demographic and medical consequences of the postponement of parenthood. Hum Reprod Update. 2012;18(1):29–43. doi: 10.1093/humupd/dmr040. [DOI] [PubMed] [Google Scholar]
- 11.Kainz K. The role of the psychologist in the evaluation and treatment of infertility. Wom Health Issues. 2001;11(6):481–485. doi: 10.1016/s1049-3867(01)00129-3. [DOI] [PubMed] [Google Scholar]
- 12.Wang J., Sauer M.V. In vitro fertilization (IVF): a review of 3 decades of clinical innovation and technological advancement. Therapeut Clin Risk Manag. 2006;2(4):355–364. doi: 10.2147/tcrm.2006.2.4.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sharma R.S., Saxena R., Singh R. Infertility & assisted reproduction: a historical & modern scientific perspective. Indian J Med Res. 2018;148(Suppl):S10–S14. doi: 10.4103/ijmr.IJMR_636_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Malhotra N., Shah D., Pai R., Pai H.D., Bankar M. Assisted reproductive technology in India: a 3 year retrospective data analysis. J Hum Reprod Sci. 2013;6(4):235–240. doi: 10.4103/0974-1208.126286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Darvishi A., Goudarzi R., Zadeh V.H., Barouni M. Cost-benefit Analysis of IUI and IVF based on willingness to pay approach; case study: Iran. PLoS One. 2020;15(7) doi: 10.1371/journal.pone.0231584. 2020 Jul 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kalampokas T., Botis S., Kedikgianni-Antoniou A., Papamethodiou D., Kivellos S., Papadimitriou V., et al. Homeopathy for infertility treatment: a case series. Clin Exp Obstet Gynecol. 2014;41(2):158–159. [PubMed] [Google Scholar]
- 17.Rayner J.A., McLachlan H.L., Forster D.A., Cramer R. Australian women's use of complementary and alternative medicines to enhance fertility: exploring the experiences of women and practitioners. BMC Compl Alternative Med. 2009;9:52. doi: 10.1186/1472-6882-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Perry T.E., Hirshfeld-Cytron J. Role of complementary and alternative medicine to achieve fertility in uninsured patients. Obstet Gynecol Surv. 2013;68(4):305–311. doi: 10.1097/OGX.0b013e318286f780. [DOI] [PubMed] [Google Scholar]
- 19.Balk J., Catov J., Horn B., Gecsi K., Wakim A. The relationship between perceived stress, acupuncture, and pregnancy rates among IVF patients: a pilot study. Compl Ther Clin Pract. 2010;16(3):154–157. doi: 10.1016/j.ctcp. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Galhardo A., Cunha M., Pinto-Gouveia J. Mindfulness-based program for infertility: efficacy study. Fertil Steril. 2013;100:1059–1067. doi: 10.1016/j.fertnstert.2013.05.036. [DOI] [PubMed] [Google Scholar]
- 21.Smith J.F., Eisenberg M.L., Millstein S.G., Nachtigall R.D., Shindel A.W., et al. The use of complementary and alternative fertility treatment in couples seeking fertility care: data from a prospective cohort in the United States. Fertil Steril. 2010;93:2169–2174. doi: 10.1016/j.fertnstert.2010.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chaudhry N., Bhandari R.B., Gaur V. Yoga perspective on personal excellence and well-being. J Ayurveda Integr Med. 2023;14(3) doi: 10.1016/j.jaim.2023.100717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Varambally S., Gangadhar B.N. Current status of yoga in mental health services. Int Rev Psychiatr. 2016;28(3):233–235. doi: 10.3109/09540261.2016.1159950. [DOI] [PubMed] [Google Scholar]
- 24.Woodyard C. Exploring the therapeutic effects of yoga and its ability to increase quality of life. Int J Yoga. 2011;4(2):49–54. doi: 10.4103/0973-6131.85485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Thimmapuram T., Pargament R., Sibliss K., Grim R., Risques R., Toorens E. Effect of heartfulness meditation on burnout, emotional wellness, and telomere length in health care professionals. J Community Hosp Intern Med Perspect. 2007;7(1):21–27. doi: 10.1080/20009666.2016.1270806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arya N.K., Singh K., Malik A., Mehrotra R. Effect of Heartfulness cleaning and meditation on heart rate variability. Indian Heart J. 2018;70(Suppl 3):S50–S55. doi: 10.1016/j.ihj.2018.05.004. Suppl 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iyer R.B., Iyer B.N. The impact of heartfulness-based elective on middle school students. Am J Health Behav. 2019;43(4):812–823. doi: 10.5993/AJHB.43.4.14. [DOI] [PubMed] [Google Scholar]
