Abstract
The MICs of 13 antibiotics (doxycycline, thiamphenicol, rifampin, amoxicillin, gentamicin, co-trimoxazole, ciprofloxacin, pefloxacin, ofloxacin, erythromycin, josamycin, clarithromycin, and pristinamycin) were determined for 27 available rickettsial species or strains. We used two in vitro cell culture methods described previously: the plaque assay and the microplaque colorimetric assay. Our results confirm the susceptibilities of rickettsiae to doxycycline, thiamphenicol, and fluoroquinolones. Beta-lactams, aminoglycosides, and co-trimoxazole were not active. Typhus group rickettsiae were susceptible to all macrolides tested, whereas the spotted fever group rickettsiae, R. bellii, and R. canada were more resistant, with josamycin, a safe alternative for the treatment of Mediterranean spotted fever, being the most effective compound. Strain Bar 29, R. massiliae, R. montana, R. aeschlimannii, and R. rhipicephali, which are members of the same phylogenetic subgroup, were more resistant to rifampin than the other rickettsiae tested. Heterogeneity in susceptibility to rifampin, which we report for the first time, may explain in vivo discrepancies in the effectiveness of this antibiotic for the treatment of rickettsial diseases. We hypothesize that rifampin resistance and erythromycin susceptibility may reflect a divergence during the evolution of rickettsiae.
All members of the genus Rickettsia are obligate gram-negative intracellular bacteria. The genus comprises typhus group rickettsiae which includes R. prowazekii, the agent of epidemic typhus, and R. typhi, the agent of murine typhus; R. tsutsugamushi, reclassified as Orienta tsutsugamushi (41), the agent of scrub typhus; and spotted fever group (SFG) rickettsiae. For three species, classification remains to be firmly established: R. canada and R. bellii, which were previously classified in the typhus and SFG rickettsiae, respectively, and which may represent new groups (35); and R. felis, the agent of pseudotyphus described in 1994 in California (38).
The number of recognized SFG rickettsioses has recently increased. The six SFG rickettsioses previously described are Rocky Mountain spotted fever caused by R. rickettsii, Mediterranean spotted fever caused by R. conorii, Siberian tick typhus caused by R. sibirica, Israeli spotted fever caused by R. conorii serotype israeli, Queensland tick typhus caused by R. australis, and rickettsialpox caused by R. akari. Since 1984, six new SFG rickettsioses were described: the Japanese spotted fever caused by R. japonica described in 1984 (43), Flinders Island spotted fever caused by R. honei described in 1991 (40), Astrakhan fever caused by R. conorii serotype astrakhan reported in 1991 (41), African tick-bite fever caused by R. africae described in 1992 (17), a new spotted fever due to “Rickettsia mongolotimonae” reported in 1996 (31, 48) in France, and very recently, R. slovaca isolated in our laboratory from a tick from a patient (32). Other SFG rickettsiae isolated from arthropods include R. rhipicephali, R. montana, R. parkeri, and Thai tick typhus rickettsiae and, more recently, R. massiliae isolated in the Mediterranean area (2), R. helvetica isolated in Switzerland (1), strain Bar 29 isolated in Spain (3), and R. aeschlimannii isolated in Morocco (4).
Tetracyclines remain the antibiotics of choice for the treatment of rickettsial diseases, with fluoroquinolones used as alternative drugs (29). Adverse effects from both tetracyclines and fluoroquinolones limit their use, and these antibiotics are contraindicated in pregnant women and young children. Chloramphenicol, which has been proposed as an alternative, is poorly effective in vitro and may induce bone marrow aplasia. Josamycin has been used successfully to treat pregnant women and children suffering from Mediterranean spotted fever (5). There is a need for reliable therapeutic alternatives to tetracyclines for other rickettsial diseases and for drugs that can be administered to children and pregnant women. Reports of the in vitro susceptibilities of the rickettsiae are limited, and only a few species (mainly R. conorii and R. rickettsii) have been extensively studied (3, 20). Here we report the first extensive study evaluating the in vitro susceptibilities of almost all known rickettsial species and describe the heterogeneity of the antibiotic susceptibilities among the rickettsiae.
MATERIALS AND METHODS
Antibiotic preparation.
Stock solutions of the 13 antibiotics to be tested were prepared and stored at −20°C. The antibiotics used were doxycycline (Pfizer, Neuilly, France), gentamicin (Dakota Pharm, Creteil, France), rifampin (Cassenne, Puteaux, France), erythromycin (Abbott Laboratories, Rungis, France), co-trimoxazole (Roche, Paris, France), thiamphenicol (Sanofi Winthrop, Gentilly, France), amoxicillin (Beecham Laboratories, Nanterre, France), pefloxacin (Rhône Poulenc Rorer, Neuilly sur Seyne, France), ofloxacin (Diamant, Puteaux, France), ciprofloxacin (Bayer Pharma, Sens, France), clarithromycin (Abbott Laboratories), josamycin (Rhône Poulenc Rorer), and pristinamycin (Rhône Poulenc Rorer). Stock solutions were prepared by solubilization of antibiotic powders in sterile distilled water; however, clarithromycin, josamycin, and pristinamycin were first dissolved in methanol before being diluted in sterile distilled water. Final antibiotic solutions were made up fresh before use by dilution of concentrated stock solutions in Eagle’s minimal essential medium (MEM) supplemented with 4% fetal calf serum and 2 mM l-glutamine.
