Abstract
With increasing evidence of emotional well-being disorders associated with polycystic ovary syndrome (PCOS), effective screening processes are of utmost importance. We studied the impact of using questionnaires to screen for emotional and psychosexual well-being across different models of care for PCOS. We analysed the data from the surveys to assess the difference in the prevalence of emotional and psychosexual ill-being across ethnicity and region. In this prospective cohort study, we invited all women attending consultations for PCOS in Birmingham, UK, and Bengaluru and Navi Mumbai, India. Those who consented to participate in the study were invited to complete a pre-clinic survey about socio-demographic data, Hospital Anxiety and Depression Scale (HADS), Body Image Concern Inventory (BICI), Beliefs about Obese Person scale (BAOP), and Female Sexual Function Index score (FSFI) and a post-clinic survey on clinic experience, lifestyle advice, and specialist referral. A total of 115 women were included in this study. The rate of questionnaire completion was 98.3% (113/115), 97.4% (112/115), 93.04% (107/115), and 84.3% (97/115) for HADS, BICI, BAOP, and FSFI, respectively. In the post-clinic survey, 28.8% reported they were screened for anxiety, 27.1% for depression, and 45.8% for body image concerns. The prevalence of anxiety, depression, and body dysmorphic disorder through pre-clinic survey was 56.5% (50.0% UK vs 59.5% India, P = 0.483), 16.5% (13.9% UK vs 17.7% India, P = 0.529), and 29.6% (36.1% UK vs 26.6% India, P = 0.208), respectively. Surveys with validated questionnaires can improve screening for emotional and psychosexual well-being associated with PCOS which may be missed by ad hoc screening during consultations.
Key Words: PCOS, polycystic ovary syndrome, emotional well-being, psychosexual well-being, models of care
Introduction
Polycystic ovary syndrome (PCOS) is one of the most common endocrine conditions in women that significantly impact reproduction, metabolism, and emotional and psychosexual well-being (1, 2, 3). While most models of care (MoC) for PCOS are geared to assess and manage cardiometabolic risk, few screen for emotional and psychosexual well-being (4). Several studies have established a strong association and increased risk of anxiety, depression, body image distress, and psychosexual dysfunction with PCOS (5, 6, 7). The international PCOS guideline recommends appropriate screening, assessment, and treatment strategies for anxiety, depression, psychosexual dysfunction, eating disorders, and body image (8). Further clear guidance for implementing these recommendations could be beneficial. In the UK, the National Institute of Health and Care Excellence (NICE) guideline recommends that healthcare professionals ‘ask about emotional wellbeing and manage as appropriate’ in those affected with PCOS (9), again, without any specific advice on how to screen or manage the same. The direct healthcare costs associated with depression, anxiety, and eating disorders in PCOS were estimated to be $6.069 billion per year in 2021 in the United States of America (USA) (10). The overall disease burden on the National Health Service (NHS) from PCOS was estimated to be >£7 billion in 2014 (11). These healthcare costs will continue to increase with the growing population. With limited resources, developing efficient models of care (MoC) to screen and manage emotional well-being concerns in PCOS is important.
Patient surveys have been traditionally used to assess patients’ experience of healthcare services. These can inform healthcare professionals to build care services grounded in empathy and compassion, truly giving meaning to the co-created MoC (12). However, there is limited literature on its use to assess PCOS services. Pre-clinic surveys have been used to explore patient visit goals and obtain interim history (13). However, there is greater potential to utilise it as a screening tool.
In this study, we describe how we established a uniform pre-clinic screening for emotional well-being in three different MoCs and explored the experiences of people attending the clinic through the post-clinic survey. We then analysed the data from pre-clinic surveys to compare the differences in emotional and psychosexual well-being across ethnicity and country of residence.
Methods
This prospective cohort study was conducted from October 2020 to August 2021 at three reproductive endocrine centres with dedicated PCOS clinics – Birmingham in the UK and Bengaluru and Navi Mumbai in India. A brief description of these MoCs is as follows:
Birmingham, UK. This public-funded, free-to-end-user tertiary care centre has a dedicated clinic called the endocrine gynaecology clinic in a public setting. This clinic has been functioning since 2019, where women with suspected or confirmed PCOS undergo outpatient consultation. It is a clinic led by an endocrinologist/s who can triage for multiple conditions associated with PCOS and can then be referred to appropriate specialists such as dermatologists, weight management specialists, and gynaecologists. An endocrinologist triages all patients to refer them to an appropriate initial consultation. A nurse measures all patients’ height, weight, and blood pressure, followed by drawing blood samples to perform tests recommended by the consultant. The diagnosis of PCOS is established based on Rotterdam criteria. Women attending this clinic are screened, managed, or referred to a relevant specialist for type 2 diabetes mellitus, hypertension, coronary heart disease, lipid disorders, and venous thromboembolic disease. In addition, these women undergo anthropometric (weight, height, and body mass index (BMI)), metabolic (blood tests for lipid profile, fasting glucose, and metabolic syndrome score), and dermatologic (modified Ferriman–Gallwey score) assessments as part of their clinic consultation. Patients are also screened and advised for lifestyle factors: healthy diet, exercise, smoking cessation, and alcohol consumption.
