Highlights
-
•
Assessed the impact of recovery housing on healthcare utilization outcomes.
-
•
Recovery housing helped reduced readmission to inpatient substance use treatment.
-
•
People in recovery housing had reduced use of the emergency department.
-
•
People in recovery housing had increased use of primary care.
Keywords: Healthcare utilization, Recovery housing, Substance use disorder, Homelessness
Abstract
Introduction
Central City Concern (CCC) operates several recovery housing sites in the Portland, Oregon metropolitan region, including the Blackburn Center (Blackburn) and the Richard L. Harris Building (Harris). This retrospective, observational study was designed to assess recovery housing's impact on inpatient detoxification readmission rates and healthcare utilization patterns.
Methods
Our study population consisted of individuals discharged from CCC's Hooper Detox Stabilization Center from June 2019 to September 2020. A total of 75 clients housed at Blackburn, 63 clients housed at Harris, and 57 clients discharged as unhoused were included in the study sample. Using logistic regression for each of the two recovery housing groups relative to the unhoused group, we examined differences in readmissions to inpatient detoxification after their qualifying discharge. We then used Difference-In-Difference model to compare the per member per year (PMPY) use of different domains of health care before and after their qualifying discharge.
Results
Compared to clients discharged as unhoused, Blackburn and Harris residents had lower risk of readmissions to inpatient detoxification treatment at 90- and 180-days post-discharge. Additionally, while the mean number of PMPY emergency department visits increased for clients discharged as unhoused in the post period, the average number of emergency department visits decreased for clients who obtained recovery housing at Blackburn (DiD=-3.65 PMPY, p-value=0.02) and at Harris (DiD=-3.87 PMPY, p-value=0.01).
Conclusion
Findings highlight the impact and importance of recovery housing for individuals managing a substance use disorder and the value of healthcare system and public sector investment housing like Blackburn and Harris.
1. Introduction
There is a growing consensus and consistent evidence that housing improves health outcomes, particularly among those with the most serious mental and physical health considerations (Khatana et al., 2020; Racine et al., 2020). Access to stable housing has also been identified as an integral component for supporting recovery from substance use disorder (SUD) (Polcin, 2009; SAMHSA, 2012). Yet, many individuals are unstably housed when entering treatment for SUD. A national study found that nearly one third of individuals entering SUD treatment reported being marginally housed in the month prior to treatment entry (Eyrich-Garg et al., 2008). Housing is frequently cited as a top need among individuals in recovery (Laudet and White, 2010). Moreover, returning to former residences after exiting controlled environments such as inpatient detoxification may increase risk of relapse (Shaham et al., 2003).
Recovery housing has been identified as a promising model of service delivery to house and support individuals exiting SUD treatment. Recovery housing generally refers to substance-free, safe, and healthy living environments with integrated peer supports that support recovery from SUD and associated issues (Mericle et al., 2017; The Society for Community Research, 2013). These types of residences have different names (e.g., Oxford Houses, sober living houses, sober homes) and offer varying levels of services, support, and oversight with a range of operational practice standards (National Association of Recovery Residences, 2012).
Evaluations of recovery housing have shown positive outcomes in terms of reduced substance use, increased rates of employment and income, decreased criminal justice involvement, as well as improved behavioral health outcomes (Kelly, 2018; Reif et al., 2014; Vanderplasschen et al., 2013). Given the relationship between housing stability and access to healthcare services (Cohen-Cline et al., 2022; Stergiopoulos et al., 2019; Wright et al., 2016), recovery housing may also serve to support better health and recovery by impacting use of health care. Yet, few studies have assessed the effect of recovery housing on health care utilization outcomes. Moreover, lack of consistency in recovery housing models has made it difficult to assess evidence across programs (Kelly, 2018; Reif et al., 2014).
Central City Concern (CCC) provides transition support services to people experiencing homelessness in the Portland metro region. In partnership with six local healthcare organizations, CCC created the Blackburn Center (Blackburn), which consists of 165 housing units divided into three types of housing including 80 units of short-term recovery housing that offers stays of approximately 6 months to support residents navigating substance use treatment after discharge from CCC's Hooper Detoxification Stabilization Center (HDSC). Blackburn includes an on-site federally qualified healthcare center and provides wrap-around recovery and rehabilitation services, such as inpatient treatment and case management of complex needs. In addition to Blackburn, CCC operates other recovery housing sites including the Richard L. Harris Building (Harris). Similar to Blackburn, Harris offers a drug- and alcohol-free living environment with co-located primary care, mental health, and recovery services.