Rickettsial strains.
The rickettsial strains studied are listed in Table 1. They were grown in Vero cell monolayers cultured in MEM supplemented with 4% fetal calf serum and 2 mM l-glutamine. Cell cultures were incubated at 32°C, and the rates of infection of the Vero cells were monitored daily by Gimenez staining (9) of cell samples obtained by gentle scraping of the cell monolayers. Rickettsiae were harvested after 3 to 6 days of incubation of cell cultures, when multiplication was optimal.
TABLE 1.
Rickettsial strains, sources of the strains, strain origins, and human diseases caused by pathogenic strains
| Strain | Sourcea | Origin | Disease |
|---|---|---|---|
| R. rickettsii R | ATCC | Dermacentor andersoni | Rocky Mountain SFb |
| R. conorii | |||
| Moroccan | ATCC | Unknown | Mediterranean SF |
| Seven | ATCC | Unknown | Mediterranean SF |
| M1 | GRIC | Rhipicephalus sanguineus | Unknown |
| Israeli CDC1 | G. A. Dasch | Human | Israeli SF |
| Astrakhan A-167 | UR | Rhipicephalus pumilio | Astrakhan fever |
| R. sibirica 246 | GRIC | Dermacentor nuttali | Siberian tick typhus |
| R. australis Phillips | G. A. Dasch | Human | Queensland tick typhus |
| R. akari MK | ATCC | Human | Rickettsialpox |
| R. japonica YM | D. H. Walker | Human | Oriental SF |
| R. honei RB | GRIC | Human | Flinders Island SF |
| R. africae ESF-5 | G. A. Dasch | Amblyomma variegatum | African tick bite fever |
| “R. mongolotimonae” | UR | Haemophysalis asaiaticum | SF |
| R. slovaca | UR | Human | SF |
| R. slovaca 13-B | G. A. Dasch | Dermacentor marginatus | Unknown |
| R. rhipicephali 3-7-6 | G. A. Dasch | Rhipicephalus sanguineus | Unknown |
| R. montana VR-611 | ATCC | Dermacentor sp. | Unknown |
| R. parkeri Maculatum 20 | D. H. Walker | Amblyomma maculatum | Unknown |
| R. massiliae Mtu1 | UR | Rhipicephalus turanicus | Unknown |
| Bar 29 | UR | Rhipicephalus sanguineus | Unknown |
| “R. aeschlimanii” | UR | Hyaloma marginatum | Unknown |
| Thai tick typhus rickettsia | G. A. Dasch | Ixodes or Rhipicephalus | Unknown |
| R. helvetica C6P9 | W. Burgdorfer | Ixodes ricinus | Unknown |
| R. bellii 369L42-1 | D. H. Walker | Dermacentor variabilis | Unknown |
| R. canada 2678 | GRIC | Haemophysalis | Unknown |
| R. prowazekii Breinl | ATCC | Human | Epidemic typhus |
| R. typhi Wilmington | ATCC | Human | Murine typhus |
ATCC, American Type Culture Collection, Rockville, Md.; GRIC, Gamaleya Research Institute Collection; G. A. Dasch, Naval Medical Research Institute, Bethesda, Md.; UR, Unité des Rickettsies, CNRS UPRES A, Marseille, France; D. H. Walker, University of Texas, Galveston; W. Burgdorfer, Rocky Mountain Laboratory, Hamilton, Mont.
SF, spotted fever.
Plaque formation with R. africae, strain Bar 29, R. aeschlimannii, “R. mongolotimonae,” R. japonica, and R. slovaca in L929 and Vero cells.
The rickettsial species R. africae, strain Bar 29, R. aeschlimannii, “R. mongolotimonae,” R. japonica, and R. slovaca did not cause cytopathic effects in primary cultures. In order to perform susceptibility tests by both the plaque assay and the dye uptake assay, we adapted these species to different cell cultures to obtain plaque formation. Infected Vero cells were harvested in MEM, mechanically disrupted, and centrifuged at 700 × g for 10 min, and the supernatant was pelleted by centrifugation at 7,500 rpm for 10 min (Sorvall RC-2B). The supernatant was discarded, and the rickettsiae were inoculated onto L929 cell monolayers cultured in MEM with 4% fetal calf serum and 2 mM l-glutamine. After 1 h of gentle agitation at room temperature, 25 ml of fresh medium was added to the cultures, which were incubated at 32°C for 5 to 7 days. The procedure was repeated until cytopathic effects on L929 cells became apparent. Rickettsiae were then harvested, purified as described above, and inoculated onto Vero cells. Further passages in Vero cell cultures were carried out as described above until cytopathic effects occurred in this cell line.
Antibiotic susceptibility testing.
The bacteriostatic activities of 13 antibiotics were evaluated by a dye uptake assay and a plaque assay as described previously (26). During antibiotic challenges, the lack of toxic effects of each antibiotic on Vero cells was verified.
(i) Plaque assay.