Bengaluru, India. This is a tertiary Reproductive Endocrine clinic in a private setting with a special area of interest in PCOS since 2016. Patients Attending This Clinic Are Women with PCOS in Bengaluru and Surrounding Areas. It is a multidisciplinary clinic comprising an endocrinologist, an infertility specialist, a gynaecologist, a dermatologist, a nutritionist, a physiotherapist, and a specialist nurse. The endocrinologist, nurse, and nutritionist work jointly in the clinic and the rest offer care through service referrals. An endocrinologist, nurse, and nutritionist see all patients attending the clinic. Women attending these clinics are screened, managed, and referred for type 2 diabetes mellitus, hypertension, coronary heart disease, lipid disorders, dermatological issues, non-alcoholic fatty liver disease, and obstructive sleep apnoea. In addition, these women undergo anthropometric (weight, height, and BMI), metabolic (blood tests for lipid profile, fasting glucose and metabolic syndrome score), and dermatologic (modified Ferriman–Gallwey score) assessments as part of their clinic consultation. Patients are also screened and advised for lifestyle factors, such as healthy diet, exercise, smoking cessation, and alcohol consumption.
Navi Mumbai, India. This tertiary clinic in a private setting has offered reproductive endocrinology services to women with PCOS in Mumbai and surrounding areas since 2016. This multidisciplinary clinic comprises an endocrinologist, a nutritionist, and a nurse. All three specialists see all patients attending the clinic. Women attending these clinics are also screened, managed, or referred for type 2 diabetes mellitus, hypertension, coronary heart disease, lipid disorders, venous thromboembolic disease, and dermatological conditions. These women undergo anthropometric (weight, height, and BMI), metabolic (blood tests for lipid profile, fasting glucose, and metabolic syndrome score), and dermatologic (modified Ferriman–Gallwey score) assessments as part of their clinic consultation. Patients in this clinic are also screened and advised for lifestyle factors, such as healthy diet, exercise, smoking cessation, and alcohol consumption.
Before this study, all three clinics screened for psychological conditions associated with PCOS, such as anxiety and depression through leading questions during the initial consultation. If any concern was identified, these patients were referred to psychology services for further assessment and management.
All women attending the above clinics during the study period were sent a participant information leaflet and invited to participate in this study. Those who refused to participate were excluded from the study. All women who expressed interest in participating completed both pre- and post-clinic surveys.
-
Pre-clinic survey (Supplementary Table 1, see section on supplementary materials given at the end of this article) had questions on
Demographics (age, country of birth and residence, highest education qualification, marital status, number of children, and occupation).
Hospital Anxiety and Depression Scale (HADS); total score achievable is 21, a score of 8–10 is defined as a borderline case and a score of ≥11 is defined as a case of anxiety or depression (14).
Body Image Concern Inventory (BICI) to assess self-reported measures of dysmorphic appearance concerns. This validated questionnaire consists of a 19-item questionnaire evaluating opinions and appearance concerns. Each item uses a Likert-scale rating of frequency of feeling or performed the ‘described behaviour’. The BICI ranges from 19 to 95, where a score of ≥72 suggests body dysmorphic disorder (BDD) (15).
Beliefs about Obese Persons scale (BAOP) to examine beliefs about the causes of obesity. It is an eight-item questionnaire where a higher score suggests weight-related bias (16).
Female Sexual Function Index (FSFI) assesses the domains of sexual function: desire, arousal, lubrication, orgasm, satisfaction, and pain and provides a score regarding sexual function. Total score achievable is 36, a lower FSFI score suggests psychosexual dysfunction (17).
Post-clinic survey (Supplementary Table 2) included questions to understand patient experience and lifestyle recommendation participants received in the clinic.