The purpose of this study was to assess the impact of recovery housing at (two separate recovery housing sites) on inpatient detoxification treatment readmission rates and health care utilization outcomes in comparison to those who did not obtain housing after exiting inpatient SUD treatment.
2. Methods
2.1. Study design and sample
This study employed a retrospective, observational design that explored outcomes for patients discharged from inpatient SUD treatment to: 1. Blackburn recovery housing; 2. Harris recovery housing, or 3. no housing available so discharged as unhoused. The study was reviewed and approved by the Providence St. Joseph Health Institutional Review Board.
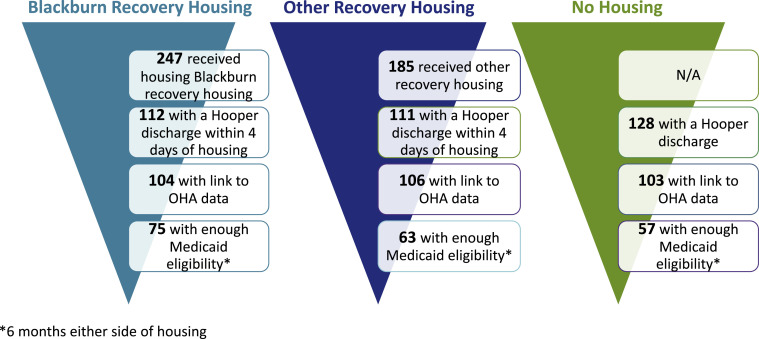
Our study population consisted of individuals discharged from HDSC from June 2019 to September 2020. To be eligible for inclusion in the study, clients had to be Medicaid members with at least six months of Medicaid enrollment on either side of their discharge date. Clients in Blackburn and Harris housing groups were required to be housed within 4 days of the original HDSC discharge. Clients in the discharged as unhoused group were had a program exit labeled as “homeless” in either CCC or HDSC data. In total, 75 clients housed through Blackburn, 63 clients housed at Harris, and 57 clients discharged into homelessness met all eligibility criteria and were included in the study sample (Fig. 1).
Fig. 1.
Study population and eligibility criteria for study participants at each discharge site.
Unique Medicaid identifiers from the HDSC data were matched to Oregon Health Authority Medicaid claims data. Claims data was requested for the period from March 2018 to May 2021, so each client would have a year of health care utilization on either side of their discharge date from HDSC. To be included in the analysis, clients had to have at least six months, non-continuous, of eligibility data within the year before and after their discharge date from HDSC.
2.2. Study measures
The primary outcomes for the analysis of recovery housing were readmission to HDSC within 90- and 180-day windows, as well as hospital and healthcare utilization before and after being housed. Healthcare utilization was defined using modified Healthcare Effectiveness Data and Information Set (HEDIS) measures for inpatient, emergency department, outpatient mental health, primary care, specialty care, and dental care events.
2.3. Statistical analysis
We used descriptive statistics to assess the demographic make-up of the three study groups. Comparisons for readmissions to HDSC were made using separate generalized linear models with a modified Poisson regression to estimate risk ratios for each of the two recovery housing groups relative to the homeless group, while comparisons for utilization outcomes were made using Difference-In-Difference (DiD) models. Our Difference-In-Difference models employee a linear regression and an interaction term between study group (Blackburn or Harris versus Discharged as Unhoused) and time (before and after discharge from HDSC). We only present the interaction term in our tables as this is the measure of true change between the two groups over time. All models adjusted for age, the month of discharge from the HDSC, and medical complexity as determined by the Chronic Illness and Disability Payment System (CDPS) score, a diagnostic classification system used by Medicaid programs to assess risk of healthcare utilization based on health diagnoses (Kronick et al., 2000). Race was determined through claims data and program records and is included descriptively to call attention to the impact of institutional racism on housing, homelessness, health, and healthcare rather than as a biological construct (Boyd et al., 2020). All analysis was conducted in R version 4.0.3.
