Abstract
Background
One of the core aims of the European Union of Medical Specialists is to harmonize training across Europe by creating European Training Requirements for all medical specialties including Ophthalmology. The theoretical part is already defined by the EBO, however as ophthalmology also includes surgical skills, we herein propose a surgical minimum curriculum for ophthalmology residents in Europe.
Methods
National and international ophthalmic training curricula which are publicly available in English were reviewed and compared. The final proposal was created from 5 criteria: 1. Disease prevalence; 2. Patient safety; 3. Case-trainee ratio; 4. Skill transfer; and 5. Technical difficulty.
Results
In total 7 different training curricula from across the world were compared. Among the surgical procedures, cataract surgery has the highest median number of procedures required to be completed during residency: 86 procedures (50–350). Followed by oculoplastics: 28 procedures (10–40) and panretinal photocoagulation: 27.5 procedures (10–49) Full procedural competence is proposed in 9 surgical skills, including YAG laser posterior capsulotomy, retinal argon laser, intravitreal injection, corneal foreign body removal, removal of corneal sutures, facial and periocular laceration repair, eyelid laceration repair, minor eyelid procedures, and punctal occlusion. These procedures are deemed essential and feasible for all ophthalmology residents in Europe to perform independently upon completion of their training.
Conclusion
This proposal should be regarded as a recommendation based on comparable surgical curricula in use worldwide to establish standards across European countries and may serve as valuable insight to those responsible for compiling ETRs for ophthalmology, or their national curriculums.
Subject terms: Education, Health occupations
Introduction
The European Union (EU) is a political and economic integration of 27 member states that guarantees the free movement of its citizens across state borders within the Union [1]. This partnership not only permits cross-border access to healthcare for patients in different Member States of the EU, it also enables any healthcare providers to practice in any one of the Member States once they have attained the qualification in their home country [1]. The European Parliament and the Council of the EU have previously listed 3 values as being the most important across the whole Europe: universality, equity, and solidarity [2]. Beneath these overarching values, there is also a set of operating principles that are shared across the EU. These include good quality healthcare and a systematic approach to ensuring patient safety, the latter of which include the training for health professionals [3]. These values were reaffirmed in a later EU directive on the application of patients’ rights in cross-border healthcare in 2011 [3]. Citizens within the EU should be assured that the doctors they see have acquired a standard level of knowledge and skills, irrespective of the EU nation in which the doctor received their training [2].
However, there is much heterogeneity in post-graduate training of doctors across the EU. In recognition of this challenge for standardisation, the European Union of Medical Specialists (UEMS) adopted a Charter on Post Graduate Training which aimed to provide the recommendations at European level for good medical training [4], while not superseding the national authorities’ competence in defining the content of postgraduate training in their own state. To create harmonisation of the training standards, UEMS had set a goal to create European Training Requirements (ETR) [4].
To date, more than 50 European Training Requirements (ETR) documents, in subspecialities from Anaesthesiology to Vascular surgery have been adopted by the UEMS Council, detailing the theoretical knowledge, clinical skill competencies and assessments for the resident, as well as guidance on delivery of these for the mentor [4, 5].
In UEMS Section for Ophthalmology, a working group known as the European Board of Ophthalmology (EBO) was formed in 1992 [4], charged specifically with overseeing the standards of training and to guarantee in every country of the EU a high level of quality and the highest possible level of training of the candidate specialists. An ETR for European Ophthalmology has yet to be established. While the EBO has organized an annual diploma examination (EBOD) since 1995, this examination is focused on the assessment of fundamental knowledge deemed necessary for an ophthalmologist [6], but does not assess clinical skills including the ability to perform basic ophthalmic surgical procedures to a safe and competent level.
Recently, a survey of European ophthalmology residents has determined that there is great heterogeneity in the surgical training opportunities and experiences among early career ophthalmologists in the EU [7]. In some European countries, residents do not perform any procedures, and over 40% indicated that they were unsatisfied with their surgical training during residency [7]. According to the survey results, many final year residents did not perform phacoemulsification surgery (34%), pterygium excision (46.9%), or repair of eyelid laceration (31.3%). There were only 11 European countries where residents performed 50 phacoemulsification surgeries or more during their entire residency period: Belgium, France, Greece, Hungary, Israel, Malta, Netherlands, Portugal, Spain, Turkey and United Kingdom [7].