Design and data collection
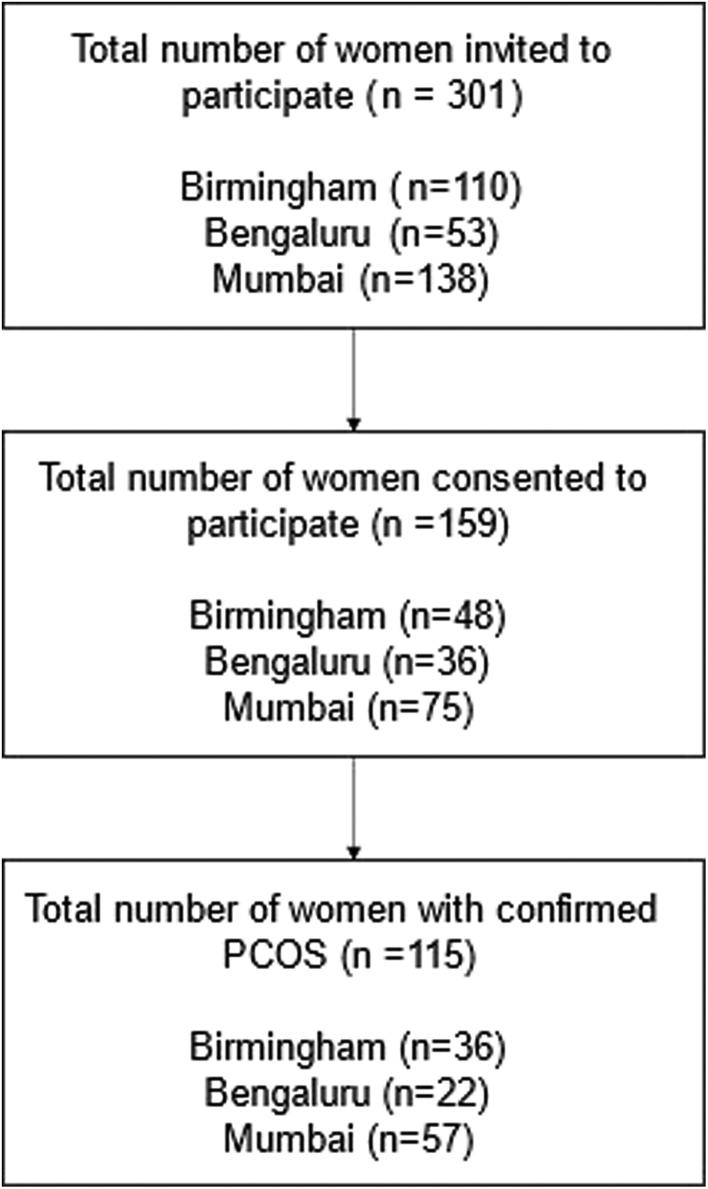
The list of women offered the clinic consultation was obtained through a booking system. These women were contacted by the members of the research team initially via text messages followed by telephone calls to explain about the survey. Once they agreed to participate in the study, they were sent a link to the pre-clinic survey via a text message. A unique code was also provided to pseudonymise the data and link the pre- and post-clinic surveys. Post-clinic surveys were sent to these women via a link through text messages within 24 h of their appointment. The process of participant recruitment is described in Fig. 1.
Figure 1.
The process of participant recruitment.
Statistical analysis
All data were compiled and processed using Microsoft Excel. Statistical analysis was performed using STATA 14.2. All exposure measures were calculated per the guidance of the validated questionnaires in the literature: HADS anxiety score, HADS depression score, BICI score, BAOP score, and FSFI score. We reported median and interquartile ranges (IQRs) for the diagnoses scores and frequency and percentages for all patients and patients stratified by their birthplace and ethnicity. For the analysis, we recoded primary exposure variables such as ethnicity and country of birth as dichotomous variables due to low samples in each individual category. Ethnicity was grouped into White ethnic women (White British and White Irish) and non-White ethnic women including the remaining ethnic groups. For the country of birth analysis, we only grouped women into those born in the UK and those born in India.
We used logistic regression models to obtain adjusted odds ratios and 95% confidence intervals (CIs) for each diagnostic outcome variable (anxiety, depression, and BDD) derived from the scores’ cut-off. We used linear regression models to obtain adjusted beta coefficients and 95% CI for each continuous outcome variable (HADS: anxiety and depression scores; BICI scores; BAOP scores; FSFI domain scores). We adjusted for age category, level of education, marital status, and parity in the logistic and linear regression models.
Details of ethics approval
This study has received approval from the HRA and Health and Care Research Wales (HCRW) approval (IRA project ID: 299243; REC reference: 22/PR/1178), Institutional Ethics Committee – Biomedical Research, Apollo Hospitals, Navi Mumbai (Application reference: AHM-ACD-021/02-21), and Ethics committee – Ramaiah Medical College in Bengaluru (Reference: MSRMC/EC/AP-07/05-2021).
