Abstract
This cross-sectional study examines antibiotic exposure, days of therapy, types of antibiotics, and changes in use patterns among newborns in neonatal intensive care units (NICUs) across the US from 2009 to 2021.
Antibiotic stewardship interventions leading to reductions in antibiotic use in neonatal intensive care units (NICUs) have been reported for individual centers.1,2,3 The uptake of and opportunities for antibiotic stewardship in the larger NICU population, however, have not been well documented. The objective of this study was to assess trends in antibiotic use across a large cohort of infants who were admitted to US academic and community NICUs over a 13-year period.
Methods
This repeated cross-sectional cohort study used the Premier Healthcare Database. The Children’s Hospital of Philadelphia Institutional Review Board deemed this study exempt from ethics review and waived the informed consent requirement owing to the deidentified nature of the data. We followed the STROBE reporting guideline.
Inclusion criteria were birth from January 1, 2009, to December 31, 2021, with admission to the NICU at the same facility as the birth. Antibiotic exposure was a charge for at least 1 dose of parenteral antibiotic. Days of therapy (DOT) were aggregate antibiotic days per 1000 patient-days, accounting for each antibiotic administered on a given day. Outcomes were changes from 2009 to 2021 in the proportion of infants with antibiotic exposure and DOT per 1000 patient-days. Absolute and relative differences in the proportion of infants with antibiotic exposure, exposure to specific antibiotics, and DOT were calculated. Generalized linear regression was used to estimate mean annual absolute differences from 2009 to 2021 in the proportion of infants with antibiotic exposure and annual relative difference in DOT; both models accounted for clustering by NICU.
Two-sided P < .05 indicated statistical significance. Statistical analyses were performed using SAS, version 9.4 (SAS Institute). Further details are described in the eMethods in Supplement 1.
Results
The analysis included 1 395 791 infants (763 498 males [54.7%], 632 293 females [45.3%]) from 735 NICUs (1424 NICUs exist nationally4). Most NICUs were urban (571 [77.7%]) and nonteaching (482 [65.6%]), and the median (IQR) length of stay was 5 (3-13) days. Median (IQR) number of infants contributed per center per year was 146 (48-307) and did not change over the study period.
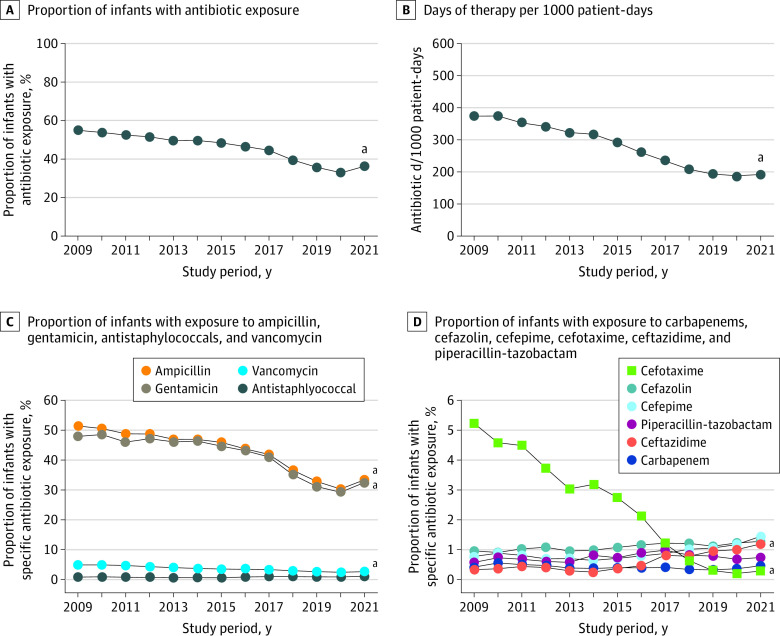
Overall, 44.8% of infants in NICUs received antibiotics. The most common antibiotics prescribed during the study were ampicillin, gentamicin, vancomycin, and cefotaxime. The proportion of infants receiving antibiotics decreased from 54.8% in 2009 to 35.9% in 2021, a 34.4% relative reduction, with an annual absolute difference of −1.9% (95% CI, −2.6% to −1.3%; P < .001) (Table; Figure). Overall, DOT were 274 per 1000 patient-days and decreased from 374 in 2009 to 192 in 2021, a 48.7% relative reduction, with an annual relative difference of −6.9% (95% CI, −8.1% to −5.7%; P < .001) (Table; Figure). The most significant reductions were for ampicillin and gentamicin, which had relative reductions of −35.0% and −32.3%, respectively, and with an annual absolute differences of −1.9% and −1.8%, respectively. Vancomycin use decreased by half during the study, cefotaxime use declined by almost 20-fold, and ceftazidime use increased by 5-fold. There were no significant annual changes for cefazolin, cefepime, piperacillin-tazobactam, antistaphylococcal penicillins, or carbapenems (Table; Figure).