3. Results
We identified 112 clients housed at Blackburn and 111 housed at Harris within four days of their discharge from HDSC. Of those clients housed at Blackburn, 104 (92.9 %) matched to Medicaid claims data and 75 (67.0 %) had sufficient eligibility to be included in the analysis. Of those clients housed at Harris, 106 (95.5 %) matched to Medicaid claims data and 63 (57.8 %) had sufficient eligibility to be included in the analysis. We identified 128 clients discharged as homeless from HDSC during the study window. Of those clients discharged as homeless, 103 (80.5 %) matched to Medicaid claims data and 57 (44.5 %) had sufficient eligibility to be included in the analysis.
Overall, the demographic and health characteristics of clients discharged into Blackburn, Harris, and as unhoused were roughly similar (Table 1). The majority of clients across all three groups were aged 45 years old or younger with a mean age between 36 and 37 years old. Clients predominantly identified as male and most identified as White. Nearly all clients had at least one chronic physical health or behavioral health condition. Among clients who completed their stay in recovery housing, clients at Blackburn stayed a mean of 138.7 (sd=92.1) days and clients at Harris stayed a mean of 131.4 (sd=112.8) days (data not shown).
Table 1.
Demographic characteristics and chronic health condition summary of blackburn recovery housing clients, harris recovery housing clients, and clients discharged as unhoused.
| Blackburn Recovery Housing | Harris Recovery Housing | Unhoused | ||
|---|---|---|---|---|
| Count | 75 | 63 | 57 | |
| %^ | %^ | %^ | ||
| Age group | ||||
| 35 and under | 53.33 | 60.32 | 43.86 | |
| 36 - 45 | 22.67 | 20.63 | 35.09 | |
| 46 - 55 | 22.67 | 14.29 | 14.04 | |
| 56 and over | 1.33 | 4.76 | 7.02 | |
| Mean | 36.87 | 36.14 | 37.98 | |
| Sex | ||||
| Female | 29.33 | 25.40 | 17.54 | |
| Male | 70.67 | 74.60 | 82.46 | |
| Race | ||||
| Black | 14.67 | 7.94 | 7.14 | |
| Multiracial | 4.00 | 1.59 | 8.93 | |
| White | 74.67 | 84.13 | 66.07 | |
| Another Race | 6.67 | 6.35 | 17.86 | |
| CHRONIC CONDITIONS SUMMARY | ||||
| None | 3.23 | 1.75 | 2.08 | |
| At least one physical condition | 9.68 | 8.77 | 10.42 | |
| At least one behavioral condition | 33.87 | 50.88 | 37.50 | |
| At least one physical and behavioral condition | 53.23 | 38.60 | 50.00 | |
| CDPS* score (Mean) | 2.35 | 2.40 | 2.27 |
Chronic disability payment system.
Percentage unless otherwise stated.
After adjusting for age, medical complexity, and month of discharge from HDSC, clients obtaining housing through Blackburn had 0.61 (p-value 0.04) times the risk of readmission to HDSC 90 days after discharge compared to individuals discharged as unhoused. Although less impactful, this pattern held through 180 days post-discharge with clients housed at Blackburn having 0.76 (p-value 0.12) times the risks of readmission compared to the unhoused group. Similarly, clients housed in Harris had reduced risk of readmission at both 90 (aRR 0.75, p-value 0.22) and 180 (aRR 0.79, p-value 0.22) days compared to the unhoused group. No differences in readmission rates were observed between clients housed in Blackburn and those housed in Harris (Appendix Table 1). Table 2
Table 2.
HDSC Readmission outcomes of blackburn recovery housing and harris recovery housing clients relative to clients discharged as unhoused.