Results
Composition of the overall cohort and overall emotional and psychosexual well-being
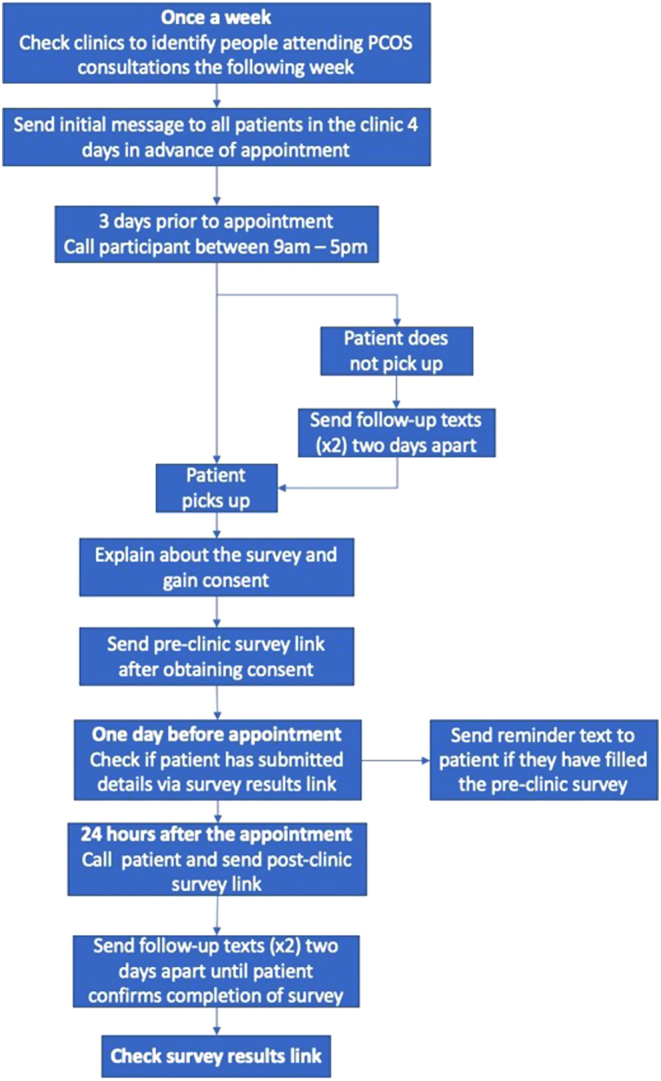
A total of 110 women in Birmingham, 53 in Bengaluru, and 138 in Navi Mumbai were approached to participate in the study. Of these, 159 women (48 in Birmingham, 36 in Bengaluru, and 75 in Mumbai) consented to participate and completed the pre-clinic survey. Of 159, 115 (72.3%) had confirmed PCOS diagnosis by a healthcare professional and were included in the analysis: 28.7% (36/115) lived in the UK; 68.7% (79/115) lived in India (22/79 from Bengaluru and 57/79 from Mumbai) (Fig. 2). As high as 53% of participants were aged between 26 and 35 years, 40% had an undergraduate or bachelor’s degree, 45.2% were in full-time employment, 49.6% were single, and 63.5% had no children. Table 1 presents the participants’ demographics.
Figure 2.
Consort diagram illustrating the recruitment of women with PCOS for the study.
Table 1.
Participant demographics.
| Overall n (%), total n = 115 | United Kingdom n (%), total n = 36 | India n (%), total n = 79 | ||
|---|---|---|---|---|
| Age (years) | ≤17 | 1.7 | 2.8 | 1.3 |
| 18–25 | 34.8 | 22.2 | 40.5 | |
| 26–35 | 53 | 63.9 | 48.1 | |
| 36–45 | 8.7 | 5.6 | 10.1 | |
| Education level | No formal qualifications | 0.9 | 2.8 | NAa |
| GCSE or equivalent | 1.7 | 5.6 | NAa | |
| A-levels or equivalent | 9.5 | 36.1 | 5.1 | |
| Undergraduate or bachelor's degree | 40 | 46.7 | 50.6 | |
| Post-graduate degree | 31.3 | 19.4 | 36.7 | |
| Employment status | Full-time employment | 45.2 | 52.8 | 41.8 |
| Part-time employment | 11.3 | 22.2 | 6.3 | |
| No paid work | 40.9 | 19.4 | 50.6 | |
| Retired | 0.9 | NAa | 1.3 |
aNA, not applicable.
The rate of questionnaire completion was 98.3% (113/115), 97.4% (112/115), 93.04% (107/115), and 84.3% (97/115) for HADS, BICI, BAOP, and FSFI, respectively.
A total of 56.5% (65/115) had anxiety (HADS anxiety score: median (IQR)-11 (8–14)) and 16.5% (19/115) had depression (HADS depression score: 7 (4–9.5)). As high as 10.7% and 46% had borderline anxiety and depression, respectively, and 29.6% (34/115) had BDD (BICI ≥72); the median BICI score in the overall cohort was 57.8 (IQR 42.3–75). The median score for BAOP was 15.5 (IQR 13–18), where a higher score indicates stronger beliefs that people with obesity cannot control their weight (18). The overall results of the FSFI questionnaire had a median score of 20.4 (IQR 7.5–25.2). The FSFI domains scores were as follows: desire (3.6 (2.4–3.6)), arousal (3.3 (0.75–4.2)), lubrication (4.2 (0.0–5.25)), orgasm (3.2 [0.0-5.2]), satisfaction (3.6 (2.4–4.8)), and pain (2.0 (0.0–4.4)).