In concordance with the missions of UEMS and EBO, it is evident that there is a need for the standards of residency training among European programs to be harmonized, including surgical training, so that the values of EU Health Systems can be upheld. In this paper, we review different ophthalmology residency training curricula from across the world, and after taking into consideration disease prevalence in each nation, patient safety, case-trainee ratio, skills transfer, and technical difficulty, and on the basis of this information, we have proposed a minimum surgical curriculum for residency training in Europe.
Methodology
In 2018, under the direction of the European Society of Ophthalmology Young Ophthalmologists (SOE YO) committee, a steering committee consisting of the authors of this article was formed to assess the issue of heterogeneity of European ophthalmology residency training. National and international ophthalmic training curricula that were publicly available in English language were reviewed. Details of the surgical training required, including the list of procedures, the levels of competency, and the minimum number of cases required as stipulated by these curricula were compared in order to develop a shortlist of surgical skills applicable to all European residents irrespective of national borders. Additionally, we performed a comprehensive survey of a cohort of current and recently graduated European ophthalmology residents, members of the EBO and ICO, and ophthalmic educators from around the globe, to further help inform the curriculum development.
During the development of this shortlist of surgical skills, the following aspects were considered to ensure that the skills included are relevant to the needs of the European patient population:
Disease Prevalence – is there a significant surgical caseload of the condition across different parts of Europe?
Patient Safety – is it safe for the patient that a resident ophthalmologist performs the surgical procedure, either independently or under an appropriate level of supervision?
Case-Trainee Ratio – is it possible for all European residents to obtain the necessary surgical experience during their training?
Skills Transfer – can the procedure be mastered using surgical skills acquired in another procedure?
Technical Difficulty – how easy would it be for a trainee to attain an appropriate level of competence for the surgical procedure?
After a list of basic surgical skills were compiled, the training outcome (i.e., a level of competence that a resident ophthalmologist should reach by the end of their residency training) was assigned based on a consensus drawn from the national and international curricula and finally determined by the steering committee.
The 3 levels of competences used were:
Full competence: the resident is capable of completing the entire procedure, including the pre- and post-operative evaluation and management, without supervision.
Supervised competence: the resident is capable of completing the entire procedure, but must be done under the supervision of an ophthalmologist so that the latter could take over the procedure, in order to prevent or manage complications if necessary.
Assistant: the resident can actively assist an ophthalmologist during the procedure.
Results
In total, seven training curricula were identified and reviewed. These included: the International Council of Ophthalmology Training Curriculum (ICO) [8]; the Irish College of Ophthalmologists Curriculum: Specialist Training in Surgical Ophthalmology [9]; the Royal College of Ophthalmologists (United Kingdom) Curriculum for Ophthalmic Specialist Training (RCOPH) [10]; the Objectives of Training in the Specialty of Ophthalmology by the Royal College of Physicians and Surgeons of Canada [11]; the All India Ophthalmological Society National Curriculum for Ophthalmology Residency Training (AIOS) [12]; the Pan-America Association of Ophthalmology (PAAO) [13]; and the United States Accreditation Council for Graduate Medical Education (ACGME) Program Requirements and Case Log Information in Ophthalmology (US) [14].
