See article vol. 30: 1364-1375
Endothelial Dysfunction and ASCVD
A growing number of evidence suggests that endothelial dysfunction is associated with cardiovascular events 1 , 2) . Nitric oxide (NO) plays a significant role in the maintenance of vascular endothelial function by inhibiting vasoconstriction, vascular smooth muscle cell proliferation, leukocyte adhesion, and platelet aggregation. As the concept that endothelial dysfunction may be regarded as the integrated risk of the risk factors and serves as a sensitive marker for their functional significance, the development and introduction of novel, cost-effective, noninvasive, and reproducible tests to assess endothelial function may conceivably promote the use of these tests for clinical application and practice 1 , 2) .
L-Arginine/L-Ornithine Ratio and Onset of ASCVD
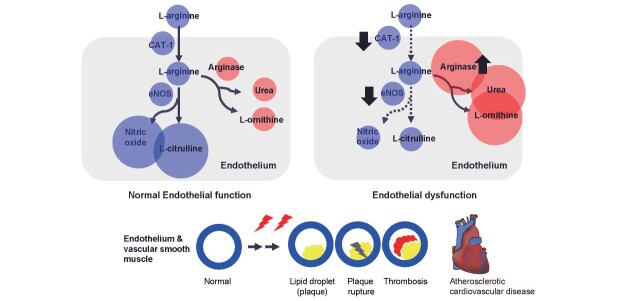
L-arginine has received much interest during the past two decades because of its potential effects on whole-body NO production and the augmentation of NO-dependent signaling pathways. L-arginine is a source of nitrogen, which is converted to NO by eNOS (endothelial NO synthase) and is involved in maintaining vascular function. Therefore, decreased L-arginine use can be involved in vascular endothelial damage owing to NO bioavailability. Even with normal L-arginine levels, vascular endothelial dysfunction may occur and is referred to as “arginine paradox” 3) . The global L-arginine bioavailability ratio (GABR) may be a better predictor of coronary artery disease than L-arginine, but its diagnostic potential has not been examined 4) . Ishinoda et al. reported that the L-arginine/L-ornithine ratio is a predictor of cardiovascular death in this issue 5) . L-arginine concentrations are decreased in the acute critical stage 6) , although L-arginine production is not decreased 7) , suggesting altered L-arginine metabolism. Sepsis and/or altered cytokine states have been reported to activate cationic amino acid transporter-2 (CAT-2), an inhibitor of L-arginine uptake, and deactivate cationic amino acid transporter-1 (CAT-1) 8) , an uptaker of L-arginine. This fact may suggest that iNOS (inducible NOS) transport increases and eNOS transport decreases in the acute critical stage, as Ishinoda discussed 5) . In contrast, in the chronic phase, decreased L-arginine availability may occur. A possible mechanism is an increased arginase activity 9) ( Fig.1 ) . Arginase activity is involved in the metabolism of L-arginine and L-citrulline to L-ornithine and urea, which is conjugated with eNOS action to convert L-arginine and L-citrulline to NO 9 , 10) , and thus it, in turn, may inhibit the utilization of the conversion of L-arginine to NO by eNOS 9 , 10) . CAT-1 can also suppress the conversion utilization of L-arginine to NO by increasing L-arginine 10) . The L-arginine/L-ornithine ratio may indicate the condition of the above metabolic derangement involved in these NO production.
Fig.1. A possible underlying mechanism by which maintenance of L-arginine/L-ornithine ratio is associated with the prevention of atherosclerotic cardiovascular disease.
CAT-1: cationic amino acid transporter- 1; eNOS: endothelial nitric oxide synthase.
Future studies are required to clarify the following: 1) whether the L-arginine/L-ornithine ratio really indicates the above assumption in the clinical setting of endothelial dysfunction, 2) if so, how this marker can be used as a biomarker of the onset of atheoxclerotic cardiovacular disease.
Conflict of Interest
None.
References
- 1).Lerman A, Zeiher AM. Endothelial function. Circulation, 2005; 111: 363-368 [DOI] [PubMed] [Google Scholar]
- 2).Deanfield JE, Halcox JP, Rabelink TJ. Endothelial function and dysfunction. Circulation, 2007; 115: 1285-1295 [DOI] [PubMed] [Google Scholar]
- 3).Bode-Böger SM, Scalera F, Ignarro LJ. The L-arginine paradox: Importance of the L-arginine/asymmetrical dimethylarginine ratio. Pharmacol Ther, 2007; 114: 295-306 [DOI] [PubMed] [Google Scholar]
- 4).Tang WH, Wang Z, Cho L, Brennan DM, Hazen SL. Diminished global arginine bioavailability and increased arginine catabolism as metabolic profile of increased cardiovascular risk. J Am Coll Cardiol, 2009; 53: 2061-207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5).Ishinoda Y, Masaki N, Hitomi Y, Taruoka A, Kawai A, Iwashita M, et al. A low arginine/ornithine ratio is associated with long-term cardiovascular mortality. J Atheroscler Thromb, 2023; 30: 1364-1375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Milewski PJ, Threlfall CJ, Heath DF, Holbrook IB, Wilford K, Irving MH. Intracellular free amino acids in undernourished patients with or without sepsis. Clin Sci (Lond), 1982; 62: 83-91 [DOI] [PubMed] [Google Scholar]
- 7).Argaman Z, Young VR, Noviski N, Castillo-Rosas L, Lu XM, Zurakowski D, et al. Arginine and nitric oxide metabolism in critically ill septic pediatric patients. Crit Care Med, 2003; 31: 591-597 [DOI] [PubMed] [Google Scholar]
- 8).Schwartz D, Schwartz IF, Gnessin E, Wollman Y, Chernichovsky T, Blum M, et al. Differential regulation of glomerular arginine transporters (CAT-1 and CAT-2) in lipopolysaccharide-treated rats. Am J Physiol Renal Physiol, 2003; 284: F788-795 [DOI] [PubMed] [Google Scholar]
- 9).Bahadoran Z, Mirmiran P, Kashfi K, Ghasemi A. Endogenous flux of nitric oxide: Citrulline is preferred to Arginine. Acta Physiol (Oxf), 2021; 231: e13572 [DOI] [PubMed] [Google Scholar]
- 10).Caldwell RB, Toque HA, Narayanan SP, Caldwell RW. Arginase: an old enzyme with new tricks. Trends Pharmacol Sci, 2015; 36: 395-405 [DOI] [PMC free article] [PubMed] [Google Scholar]