Country of residence and impact on emotional and psychosexual well-being
Emotional and psychosexual well-being were investigated and compared between women from the UK (36/115) and India (79/115). There is a trend for a higher incidence of anxiety (UK vs India: 50.0% vs 59.5%; P = 0.483), depression (13.9% vs 17.7%; P = 0.529), and sexual dysfunction (overall score: 23.1 vs 17.3; P = 0.413) in people from India, compared to those from the UK. Conversely, people in the UK had greater trends for having BDD (36.1% vs 26.6%; P = 0.208). However, the difference in emotional, psychological and sexual well-being across countries was not statistically significant when adjusted for age, educational status, marital status, and parity (Tables 2 and 3).
Table 2.
Scores of validated questionnaires based on country of birth. Linear regression model, adjusted for age category, level of education, marital status, and parity.
| United Kingdom (n = 36) (reference) | India (n = 79) | Adjusted coefficient (95% CI) | P-value | |
|---|---|---|---|---|
| HADS anxiety score | 11 (7.75–12.25)a | 12 (8–14)a | 0.373 (–3.112 to 3.858) | 0.832 |
| HADS depression score | 5 (2.75–9.25)a | 8 (4–10)a | 0.227 (–2.839 to 3.292) | 0.883 |
| BICI | 69 (55.75–75)a | 52.5 (39.75–75)a | –12.798 (–27.768 to 2.172) | 0.093 |
| BAOP | 16 (13.25–18.875)a | 15 (12.5–17.5)a | –0-.972 (–4.409 to 2.464) | 0.575 |
| FSFI overall | 23.1 (13.15–26.15)a | 17.65 (6.85–24.45)a | –3.038 (–10.394 to 4.317) | 0.413 |
| FSFI desire | 3.0 (1.8–3.6)a | 3.6 (2.4–4.2)a | 0.106 (–0.8180 to 1.031) | 0.819 |
| FSFI arousal | 3.3 (1.8–4.2)a | 3.0 (0.0–4.13)a | –0.640 (–2.216 to 0.936) | 0.421 |
| FSFI lubrication | 4.5 (3.0–6.0)a | 3.6 (0.0–5.03)a | –0.843 (–2.829 to 1.143) | 0.400 |
| FSFI orgasm | 4.0 (1.8–5.2)a | 2.4 (0.0–5.1)a | –0.755 (–2.667 to 1.157) | 0.434 |
| FSFI satisfaction | 3.6 (2.4–5.0)a | 3.6 (2.4–4.8)a | –0.136 (–1.446 to 1.173) | 0.836 |
| FSFI pain | 4.0 (0.0–5.8)a | 0.0 (0.0–3.9)a | –0.771 (–2.440 to 0.898) | 0.360 |
aMedian (IQR).
BAOP, Belief about Obese Persons; BICI, Body Image Concern Inventory; FSFI, Female Sexual Function Index; HADS, Hospital Anxiety and Depression Scale.
Table 3.
Diagnoses of anxiety and depression (based on hospital anxiety and depression scores) and BDD (based on Body Image Concern Inventory) in women with polycystic ovary syndrome from India and the UK. Logistic regression model, adjusted for age category, level of education, marital status, and parity.
| United Kingdom (n = 36) (reference) | India (n = 79) | Adjusted odds ratio (95% CI) | P-value | |
|---|---|---|---|---|
| Anxiety | 18 (50.0%) | 47 (59.5%) | 2.03 (0.28–14.77) | 0.48 |
| Depression | 5 (13.9%) | 14 (17.7%) | 2.27 (0.18–29.23) | 0.53 |
| Body dysmorphic disorder | 13 (36.1%) | 21 (26.6%) | 0.28 (0.04–2.05) | 0.21 |
Ethnicity and impact on emotional and psychosexual well-being
The emotional and psychosexual well-being were further compared between people of White ethnicity (17/115) and non-White ethnicity (98/115) living in both UK and India. There is a trend for a higher prevalence of anxiety (White vs non-White: 52.9% vs 57.1%; P = 0.056), depression (5.9% vs 18.4%; P = 0.287), and sexual dysfunction (overall score: 23.2 vs 18.5; P = 0.786) in people of non-White ethnicity. Conversely, people of White ethnicity had greater trends for having BDD (41.2% vs 27.6%; P = 0.478). However, the difference in emotional, psychological, and sexual well-being across ethnicities was not statistically significant when adjusted for age, educational status, marital status, and parity (Supplementary Tables 1 and 2).
Lifestyle advice and intervention planning
A total of 59 of 115 women who completed the pre-clinic survey and have PCOS completed the post-clinic survey. As high as 96.6% of women reported either a ‘very good’ (78.0%) or a ‘good’ overall experience of the clinic service; 93.2% of women felt they could ask important questions to the doctor and receive answers they could understand; and 96.6% of women felt involved in the decision-making process surrounding their care and treatment in the clinic.