Table. Antibiotic Use Trends Among 1 395 791 Infants Admitted to Neonatal Intensive Care Units From 2009 to 2021.
| Antibiotic use, No. (%)a | Absolute difference, %b,a | Relative difference, %c,a | Annual absolute or relative difference (95% CI), %d,a | P value | |||
|---|---|---|---|---|---|---|---|
| Overall | 2009 | 2021 | |||||
| DOTe,a | 273.7 | 373.6 | 191.6 | −181.9 | −48.7 | −6.9 (−8.1 to −5.7) | <.001 |
| Any antibiotic | 625 208 (44.8) | 36 021 (54.8) | 32 931 (35.9) | −18.9 | −34.4 | −1.9 (−2.6 to −1.3) | <.001 |
| Ampicillin | 591 421 (42.4) | 33 858 (51.5) | 30 674 (33.4) | −18.0 | −35.0 | −1.9 (−2.5 to −1.3) | <.001 |
| Gentamicin | 572 145 (41.0) | 31 564 (48.0) | 29 840 (32.5) | −15.5 | −32.3 | −1.8 (−2.3 to −1.2) | <.001 |
| Vancomycin | 49 905 (3.6) | 3233 (4.9) | 2429 (2.6) | −2.3 | −46.8 | −0.2 (−0.3 to −0.1) | <.001 |
| Cefotaxime | 31 368 (2.2) | 3444 (5.2) | 261 (0.3) | −5.0 | −95.5 | −0.4 (−0.5 to −0.3) | <.001 |
| Cefazolin | 15 379 (1.1) | 632 (1.0) | 1172 (1.3) | 0.3 | 31.2 | 0.03 (−0.004 to 0.06) | .09 |
| Cefepime | 12 421 (0.9) | 508 (0.8) | 1325 (1.4) | 0.7 | 90.6 | 0.04 (−0.05 to (0.1) | .39 |
| Ceftazidime | 8414 (0.6) | 217 (0.3) | 1092 (1.2) | 0.9 | 272.7 | 0.06 (0.02 to 0.1) | .001 |
| Piperacillin-tazobactam | 10 463 (0.7) | 377 (0.6) | 677 (0.7) | 0.2 | 34.9 | 0.02 (−0.02 to 0.05) | .34 |
| Antistaphylococcalf | 11 670 (0.8) | 550 (0.8) | 1027 (1.1) | 0.3 | 35.9 | 0.02 (−0.01 to 0.06) | .22 |
| Carbapenemg | 5687 (0.4) | 274 (0.4) | 422 (0.5) | 0.04 | 9.6 | −0.01 (−0.03 to 0.01) | .44 |
Abbreviation: DOT, days of therapy.
All proportions and DOT values were rounded to 1 significant decimal place. The absolute and relative differences were calculated using the respective values before rounding and were then rounded to 1 significant decimal place.
Absolute difference calculated as 2009 value subtracted from 2021 value.
Relative difference calculated as absolute difference divided by 2009 value.
Generalized linear regression was used to estimate annual absolute or relative difference with 95% CI and P value, accounting for clustering by neonatal intensive care unit. Annual relative difference of antibiotic days per patient-days was reported for DOT, whereas annual absolute difference of proportion of infants with antibiotic exposure during admission was reported for antibiotic exposure.
DOT were defined as antibiotic days/1000 patient-days.
Antistaphylococcal includes nafcillin and/or oxacillin.
Carbapenem includes meropenem, ertapenem, imipenem, and/or doripenem.
Figure. Trends of Antibiotic Use Among Infants Admitted to Neonatal Intensive Care Units From 2009 to 2021.
aStatistically significant absolute or relative annual change.
Discussion
This cross-sectional study of daily pharmacy charge data from almost 1.4 million infants who were admitted to 735 NICUs found that overall antibiotic use declined substantially over time, primarily because of reductions in ampicillin and gentamicin. These findings likely reflect the penetration of national calls for neonatal antibiotic stewardship efforts and refined early-onset infection risk-assessment strategies.5,6 Nationwide shortage and subsequent discontinuation of cefotaxime likely played a role in the drastic decline in cefotaxime use and the concomitant increase in ceftazidime use.
A study strength was the large cohort of NICU infants from both academic and community hospitals across all US regions over a contemporary 13-year period. Limitations were inclusion of only newborns who were admitted to the NICU and unavailable antibiotic indications and microbiology data.
eMethods. Supplemental Methods
Data Sharing Statement
References
- 1.Garber SJ, Dhudasia MB, Flannery DD, Passarella MR, Puopolo KM, Mukhopadhyay S. Delivery-based criteria for empiric antibiotic administration among preterm infants. J Perinatol. 2021;41(2):255-262. doi: 10.1038/s41372-020-00784-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dhudasia MB, Mukhopadhyay S, Puopolo KM. Implementation of the sepsis risk calculator at an academic birth hospital. Hosp Pediatr. 2018;8(5):243-250. doi: 10.1542/hpeds.2017-0180 [DOI] [PubMed] [Google Scholar]
- 3.Meyers JM, Tulloch J, Brown K, Caserta MT, D’Angio CT; Golisano Children’s Hospital NICU Antibiotic Stewardship Team. A quality improvement initiative to optimize antibiotic use in a level 4 NICU. Pediatrics. 2020;146(5):e20193956. doi: 10.1542/peds.2019-3956 [DOI] [PubMed] [Google Scholar]
- 4.Pineda R, Knudsen K, Breault CC, Rogers EE, Mack WJ, Fernandez-Fernandez A. NICUs in the US: levels of acuity, number of beds, and relationships to population factors. J Perinatol. 2023;43(6):796-805. doi: 10.1038/s41372-023-01693-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Puopolo KM, Benitz WE, Zaoutis TE; Committee on Fetus and Newborn; Committee on Infectious Diseases. Management of neonates born at ≥35 0/7 weeks’ gestation with suspected or proven early-onset bacterial sepsis. Pediatrics. 2018;142(6):20182894. doi: 10.1542/peds.2018-2894 [DOI] [PubMed] [Google Scholar]
- 6.Dukhovny D, Buus-Frank ME, Edwards EM, et al. A collaborative multicenter QI initiative to improve antibiotic stewardship in newborns. Pediatrics. 2019;144(6):e20190589. doi: 10.1542/peds.2019-0589 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. Supplemental Methods
Data Sharing Statement