Confluent Vero cells, which were grown in MEM supplemented with 4% fetal calf serum and 2 mM l-glutamine in petri dishes, were infected with 1 ml of a solution containing 104 PFU of rickettsiae as described previously (26). After rocking the petri dishes for 1 h at 22°C, the infected cells were overlaid with 4 ml of MEM containing 2% fetal calf serum and 0.5% agar. The antibiotics were added to a volume of 200 μl at twofold serial final concentrations. The petri dishes were incubated for 7 to 10 days at 37°C in a 5% CO2 incubator. The cells were then fixed with 4% formaldehyde and stained with 1% crystal violet in 20% ethanol (26). The MIC was the lowest concentration of antibiotic causing complete inhibition of plaque formation. Experiments were carried out in duplicate to verify the results.
(ii) Dye uptake assay.
Vero cells, grown in MEM supplemented with 4% fetal calf serum and 2 mM l-glutamine in microtiter plates, were inoculated with rickettsiae so that 2,000 PFU of rickettsiae was added to each well of the second row, 200 PFU was added to each well of the third row, and 20 PFU was added to each well of the fourth row. The first row contained only MEM and was used as an uninfected control, whereas 2,000 PFU of rickettsiae was added to each well of the next eight rows for the antibiotic assay. Four serial dilutions of each antibiotic were tested. The plates were incubated for 5 to 7 days at 37°C in a 5% CO2 incubator, then the cell culture supernatant of each well was replaced by 50 μl of neutral red dye (0.15% in saline [pH 5.5]), and the plates were incubated for 1 h at 37°C in a 5% CO2 incubator, as described previously (26). Dye not taken up by the cells was removed by three washes with phosphate-buffered saline (pH 6.5), and the dye absorbed by the cells was extracted by the addition 100 μl of phosphate ethanol buffer (10% ethanol in phosphate-buffered saline adjusted to pH 4.2) per well. The optical density (OD) at 492 nm of the cell supernatant in each well was determined with a spectrophotometer. The MIC was the first dilution for which the mean OD at 492 nm of the corresponding row was between the OD of the control cell row and the OD of the row containing 20 PFU per well. Experiments were carried out in duplicate to verify the results.
RESULTS
Plaque formation with R. africae, strain Bar 29, R. aeschlimannii, “R. mongolotimonae,” R. japonica, and R. slovaca in L929 and Vero cells.
Attempts to produce cytopathic effects and plaque formation with the species R. africae, strain Bar 29, R. aeschlimannii, “R. mongolotimonae,” R. japonica, and R. slovaca in L929 and Vero cells were successful. Plaque formation in L929 cells occurred after the first passage for R. japonica and after the second passage for the other strains. Plaque formation in Vero cells inoculated with L929 cell-adapted rickettsiae appeared after the second passage for R. japonica, the fourth passage for R. africae and strain Bar 29, and the fifth passage for “R. mongolotimonae,” R. aeschlimannii, and R. slovaca. Cytopathic effects were visible in Vero cells after 7 to 10 days following infection with rickettsiae.
Plaque morphology.
The time for plaque formation and the sizes of the plaques varied among the different rickettsial species studied. In the first group, including R. rickettsii, R. conorii (Moroccan, M1, and Seven strains), R. australis, Thai tick typhus rickettsia, Astrakhan fever rickettsia, R. honei, R. israeli, R. montana, R. parkeri, and R. bellii, plaque formation occurred within 5 days after infection, and the plaques were 2 to 3 mm in diameter. In contrast, in the second group, including R. canada, R. akari, R. sibirica, R. aeschlimannii, strain Bar 29, R. rhipicephali, R. slovaca, “R. mongolotimonae,” R. africae, R. japonica, R. sibirica, R. massiliae, and R. helvetica, plaque formation was observed only after up to 8 days of incubation and the plaques were smaller (0.5 to 1 mm in diameter). With the typhus group rickettsia, plaque formation occurred within 7 days after infection, and the plaques were 0.5 to 1 mm in diameter.
Antibiotic susceptibilities.
The results of the studies of the in vitro susceptibilities of rickettsiae to antibiotics are summarized in Table 2. The antibiotics tested in the dye uptake and the plaque assays were not toxic for the Vero cells at the concentrations used. Results obtained from the dye uptake endpoint were identical to or within one twofold dilution of the plaque assay results. Sensitivities to amoxicillin, gentamicin, and co-trimoxazole were poor. A bacteriostatic effect was shown with amoxicillin at concentrations of 128 to 256 μg/ml and with gentamicin at concentrations of 4 to 16 μg/ml. Doxycycline was the most effective antibiotic against all strains tested, with MICs ranging from 0.06 to 0.25 μg/ml. The MICs of thiamphenicol ranged from 0.5 to 4 μg/ml, while the MICs were 0.25 to 1 μg/ml for ciprofloxacin, 0.25 to 2 μg/ml for ofloxacin, and 0.5 to 2 μg/ml for pefloxacin. Of the macrolide antibiotics, josamycin was the most effective, with MICs ranging from 0.5 to 1 μg/ml, while the MICs of pristinamycin were 1 to 8 μg/ml and those of clarithromycin were 0.5 to 4 μg/ml. Erythromycin at concentrations ranging from 2 to 8 μg/ml was bacteriostatic for most of the rickettsial strains tested, whereas typhus group rickettsiae were more susceptible (MICs, 0.125 to 1 μg/ml). Susceptibilities to rifampin varied, with R. prowazekii, R. typhi, R. canada, R. bellii, and most SFG rickettsiae being susceptible to rifampin (MIC range, 0.03 to 1 μg/ml), while R. massiliae, R. montana, R. rhipicephali, R. aeschlimannii, and strain Bar 29 were more resistant (MICs, 2 to 4 μg/ml).