A total of 28.8% (Birmingham vs India: 36.8% vs 25%) of women with PCOS reported they were screened for anxiety during consultation, 27.1% (42.1% vs 20%) for depressive symptoms, 45.8% (52.6% vs 42.5%) for body image concerns, 20.3% (15.8% vs 22.5%) for disordered eating, and 22% (26.3% vs 20%) for obstructive sleep apnoea during their consultation. Lifestyle advice was discussed in 74.6% of consultations, and the following were taken into consideration during this discussion: participants’ preference (49.2%; Birmingham vs India: 47.4% vs 50%), culture (32.2%; 21.1% vs 37.5%), ethnicity (30.5%; 21.1% vs 35%), socioeconomic background (37.3%; 26.3% vs 42.5%), and BMI (42.4%; 57.9% vs 35%). Clinicians made the following recommendations to women as part of lifestyle advice: healthy eating (61%; 57.9% vs 62.5%), regular physical activity (61%; 47.4% vs 67.5%), behavioural strategies (25.4%; 10.5% vs 32.5%), and SMART goals (23.7%; 5.3% vs 32.5%). Clinicians referred women with PCOS to dieticians (30.5%; 15.8% vs 37.5%), weight management specialist physicians (16.9%; 10.5% vs 20%), psychologists (8.5%; 0.0% vs 12.5), physiotherapists (5.1%; 0.0% vs 7.5%), weight management specialist surgeons (3.4%; 0.0% vs 5%), and commercial weight management programmes (6.8%; 0.0% vs 10%).
Discussion
There is a high incidence of emotional ill-being and psychosexual dysfunction in women with PCOS, which warrants better screening. While the current screening for emotional well-being is inadequate regardless of the model of care, the screening rate was better with the pre-clinic survey compared to ad hoc screening in routine MoC. The frequency of screening rates during consultations for anxiety, depression, and body image concerns as reported by women with POCS in post-clinic surveys were 28.8%, 27.1%, and 45.8%. In comparison, 98.3% and 97.4% of women with PCOS completed the pre-clinic questionnaires (HADS and BICI, respectively) to screen anxiety, depression, and body image concerns. While accepting the limitations in the frequency of post-clinic survey completion and recall bias, the pre-clinic survey completion rate suggests a better screening than screening during consultation. Existing literature also suggests limited screening for emotional well-being, which aligns with our paper’s values (19, 20, 21). Therefore, such screening tools could help address the unmet need. This study notes a high survey completion rate amongst women who agreed to participate in screening. However, a few factors still affect agreeance to complete pre-clinic surveys. This has been acknowledged as a limitation in this paper and needs to be considered when implementing this screening strategy for future interventions.
The post-clinic survey identified that although most participants had a positive experience during the clinic visits, there was a varied exposure for women with PCOS regarding lifestyle advice and referral to specialist services. This is another area of unmet needs, and clinicians need resources and services to signpost patients to evidence-based information to standardise advice and information dissemination.
Although we did not find a significant difference across ethnicities or countries of residence, there was a trend towards a predisposition for non-White ethnicity and people from India to have emotional and sexual ill-being, as noticed in our previous study (22). The lack of significance may be due to the low sample size in the current study as noted by wider confidence intervals.
Several studies report the benefits of multidisciplinary clinics with psychological input (23, 24, 25). However, there is limited information on how the patients were screened, which is an important information to enable other similar services to implement such practices. A few studies report limited screening for emotional well-being, mainly focusing on anxiety and depression (19, 20). Torres-Zegarra et al. report a multidisciplinary clinic where a psychologist evaluated all attendees of a PCOS clinic for mental health symptoms, appetite self-regulation, and emotional eating (26). While the model described by Torres-Zegarra et al. ensures comprehensive work-up, it requires significant resources which is currently stretched to its limit in the UK. Our model of pre-clinic screening using validated questionnaires simplifies the screening process with modest use of resources with pick-up rates better than a clinician screening within the consultation time. Adopting the HADS questionnaire at the beginning of routine consultation may be clinically beneficial and efficient in screening for psychological ill-being. If this screens positively for anxiety or depression, patients can be offered further screening targeting psychosexual health, such as the BICI, BAOP, and FSFI questionnaires. This also frees up valuable consultation time to focus on patient concerns and individualise approaches for those who screen positively for emotional or psychosexual ill-being.
The post-clinic survey in our study provides an easy way to measure patient experiences which can then be used to fine-tune the MoC to meet patient needs. There is further potential to match pre- and post-clinic surveys to explore the provision of individualised care.
This study was focused on improving screening rates of psychological well-being in women with PCOS. This study highlights how pre-standardised questionnaires can be beneficial in such screening. Future studies can focus on further investigating the clinical outcomes of specialist interventions following screening for managing anxiety, depression, and BDD. This will be useful to guide holistic management in newly diagnosed PCOS associated with psychological illnesses.
