Rates of type 2 diabetes (T2D) are increasing, and many individuals with T2D do not meet glycemic targets. 1 For many patients with T2D, their primary care provider (PCP) is the only physician treating their diabetes. 2 In this retrospective, observational study, we used real-world data from 13 AMGA (American Medical Group Association) member health care organizations across the United Sates to assess whether real-time continuous glucose monitoring (RT-CGM) initiation was associated with improvements in glycemic metrics among individuals with T2D receiving primary care.
A retrospective analysis was performed using electronic health records and outbound administrative claims data, which were extracted, mapped, and normalized by Optum. Included individuals had a T2D diagnosis, were 18 to 85 years of age, had ≥1 outpatient PCP visit 18 months prior to RT-CGM use, initiated RT-CGM between August 1, 2015, and September 30, 2020, and had glycated hemoglobin (HbA1c) values ≤12 months prior to RT-CGM initiation (baseline) and three to nine months after RT-CGM initiation (follow-up). Exclusion criteria included diagnosis of T1D or gestational diabetes, evidence of palliative care or hospice, death within nine months of RT-CGM initiation, and evidence of prior CGM use. The primary outcome was change in HbA1c from baseline to follow-up. Individuals were stratified by baseline HbA1c (≤7.5% and >7.5%) and insulin regimen.
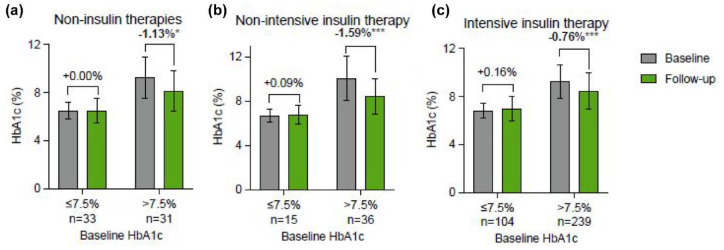
Participants (n = 458) were 61 [54-70] years of age (median [interquartile range]), 50% female, and 85% white, and the insured status was 50% commercial, 43% Medicare, and 2% Medicaid. The average number of PCP visits in the prior year was mean (SD) of 3.7 (2.9). Intensive insulin therapy (IIT, prandial ± basal insulin) was used by 75% (343/458) of participants, non-intensive insulin therapy (NIIT, basal insulin) was used by 11% (51/458), and non-insulin therapies (NITs) were used by 14% (64/458). Among individuals with baseline HbA1c >7.5%, HbA1c significantly decreased regardless of the insulin therapy regimen (Figure 1). Glycated hemoglobin did not significantly change in individuals with baseline HbA1c ≤7.5%.
Figure 1.
Change in HbA1c stratified by baseline HbA1c. Baseline and follow-up HbA1c stratified by baseline HbA1c in individuals on (a) non-insulin therapy, (b) non-intensive insulin therapy (bolus insulin), and (c) intensive insulin therapy (prandial ± basal insulin).
Abbreviation: HbA1c, glycated hemoglobin. *P < .05. **P < .01. ***P < .001.
These results align with others in the literature. In Beck et al, initiation of RT-CGM by individuals with T2D on IIT experienced a significantly greater decrease in HbA1c (–1.0% with RT-CGM vs –0.6% for Controls). 3 In Grace et al, individuals with T2D on NIIT or NIT experienced a mean change in HbA1c of –3.0 percentage points after initiating RT-CGM. 4 Both studies required baseline HbA1c >7.5% for inclusion.3,4
Strengths of this study include the relatively large population and the diversity of insulin use and insurance coverage. Study limitations include the lack of a control group and the lack of CGM-based glycemic metrics. We do not know why participants initiated RT-CGM or the extent of their adherence to RT-CGM or their insulin regimens. We also do not know how insulin was delivered or whether any medications were changed between baseline and follow-up. Study generalizability is limited by the inclusion of only RT-CGM systems and the all-US population.
These findings suggest that RT-CGM initiation can improve HbA1c in primary care patients with poorly controlled T2D regardless of their insulin therapy reg. This real-world evidence supports further studies of RT-CGM’s benefits in the broader T2D population.
Acknowledgments
The authors thank Courtney Green for editorial assistance. Dexcom is a registered trademark of Dexcom, Inc. in the United States and other countries.
Footnotes
Abbreviations: AMGA, American Medical Group Association; CGM, continuous glucose monitoring; HbA1c, glycated hemoglobin; IIT, intensive insulin therapy; NIT, non-insulin therapies; NIIT, non-intensive insulin therapy; PCP, primary care provider; RT-CGM, real-time continuous glucose monitoring; T2D, type 2 diabetes.
Authors’ Note: This work was presented in part at the 82nd American Diabetes Association meeting in New Orleans, LA, on June 3-7, 2022.
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: SS and ELC are employees of American Medical Group Association (AMGA). GJN and RT are employees of Dexcom, Inc.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The work was funded by Dexcom, Inc.
ORCID iD: Gregory J. Norman  https://orcid.org/0000-0001-7989-9597
https://orcid.org/0000-0001-7989-9597
References
- 1. Centers for Disease Control and Prevention. National diabetes statistics report. https://www.cdc.gov/diabetes/data/statistics-report/index.html.
- 2. Healy AM, Shubrook JH, Schwartz FL, Cummings DM, Drake AJ, III, Tanenberg RJ. Endocrinologists’ opinions of diabetology as a primary care subspecialty. Clin Diabetes. 2018;36(2):168-173. doi: 10.2337/cd17-0097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Beck RW, Riddlesworth TD, Ruedy K, et al. Continuous glucose monitoring versus usual care in patients with type 2 diabetes receiving multiple daily insulin injections: a randomized trial. Ann Intern Med. 2017;167(6):365-374. doi: 10.7326/M16-2855. [DOI] [PubMed] [Google Scholar]
- 4. Grace T, Salyer J. Use of real-time continuous glucose monitoring improves glycemic control and other clinical outcomes in type 2 diabetes patients treated with less intensive therapy. Diabetes Technol Ther. 2022;24(1):26-31. doi: 10.1089/dia.2021.0212. [DOI] [PMC free article] [PubMed] [Google Scholar]