| Unhoused | Blackburn Recovery Housing | Harris Recovery Housing | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Count | 57 | 75 | Logistic Regression^ | 63 | Logistic Regression^ | |||||||
| % | 95% C.I. | % | 95% C.I. | aRR | 95 % C.I. | p-value | % | 95 % C.I. | aRR | 95 % C.I. | p-value | |
| Readmit to HDSC - 90 days | 0.04 | 0.22 | ||||||||||
| No | 68.42 | (55.35–79.11) | 85.33 | (75.42–91.69) | 1.00 | – | 79.37 | (67.63–87.62) | 1.00 | – | ||
| Yes | 31.58 | (20.89–44.65) | 14.67 | (8.31–24.58) | 0.61 | (0.38–0.98) | 20.63 | (12.38–32.37) | 0.75 | (0.48–1.18) | ||
| Readmit to HDSC - 180 days | 0.12 | 0.22 | ||||||||||
| No | 59.65 | (46.55–71.5) | 72.00 | (60.84–80.98) | 1.00 | – | 69.84 | (57.49–79.86) | 1.00 | – | ||
| Yes | 40.35 | (28.5–53.45) | 28.00 | (19.02–39.16) | 0.76 | (0.54–1.08) | 30.16 | (20.14–42.51) | 0.79 | (0.54–1.15) | ||
Adjusted for age (continuous), CDPS risk score, and month of discharge from Hooper Detox.
Compared to clients discharged as unhoused, obtaining recovery housing impacted health care utilization patterns in the 12 months after discharge from HDSC, adjusting for age, medical complexity, and month of discharge (Table 3). While the mean number of emergency department visits increased per member per year (PMPY) for clients discharged as unhoused in the post period, the average number of emergency department visits decreased for clients who obtained recovery housing at Blackburn (DiD=−3.65 PMPY, p-value=0.02) and at Harris (DiD=−3.87 PMPY, p-value=0.01) when compared to the change in the unhoused group. Similarly, the mean number of inpatient stays PMPY increased for clients discharged as unhoused, while the average number of inpatient stays decreased for clients who obtained recovery housing at Blackburn (DiD=−0.24, p-value=0.14) and at Harris (DiD=−0.30, p-value=0.10).
Table 3.
PMPY Healthcare utilization of blackburn recovery housing and harris recovery housing clients compared to clients dischared as unhoused.
| Unhoused Discharge |
Blackburn Recovery Housing |
Harris Recovery Housing |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | DiD^ | Pre | Post | DiD^ | |||
| Count | 57 | 57 | 75 | 75 | 63 | 63 | ||||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Est | p-value | Mean (SD) | Mean (SD) | Est | p-value | |
| Healthcare Events Per Year | ||||||||||
| Inpatient | 0.19 (0.46) | 0.36 (1.14) | 0.2 (0.55) | 0.13 (0.35) | −0.24 | 0.14 | 0.22 (0.65) | 0.1 (0.35) | −0.30 | 0.10 |
| Emergency department | 3.56 (4.88) | 6.59 (10.35) | 3.68 (7.48) | 3.06 (5.15) | −3.65 | 0.02 | 3.27 (4.02) | 2.44 (3.96) | −3.87 | 0.01 |
| Outpatient mental health | 1.75 (3.42) | 1.85 (4.83) | 3.11 (7.15) | 4.7 (7.77) | 1.49 | 0.29 | 4.32 (9.69) | 4.2 (9.23) | −0.22 | 0.90 |
| Primary care provider | 2.33 (3.66) | 2.77 (4.73) | 2.87 (3.11) | 6.33 (7.67) | 3.02 | 0.01 | 2.38 (3.33) | 5.18 (7.24) | 2.36 | 0.04 |
| Specialty care | 0.42 (1.25) | 0.48 (1.07) | 0.5 (0.83) | 0.63 (1.59) | 0.07 | 0.80 | 0.43 (0.94) | 0.55 (1.08) | 0.05 | 0.85 |
| Any dental | 0.39 (0.98) | 0.43 (1.14) | 0.91 (1.89) | 1.39 (2.1) | 0.44 | 0.24 | 1.47 (3.57) | 1.22 (3.26) | −0.29 | 0.64 |
Adjusted for age (continuous), CDPS risk score, and month of discharge from Hooper Detox.
Conversely, the mean number of primary care visits PMPY did not change after discharge compared to prior for unhoused clients, but PMPY primary care visits increased for those discharged to recovery housing at Blackburn (DiD = +3.02 PMPY, p-value = 0.01) or at Harris (DiD = +2.36, p-value = 0.04) relative to the unhoused group. We did not observe any meaningful differences in the amount of inpatient, outpatient mental health, specialty care, or dental care used between clients who obtained recovery housing and those who did not. Additionally, we did not observe any differences in healthcare utilization patterns when comparing clients housed in Blackburn to those housed in Harris (Appendix Table 2).