We did not screen for eating disorders, but this will be a feasible addition to the pre-clinic screening surveys. The post-clinic survey can also assess patient experiences which can be used to fine-tune the model to suit the patient needs. Language barrier may be an issue in those women who do not speak English. However, this was <10% of those who were screened during our study. With increasing global illiteracy, we anticipate this to be a major issue in the long term. The small sample size and participants from only two countries limit generalising these results. Given that PCOS can present with various symptoms, including hirsutism, subfertility, and metabolic issues, it was important to investigate the employment of specialists in such reproductive clinics. Our study looked at different clinic compositions at different centres; not all clinics had the same specialists. This may have led to an element of selection bias of women attending this clinic and can be considered a limiting factor of this paper. The isolating nature of the pandemic could have also been a confounding factor affecting emotional and psychosexual well-being in women with PCOS. However, the prospective nature of the study and positive experience in the clinic may suggest the latter may not have had a significant impact on our findings. Furthermore, results were adjusted for patient demographics, reducing the study’s confounding bias.
Conclusion
We describe three MoCs for PCOS where screening rates for emotional and psychosexual well-being were improved through pre-clinic surveys, and variations in patient experience were identified through a post-clinic survey with modest resources. The high incidence of both emotional concerns and psychosexual dysfunction in women with PCOS elicts the need to increase regularity and standardisation of screening for psychological well-being in this cohort. Further research with larger cohorts spread across multiple countries is warranted to study the various factors affecting the screening and management of emotional and psychological well-being.
Supplementary Materials
Declaration of interest
None.
Funding
There was no funding for this study.
References
- 1.Kempegowda P Melson E Manolopoulos KN Arlt W & O’Reilly MW. Implicating androgen excess in propagating metabolic disease in polycystic ovary syndrome. Therapeutic Advances in Endocrinology and Metabolism 2020112042018820934319. ( 10.1177/2042018820934319) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Al Wattar BH, Teede H, Garad R, Franks S, Balen A, Bhide P, Piltonen T, Romualdi D, Laven J, Thondan M, et al. Harmonising research outcomes for polycystic ovary syndrome: an international multi-stakeholder core outcome set. Human Reproduction 202035404–412. ( 10.1093/humrep/dez272) [DOI] [PubMed] [Google Scholar]
- 3.Joham AE Norman RJ Stener-Victorin E Legro RS Franks S Moran LJ Boyle J & Teede HJ. Polycystic ovary syndrome. Lancet. Diabetes and Endocrinology 202210668–680. ( 10.1016/S2213-8587(2200163-2) [DOI] [PubMed] [Google Scholar]
- 4.Tay CT Pirotta S Teede HJ Moran LJ Robinson T Skouteris H Joham AE & Lim SS. Polycystic ovary syndrome models of care: a review and qualitative evaluation of a guideline-recommended integrated care. Seminars in Reproductive Medicine 202139133–142. ( 10.1055/s-0041-1727191) [DOI] [PubMed] [Google Scholar]
- 5.Deeks AA Gibson-Helm ME Paul E & Teede HJ. Is having polycystic ovary syndrome a predictor of poor psychological function including anxiety and depression? Human Reproduction 2011261399–1407. ( 10.1093/humrep/der071) [DOI] [PubMed] [Google Scholar]
- 6.Dokras A Stener-Victorin E Yildiz BO Li R Ottey S Shah D Epperson N & Teede H. Androgen Excess- polycystic ovary syndrome Society: position statement on depression, anxiety, quality of life, and eating disorders in polycystic ovary syndrome. Fertility and Sterility 2018109888–899. ( 10.1016/j.fertnstert.2018.01.038) [DOI] [PubMed] [Google Scholar]
- 7.Alur-Gupta S Chemerinski A Liu C Lipson J Allison K Sammel MD & Dokras A. Body image distress increased in women with PCOS and mediates depression and anxiety. Fertility and Sterility 2019112930–938.e1. ( 10.1016/j.fertnstert.2019.06.018) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Teede HJ, Misso ML, Costello MF, Dokras A, Laven J, Moran L, Piltonen T, Norman RJ, Andersen M, Azziz R, et al. Recommendations from the international evidence-based guideline for the assessment and management of polycystic ovary syndrome. Fertility and Sterility 2018110364–379. ( 10.1016/j.fertnstert.2018.05.004) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Polycystic ovary syndrome, Health topics A to Z, CKS. NICE. (available at: https://cks.nice.org.uk/topics/polycystic-ovary-syndrome/#!scenario) [Google Scholar]