TABLE 2.
In vitro susceptibilities of rickettsiae to antibiotics
| Antibiotic | MIC range (μg/ml)a
|
||||
|---|---|---|---|---|---|
| Group 1 | Group 2 | Group 3 | Group 4 | Group 5 | |
| Doxycycline | 0.06–0.125 | 0.06–0.125 | 0.06–0.25 | 0.06–0.25 | 0.06–0.125 |
| Thiamphenicol | 0.5–2 | 0.5–2 | 0.5–4 | 0.5–2 | 1–2 |
| Rifampin | 0.06–1 | 0.03–0.5 | 0.06–0.5 | 2–4 | 0.06–0.25 |
| Amoxicillin | 128 | 128–256 | 128–256 | 128–256 | 128 |
| Gentamicin | 4–8 | 8–16 | 8–16 | 8–16 | 16 |
| Co-trimoxazoleb | >8/2 | >8/2 | >8/2 | >8/2 | >8/2 |
| Erythromycin | 2–8 | 2–8 | 2–8 | 1–8 | 0.125–1 |
| Clarithromycin | 1–4 | 0.5–4 | 0.5–4 | 0.5–2 | 0.5–1 |
| Josamycin | 0.5–1 | 0.5–1 | 0.5–1 | 0.5–2 | 0.5–1 |
| Pristinamycin | 1–4 | 1–8 | 2–4 | 1–4 | 2–4 |
| Ciprofloxacin | 0.5–1 | 0.5–1 | 0.25–1 | 0.25–1 | 0.5–1 |
| Ofloxacin | 0.5–1 | 0.5–1 | 0.25–2 | 0.5–1 | 1 |
| Pefloxacin | 0.5–2 | 0.5–1 | 0.5–1 | 0.5–1 | 1 |
MIC ranges determined by both the plaque assay and the dye uptake assay are specified for the following five rickettsial groups: group 1, R. rickettsii, R. conorii Moroccan, Seven, and Israeli, R. sibirica, R. australis, and R. akari; group 2, R. japonica, R. honei, R. conorii Astrakhan, R. africae, “R. mongolotimonae,” strain 13B, and the human isolate of R. slovaca; group 3, R. bellii, R. canada, R. helvetica, R. conorii M1, R. parkeri, and Thai tick typhus rickettsia; group 4, Bar 29, R. massiliae, R. aeschlimanii, R. montana, R. rhipicephali; and group 5, R. typhi and R. prowazekii.
For co-trimoxazole, MICs are of sulfamethoxazole/trimethoprim.
DISCUSSION
Rickettsiae are gram-negative bacteria primarily associated with arthropods, which are the vectors for human infections. Since they are obligate intracellular bacteria, in vitro studies of their susceptibilities to antibiotics necessitate the use of cell culture systems. Only limited studies of the in vitro antibiotic susceptibilities of SFG rickettsiae other than R. conorii and R. rickettsii have been reported (3, 20). On the other hand, the number of SFG rickettsiae has recently increased as new species have been isolated by the shell vial centrifugation technique (19) and characterized by genomic studies (34, 35). The aim of our study was to determine the antibiotic susceptibilities of most of the rickettsial species described to date and to evaluate the variability in antibiotic susceptibilities among these organisms. Only “R. amblyommii,” R. felis and the AB bacterium, which were not available to us, were excluded from our study.
Previous reports have indicated that R. japonica (43), R. africae (17), and strain Bar 29 (3) did not cause cytopathic effects on Vero cell monolayers. In our study we were able to adapt R. africae, strain Bar 29, R. aeschlimannii, “R. mongolotimonae,” R. japonica, and R. slovaca to Vero cells and to induce cytopathic effects and plaque formation. Thus, all rickettsial species studied produced plaques, although we found two typical plaque morphologies. Large plaques were obtained with R. conorii and R. rickettsii strains, as described previously (44), and also with R. australis, Thai tick typhus rickettsia, Astrakhan fever rickettsia, R. honei, R. israeli, R. montana, R. parkeri, and R. bellii. In contrast, the plaques produced by R. canada, R. akari, R. sibirica, R. aeschlimannii, strain Bar 29, R. rhipicephali, R. slovaca, “R. mongolotimonae,” R. africae, R. japonica, R. sibirica, R. massiliae, and R. helvetica were smaller and resembled those observed with typhus group rickettsiae (44). Such discrepancies were reported previously (44), and the investigators hypothesized that the culture conditions and the nature of the host cells may influence the metabolism and pathogenicity of rickettsiae.