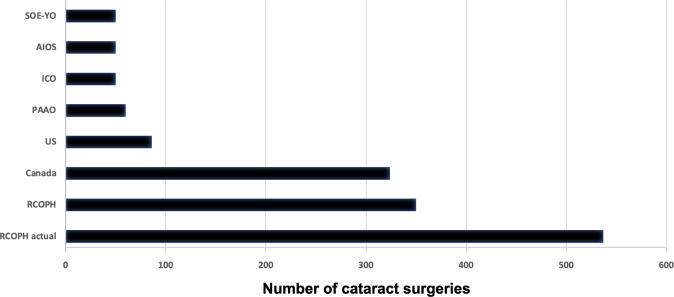
Table 1 summarizes the basic surgical skills and their respective requirements according to six of the seven different national and international curricula. Due to the differences between the curricula, a number of eyelid procedures were combined in the category of oculoplastic procedures to allow better comparison. The requirements for cataract, glaucoma and strabismus surgeries were detailed in all the curricula. In contrast, pterygium surgery and corneal transplantations were only described in 1 (i.e.,, Canada) and 2 (i.e.,, RCOPH and AIOS) curricula, respectively. Recently, RCOPH increased the surgical case numbers performed overall by trainees, being much higher than the minimum requirement from 2009–2015 [15]. Thus, we included both RCOPH curricula in Table 1, adding “RCOPH-actual” as an additional column to inform about numbers requested in the most recent curriculum. Among the surgical procedures, cataract surgery has the highest median number of procedures required to be completed during residency (86 procedures, range 50–350), followed by oculoplastics (28 procedures, range 10–40) and panretinal photocoagulation (27.5 procedures, range 10–49). Looking into the differences between the various curricula, the most intensive surgical training is given in UK, Ireland and Canada. Those curricula describe the need of performing more than 300 cataract surgeries (Fig. 1), more than 30 strabismus surgeries and 9 or more of glaucoma surgical procedures. US, AIOS, PAAO and ICO are most aligned towards describing a less surgical training profile compared to the previous curricula. They all require less than 100 cataract surgeries to be performed by the resident (Fig. 1), and 10 or less strabismus and glaucoma surgeries. The Irish College of Ophthalmologists curriculum is not part of Table 1, since it divides its surgical training into basic and higher levels, with emphasis on trainer-verified competency level and logbook over case numbers alone, which makes comparisons more difficult.
Table 1.
Basic surgical skills and their respective requirements according to six of the seven different national and international curricula compared in this manuscript.
| Procedure | Canada | US min | ICO Min | RCOPH | RCOPH Actual (median) | AIOS | PAAO | MEDIAN (RANGE) | SOE YO |
|---|---|---|---|---|---|---|---|---|---|
| Cataract | 324 | 86 | 50 | 350 | 537 | 50 | 60 phaco 5 ECCE | 86 (50–537) | 50 |
| Glaucoma (filtering/shunt) | 9 | 5 | 10 | 30# | 51 | 5 | 10 | 10 (5–51) | |
| Strabismus (horizontal muscles) | 48 | 10 | 10 | 20 | 32 | 5 | 10 | 10 (5–32) | 10 |
| Oculoplastic (lid laceration, chalazion, entropion, ectropion, ptosis) | 10–49 | 28 | 20 | 40 | 97 | n/a | n/a | 28 (20–97) | 50 |
| Laser – Yag Capsulotomy | 10–49 | 5 | 5 | 2 | n/a | n/a | 5 | 5 (2–25) | FC |
| Laser Trabeculoplasty | 10–49 | 5 | 5 | 8 | n/a | n/a | n/a | 5 (4–25) | 20 |
| Laser iridotomy | 10–49 | 4 | 5 | n/a | n/a | n/a | 15 (2–25) | ||
| Laser PRP | 10–49 | 20 | 10 | 40 | 140 | n/a | 30 | 27.5 (10–140) | FC |
| Focal Laser DR | n/a | 5 | 5 | n/a | n/a | n/a | 5 (5) | ||
| Intravitreal injection | 10–49 | n/a | 20 | 2 | n/a | n/a | n/a | 15 (5–25) | FC |
| Vitrectomy | 0–4 | n/a | n/a | 20 assist | n/a | 2 assist | n/a | n/a | assist |
| Pterygium (basic) | 5–9 | n/a | n/a | n/a | n/a | n/a | n/a | n/a | 10 |
| Globe trauma | n/a | 4 | n/a | 2 | n/a | 2 | n/a | n/a | 3 |
| Corneal transplant | n/a | n/a | n/a | 6 assist | 9 | 2 assist | n/a | n/a | n/a |
All numbers are numbers of procedures that the resident should minimum perform during their residency in the stated curriculum. For calculation of median using the Canadian range 10–49 we have used 25. US United States of America, (ACGME), ICO International Council of Ophthalmology, RCOPH The Royal College of Ophthalmologists, AIOS All India Ophthalmological Society, PAAO Pan-American Association of Ophthalmology, SOE-YO European Society of Ophthalmology’s Young Ophthalmologist, n/a not available, FC Full competence.