4. Discussion
Access to safe and stable housing has been identified as an integral component to supporting individuals in recovery from SUD (Khatana et al., 2020; Racine et al., 2020; SAMHSA, 2012). The current study adds to the growing body of evidence identifying housing as a key determinant of health and health care use for individuals with complex health needs like SUD (Cohen-Cline et al., 2022; Stergiopoulos et al., 2019; Wright et al., 2016). These findings also serve to extend the evidence base for recovery housing by demonstrating reduced relapse as measured by readmission rates for inpatient substance use care, increased primary care utilization, as well as reduced emergency department utilization among individuals discharged from inpatient detoxification into recovery housing.
Our study of recovery housing at CCC confirmed our overall impression and previous research that providing housing for people who are in recovery helps reduce readmission rates to inpatient recovery and detoxification programs compared to those discharged into homelessness. This pattern held true for clients housed in recovery housing at 90- and 180-days. Previous studies corroborate this finding showing that housing stability is associated with a decreased risk of readmission to detoxification programs (Running Bear et al., 2022) and that housing instability is a significant predictor of readmission to detoxification programs (Callaghan, 2003; Callaghan and Cunningham, 2002). Accordingly, these findings highlight the importance of housing supports as an essential consideration in the continuum of care provided to individuals exiting inpatient detoxification programs.
We also found that use of primary care services increased for individuals in recovery housing while use of emergency services decreased. These results indicate that when provided with access to healthcare services, clients made greater use of the services which has important implications for recovery housing models. To date, few studies have assessed the impact of recovery housing on patterns of healthcare utilizaton. By establishing a better understanding of recovery housing clients' healthcare utilization patterns, these findings can be leveraged to develop more sustainable sources of funding for recovery housing sites. Recovery housing sites typically rely on out-of-pocket fees to support operations which makes funding a commonly reported barrier for ongoing operations (Mericle et al., 2015). However, the patterns of health care use observed in our study, specifically the increased use of outpatient care and the reduction in use of more costly acute care services, aligns with health care system transformation efforts and strategies to achieve better care, better health, and better cost. Cost savings derived from improved patterns of health care utilization may serve as the basis for encouraging public and private insurers to cover these types of services which could establish more reliable sources of revenue and ensure greater access to recovery housing.
Our study revealed no significant differences in outcomes between those housed in Blackburn and those in Harris alternative recovery housing. An ongoing limitation of prior research assessing the effectiveness of recovery housing has centered on the lack of consistent defining characteristics and practices across different organizational models (Mericle et al., 2022; Pannella Winn and Paquette, 2016). Our study findings indicate that recovery housing has a positive impact on healthcare utilization outcomes despite varying levels of services at the Blackburn and Harris sites.
While the study yielded useful information, it did have some limitations. First, the small sample size may have limited our ability to detect statistical significance. In additional, a small percentage of the individuals in our study did not match to Medicaid claims data; thus, limiting our ability to generalize our findings to individuals who are uninsured or have other insurance types. Individuals who do not qualify for Medicaid may face additional barriers in accessing health care (e.g., citizenship status) which may impact their patterns of utilization following discharge from HSDC. Future studies may want to prioritize uninsured individual to better understand their unique needs. Study participants were also predominantly white and male, and the observed results may not reflect the experiences of a more diverse population. For example, we did observe a smaller proportion of individuals discharged as homeless identified as White. However, the size of our sample inhibited our ability to include race as a variable in our analytic models. Given pervasive inequities in SUD, housing access alongside the well-established barriers to health and healthcare for systemically marginalized groups (Williams and Cooper, 2019), this is certainly a limitation of the current study and highlights the needs for additional research focused on the needs of communities of color with SUD and experiencing housing instability. Additionally, the COVID-19 pandemic occurred during the study window and certainly impacted healthcare utilization during this time. Even so, the inclusion of a comparison group is a strength of the study and may help to mitigate the potential exogenous impact of the pandemic on the study results.
5. Conclusion
This study demonstrated improved healthcare outcomes among participants who were housed in recovery housing following discharge from inpatient SUD treatment. There was a noted reduction in the number of emergency room visits, increased engagement with primary care providers, and a reduction in the rate of re-admissions to the HDSC.