Although beta-lactams and aminoglycosides are not effective in the treatment of rickettsial diseases, we found that high concentrations of both gentamicin and amoxicillin caused rickettsiostatic activity. Wisseman et al. (45) have shown that both penicillin G and gentamicin at concentrations of 100 and 10 μg/ml, respectively, have significant inhibitory actions on R. prowazekii plaque formation, and they have shown (46) that penicillin G induces the formation of spheroplasts. Co-trimoxazole was not effective against any of the strains tested in our study, which is consistent with the results of previous experiments with R. rickettsii and R. conorii (26). Furthermore, isolation of SFG rickettsiae from ticks by use of co-trimoxazole in the culture medium to prevent overgrowth of bacterial contaminants has been reported (16), and Ruiz Beltran and Herrero Herrero (37) reported that co-trimoxazole is ineffective in the treatment of rickettsioses. Thiamphenicol was found to be less effective than its analog compound chloramphenicol (26), which has long been considered an alternative antibiotic for the treatment of patients with rickettsial diseases. The potential risk of aplastic anemia in patients treated with this drug has limited its use, however, and a relapse has been reported in a patient in Israel with Mediterranean spotted fever treated with chloramphenicol (39).
Previous experiments with R. conorii and R. rickettsii strains have shown that tetracyclines are the most effective antibiotics against these organisms (26, 28), and doxycycline remains the first-line antibiotic therapy for patients with rickettsial diseases. In our study, doxycycline was highly effective against all the strains tested. However, Yagupsky and Gross (47) described a child in Israel with an SFG rickettsioses who was treated with a 3.5-day course of doxycycline and who subsequently suffered a relapse of the disease, which indicates that the in vivo activity of doxycycline may be only rickettsiostatic. Our results show that fluoroquinolones are very effective against rickettsiae and confirm previous experiments with R. rickettsii and R. conorii (13, 21, 24, 26, 30). Patients suffering from Mediterranean spotted fever have been successfully treated with ciprofloxacin (10, 25, 36), ofloxacin (7), and pefloxacin (14). Fluoroquinolones may be considered a safe alternative to tetracyclines for the treatment of rickettsial diseases. However, the potential toxicity of doxycycline and fluoroquinolones contraindicate their use during pregnancy and childhood. The macrolide compounds may represent a safe alternative for this population. However, a wide variability in the susceptibilities of SFG rickettsiae to macrolides has been described previously (20, 26, 27). Our results confirm that typhus group rickettsiae are susceptible to macrolide compounds, whereas SFG rickettsiae are more resistant. Variability in the results of in vitro studies on the rickettsiostatic activities of the newer macrolide compounds clarithromycin and azithromycin against R. conorii and R. rickettsii have been reported (12, 18, 20). In our study, josamycin was the most effective macrolide against the SFG rickettsiae. Two macrolide antibiotics, erythromycin and josamycin, have been evaluated in vivo (5, 22). Studies have reported clinical failures with erythromycin against Mediterranean spotted fever (22, 23), whereas josamycin proved to be useful both in adults and in children (5). Josamycin may represent a safe alternative for the treatment of other rickettsial diseases in children and pregnant women, but clinical trials are needed.
Susceptibility to rifampin also varied, with R. massiliae, strain Bar 29, R. rhipicephali, R. aeschlimannii, and R. montana being more resistant than the other rickettsiae. These results are comparable to those of previous experiments with R. rickettsii, R. conorii, and strain Bar 29 (3, 26). Bella et al. (6) reported therapeutic failures with rifampin administration to children with Mediterranean spotted fever in Catalonia in Spain. We suggest that such therapeutic failures are due to rifampin-resistant rickettsiae, because acquired resistance to rifampin, yet to be studied in rickettsiae, has been shown to occur in Mycobacterium tuberculosis, Mycobacterium leprae, Escherichia coli, and Neisseria meningitidis with mutations in the rpoB gene encoding the beta subunit of the RNA polymerase (8, 11, 15, 42). These mutations prevent rifampin from binding to the target enzyme and thereby inhibit its activity.
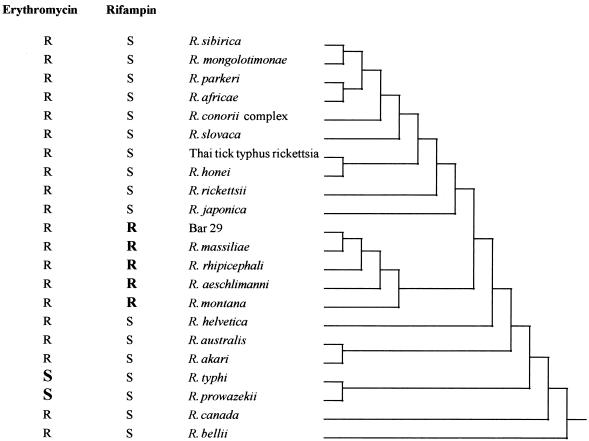
It is noteworthy that all rifampin-resistant strains belonged to a single phylogenetic subgroup (Fig. 1) that we have recently described (33, 35). Rifampin resistance may then reflect a divergence during the evolution of this subgroup in the gene encoding the RNA polymerase. Likewise, we hypothesize that the high levels of susceptibility of R. typhi and R. prowazekii to macrolides compared to those of the other rickettsiae tested may reflect a divergent strategic evolution involving susceptibility to macrolide antibiotics.