Fig. 1. Disparities in surgical case numbers of cataract performed during training according to the analysed curricula.
US United States of America (ACGME), ICO International Council of Ophthalmology, RCOPH The Royal College of Ophthalmologists, AIOS All India Ophthalmological Society, PAAO Pan-American Association of Ophthalmology, SOE-YO European Society of Ophthalmology’s Young Ophthalmologist.
The SOE YO steering committee propose a minimum training requirement that European ophthalmology residents should attain by the end of their residency, and this includes a minimum set of basic surgical competences as shown in Table 2. These were selected by the steering committee based upon the 5 criteria outlined in the method section. The minimum set of procedures are categorized into laser procedures, injections, and surgical procedures for cornea, cataract, oculoplastics, glaucoma, strabismus, trauma, retina and keratorefractive surgery. Full procedural competence is required in 9 basic surgical skills, including YAG laser capsulotomy, retinal argon laser (except macular laser), intravitreal injection, corneal foreign body removal, removal of corneal sutures, facial and periocular wound repair, eyelid laceration repair (without canalicular involvement), minor eyelid procedures, and punctal occlusion. All of these procedures are deemed essential and feasible for all ophthalmology residents in Europe to perform independently upon completion of their training. The disease for which these procedures are required are frequently encountered in the EU, the procedures themselves are of relatively low-risk, and so trainee supervision is possible whilst maintaining patient safety, and skill attainment to a high level of competency can be achieved with relatively few cases.
Table 2.
The SOE YO steering committee’s suggestion for a minimum training requirement that European ophthalmology residents should attain by the end of their residency.
| Full competence | Supervised primary surgeon | Assistant | |
|---|---|---|---|
| Laser | |||
| YAG laser capsulotomy | X | ||
|
Glaucoma lasers: - YAG laser iridotomy - Selective Laser Trabeculoplasty - Cyclodiode laser |
n = 20 | ||
|
Retinal argon lasers: - Panretinal photocoagulation - Laser for retinal breaks |
X | ||
| Macular laser for diabetic retinopathy (focal/grid laser) | X | ||
| Injections | |||
|
Ocular anaesthesia: - Peribulbar - Retrobulbar - Subtenon - Subconjunctival |
n = 10 | ||
| Intravitreal injection | X | ||
| Cornea | |||
| Anterior chamber paracentesis | X | ||
| Corneal foreign body removal | X | ||
| Conjunctival suturing | X | ||
| Removal of corneal sutures | X | ||
| Simple pterygium excision | n = 10 | ||
| Complicated Pterygium surgery (e.g., recurrent, large) | X | ||
| Corneal biopsy | X | ||
| EDTA chelation for calcific band keratopathy | X | ||
|
Corneal transplantation: - Penetrating (PKP) - Anterior lamellar (ALK) - Endothelial (DSEK/DMEK) |
X | ||
| Cataract | |||
| Phacoemulsification – basic | n = 50 | ||
| Phacoemulsification – complex | X | ||
| Oculoplastics | |||
| Facial and periocular wound repair | X | ||
| Eyelid laceration repair (no canalicular involvement) | X | ||
|
Minor eyelid procedures - Incisional biopsy - Excisional biopsy - Shave excision of eyelid lesion - Epilation of lashes - Incision and drainage of lesion |
X | ||
|
Basic adnexal procedures - Blepharoplasty - Brow ptosis repair - Entropion/ectropion repair - Wedge excision of eyelid lesion - Temporal artery biopsy |
n = 50 | ||
| Nasolacrimal duct probing ± placement of lacrimal stents | X | ||
| Punctal occlusion (temporary or permanent) or insert plugs | X | ||
| Ptosis | X | ||
| Enucleations/ evisceration | X | ||
| Botulinum-toxin skin injections | X | ||
| Glaucoma | |||
| Trabeculectomy/ aqueous shunt | X | ||
| Strabismus | |||
| Strabismus surgery | n = 10 | ||
| Trauma | |||
|
Globe rupture repair - Corneal laceration - Corneoscleral laceration - Scleral laceration or rupture - Globe perforation |
n = 3 | ||
| Retina | |||
| Vitreous aspiration biopsy | X | ||
| Retinal detachment | X | ||
|
Pars plana vitrectomy procedure - Retinal detachment repair - Retinal membrane peel |
X | ||
| Keratorefractive Surgery | |||
| LASIK/LASEK/PTK/PRK/SMILE | X | ||
There is no minimum number of procedures for both Full Competence and Assistant, so in these procedures we have just made a cross (X) to indicate the column. n number of pro cedures.