Overall, the improved outcomes demonstrated by residents at CCC recovery housing sites highlights the impact and importance of recovery housing for individuals managing a SUD and the value of healthcare system and public sector investment in housing like Blackburn and Harris. While additional research with a broad, cross-sector scope would be needed to thoroughly assess the overall impact on an urban population center, the evidence for local efficacy is clear: providing housing improves outcomes.
CRediT authorship contribution statement
Sarah E. Roth: Methodology, Writing – review & editing, Writing – original draft. Kyle G. Jones: Methodology, Formal analysis, Writing – review & editing. Keri B. Vartanian: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review & editing.
Declaration of Competing Interest
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests:
Keri Vartanian reports financial support was provided by Adventist Health. Keri Vartanian reports financial support was provided by Kaiser Permanente Northwest. Keri Vartanian reports financial support was provided by Oregon Health & Science University. Keri Vartanian reports financial support was provided by Legacy Health System. Keri Vartanian reports financial support was provided by CareOregon Inc.
Acknowledgments
Role of funding source
This research was funded by six healthcare organizations investing in public health and housing in the Pacific Northwest: Adventist Health, Kaiser Permanente Northwest, Oregon Health & Science University, Legacy Health, CareOregon, and Providence Health & Services.
Acknowledgments
The authors wish to thank the research staff who helped with this study including A. Gilmore. We would also like to thank M. Sutcliffe, Ph.D. and R. Marsillo, for their support of this manuscript.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.dadr.2023.100192.
Appendix. Supplementary materials
References
- Boyd R.W., Lindo E.G., Weeks L.D., McLemore M.R. On racism: a new standard for publishing on racial health inequities. Health Aff. 2020;10(10.1377):1. Blog. [Google Scholar]
- Callaghan R.C., Cunningham J.A. Gender differences in detoxification: predictors of completion and re-admission. J. Subst. Abuse Treat. 2002;23(4):399–407. doi: 10.1016/S0740-5472(02)00302-1. [DOI] [PubMed] [Google Scholar]
- Callaghan R.C. Risk factors associated with dropout and readmission among first nations individuals admitted to an inpatient alcohol and drug detoxification program. Can. Med. Assoc. J. 2003;169(1) http://www.cmaj.ca/content/169/1/23.abstract 23 LP -27. [PMC free article] [PubMed] [Google Scholar]
- Cohen-Cline H., Jones K., Vartanian K.B. Local housing choice voucher distribution policies impact healthcare utilization: a randomized natural experiment. J. Urban Health. 2022;99(2):260–267. doi: 10.1007/s11524-022-00609-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eyrich-Garg K.M., Cacciola J.S., Carise D., Lynch K.G., McLellan A.T. Individual characteristics of the literally homeless, marginally housed, and impoverished in a US substance abuse treatment-seeking sample. Soc. Psychiatry Psychiatr. Epidemiol. 2008;43(10):831–842. doi: 10.1007/s00127-008-0371-8. [DOI] [PubMed] [Google Scholar]
- Kelly, J., 2018. SAMHSA recovery research and evaluation technical expert panel summary report. https://www.chestnut.org/Resources/4bb80a22-dc04-42c4-857f-8b468d5092a6/SAMHSA-Recovery-Research-Report-2018.pdf. Accessed 4 October 2023.
- Khatana S.A.M., Wadhera R.K., Choi E., Groeneveld P.W., Culhane D.P., Kushel M., Kazi D.S., Yeh R.W., Shen C. Association of homelessness with hospital readmissions—An analysis of three large states. J. Gen. Intern. Med. 2020;35(9):2576–2583. doi: 10.1007/s11606-020-05946-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kronick R., Gilmer T., Dreyfus T., Lee L. Improving health-based payment for medicaid beneficiaries: CDPS. Health Care Financ. Rev. 2000;21(3):29–64. http://www.ncbi.nlm.nih.gov/pubmed/11481767 [PMC free article] [PubMed] [Google Scholar]
- Laudet A.B., White W. What are your priorities right now? Identifying service needs across recovery stages to inform service development. J. Subst. Abuse Treat. 2010;38(1):51–59. doi: 10.1016/j.jsat.2009.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mericle A.A., Miles J., Cacciola J. A critical component of the substance abuse continuum of care: recovery homes in Philadelphia. J. Psychoact. Drugs. 2015;47(1):80–90. doi: 10.1080/02791072.2014.976726. [DOI] [PubMed] [Google Scholar]
- Mericle A.A., Polcin D.L., Hemberg J., Miles J. Recovery housing: evolving models to address resident needs. J. Psychoact. Drugs. 2017;49(4):352–361. doi: 10.1080/02791072.2017.1342154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mericle A.A., Patterson D., Howell J., Subbaraman M.S., Faxio A., Karriker-Jaffe K.J. Identifying the availability of recovery housing in the U.S The NSTARR project. Drug Alcohol Depend. 2022;230 doi: 10.1016/J.DRUGALCDEP.2021.109188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Association of Recovery Residences. (2012). A primer on recovery residences: fAQs. www.narronline.com Accessed 4 October 2023.