FIG. 1.
Dendrogram representing phylogenetic relationships among Rickettsia species. The dendrogram was constructed by the parsimony method and includes data determined from analysis of the gltA and ompA genes (33). The susceptibilities of Rickettsia species to erythromycin and rifampin are specified. S, susceptible; R, resistant.
In summary, our report describes the antibiotic susceptibilities of most rickettsial species to a number of antibiotics. Our results confirm the in vitro activities of doxycycline, fluoroquinolones, and josamycin, which are currently used against SFG rickettsioses. We have shown for the first time variability in susceptibility to rifampin. In vivo discrepancies in the effectiveness of rifampin for the treatment of rickettsial diseases may be due to rifampin-resistant strains, although further studies with people are needed to validate this hypothesis. The availability of a larger number of strains in the future should allow further evaluation of variability in susceptibilities to antibiotics among Rickettsia species.
ACKNOWLEDGMENT
We thank P. Kelly for reviewing the manuscript.
REFERENCES
- 1.Beati L, Peter O, Burgdorfer W, Aeschlimann A, Raoult D. Confirmation that Rickettsia helvetica sp. nov. is a distinct species of the spotted fever group of rickettsiae. Int J Syst Bacteriol. 1993;43:521–526. doi: 10.1099/00207713-43-3-521. [DOI] [PubMed] [Google Scholar]
- 2.Beati L, Raoult D. Rickettsia massiliae sp. nov., a new spotted fever group Rickettsia. Int J Syst Bacteriol. 1993;43:839–840. doi: 10.1099/00207713-43-4-839. [DOI] [PubMed] [Google Scholar]
- 3.Beati L, Roux V, Ortuno A, Castella J, Segura Porta F, Raoult D. Phenotypic and genotypic characterization of spotted fever group rickettsiae isolated from Catalan Rhipicephalus sanguineus ticks. J Clin Microbiol. 1996;34:2688–2694. doi: 10.1128/jcm.34.11.2688-2694.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beati L, Meskini M, Thiers B, Raoult D. Rickettsia aeschlimannii sp. nov., a new spotted fever group rickettsia associated with Hyalomma marginatum ticks. Int J Syst Bacteriol. 1997;47:548–554. doi: 10.1099/00207713-47-2-548. [DOI] [PubMed] [Google Scholar]
- 5.Bella F, Font B, Uriz S, Muñoz T, Espejo E, Traveria J, Serrano J A, Segura F. Randomized trial of doxycycline versus josamycin for Mediterranean spotted fever. Antimicrob Agents Chemother. 1990;34:937–938. doi: 10.1128/aac.34.5.937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bella F, Espero E, Uriz S, Serrano J A, Allegre M A, Tort J. Randomized trial of 5-day rifampin versus 1-day doxycycline therapy for MSF. J Infect Dis. 1991;164:433–434. doi: 10.1093/infdis/164.2.433. [DOI] [PubMed] [Google Scholar]
- 7.Bernard, E., M. Carles, S. Politano, C. Laffont, and P. Dellamonica. 1989. Rickettsiosis caused by Rickettsia conorii: treatment with ofloxacin. Rev. Infect. Dis. 11(Suppl. 5):989.
- 8.Carter P E, Abadi F J R, Yakubu D E, Pennington T H. Molecular characterization or rifampin-resistant Neisseria meningitidis. Antimicrob Agents Chemother. 1994;38:1256–1261. doi: 10.1128/aac.38.6.1256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gimenez D F. Staining rickettsiae in yolk-sac cultures. Stain Technol. 1964;39:135–140. doi: 10.3109/10520296409061219. [DOI] [PubMed] [Google Scholar]
- 10.Gudiol F, Pallares R, Carratala J, Bolao F, Ariza J, Rufi G, Viladrich P F. Randomized double-blind evaluation of ciprofloxacin and doxycycline for Mediterranean spotted fever. Antimicrob Agents Chemother. 1989;33:987–988. doi: 10.1128/aac.33.6.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Honore N, Cole S T. Molecular basis of rifampin resistance in Mycobacterium leprae. Antimicrob Agents Chemother. 1993;37:414–418. doi: 10.1128/aac.37.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ives T J, Manzewitsch P, Regnery R L, Butts J D, Kebede M. In vitro susceptibilities of Bartonella henselae, B. quintana, B. elizabethae, Rickettsia rickettsii, R. conorii, R. akari, and R. prowazekii to macrolide antibiotics as determined by immunofluorescent antibody analysis of infected Vero cell monolayers. Antimicrob Agents Chemother. 1997;41:578–582. doi: 10.1128/aac.41.3.578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jabarit-Aldighieri N, Torres H, Raoult D. Susceptibility of Rickettsia conorii, R. rickettsii, and Clostridium burnetii to PD 127,391, PD 131,628, pefloxacin, ofloxacin, and ciprofloxacin. Antimicrob Agents Chemother. 1992;36:2529–2532. doi: 10.1128/aac.36.11.2529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Janbon, F., O. Jonquet, J. Reynes, and A. Bertrand. 1989. Use of pefloxacin in the treatment of rickettsiosis and coxiellosis. Rev. Infect. Dis. 11(Suppl. 5):990–991.