In total, 7 surgical skills were assigned a training requirement, including basic adnexal procedures and phacoemulsification cataract surgery (50 cases each). These were also included in Table 1 to allow comparisons. The training requirement recommended by the SOE YO steering committee are based upon those mandated by the 7 national and international training curriculums used in this paper.
A number of surgical skills require subspecialist training after residency before basic proficiency can be achieved, yet it remains important for residents to develop an understanding of the procedure. Examples include retinal detachment repair or corneal transplantation. The training recommendation by the SOE YO steering committee is the experience of assisting in such procedures.
Discussion
In this paper, we reviewed and compared 7 different training curricula from across the world. After surveying expert educators worldwide and European ophthalmology trainees, and after taking into consideration the disease prevalence in EU nations, patient safety during surgical training of residents, case-trainee ratio, ease of skills transfer from mentor to resident, and technical difficulty of each procedure, we proposed a minimum basic surgical curriculum for ophthalmology residents training in the European Union.
As highlighted by UEMS and EBO, there is a need in ophthalmology for a surgical training curriculum, in order to facilitate the harmonization of training standards across Europe. An often cited case against training standardization is the historical diversity of training within Europe, and important differences in cultural traditions, practice patterns, and training resources across the continent [16]. Indeed, our recent publication on European ophthalmology training has shown great disparities in training experiences among residents [7]. Nevertheless, it is important to ensure the highest quality of patient care and patient safety consistently across EU nations [2, 3]. Many other medical and surgical subspecialties have already successfully adopted EU-wide training standards and established systems for training accreditation [17–31]. Ophthalmology has always been at the forefront of innovation and should join the other specialties in embracing training harmonization, with the aim to enhance training standards and ultimately improve patient safety across the EU.
Our paper focuses on surgical training, as we have found this to be the area with the most contrasting training experience among European trainees [7]. We reviewed 7 surgical national and international curricula and consulted a medical educationist in the field, before proposing a minimum basic surgical curriculum. The goal of having a basic surgical skill curriculum is to elevate the overall surgical competence across Europe and reduce the differences in exposure to surgical training, giving trainees equal access to training and increasing patients’ access to safe and effective eyecare. As shown in Table 1, our proposal is comparable to other established curricula in scope, procedure numbers, and definitions of competence. To avoid being overly ambitious, we purposedly included only the core surgical skills that are essential for any given resident to independently practice comprehensive ophthalmology within the EU upon completion of residency training. We hope this will ease the adoption of this proposed curriculum even in countries where training resources are less abundant.
In Europe, the most common method of cataract extraction is phacoemulsification, a procedure that requires dedicated supervised training to attain surgical competence, yet many newly qualified European ophthalmologists have never performed any steps let alone a full case of cataract surgery by the end of their residency training [7, 32]. We propose a minimum number of 50 completed cases of phacoemulsification under supervision, which would allow newly qualified comprehensive ophthalmologists to be competent in independently managing cataract surgery patients in the community. Crucially, previous studies have shown that the complication rate among residents who have performed between 50 and 250 cataract surgeries is around 0.8%, which is generally considered to be an acceptable level of training benefit-risk ratio. Our proposed surgical requirement should be regarded as the absolute minimum instead of a training cap, as even lower rates of complications could be reached once the residents have completed 250 to 350 cases [33–37]. It is not unusual for ophthalmology residents outside the EU to emerge from their training programs with ≥ 250 completed cases [38], a level of experience in line with the opinion of the European residents [7]. However, it should be noted that large differences exist in the national number of residents in each European country, and with the low mentor/mentee ratio means that this may not allow for uniform phacoemulsification training of all residents with completion of the proposed number of cases.