- 10.Bonner A. PMON218 direct costs of mental health disorders in PCOS: systematic review and meta-analysis. Journal of the Endocrine Society 20226(Supplement_1) A711–A712. ( 10.1210/jendso/bvac150.1467) [DOI] [Google Scholar]
- 11.Ding T Hardiman PJ Petersen I & Baio G. Incidence and prevalence of diabetes and cost of illness analysis of polycystic ovary syndrome: a Bayesian modelling study. Human Reproduction 2018331299–1306. ( 10.1093/humrep/dey093) [DOI] [PubMed] [Google Scholar]
- 12.Patient Satisfaction Surveys. NEJM Catalyst. (available at: https://catalyst.nejm.org/doi/full/10.1056/CAT.18.0288) [Google Scholar]
- 13.Shucard H Muller E Johnson J Walker J Elmore JG Payne TH Berman J & Jackson SL. Clinical use of an electronic pre-visit questionnaire soliciting patient visit goals and interim history: a retrospective comparison between safety-net and non-safety-net clinics. Health Services Research and Managerial Epidemiology 202291–7. ( 10.1177/23333928221080336) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zigmond AS & Snaith RP. The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica 198367361–370. ( 10.1111/j.1600-0447.1983.tb09716.x) [DOI] [PubMed] [Google Scholar]
- 15.Littleton HL Axsom D & Pury CLS. Development of the body image concern inventory. Behaviour Research and Therapy 200543229–241. ( 10.1016/j.brat.2003.12.006) [DOI] [PubMed] [Google Scholar]
- 16.Allison DB Basile VC & Yuker HE. The measurement of attitudes toward and beliefs about obese persons. International Journal of Eating Disorders 199110599–607. (). [DOI] [Google Scholar]
- 17.Rosen R Brown C Heiman J Leiblum S Meston C Shabsigh R Ferguson D & D’Agostino R. The Female Sexual Function Index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex and Marital Therapy 200026191–208. ( 10.1080/009262300278597) [DOI] [PubMed] [Google Scholar]
- 18.Tsai MC Strong C Latner JD Lin YC Pakpour AH Lin CY & Wang SM. Attitudes toward and beliefs about obese persons across Hong Kong and Taiwan: wording effects and measurement invariance. Health and Quality of Life Outcomes 201917134. ( 10.1186/s12955-019-1198-6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boyle J Hollands G Beck S Hampel G Wapau H Arnot M Browne L Teede HJ & Moran LJ. Process evaluation of a pilot evidence-based polycystic ovary syndrome clinic in the Torres Strait. Australian Journal of Rural Health 201725175–181. ( 10.1111/ajr.12288) [DOI] [PubMed] [Google Scholar]
- 20.Tay CT Moran LJ Wijeyaratne CN Redman LM Norman RJ Teede HJ & Joham AE. Integrated model of care for polycystic ovary syndrome. Seminars in Reproductive Medicine 20183686–94. ( 10.1055/s-0038-1667310) [DOI] [PubMed] [Google Scholar]
- 21.Melson E, Davitadze M, Malhotra K, Mousa A, Teede H, Boivin J, Thondan M, Tay CT, Kempegowda P. & PCOS SEva Working Group. A systematic review of models of care for polycystic ovary syndrome highlights the gap in the literature, especially in developing countries. Frontiers in Endocrinology 2023141217468. ( 10.3389/fendo.2023.1217468) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sheikh J, Hebbar M, Zia N, Wicks S, Jayaprakash S, Narendran A, Khalil H, Melson E, Busby M, Tahrani A, et al. Increased anxiety, depression and body dysmorphia in women with polycystic ovary syndrome: results from blue morpho survey. Endocrine Abstracts 202173AEP175. ( 10.1530/endoabs.73.AEP175) [DOI] [Google Scholar]
- 23.Ghosh D Murphy C & Elsheikh M. A 2 year audit of the polycystic ovary syndrome (PCOS) clinic at the Royal Berkshire Hospital. Endocrine Abstracts 20059P79. (available at: https://www.endocrine-abstracts.org/ea/0009/ea0009p79) [Google Scholar]
- 24.Bekx MT Connor EC & Allen DB. Characteristics of adolescents presenting to a multidisciplinary clinic for polycystic ovarian syndrome. Journal of Pediatric and Adolescent Gynecology 2010237–10. ( 10.1016/j.jpag.2009.04.004) [DOI] [PubMed] [Google Scholar]
- 25.Geier LM Bekx MT & Connor EL. Factors contributing to initial weight loss among adolescents with polycystic ovary syndrome. Journal of Pediatric and Adolescent Gynecology 201225367–370. ( 10.1016/j.jpag.2012.06.008) [DOI] [PubMed] [Google Scholar]
- 26.Torres-Zegarra C Sundararajan D Benson J Seagle H Witten M Walders-Abramson N Simon SL Huguelet P Nokoff NJ & Cree-Green M. Care for adolescents with polycystic ovary syndrome: development and prescribing patterns of a multidisciplinary clinic. Journal of Pediatric and Adolescent Gynecology 202134617–625. ( 10.1016/j.jpag.2021.02.002) [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



 This work is licensed under a
This work is licensed under a