- 15.Jin D J, Gross C A. Mapping and sequencing of mutations in the Escherichia coli rpoB gene that leads to rifampin resistance. J Mol Biol. 1988;202:45–58. doi: 10.1016/0022-2836(88)90517-7. [DOI] [PubMed] [Google Scholar]
- 16.Kelly P J, Raoult D, Mason P R. Isolation of spotted fever group rickettsiae from triturated ticks using a modification of the centrifugation shell-vial technique. Trans R Soc Trop Med Hyg. 1991;85:397–398. doi: 10.1016/0035-9203(91)90303-g. [DOI] [PubMed] [Google Scholar]
- 17.Kelly P J, Beati L, Mason P R, Matthewman L A, Roux V, Raoult D. Rickettsia africae sp. nov., the etiologic agent of African tick bite fever. Int J Syst Bacteriol. 1996;46:611–614. doi: 10.1099/00207713-46-2-611. [DOI] [PubMed] [Google Scholar]
- 18.Keysary A, Itzhaki A, Rubinstein E, Oron C, Keren G. The in vitro antirickettsial activity of macrolides. J Antimicrob Chemother. 1996;38:727–731. doi: 10.1093/jac/38.4.727. [DOI] [PubMed] [Google Scholar]
- 19.Marrero M, Raoult D. Centrifugation-shell vial technique for rapid detection of Mediterranean spotted fever rickettsia in blood culture. Am J Trop Med Hyg. 1989;40:197–199. doi: 10.4269/ajtmh.1989.40.197. [DOI] [PubMed] [Google Scholar]
- 20.Maurin M, Raoult D. In vitro susceptibilities of spotted fever group rickettsiae and Coxiella burnetii to clarithromycin. Antimicrob Agents Chemother. 1993;37:2633–2637. doi: 10.1128/aac.37.12.2633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Maurin M, Raoult D. Bacteriostatic and bactericidal activity of levofloxacin against Rickettsia rickettsii, Rickettsia conorii, Israeli spotted fever group rickettsiae and Coxiella burnetii. J Antimicrob Chemother. 1997;39:725–730. doi: 10.1093/jac/39.6.725. [DOI] [PubMed] [Google Scholar]
- 22.Munoz Espin T, Lopez Pares P, Espejo Arenas E, Font Creus B, Martinez Vila I, Traveria Casanova J, Segura Porta F, Bella Cueto F. Erythromycin versus tetracycline for treatment of Mediterranean spotted fever. Arch Dis Child. 1986;61:1027–1029. doi: 10.1136/adc.61.10.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Raoult D, Jean-Pastor M J, Xeridat B, Garnier J M, Weiller P J, Garcin G, Privat Y, Gallais H, Casanova P. La fièvre boutonneuse méditrerranéenne. A propos de 154 cas récents. Ann Dermatol Venerol. 1983;110:909–914. [PubMed] [Google Scholar]
- 24.Raoult D, Rousselier P, Galicher V, Perez R, Tamalet J. In vitro susceptibility of Rickettsia conorii to ciprofloxacin as determined by suppressing lethality in chicken embryos and by plaque assay. Antimicrob Agents Chemother. 1986;29:424–425. doi: 10.1128/aac.29.3.424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Raoult D, Gallais H, De Micco P, Casanova P. Ciprofloxacin therapy for Mediterranean spotted fever. Antimicrob Agents Chemother. 1986;30:606–607. doi: 10.1128/aac.30.4.606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Raoult D, Rousselier P, Vestris G, Tamalet J. In vitro susceptibility of Rickettsia rickettsii and Rickettsia conorii as determined by plaque assay and by microplaque colorimetric assay. J Infect Dis. 1987;155:1059–1062. doi: 10.1093/infdis/155.5.1059. [DOI] [PubMed] [Google Scholar]
- 27.Raoult D, Rousselier P, Tamalet J. In vitro evaluation of josamycin, erythromycin, and spiramycin against Rickettsia rickettsii and Rickettsia conorii. Antimicrob Agents Chemother. 1988;32:255–256. doi: 10.1128/aac.32.2.255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Raoult D, Walker D H. Rickettsia rickettsii and other spotted fever group rickettsiae. In: Mandell G L, Gordon R J, Bennett J E, editors. Principles and practice of infectious diseases. 3rd ed. New York, N.Y: Churchill Livingstone; 1990. pp. 1465–1469. [Google Scholar]
- 29.Raoult D, Drancourt M. Antimicrobial therapy of rickettsial diseases. Antimicrob Agents Chemother. 1991;35:2457–2462. doi: 10.1128/aac.35.12.2457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Raoult D, Bres P, Drancourt M, Vestris G. In vitro susceptibilities of Coxiella burnetii, Rickettsia rickettsii, and Rickettsia conorii to the fluoroquinolone sparfloxacin. Antimicrob Agents Chemother. 1991;35:88–91. doi: 10.1128/aac.35.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Raoult D, Brouqui P, Roux V. A new proposed fever group rickettsiosis. Lancet. 1996;348:412. doi: 10.1016/s0140-6736(05)65037-4. [DOI] [PubMed] [Google Scholar]