Simulation training is an important adjunct of surgical training - it allows trainees to practice basic microsurgical manoeuvres and can reduce unnecessary complications upon transition to surgery in patients [39]. Simulation models commonly available for ophthalmic purposes include animal tissue model, life-size artificial eye model, and virtual reality platform (e.g., EyeSi simulator). Many comparisons have been drawn in the training of ophthalmic surgeons and airline pilots. Indeed, the aviation industry is often regarded as setting the standards in simulation training, the introduction of which has dramatically reduced flight accidents [40]. However, surgical simulation has some important limitations. Many EU ophthalmology residents, especially those in regions that are resource-lacking do not have ready access to these models or devices. Furthermore, while the acquisition of new technical skills could be greatly facilitated, the non-technical aspect of perioperative ophthalmic care such as communication, leadership or handling of stress during complicated surgery are less well served by our current simulation models [40]. It is notable that the accreditation of airline pilots requires many hours of practical training under supervision, and only a portion of which can be completed by flight simulation [41]. Similarly, we believe simulation training should not be a replacement for hands-on surgical experience in residency training, and that the transition to real-life surgery should be done during residency in a supervised setting to ensure patient safety.
Conclusion
Considering all the differences in EU member countries, there is an urgent need for an ETR for ophthalmology to be established to ensure standardization of patient care across the EU. The ETR should not be a law, but a recommendation that member states will normally follow by developing their national curricula over time. Additionally, creation of an ETR will further create a more common platform to enter into fellowships/subspecialist training in continental Europe. Here, we suggest a minimum surgical curriculum for the ETR in ophthalmology in Europe, based upon established standard curricula from across the world. Through the harmonisation of theoretical knowledge as well as surgical skills, we hope the ever-expanding European ophthalmic community will improve the basic training, producing better trained ophthalmologists to ensure that our patients across the continent benefit from safer and better ophthalmic care in the future.
Summary
What was known before
The European Union of Medical Specialists aims to harmonize medical training across Europe, including ophthalmology.
There is an urgent need for a European Training Requirements for ophthalmology to be established to ensure standardization of patient care across the EU.
What this study adds
A surgical minimum curriculum has been proposed for ophthalmology residents based on a review of 7 national and international training curricula.
The proposal includes full procedural competence in 9 essential surgical skills, with the highest median number of procedures required being cataract surgery.
The proposal is based on comparable curricula worldwide and serves as a recommendation for establishing standards across European countries.
Acknowledgements
Marko Hawlina for support and guidance.
Author contributions
All authors (MG, SF, JP, JC, AK, CQ, RP, AS, MR) have participated in the steering committee formed to assess the issue of heterogeneity of European ophthalmology residency training. The steering committee worked under the European Society of Ophthalmology Young Ophthalmologists (SOE YO) committee lead by MR. All authors (MG, SF, JP, JC, AK, CQ, RP, AS, MR) have taken part in developing and analysing the results. MG, SF, and MR wrote the initial manuscript. All authors have contributed and commented on the final manuscript.
Funding
JC: Employee, Roche Products Ltd, UK. SF: Consultant for Santen, US; Research support from Dompè, US. MR: Consultant for Santen Denmark. All other authors have no financial disclosures to declare.