- Pannella Winn L., Paquette K. Bringing recovery housing to scale in Ohio: lessons learned. J. Dual Diagn. 2016;12(2):163–174. doi: 10.1080/15504263.2016.1173971. [DOI] [PubMed] [Google Scholar]
- Polcin D.L. Communal-living settings for adults recovering from substance abuse. J. Groups Addict. Recovery. 2009;4(1–2):7–22. doi: 10.1080/15560350802712355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Racine M.W., Munson D., Gaeta J.M., Baggett T.P. Thirty-day hospital readmission among homeless individuals with Medicaid in Massachusetts. Med. Care. 2020;58(1):27–32. doi: 10.1097/MLR.0000000000001234. [DOI] [PubMed] [Google Scholar]
- Reif S., George P., Braude L., Dougherty R.H., Daniels A.S., Ghose S.S., Delphin-Rittmon M.E. Recovery housing: assessing the evidence. Psychiatr. Serv. 2014;65(3):295–300. doi: 10.1176/appi.ps.201300243. [DOI] [PubMed] [Google Scholar]
- Running Bear U., Hanson J.D., Noonan C., Muller C., Trojan J., Manson S.M. Factors associated with readmission to alcohol and opioid detoxification in the Alaska Interior. Am. J. Addict. 2022;31(5):406–414. doi: 10.1111/AJAD.13288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAMHSA., 2012. SAMHSA’s working definition of recovery: 10 guiding principles of recovery. https://store.samhsa.gov/sites/default/files/d7/priv/pep12-recdef.pdf. Accessed 4 October 2023.
- Shaham Y., Shalev U., Lu L., de Wit H., Stewart J. The reinstatement model of drug relapse: history, methodology and major findings. Psychopharmacology. 2003;168(1):3–20. doi: 10.1007/s00213-002-1224-x. (Berl.) [DOI] [PubMed] [Google Scholar]
- Stergiopoulos V., Mejia-Lancheros C., Nisenbaum R., Wang R., Lachaud J., O'Campo P., Hwang S.W. Long-term effects of rent supplements and mental health support services on housing and health outcomes of homeless adults with mental illness: extension study of the at home/Chez Soi randomised controlled trial. Lancet Psychiatry. 2019;6(11):915–925. doi: 10.1016/S2215-0366(19)30371-2. [DOI] [PubMed] [Google Scholar]
- The Society for Community Research The role of recovery residences in promoting long-term addiction recovery. Am. J. Community. Psychol. 2013;52(3–4):406–411. doi: 10.1007/s10464-013-9602-6. [DOI] [PubMed] [Google Scholar]
- Vanderplasschen W., Colpaert K., Autrique M., Rapp R.C., Pearce S., Broekaert E., Vandevelde S. Therapeutic communities for addictions: a review of their effectiveness from a recovery-oriented perspective. Sci. World J. 2013;2013 doi: 10.1155/2013/427817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams D.R., Cooper L.A. Reducing racial inequities in health: using what we already know to take action. Int. J. Environ. Res. Public Health. 2019;16(4) doi: 10.3390/ijerph16040606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright B.J., Vartanian K.B., Li H.F., Royal N., Matson J.K. Formerly homeless people had lower overall health care expenditures after moving into supportive housing. Health Aff. 2016;35(1):20–27. doi: 10.1377/hlthaff.2015.0393. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.