- 32.Raoult D, Berbis P, Roux V, Xu W, Maurin M. A new tick-transmitted disease due to Rickettsia slovaca. Lancet. 1997;350:112–113. doi: 10.1016/S0140-6736(05)61814-4. [DOI] [PubMed] [Google Scholar]
- 33.Raoult D, Roux V. Rickettsioses as paradigms of new or emerging infectious diseases. Clin Microbiol Rev. 1997;10:694–719. doi: 10.1128/cmr.10.4.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Roux V, Raoult D. Phylogenetic analysis of the genus Rickettsia by 16S rDNA sequencing. Res Microbiol. 1995;146:385–396. doi: 10.1016/0923-2508(96)80284-1. [DOI] [PubMed] [Google Scholar]
- 35.Roux V, Rydkina E, Eremeeva M, Raoult D. Citrate synthase gene comparison, a new tool for phylogenetic analysis, and its application for the rickettsiae. Int J Syst Bacteriol. 1996;47:252–261. doi: 10.1099/00207713-47-2-252. [DOI] [PubMed] [Google Scholar]
- 36.Ruiz Beltran R, Herrero Herrero J I. Evaluation of ciprofloxacin and doxycycline in the treatment of Mediterranean spotted fever. Eur J Clin Microbiol Infect Dis. 1992;11:427–431. doi: 10.1007/BF01961857. [DOI] [PubMed] [Google Scholar]
- 37.Ruiz Beltran R, Herrero Herrero J I. Deleterious effect of trimethoprim-sulfamethoxazole in Mediterranean spotted fever. Antimicrob Agents Chemother. 1992;36:1342–1344. doi: 10.1128/aac.36.6.1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schriefer M E, Sacci J B J, Dumler J S, Bullen M G, Azad A F. Identification of a novel rickettsial infection in a patient diagnosed with murine typhus. J Clin Microbiol. 1994;32:949–954. doi: 10.1128/jcm.32.4.949-954.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shaked Y, Samra Y, Maier M K, Rubinstein E. Relapse of rickettsial Mediterranean spotted fever and murine typhus after treatment with chloramphenicol. J Infect Dis. 1989;18:35–37. doi: 10.1016/s0163-4453(89)93567-6. [DOI] [PubMed] [Google Scholar]
- 40.Stewart R S. Flinders Island spotted fever: a newly recognised endemic focus of tick typhus in Bass Strait. Part 1. Clinical and epidemiological features. Med J Aust. 1991;154:94–99. doi: 10.5694/j.1326-5377.1991.tb120993.x. [DOI] [PubMed] [Google Scholar]
- 41.Tarasevich I V, Makarova V, Stepanov A, Mistkarova E, Balayeva N M, Raoult D. Astrakhan fever: new spotted fever group rickettsiosis. Lancet. 1991;337:172–173. doi: 10.1016/0140-6736(91)90833-b. [DOI] [PubMed] [Google Scholar]
- 42.Telenti A, Imboden P, Marchesi F, Lowrie D, Cole S, Coslton M J, Matter L, Schopfer K, Bodmer T. Detection of rifampicin-resistant mutations in Mycobacterium tuberculosis. Lancet. 1993;341:647–650. doi: 10.1016/0140-6736(93)90417-f. [DOI] [PubMed] [Google Scholar]
- 43.Uchida T, Uchiyama T, Kumano K, Walker D H. Rickettsia japonica sp. nov., the etiological agent of spotted fever group rickettsiosis in Japan. Int J Syst Bacteriol. 1992;42:303–305. doi: 10.1099/00207713-42-2-303. [DOI] [PubMed] [Google Scholar]
- 44.Wike D A, Tallent G, Peacock M G, Ormsbee R A. Studies of the rickettsial plaque assay technique. Infect Immun. 1972;5:715–722. doi: 10.1128/iai.5.5.715-722.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wisseman C L, Jr, Waddell A D, Walsh W T. In vitro studies of the action of antibiotics on Rickettsia prowazekii by two basic methods of cell culture. J Infect Dis. 1974;130:564–574. doi: 10.1093/infdis/130.6.564. [DOI] [PubMed] [Google Scholar]
- 46.Wisseman C L, Jr, Silverman D J, Waddell A, Brown D T. Penicillin-induced unstable intracellular formation of spheroplasts by rickettsiae. J Infect Dis. 1982;146:147–158. doi: 10.1093/infdis/146.2.147. [DOI] [PubMed] [Google Scholar]
- 47.Yagupsky P, Gross E M. Relapse of Israeli spotted fever treated with doxycycline. Trans R Soc Trop Med Hyg. 1985;79:139–140. doi: 10.1016/0035-9203(85)90265-2. [DOI] [PubMed] [Google Scholar]
- 48.Yu X, Fan M, Xu G, Liu Q, Raoult D. Genotypic and antigenic identification of two new strains of spotted fever group rickettsiae isolated from China. J Clin Microbiol. 1993;31:83–88. doi: 10.1128/jcm.31.1.83-88.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]