Data availability
All data generated or analysed during this study are included in this published article.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.European Parliament and the Council of the European Union. EUR-Lex - 32005L0036 - EN - EUR-Lex [Internet]. Official Journal of the European Union. 2005 [cited 2022 Feb 16]. https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=celex%3A32005L0036
- 2.European Parliament and the Council of the European Union. Council conclusions on common values and principles in European Union Health Systems. J Eur Union. 2006;146:1–3. [Google Scholar]
- 3.European Parliament and the Council of the European Union. Directive 2011/24/EU of the European Parliament and of the Council of 9 March 2011 on the application of patients’ rights in cross-border healthcare. J Eur Union. 2011;88:45–65. [Google Scholar]
- 4.Union E, Medical OF Charter on training of medical specialists in the european community charter adopted by the Management Council of the UEMS, October 1993 [Internet]. 1993 [cited 2022 Feb 16]. https://www.uems.eu/__data/assets/pdf_file/0011/1415/906.pdf
- 5.UEMS. European Standards in Medical Training - UEMS ETRs [Internet]. www.uems.eu. 2022 [cited 2022 Aug 9]. Available from: https://www.uems.eu/areas-of-expertise/postgraduate-training/european-standards-in-medical-training
- 6.Mathysen DGP, Aclimandos W, Roelant E, Wouters K, Creuzot-Garcher C, Ringens PJ, et al. History and future of the European Board of Ophthalmology Diploma examination. Acta Ophthalmol [Internet] 2013;91:589–93. doi: 10.1111/j.1755-3768.2012.02422.x. [DOI] [PubMed] [Google Scholar]
- 7.Anaya-Alaminos R, Rassmussen ML, Fung SSM, Potic J, González-Andrades M Comparative Analysis of European Residency Programs: Benchmarking and Harmonizing Ophthalmology Training in Europe. Eye (Lond). 2023;37:725–31. [DOI] [PMC free article] [PubMed]
- 8.ICO. Residency - International Council of Ophthalmology [Internet]. [cited 2022 Jul 22]. Available from: https://icoph.org/education/residency/
- 9.Irish College of Ophthalmologists RM. Curriculum Specialist Training in Surgical Ophthalmology [Internet]. Pdf. 2021 [cited 2022 Jul 22]. p. 1–58. Available from: https://www.eyedoctors.ie/medium/images/ICO_Specialist_Training_in_Surgical_Ophthalmology_Curriculum-d.pdf
- 10.The Royal College of Ophthalmologists. Curriculum for Ophthalmic Specialist Training [Internet]. [cited 2022 Jul 22]. Available from: https://curriculum.rcophth.ac.uk/curriculum/ost/
- 11.The Royal College of Physicians and Surgeons of Canada. Objectives of Training in the Specialty of Ophthalmology | © 2015 The Royal College of Physicians and Surgeons of Canada. [Internet]. [cited 2022 Jul 22]. Available from: https://www.royalcollege.ca/rcsite/documents/ibd/ophthalmology-otr-e
- 12.Grover AK, Honavar SG, Azad R, Verma L. A national curriculum for ophthalmology residency training. Indian J Ophthalmol. 2018;66:752–83. doi: 10.4103/ijo.IJO_327_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.PAAO. Requisitos Recomendados por la PAAO para el Programa de Residencia Médica en Oftalmología. 2013.
- 14.Accreditation Council for Graduate Medical Education (ACGME). ACGME Program Requirements for Graduate Medical Education in Ophthalmology. 2022.
- 15.Hoffman J, Spencer F, Ezra D, Day AC. Changes in UK ophthalmology surgical training: analysis of cumulative surgical experience 2009–2015. BMJ Open. 2017;7:e018526. doi: 10.1136/bmjopen-2017-018526.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cimberle M. Lack of standardization, insufficient surgical training take toll on development of European young ophthalmologists. Halio Ophtalmology [Internet]. 2016 [cited 2022 Aug 7]; Available from: https://www.healio.com/news/ophthalmology/20160815/lack-of-standardization-insufficient-surgical-training-take-toll-on-development-of-european-young-op.
- 17.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists - European Training Requirements for the Specialty of Plastic, Reconstructive and Aesthetic Surgery [Internet]. 2015. Available from: www.uems.eu.
- 18.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists- European Training Requirements for Breast Surgery [Internet]. 2015. Available from: www.uems.eu.
- 19.UEMS. European Training Requirements in Obstetrics and Gynaecology UEMS Section Obstetrics and Gynaecology / European Board and College of Obstetrics and Gynaecology Standing Committee on Training and Assessment. 2018.
- 20.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists - Section of surgery, division of transplantation. European training requirements in transplantation surgery. [Internet]. 2018. Available from: www.uems.eu
- 21.UEMS. European Training Requirements for Pediatric Surgery European Standards of Postgraduate Medical Specialist Training Preamble. 2020.