- 28.Van't Westeinde A., Patel K.D. Heartfulness meditation: a yogic and neuroscientific perspective. Front Psychol. 2022;13 doi: 10.3389/fpsyg.2022.806131. 2022 May 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sengupta P. Health impacts of yoga and pranayama: a state-of-the-art review. Int J Prev Med. 2012;3(7):444–458. [PMC free article] [PubMed] [Google Scholar]
- 30.Sengupta P., Chaudhuri P., Bhattacharya K. Male reproductive health and yoga. Int J Yoga. 2013 Jul;6(2):87–95. doi: 10.4103/0973-6131.113391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sengupta P. Challenge of infertility: how protective the yoga therapy is? Ancient Sci Life. 2012;32(1):61–62. doi: 10.4103/0257-7941.113796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Gaskins A.J., Chavarro J.E. Diet and fertility: a review. Am J Obstet Gynecol. 2018;218(4):379–389. doi: 10.1016/j.ajog.2017.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chavarro J.E., Rich-Edwards J.W., Rosner B.A., Willett W.C. Diet and lifestyle in the prevention of ovulatory disorder infertility. Obstet Gynecol. 2007;110(5):1050–1058. doi: 10.1097/01.AOG.0000287293.25465.e1. [DOI] [PubMed] [Google Scholar]
- 34.Panth N., Gavarkovs A., Tamez M., Mattei J. The influence of diet on fertility and the implications for public health nutrition in the United States. Front Public Health. 2018;6:211. doi: 10.3389/fpubh.2018.00211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mumford S.L., Johnstone E., Kim K., Ahmad M., Salmon S., Summers K., et al. A prospective cohort study to evaluate the impact of diet, exercise, and lifestyle on fertility: design and baseline characteristics. Am J Epidemiol. 2020;189(11):1254–1265. doi: 10.1093/aje/kwaa073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Manheimer E., Zhang G., Udoff L., Haramati A., Langenberg P., Berman B.M., et al. Effects of acupuncture on rates of pregnancy and live birth among women undergoing in vitro fertilisation: systematic review and meta-analysis. BMJ. 2008;336(7643):545–549. doi: 10.1136/bmj.39471.430451.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wu X., Stener-Victorin E., Kuang H., et al. Effect of acupuncture and clomiphene in Chinese women with polycystic ovary syndrome: a randomized clinical trial. JAMA. 2017;317(24):2502–2514. doi: 10.1001/jama.2017.7217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dumbala S., Bhargav H., Satyanarayana V., et al. Effect of yoga on psychological distress among women receiving treatment for infertility. Int J Yoga. 2020;13(2):115–119. doi: 10.4103/ijoy.IJOY_34_19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Homan G.F., Davies M., Norman R. The impact of lifestyle factors on reproductive performance in the general population and those undergoing infertility treatment: a review. Hum Reprod Update. 2007;13(3):209–223. doi: 10.1093/humupd/dml056. [DOI] [PubMed] [Google Scholar]
- 40.Smith J.F., Eisenberg M.L., Millstein S.G., et al. The use of complementary and alternative fertility treatment in couples seeking fertility care: data from a prospective cohort in the United States. Fertil Steril. 2010;93(7):2169–2174. doi: 10.1016/j.fertnstert.2010.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Li J., Long L., Liu Y., He W., Li M. Effects of a mindfulness-based intervention on fertility quality of life and pregnancy rates among women subjected to first in vitro fertilization treatment. Behav Res Ther. 2016;77:96–104. doi: 10.1016/j.brat.2015.12.010. [DOI] [PubMed] [Google Scholar]
- 42.Brandes M., van der Steen J.O.M., Bokdam S.B., Hamilton C.J.C.M., de Bruin J.P., Nelen W.L.D.M., et al. When and why do subfertile couples discontinue their fertility care? A longitudinal cohort study in a secondary care subfertility population. Hum Reprod. 2009;24:3127–3134. doi: 10.1093/humrep/dep340. [DOI] [PubMed] [Google Scholar]
- 43.Rajkhowa M., McConnell A., Thomas G.E. Reasons for discontinuity of IVF treatment: a questionnaire study. Hum Reprod. 2006;21:358–363. doi: 10.1093/humrep/dei355. [DOI] [PubMed] [Google Scholar]
- 44.Van Balen F., Verdurmen J., Ketting E. Choices and motivations of infertile couples. Patient Educ Counsel. 1997;31(1):19–27. doi: 10.1016/s0738-3991(97)01010-0. [DOI] [PubMed] [Google Scholar]