- 22.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists Training Requirements in Orthopaedics & Traumatology [Internet]. 2017. Available from: www.uems.net
- 23.UEMS. European Training Curriculum for Radiology [Internet]. 2014. Available from: https://www.uems.eu/_data/assets/pdf_file/0018/72270/UEMS-2018.37-European-Training-Requirements-in-Radiology.pdf
- 24.UESM. Union Européenne des Médecins Spécialistes European union of medical specialists - Training Requirements for the Competency of Rare and Undiagnosed Diseases [Internet]. 2020. Available from: www.uems.eu
- 25.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists -Training Requirements for the Specialty of Geriatric Medicine [Internet]. 2020. Available from: https://www.who.int/ageing/publications/health-workforce-ageing-populations.pdf.
- 26.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists - European Union of Medical Specialists section and board og vaskular surgery training requrements section and board of vaskular surgery. [Internet]. 2021. Available from: www.uemsvascular.com.
- 27.UEMS. European Training Requirements for the Specialty of General Surgery. 2021.
- 28.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists - Training Requirements for the Specialty of Neurological Surgery [Internet]. 2021. Available from: www.uems.eu
- 29.UEMS. European Requirements for Training in Neonatology [Internet]. 2021. Available from: www.newborn-health-standards.org
- 30.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists - european Training requrements for Neurology. 2022.
- 31.UEMS. Union Européenne des Médecins Spécialistes European union of medical specialists -Training Requirements for the Specialty of Endocrine surgery [Internet]. 2022. Available from: www.uems.eu
- 32.Muttuvelu DV, Andersen CU. Cataract surgery education in member countries of the European Board of Ophthalmology. Can J Ophthalmol [Internet] 2016;51:207–11. doi: 10.1016/j.jcjo.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 33.Bell CM, Hatch WV, Cernat G, Urbach DR. Surgeon volumes and selected patient outcomes in cataract surgery: a population-based analysis. Ophthalmology. 2007;114:405–10. doi: 10.1016/j.ophtha.2006.08.036. [DOI] [PubMed] [Google Scholar]
- 34.Randleman JB, Wolfe JD, Woodward M, Lynn MJ, Cherwek DH, Srivastava SK. The resident surgeon phacoemulsification learning curve. Arch Ophthalmol. 2007;125:1215–9. doi: 10.1001/archopht.125.9.1215. [DOI] [PubMed] [Google Scholar]
- 35.Rutar T, Porco TC, Naseri A. Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmology. 2009;116:431–6. doi: 10.1016/j.ophtha.2008.10.028. [DOI] [PubMed] [Google Scholar]
- 36.Puri S, Kiely AE, Wang J, Woodfield AS, Ramanathan S, Sikder S. Comparing resident cataract surgery outcomes under novice versus experienced attending supervision. Clin Ophthalmol. 2015;9:1675–81. doi: 10.2147/OPTH.S85769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gupta S, Haripriya A, Vardhan SA, Ravilla T, Ravindran RD. Residents’ Learning Curve for Manual Small-Incision Cataract Surgery at Aravind Eye Hospital, India. Ophthalmology. 2018;125:1692–9. doi: 10.1016/j.ophtha.2018.04.033. [DOI] [PubMed] [Google Scholar]
- 38.Ho J, Claoué C. Cataract skills: how do we judge competency? J R Soc Med. 2013;106:2–4. doi: 10.1177/0141076813476412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McCannel CA. Simulation Surgical Teaching in Ophthalmology. Ophthalmology. 2015;122:2371–2. doi: 10.1016/j.ophtha.2015.08.036. [DOI] [PubMed] [Google Scholar]
- 40.Rasmussen RC, Grauslund J, Vergmann AS. Simulation training in vitreoretinal surgery: A systematic review. BMC Ophthalmol. 2019;19:90.. doi: 10.1186/s12886-019-1098-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Federal Aviation Administration. Pilot Certification and Qualification Requirements for Air Carrier Operations. 2013 [cited 2022 Jul 22]; Available from: https://www.faa.gov/regulations_policies/rulemaking/recently_published/media/2120-aj67.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analysed during this study are included in this published article.